Abstract
The glycoproteins (GP) of enveloped viruses facilitate entry into the host cell by interacting with specific cellular receptors. Despite extensive study, a cellular receptor for the deadly filoviruses Ebolavirus and Marburgvirus has yet to be identified and characterized. Here, we show that T-cell Ig and mucin domain 1 (TIM-1) binds to the receptor binding domain of the Zaire Ebola virus (EBOV) glycoprotein, and ectopic TIM-1 expression in poorly permissive cells enhances EBOV infection by 10- to 30-fold. Conversely, reduction of cell-surface expression of TIM-1 by RNAi decreased infection of highly permissive Vero cells. TIM-1 expression within the human body is broader than previously appreciated, with expression on mucosal epithelia from the trachea, cornea, and conjunctiva—tissues believed to be important during in vivo transmission of filoviruses. Recognition that TIM-1 serves as a receptor for filoviruses on these mucosal epithelial surfaces provides a mechanistic understanding of routes of entry into the human body via inhalation of aerosol particles or hand-to-eye contact. ARD5, a monoclonal antibody against the IgV domain of TIM-1, blocked EBOV binding and infection, suggesting that antibodies or small molecules directed against this cellular receptor may provide effective filovirus antivirals.
Keywords: viral entry, viral receptor, virion internalization
The Filoviridae family of viruses is composed of two genera, Ebolavirus and Marburgvirus, which cause hemorrhagic fever in humans and nonhuman primates. Infection with some strains of filoviruses causes fatality in 50–90% of human cases (1). The viral glycoprotein (GP) of Ebolavirus, which consists of surface-exposed subunit GP1 attached to membrane-bound subunit GP2 by a disulfide bond (2), mediates binding to, penetration of, and fusion with host-cell membranes (3, 4). Pseudovirions bearing Ebolavirus GP transduce a broad range of cells through interactions that require the GP1 receptor-binding domain (RBD) (5–8). Upon internalization into low-pH endosomes, the filovirus GP1 is proteolyzed by cathepsins B and L, leading to GP2-dependent fusion of the viral and host membranes (9–12). Several proteins enhance filovirus entry in host cells, including the C-type lectins L-SIGN, DC-SIGN, and hMGL, as well as RhoB/C, integrin α5β1, folate receptor-α, and the tyrosine kinase receptor Axl (13–26); however, because none of these molecules has been shown to interact with the RBD of the filovirus GP1, it is unlikely that any of these proteins serve as a receptor for this family of viruses. Thus, we used gene correlation analysis to search for additional potential receptors. Here, we identify T-cell Ig and mucin domain 1 (TIM-1), which interacts with Zaire ebolavirus (EBOV) GP and enhances EBOV infection by 10- to 30-fold upon expression, providing strong evidence that TIM-1 serves as a receptor for EBOV. As we found that TIM-1 is expressed on a number of mucosal epithelial surfaces, we propose that TIM-1/EBOV interactions may serve as a conduit for filovirus entry into the human body.
Results
Correlation of TIM-1 Gene Expression with EBOV GP-Dependent Transduction.
An innovative bioinformatics approach, comparative genetics analysis (CGA), was used to identify candidate genes involved in EBOV entry. This technique differs from previous gene discovery approaches as it correlates cellular gene expression with virus transduction efficiency across a panel of human tumor lines (27, 28). Although EBOV is a biosafety level 4 (BSL-4) pathogen, we performed our transduction screen under BSL2 conditions using a green fluorescent protein-expressing vesicular stomatitis virus (VSVΔG-eGFP) pseudotyped with either EBOV GP or VSV G (3). The EBOV GP that was used lacked the GP1 mucin domain (EBOV GP ΔO), as this form of GP confers the same tropism as full-length GP, contains the complete putative RBD, and produces higher pseudovirion titers (23, 29, 30). Fifty-four lines from the NCI-60 panel of human tumor cells were evaluated for permissiveness to both EBOV GP and VSV G-dependent transduction (Fig. 1 A and B). EBOV GP pseudovirions most effectively transduced renal, central nervous system, and non–small-cell lung carcinoma cell lines, with limited transduction of leukocyte lines. The EBOV transduction profile of the 54 cell populations served as a seed file for comparison with known gene expression patterns via the COMPARE algorithm available on the Developmental Therapeutic Program (NCI) Web site (http://www.dtp.nci.nih.gov/docs/compare/compare.html), with the goal of identifying potential cellular receptors for this virus. Candidate EBOV cellular receptors identified by this correlation analysis were prioritized according to the following criteria: (i) genes with an expression profile that highly correlated with EBOV GP pseudovirion transduction, as determined by a Pearson correlation coefficient (PCC); (ii) genes positively correlated with EBOV pseudovirion transduction but not with VSV G pseudovirion transduction; and (iii) genes encoding a cell surface-associated protein.
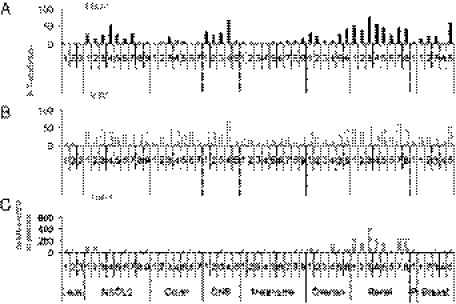
Fig. 1.
