Abstract
This study sought to evaluate the extent to which the pain coping profiles observed by Walker and colleagues [28] in a sample of patients with chronic abdominal pain also were evident in a sample of adolescent patients who presented to a tertiary care clinic for evaluation of a variety of diverse pain conditions. In addition, we aimed to evaluate the relation of these pain coping profiles to patients’ emotional and physical functioning. Participants (n = 254) were adolescent patients aged 12–17 years. Patients completed the Pain Response Inventory (PRI) as well as measures of pain, somatic symptoms, anxiety and depressive symptoms, and functional disability. Using the PRI classification algorithm developed by Walker and colleagues [28], we successfully classified all the patients in our sample. We also found that the pain coping profiles successfully differentiated among patients with different levels of symptoms, disability, and emotional distress, further demonstrating the external validity of these profiles. Results have implications for tailoring pain treatment interventions to patients’ particular coping profiles.
Keywords: Chronic pain, Coping, Adolescents
1. Introduction
The Pain Response Inventory (PRI) is a multidimensional questionnaire that assesses children’s coping with chronic abdominal pain [17,31,32]. In their recent review of pediatric pain coping instruments, Blount and colleagues [2] classified the PRI as a well-established instrument that expands the literature on children’s coping with pain. Previous research has demonstrated that the PRI is useful in predicting how children’s pain experiences influence their functioning; for example, passive coping strategies – which involve orientation away from the stressor and include responses such as catastrophizing and disengagement – have been associated with higher levels of pain, somatic and depressive symptoms [11,32], and disability [11,31]. In contrast, accommodative coping strategies that involve efforts to accept or adapt to the stressor (including acceptance and self-encouragement) have been associated with decreases in pain [32] and depressive symptoms [31].
In the initial PRI validation, structural equation modeling supported a hierarchical classification of coping strategies in which the 13 subscales loaded on three higher order factors labeled Active, Passive, and Accommodative Coping. However, Walker and colleagues [32] noted that several subscales loaded on more than one higher order factor suggesting that specific coping strategies may serve different functions depending on the circumstances. For example, the finding that pain catastrophizing loaded on both the Passive and Active factor, is consistent with the notion that catastrophizing can function as passive disengagement or an active strategy when used in conjunction with support-seeking (cf. [27]). Recently, Walker and colleagues [28] used cluster analytic techniques to identify PRI profiles that summarize the pain coping activities of patients with chronic abdominal pain (cf. [26]). These profiles described distinct and meaningful patterns of coping associated with different levels of emotional and physical distress. For example, patients labeled Avoidant Copers responded to pain with catastrophizing and activity disengagement and were characterized by high levels of depressive symptoms and disability. Dependent Copers also catastrophized about their pain but sought social support to cope with their pain and were characterized by somewhat lower levels of depression and disability than Avoidant Copers. Similarly, Self-Reliant Copers, who frequently relied on accommodative coping strategies such as acceptance and self-encouragement, had relatively lower levels of depressive symptoms and disability compared to both Dependent and Avoidant Copers. Engaged Copers, characterized by higher levels of distraction and social support-seeking, also had lower levels of depressive symptoms and disability, representing a more resilient response to pain.
The purpose of this study was to assess whether the pain coping typology developed by Walker and colleagues [28] on a sample of patients with abdominal pain also would successfully classify the coping strategies of patients with diverse pain complaints. In addition, we sought to evaluate the relation of these coping profiles to patients’ emotional and physical functioning to better understand patterns of coping activity that may mediate the relation between pain and health outcomes. Finally, we aimed to examine whether different pain diagnoses were differentially associated with particular pain coping profiles.
2. Methods
2.1. Participants
Potential study participants included all patients aged 12–17 years, with at least three months duration of chronic pain who underwent a multidisciplinary pain evaluation at a tertiary pain clinic at Children’s Hospital Boston between October 2004 and October 2006.
Of the 524 patients seen by the Pain Treatment Service during this time, 124 did not meet the age range criterion (12–17 years). Thirty-eight patients did not meet the 3-month pain duration criterion. In addition, 108 patients were ineligible due to missing, incomplete, or invalid questionnaire data. No differences were found between patients with missing data and those with complete data in terms of the child’s age or gender. Only one patient refused to complete the questionnaires.
