Abstract
Objective
To assess the efficacy of obstetric maneuvers for resolving shoulder dystocia, and the effect that these maneuvers have on neonatal injury when shoulder dystocia occurs.
Methods
Using an electronic database encompassing 206,969 deliveries, we identified all women with a vertex fetus beyond 34 0/7 weeks of gestation who incurred a shoulder dystocia during the process of delivery. Women whose fetuses had a congenital anomaly and women with an antepartum stillbirth were excluded. Medical records of all cases were reviewed by trained abstractors. Cases involving neonatal injury (defined as brachial plexus injury, clavicular or humerus fracture, or hypoxic ischemic encephalopathy or intrapartum neonatal death attributed to the shoulder dystocia) were compared to those without injury.
RESULTS
Among 132,098 women who delivered a term cephalic liveborn fetus vaginally, 2,018 incurred a shoulder dystocia (1.5%), and 101 (5.2%) of these incurred a neonatal injury. Delivery of the posterior shoulder was associated with the highest rate of delivery when compared to other maneuvers (84.4% compared with 24.3% to 72.0% for other maneuvers; P<.005 to P<.001) and similar rates of neonatal injury (8.4% compared with 6.1% to 14.0%; P=.23 to P=.7). The total number of maneuvers performed significantly correlated with the rate of neonatal injury (P<.001).
CONCLUSIONS
Delivery of the posterior shoulder should be considered following McRoberts maneuver and suprapubic pressure in the management of shoulder dystocia. The need for additional maneuvers was associated with higher rates of neonatal injury.
Introduction
Shoulder dystocia remains an important cause of neonatal and maternal injury with a reported incidence between 0.6% and 1.4% of vaginal births (1). Maternal injuries include a higher rate of postpartum hemorrhage and fourth degree lacerations(2). Major neonatal injuries attributed to shoulder dystocia include brachial plexus palsies, fractures of the clavicle and humerus, hypoxic ischemic encephalopathy and in rare cases, neonatal death(1). Fortunately, only a minority of shoulder dystocias result in neonatal injury with reported rates of injury ranging from 4% to 40% of cases(1). Nonetheless, shoulder dystocia remains a challenge to birth attendants as shoulder dystocia is among the four largest causes of monetary awards for obstetrical tort cases in the United States.(3)
Efforts to address shoulder dystocia have focused mainly on training in the acute management of shoulder dystocia and developing risk strategies to identify women at risk for shoulder dystocia so that a prophylactic cesarean delivery could be considered. Although numerous attempts to identify women at risk for shoulder dystocia have been made, the sensitivity and specificity of these efforts have been poor(4–6). Thus, the large number of prophylactic cesarean deliveries that would be needed to avoid a single (7)case of shoulder dystocia resulting in a permanent neonatal injury poses a prohibitive financial cost and would result in substantial maternal morbidity(6).
Physician and nurse training in the acute management of shoulder dystocia has been widely accepted despite there being little objective evidence that this training impacts neonatal and maternal injuries(7). This may in part due to the fact that the maneuvers utilized and the order in which they are performed are largely based on provider preference, expert opinion and theoretical models (8)(9). Little objective study of the different maneuvers and their impact on neonatal injury has been performed. The objective of this study was to estimate the efficacy obstetric maneuvers for resolving shoulder dystocia and the impact that these maneuvers have on neonatal injury when shoulder dystocia occurs by examining a large cohort of women and their neonates in whom shoulder dystocia was encountered.
Methods
The Consortium on Safe Labor was formed in response to a request issued by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Members of this group were selected based on numerous criteria including a history of archiving data from hospital based electronic medical records and geographic representation from the 9 ACOG districts. The 12 centers in the consortium were able to retrospectively aggregate maternal and neonatal outcomes from 228,668 women who delivered 233,844 infants during the time period of 2002-08. Institutional review board approval was obtained from all 12 centers, NICHD and the EMMES Corporation prior to the initiation of the project. Among women who had sequential births during the time course of the study, information was only collected from their first delivery.
Women who incurred a shoulder dystocia during the process of vaginal delivery were identified among this cohort. Cases were initially identified by examining either direct physician and/or nursing entry in the medical record or ICD-9 codes, depending upon the individual centers’ use of electronic medical records. Identified cases were included, if they required either an additional obstetrical maneuver or had a documented delivery of head to body time of 60 seconds or greater. Women were included if they delivered a singleton, vertex fetus beyond 34 and 0/7 weeks. Cases of major fetal anomalies and fetal death prior to the onset of the second stage of labor were excluded. Women who had a cesarean delivery following cephalic replacement (Zavanelli maneuver) were included. Following initial identification, all cases of shoulder dystocia were confirmed and the entire medical records of both the mother and her newborn were reviewed by trained obstetrical abstractors using a common abstraction form.