TIM-1 expression positively correlates with EBOV GP-dependent transduction, but not with VSV G-dependent transduction in a gene correlation assay. Relative transduction efficiency of (A) EBOV GP- or (B) VSV G-mediated transduction into the same NCI-60 cell lines. (C) Relative TIM-1 expression in the same 54 cell lines of the NCI-60 panel assessed by gene array analysis. Results of gene array studies of cells in the NCI-60 panel are available on the NCI-DTP website at http://dtp.nci.nih.gov/docs/compare/compare.html (GC185412).
Expression of the T-cell Ig and mucin domain 1 (TIM-1, also known as Kim-1 or HAVcr1) gene correlated with EBOV GP ΔO transduction (PCC = 0.601; P < 0.00003) but did not correlate with VSV G-dependent transduction (Fig. 1). Whereas expression of a previously characterized entry factor, Axl (24), also correlated with EBOV GP transduction in our screen (PCC = 0.501), the correlation was stronger between TIM-1 and virus transduction. TIM-1 was not expressed in all permissive cell lines, suggesting that additional, currently unidentified cellular proteins may also enhance filovirus entry. TIM-1 is a type 1 transmembrane protein composed of an extracellular Ig variable (IgV) domain, a mucin-like domain, a transmembrane domain, and a cytoplasmic tail (31, 32). The protein is expressed on dividing cells of the kidney epithelium and on activated Th2 cells (32), and binds to phosphatidylserine (PS) as well as family member TIM-4, resulting in the clearance of apoptotic cells and activation of T-cell proliferation, respectively (33–36). Previous work also identified TIM-1 as a receptor for hepatitis A virus (37).
Cell Surface TIM-1 Enhances EBOV GP-Dependent Entry.
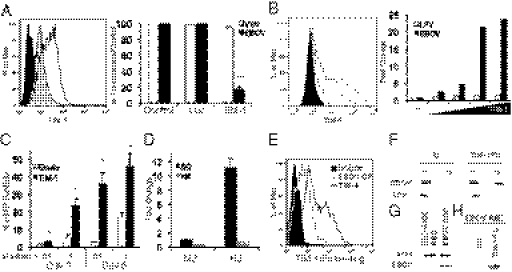
The monkey kidney cell line Vero, which has been extensively used to investigate EBOV infection (9, 11, 12, 26, 38, 39), expresses TIM-1 on its plasma membrane (Fig. 2A, Left). We investigated whether EBOV transduction requires endogenous TIM-1 by transfecting Vero cells with siRNAs targeting TIM-1 or luciferase. Cell-surface expression of TIM-1 was abundant on Vero cells transfected with the luciferase siRNA, but was reduced in cells transfected with the TIM-1 siRNA (Fig. 2A, Left). Susceptibility of Vero cells to EBOV GP ΔO, but not VSV-G, pseudovirion transduction was greatly decreased when cells were depleted of cell surface TIM-1 (Fig. 2A, Right).
Fig. 2.
TIM-1 serves as a receptor for EBOV. (A) Reduced plasma membrane-associated TIM-1 decreases EBOV GP pseudovirion transduction. Vero cells were transfected with either luciferase or TIM-1 siRNA. (Left) TIM-1 surface expression at 48 h following transfection as assessed by flow cytometry (filled black histogram represents TIM-1 RNAi-transfected cells immunostained with an isotype control antibody; unfilled black histogram shows TIM-1 expression in luc siRNA-transfected cells immunostained with anti–TIM-1 mAb ARD5; gray histogram demonstrates TIM-1 expression in TIM-1 siRNA-transfected cells incubated with anti–TIM-1 mAb ARD5). (Right) EBOV transduction of transfected Vero cells. Cells were transduced with VSV pseudotyped with either EBOV GP ΔO or VSV G GP (MOI = 0.05). (B and C) Ectopic expression of TIM-1 enhances EBOV transduction. (B Left) Surface TIM-1 expression at 48 h following transfection. HEK 293T cells were transfected with 3 μg of empty plasmid (filled black histogram) or increasing amounts of hTIM-1 (gray, 3 ng; black dashed, 30 ng; gray dashed, 300 ng; black, 3 μg). (Right) Transduction of the transfected cells by EBOV GP ΔO (filled bars) or Lassa fever virus GP (unfilled bars) pseudotyped VSV at 48 h following transfection. Data are fold increase in entry over cells transfected with empty vector (MOI = 0.01). Data are representative of three independent replicates. (C) NCI-H522 cells were transfected with empty vector or TIM-1. Cells were infected with 0.1 or 1 μL of replication competent EBOV GP ΔO VSV (MOI = 2.5 × 103 or 2.5 × 104 as assessed in Vero cells). (D) Transduction of EBOV GP RBD mutant K114A/K115A is minimally enhanced by TIM-1 expression. TIM-1null M2 or TIM-1+ H3 cells were transduced with reverse transcriptase normalized FIV pseudotyped with either wild-type EBOV GP ΔO (WT) or EBOV GP ΔO-KK. (E) EBOV GP expression on the surface of HEK 293T cells enhances soluble TIM-1 binding. HEK 293T cells transfected with an empty plasmid (black filled histogram), a plasmid expressing EBOV GP ΔO (gray unfilled histogram), or a plasmid expressing TIM-4 (black unfilled histogram) were incubated with TIM-1/Fc for 1 h at 4 °C. Binding was analyzed by flow cytometry. (F) EBOV pseudovirions bind to soluble TIM-1. Human Ig or TIM-1/Fc bound Protein A beads were incubated with EBOV ΔO GP or LFVGP pseudotyped FIV for 1 h at 37 °C. Beads were washed to remove unbound virus (letter U) and virion binding to beads (letter B). Binding was evaluated by immunoblotting for FIV capsid. (G) Ability of thermolysin-cleaved, wild-type EBOV GP to bind to TIM-1+ H3 cells, but not thermolysin-cleaved EBOV GP K114A/K115A. The purified, trimerized EBOV GPs were treated with thermolysin to generate the 19-kDa form containing the RBD. The processed GPs were incubated with H3 cells, washed, and lysed. H3 cell actin levels are also shown. (H) Ability of TIM-1/Fc, but not the isotype control, to coimmunoprecipitate soluble, thermolysin-cleaved EBOV GP. *P < 0.05, ***P < 0.0001.