The total sample included 254 patients who were primarily Caucasian (90.7%) and female (76.8%), reflective of the population of children seen in this tertiary care clinic setting. The mean age was 14.69 years (SD = 1.49). Participants’ primary medical diagnoses included headaches (33.7%; including migraine, tension-type headache, combined and daily chronic headache), neuropathic pain (24.8%; including complex regional pain syndrome and neuralgia), musculoskeletal pain (21.5%; including scoliosis, idiopathic pain, juvenile rheumatoid arthritis and hypermobility syndromes), abdominal pain (11.8%; including functional abdominal pain and inflammatory bowel disease), diffuse pain (4.5%; including fibromyalgia or description of pain in three or more areas without a clear etiology), and other pain (3.7%; e.g., chest, ear, bladder). At the time of the evaluation, patients’ mean duration of pain was greater than two years, M = 27.83 months (SD = 30.34, range = 3–154 months).
Family Socioeconomic Status (SES) based on the four-factor index of social status [9] ranged from 21 (semi-skilled workers) to 66 (business owner; professional), with a mean of 49.87 (minor professional; technical), SD = 10.95. The majority of mothers (84.4%) and fathers (78.4%) completed post-high school education.
2.2. Measures
2.2.1. Pain coping strategies
The Pain Response Inventory (PRI) [32] is a 60-item self-report questionnaire that assesses children’s responses to pain. The PRI comprises 13 subscales that describe a response to pain. Responses range from never (0) to always (4), with higher scores indicating greater use of a pain coping response. Mean scores are computed for each subscale. In the current study, the two subscales that are specific to children with abdominal pain (Condition-Specific Strategies and Massage/Guard) were eliminated from analyses. The PRI has demonstrated validity and reliability [32]. In the current study, with the exception of a single subscale (Rest, alpha = .69), coefficient alpha levels of the subscales ranged from .74 to .94.
2.2.2. Functional disability
The Functional Disability Inventory (FDI) [5,30] assesses children’s self-reported difficulty in physical and psychosocial functioning in the past two weeks due to their physical health. The FDI consists of 15 items concerning perceptions of activity limitations. Responses range from no trouble (0) to impossible (4). Total scores are computed by summing the items. Higher scores indicate greater disability. The FDI has demonstrated reliability and validity [5,30]; alpha reliability for the current sample was .89.
2.2.3. Somatic symptoms
The Children’s Somatization Inventory (CSI) [8,29] assesses the severity of nonspecific somatic symptoms (e.g., “weakness,” “dizziness”) that need not have organic disease etiology [29]. Respondents rate the extent to which they have experienced each of the 35 symptoms during the last two weeks using a 5-point scale ranging from not at all (0) to a whole lot (4). Higher scores indicate higher levels of somatic symptoms; total scores are computed by summing the items. The CSI has been found to have adequate reliability and validity [29]. Alpha reliability in the current sample was .87.
2.2.4. Symptoms of anxiety
The revised children’s manifest anxiety scale (RCMAS) [21,22] is a 37-item questionnaire that assesses symptoms of anxiety. Respondents rate whether they have experienced each item with a yes/no scale, dummy-coded as “0” or “1”. Total anxiety scores are calculated by summing all items with the exception of the Lie scale items and are converted to T-scores. Higher scores indicate higher levels of anxiety symptoms. The RCMAS is a well-validated and reliable measure of anxiety for children and adolescents [21,22]. Alpha reliability in the current sample was .88.
2.2.5. Symptoms of depression
The children’s depression inventory (CDI) [15,16] contains 27 self-report items representing depressive symptoms. Items are rated on a 3-point scale from 0 to 2 and summed to obtain a total score that was converted to a T-score. Higher scores indicate higher levels of depressive symptoms. The CDI has been found to have adequate reliability and validity [25]. Alpha reliability in this sample was .87.
2.2.6. Pain intensity
As part of the semi-structured interview with the clinical psychologist, children were asked to provide their current pain rating on a standard 11-point numeric rating scale from 0 (no pain) to 10 (most pain possible).
2.2.7. Basic demographic information
Parents provided the basic demographic information (e.g., child’s age and gender, parents’ occupations, education, and marital status) on the Pain Treatment Service Demographic Information form.
2.3. Procedure
Approval from the hospital’s Institutional Review Board was obtained prior to conducting the retrospective chart review. All the questionnaires were mailed to families prior to the child’s multidisciplinary pain clinic evaluation. Parents and children were asked to complete the questionnaires individually and return them on the date of the evaluation. If parents and children had not completed the questionnaires prior to the appointment, they were asked to do so when they arrived for their evaluation. Children then underwent evaluation by a physician, physical therapist, and clinical psychologist. All questionnaires were reviewed by the psychologist prior to the clinical interview. Patients’ pain diagnoses, assigned by a pain management physician during the multidisciplinary evaluation, were obtained from a review of their medical records.