Our two primary outcomes of interest were successful use of a maneuver leading to delivery of the neonate and development of a neonatal injury attributable to the management of the shoulder dystocia. For the purposes of this analysis, neonatal injury was strictly defined as a brachial plexus injury (Erb’s palsy or Klumpke’s palsy), non-intentional fracture of the clavicle or humerus diagnosed by radiography, and/or hypoxic ischemic encephalopathy or neonatal death attributable to the management of the shoulder dystocia. Brachial plexus injuries were deemed present if they were assessed by an attending physician and attributed in the final diagnosis. Rule out diagnoses were not included. Cases of hypoxic ischemic encephalopathy were initially identified through chart abstraction if they had an Apgar score<4 at 5 minutes. Cases of hypoxic ischemic encephalopathy also needed to have an umbilical cord pH < 7.0, base deficit >12mmol and neurologic sequelae (seizures, coma, hypotonicity within 72 hours of birth) or multiple organ involvement (kidneys, lung, heart) Bruising, cephalohematomas or other soft tissue injuries that might have resulted from the management of the shoulder dystocia were not classified as neonatal injuries. Because of the retrospective nature of our study, we attributed success of a maneuver if it was clearly described as the last or only maneuver that relieved the shoulder dystocia. If the nature of the documentation was such that the multiple maneuvers were used and the final maneuver culminating in delivery could not be determined, then we excluded these deliveries in our analysis of success. Our primary exposure of interest was the maneuvers which were employed to relieve the shoulder dystocia. For the purpose of classification these were divided into the following categories: McRoberts maneuver, suprapubic pressure, Rubin maneuver, delivery of the posterior shoulder, Woods corkscrew maneuver, Gaskin maneuver (delivery in the maternal knee chest position), Zavanelli maneuver, and fundal pressure. We did not differentiate use of “prophylactic” maneuvers, such as McRoberts, from therapeutic maneuvers. Primary management was attributed to the attending physician, midwife or resident who delivered the neonate and thus initiated the maneuvers. Other variables in the acute obstetrical management of these patients were also garnered from the chart.
Categorical variables were evaluated using a Chi-square test or Fisher’s exact test when appropriate. Continuous variables were analyzed using a Student’s t-test with unequal variance or Wilcoxon rank sum test if indicated. The Cochran-Armitage test for trend was used where appropriate.
It was recognized that a potential bias of attributing a fetal injury to a specific maneuver might occur due to the non-random way in which they were employed in clinical practice. In other studies, secondary maneuvers (i.e., delivery of the posterior shoulder, Woods corkscrew and Rubin’s maneuver) were more likely to be used in more difficult cases after primary maneuvers (McRoberts maneuver and suprapubic pressure) had been unsuccessful(1). Moreover, neonates could be exposed to multiple maneuvers confounding attribution of an injury to a specific maneuver. We thus took two approaches to examining this issue. One approach was to compare the rate of fetal injury by the maneuver that successfully relieved the shoulder dystocia. Multivariate Logistic regression was used to examine the association between maneuver type, potential exposure to multiple maneuvers and successful delivery and neontatal injury, adjusting for site, maternal age, maternal race, parity and birthweight. As a successful vaginal delivery occurred in all cases save one excluded case, we chose to perform a repeated measures analysis using GENMOD controlling for these same variables. Statistical analysis was performed by the EMMES Corporation which served as the data coordinating center for this project using Statistical Analysis Software (Version 9.1., SAS Institute Inc., Cary, NC) and STATA (Version 10.0. STATA Corporation, College Station, TX).
