Abstract
Objectives
To evaluate the efficacy of an Internet behavioral weight loss program; and determine if adding periodic in-person sessions to an Internet intervention improves outcomes.
Methods
481 healthy overweight adults (28% minority) were randomized to one of 3 delivery methods of a behavioral weight loss program with weekly meetings: Internet (n=160), InPerson (n=159), or Hybrid (Internet+InPerson, n=162). Outcome variables were weight at baseline and 6 months and percent of subjects achieving a 5 and 7% weight loss. The study took place in two centers in Vermont and Arkansas from 2003 to 2008.
Results
Conditions differed significantly in mean weight loss [8.0 (6.1)kg vs. 5.5 (5.6)kg vs. 6.0 (5.5)kg], for InPerson, Internet, and Hybrid respectively, p<0.01, n=462). Weight loss for InPerson was significantly greater than the Internet and Hybrid conditions (p<0.05). Although the proportion reaching a 5% weight loss did not differ, the proportion losing 7% did differ significantly (56.3% vs. 37.3% vs. 44.4% for InPerson, Internet, and Hybrid respectively, p<0.01).
Conclusions
These results demonstrate that the Internet is a viable alternative to in-person treatment for the delivery and dissemination of a behavioral weight-control intervention. The addition of periodic in-person sessions did not improve outcomes.
Introduction
Obesity treatment programs that combine dietary restriction, physical activity and behavior therapy and are delivered in group formats are considered the gold standard of treatment. These approaches reliably produce mean weight losses of 7–9% (Wadden, TA et al.; 2006, Writing Group of the PREMIER Collaborative Research Group, 2003),. However, access and adherence to such programs may be limited due to numerous barriers such as program availability, patient proximity, transportation concerns and time constraints (Wadden et al., 2007). Internet-based treatment programs may reduce some of these barriers, and the use of the Internet to deliver obesity treatment has grown substantially in recent years. However, only a few Internet-based interventions have managed to induce clinically significant weight losses of 5% or greater (Gold et al., 2007; Micco et al., 2007; Tate et al., 2006) and the average reported weight losses of internet-delivered interventions are consistently modest in comparison to those achieved in trials that implement treatment in person. Moreover, none of the published Internet trials have ever directly compared a gold standard, in-person intervention to an online format of the intervention. Therefore, it has never been possible to directly assess differences in the adherence, compliance and treatment outcomes of an online program compared to an in-person approach. As internet treatment methodologies proliferate, it is important to understand their comparative efficacy.
Internet programs have varied in the extent to which they mimic characteristics of successful in-person obesity treatment interventions, with some programs providing intensive interactive contact with group members and a professionally-trained behavioral therapist (Gold et al., 2007; Harvey-Berino et al., 2004 Micco et al., 2007). and others offering more limited social interaction (Tate et al., 2001, 2003). and achieving more limited weight losses. Social support has been established as an important component in enhancing weight loss outcomes (Wing & Jeffery, 1999), but all studies which demonstrate that the addition of social support potentiates behavioral weight control methods have provided face-to-face social support rather than virtual support. Thus, it is possible that an innovative “hybrid” design that couples the support of in-person, face-to-face group intervention with the barrier-reducing potential of the Internet may produce superior overall weight loss results.
Therefore, the purpose of this study was to directly evaluate the comparative efficacy of a comprehensive behavioral weight loss treatment program delivered online with the same program delivered in-person and with an innovative combined in-person and online approach. A secondary aim was to evaluate the treatment adherence (e.g., attendance at weekly sessions, self monitoring frequency) and perceived social support across the different treatment delivery modalities.
Methods
Participants
Overweight adults with a body mass index [BMI; calculated as weight (kg)/ height (m2)] between 25 and 50 and access to a computer with an Internet connection were recruited at two clinical centers. Exclusion criteria included a history of major medical or psychiatric conditions; recent changes in medication known to affect weight; current, planned or recent pregnancy; medical conditions that would prohibit exercise; and a schedule that would prohibit or restrict attendance at a designated time for weekly group meetings. Recruitment was conducted from February 2003 to March 2005 and the study was approved by the Committee on Human Research in the Behavioral Sciences at the University of Vermont and the Institutional Review Board at the University of Arkansas for Medical Sciences.
