Abstract
Purpose
Cryptococcal meningitis is a relatively common opportunistic infection in human immunodeficiency virus (HIV) patients and it can frequently occur in immunocompetent hosts without any apparent underlying disease. Nevertheless, little is known about cyptococcal meningitis in the Korean population. The purpose of this study was to evaluate the clinical features and initial laboratory findings of cryptococcal meningitis in patients with and without HIV at a tertiary care teaching hospital.
Materials and Methods
We performed a retrospective study at a tertiary care teaching hospital from January 2001 to December 2009. Eleven HIV positive patients and nine HIV negative patients were included.
Results
The most common symptoms were headache and fever in cryptococcal meningitis, and diabetic mellitus, end stage renal disease and liver cirrhosis were the main associated conditions in patients without HIV. Patients with HIV showed lower peripheral CD4+ cell counts (median: 9, range: 1-107) and a higher burden of cryptococcus than patients without HIV. There were no statistically significant differences in serum CRP level and other cerebrospinal fluid parameters between patients with HIV and without HIV. The in-hospital mortality was 10%, and recurrence of cyptococcal meningitis was observed in 3 patients with HIV and this occurred within 5 months of the first episode.
Conclusion
Cryptococcal meningitis is fatal without treatment, therefore, rapid recognition of symptoms such as fever and headache and diagnosis is required to decrease the mortality. Recurrence of meningitis after treatment should carefully be followed up, especially in advanced HIV patients.
Keywords: Cryptococcal meningitis, HIV, neurologic symptom
INTRODUCTION
Cryptococcus neoformans is an ubiquitous encapsulated yeast that causes significant infections, which range from asymptomatic pulmonary colonization to life threatening meningoencephalitis.1
Cryptococcosis occurs among immunocompromised hosts due to one of the following conditions: human immunodeficiency virus (HIV) infection, prolonged treatment with glucocorticoids, organ transplantation, malignancy, sarcoidosis, and in immunocompetent hosts who are without any apparent underlying condition.2,3 The most common sites of infection are the central nervous system and lungs.1-3 C. neoformans infection occurs following inhalation through the respiratory tract. The organism disseminates hematogenously and has a propensity to localize to the central nervous system, causing meningitis/meningoencephalitis.4,5 Although the incidence of cryptococcal meningitis has declined in HIV patients who are undergoing antiretroviral therapy, cryptococcal disease remains a leading cause of mortality in the developing world.6 C. neoformans usually infects HIV infected patients with CD4 T lymphocytes counts <100 cells/µL. The burden of organisms is generally higher, and the inflammatory response is much less in HIV infected patients than in non HIV infected patients. On the other hand, patients without HIV infection usually have a longer duration of symptoms, higher cerebrospinal fluid (CSF) cell counts, lower glucose levels and a lower burden of organism than do the patients with HIV infection.7,8
This infection is fatal without treatment. Therefore, rapid recognition, diagnosis and treatment are required to decrease the mortality. However, little is known about cryptococcal meningitis in the Korean population. We report herein our experience of cryptococcal meningitis and evaluation of the clinical features and initial laboratory findings of cryptococcal meningitis in patients with and without HIV.
MATERIALS AND METHODS
We retrospectively reviewed the medical records of patients with cryptococcal meningitis and who were admitted to Pusan National University Hospital, Busan, South Korea, from January 2001 to December 2009. Cryptococcal meningitis was defined as the clinical features of meningitis/meningoencephalitis along with a positive CSF cryptococcal antigen test or a positive CSF India ink preparation or isolation of Cryptococcus neoformans in the CSF cultures. HIV infection was confirmed by a combination of ELISA and Western blotting. The patients' demographic data, predisposing condition, presenting symptoms, initial laboratory findings (serum WBC, serum CRP, CSF cryptococcal antigen titer, CSF glucose, CSF cell count and cryptoccus culture of the blood/CSF), treatments and outcomes were included. The CD4+ cell count and plasma viral load, the duration of antiretroviral therapy (ART) before cryptococcal meningitis and the ART regimen were checked in the patients with HIV. The patients with cryptococcal meningitis were treated according to the practice guidelines for the management of cryptococcal disease.9 The patients with HIV received amphotericin B 0.7 mg/kg+flucytosine 400 mg/kg per day followed by fluconazole 200 mg per day, and the patients without HIV received amphotericin B 0.5 mg/kg/day followed by fluconazole 200 mg per day.