Results
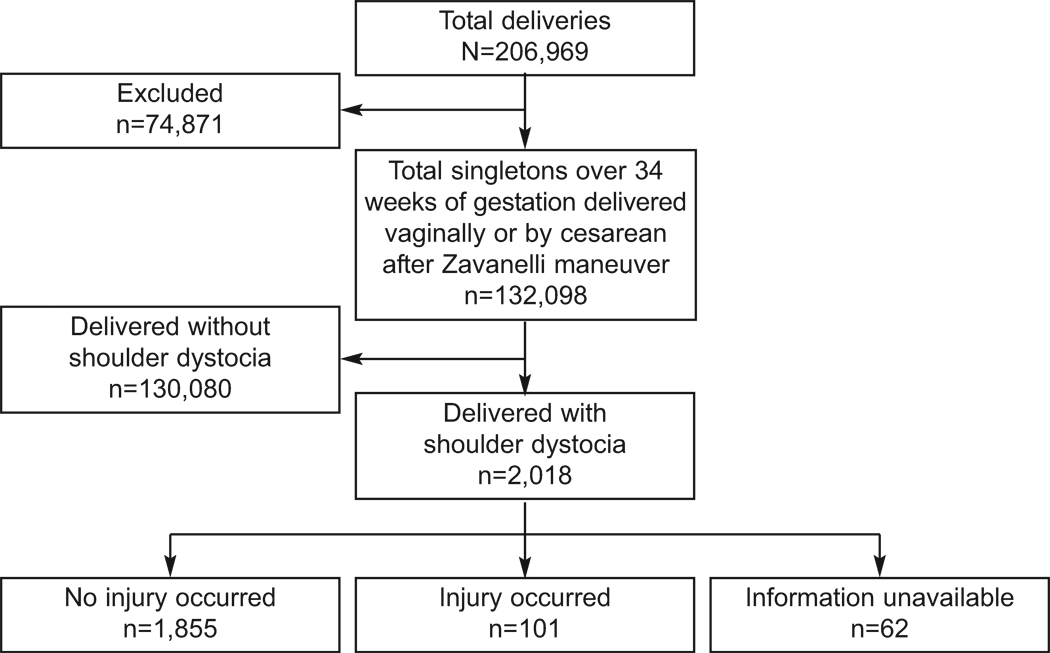
Among the total cohort of 228,668 women, 206,969 had either a single birth or first birth included in the analyzed cohort. Of this group, 132,098 delivered a singleton vertex liveborn fetus vaginally and a single neonate underwent cephalic replacement with cesarean delivery (Zavenelli maneuver) beyond 34 and 0/7 weeks gestation; thus, the total population included 132,098 deliveries. A total of 2,018 cases of shoulder dystocia were reported (average 1.5%-institutional ranges from 0.2 % to 3.0%). Information regarding neonatal injury was unavailable in 62 of these 2018 neonates. A total of 101 neonates incurred a neonatal injury (5.2% 95% CI 4.1% to 6.2 %), 1855 did not suffer an injury, and in 62 no information was available (See Figure 1). The types and natures of the neonatal injuries are presented in Table 1. The most common neonatal injury was an Erb’s Palsy (59.4% 95% CI 49.6% to 69.1%) followed by a clavicular fracture (38.6% 95% CI 29.3% to 48.7%). A total of eight fetuses incurred multiple injuries. No cases of neonatal death attributable to shoulder dystocia occurred although 6/101 (5.9% 95% CI 1.2% to 10.7%) had hypoxic ischemic encephalopathy
Figure 1.
Flow of participants through the study.
Table 1.
Neonatal Injuries (N=101)
| Type of Injury | N | Percentage* |
|---|---|---|
| Erb's Palsy | 60 | 59.4% |
| Klumpke's Palsy | 4 | 4.0% |
| Clavicular Fracture | 39 | 38.6% |
| Humerus Fracture | 2 | 2.0% |
| Hypoxic Ischemic Encephalopathy | 6 | 5.9% |
| Neonatal Death | 0 | 0.0% |
Ten fetuses incurred multiple injuries
Maternal & Neonatal demographics are presented in Table 2. Women whose fetuses incurred a neonatal injury tended to be younger, Black/non-Hispanic and less parous. As would be anticipated, the mean weight of the infants with a neonatal injury was greater; however, the mean difference in the two groups was only 92 grams.
Table 2.