The human embryonic kidney cell line HEK 293T does not express TIM-1 and is less permissive than Vero cells to replication of an infectious VSV/eGFP containing EBOV GP ΔO in place of VSV-G (Fig. 2B, Left, and Fig. S1). Transient transfection of increasing amounts of a human TIM-1–expressing plasmid resulted in a dose-dependent enhancement of EBOV GP transduction compared with cells transfected with a control plasmid (Fig. 2B, Right). In contrast, EBOV GP transduction was unaffected by expression of TIM family member TIM-3 (Fig. S2 A and B). This increase in transduction was specific for EBOV GP, as expression of TIM-1 had no effect on transduction of Lassa fever virus (LFV) pseudovirions.
We further evaluated the ability of ectopic TIM-1 expression to mediate EBOV infection in another TIM-1null cell line NCI-H522 that is poorly permissive for EBOV infection (NSCLC line 9 in the NCI-60; Fig. 1 and Fig. S1). Transient transfection of a TIM-1–expressing plasmid into these cells resulted in TIM-1 surface expression in about 55% of the population (Fig. S2E). Using our replication competent EBOV GP VSV, we found that TIM-1–expressing NCI-H522 cells supported significantly greater virus replication than NCI-H522 cells transfected with empty vector (Fig. 2C). Thus, in both poorly (NCI-H522) and moderately (293T) permissive TIM-1null cells, expression of TIM-1 significantly and specifically increased EBOV GP-dependent entry.
Stable as well as transient expression of TIM-1 in HEK 293T cells led to enhanced EBOV GP/VSV infection, but not wild-type VSV (Indiana), (Fig. S2 C and D). The TIM-1+ line H3 and the TIM-1null line M2 were used to assess the importance of EBOV GP RBD residues in TIM-1–dependent transduction. The EBOV GP RBD mutant K114A/K115A that has reduced binding and transduction of host cells (5, 7, 40) was transduced into M2 and H3 cells. TIM-1–mediated transduction of mutant K114A/K115A virions was reduced by 86% compared with wild-type EBOV GP pseudovirions, indicating that residues within the EBOV GP RBD are critical for TIM-1–dependent virus transduction (Fig. 2D).
H3 cells were also used to evaluate the ability of a TIM-1/Fc-expressing plasmid to inhibit transduction of EBOV GP VSV pseudovirions (Fig. S3). Transfection of either TIM-1/Fc or soluble EBOV GP led to an incomplete but significant reduction of EBOV GP-dependent transduction, demonstrating the ability of either of these ectodomains to compete for virus entry.
TIM-1 and EBOV GP Interact.
To determine if EBOV GP and TIM-1 interact, we assessed binding using several different assays. Initial studies demonstrated binding of soluble TIM-1/Fc to HEK 293T cells that were transfected with plasmids expressing EBOV GP ΔO (41) or family member TIM-4. Previous studies have demonstrated that TIM-1 and TIM-4 interact (35). Soluble TIM-1 bound to both the TIM-4–expressing cells and EBOV GP-expressing cells, but not to cells transfected with empty plasmid (Fig. 2E). In addition, soluble TIM-1/Fc immunoprecipitated pseudovirions containing EBOV GP ΔO, but not LFV GP (Fig. 2F). To examine this interaction further, soluble, trimerized EBOV GP was treated with thermolysin to generate the RBD-containing, 19-kDa processed form of GP1. We found that EBOV GP RBD bound more efficiently to TIM-1+ H3 cells than a thermolysin-cleaved RBD binding mutant K114A/K115A (Fig. 2G) and pulled-down purified TIM-1/Fc (Fig. 2H) (35). This data demonstrates a direct interaction between EBOV GP and TIM-1 that is dependent on the RBD domain.
TIM-1 Is Expressed on Human Airway and Eye Mucosal Epithelium.
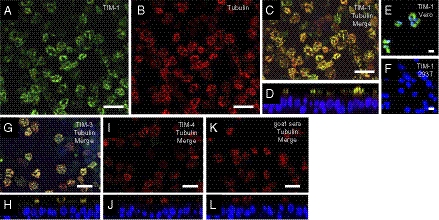
One established route of infection for Ebolavirus is the inhalation of aerosolized particles (42). Consistent with this route of infection, EBOV pseudovirions have been demonstrated to transduce well-differentiated primary human airway epithelia via the apical mucosal surface (23). TIM-1 expression in the airway had not been previously reported, but we observed abundant expression of TIM-1 on the apical surface of well-differentiated primary cultures of human airway epithelial cells where it colocalized extensively with the cilia marker β-tubulin (Fig. 3 A–D). Not only TIM-1, but also family member TIM-3, was detected on the cilia of these airway epithelial cultures; in contrast, family member TIM-4 was not evident on these cells (Fig. 3 G–J).
Fig. 3.
