Abstract
Overnutrition characterized by overconsumption of food rich in fat and carbohydrates is a significant contributor to hypertension, type 2 diabetes, and the cardiorenal syndrome. Overnutrition activates the renin-angiotensin-aldosterone system (RAAS) and causes chronic exposure of cardiovascular and renal tissue to increased circulating nutrients, insulin (INS), and angiotensin II (ANG II). Emerging evidence suggests that overnutrition, aldosterone, and ANG II promote INS resistance, a chronic condition that underlies these co-morbidities, through activation of the mammalian target of the rapamycin (mTOR)/S6 kinase 1 (S6K1) signaling pathway in cardiovascular tissue and the kidney. However, a novel ANG II type 2 receptor (AT2R)-mediated cross talk between the RAAS and mTOR pathways ameliorates overnutrition-induced activation of mTOR/S6K1 signaling in cardiovascular tissue of rats, mice, and humans and confers cardioprotection.
Key Words: Overnutrition, Hypertension, Insulin metabolic signaling, Progressive kidney disease
Introduction
Diminished insulin (INS) metabolic signaling is a common feature of disease states such as obesity, hypertension, diabetes, and the cardiorenal metabolic syndrome (CRS). Overnutrition (especially that characterized by excess intake of fat and carbohydrates) is a major factor in the increased prevalence of hypertension, CRS, and diabetes. These co-morbidities may be driven by decreases in INS-mediated vascular relaxation, and glucose transport in cardiovascular (CV) and skeletal muscle tissue [1,2,3,4,5,6,7]. In addition to overnutrition, several other mechanisms, such as enhanced activation of the renin-angiotensin-aldosterone system (RAAS), inflammation, and associated abnormalities in INS metabolic signaling, may help explain the linkage between INS resistance, hypertension and the CRS [8,9,10,11,12,13,14,15].
There is emerging evidence that overnutrition, aldosterone and angiotensin (ANG) II may promote INS resistance through the mammalian target of rapamycin (mTOR)/S6 kinase 1 (S6K1) signaling pathway. The mTOR molecule, a highly conserved nutrient sensor, modulates INS metabolic signaling through its phosphorylation [(P)] of S6K1, an evolutionarily conserved serine (Ser) kinase [16,17,18,19,20,21]. Evidence is mounting that chronic activation of S6K1, by excessive nutrients, promotes INS resistance in fat, liver, heart, skeletal muscle, and renal tissue through increased Ser(P) of the critical INS signaling/docking molecule, INS receptor substrate protein-1 (IRS-1), leading to impaired phosphoinositol 3-kinase (PI3-K) engagement and protein kinase B (Akt) stimulation [21,22,23]. Our recent work indicates that S6K1 is activated in CV tissue of an overnutrition rodent model that exhibits diminished INS metabolic signaling and biological consequences, such as impaired nitric oxide (NO)-mediated vascular relaxation, cardiac diastolic dysfunction, and promotion of kidney tubulointerstitial fibrosis.
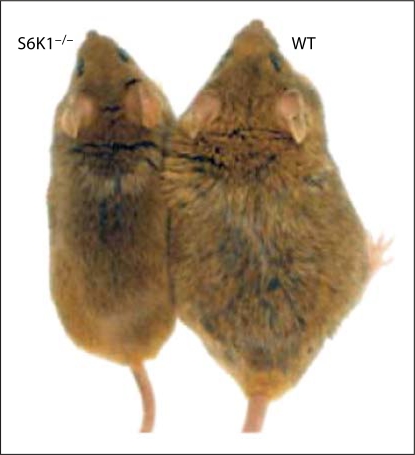
Research conducted in classically INS-sensitive tissue, such as muscle and liver, indicates that S6K1 is activated in conditions of INS resistance due to excessive intake of fat, sucrose, and protein [17,18,19,20]. Evidence for the importance of S6K1 signaling in INS resistance is based on findings that a murine knockout model of S6K1 mice maintained on a high-fat diet still remains INS sensitive (fig. 1) and siRNA knockdown of S6K1 protein in cells potentiates INS metabolic signaling [16]. Further, Ser(P) of IRS-1 was reduced in S6K1−/– mice and siRNA-treated cells [16]. Studies conducted in fibroblasts exhibiting constitutive S6K1 activation revealed that certain IRS-1 Ser moieties (Ser265, Ser302, Ser632, and Ser1097 of mouse IRS-1) are substrates for S6K1 [22]. In man, overnutrition-related reductions in glucose disposal are associated with overactivation of S6K1 and IRS-1 Ser(P) [19]. Thus, S6K1 is a convergence point that has evolved to suppress INS metabolic signaling under conditions of nutrient overload.