Maternal and Neonatal Variables
| Variable | With neonatal injury |
Without neonatal injury |
P- value |
|---|---|---|---|
| Maternal age years (mean) | 25.9 | 27.8 | 0.002 |
| Maternal: Race(%) | 0.0009 | ||
| White/non-hispanic | 44.1% | 54.5% | |
| Black/non-hispanic | 38.7% | 22.4% | |
| Hispanic | 17.2% | 19.8% | |
| Asian/Pacific Islander | 0.0% | 3.2% | |
| Gravidity (mean) | 2.3 | 2.8 | 0.01 |
| Parity(Mean) | 0.8 | 1.2 | 0.002 |
| BMI(kg/m2) at admission | 35.6 | 32.3 | <0.001 |
| Pre Gestational Diabetes | 9.70% | 4.5 | 0.02 |
| Gestational Diabetes | 6.80% | 6 | 0.74 |
| Regional Anesthesia(%) | 95.8% | 87.1% | 0.1 |
| Newborn birth weight(g) (mean) | 3944 | 3852 | 0.04 |
| Second Stage of labor Minutes | 0.569 | 57.9 | 0.9 |
Obstetrical management is detailed in Table 3. No significant differences were seen in injury rates when the shoulder dystocia was primarily managed by resident physicians compared to midwives or attending physicians (rate of injury Attending Physicians 5.2%, Midwives 2.9%, Resident physicians 7.4%- p values 0.099). Shoulder dystocia cases occurring after an operative vacuum vaginal delivery were more likely to incur a neonatal injury compared to those when the head delivered spontaneously (22.8% vs. 14.5%, respectively; p-value= 0.031). A similar trend was not seen with forceps though the small numbers of forceps deliveries precludes meaningful comment on this issue. Though a statistically significant difference in the type of operative vaginal delivery (Mid, Low, Outlet, Not recorded) was noted, this mostly reflects the higher rate of “not recorded” seen in patients without neonatal injury. In cases involving a neonatal injury it would be anticipated that documentation would be more complete which may explain this finding. When a vacuum assisted vaginal delivery was performed, neither the number of “popoffs” nor duration of vacuum usage reported differed between women whose neonates incurred an injury and those who did not.
Table 3.
Obstetric Interventions
| Category | With fetal injury N(%) |
Without fetal injury N(%) |
P-value* |
|---|---|---|---|
| Labor and delivery performed by | 0.099 | ||
| Attending | 72(71.3%) | 1318(71.2%) | |
| Resident | 21(20.8%) | 262(14.2%) | |
| Nurse midwife | 8(7.9%) | 269(14.5%) | |
| Medical student | 0(0.0%) | 2(0.1%) | |
| Vacuum | 22(22.8%) | 264(14.4%) | 0.025 |
| Forceps | 3(3.0%) | 54(2.9%) | 0.928 |
| Type of forceps or vaccum/forceps | 0.0059 | ||
| Mid | 1(4.0%) | 4(1.3%) | |
| Low | 7(28.0%) | 127(39.9%) | |
| Outlet | 13(52.0%) | 68(21.4%) | |
| Not recorded | 4(16.0%) | 119(37.4%) | |
| Duration of Operative delivery(minutes) | 3.08 | 3.46 | 0.6908 |
| Recorded No. of "Popoffs" | 0.88 | 0.98 | 0.7273 |
| Episiotomy | 42(42.0%) | 472(26.0%) | 0.0008 |
Note the unit of analysis is by maneuver attempted- as such women with multiple maneuvers can appear in multiple columns.
In terms of obstetrical maneuvers to relieve shoulder dystocia, a total of 3,751 maneuvers were performed in 2,016 of the 2,018 cases (average number of maneuvers per case 1.86). The maneuvers utilized to relieve the shoulder dystocia are presented in Table 4. Due to their low rate of utilization, the Gaskin maneuver (performed 22 times with 1 neonatal injury), Zavanelli maneuver (performed 1 time) and fundal pressure (utilized in 3 cases) are not presented in Table 4. In 65.7% of cases the order in which the maneuver was utilized could be determined. Reporting ranges were noted to be similar among the measures ranging from 58.1% to 70.2%.
Table 4.