Screening Procedures
Interested individuals applied to participate via a study recruitment website that assessed computer hardware and connectivity, as well as self-reported body weight and height information and treatment meeting availability. Informed consent was obtained at the first of two in-person screening and baseline data collection visits. The group randomized design incorporated a total of 5 trial waves stratified within each site. Each trial wave consisted of three intact groups of 12–18 participants recruited at each site who were able to attend predetermined meeting times. Each group within each wave was stratified by their baseline BMI percentile values (25th, 50th, 75th) prior to randomization. The three intervention treatment arms were then randomized to one of the three meeting times using a biased coin approach.
Behavioral Weight Control Conditions
All conditions received a 6-month manualized comprehensive behavioral weight loss program that met weekly in face-to-face groups (for InPerson) or online via a synchronous chat group (for Internet and Hybrid conditions). The Hybrid group substituted an in-person meeting for an online chat once a month. Programs received identical behavioral lessons and individualized counselor feedback on progress toward meeting exercise and dietary intake goals. Group counselors used a written protocol that outlined standard lessons with counselor guides to ensure comparability of intervention methods.
Counselors included behaviorally-trained graduate students, clinical psychologists, and registered dieticians with extensive weight management experience and were cross-trained such that they were competent to deliver the intervention across modalities. Counselors facilitated the web chats or in-person meetings and provided the feedback on self-monitoring journals and homework. Participants assigned to the Hybrid condition had a primary counselor who moderated the online chat (3/mo) and provided feedback on journals and homework (weekly) and a different counselor who conducted their In-person meetings (1/mo). Participants at the two clinical sites were not mixed online.
Treatment Components Common to all Conditions
The weight loss treatment program focused on the modification of eating and exercise habits through the use of behavioral strategies and self-management skills. Participants were prescribed a calorie restricted diet and given a dietary fat goal corresponding to <25% of calories from fat. Graded exercise goals were provided which progressed to 200 min/week of moderate to vigorous exercise like walking, and pedometers were provided. Behavioral strategies included self monitoring, stimulus control, problem solving, goal setting, relapse prevention, and assertiveness training (Boutelle & Kirschenbaum, 1998; D'Zurilla & Goldfried, 1971; Perri et al., 2001; Perry et al., 1990). Homework assignments corresponding to these strategies were provided weekly. Subjects were instructed to record their dietary intake, minutes of physical activity and weight daily in either an online journal (for Internet and Hybrid) or a paper journal (InPerson) and to submit journals weekly. All groups met weekly for an hour-long session; therefore, the schedule of contact was the same for all conditions.
In-Person
Subjects were weighed by study staff prior to beginning their group session, which consisted of 15–20 participants. Each week they received materials that covered the topic introduced that session. In addition to the paper journal for self-monitoring dietary intake and physical activity, there were provided a commercially-available calorie and fat counting book. Implementation of group sessions was similar to the procedures used in other trials of in-person group behavioral weight control (Wadden et al., 2006).
Internet condition
Participants in the Internet condition met weekly in small groups of 15 to 20 individuals in a secure online chat room. They were asked to review the week's session material prior to the chat meeting with a new lesson becoming available every week. Participants had access to an online database to help monitor calorie intake (Calorie King, Family Health Network, Costa Mesa, CA). The Web site also included educational resources, a bulletin board for group communication, weekly tips and recipes, a BMI calculator, and local physical activity events (Krukowski et al., 2008).
Hybrid condition
Participants in this condition had access to the same Internet treatment program described above. However, once a month they substituted an in-person group meeting for an online chat. Session materials were delivered electronically, even in weeks when they met in-person. On those weeks that they met in-person, participants were weighed by study staff prior to the group meeting.
Dependent Measures
All outcomes were assessed at baseline and 6 months unless stated otherwise.
