Abstract
Isocitrate dehydrogenases (IDHs) catalyse oxidative decarboxylation of isocitrate to α-ketoglutarate (α-KG). IDH1 functions in the cytosol and peroxisomes, whereas IDH2 and IDH3 are both localized in the mitochondria. Heterozygous somatic mutations in IDH1 occur at codon 132 in 70% of grade II–III gliomas and secondary glioblastomas (GBMs), and in 5% of primary GBMs. Mutations in IDH2 at codon 172 are present in grade II–III gliomas at a low frequency. IDH1 and IDH2 mutations cause both loss of normal enzyme function and gain-of-function, causing reduction of α-KG to D-2-hydroxyglutarate (D-2HG) which accumulates. Excess hydroxyglutarate (2HG) can also be caused by germline mutations in D- and L-2-hydroxyglutarate dehydrogenases (D2HGDH and L2HGDH). If loss of IDH function is critical for tumourigenesis, we might expect some tumours to acquire somatic IDH3 mutations. Alternatively, if 2HG accumulation is critical, some tumours might acquire somatic D2HGDH or L2HGDH mutations. We therefore screened 47 glioblastoma samples looking for changes in these genes. Although IDH1 R132H was identified in 12% of samples, no mutations were identified in any of the other genes. This suggests that mutations in IDH3, D2HGDH and L2HGDH do not occur at an appreciable frequency in GBM. One explanation is simply that mono-allelic IDH1 and IDH2 mutations occur more frequently by chance than the bi-allelic mutations expected at IDH3, D2HGDH and L2HGDH. Alternatively, both loss of IDH function and 2HG accumulation might be required for tumourigenesis, and only IDH1 and IDH2 mutations have these dual effects.
Introduction
Gliomas are the most common primary brain tumour, accounting for 70% of all primary central nervous system neoplasms. They show wide diversity with respect to location, morphology, genetic status and response to therapy.
Grade I gliomas occur more in children than in adults, are generally curable with complete surgical resection and rarely evolve into higher-grade lesions. WHO grade II or III gliomas are invasive, progress to higher-grade lesions and have a poor outcome. Glioblastoma (GBM), the most common and most malignant glioma, has a very poor prognosis and may develop rapidly without evidence of a less malignant precursor lesion (primary glioblastoma), or less commonly through progression from a lower grade tumour (secondary glioblastoma) [1], [2].
Isocitrate dehydrogenases (IDHs) catalyse the oxidative decarboxylation of isocitrate to α-ketoglutarate (α-KG) and reduce NAD+ or NADP+ to NADH or NADPH. IDH1 and IDH2 are homodimeric, NADP+-dependent enzymes that share considerable sequence similarity and an almost identical protein structure [3]. IDH3 is a heterotetramer composed of two α, one β and one γ subunit. IDH3 is a NAD+-dependent enzyme. IDH1 is localised to the cytoplasm and peroxisomes, it is highly expressed in the liver and to a lesser level in other tissues [4]. As well as being involved in catalysing the conversion of isocitrate to α-KG, IDH1 is thought to play a role in cellular metabolic processes such as lipid and glucose metabolism [5], [6], and has been shown to be involved in cellular defence against reactive oxygen species and radiation [7], [8], [9].
IDH2 is localised to the mitochondria, is highly expressed in heart, muscle, activated lymphocytes and moderately in other tissues [4]. IDH2 plays a key role in the regulation of the tricarboxylic acid cycle (TCA) and like IDH1, has been shown to have a protective role against insults such as oxidative stress [9], [10], [11].
IDH3 is also localised to the mitochondria and plays a central role in the TCA cycle.
In 2008, a genome-wide sequencing study identified somatic mutations in IDH1 in 18 (12%) of 149 patients with GBM [12] and it was subsequently found that GBMs without IDH1 mutations often have mutations affecting IDH2 [13]. Both IDH1 and IDH2 mutations are more frequent in grade II-III gliomas and secondary glioblastoma (70–75%) than in primary glioblastoma (5%) [14], are present at higher frequencies in younger patients, and are associated with a relatively favourable prognosis [13], [15]. IDH1 and IDH2 mutations are mono-allelic, somatic, missense changes. Mutations in IDH1 almost always affect R132, which is the binding site for isocitrate [12]. Mutations in IDH2 exclusively affect R172 and R140; the former of these arginines is analogous to IDH1 R132 [13] [16].