Fig. 1.
Wild-type (WT) and S6K1−/– mice after 6 months of high-fat diet. Reprinted with permission from Macmillan Publishers Ltd. (Nature[16], Copyright 2004).
Over the past several years, we have explored the mechanisms by which ANG II and aldosterone contribute to CV and skeletal muscle INS resistance [2,10]. Recent research from our laboratory suggests that ANG II may inhibit INS metabolic signaling in CV tissue, in part by promoting S6K1-mediated IRS-1 Ser(P). This work in cultured endothelial cells and cardiomyocytes, and in ex vivo CV and skeletal muscle tissue, suggests that excessive Ser(P) of IRS-1 interferes with IRS-1/phosphoinositol 3-kinase (PI3-K) docking and the consequent activation of Akt. In skeletal muscle, cardiomyocytes and vascular smooth muscle cells (VSMCs), the PI3-K/Akt pathway stimulates glucose transporter-4 (GLUT4) recruitment to the plasma membrane resulting in glucose uptake in all three tissues, as well as relaxation of the vasculature [24,25] and diastolic relaxation of the heart [26,27,28]. INS-mediated signaling via this pathway promotes INS-induced vasorelaxation through increased endothelial NO synthase (eNOS) activity and reductions in myosin light chain (MLC) activation in VSMCs and decreases in calcium (Ca2+) in cardiac tissue [29].
Utilizing rodent models of RAAS activation (ANG II-infused C57BL/6 mice and transgenic Ren2 rats) and overnutrition [db/db mice and Zucker Obese (ZO) rats], we have recently made the novel observation that cardiac and skeletal muscle S6K1 activation and Ser(P) of IRS-1 is increased in concert with reduced tissue INS metabolic signaling [2,6,10]. In vivo treatment with a low dose of ANG II type 1 receptor (AT1R) blocker substantially reduced S6K1 activation/IRS-1 Ser(P) and improved INS metabolic signaling. Emerging data suggest that AT1R-mediated activation of mTOR/S6K1 signaling is involved in cardiac hypertrophy and increases protein synthesis in VSMCs [30,31,32]. Thus, AT1R-induced mTOR/S6K1 activation interferes with INS metabolic signaling and biological responses in CV as well as other tissues.
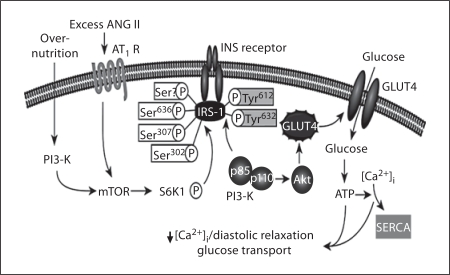
CV Effects of Overnutrition and RAAS (mTOR/S6K1)-Mediated INS Resistance
INS induces vasodilation by enhancing Akt stimulation of eNOS(P) activation and NO production. The role of INS-stimulated IRS-1 tyrosine (Tyr) (P) in mediating eNOS activation is underscored by the observation that IRS-1 overexpression in aortic endothelial cells increases NO production [33], and introduction of a mutant IRS-1 unable to bind to the p85 subunit of PI3-K [33] reduces INS-stimulated NO production. In VSMC, ANG II increases intracellular calcium ([Ca2+]i) and promotes MLC kinase activation [34]. INS decreases ANG II-induced increases in VSMC [Ca2+]i and MLC kinase activity [1]. INS normally promotes myocardial glucose uptake and utilization, mechanical-electrical coupling and diastolic relaxation via signaling through the IRS-1/PI3-K/Akt pathway [35,36,37] (fig. 2). INS metabolic signaling increases coronary vessel NO production which, in turn, contributes to the beneficial effects of INS on glucose uptake, coronary blood flow, and diastolic relaxation [36,37,38,39,40,41]. These observations suggest coupling between the metabolic and coronary vascular actions of INS metabolic signaling in the heart. These beneficial cardiac effects of INS metabolic signaling are decreased in states of INS resistance [37,38,39,40,41,42,43,44]. We have observed ANG II-induced inhibition of NO production can be reversed by inhibition of mTOR/S6K1 in endothelial cells. Cardiomyocytes and cardiac fibroblasts express high-affinity AT1R [10] and many of the adverse effects of ANG II are due to AT1R-mediated signaling.