Body Weight
Weight change was the primary dependent measure. Weight was measured in street clothes, without shoes, on a calibrated scale. Height was measured using a wall mounted stadiometer (Seca Corporation, Hanover, MD). BMI was calculated as weight (kg) / height (m2).
Behavior
Dietary intake was measured with a self-report food frequency questionnaire, Block Version 98.2 (NutritionQuest, Berkley, CA) assessing usual intake over the previous 6 months. The food frequency questionnaire had been validated against 3-day diet records (Block et al., 1986) and yields discrepancies of less than 1% for changes in calorie and percent fat intake (Jeffrey et al., 1993). Daily energy intake and percent calories from fat were estimated using scoring algorithms performed by NutritionQuest (Berkeley, CA). The Paffenbarger Physical Activity Questionnaire (Pafenbarger et al., 1978) was used to estimate energy expended in physical activity. This measure has been shown to distinguish treatment conditions in previous studies (Wing et al., 1998).
Process Data
Counselors recorded participant attendance at group sessions and self-monitoring journal submissions. Data on social support were collected at 6-months. The Perceived Social Support Scale (Procidano & Heller, 1983) was used to assess the level of support group members perceived from other members of their intervention group. The scale has been shown to have good internal consistency (r=0.90), good test-retest reliability (r=0.83) and good predictive validity (Procidano & Heller, 1983). Scores range from 0 to 20, with higher scores representing more perceived support. The Working Alliance Inventory (Horvath & Luborsky, 1993) gauged participants' perception of support received from their weight loss counselor, with possible scores ranging from 12 to 84, and was collected at 6-months. The scale has been shown to have good convergent and divergent validity and an internal reliability estimate of r=0.85, with higher scores representing better bonding with the group counselor (Horvath & Luborsky, 1993).
Statistical Analysis
Sample size calculations were based on a 3×3 repeated measures design assuming no differences in site, with a 1% significance level to allow for post-hoc analysis. Using weight loss outcome standard deviations from a previous trial (Micco et al., 2007), a sample size of 482 (approximately 160 subjects per condition) allowed for 83% power to detect a main treatment effect and 99% power to detect both a time effect and a group by time interaction. Intention- to-treat analyses were used to analyze weight loss, with baseline value carried forward for individuals missing 6-month outcome data. Mixed models were used to compare treatment groups on baseline characteristics, adherence measures and baseline to six-month change in weight, physical activity and dietary outcomes. Analyses of weight change were adjusted for baseline values. Due to the nested nature of the data (i.e. wave within site), mixed model analyses of variance were used for comparing the treatment groups on continuous outcome measures. The models included treatment and site as fixed main effects, wave within site as a random main effect and the associated interactions of the main effects. If a significant treatment effect was detected, pair-wise comparisons were performed. A similar mixed model approach was used for dichotomous outcome measures using the SAS GLIMMIX procedure with a binary distribution. Comparisons of participants who did and did not complete the 6-month assessment were done using t-tests for continuous measures and chi-square tests for categorical measures. All analyses were run using SAS Version 9.1 (SAS Institute: Cary, NC).
Results
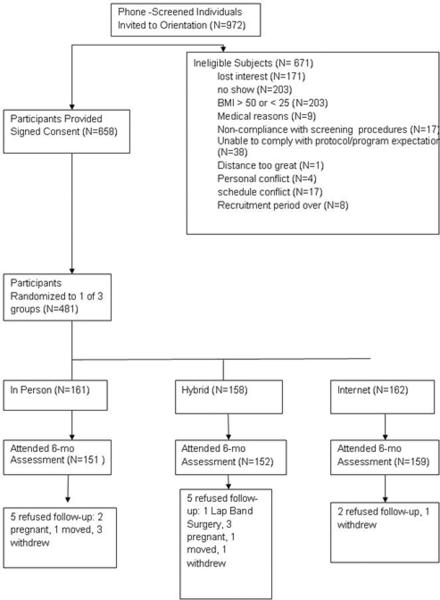
Four hundred and eighty-one overweight individuals were randomized (n= 238 from AR; n=243 from VT), representing 49.4% of those who initially indicated interest in participation (Figure 1). Participants were predominantly female (93%) and obese (82%), with 28% African Americans. There were no baseline differences between treatment conditions on sociodemographic characteristics, weight, dietary intake or exercise level (Tables 1 and 2). Ninety-six percent of randomized participants attended the 6-month assessment (n=462; Figure 1). There was no significant difference among treatment groups in the percentage of participants completing assessments. At baseline participants who did not complete 6-month assessments were younger (p<0.001) and less likely to be married (p=0.03) than those completing assessments.