TIM-1 is expressed on cilia of human airway epithelia. (A) Detection of TIM-1 expression on the surface of well-differentiated human airway epithelial cultures using goat anti–TIM-1 antisera and Alexa 488-conjugated rabbit anti-goat antisera (green). (B) Immunostaining of β-tubulin within epithelial cilia using a mouse anti-tubulin monoclonal antibody and Cy3-conjugated goat anti-mouse (red). (C) Merged image of A and B. (D) Vertical section of merged image. To-Pro-3 (blue) identifies the nuclei. (E) Vero cells and (F) HEK293T cells stained with anti–TIM-1 antisera and Alexa 488-conjugated secondary (green). (G) A well-differentiated human airway epithelial culture stained for TIM-3 (green) and β-tubulin (red). (H) Vertical section of G. (I) Human airway epithelia stained for TIM-4 (green) and β-tubulin (red). (J) Vertical section of I. (K) Human airway epithelia immunostained with normal goat sera (green) and mouse anti–β-tubulin (red). (L) Vertical section of K. (Scale bar = 20 μM.)
Our observation that the apical surface of the airway epithelium expresses TIM-1 led us to examine additional mucosal epithelial surfaces for its expression. As in the case of well-differentiated airway epithelia, fixed sections of human conjunctiva, cornea, trachea, and kidney tubules also expressed TIM-1 (Fig. S4); expression in the kidney tubules was consistent with previous reports (34). Whereas TIM-1 was apically located on the tracheal epithelium, in the corneal and conjunctival epithelium robust expression was limited to the basal layer, suggesting that a break in the epithelial surface would be required for TIM-1 to interact with EBOV GP in these tissues.
TIM-1 Is Expressed on a Broad Range of Epithelial Cells in Vitro.
TIM-1 also was found on the cell surface of a variety of human epithelial lines known to be highly permissive for EBOV. For instance, TIM-1 was robustly expressed on the surface of seven of the eight renal cell lines of the NCI-60 panel, consistent with TIM-1 mRNA expression on the microarray (Fig. S5). These same seven lines were highly permissive for EBOV GP ΔO pseudovirion transduction (Fig. 1A). Only one renal line (SN12C, no. 6 in the NCI-60 renal cell panel; Fig. 1) did not express surface TIM-1, and it was poorly permissive for EBOV. In addition, TIM-1 was expressed on the surface of the hepatoma line Huh-7. Notably, TIM-1 expression was not observed in cells of nonepithelial origin, such as the neuroblastoma line SNB-19 that we previously demonstrated to be highly permissive for EBOV (5). Though these studies indicate that TIM-1 enhances EBOV in epithelial populations, they also provide evidence that additional cell-surface proteins must mediate productive entry of EBOV GP, because some cell types relevant to in vivo infection (such as macrophages) do not express TIM-1 (34), and EBOV transduction of some highly permissive cell lines investigated in our studies (e.g., SNB-19 cells) was independent of TIM-1 expression.
Monoclonal Antibodies Directed Against the TIM-1 IgV Domain Block EBOV Infection.
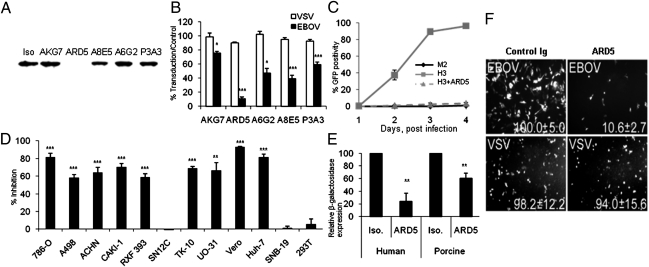
Five monoclonal antibodies (mAbs) against the TIM-1 ectodomain were assessed for their ability to inhibit EBOV GP ΔO pseudovirion binding to Vero cells. The epitope for each has been partially mapped, with AKG7 binding to the mucin domain and the other four binding to the IgV domain (41, 43). Of the anti–TIM-1 antibodies, ARD5 was able to completely block EBOV pseudovirion binding to Vero cells (Fig. 4A) and, over a range of ARD5 concentrations, inhibition of EBOV binding was dose dependent (Fig. S6). Consistent with the binding studies, ARD5 abrogated EBOV GP-dependent transduction, although all five mAbs decreased EBOV GP pseudovirion transduction to some extent (Fig. 4B). None of the mAbs affected VSV G-dependent entry. ARD5 was also highly efficacious at blocking replication of infectious EBOV GP ΔO VSV in the TIM-1+ H3 clonal line over a 4-d infection (Fig. 4C). The IgV epitope for ARD5 is outside of the TIM-1 PS binding pocket, whereas A6G2, which was much less effective in blocking transduction, prevents TIM-1 binding of PS (41). Thus, regions of the IgV domain other than the PS-binding pocket appear to be important for EBOV GP interactions.
Fig. 4.