Initial investigations demonstrated that mutated IDH1 had a reduced affinity for isocitrate [17]. Furthermore, expression of mutant IDH1 in cultured cells has been shown to reduce the formation of the enzyme products, α-KG and NADPH [13], [17], [18]. These structural and biochemical findings suggested that IDH mutation results in loss of function, the most plausible mechanism being a dominant negative effect through the formation of catalytically inactive heterodimers of mutant and wild type proteins [17]. Deficiency of α-KG might lead to defective function of α-KG-dependent enzymes such as HIF prolyl hydroxylases.
Subsequent evidence has emerged suggesting that mutant IDH1 and IDH2 are not simply inactive enzymes, but instead possess novel enzymatic activity [16], [19], [20]. Dang et al. demonstrated that mutant, but not wild type, IDH1 catalyses the reduction of α-KG to D-2HG while converting NADPH to NADP+. D-2HG accumulates in glioblastoma cells with IDH1 R132H mutations [19]. The role of 2HG in tumourigenesis is unclear, although it may act as an oncometabolite, perhaps competitively inhibiting α-KG-dependent enzymes [21] [22]. One of the rationales for a role of 2HG in tumour formation is derived from the observation of patients suffering from hereditary 2-hydroxyglutaric aciduria. This is a rare inherited metabolic disorder, caused by homozygous inactivating germline 2-hydroxyglutarate dehydrogenase (2HGDH) mutations, that is weakly associated with brain tumours.
If IDH loss-of-function alone is critical for tumourigenesis, we might expect IDH3 mutations to occur in brain tumours, including those sub-types with relatively low frequencies of IDH1 and IDH2 mutations. Alternatively, if accumulation of 2HG alone is critical, we might expect mutations in D2HGDH and/or L2HGDH. A further, more speculative line of reasoning is that, if patients with mutations in IDH1 and IDH2 have normal D2HGDH and L2HGDH function, excess 2HG should simply be converted back to α-KG by 2HGDH. The failure of this to occur might be due to saturation of the 2HGDH enzymes, but raises the possibility that patients with IDH1 and IDH2 mutations might also require inactivating mutations in D2HGDH and L2HGDH for 2HG to accumulate.
We therefore analysed a set of GBM for mutations in IDH1, IDH2, IDH3, D2HGDH and L2HGDH.
Results and Discussion
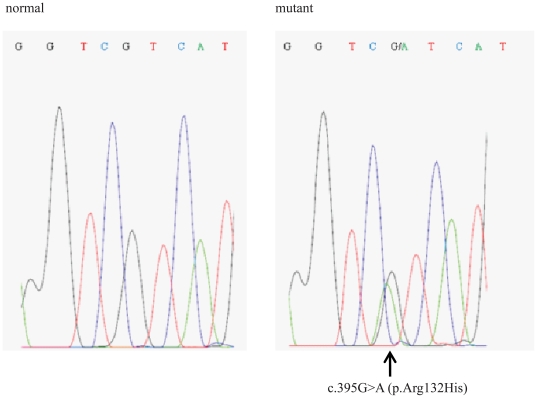
We studied 47 glioblastomas (WHO grade IV). Heterozygous mutations of IDH1 were found in 6/47 tumours (12%). All 6 mutations were single base substitutions c.395G>A occurring at residue R132, resulting in an arginine to histidine (p.R132H) substitution (Figure 1). This frequency is consistent with previously described data. No mutations were found in IDH2, in keeping with the lower frequency of such changes than mutations in IDH1. We sequenced all the exons of IDH3A, IDH3B and IDH3G, which encode the α, β, and γ subunits of the IDH3 heterotetramer, and all the exons of D2HGDH and L2HGDH. In all cases examined we did not find any mutations. Known SNPs were found within each gene (details not shown).
Figure 1. Identification of the G395A mutation at codon 132 by sequence analysis of the IDH1 gene.
The electropherogram shows a representative example of the heterozygous, single base G-to-A substitution at nucleotide position 395 of the IDH1 gene (right panel) and the corresponding wild-type sequence (left panel). The mutation was detected in 6 out of 47 glioblastomas analyzed.