Figure 1.
Participant flow diagram
Table 1.
Baseline Characteristics
| Variable | Total Sample (n=481) | Internet (n=161) | InPerson (n=158) | Hybrid (n=162) | p-value |
|---|---|---|---|---|---|
| Female (%) | 93 | 92 | 94 | 94 | 0.64 |
| African American (%) | 28 | 30 | 29 | 26 | 0.59 |
| Married, No (%) | 66 | 68 | 67 | 62 | 0.35 |
| College graduate, % | 65 | 69 | 62 | 63 | 0.39 |
| Age [years; mean (SD)] | 46.6(9.9) | 46.2(9.8) | 46.7(10.2) | 46.7(9.6) | 0.74 |
| Weight [kgs; mean(SD)] | 97.0(17.7) | 97.2(18.7) | 97.4(18.5) | 96.5(16) | 0.92 |
| BMI [kg/m2; mean (SD]a | 35.7(5.6) | 35.6(5.7) | 36.0(5.7) | 35.6(5.5) | 0.82 |
Data are given as means(SD) (number of participants).
Table 2.
Mean Weight Loss from Baseline to 6 months with Observed Data and Intent-to-Treat
| Observed Data | Baseline Carried Forward | |||||||
|---|---|---|---|---|---|---|---|---|
| Internet (n=159) | InPerson (n=150) | Hybrid (n=153) | p-value | Internet (n=161) | InPerson (n=158) | Hybrid (n=162) | p-value | |
| Weight Loss [kgs; mean(SD)] | −5.5(5.6) | −8.0(6.1) | −6.0 (5.5) | <0.01 | −5.5(5.6) | −7.6(6.2) | −5.7(5.5) | <0.01 |
| Percent weight lost [mean(SD)] | −5.8(5.4) | −8.3(6.1) | −6.4 (5.7) | <0.01 | −5.7(5.4) | −7.9(6.2) | −6.0(5.8) | <0.01 |
| Percent losing ≥ 5% (%) | 52.8 | 65.3 | 58.8 | 0.12 | 52.2 | 62.0 | 55.6 | 0.23 |
| Percent losing ≥ 7% (%) | 37.7 | 56.0 | 44.4 | 0.02 | 37.3 | 53.2 | 42.0 | 0.03 |
Body Weight Change
Weight change outcomes were examined with observed data (completers) and the previously described intent-to-treat analyses (Table 2). The pattern of statistical significance with observed or imputed weights was identical. Weight losses differed significantly between conditions [8.0 (6.1)kg vs. 5.5 (5.6)kg vs. 6.0 (5.5)kg], for InPerson, Internet, and Hybrid respectively, p<0.01]; pair-wise comparisons indicated mean weight loss achieved InPerson was significantly greater than mean weight loss achieved by either the Internet and Hybrid conditions. The Internet and Hybrid conditions did not differ significantly from each other. Similarly, the treatment conditions differed significantly in the mean percentage of initial body weight lost at 6 months (p<0.01), with InPerson losing a significantly greater percentage of body weight than either the Internet or Hybrid conditions. Again, the Internet and Hybrid conditions did not differ significantly from each other. The proportion of participants who lost 5% or more did not differ significantly by condition (p=0.12). There was however, a significant difference in the proportion of subjects achieving a 7% weight loss (56.3% vs. 37.3% vs. 44.4% for InPerson, Internet, and Hybrid respectively, p<0.01). The InPerson condition had the highest proportion of subjects reaching this milestone and differed significantly from the Internet condition, which had the lowest proportion. The Hybrid was intermediate between the other two conditions, and did not differ significantly from either.