TIM-1 mAb ARD5 inhibits EBOV entry. (A) Ability of anti–TIM-1 monoclonal antibodies to block EBOV pseudovirion binding to Vero cells. Cells were incubated with indicated mAb and then incubated with EBOV GP ΔO pseudotyped FIV for an additional hour at 4 °C. Lysates were probed for FIV capsid by immunolotting and normalized for β-actin expression. (B) Ability of five anti-human TIM-1 monoclonal antibodies to block EBOV GP transduction. 786-O cells (renal cell line 4 in the NCI-60 panel; Fig. 1C) were preincubated for 1 h at 4 °C with monoclonal antibodies against the ectodomain of human TIM-1. Cells were shifted to 37 °C and transduced with VSV pseudotyped with either EBOV GP ΔO or VSV G (MOI= 0.01). (C) ARD5 inhibits recombinant, infectious EBOV GP VSV infection of H3 cells. M2 (TIM-1−) or H3 (TIM-1+) HEK 293T cells were plated and H3 cells preincubated with ARD5. Cells were then infected with EBOV GP VSV (MOI = 25 as assessed in Vero cells). (D) Ability of ARD5 to inhibit EBOV GP-dependent transduction of permissive cell lines. Equal numbers of each cell line were preincubated with ARD5 for 1 h at 4 °C. Cells were shifted to 37 °C and transduced with VSV pseudotyped with EBOV GP ΔO (MOI = 0.05). Findings are shown as percent inhibition compared with isotype control populations. (E) ARD5 inhibits EBOV GP-mediated entry into well-differentiated human and porcine airway epithelial cultures. Cells were incubated with ARD5 or isotype control and then transduced with EBOV GP ΔO pseudotyped FIV at an MOI of 5. (F) ARD5 treatment inhibits EBOV infection. Vero cells were treated for 30 min with ARD5 or isotype control and then challenged with either a replication-competent EBOV or VSV that express eGFP upon infection. *P < 0.05, **P < 0.001, ***P < 0.0001.
The ability of ARD5 to block EBOV pseudovirion transduction was evaluated in an additional series of cells (Fig. 4D). ARD5 inhibited EBOV GP ΔO pseudovirion transduction in all cell lines expressing surface TIM-1, but not in lines that do not express TIM-1 (e.g., SN12C, SNB-19, HEK 293T). ARD5 inhibition of EBOV transduction of TIM-1–expressing Vero cells was time sensitive (Fig. S7A), with the inhibition being reduced as the mAb was added at later time points during virus transduction. ARD5 also inhibited both Marburgvirus GP (MARV) and full-length EBOV GP pseudovirion transduction into Vero cells with a similar dose–response curve, implicating TIM-1 in the entry of both filoviruses into epithelial cells (Fig. S7B).
We assessed the ability of ARD5 to block EBOV transduction of cells that are potentially relevant to filovirus transmission in vivo. ARD5 decreased EBOV GP ΔO pseudovirion entry into well-differentiated human and porcine airway cultures (Fig. 4E), suggesting that the TIM-1 residues responsible for EBOV GP interactions must be evolutionarily conserved. Conservation of the IgV domain is consistent with the wide host range reported for filoviruses. As the gastrointestinal tract has also been implicated as a route of EBOV transmission (44), we evaluated EBOV GP ΔO pseudovirion transduction of the TIM-1–expressing intestinal epithelial cell line Caco-2. Loss of availability of TIM-1 on the surface of Caco-2 cells as a consequence of either ARD5 application or TIM-1 siRNA treatment reduced EBOV transduction (Fig. S8). Supporting a role for TIM-1 in filovirus entry into a broad range of epithelial cells within the body, ARD5 and TIM-1 siRNA also reduced EBOV transduction into the hepatocellular carcinoma line Huh-7 (Fig. 4D).
ARD5 mAb Inhibits Infectious EBOV.
Our previous experiments were performed with either EBOV GP pseudovirions or recombinant, infectious EBOV GP VSV. Importantly, we also assessed whether ARD5 blocked infectious EBOV replication. Preincubation of Vero E6 cells with ARD5 decreased infection of infectious, replication-competent EBOV by 90% during a 28-h replication period, but had no effect on replication of wild-type VSV (Fig. 4F).
Discussion
The lack of a characterized cellular receptor is a major roadblock to understanding the pathogenesis of EBOV and MARV, and to developing antiviral therapies. This study was designed to overcome the deficiency. Here, we show that human TIM-1 serves as a receptor for filovirus infection of epithelial cells and cell lines from a broad range of tissues. A siRNA that reduced cell surface TIM-1 expression specifically decreased EBOV entry into a highly permissive cell line. Consistent with this finding, incubation of TIM-1–expressing cells with the TIM-1 mAb ARD5 decreased both EBOV binding and infection. Conversely, ectopic expression of TIM-1, but not family member TIM-3, significantly increased EBOV GP-mediated transduction and infection of poorly permissive cell lines. The ectodomain of TIM-1 interacted with EBOV GP RBD, and mutations in the RBD that are known to decrease binding to permissive cells significantly decreased TIM-1–dependent entry, indicating the importance of RBD residues for TIM-1 interactions.
Before this study, TIM-1 expression had been appreciated on two disparate cell types: Th2 cells and kidney epithelium (32). Our studies demonstrate that a much broader range of mucosal epithelium expresses TIM-1. These mucosal populations include the trachea, conjunctiva, and cornea. As experimental EBOV infection via aerosolization and ocular inoculation has been demonstrated (42, 45), these TIM-1+ cells may be some of the first cells infected by the virus and are likely to serve as routes of filovirus infection following hand-eye or hand-nose contact, or after droplet exposure.
All TIM-1+ cells investigated were readily infected with EBOV and, uniformly, EBOV infection of TIM-1–expressing cells was at least partially and in some cases fully inhibited by the TIM-1 mAb ARD5. This finding demonstrates the importance of TIM-1 expression for filovirus infection of these target cells. Because the epitope for ARD5 has been mapped to the IgV residues residing outside of the PS binding pocket (43), we propose that EBOV GP interacts with TIM-1 through IgV amino acids that have not been previously implicated as functionally important in ligand interactions.