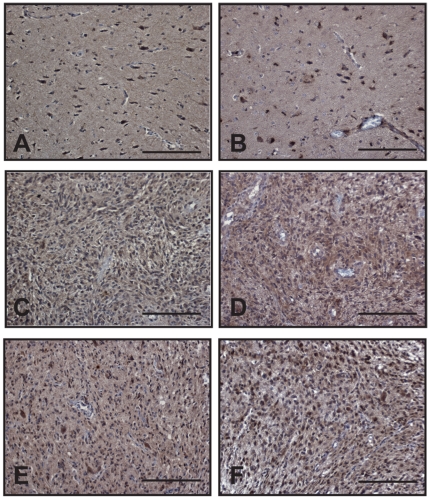
We then wondered whether D2HGDH or L2HGDH might be inactivated by other mechanisms such as promoter methylation or miRNA over-expression. We therefore evaluated the expression of the corresponding proteins in human glioblastomas samples (Figure 2). D2HGDH and L2HGDH were detected in GBMs carrying wild type IDH1 and IDH2 genes, as well as in IDH1-mutants tumours. It is highly unlikely that the loss of D2HGDH or L2HGDH expression plays an important role in the pathogenesis of human GBMs.
Figure 2. D2HGDH and L2HGDH are expressed in wildtype IDH1/2 and IDH1 R132H glioblastomas.
Expression of D2HGDH and L2HGDH in normal brain is shown respectively in panels A and B. D2HGDH and L2HGDH were detected in brain tumour samples carrying either wild-type IDH1/IDH2 (C and D) or mutated IDH1 allele (E and F) by immunohistochemistry. Scale bar represents 50 µm in all panels.
Mutations in IDH3, D2HGDH and L2HGDH (or loss of expression of the 2HGDHs) do not therefore occur at an appreciable frequency in GBM. One explanation is simply that mono-allelic IDH1 and IDH2 mutations occur more frequently by chance than the bi-allelic mutations expected at IDH3, D2HGDH and L2HGDH. Alternatively, both loss of IDH function and 2HG accumulation are required for tumourigenesis, and only IDH1 and IDH2 mutations have these dual effects. It is also possible that 2HG accumulation is an epiphenomenon and that IDH3 loss-of-function does not lead to sufficient deficiency of α-KG to promote tumourigenesis. There might also be an unknown mechanism of tumourigenesis that is specific to defects in IDH1 or IDH2.
Moreover our data suggest that in patients with mutations of IDH1 and IDH2 and normal D2HGDH and L2HGDH function, the excess 2HG is not converted back to α-KG by 2HGDH, perhaps due to the saturation of the latter enzyme. A recent report identified heterozygous germline IDH2 mutations in patients with idiopathic D-2-hydroxyglutaric aciduria, carrying no mutations in D2HGDH and consistently increased D-2HG levels in body fluids [23]; interestingly, the patient did not develop brain tumours.
The mechanisms by which IDH1 and IDH2 mutations cause tumourigenesis remain largely unclear, as do the putative alternative functional deficiencies in IDH-wildtype gliomas. However, even if 2HG has no direct pathogenic role it has potential as a specific marker of IDH1 or IDH2 mutations, to diagnose or monitor IDH-mutant glioma [24].
Materials and Methods
Sample collection
All brain tumours were obtained from the neuropathology department at The Royal Free Hospital, Hampstead, London. All 47 samples analysed were confirmed to be WHO grade IV glioblastoma. We have worked solely on anonymously samples. Study of these has been approved by Oxfordshire REC B 05/Q1605/66.
DNA extraction
DNA was extracted from paraffin embedded samples using DNeasy Blood and Tissue from QuiagenR (Alameda, CA), following the manufacturer's instructions.
Sequencing analysis
Mutation screening of each gene was performed by direct sequencing of genomic DNA in forward and reverse orientations using the Applied Biosystems BigDye terminator reaction kit and the AB 3730xl sequencing machine (Applied Biosystems, Foster City, CA). Primer sequences were designed to encompass the coding region and splice sites of exon 4 of IDH1 and IDH2, and all exons of IDH3A (RefSeq: NM_005530.2), IDH3B (RefSeq: NM_174855.1), IDH3G (RefSeq: NM_004135.2 for the transcript variant 1 and RefSeq: NM_174869.1 for the transcript variant 2), L2HGH (RefSeq: NM_024884.2) and D2HGDH (RefSeq: NM_024884.2). Primer sequences and PCR conditions are available on request.