Fig. 2.
Function/metabolic effects of INS in cardiac muscle cells.
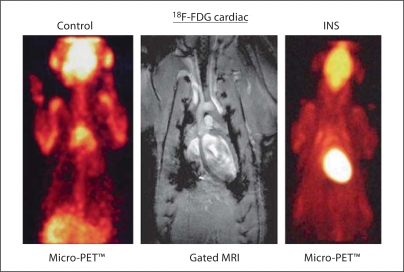
To evaluate the cardiac functional effects of INS metabolic signaling we utilize positron emission tomography (PET). In the INS-resistant state, myocardial glucose uptake and metabolism is impaired, leading to diastolic dysfunction, attenuated myocardial blood flow, and impaired ischemic reconditioning. PET imaging, using 18F-deoxyglucose (18FDG), is used to evaluate INS-stimulated glucose uptake (fig. 3) [41,45]. We have utilized magnetic resonance imaging in conditions of overnutrition and excessive tissue RAAS activation, and have demonstrated impaired/prolonged diastolic relaxation [7]. We have further demonstrated that both impaired INS-stimulated glucose uptake and diastolic dysfunction are related to impaired systemic and myocardial INS metabolic signaling in models of obesity and increased tissue RAAS expression [2,7]. Interestingly, we have also observed that drug treatments that improved INS resistance in rodent models of overnutrition attenuated mTOR/S6K1 signaling. Collectively, these observations indicate that a combination of enhanced tissue RAAS activation and a westernized high-sucrose/high-fat diet will reduce INS metabolic signaling and enhance mTOR/S6K1 activation to a greater extent than either intervention alone.
Fig. 3.
Micro-PET determination of INS/glucose uptake [Cooper, Am J Physiol Heart Circ Physiol, 2007; American Physiological Society, used with permission].
AT2R↔mTOR Signaling Loop in Overnutrition, Hyperinsulinemia, and Excess RAAS Activation
Accumulating evidence suggests that AT2R is a modulator of cardiac pathology [46,47,48,49,50,51]. AT2R is up-regulated in failing human hearts [50], the vasculature of diabetic patients [47], and animal models of INS resistance, myocardial infarction, senescence, and hyperinsulinemia [49,52]. AT2R signaling reduces fibroblast growth and myocardial hypertrophy [53]. The suppression of AT2R activation interferes with anti-hypertrophic/anti-fibrotic effects of AT1R blockade in experimental myocardial infarction [54,55,56,57,58]. In cardiomyocyte-specific AT2R transgenic mice, moderate overexpression of AT2R in ventricular myocytes is cardioprotective under conditions of pressure overload induced by aortic banding [54]. On the other hand, excessive AT2R overexpression in ventricular myocytes leads to dilated cardiomyopathy [56].
Signaling pathways that increase AT2R protein in cardiac pathology are not well understood. Interestingly, hyperinsulinemia-induced cardiac hypertrophy is accompanied by a reduction in AT1R, an increase in AT2R, and activation of S6K1 via the PI3-K/Akt signaling pathway [57]. The association between increases in AT2R protein and S6K1 activation in INS-induced cardiac hypertrophy prompts us to posit that mTOR/S6K1-induced increases in translation could, in part, contribute to increases in AT2R protein levels. Thus, conditions that activate mTOR-mediated signaling in cardiac tissue could also elevate AT2R protein levels [58,59,60]. Activated mTOR nucleates two large protein complexes, mTOR-Raptor complex 1 (mTORC1) and mTOR-Rictor complex 2 (mTORC2) that mediate mTOR signaling. When associated with Raptor, mTOR functions as the physiological Thr389 kinase for its substrate S6K1 [61,62]. Ribosomal protein S6 (RPS6) is a substrate of S6K1 and a key factor for protein synthesis in various cell types [62,63]. Thus, activation of mTOR/S6K1 increases translation of different proteins via the S6K1-RPS6 pathway. The second substrate of mTOR is 4E-BP, which in its hypophosphorylated form functions as a translational repressor by binding to translation initiation factor eIF4E. In this context, mTORC1 enhances protein synthesis by inhibitory phosphorylation of 4E-BP on Thr37 and Thr46. Interestingly, hyperinsulinemia-induced cardiac hypertrophy is accompanied by a reduction in AT1R, an increase in AT2R, and activation of S6K1 [57]. The association between increases in AT2R protein and S6K1 activation in INS-induced cardiac hypertrophy prompted us to posit the existence of an mTOR-S6K1↔AT2R signaling loop that may serve to protect the heart during conditions of overnutrition.