Not all permissive cells were found to be TIM-1+. Nonepithelial cells, such as the neuroblastoma line SNB-19, do not express TIM-1, and, not surprisingly, EBOV infection of these cells was not inhibited by ARD5. As macrophages and dendritic cells are thought to be major targets of filoviruses (46, 47), but do not express TIM-1 (33), additional functional receptors for filoviruses remain to be identified.
Depending on the virus, cell-surface expression of a receptor can enhance virus infectivity from several fold to104-fold or more. For instance, hepatitis C virus (HCV) is appreciated to interact with at least four different human cell-surface proteins, leading to virus entry (48). Expression of any one of these proteins results in a modest two- to fivefold increase in virus infection, and combined expression of these proteins enhances HCV infection by 12- to 50-fold (48). In contrast to this example, where multiple surface proteins are required for optimal virus entry, ACE2 or SCARB2 expression yield more than 104-fold increase in SARS or enterovirus 71 infections, respectively (49–51), suggesting that each of these surface proteins is not only necessary but sufficient for virus entry. TIM-1 expression leads to a 10- to 30-fold increase in EBOV infectivity of poorly permissive cells, suggesting the possibility that TIM-1 acts in concert with other plasma membrane-associated proteins, such as previously described C-type lectins or Axl, to mediate productive uptake of filoviruses.
The ability of ARD5 to block EBOV and MARV infections of TIM-1+ cells provides a potentially efficacious and broad-spectrum antiviral therapy for this group of viruses. This monoclonal antibody or other agents that bind to the same TIM-1 residues may prove effective at prophylactically interfering with filovirus entry into the body. Furthermore, such antivirals that target cellular rather than viral proteins may decrease the rapid evolution of virus antiviral resistance to therapeutic agents.
Materials and Methods
Correlation of Transduction with Microarray Gene Expression Pattern.
Cells (4 × 104) of each NCI-60 cell line were plated and transduced with equivalent quantities of VSVΔG/eGFP pseudotyped with either VSV G or EBOV GP ΔO [multiplicity of infection (MOI) = ∼1 in the highly permissive SNB-19 cell line]. Viral transduction efficiency was assessed 24 h post transduction by flow cytometry-based analysis of EGFP expression. The average percentage of eGFP-expressing cells from three independent assays was used as a seed file for COMPARE analysis performed at http://dtp.nci.nih.gov/compare/. Statistical analysis of these correlation findings was performed using the SAS software package (SAS Institute).
TIM-1 Immunoprecipitations.
A total of 2.5 μg of TIM-1/Fc or human Ig was incubated with immobilized Protein A agarose beads overnight at 4 °C (Thermo Scientific). Unbound protein was washed away with PBS. Equal quantities of EBOV GP pseudotyped FIV were incubated with beads for 1 h at 37 °C. Unbound virus was washed away using IP buffer (1× PBS, 0.1% Nonidet P-40). Bound virus was denatured in 1% SDS and immunoblotted for the presence of FIV capsid. TIM-1/Fc interactions with soluble GP were evaluated using a trimerized, thermolysin-cleaved EBOV GP-His construct.
Virus Transduction.
Cells (4 × 104) of the cell population of interest were seeded in a 48-well plate. Cells were transduced with either vesicular stomatitis virus or feline immunodeficiency virus pseudotyped particles at an MOI of 0.01. Viral entry was assayed 24 or 48 h after transduction by quantifying the number of eGFP- or β-gal–expressing cells, respectively.
Detailed materials and methods can be found in SI Materials and Methods.
Supplementary Material
Acknowledgments
We thank Dr. Jianqiang Shao in the University of Iowa Central Microscopy Core for his expert assistance with the confocal studies, and Yen-Ming Hsu and Véronique Bailly at Biogen Idec for purification of TIM-1/Fc protein. We also thank Drs. Stanley Perlman, C. Martin Stoltzfus, Beverly Davidson, Richard Roller, and Michael Welsh for critical evaluation of this manuscript. We acknowledge support from National Institutes of Health (NIH) Grants AI064526, AI073330, and AI082409 (to W.M.); AI063513 and AI057156 (to R.A.D.); and HL075363 (to P.B.M.). Support was also received from the Intramural National Institute of Allergy and Infectious Diseases Biodefense and NIH National Institute of Dental and Craniofacial Research (J.C.), the University of Iowa in Vitro Models and Cell Culture Core Grant NIH DK54759, Cell Morphology and Pathology Core Grant NIH DK54759, and Central Microscopy Core Grants NIH DK054759 and NIH CA086862. A.S.K., N.J.L, and S.M.-T. were supported by T32 AI 007533-12.
Footnotes
The authors declare no conflict of interest.
*This Direct Submission article had a prearranged editor.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1019030108/-/DCSupplemental.