Immunohistochemistry
Formalin-fixed, paraffin-embedded tissue sections (4 µm) were de-waxed in xylene and rehydrated through graded alcohols to water. Endogenous peroxidase was blocked using 1.6% H2O2 for 20 minutes. For antigen retrieval, sections were pressure cooked in 10 mmol/L citrate buffer (pH6.0) for 5 minutes. Sections were blocked with 10% serum for 30 minutes. Slides were incubated with primary polyclonal antibodies anti human D2HGDH (ProteinTech Group, Chicago, IL 60612, 1∶50), or anti human L2HGDH (ProteinTech Group, Chicago, IL 60612, 1∶100) for 1 hour. Goat anti-rabbit secondary antibody was applied for one hour at room temperature. Sections were then incubated in ABC (Vector labs) for 30 minutes. DAB solution was applied for 2–5 minutes and development of the colour reaction was monitored microscopically. Slides were counterstained with haematoxylin, dehydrated, cleared and then mounted. Images were taken at 20× magnification.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work was supported by Oxford Comprehensive Biomedical Core (BRC), the charity Mothers and Daughters, the University College London Hospitals, Experimental Cancer Medicine Centre, and a core centre grant from the Wellcome Trust (075491/Z/04). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
References
- 1.Ohgaki H. Epidemiology of brain tumours. Methods Mol Biol. 2009;472:323–342. doi: 10.1007/978-1-60327-492-0_14. [DOI] [PubMed] [Google Scholar]
- 2.Wen PY, Kesari S. Malignant gliomas in adults. N Engl J Med. 2008;359:492–507. doi: 10.1056/NEJMra0708126. [DOI] [PubMed] [Google Scholar]
- 3.Xu X, Zhao J, Xu Z, Peng B, Huang Q, et al. Structures of human cytosolic NADP-dependent isocitrate dehydrogenase reveal a novel self-regulatory mechanism of activity. J Biol Chem. 2004;279:33946–33957. doi: 10.1074/jbc.M404298200. [DOI] [PubMed] [Google Scholar]
- 4.Reitman ZJ, Yan H. Isocitrate dehydrogenase 1 and 2 mutations in cancer: alterations at a crossroads of cellular metabolism. J Natl Cancer Inst. 2010;102:932–941. doi: 10.1093/jnci/djq187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haselbeck RJ, McAlister-Henn L. Function and expression of yeast mitochondrial NAD- and NADP-specific isocitrate dehydrogenases. J Biol Chem. 1993;268:12116–12122. [PubMed] [Google Scholar]
- 6.Joseph JW, Jensen MV, Ilkayeva O, Palmieri F, Alarcon C, et al. The mitochondrial citrate/isocitrate carrier plays a regulatory role in glucose-stimulated insulin secretion. J Biol Chem. 2006;281:35624–35632. doi: 10.1074/jbc.M602606200. [DOI] [PubMed] [Google Scholar]
- 7.Minard KI, McAlister-Henn L. Dependence of peroxisomal beta-oxidation on cytosolic sources of NADPH. J Biol Chem. 1999;274:3402–3406. doi: 10.1074/jbc.274.6.3402. [DOI] [PubMed] [Google Scholar]
- 8.Lee SM, Park SY, Shin SW, Kil IS, Yang ES, et al. Silencing of cytosolic NADP(+)-dependent isocitrate dehydrogenase by small interfering RNA enhances the sensitivity of HeLa cells toward staurosporine. Free Radic Res. 2009;43:165–173. doi: 10.1080/10715760802653661. [DOI] [PubMed] [Google Scholar]
- 9.Lee SH, Jo SH, Lee SM, Koh HJ, Song H, et al. Role of NADP+-dependent isocitrate dehydrogenase (NADP+-ICDH) on cellular defence against oxidative injury by gamma-rays. Int J Radiat Biol. 2004;80:635–642. doi: 10.1080/09553000400007680. [DOI] [PubMed] [Google Scholar]