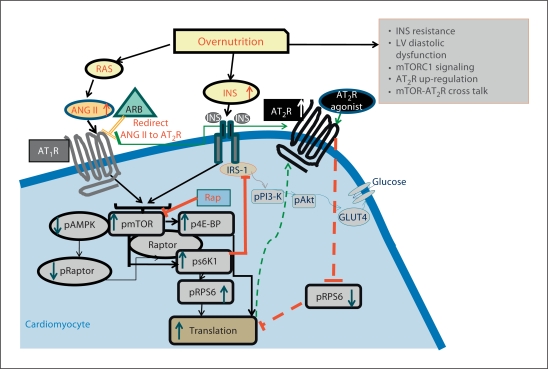
We have recently shown that the ZO rat, a genetic model for overnutrition and the CRS, has significant maladaptive changes in cardiac tissue [2,7,10]. The ZO rat heart exhibits prolonged diastolic relaxation time and reduced initial diastolic filling rate as well as increased interstitial and pericapillary fibrosis, and elevated 3-nitrotyrosine and NADPH oxidase-dependent superoxide production compared to heart tissue of syngeneic Zucker lean (ZL) controls [7]. Since overnutrition, a predicted activator of mTOR, is the key contributor for cardiac pathology in this model system, we tested for co-existence of mTOR-mediated signaling and elevation of AT2R in the left ventricle of the ZO rat heart. Our recent data show increased cardiac activation of mTOR signaling, characterized by downstream activation of RPS6 and inhibition of 4E-BP in hypertrophic hearts of 12-week-old ZO rats, which manifest diastolic dysfunction. Moreover, in the ZO rat heart, AMP kinase, normally a compensatory negative modulator of mTOR, remained unactivated in ZO compared to ZL cardiac tissue. Second, as in the case of failing human hearts, we observed that dysfunctional, hypertrophied ZO rat hearts exhibited an increase in AT2R protein levels. Since AT2R functions as a cell growth inhibitor and has cardioprotective effects, this observation suggests that the increase in the AT2R protein can be a downstream event of mTOR-S6K1 signaling and the subsequent increase in translation (fig. 4). Additionally, we observed that chronic exposure to ANG II or INS induced mTOR/S6K1 signaling and increased AT2R protein in mouse cardiomyocytes and human VSMCs. Interestingly, drug treatments that attenuated mTOR/S6K1 signaling in CV tissue of the ZO rat, mouse cardiomyocytes or human VSMCs also reduced AT2R protein. Conversely, agonist activation of AT2R in cardiomyocytes inhibited stimulatory phosphorylation of RPS6, the downstream effector of mTOR/S6K1 signaling. These findings suggest a novel branch of cross talk between RAAS and mTOR mediated by AT2R and the existence of a novel signaling loop (mTOR↔AT2R signaling loop) in CV tissue of rats, mice and humans in conditions of overnutrition.
Fig. 4.
Up-regulation of the AT2R may be a protective feedback mechanism to regulate excess mTOR/S6K1 signaling in cardiomyocytes. Excess nutrients (due to overnutrition) or chronic exposure to ANG II/INS can activate mTOR/S6K1 signaling, increase translation, induce myocardial remodeling and left-ventricular hypertrophy, and up-regulate AT2R protein levels. AT2R can be activated by redirected ANG II (due to ANG receptor blocker-mediated inhibition of ANG II binding to the AT1R) or AT2R agonist. AT2R signaling inhibits phosphorylation of RPS6 and regulates excess mTOR/S6K1 signaling and subsequent cardiac pathology.