References
- 1.Dolnik O, Kolesnikova L, Becker S. Filoviruses: Interactions with the host cell. Cell Mol Life Sci. 2008;65:756–776. doi: 10.1007/s00018-007-7406-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Volchkov VE, Feldmann H, Volchkova VA, Klenk H-D. Processing of the Ebola virus glycoprotein by the proprotein convertase furin. Proc Natl Acad Sci USA. 1998;95:5762–5767. doi: 10.1073/pnas.95.10.5762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Takada A, et al. A system for functional analysis of Ebola virus glycoprotein. Proc Natl Acad Sci USA. 1997;94:14764–14769. doi: 10.1073/pnas.94.26.14764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wool-Lewis RJ, Bates P. Characterization of Ebola virus entry by using pseudotyped viruses: Identification of receptor-deficient cell lines. J Virol. 1998;72:3155–3160. doi: 10.1128/jvi.72.4.3155-3160.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brindley MA, et al. Ebola virus glycoprotein 1: Identification of residues important for binding and postbinding events. J Virol. 2007;81:7702–7709. doi: 10.1128/JVI.02433-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuhn JH, et al. Conserved receptor-binding domains of Lake Victoria marburgvirus and Zaire ebolavirus bind a common receptor. J Biol Chem. 2006;281:15951–15958. doi: 10.1074/jbc.M601796200. [DOI] [PubMed] [Google Scholar]
- 7.Dube D, et al. The primed ebolavirus glycoprotein (19-kilodalton GP1,2): Sequence and residues critical for host cell binding. J Virol. 2009;83:2883–2891. doi: 10.1128/JVI.01956-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Manicassamy B, Wang J, Jiang H, Rong L. Comprehensive analysis of ebola virus GP1 in viral entry. J Virol. 2005;79:4793–4805. doi: 10.1128/JVI.79.8.4793-4805.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sanchez A. Analysis of filovirus entry into vero e6 cells, using inhibitors of endocytosis, endosomal acidification, structural integrity, and cathepsin (B and L) activity. J Infect Dis. 2007;196(Suppl 2):S251–S258. doi: 10.1086/520597. [DOI] [PubMed] [Google Scholar]
- 10.Lee JE, Saphire EO. Neutralizing ebolavirus: Structural insights into the envelope glycoprotein and antibodies targeted against it. Curr Opin Struct Biol. 2009;19:408–417. doi: 10.1016/j.sbi.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chandran K, Sullivan NJ, Felbor U, Whelan SP, Cunningham JM. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science. 2005;308:1643–1645. doi: 10.1126/science.1110656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schornberg K, et al. Role of endosomal cathepsins in entry mediated by the Ebola virus glycoprotein. J Virol. 2006;80:4174–4178. doi: 10.1128/JVI.80.8.4174-4178.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simmons G, et al. Folate receptor alpha and caveolae are not required for Ebola virus glycoprotein-mediated viral infection. J Virol. 2003;77:13433–13438. doi: 10.1128/JVI.77.24.13433-13438.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quinn K, et al. Rho GTPases modulate entry of Ebola virus and vesicular stomatitis virus pseudotyped vectors. J Virol. 2009;83:10176–10186. doi: 10.1128/JVI.00422-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Simmons G, et al. DC-SIGN and DC-SIGNR bind ebola glycoproteins and enhance infection of macrophages and endothelial cells. Virology. 2003;305:115–123. doi: 10.1006/viro.2002.1730. [DOI] [PubMed] [Google Scholar]
- 16.Alvarez CP, et al. C-type lectins DC-SIGN and L-SIGN mediate cellular entry by Ebola virus in cis and in trans. J Virol. 2002;76:6841–6844. doi: 10.1128/JVI.76.13.6841-6844.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan SY, et al. Folate receptor-alpha is a cofactor for cellular entry by Marburg and Ebola viruses. Cell. 2001;106:117–126. doi: 10.1016/s0092-8674(01)00418-4. [DOI] [PubMed] [Google Scholar]
- 18.Takada A, et al. Human macrophage C-type lectin specific for galactose and N-acetylgalactosamine promotes filovirus entry. J Virol. 2004;78:2943–2947. doi: 10.1128/JVI.78.6.2943-2947.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ji X, et al. Mannose-binding lectin binds to Ebola and Marburg envelope glycoproteins, resulting in blocking of virus interaction with DC-SIGN and complement-mediated virus neutralization. J Gen Virol. 2005;86:2535–2542. doi: 10.1099/vir.0.81199-0. [DOI] [PubMed] [Google Scholar]
- 20.Marzi A, et al. Analysis of the interaction of Ebola virus glycoprotein with DC-SIGN (dendritic cell-specific intercellular adhesion molecule 3-grabbing nonintegrin) and its homologue DC-SIGNR. J Infect Dis. 2007;196(Suppl 2):S237–S246. doi: 10.1086/520607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Takada A, et al. Downregulation of beta1 integrins by Ebola virus glycoprotein: Implication for virus entry. Virology. 2000;278:20–26. doi: 10.1006/viro.2000.0601. [DOI] [PubMed] [Google Scholar]
- 22.Schornberg KL, et al. Alpha5beta1-integrin controls ebolavirus entry by regulating endosomal cathepsins. Proc Natl Acad Sci USA. 2009;106:8003–8008. doi: 10.1073/pnas.0807578106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sinn PL, et al. Lentivirus vectors pseudotyped with filoviral envelope glycoproteins transduce airway epithelia from the apical surface independently of folate receptor alpha. J Virol. 2003;77:5902–5910. doi: 10.1128/JVI.77.10.5902-5910.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shimojima M, et al. Tyro3 family-mediated cell entry of Ebola and Marburg viruses. J Virol. 2006;80:10109–10116. doi: 10.1128/JVI.01157-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shimojima M, Ikeda Y, Kawaoka Y. The mechanism of Axl-mediated Ebola virus infection. J Infect Dis. 2007;196(Suppl 2):S259–S263. doi: 10.1086/520594. [DOI] [PubMed] [Google Scholar]