Outcomes of Obstetric Maneuvers
| Rate of Success with a Particular Maneuver | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Maneuver | Total N |
N with order documented | First | Second | Third | Fourth | Fifth+ | P-value' | Overall | P-value |
| McRoberts | 1679 | 1123 (66.9%) | 213/918 (23.2%) | 49/186 (26.3%) | 11/19 (57.9%) | -- | -- | 0.0067 | 273/1123 (24.3%) | <0.001 |
| Suprapubic pressure | 1386 | 875 (63.1%) | 58/116 (50.0%) | 406/635 (63.9%) | 74/116 (63.8%) | 6/8 (75.0%) | -- | 0.0002 | 544/875 (62.2%) | <0.001 |
| Delivery of posterior shoulder | 262 | 179 (68.3%) | 7/8 (87.5%) | 28/32 (87.5%) | 55/73 (75.3%) | 40/45 (88.9%) | 21/21 (100.0%) | 0.4642 | 151/179 (84.4%) | Referrant |
| Rubin maneuver | 86 | 50 (58.1%) | 4/6 (66.7%) | 4/5 (80.0%) | 16/27 (59.3%) | 9/12 (75.0%) | -- | 0.7760 | 33/50 (66.0%) | <0.005 |
| Woods corkscrew | 315 | 221 (70.2%) | 14/19 (73.7%) | 27/34 (79.4%) | 78/114 (68.4%) | 35/49 (71.4%) | 5/5 (100.0%) | 0.7031 | 159/221 (72.0%) | <0.005 |
| Rate of Injury with Attempted Maneuver | ||||||||||
| Maneuver | N with order documented | First | Second | Third | Fourth | Fifth+ | P-value' | Overall | ||
| McRoberts | 1679 | 1123(66.9%) | 51/918 (5.6%) | 15/186 (8.1%) | 2/19 (10.5%) | -- | -- | 0.15 | 68/1123 (6.1%) | 0.25 |
| Suprapubic pressure | 1386 | 875(63.1%) | 6/116 (5.17%) | 39/635 (6.1%) | 10/116 (8.6%) | 1/8 (12.5%) | -- | 0.26 | 56/875 (6.4%) | 0.34 |
| Delivery of posterior shoulder | 262 | 179(68.3%) | 0/8 (0.0%) | 0/32 (0.0%) | 2/73 (2.7%) | 8/45 (17.78%) | 5/21 (23.8%) | <.0001 | 15/179 (8.4%) | Referrant |
| Rubin maneuver | 86 | 50(58.1%) | 0/6 (0.0%) | 0/5 (0.0%) | 5/27 (18.5%) | 2/12 (16.7%) | -- | 0.27 | 7/50 (14.0%) | 0.23 |
| Woods corkscrew | 315 | 221(70.2%) | 0/19 (0.0%) | 0/34 (0.0%) | 13/114 (11.4%) | 7/49 (14.3%) | 1/5 (20.0%) | 0.01 | 21/221 (9.5%) | 0.7 |
"Conchran-Amitage for trend" Delivery of Posterior Shoulder used as referent
When examining the number of deliveries that included the different maneuver types, irrespective of order 84.4% of deliveries had successful resolution of the shoulder dystocia when delivery of posterior shoulder was attempted. This was higher than the other maneuvers which ranged from 24.3% (McRoberts) to 72.0% (Woods corkscrew) (Table4). Recognizing that McRoberts and suprapubic pressure are the primary maneuvers recommended by ACOG, we chose to examine women who had already undergone these maneuvers and examine only the third manuever after McRoberts and suprapubic pressure had failed. Given the potential for biases due to differences in maternal age, maternal race, parity, neonatal birthweight and site of care we chose to control for these potential confounders using logistic regression. When compared to delivery of the posterior shoulder, we found that Rubins Maneuver was clearly less successful (OR 0.33 95% CI 0.11 to 0.98 P- value<0.05). Using this methodology, Woods corkscrew was not less successful (OR 0.58 95% CI 0.26 to 1.3 P-value 0.20), though this may reflect the small numbers of patients who underwent this maneuver as the third manuever. None of the maneuvers demonstrated a loss of efficacy when examined as to which order they were utilized and in fact both McRoberts and suprapubic pressure became more effective the later they were used. This suggests strongly that all maneuvers have potential benefit regardless of whether one has attempted prior maneuvers.