3. Results
3.1. Replication and comparison of coping profiles
Using the PRI classification algorithm developed by Walker and colleagues [28], we analyzed whether study participants could be classified into the same coping profiles (see Walker et al. [28] for a complete description of the statistical procedures used). The algorithm used in both studies can be used to classify participants in other studies using the PRI; SPSS syntax is available from the last author).
All the 254 patients in this study were successfully classified into the coping profiles derived by Walker and her colleagues [28]. Using frequency analyses, comparison of the percentage of patients in each coping cluster of our sample to those in the original sample [28] showed that patients in both samples were similarly distributed across each profile: our sample comprised 15% Avoidant Copers (vs. 10% in the original sample); 22% Dependent Copers (vs. 19%), 12% Engaged Copers (vs. 19%), 28% Infrequent Copers (vs. 30%), and 3% Inconsistent Copers (vs. 4%). The one exception was the higher percentage of Self-Reliant Copers in the current sample (23% vs. 14%). Due to the small number of patients classified as Inconsistent Copers (n = 8), we eliminated these patients from further analyses.
3.2. Characterization of coping profiles
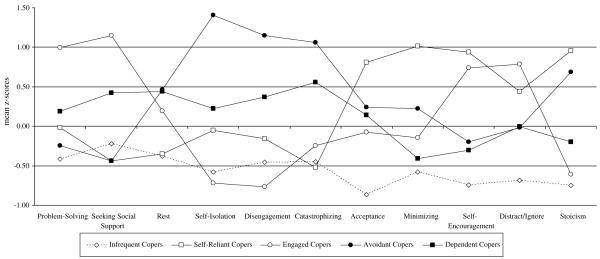
We next conducted ANOVAs to compare the profile groups on individual PRI subscales (see Table 1) as well as on reports of pain, disability, somatic symptoms, and emotional functioning (see Table 2). Post hoc examination of significant between-groups differences in individual PRI subscale scores, pain, disability, somatic symptoms, or emotional functioning employed Bonferroni corrections for multiple comparisons. Each post hoc test examined means between five coping profiles (Avoidant, Dependent, Engaged, Infrequent, and Self-Reliant), so the Bonferroni-adjusted alpha rate was .005, which maintained a family-wise alpha level of .05 for each analysis. Statistical comparisons are reported in the tables and are described below. Additionally, z-scores for each coping strategy were calculated in the total sample and are displayed, by coping profile, in Fig. 1. The use of standardized scores in Fig. 1 simplifies the identification of relative peaks and valleys which represent the most and least frequently used strategies for each coping profile group.
Table 1.
PRI subscale means and standard deviations by coping cluster
| Total (n = 246) | F | p | Avoidant copers (n = 37) |
Dependent copers (n = 54) |
Self-reliant copers (n = 57) |
Engaged copers (n = 29) |
Infrequent copers (n = 69) |
|
|---|---|---|---|---|---|---|---|---|
| Problem solving | 2.45 (.83) | 13.53 | .00 | 2.25 (.69)a,b | 2.61 (.72)b | 2.44 (.78)a,b | 3.28 (.65)c | 2.11 (.82)a |
| Seeking social support | 1.71 (.94) | 23.77 | .00 | 1.29 (.80)a | 2.11 (.74)b | 1.29 (.77)a | 2.79 (.71)c | 1.50 (.91)a |
| Rest | 2.26 (.78) | 10.55 | .00 | 2.62 (.71)b | 2.60 (.60)b | 1.98 (.74)a | 2.41 (.76)a,b | 1.96 (.79)a |
| Self-isolation | 1.11 (1.06) | 52.87 | .00 | 2.60 (.92)a | 1.35 (.82)b | 1.06 (.93)b | .35 (.55)c | .50 (.63)c |
| Disengagement | .90 (.79) | 33.77 | .00 | 1.81 (.72)a | 1.19 (.61)b | .78 (.72)c | .29 (.46)d | .54 (.61)c.d |
| Catastrophizing | 1.40 (.85) | 33.87 | .00 | 2.30 (.78)a | 1.87 (.62)b | .96 (.68)c | 1.19 (.75)c | 1.02 (.65)c |
| Acceptance | 1.85 (.91) | 36.88 | .00 | 2.07 (.92)a | 1.98 (.70)a | 2.59 (.74)b | 1.78 (.75)a | 1.06 (.61)c |
| Minimizing | 1.16 (1.01) | 37.06 | .00 | 1.39 (.95)a | .75 (.66)b | 2.19 (.98)c | 1.02 (.88)a,b | .57 (.60)b |
| Self-encouragement | 2.10 (.95) | 49.75 | .00 | 1.91 (.85)a | 1.81 (.59)a | 2.99 (.62)b | 2.81 (.80)b | 1.39 (.74)c |
| Distract/Ignore | 2.20 (.86) | 20.20 | .00 | 2.18 (.83)a | 2.19 (.74)a | 2.57 (.75)a,b | 2.87 (.65)b | 1.61 (.74)c |
| Stoicism | 1.71 (1.00) | 59.06 | .00 | 2.40 (.65)a | 1.51 (.70)b | 2.67 (.74)a | 1.10 (.83)b,c | .96 (.70)c |
Note. Within rows, means with different subscripts differ significantly at p < .005.