Impact of Overnutrition and mTOR Signaling on the Kidney
There is emerging evidence that the mTOR/S6K1 pathway is involved in a spectrum of kidney diseases, including that of diabetic kidney disease [64,65,66,67,68,69,70]. Diabetic kidney disease is often characterized by progression of albuminuria to proteinuria and a gradual but progressive decline in glomerular filtration rate [71,72]. Many individuals who are destined to develop diabetic kidney disease manifest the clinical characteristics of the CRS prior to the development of overt diabetes [72]. In evolving through the renal abnormalities characterizing the CRS to that of diabetic kidney disease, the morphological process is characterized by glomerular hypertrophy and hyperfiltration, podocyte loss and associated glomerulosclerosis, and finally progressive tubulointerstitial fibrosis [72].
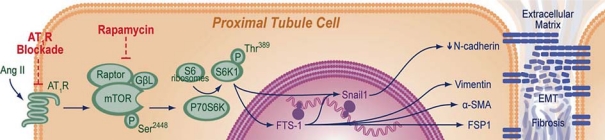
The initial hypertrophic process is likely mediated by overnutrition and RAAS stimulation of the mTOR signaling pathway [64,70,73]. The mTOR molecule is a large protein with many domains, and when complexed with GβL and Raptor (regulatory-associated protein of mTOR) it forms the rapamycin-sensitive complex referred to as mTORC1 [35,44,63]. The activity of mTORC1 appears to be regulated through a dynamic interaction between mTOR and Raptor mediated by GβL. While the initial hypertrophic and proliferative lesions in diabetic kidney disease are now thought to occur through mTOR, the regulatory role of S6K1, the substrate of mTORC1, in the kidney appears to occur through promotion of proximal tubule epithelial cell fibrosis [64,65,66,67,68,69,70]. Recent data suggest that targeting reductions in mTOR activity by targeting mTORC1 and S6K1 with rapamycin treatment improves tubulointerstitial fibrosis and proteinuria in rodent models of diabetic nephropathy and polycystic kidney disease [64,65,66,67,68,69,70].
Rapamycin is clinically used to suppress rejection of transplanted organs. In addition to its immunosuppressive actions, rapamycin inhibits growth factor-mediated proliferation and promotes survival of many non-immune cells, including renal tubular cells and fibroblasts [64,65,66,67,68,69,70,73,74,75]. There is increasing interest in using rapamycin to promote prolonged survival in aging as well as expanding its use in chronic disease management.
Recent data suggest that aldosterone stimulates proliferation of mesangial cells [76], in part through downstream mTOR/S6K1 signaling [76]. Tubulointerstitial fibrosis is the critical mechanism by which tubular atrophy and loss of nephron mass occur and thereby promote progressive kidney disease [77,78]. In young rodent models of kidney disease, ANG II has been shown to induce epithelial-mesenchymal transition (EMT) through actions on the AT1R in the proximal tubule, a process that leads to tubulointerstitial fibrosis [79,80,81,82].
EMT and disruption of adhesion molecules contribute to tubulointerstitial fibrosis [83,84]. EMT is a phenotypic conversion with loss of epithelial cell-basement membrane adherens junctions and acquisition of a fibroblastic phenotype. Disruption of adhesion molecules is the first phase of EMT that results in tissue fibrosis [85,86,87]. Recent evidence has established EMT as a critical initial mechanism for tubulointerstitial fibrosis in humans and other species. Tubulointerstitial fibrosis is characterized by loss of differentiated epithelial cells and activation of renal fibroblasts leading to fibrosis. Under unstressed, basal conditions, proximal tubule cells are attached to each other and to the basement membrane through specialized junctional complexes (adherens junctions) that include molecules such as cadherin. During injury, epithelial cells lose polarity and the mechanisms of adhesion. The best-studied cadherin in the promotion of EMT is E-cadherin, which typically resides in epithelial tissue; however, it is not found in human proximal tubule cells. Recent data suggest the cadherin in the kidney and specific to the proximal tubule is N-cadherin [87,88]. N-cadherin in the proximal tubule has been shown to bind cytoskeletal components that provide a structural foundation for adherens junctions. Of note, cadherins not only function as static structural components of adherens junctions but also play a role in cell signaling pathways [88]. Alterations in cadherin expression have been studied in various carcinogenesis models to understand the mechanism of EMT in the fibrotic process [83,84,85]. Recent evidence further indicates the mTOR pathway is a critical player in the progression of tubulointerstitial fibrosis to progressive kidney disease [64,65,66,67,68,69,70]. Therefore, the collective evidence from rodent and culture models further suggests targeting reductions in RAAS activity may slow progressive kidney disease through potential mechanisms that improve cadherin expression as well as promote survival [10] (fig. 5).