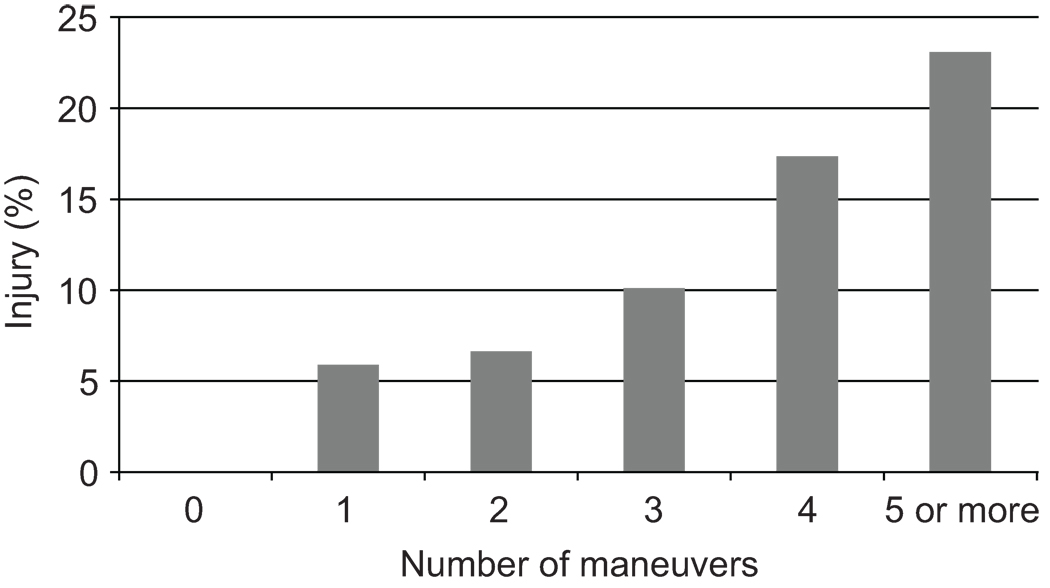
In regards to neonatal injury, as expected, managing shoulder dystocia that included the primary maneuvers of McRoberts and suprapubic pressure resulted in the lowest percent of neonates with an injury (6.1% to 14.0%). Both delivery of the posterior shoulder and the Woods corkscrew maneuver demonstrated a significant trend towards fetal injury if they were successful as the fourth or fifth maneuver. This trend could not be confirmed in neonates who were delivered by either the McRoberts maneuver or Suprapubic pressure; though these maneuvers were used sparingly beyond the second maneuver. Likewise, Rubins maneuver was not affected by its timing, but it was only performed in a limited number of cases (N=50). As anticipated, when examined from the perspective of only how many maneuver were performed rather than the specific maneuvers utilized, a strong association with the number of maneuvers and the risk of neonatal injury was demonstrated (Figure 2). This was particularly true upon utilization of a fourth maneuver.
Figure 2.
Percentage with injury by number of maneuvers.
We likewise examined the risk of being exposed to specific maneuvers and their association with neonatal injury through multiple logistic regression, after adjusting for maternal age, maternal race, parity, birthweight and site (Table 5). Because of this method, we were able to include use of all maneuvers and not just those that had clear documentation leading to successful delivery. Use of the Rubin and Woods corkscrew maneuvers were associated with a significantly higher risk of neonatal injury; though interestingly the only secondary maneuver not associated with injury was delivery of the posterior shoulder. This once again mostly likely reflects that these two maneuvers were used as secondary maneuvers and therefore in more difficult cases.
Table 5.
Multiple logistic regression of Neonatal injury based on exposure to Obstetric Maneuvers*
| Manuever | Odds Ratio(95%tile CI) | P Value |
|---|---|---|
| MacRoberts(N=1176) | 1. 43(0.53 to 3.86) | 0.48 |
| Suprapubic pressure(n=927) | 0.98(0.51 to 1.88) | 0.95 |
| Woods corkscrew(N=240) | 2.22(1.22 to 4.04) | 0.009 |
| Rubin maneuver(N=51) | 1.54(0.83 to 2.85) | 0.17 |
| Delivery of posterior shoulder(N=192) | 1.36(0.71 to 2.61.) | 0.358 |
Adjusted for Parity, Maternal age, Maternal Race, Site of Care and Birthweight
Recognizing both the rarity and importance of hypoxic ischemic encephalopathy(HIE) as a complication of shoulder dystocia, we chose to examine factors associated with our six cases. Among these cases the mean time of delivery between delivery of the head and the remainder of the body was 10,75 minutes (range 3 to 20 minutes) with all cases reporting 5+ maneuvers. Among these six cases, only one woman had diabetes and only one underwent a vacuum delivery. The mean birthweight of these neonates was 4246 grams.
An issue of concern secondary to the nature of the study is the heterogenous nature of the populations and approaches taken by the various centers. Statistically different rates of shoulder dystocia (P value<0.001) and fetal injury (P value<0.001) are reported by different centers within our study. We believe that these differences can largely be attributed to differences in important causes of shoulder dystocia that also differ between centers (e.g. birthweight, diabetes, and BMI (all P values <0.001). Nonetheless the clinical approach to these patients, which is the primary focus of this investigation, remains relatively consistent with 10 of 12 centers using McRoberts and suprapubic pressure as the primary maneuvers in 100% of cases and the remaining two centers using them in 94.9% and 98.0% of cases.