Table 2.
Means and standard deviations for psychosocial characteristics in the total sample and in each cluster
| Total (n = 246) | F | p | Avoidant copers (n = 37) |
Dependent copers (n = 54) |
Self-reliant copers (n = 57) |
Engaged copers (n = 29) |
Infrequent copers (n = 69) |
|
|---|---|---|---|---|---|---|---|---|
| Pain | 4.20 (2.96) | 1.75 | .14 | 4.11 (2.76)a | 4.30 (2.83)a | 4.85 (3.01)a | 4.55 (2.97)a | 3.51 (3.05)a |
| Disability | 21.30 (11.78) | 3.92 | .00 | 23.89 (10.15)a,b | 24.91 (11.97)b | 19.82 (10.17)a,b | 22.93 (12.65)a,b | 17.64 (12.33)a |
| Symptoms | 26.92 (15.31) | 6.14 | .00 | 35.42 (18.02)a | 27.80 (14.91)a,b | 28.25 (14.05)a | 27.43 (14.05)a,c | 20.17 (13.04)c |
| Depression | 50.75 (11.62) | 19.98 | .00 | 62.49 (12.73)a | 52.27 (10.18)b | 50.96 (10.96)b,c | 43.59 (7.98)c | 46.07 (8.84)c |
| Anxiety | 47.96 (12.13) | 15.40 | .00 | 57.61 (9.60)a | 52.54 (12.10)a,b | 47.65 (11.13)b,c | 40.69 (11.89)c | 42.67 (9.31)c |
Note. Within rows, means with different subscripts differ significantly at p < .005.
Fig. 1.
Standardized scores for coping strategies characterizing each coping profile.
3.2.1. Avoidant Copers
This cluster of 37 patients (15% of the sample) had elevations on the self-isolation, disengagement, and stoicism subscales with a significant decline on the seeking social support subscale, indicating that these patients typically responded to pain by isolating themselves and discontinuing their activities, as well as attempting to hide their feelings from others. Indeed, they reported significantly more self-isolation than any other group. They also reported significantly higher levels of pain catastrophizing than any other group. Patients in the Avoidant Copers group reported significantly higher levels of depression than any other group of patients.
3.2.2. Dependent Copers
In this group of 54 patients (22% of the sample), catastrophizing was a frequent response to pain, although the level of catastrophizing was significantly lower than for Avoidant Copers. Compared to the Avoidant Copers, Dependent Copers used significantly more support-seeking and significantly less self-isolation and activity disengagement. Dependent Copers reported levels of disability and somatic symptoms as high as those reported by Avoidant Copers. However, Dependent Copers reported significantly lower levels of depressive symptoms than Avoidant Copers.
3.2.3. Self-Reliant Copers
The most frequent coping strategies used by this group of 57 patients (23% of the sample) were accommodative strategies including Self-Encouragement, Acceptance, and Minimization. Their scores on these strategies were significantly higher than those for both Avoidant and Dependent Copers. Compared to Avoidant and Dependent Copers, they also reported significantly less frequent resting, disengagement, and catastrophizing. Self-Reliant Copers had the highest scores of all groups on stoicism. Self-Reliant Copers did not differ significantly from Avoidant and Dependent Copers with respect to disability and somatic symptoms. However, Self-Reliant Copers had significantly lower levels of depressive symptoms and anxiety than Avoidant Copers.
3.2.4. Engaged Copers
Patients in this cluster (n = 29; 12% of the sample) reported significantly higher levels of problem-solving and seeking social support than patients in any other cluster. They also reported significantly higher levels of self-encouragement and distraction than all but the Self-Reliant Copers. Their level of depressive symptoms was significantly lower than those for Avoidant, Dependent, and Self-Reliant Copers. Finally, Engaged Copers reported significantly lower levels of anxiety than Avoidant and Dependent Copers.