Self-reported Dietary Intake and Physical Activity
Energy intake and expenditure at baseline and 6-months are presented in Table 3. The treatment by time interaction for calorie intake was not significant, indicating that there were no differences in change in self-reported intake between conditions. All conditions reported reductions in calorie intake [M=−580(676) kcal/d]. Similarly, there was no difference by condition in the change in the percent of calories consumed as fat [M=−4.4(5.9)%] or in the change in energy expended in physical activity from baseline to 6-months [M=+598(1468) kcal/wk].
Table 3.
Mean Energy Intake and Physical Activitya from Baseline to 6 Months
| Variable | Internet (n=135–159) | InPerson (n=136–159) | Hybrid (n=134–162) | P valueb |
|---|---|---|---|---|
| Dietary intake, kcal/d | ||||
| Baseline | 2008.1(725.2) | 1988.1(850.0) | 2069.9(799.3) | |
| 6 mo | 1435.3(458.6) | 1453.1(676.1) | 1409.8(547.8) | 0.46 |
| Fat intake, %/d | ||||
| Baseline | 36.8(5.7) | 37.6(6.1) | 37.4(5.3) | |
| 6 mo | 33.5(6.2) | 32.4(5.9) | 32.9(5.1) | 0.14 |
| Physical activity, kcal/wk | ||||
| Baseline | 1205.8(1128.7) | 1203.1(1302.5) | 1145.4(1042.1) | |
| 6 mo | 1877.5(1495.4) | 1930.4(1730.5) | 1613.1(1147.4) | 0.49 |
Data are given as means(SD) (number of participants).
P values are for the differences in the change scores of baseline-6mo.
Attendance and Self-monitoring
Attendance was calculated as proportion of online chats or in-person groups attended out of a possible 24 sessions. Similarly, compliance with self-monitoring was calculated as percent of weeks that subjects submitted a journal (either a paper journal or on-line, as appropriate). There were no differences in group sessions attended across conditions (76% for Internet vs. 71% for InPerson vs. 72% for Hybrid, p=0.25) or in the proportion of self-monitoring journals submitted (73% for Internet vs. 63% for InPerson vs. 71% in Hybrid, p=0.13).
Social Support
Perceived group support differed significantly between conditions (p<0.02). InPerson participants perceived their group members to be significantly more supportive than individuals participating in the Internet condition. However, the Hybrid group did not differ significantly from the InPerson or the Internet conditions on perceived group support [6.4(3.1) vs. 7.9(3.0) vs. 6.8(3.0), for the Internet, InPerson and Hybrid conditions respectively, p<0.02]. In contrast, participants rated their working alliance with their primary counselor similarly in all conditions (41.1(5.2) vs. 41.6(5.7) vs. 41.6(5.1) for the Internet, InPerson and Hybrid conditions respectively, p=.30). However, Hybrid participants rated their working alliance with their in-person (secondary) counselor [mean=39.7(5.8)] as significantly poorer than the working alliance with their primary online counselor [mean=41.6(5.7)] (p<0.001).
Discussion
This is the first study to directly compare weight loss outcomes from an in-person behavioral weight control intervention with one delivered exclusively online. While weight losses of the in-person participants were superior, individuals enrolled in the Internet treatment programs lost clinically meaningful amounts of weight as well. Specifically, over half of Internet subjects lost at least 5% of their baseline weight. This amount of weight loss has been associated with reduced chronic disease risk (National Institutes of Health/National Heart, Lung, and Blood Institute, 1998). It is important to note that although the weight losses achieved in the current study were smaller than those in the in-person program, they are among the highest achieved by an online weight control program reported to date (Gold et al., 2007; Harvey-Berino et al., 2004; Micco et al., 2007). Further, this is the first study to examine internet delivered weight management that has included a significant proportion of minority participants, a group that has demonstrated modest response to available behavioral weight management technologies (Kumanyika, 2008; West et al., 2007) but for whom the burden of obesity is high (Ogden, 2009). Finally, the weight losses achieved in the InPerson condition in the current study were substantial, comparable to the average 1-year losses reported in the Diabetes Prevention Program (Diabetes Prevention Program Research Group, 2002) and the Look AHEAD trial (Wadden et al., 2006). Thus, the weight losses against which the online condition was compared were among some of the best reported in the literature.