The median treatment duration of amphotericin B was 32.2 days (range: 11-80), and median duration of fluconazole was 110 days (range: 28-695) in this study.
Statistical analysis
Statistical analysis was done using SPSS version 12.0 (SPSS Corp, Chicago, IL, USA). The descriptive analysis consisted of the median and range for various parameters. The initial laboratory findings between the patients with and without HIV were compared using the chi-square test for categorial variables, t-test or ranksum test for numerical variables. p values <0.05 were considered to be statistically significant.
RESULTS
Demographic features and clinical outcomes
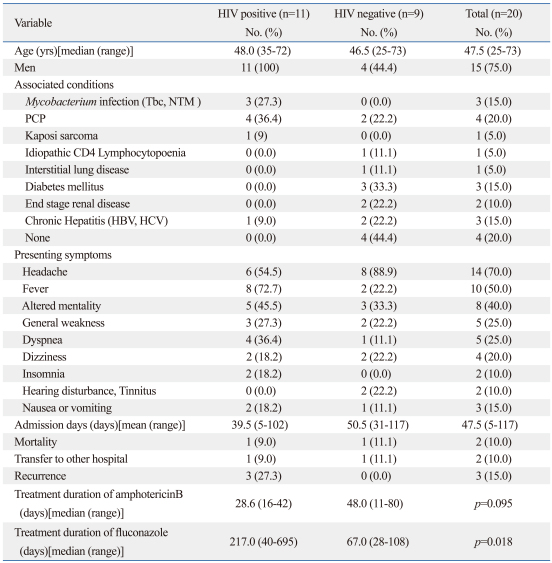
The demographics, clinical outcomes and treatment of the patients with or without HIV are shown in Table 1.
Table 1.
The Demographics and Clinical Outcomes of the 20 Patients with Cryptococcal Meningitis
HIV, human immunodeficiency virus; NTM, nontuberculous mycobacteria; PCP, pneumocystis (carinii) jiroveci pneumonia; HBV, hepatitis B virus; HCV, Hepatitis C virus.
Twenty patients who were diagnosed with cryptococcal meningitis were analyzed. The median age was 47.5 years (range: 25-73 years). Fifteen patients (75%) were men and five patients (25%) were women. All the HIV positive patients (n=11) were men. There were 11 (55%) and 9 (45%) patients with HIV and without HIV, respectively.
The underlying conditions in the patients without HIV were idiopathic CD4 lymphocytopenia (n=1; 11.1%), diabetes mellitus (n=3; 33.3%), end stage renal disease (n=2; 22.2%), liver cirrhosis (n=2; 22.2%), and interstitial lung disease with steroid use (n=1; 11.1%), and four patients (44.4%) had no apparent underlying disease at the time of diagnosis of cryptococcal meningitis. Mycobacterium infection (n=3; 27.3%), pneumocystis (carinii) jiroveci pneumonia (PCP) (n=4; 36.4%), kaposi sarcoma (n=1; 9%) and liver cirrhosis (n=1; 9%) were concurrently observed in the patients with HIV; pneumocystis (carinii) jiroveci pneumonia (PCP) was associated with 2 patients (22.2%) without HIV.