3.2.5. Infrequent Copers
This cluster represented the largest number of patients (n = 69; 28% of the sample) and was characterized by low scores on the majority of PRI subscales, indicating that patients in this group did not typically use any of the pain coping strategies assessed by the PRI. Infrequent Copers reported lower levels of pain, disability, and somatic symptoms than any other group. They also reported relatively low levels of anxiety and depression.
3.3. Demographic characteristics of the coping profiles
Table 3 presents the demographic characteristics of the five coping profile groups. Descriptive statistics were conducted to examine means and standard deviations for patients’ ages and pain duration. One-way ANOVAs were then computed to examine whether patients’ age and pain duration differed by pain diagnosis. Frequency analyses were calculated to examine the percentage of parents with post-high school education, and omnibus chi-square analyses were then conducted to compare whether the percentage of parents with post-high school education differed by pain diagnosis. To compare the percentage of females in each pain coping profile, we conducted an omnibus chi-square analysis with 15 follow-up chi-square analyses, each of which compared the gender breakdown of two clusters (e.g., Infrequent vs. Avoidant, Infrequent vs. Dependent, Avoidant vs. Dependent, etc.). There were no significant differences in age, pain duration, or parental education across profile groups. Pain duration did not differ significantly across groups and exceeded years in all groups. Parents of the majority of patients had a post-high school education. More than two-thirds of all groups were female; nonetheless, there were significant gender differences, with a significantly greater proportion of girls classified as Self-Reliant Copers (84.2%) and Engaged Copers (89.7%) than Infrequent Copers (68%) and Dependent Copers (68.5%).
Table 3.
Demographic characteristics by cluster
| Total (n = 246) |
Avoidant copers (n = 37) |
Dependent copers (n = 54) |
Self-reliant copers (n = 57) |
Engaged copers (n = 29) |
Infrequent copers (n = 69) |
|
|---|---|---|---|---|---|---|
| Child age Mean (SD) | 14.69 (1.49) | 15.03 (1.44)a | 14.59 (1.60)a | 14.91 (1.33)a | 14.52 (1.55)a | 14.48 (1.50)a |
| Child sex Percentage female | 76.8% | 83.8%a,b | 68.5%a | 84.2%b | 89.7%b | 68.1%a |
| Child pain duration in months Mean (SD) |
27.83 (30.34) | 31.56 (28.78)a | 34.26 (35.71)a | 28.19 (34.83)a | 18.10 (19.66)a | 24.72 (25.29)a |
| Fathers with post-high school education Percentage |
78.4% | 75.0%a | 81.6%a | 88.2%a | 80.8%a | 68.7%a |
| Mothers with post-high school education Percentage |
84.4% | 83.3%a | 78.4%a | 89.1%a | 92.7%a | 82.1%a |
Note. Within rows, means or percentages with different subscripts differ significantly at p < .05.
Table 4 presents the pain diagnosis by cluster groupings. Frequency analyses were used to examine the number and percentage of patients with each diagnosis and coping profile. We also used a one-way ANOVA to examine whether patients’ coping cluster groups differed as a function of their pain diagnosis for all diagnoses other than diffuse or other pain, as these groups had too few patients for meaningful comparisons. We found no differences in patients’ coping profiles as a function of their pain diagnoses.
Table 4.
Pain Diagnosis By Cluster (N, %)
| Total (n = 246) |
Avoidant copers (n = 37) |
Dependent copers (n = 54) |
Self-reliant copers (n = 57) |
Engaged copers (n = 29) |
Infrequent copers (n = 69) |
|
|---|---|---|---|---|---|---|
| Diffuse pain | 11, 4.5 | 1, 9.1 | 4, 36.4 | 2, 18.2 | 1, 9.1 | 4, 36.4 |
| Headache | 83, 33.7 | 13, 15.7 | 20, 24.1 | 17, 20.5 | 4, 4.8 | 29, 34.9 |
| Abdominal Pain | 29, 11.8 | 8, 27.6 | 7, 24.1 | 5, 17.2 | 5, 17.2 | 4, 13.8 |
| Neuropathic Pain | 61, 24.8 | 9, 14.8 | 14, 23.0 | 18, 29.5 | 11, 18.0 | 9, 14.8 |
| Musculoskeletal Pain | 53, 21.5 | 6, 11.3 | 8, 15.1 | 14, 26.4 | 6, 11.3 | 19, 35.8 |
| Other | 9, 3.7 | – | 2, 22.2 | 1, 11.1 | 2, 22.2 | 4, 44.4 |
Note: There were no differences between groups.