The addition of minimal in-person support did not significantly improve weight loss over and above online delivered program alone. Recent research by Micco and colleagues (2007) also suggests that little advantage is conferred by including in-person contact within an online intervention. While other research has evaluated computer technology as an adjunct to face-to-face communication (Glasgow et al., 1999; Gustafson et al., 1999), the present investigation is only the second to evaluate this hybrid model for weight loss. Given the complexity of managing two forms of intervention delivery, and the burden of travel to periodic in-person meetings, coupled with the apparent absence of improved weight loss outcomes, it is harder to advocate for the future potential of this approach. However, it is reasonable to consider that while the in-person meetings added little to the weight loss outcomes in this study, periodic in-person support could be a valuable addition to a clinical intervention as they could allow for other types of medical monitoring.
The treatment conditions resembled each other in several ways. All groups reported similar changes in diet and physical activity behaviors, which may not be surprising given the well-established measurement error associated with these self-report measures (Scagliusi et al., 2003). Also, attendance at group meetings and self monitoring did not differ between groups, although both self-monitoring and attendance tend to predict weight loss success in other studies (Acharya et al., 2009; Boutelle & Kirschenbaum, 1998). However, it is important to note that the lack of observed differences in self-monitoring and attendance may be related to the fairly high levels of compliance with both in all conditions. Subjects turned in 73% of self-monitoring journals and attended an average of 69% of their group meetings.
In contrast, the conditions did differ in perceived social support; social support is another aspect of behavioral obesity treatment that has been associated with better weight loss outcomes (Wing & Jeffery, 1999). Perceived group support was significantly higher when the intervention was delivered in-person, suggesting that social support may be one possible mechanism by which the in-person format produced the superior weight losses observed. There were no significant differences reported for alliance with the weight loss counselor across conditions, indicating that online treatment does not attenuate the therapeutic relationship. Differences were only seen in relationship to perceived group support. Online participants attended weekly chat sessions that included all group members and a consistent counselor. This is identical to the format used to deliver in-person treatment. The obvious difference is the lack of face-to-face communication. It is important to point out however, that the addition of monthly in-person contacts did not significantly increase perceived group support for the Hybrid group. In fact, participants reported lower alliance scores with their in-person counselor than their on-line counselor. Having separate on-line and in-person counselors allowed for an evaluation of a public health model of internet weight loss delivery where participants could connect virtually across a national or even international network but have periodic local, in-person meetings run by a physician's practice, community or public health organization. However, based on the results of this study, evaluating strategies to facilitate and enhance a sense of group cohesion online is warranted, and adding some face-to-face contact is not likely to be a promising avenue. However, other studies have demonstrated the beneficial impact of “engineering social support” on weight loss outcomes (Kumanyika et al., 2009; Wing & Jeffery, 1999).
Study Strengths and Limitations
This study has several strengths, including a randomized design and a protocol-driven intervention that offered treatment goals and behavioral strategies to achieve these goals that were comparable across all study conditions, allowing the difference in delivery channel to be the only distinguishing feature between the on-line and in-person programs. Additional strengths included that counselors were similarly trained and supervised, objective measures of weight were obtained, and a large, racially-diverse subject pool was included. The study did not include a no-treatment control group, outcome data are based on a six month intervention and generalization to the broader population of overweight and obese individuals may be hampered by the high education level of participants and the small number of men included in the sample.