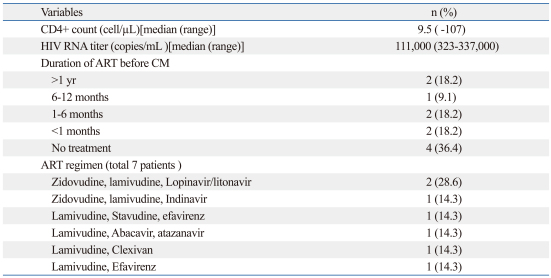
Eleven patients with HIV were studied. Their median HIV RNA titer was 111,000 copies/mL (from 323 to 337,000). The CD4 cell count ranged from 1 to 107 cells/µL. The median CD4 cell count was 9.5 cells/uL. Cryptococcal meningitis was the first AIDS-defining illness in 4 patients (36.4%). Other associated conditions were concurrently seen in 8 patients (72.7%): Mycobacterium infection (n=3; 27.3%), PCP (n=4; 36.4%), kaposi sarcoma (n=1; 9%) and liver cirrhosis (n=1; 9%) (Table 1). Seven patients received ART at presentation. Four of the 7 patients (36.4%) who received ART started it within the last six months of the index presentation, one patient (9.1%) received ART for 8 months and the other two patients received ART for more than one year before cryptococcal meningitis. Two patients were receiving a combination of lamivudine, zidovudine and lopinavir/litonavir, and the other five patients were receiving various combinations. The characteristics of the patients with HIV are shown in Table 2.
Table 2.
CD4+ count, HIV RNA Titer and ART Treatment of Cryptococcal Meningitis in the Patients with HIV
HIV, human immunodeficiency virus; ART, anti retroviral agent; CM, cryptococcal meningitis.
The most common symptom was headache (n=14; 70%), and others were fever (n=10; 50%), altered mentation ranging from confusion to a comatous state (n=8; 40%), general weakness (n=5; 25%), dyspnea (n=5; 25%), nausea or vomiting (n=3; 15%), dizziness (n=4; 20%), insomnia (n=2; 10%) and hearing disturbance/tinnitus (n=2; 10%).
The median number of admission days was 47.5 days (range: 5-117). Out of twenty patients, sixteen patients improved with treatment while two patients died and two patients were transferred to other hospitals. One of the two patients who died had high intracranial tension and diffuse cerebral edema seen on CT, and the other had acquired hospital pneumonia followed with adult respiratory distress syndrome (ARDS).
Three patients (15%) had recurrence of cryptococcal meningitis. All these patients were HIV positive and recurrence occurred within 5 months of the first episode of cryptococcal meningitis. There were no significant differences in treatment duration of amphotericin B (median number of treatment days: 28.6 days vs. 48 days; p=0.95) between the patients with HIV and without HIV. However, duration of fluconazole treatment in patients with HIV was longer than patients without HIV (median number of treatment days: 217 days vs. 67 days ; p=0.018).
The outcomes of the two transferred patients were not assessed.
The seven improved patients without HIV were followed up for at least 2 months and the nine improved HIV positive patients were followed up for at least 5 years.
Initial laboratory findings
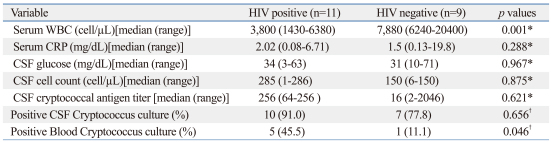
The cryptococcal antigen test for the CSF was positive in all the patients, and the Indian ink test was positive in eighteen patients (n=11, 100% in the HIV patients vs. n=7, 77.8% in the non HIV patients). The patients with HIV had lower serum WBC counts (median: 3,800 cell/µL vs. 7,880 cell/µL; p=0.001) and a higher positivity rate for cryptococcus culture of the blood (45.5% vs. 11.1%, respectively; p=0.046) than the patients without HIV. There were no significant differences between the patients with HIV and without HIV in the serum CRP (2.02 mg/dL vs. 1.5 mg/dL; p=0.288) and other initial CSF examinations such as CSF glucose level (p=0.967), CSF cell counts (p=0.875), cryptococcal antigen titer (p=0.621) and positivity rate of cryptococcus culture (p=0.656). Comparison of the initial laboratory findings (serum WBC, serum CRP, CSF cryptococcal antigen titer, CSF glucose, CSF cell count and cryptoccus culture in blood/CSF) of the patients with HIV and without HIV is shown in Table 3.
Table 3.