4. Discussion
This study sought to examine PRI pain coping profiles in a sample of patients with diverse pain complaints. Using the coping cluster algorithm developed by Walker and colleagues [28], we successfully classified all patients in our sample. We also found that the proportion of patients in our sample classified into each of the coping profiles was similar to the proportions in the original study [28]. Thus, the pain coping typology developed for patients with chronic abdominal pain also appears to be useful in classifying pain coping profiles of adolescent patients with a variety of pain conditions.
Similar to the original chronic abdominal pain sample, we found that Avoidant Copers and Dependent Copers had the most negative functioning, with higher levels of anxiety, depression and disability than patients with other coping profiles. As observed by Walker and colleagues [28], the characteristics of these coping profiles are consistent with the downward spiral of pain-related disability described in the literature [3,10]. Interestingly, Avoidant and Dependent Copers did not report higher levels of pain than other patients but instead were less equipped to adaptively cope with their pain.
In the current study, there was a greater proportion of Self-Reliant Copers as compared to the original sample [28]; however, this finding is understandable given the older age range of our adolescent sample (M = 14.69, SD = 1.49 vs. M = 11.60, SD = 2.47 in the original sample) in which developmentally we would expect a greater tendency toward independence and self-reliant coping. Lynch and colleagues [19] recently found a similar developmental trend towards increased self-reliance with age, as they found that adolescents reported significantly more positive self-encouragement strategies than younger children. Interestingly, although there were a higher proportion of males in the original Self-Reliant group [28], the current sample included significantly more females than males, and therefore, it was not possible to fully examine possible gender differences. However, the greater proportion of females in our sample is similar to demographic patterns observed in other pediatric multidisciplinary chronic pain clinic samples [7,13].
The majority of patients in our sample were classified as Infrequent Copers, indicating that they infrequently used most of the coping strategies included on the PRI. Combined with their relatively lower levels of physical and emotional symptoms, these findings appear to indicate that perhaps pain was not a significant stressor for these patients. Alternatively, perhaps these patients use coping strategies not captured by the PRI which account for their lower levels of physical and emotional symptoms. Direct observation of patients’ coping efforts during a pain episode would provide additional information on the strategies employed by these patients. Many of the patients in our tertiary care clinic report that they have few strategies with which to manage their pain or that they have abandoned certain coping strategies after they appear to be ineffective in reducing pain intensity or frequency; thus, it is possible that Infrequent Copers’ reports of limited coping strategies used is not specific to the PRI itself. Despite lower levels of disability compared to patients in other coping clusters, Infrequent Copers reported some impairment in daily activities, which likely explains why these patients sought evaluation and treatment in our multidisciplinary pain clinic.
Our findings must be interpreted in the context of study limitations. First, participants in this study were seeking evaluation at a pediatric pain clinic, and patients’ report of their coping responses and emotional distress may have been influenced by social desirability demands to present themselves in a favorable light. Past research has demonstrated that pediatric patients with chronic pain who were more strongly influenced by social desirability reported lower levels of emotional distress, perhaps due to a need to appear psychologically “normal” and legitimize the physical nature of their pain [18]. Second, although our high rates of female and Caucasian patients are similar to demographic patterns in other pediatric multidisciplinary chronic pain clinic samples [7,13], and research documents gender and ethnic discrepancies in who seeks treatment for chronic pain [14,20], the predominance of girls in the current sample and the lack of ethnic heterogeneity limit generalizability of findings. The high SES and occupational status of families in our study also may limit generalizability. Future studies should investigate possible effects of gender, ethnicity, and SES related to children’s coping with pain.
The replication of pain coping profiles across diverse pain conditions in this study provides some direction in considering whether particular pain coping profiles could be used to tailor treatment interventions. For example, a family or group intervention [1,23,24] might be particularly effective for Dependent Copers who seek social support, whereas the clinically significant levels of depressive symptoms in Avoidant Copers combined with their tendency to disengage and self-isolate suggests that they might benefit from additional psychiatric evaluation and treatment [4]. Self-Reliant Copers might be most responsive to treatments that emphasize self-management [6], while Engaged Copers, characterized by high levels of problem-solving and distraction, might benefit most from a cognitive behavioral approach to pain management that provides concrete tools such as relaxation training, guided imagery, and problem-solving to cope with pain (cf. [12]). Future research is needed to examine whether these pain coping typologies are useful in developing effective psychosocial treatment interventions for adolescents with chronic pain.