Conclusions
The major findings of this study are that in-person delivery of behavioral weight loss programs result in superior weight losses compared with online delivery. The addition of periodic in-person support to an online intervention does not enhance outcomes. Given the potential for dissemination of high quality behavioral interventions over the Internet, further research is needed to improve weight loss outcomes of web-based obesity interventions. Specifically, strategies designed to enhance social support should be considered. Obesity is widespread and public health approaches that are effective and available broadly are desperately needed.
Acknowledgements
Funding/Support: This project was supported by NIDDK R01 DK056746 to Drs. Harvey-Berino and West
Role of the Funding Source: None of the funding sources were involved in the design or conduct of the study; collection, management, analysis or interpretation of the data; or preparation, review or approval of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Trial Registration: Clinicaltrials.gov Identifier: NCT00265954
Conflict of Interest Statement The authors declare that there are no conflicts of interest.
Financial Disclosure: None reported
References
- Acharya SD, Elci OU, Sereika SM, Music E, Styn MA, Turk MW, Burke LE. Adherence to a behavioral weight loss treatment program enhances weight loss and improvements in biomarkers. Patient Prefer Adherence. 2009;3:151–60. doi: 10.2147/ppa.s5802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. Am J Epidemiol. 1986;124:453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- Boutelle KN, Kirschenbaum DS. Further support for consistent self-monitoring as a vitalcomponent of successful weight control. Obes Res. 1998;6:219–24. doi: 10.1002/j.1550-8528.1998.tb00340.x. [DOI] [PubMed] [Google Scholar]
- Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Zurilla TJ, Goldfried MR. Problem solving and behavior modification. J Abnorm Psvchol. 1971;78:107–126. doi: 10.1037/h0031360. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, McKay HG, Botes SM, Vogt TM. Interactive computer technology, behavioral science, and family practice. J Fam Pract. 1999;48:464–470. [PubMed] [Google Scholar]
- Gold BC, Burke S, Pintauro S, Buzzell P, Harvey-Berino J. Weight loss on the web: a pilot study comparing a structured behavioral intervention to a commercial program. Obesity. 2007;15:155–164. doi: 10.1038/oby.2007.520. [DOI] [PubMed] [Google Scholar]
- Gustafson DH, Hawkins R, Boberg E, Pingree S, Serlin RE, Graziano F, Chan CL. Impact of a patient-centered, computer-based health information/support system. Am J Health Behav. 1999;16:1–9. doi: 10.1016/s0749-3797(98)00108-1. [DOI] [PubMed] [Google Scholar]
- Harvey-Berino J, Pintauro S, Buzzell P, Gold EC. Effect of internet support on the long-term maintenance of weight loss. Obes Res. 2004;12:320–329. doi: 10.1038/oby.2004.40. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Luborsky L. The role of the therapeutic alliance in psychotherapy. J Consult Clin Psychol. 1993;61:561–573. doi: 10.1037//0022-006x.61.4.561. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Wing RR, Thorsen C, Burton LR, Raether C, Harvey J, Mullen M. Strengthening behavioral interventions for weight loss: A randomized trial for food provision and monetary incentives. J Consult Clin Psychol. 1993;61:1038–1045. doi: 10.1037//0022-006x.61.6.1038. [DOI] [PubMed] [Google Scholar]
- Krukowski R, Harvey-Berino J, Ashikaga T, Thomas CS, Micco N. Internet-based weight control: the relationship between Web features and weight loss. Telemed J E Health. 2008;14:775–782. doi: 10.1089/tmj.2007.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumanyika S. Ethnic minorities and weight control research priorities: where are we now and where do we need to be? Prev Med. 2008;47:583–6. doi: 10.1016/j.ypmed.2008.09.012. [DOI] [PubMed] [Google Scholar]