Discussion
Our analysis validates that McRoberts maneuver and suprapubic pressure as are widely practiced as the primary steps to relieve shoulder dystocia and that these maneuvers are associated with low rates of neonatal injury. Our study also demonstrates that delivery of the posterior shoulder had the highest overall rate of success when compared to all other maneuvers. As quick resolution of shoulder dystocia is the primary goal, delivery of the posterior shoulder following the less technically demanding maneuvers of McRoberts and suprapubic pressure would be an appropriate approach. Likewise we were able to demonstrate that the risk of neonatal injury did increase with the number of maneuvers performed, a finding consistent with other investigations (10). This finding further strengthens the argument for using the most effective maneuver (delivery of the posterior shoulder) earlier in the approach to cases of shoulder dystocia. Interestingly our study did not demonstrate a loss of efficacy of any maneuver regardless of its timing. This would suggest that at no point in the acute management of shoulder dystocia should any maneuver be completely abandoned.
Few others have investigated success rates of particular maneuvers and their relationship to birth injury. Our findings are similar to those of Chauhan et al who were likewise unable to identify any particular maneuver associated with a lower risk of neonatal injury (10). A Cochrane review of prophylactic McRoberts maneuvers suggested that its use decreased the risk of shoulder dystocia; however, this study did not demonstrate the more important outcome of whether prophylactic use of this maneuver minimizes neonatal injury (11).Poggi et al, were able to demonstrate that delivery of the posterior shoulder was associated with a marked decrease in the degree of obstruction in a geometric analysis (12). Likewise, in a computer model, Grimm et.al determined that delivery of the posterior arm lead to a 71% decrease in anterior nerve stretch and an 80% reduction in delivery force. (13) We were able to validate these models in clinical practice by demonstrating that delivery of the posterior shoulder was the most effective maneuver for the acute resolution of shoulder dystocia.
While our study did not show differences based on experience, recently two studies have been able to demonstrate lower rates of neonatal injury following implementation of drill based training (14); though this finding has not been universal (7). We believe that these drills should emphasize delivery of the posterior shoulder as the third maneuver to allow providers to become more facile and comfortable with its performance.
Our study also demonstrated that HIE is a very rare complication of shoulder dystocia with only 6 instances in 2,018 cases. All of these cases required five or more maneuvers to resolve the shoulder dystocia and were associated with a mean prolonged delivery time of 10.75 minutes. The rarity of this complication coupled with the need for multiple maneuvers and prolonged time of delivery highlight the extreme degree of difficulty in resolving these cases. Nonetheless, the small number of cases precludes meaningful comment on optimal management or prediction of these rare cases.
Some of the strengths of this study include the fact that it includes a large cohort of women delivered in multiple hospitals that are geographically diverse. Moreover, we included the entire cohort of eligible cases at each of the 12 institutions during the study period. Moreover, data were abstracted by trained research personnel who followed a common abstraction form with consistent definitions.
Limitations of the study include the operational definition of shoulder dystocia rather than objective parameters; a weakness of virtually all shoulder dystocia studies. Nonetheless, virtually all of our cases (2016 of 2018) had documentation of the use of maneuvers beyond gentle downward traction which is in keeping with the definition provided by the American College of Obstetricians and Gynecologists(1). The remaining two patients were documented to have a head to body delivery time of greater than 60 seconds. While all cases of shoulder dystocia used in the study were confirmed as actual cases, the method to initially identify cases varied in different centers; some used ICD9 coding information while others obtained this directly from their electronic medical record. Thus, there may have been differences in the sensitivity of our screening between centers.
Likewise, due to the retrospective nature of the study, we are unable to assess site differences(e.g. training in shoulder dystocia, nursing response, etc.) which may have influenced both the clinical approach to shoulder dystocia and in turn the avoidance of fetal injury. Nonetheless, we were able to demonstrate that for the overwhelming majority of patients, the currently ACOG recommended approach of McRoberts maneuver and suprapubic pressure are widely adhered to suggesting some uniformity in approach at the site level
Another limitation of our study is that our definition of neonatal injury did not differentiate those injuries that were permanent from those that spontaneously resolved. The majority of cases of brachial plexus injury (our most common injury) will resolve, suggesting that our study overestimates the rate of permanent fetal injury associated with the treatment of shoulder dystocia. Lastly, we recognize that abstracted clinical documentation can vary in its accuracy.
In summary, we were able to clearly demonstrate that delivery of the posterior shoulder was superior to other maneuvers in the acute management of shoulder dystocia with comparable rate of neonatal injury. Based on our data, we strongly encourage the early use of maneuvers to deliver the posterior shoulder when a shoulder dystocia is encountered.
Acknowledgments
Supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, through a contract (Contract No. HHSN267200603425C).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure: The authors did not report any potential conflicts of interest.