Initial Laboratory Findings of the Patients with Cryptococcal Meningitis
HIV, human immunodeficiency virus; CSF, cerebrospinal fluid.
*Using ranksum test.
†Using Chi-square test.
Chest X-ray and cranial CT or MRI were carried out in all patients. Eight patients showed abnormal lung lesion. Six patients with HIV (4: PCP, 2: pulmonary tuberculosis) and two patients without HIV (PCP) were observed. In neuroimaging, seven patients had abnormal neuroimaging. Three patients with HIV showed meningeal enhancement lesion and other four patients without HIV showed meningeal enhancement lesion (n=1), acute multiple infarction (n=2), and multiple intracranial granulomas (n=1).
DISCUSSION
In this study, the ages of patients were very diverse (median 47.5 years; range 25-73 years) and men were dominant, especially in the HIV group. Diabetic mellitus, end stage renal failure and liver cirrhosis were the major risk factors for the patients without HIV. However, four patients (20% of the total enrolled patients) had no apparent underline disease, making us to diagnose cryptococcal meningitis difficult. Fever and headache out of many various symptoms were the most common symptoms, which is consistent to the earlier reports,2,10,11 while the incidence of altered mentation (40% of the total patients and 45.5% of the patients with HIV) in our study was higher than that of the other reports (13-25% of patients).11,12 In this report, 25% of the patients had dyspnea, which could be due to associated pneumonia as PCP rather than systemic dissemination. Although focal neurologic deficits such as hearing disturbance/tinnitus were seen in a small number of patients, these symptoms were important. In two patients without apparent underlining disease, focal neurologic deficit was the main presentation of cryptococcal meningitis at admission.
Patients without HIV are known to have higher CSF cell counts, lower glucose levels and a lower burden of organism than the patients with HIV.7,8 In this study, most of the initial laboratory findings (serum CRP, CSF cryptococcal antigen titer, CSF glucose, CSF cell count and cryptoccus culture in CSF) had no statistical significance between the patients with HIV and the patients without HIV. But, there was a higher positive rate of Cryptococcus culture in blood in the patients with HIV than that in the patients without HIV (45.5% vs. 11.1%, respectively; p=0.046), indicating a higher burden of Cryptococcus in the patients with HIV. It is highly possible that these findings were due to small number of patients. Detection of cryptococcal capsular polysaccharide antigen and the Indian ink test were important tests for diagnosing cryptococcal meningitis in our study: the cryptococcal antigen test in CSF was positive for all the patients and the India ink test was positive for eighteen patients (n=11, 100% for the HIV patients vs. n=7, 77.8% for the non HIV patients).
Other studies have reported that the sensitivities, specificities and false positivity of the cryptococcal antigen test are in the range of 93-100%, 93-98% and approximately 0-0.4%, respectively, and the Indian ink test is positive in 70-90% of the patients with HIV and in only 50% of the patients without HIV.2,10,13
The CD4+ T cell count is the main predictor of an HIV patient's immunologic state.
Cryptococcal meningitis rarely occurs in patients with a CD4+ T cell counts greater than 100/µL. One study reported that average CD4+ T cell counts in patients with HIV and cryptococcosis were 73 cells/µL.14 The median CD4+ T cell count and range in this case series were 9.5 cells/µL and 1-107 cells/µL, respectively. Four of eleven patients with HIV were not receiving ART at admission, and cryptococcal meningitis was the first AIDS defining illness in those four patients. Although two out of the seven patients who were receiving ART had been on ART for more than one year before cryptococcal meningitis, these two patients' CD4+ T cell counts were very low at 30 cells/µL and 8 cells/µL, respectively. Poor compliance with ART is postulated as the cause for this. The in-hospital mortality in this case series was 10% (n=2).