- 10.Kil IS, Kim SY, Lee SJ, Park JW. Small interfering RNA-mediated silencing of mitochondrial NADP+-dependent isocitrate dehydrogenase enhances the sensitivity of HeLa cells toward tumour necrosis factor-alpha and anticancer drugs. Free Radic Biol Med. 2007;43:1197–1207. doi: 10.1016/j.freeradbiomed.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 11.Yang ES, Park JW. Regulation of ethanol-induced toxicity by mitochondrial NADP(+)-dependent isocitrate dehydrogenase. Biochimie. 2009;91:1020–1028. doi: 10.1016/j.biochi.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 12.Parsons DW, Jones S, Zhang X, Lin JC, Leary RJ, et al. An integrated genomic analysis of human glioblastoma multiforme. Science. 2008;321:1807–1812. doi: 10.1126/science.1164382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, et al. IDH1 and IDH2 mutations in gliomas. N Engl J Med. 2009;360:765–773. doi: 10.1056/NEJMoa0808710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kloosterhof NK, Bralten LB, Dubbink HJ, French PJ, van den Bent MJ. Isocitrate dehydrogenase-1 mutations: a fundamentally new understanding of diffuse glioma? Lancet Oncol. 2010 doi: 10.1016/S1470-2045(10)70053-X. [DOI] [PubMed] [Google Scholar]
- 15.Hartmann C, Meyer J, Balss J, Capper D, Mueller W, et al. Type and frequency of IDH1 and IDH2 mutations are related to astrocytic and oligodendroglial differentiation and age: a study of 1,010 diffuse gliomas. Acta Neuropathol. 2009;118:469–474. doi: 10.1007/s00401-009-0561-9. [DOI] [PubMed] [Google Scholar]
- 16.Ward PS, Patel J, Wise DR, Abdel-Wahab O, Bennett BD, et al. The common feature of leukemia-associated IDH1 and IDH2 mutations is a neomorphic enzyme activity converting alpha-ketoglutarate to 2-hydroxyglutarate. Cancer Cell. 2010;17:225–234. doi: 10.1016/j.ccr.2010.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhao S, Lin Y, Xu W, Jiang W, Zha Z, et al. Glioma-derived mutations in IDH1 dominantly inhibit IDH1 catalytic activity and induce HIF-1alpha. Science. 2009;324:261–265. doi: 10.1126/science.1170944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ichimura K, Pearson DM, Kocialkowski S, Backlund LM, Chan R, et al. IDH1 mutations are present in the majority of common adult gliomas but rare in primary glioblastomas. Neuro Oncol. 2009;11:341–347. doi: 10.1215/15228517-2009-025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dang L, White DW, Gross S, Bennett BD, Bittinger MA, et al. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature. 2009;462:739–744. doi: 10.1038/nature08617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gross S, Cairns RA, Minden MD, Driggers EM, Bittinger MA, et al. Cancer-associated metabolite 2-hydroxyglutarate accumulates in acute myelogenous leukemia with isocitrate dehydrogenase 1 and 2 mutations. J Exp Med. 2010;207:339–344. doi: 10.1084/jem.20092506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Figueroa ME, Abdel-Wahab O, Lu C, Ward PS, Patel J, et al. Leukemic IDH1 and IDH2 mutations result in a hypermethylation phenotype, disrupt TET2 function, and impair hematopoietic differentiation. Cancer Cell. 2010;18:553–567. doi: 10.1016/j.ccr.2010.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu W, Yang H, Liu Y, Yang Y, Wang P, et al. Oncometabolite 2-Hydroxyglutarate Is a Competitive Inhibitor of alpha-Ketoglutarate-Dependent Dioxygenases. Cancer Cell. 2011;19:17–30. doi: 10.1016/j.ccr.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kranendijk M, Struys EA, van Schaftingen E, Gibson KM, Kanhai WA, et al. IDH2 mutations in patients with D-2-hydroxyglutaric aciduria. Science. 2010;330:336. doi: 10.1126/science.1192632. [DOI] [PubMed] [Google Scholar]
- 24.Dang L, Jin S, Su SM. IDH mutations in glioma and acute myeloid leukemia. Trends Mol Med. 2010;16:387–397. doi: 10.1016/j.molmed.2010.07.002. [DOI] [PubMed] [Google Scholar]