- 26.Hunt CL, Kolokoltsov AA, Davey RA, Maury W. The Tyro3 receptor kinase Axl enhances macropinocytosis of Zaire ebolavirus. J Virol. 2011;85:334–347. doi: 10.1128/JVI.01278-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weller ML, et al. Epidermal growth factor receptor is a co-receptor for adeno-associated virus serotype 6. Nat Med. 2010;16:662–664. doi: 10.1038/nm.2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Di Pasquale G, et al. Identification of PDGFR as a receptor for AAV-5 transduction. Nat Med. 2003;9:1306–1312. doi: 10.1038/nm929. [DOI] [PubMed] [Google Scholar]
- 29.Jeffers SA, Sanders DA, Sanchez A. Covalent modifications of the ebola virus glycoprotein. J Virol. 2002;76:12463–12472. doi: 10.1128/JVI.76.24.12463-12472.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yang ZY, et al. Identification of the Ebola virus glycoprotein as the main viral determinant of vascular cell cytotoxicity and injury. Nat Med. 2000;6:886–889. doi: 10.1038/78645. [DOI] [PubMed] [Google Scholar]
- 31.Su EW, Lin JY, Kane LP. TIM-1 and TIM-3 proteins in immune regulation. Cytokine. 2008;44:9–13. doi: 10.1016/j.cyto.2008.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kuchroo VK, Dardalhon V, Xiao S, Anderson AC. New roles for TIM family members in immune regulation. Nat Rev Immunol. 2008;8:577–580. doi: 10.1038/nri2366. [DOI] [PubMed] [Google Scholar]
- 33.Kobayashi N, et al. TIM-1 and TIM-4 glycoproteins bind phosphatidylserine and mediate uptake of apoptotic cells. Immunity. 2007;27:927–940. doi: 10.1016/j.immuni.2007.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ichimura T, et al. Kidney injury molecule-1 is a phosphatidylserine receptor that confers a phagocytic phenotype on epithelial cells. J Clin Invest. 2008;118:1657–1668. doi: 10.1172/JCI34487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Meyers JH, et al. TIM-4 is the ligand for TIM-1, and the TIM-1–TIM-4 interaction regulates T cell proliferation. Nat Immunol. 2005;6:455–464. doi: 10.1038/ni1185. [DOI] [PubMed] [Google Scholar]
- 36.Santiago C, et al. Structures of T cell immunoglobulin mucin protein 4 show a metal-Ion-dependent ligand binding site where phosphatidylserine binds. Immunity. 2007;27:941–951. doi: 10.1016/j.immuni.2007.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Feigelstock D, Thompson P, Mattoo P, Zhang Y, Kaplan GG. The human homolog of HAVcr-1 codes for a hepatitis A virus cellular receptor. J Virol. 1998;72:6621–6628. doi: 10.1128/jvi.72.8.6621-6628.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nanbo A, et al. Ebolavirus is internalized into host cells via macropinocytosis in a viral glycoprotein-dependent manner. PLoS Pathog. 2010;6:e1001121. doi: 10.1371/journal.ppat.1001121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saeed MF, Kolokoltsov AA, Albrecht T, Davey RA. Cellular entry of ebola virus involves uptake by a macropinocytosis-like mechanism and subsequent trafficking through early and late endosomes. PLoS Pathog. 2010;6:e100110. doi: 10.1371/journal.ppat.1001110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dube D, et al. Cell adhesion promotes Ebola virus envelope glycoprotein-mediated binding and infection. J Virol. 2008;82:7238–7242. doi: 10.1128/JVI.00425-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sonar SS, et al. Antagonism of TIM-1 blocks the development of disease in a humanized mouse model of allergic asthma. J Clin Invest. 2010;120:2767–2781. doi: 10.1172/JCI39543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Johnson E, Jaax N, White J, Jahrling P. Lethal experimental infections of rhesus monkeys by aerosolized Ebola virus. Int J Exp Pathol. 1995;76:227–236. [PMC free article] [PubMed] [Google Scholar]
- 43.Binné LL, Scott ML, Rennert PD. Human TIM-1 associates with the TCR complex and up-regulates T cell activation signals. J Immunol. 2007;178:4342–4350. doi: 10.4049/jimmunol.178.7.4342. [DOI] [PubMed] [Google Scholar]
- 44.Connolly BM, et al. Pathogenesis of experimental Ebola virus infection in guinea pigs. J Infect Dis. 1999;179(Suppl 1):S203–S217. doi: 10.1086/514305. [DOI] [PubMed] [Google Scholar]
- 45.Jaax NK, et al. Lethal experimental infection of rhesus monkeys with Ebola-Zaire (Mayinga) virus by the oral and conjunctival route of exposure. Arch Pathol Lab Med. 1996;120:140–155. [PubMed] [Google Scholar]
- 46.Ströher U, et al. Infection and activation of monocytes by Marburg and Ebola viruses. J Virol. 2001;75:11025–11033. doi: 10.1128/JVI.75.22.11025-11033.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bray M, Geisbert TW. Ebola virus: The role of macrophages and dendritic cells in the pathogenesis of Ebola hemorrhagic fever. Int J Biochem Cell Biol. 2005;37:1560–1566. doi: 10.1016/j.biocel.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 48.Ploss A, et al. Human occludin is a hepatitis C virus entry factor required for infection of mouse cells. Nature. 2009;457:882–886. doi: 10.1038/nature07684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li W, et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang P, et al. Expression cloning of functional receptor used by SARS coronavirus. Biochem Biophys Res Commun. 2004;315:439–444. doi: 10.1016/j.bbrc.2004.01.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yamayoshi S, et al. Scavenger receptor B2 is a cellular receptor for enterovirus 71. Nat Med. 2009;15:798–801. doi: 10.1038/nm.1992. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.