This study provides additional support for the utility of this pain coping typology in defining distinct and meaningful patterns of coping among pediatric patients with diverse pain complaints. This study also extends the work of Walker and colleagues [28] by characterizing the coping profiles with respect to the level of patient anxiety. Future studies examining the relation of pain coping profiles to behavioral outcomes, such as health service utilization and school absenteeism, would enhance our understanding of the impact of children’s pain coping strategies on their functioning. In addition, longitudinal research that prospectively assesses the relation of coping profiles to functional outcomes and treatment responses would help to establish the pain coping profiles’ clinical utility and validity as well as the stability of these profiles over time. Finally, it will be important to assess whether the coping profiles have better predictive utility than measures of individual coping strategies.
Acknowledgment
We have no financial or other relationships that could lead to a conflict of interest.
References
- [1].Barry J, von Baeyer CL. Brief cognitive-behavioral group treatment for children’s headache. Clin J Pain. 1997;13:215–20. doi: 10.1097/00002508-199709000-00006. [DOI] [PubMed] [Google Scholar]
- [2].Blount RL, Simons LE, Devine KA, Jaaniste T, Cohen LL, Chambers C, et al. Evidence-based assessment of coping and stress in pediatric psychology. J Pediatr Psychol. 2008;33:1021–45. doi: 10.1093/jpepsy/jsm071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Bursch B, Walco GA, Zeltzer LK. Clinical assessment of chronic pain and pain-associated disability syndrome. J Dev Behav Pediatr. 1998;19:45–53. doi: 10.1097/00004703-199802000-00008. [DOI] [PubMed] [Google Scholar]
- [4].Campo JV, Perel J, Lucas A, Bridge J, Ehmann M, Kalas C, et al. Citalopram treatment of pediatric recurrent abdominal pain and comorbid internalizing disorders: an exploratory study. J Am Acad Child Adolesc Psychiatry. 2004;43:1234–42. doi: 10.1097/01.chi.0000136563.31709.b0. [DOI] [PubMed] [Google Scholar]
- [5].Claar RL, Walker LS. Functional assessment of pediatric pain patients: psychometric properties of the functional disability inventory. Pain. 2006;121:77–84. doi: 10.1016/j.pain.2005.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Connelly M, Rapoff MA, Thompson N, Connelly W. Headstrong: a pilot study of a CD-ROM intervention for recurrent pediatric headache. J Pediatr Psychol. 2006;31:737–47. doi: 10.1093/jpepsy/jsj003. [DOI] [PubMed] [Google Scholar]
- [7].Eccleston C, Crombez G, Scotford A, Clinch J, Connell HA. Adolescent chronic pain: patterns and predictors of emotional distress in adolescents with chronic pain and their parents. Pain. 2004;108:221–9. doi: 10.1016/j.pain.2003.11.008. [DOI] [PubMed] [Google Scholar]
- [8].Garber J, Walker LS, Zeman J. Somatization symptoms in a community sample of children and adolescents: further validation of the children’s somatization inventory. Psychol Assess. 1991;3:588–95. [Google Scholar]
- [9].Hollingshead AB. Four factor index of social status. Yale University; Department of Sociology: 1975. [Google Scholar]
- [10].Hyman PE, Bursch B, Sood M, Schwankovsky L, Cocjin J, Zeltzer LK, et al. Visceral pain-associated disability syndrome: a descriptive analysis. J Pediatr Gastroenterol Nutr. 2002;35:663–8. doi: 10.1097/00005176-200211000-00014. [DOI] [PubMed] [Google Scholar]
- [11].Kaminsky L, Robertson M, Dewey D. Psychological correlates of depression in children with recurrent abdominal pain. J Pediatr Psychol. 2006;31:956–66. doi: 10.1093/jpepsy/jsj103. [DOI] [PubMed] [Google Scholar]
- [12].Kashikar-Zuck S. Treatment of children with unexplained chronic pain. Lancet. 2006;367:380–2. doi: 10.1016/S0140-6736(06)68118-X. [DOI] [PubMed] [Google Scholar]
- [13].Kashikar-Zuck S, Goldschneider K, Powers S, Vaught M, Hersey A. Depression and functional disability in chronic pediatric pain. Clin J Pain. 2001;17:341–9. doi: 10.1097/00002508-200112000-00009. [DOI] [PubMed] [Google Scholar]