- Kumanyika SK, Wadden TA, Shults J, Fassbender JE, Brown SD, Bowman MA, Wu X. Trial of family/friend support for weight loss in African American adults. Obes Res. 2009;17:S78. doi: 10.1001/archinternmed.2009.337. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health/National Heart, Lung, and Blood Institute Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. Obes Res. 1998;6:51s–210s. [PubMed] [Google Scholar]
- Micco N, Gold B, Buzzell P, Leonard H, Pintauro S, Harvey-Berino J. Minimal in-person support as an adjunct to internet obesity treatment. Ann Behav Med. 2007;33:49–56. doi: 10.1207/s15324796abm3301_6. [DOI] [PubMed] [Google Scholar]
- Ogden CL. Disparities in obesity prevalence in the United States: black women at risk. Am J Clin Nutr. 2009;89:1001–2. doi: 10.3945/ajcn.2009.27592. [DOI] [PubMed] [Google Scholar]
- Paffenbarger RS, Wing AL, Hyde RT. Physical activity as an indicator of heart attack risk in college alumni. Am J Epidemiol. 1978;108:161–175. doi: 10.1093/oxfordjournals.aje.a112608. [DOI] [PubMed] [Google Scholar]
- Perri MG, Nezu AM, McKelvey WF, Shermer RI, Renjilian DA, Viegener BJ. Relapse prevention training and problem solving therapy in the long-term management of obesity. J Consult Clin Psychol. 2001;69:722–726. [PubMed] [Google Scholar]
- Perry CL, Baranowski T, Parcel GS. How individuals, environments and health behavior interact: Social Learning Theory. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education: Theory. Research and Practice. Jossey-Bass; San Francisco: 1990. [Google Scholar]
- Procidano ME, Heller K. Measures of perceived social support from friends and from family: Three validation studies. Am J Community Psychol. 1983;11:1–24. doi: 10.1007/BF00898416. [DOI] [PubMed] [Google Scholar]
- Scagliusi FB, Polacow VO, Artioli GG, Benatti FB, Lancha AH. Selective underreporting of energy intake in women: magnitude, determinants, and effect of training. J Am Diet Assoc. 2003;103:1306–13. doi: 10.1016/s0002-8223(03)01074-5. [DOI] [PubMed] [Google Scholar]
- Tate D, Wing R, Winett R. Using Internet technology to deliver a behavioral weight loss program. JAMA. 2001;285:1172–1177. doi: 10.1001/jama.285.9.1172. [DOI] [PubMed] [Google Scholar]
- Tate D, Jackvony E, Wing R. Effects of Internet behavioral counseling on weight loss in adults at risk of type 2 diabetes: A randomized trial. JAMA. 2003;289:1833–1836. doi: 10.1001/jama.289.14.1833. [DOI] [PubMed] [Google Scholar]
- Tate D, Jackvony E, Wing R. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an internet weight loss program. Arch Intern Med. 2006;166:1620–1625. doi: 10.1001/archinte.166.15.1620. [DOI] [PubMed] [Google Scholar]
- Wadden TA, West DS, Delahanty LM, Jakicic JM, Rejeski WJ, Williamson DA, Berkowitz RI, Kelley DE, Tomchee CM, Hill JO, Kumanyika SK, The Look AHEAD Research Group The Look AHEAD study: A description of the lifestyle intervention and the evidence supporting it. Obesity. 2006;14:737–752. doi: 10.1038/oby.2006.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadden TA, Butryn ML, Wilson C. Lifestyle modification for the management of obesity. Gastroenterology. 2007;132:2226–2238. doi: 10.1053/j.gastro.2007.03.051. [DOI] [PubMed] [Google Scholar]
- West DS, DiLillo V, Bursac Z, Gore SA, Greene PG. Motivational interviewing improves weight loss in women with type 2 diabetes. Diabetes Care. 2007;30:1081–7. doi: 10.2337/dc06-1966. [DOI] [PubMed] [Google Scholar]
- Wing RR, Venditti E, Jakicic J, Polley BA, Lang W. Lifestyle intervention in individuals with a family history of diabetes. Diabetes Care. 1998;21:350–359. doi: 10.2337/diacare.21.3.350. [DOI] [PubMed] [Google Scholar]
- Wing R, Jeffery R. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult Clin Psychol. 1999;67:132–138. doi: 10.1037//0022-006x.67.1.132. [DOI] [PubMed] [Google Scholar]
- Writing Group of the PREMIER Collaborative Research Group Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003;289:2083–2093. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]