Other studies also showed that acute mortality was in the range of 6-15%.15-18 The significant clinical and laboratory predictors of death during initial therapy include an abnormal mental status, a CSF antigen titer >1 : 1,024 and a CSF WBC count <20 cells/µL.8 In our study, the two patients who died had low CSF cell counts (<20), and they showed altered mentation. However, there was no relationship between in hospital mortality and the CSF antigen titer in these two patients. Although all the patients with HIV were treated with fluconazole as maintenance therapy after discharge, recurrence of infection after the initial treatment was observed in three patients. These three patients were HIV positive and recurrence occurred within 5 months of the first episode. Non compliance with taking their medication was the cause for recurrence in all of these patients.
There are not many studies on cryptococcal meningitis in the Korean population. Choi, et al.19 reported fifteen Korean patients with cryptococcosis, who were studied from 1974 to 1983. However, the study presented no data on patients with HIV, and included only one patient with cryptococcal meningitis. To our best knowledge, this is the first trial that studied the characteristics of cryptococcal meningitis in patients with or without human immunodeficiency virus in the Korean population.
This study has some limitations. The study was performed in a single tertiary hospital by retrospective chart review, and enrolled patients number was small. These facts may limit generalization of the results to the entire Korean population. Further large multicentered studies are required to obtain more accurate data on cryptococcal meningitis in the Korean population.
In summary, this study demonstrated that cryptococcal meningitis can occur not only in the HIV positive patients with low CD4+ cell counts, but also in patients without any apparent underlying disease. The most common symptoms were headache, fever and altered mentation.
Diabetic mellitus, end stage renal disease and liver cirrhosis were the main associated conditions in the patients without HIV. Patients with HIV showed very low CD4+ cell counts and a higher burden of cryptococcus than did the patients without HIV. While there were no statistically significant differences in the serum CRP level between the patients with and without HIV, other CSF examinations (glucose level, cell counts, cryptococcal antigen titer, positivity rate of cryptococcus culture) did show significant differences.
Detection of cryptococcal antigen and the Indian ink test were found to be important tools for diagnosis in this study. The in hospital mortality was 10%, in agreement with the data from other studies. Recurrence was observed in three patients with HIV, and this occurred within 5 months of the first episode. Non compliance with taking medication was the cause for recurrence in all of these patients.
ACKNOWLEDGEMENTS
The study was supported by Medical Research Institute Grant (2010), Pusan National University Yangsan Hospital.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Levitz SM. The ecology of Cryptococcus neoformans and the epidemiology of cryptococcosis. Rev Infect Dis. 1991;13:1163–1169. doi: 10.1093/clinids/13.6.1163. [DOI] [PubMed] [Google Scholar]
- 2.Perfect JR, Casadevall A. Cryptococcosis. Infect Dis Clin North Am. 2002;16:837–874. doi: 10.1016/s0891-5520(02)00036-3. [DOI] [PubMed] [Google Scholar]
- 3.Pappas PG, Perfect JR, Cloud GA, Larsen RA, Pankey GA, Lancaster DJ, et al. Cryptococcosis in human immunodeficiency virus-negative patients in the era of effective azole therapy. Clin Infect Dis. 2001;33:690–699. doi: 10.1086/322597. [DOI] [PubMed] [Google Scholar]
- 4.Igel HJ, Bolande RP. Humoral defense mechanisms in cryptococcosis: substances in normal human serum, saliva, and cerebrospinal fluid affecting the growth of Cryptococcus neoformans. J Infect Dis. 1966;116:75–83. doi: 10.1093/infdis/116.1.75. [DOI] [PubMed] [Google Scholar]