References
- 1.ACOG Committee on Practice Bulletins-Gynecology, The American College of Obstetrician and Gynecologists. ACOG practice bulletin clinical management guidelines for obstetrician-gynecologists. number 40, november 2002. Obstet Gynecol. 2002 Nov;100(5 Pt 1):1045–1050. doi: 10.1016/s0029-7844(02)02513-9. [DOI] [PubMed] [Google Scholar]
- 2.Gherman RB, Goodwin TM, Souter I, Neumann K, Ouzounian JG, Paul RH. The McRoberts' maneuver for the alleviation of shoulder dystocia: How successful is it? Am J Obstet Gynecol. 1997 Mar;176(3):656–661. doi: 10.1016/s0002-9378(97)70565-9. [DOI] [PubMed] [Google Scholar]
- 3.Mavroforou A, Koumantakis E, Michalodimitrakis E. Physicians' liability in obstetric and gynecology practice. Med Law. 2005 Mar;24(1):1–9. [PubMed] [Google Scholar]
- 4.Lewis DF, Edwards MS, Asrat T, Adair CD, Brooks G, London S. Can shoulder dystocia be predicted? preconceptive and prenatal factors. J Reprod Med. 1998 Aug;43(8):654–658. [PubMed] [Google Scholar]
- 5.Mazouni C, Porcu G, Cohen-Solal E, Heckenroth H, Guidicelli B, Bonnier P, et al. Maternal and anthropomorphic risk factors for shoulder dystocia. Acta Obstet Gynecol Scand. 2006;85(5):567–570. doi: 10.1080/00016340600605044. [DOI] [PubMed] [Google Scholar]
- 6.Rouse DJ, Owen J. Prophylactic cesarean delivery for fetal macrosomia diagnosed by means of ultrasonography--A faustian bargain? Am J Obstet Gynecol. 1999 Aug;181(2):332–338. doi: 10.1016/s0002-9378(99)70557-0. [DOI] [PubMed] [Google Scholar]
- 7.MacKenzie IZ, Shah M, Lean K, Dutton S, Newdick H, Tucker DE. Management of shoulder dystocia: Trends in incidence and maternal and neonatal morbidity. Obstet Gynecol. 2007 Nov;110(5):1059–1068. doi: 10.1097/01.AOG.0000287615.35425.5c. [DOI] [PubMed] [Google Scholar]
- 8.Gonik B, Zhang N, Grimm MJ. Prediction of brachial plexus stretching during shoulder dystocia using a computer simulation model. Am J Obstet Gynecol. 2003 Oct;189(4):1168–1172. doi: 10.1067/s0002-9378(03)00578-7. [DOI] [PubMed] [Google Scholar]
- 9.Gherman RB, Chauhan S, Ouzounian JG, Lerner H, Gonik B, Goodwin TM. Shoulder dystocia: The unpreventable obstetric emergency with empiric management guidelines. Am J Obstet Gynecol. 2006 Sep;195(3):657–672. doi: 10.1016/j.ajog.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 10.Chauhan SP, Christian B, Gherman RB, Magann EF, Kaluser CK, Morrison JC. Shoulder dystocia without versus with brachial plexus injury: A case-control study. J Matern Fetal Neonatal Med. 2007 Apr;20(4):313–317. doi: 10.1080/14767050601165805. [DOI] [PubMed] [Google Scholar]
- 11.Athukorala C, Middleton P, Crowther CA. Intrapartum interventions for preventing shoulder dystocia. Cochrane Database Syst Rev. 2006 Oct 18;4(4) doi: 10.1002/14651858.CD005543.pub2. CD005543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Poggi SH, Spong CY, Allen RH. Prioritizing posterior arm delivery during severe shoulder dystocia. Obstet Gynecol. 2003 May;10(15 Pt 2):1068–1072. doi: 10.1016/s0029-7844(02)02332-3. [DOI] [PubMed] [Google Scholar]
- 13.Grimm MJ, Costello RE, Gonik B. Effect of clinician-applied maneuvers on brachial plexus stretch during a shoulder dystocia event: Investigation using a computer simulation model. Am J Obstet Gynecol. 2010 Oct;203(4) doi: 10.1016/j.ajog.2010.05.002. 339.e1,339.e5. [DOI] [PubMed] [Google Scholar]
- 14.Grobman W, Miller DA, Burke C, Hornebogen A, Costello R. Clinical outcomes associated with implementation of a shoulder dystocia protocol. American Journal of Obstetrics & Gynecology. 2009;201(6):S125. doi: 10.1016/j.ajog.2011.05.002. [DOI] [PubMed] [Google Scholar]