- [14].Keogh E, Eccleston C. Sex differences in adolescent chronic pain and pain-related coping. Pain. 2006;123:275–84. doi: 10.1016/j.pain.2006.03.004. [DOI] [PubMed] [Google Scholar]
- [15].Kovacs M. Ratings scales to assess depression in school-aged children. Acta Paedopsychiatry. 1981;46:305–15. [PubMed] [Google Scholar]
- [16].Kovacs M, Beck AT. An empirical–clinical approach toward a definition of childhood depression. In: Schulterbrandt J, Raskin A, editors. Depression in childhood: Diagnosis, treatment, and conceptual models. Raven Press; New York: 1977. pp. 1–25. [Google Scholar]
- [17].Levy RL, Garner MD, Christie DL, Whitsett SF, Whitehead WE, Walker LS, et al. Changes in childhood recurrent abdominal pain and parental responses with cognitive behavioral therapy. Gastroenterology. 2003;124:A-530. [Google Scholar]
- [18].Logan DE, Claar RL, Scharff L. Social desirability response bias and self-report of psychological distress in pediatric chronic pain patients. Pain. 2008;136:366–72. doi: 10.1016/j.pain.2007.07.015. [DOI] [PubMed] [Google Scholar]
- [19].Lynch AM, Kashikar-Zuck S, Godschneider KR, Jones BA. Sex and age differences in coping styles among children with chronic pain. J Pain Symptom Manage. 2007;33:208–16. doi: 10.1016/j.jpainsymman.2006.07.014. [DOI] [PubMed] [Google Scholar]
- [20].Nguyen M, Ugarte C, Fuller I, Hass G, Portenoy RK. Access to care for chronic pain: racial and ethnic differences. J Pain. 2005;6:301–14. doi: 10.1016/j.jpain.2004.12.008. [DOI] [PubMed] [Google Scholar]
- [21].Reynolds CR, Richmond BO. What I think and feel: a revised measure of children’s manifest anxiety. J Abnorm Child Psychol. 1978;6:271–80. doi: 10.1007/BF00919131. [DOI] [PubMed] [Google Scholar]
- [22].Reynolds CR, Richmond B. Revised children’s manifest anxiety scale (RCMAS) manual. Western Psychological Services; Los Angeles: 1985. [Google Scholar]
- [23].Robins PM, Smith SM, Glutting JJ, Bishop CT. A randomized controlled trial of a cognitive-behavioral family intervention for pediatric recurrent abdominal pain. J Pediatr Psychol. 2005;30:397–408. doi: 10.1093/jpepsy/jsi063. [DOI] [PubMed] [Google Scholar]
- [24].Sanders M, Shepherd R, Cleghorn G, Woolford H. The treatment of recurrent abdominal pain in children: a controlled comparison of cognitive-behavioral family intervention and standard pediatric care. J Consult Clin Psychol. 1994;62:306–14. doi: 10.1037//0022-006x.62.2.306. [DOI] [PubMed] [Google Scholar]
- [25].Saylor C, Finch A, Spirito A, Bennett B. The children’s depression inventory: a systematic evaluation of psychometric properties. J Consult Clin Psychol. 1984;52:955–67. doi: 10.1037//0022-006x.52.6.955. [DOI] [PubMed] [Google Scholar]
- [26].Smith CA, Wallston KA. An analysis of coping profiles and adjustment in persons with rheumatoid arthritis. Anxiety Stress Coping. 1996;9:107–22. [Google Scholar]
- [27].Sullivan MJL, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, et al. Theoretical perspective on the relation between catastrophizing and pain. Clin J Pain. 2001;17:52–64. doi: 10.1097/00002508-200103000-00008. [DOI] [PubMed] [Google Scholar]
- [28].Walker LS, Baber KF, Garber J, Smith CA. A typology of pain coping in pediatric patients with chronic abdominal pain. Pain. 2008;137:266–75. doi: 10.1016/j.pain.2007.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Walker LS, Garber J, Greene JW. Somatization symptoms in pediatric abdominal pain patients: relation to chronicity of abdominal pain and parent somatization. J Abnorm Child Psychol. 1991;19:379–94. doi: 10.1007/BF00919084. [DOI] [PubMed] [Google Scholar]
- [30].Walker LS, Greene JW. The functional disability inventory: measuring a neglected dimension of child health status. J Pediatr Psychol. 1991;16:39–58. doi: 10.1093/jpepsy/16.1.39. [DOI] [PubMed] [Google Scholar]
- [31].Walker LS, Smith CA, Garber J, Claar RL. Testing a model of pain appraisal and coping in children with chronic abdominal pain. Health Psychol. 2005;24:364–74. doi: 10.1037/0278-6133.24.4.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Walker LS, Smith CA, Garber J, Van Slyke DA. Development and validation of the pain response inventory for children. Psychol Assess. 1997;9:392–405. [Google Scholar]