- 5.Diamond RD, May JE, Kane MA, Frank MM, Bennett JE. The role of the classical and alternate complement pathways in host defenses against Cryptococcus neoformans infection. J Immunol. 1974;112:2260–2270. [PubMed] [Google Scholar]
- 6.Jarvis JN, Harrison TS. HIV associated cryptococcal meningitis. AIDS. 2007;21:2119–2129. doi: 10.1097/QAD.0b013e3282a4a64d. [DOI] [PubMed] [Google Scholar]
- 7.Graybill JR, Sobel J, Saag M, van Der Horst C, Powderly W, Cloud G, et al. Diagnosis and management of increased intracranial pressure in patients with AIDS and cryptococcal meningitis. The NIAID Mycoses Study Group and AIDS Cooperative Treatment Groups. Clin Infect Dis. 2000;30:47–54. doi: 10.1086/313603. [DOI] [PubMed] [Google Scholar]
- 8.Saag MS, Powderly WG, Cloud GA, Robinson P, Grieco MH, Sharkey PK, et al. The NIAID Mycoses Study Group; the AIDS Clinical Trials Group. Comparison of amphotericin B with fluconazole in the treatment of acute AIDS-associated cryptococcal meningitis. N Engl J Med. 1992;326:83–89. doi: 10.1056/NEJM199201093260202. [DOI] [PubMed] [Google Scholar]
- 9.Saag MS, Graybill RJ, Larsen RA, Pappas PG, Perfect JR, Powderly WG, et al. Practice guidelines for the management of cryptococcal disease. Infectious Diseases Society of America. Clin Infect Dis. 2000;30:710–718. doi: 10.1086/313757. [DOI] [PubMed] [Google Scholar]
- 10.Bicanic T, Harrison TS. Cryptococcal meningitis. Br Med Bull. 2005;72:99–118. doi: 10.1093/bmb/ldh043. [DOI] [PubMed] [Google Scholar]
- 11.Cox GM, Perfect JR. Cryptococcus neoformans var neoformans and gattii and Trichosporon species. In: Edward LA, editor. Topley and Wilson's Microbiology and Microbial Infections. 9th ed. London: Arnold Press; 1997. [Google Scholar]
- 12.Kisenge PR, Hawkins AT, Maro VP, MeHele JP, Swai NS, Mueller A, et al. Low CD4 count plus coma predicts cryptococcal meningitis in Tanzania. BMC Infect Dis. 2007;7:39. doi: 10.1186/1471-2334-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tanner DC, Weinstein MP, Fedorciw B, Joho KL, Thorpe JJ, Reller L. Comparison of commercial kits for detection of cryptococcal antigen. J Clin Microbiol. 1994;32:1680–1684. doi: 10.1128/jcm.32.7.1680-1684.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Crowe SM, Carlin JB, Stewart KI, Lucas CR, Hoy JF. Predictive value of CD4 lymphocyte numbers for the development of opportunistic infections and malignancies in HIV infected persons. J Acquir Immune Defic Syndr. 1991;4:770–776. [PubMed] [Google Scholar]
- 15.van der Horst CM, Saag MS, Cloud GA, Hamill RJ, Graybill JR, Sobel JD, et al. National Institute of Allergy and Infectious Disease Mycoses Study Group; AIDS Clinical Trials Group. Treatment of cryptococcal meningitis associated with the acquired immunodeficiency syndrome. N Engl J Med. 1997;337:15–21. doi: 10.1056/NEJM199707033370103. [DOI] [PubMed] [Google Scholar]
- 16.Lortholary O, Poizat G, Zeller V, Neuville S, Boibieux A, Alvarez M, et al. Long-term outcome of AIDS-associated cryptococcosis in the era of combination antiretroviral therapy. AIDS. 2006;20:2183–2191. doi: 10.1097/01.aids.0000252060.80704.68. [DOI] [PubMed] [Google Scholar]
- 17.Brouwer AE, Rajanuwong A, Chierakul W, Griffin GE, Larsen RA, White NJ, et al. Combination antifungal therapies for HIV-associated cryptococcal meningitis: a randomized trial. Lancet. 2004;363:1764–1767. doi: 10.1016/S0140-6736(04)16301-0. [DOI] [PubMed] [Google Scholar]
- 18.Robinson PA, Bauer M, Leal MA, Evans SG, Holtom PD, Diamond DA, et al. Early mycological treatment failure in AIDS-associated cryptococcal meningitis. Clin Infect Dis. 1999;28:82–92. doi: 10.1086/515074. [DOI] [PubMed] [Google Scholar]
- 19.Choi KG, Choi IS, Kim KH. A clinical study of cryptococcal infection. J Korean Neurol Assoc. 1984;2:14–20. [Google Scholar]