Fig. 5.
Proposed mechanism by which ANG II promotes an exaggerated response on mTOR in the kidney with downstream activation of S6K1 and associated tubulointerstitial fibrosis. FTS-1 = Fibroblast transcription site-1; FSP1 = fibroblast secretory protein-1.
Disclosure Statement
The authors have no conflict of interest.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Whaley-Connell A, Pulakat L, DeMarco VG, Hayden MR, Habibi J, Henriksen EJ, Sowers JR. Overnutrition and the cardiorenal syndrome: use of a rodent model to examine mechanisms. Cardiorenal Med. 2011;1:23–30. doi: 10.1159/000322827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schenk S, Saberi M, Olefsky JM. Insulin sensitivity: modulation by nutrients and inflammation. J Clin Invest. 2008;118:2992–3002. doi: 10.1172/JCI34260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim JA, Wei Y, Sowers JR. Role of mitochondrial dysfunction in insulin resistance. Circ Res. 2008;102:401–414. doi: 10.1161/CIRCRESAHA.107.165472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morris EM, Whaley-Connell AT, Thyfault JP, Britton SL, Koch LG, Wei Y, Ibdah JA, Sowers JR. Low aerobic capacity and high-fat diet contribute to oxidative stress and IRS-1 degradation in the kidney. Am J Nephrol. 2009;30:112–119. doi: 10.1159/000204362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whxaley-Connell A, Sowers JR. Hypertension and insulin resistance. Hypertension. 2009;54:462–464. doi: 10.1161/HYPERTENSIONAHA.109.134460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou X, Ma L, Habibi J, Whaley-Connell A, Hayden MR, Tilmon RD, Brown AN, Kim JA, DeMarco VG, Sowers JR. Nebivolol improves diastolic dysfunction and myocardial remodeling through reductions in oxidative stress in the Zucker obese rat. Hypertension. 2010;55:880–888. doi: 10.1161/HYPERTENSIONAHA.109.145136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferreira AJ, Santos RA, Bradford CN, Mecca AP, Sumners C, Katovich MJ, Raizada MK. Therapeutic implications of the vasoprotective axis of the renin-angiotensin system in cardiovascular diseases. Hypertension. 2010;55:207–213. doi: 10.1161/HYPERTENSIONAHA.109.140145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Motley ED, Eguchi K, Gardner C, Hicks AL, Reynolds CM, Frank GD, Mifune M, Ohba M, Eguchi S. Insulin-induced Akt activation is inhibited by angiotensin II in the vasculature through protein kinase C-alpha. Hypertension. 2003;41(3 Pt 2):775–780. doi: 10.1161/01.HYP.0000051891.90321.12. [DOI] [PubMed] [Google Scholar]
- 10.Sowers JR, Whaley-Connell A, Hayden MR. the role of overweight and obesity in the cardiorenal syndrome. Cardiorenal Med. 2011;1:5–12. doi: 10.1159/000322822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Andreozzi F, Laratta E, Sciacqua A, Perticone F, Sesti G. Angiotensin II impairs the insulin signaling pathway promoting production of nitric oxide by inducing phosphorylation of insulin receptor substrate-1 on Ser312 and Ser616 in human umbilical vein endothelial cells. Circ Res. 2004;94:1211–1218. doi: 10.1161/01.RES.0000126501.34994.96. [DOI] [PubMed] [Google Scholar]
- 12.Sahar S, Dwarakanath RS, Reddy MA, Lanting L, Todorov I, Natarajan R. Angiotensin II enhances interleukin-18 mediated inflammatory gene expression in vascular smooth muscle cells: a novel cross-talk in the pathogenesis of atherosclerosis. Circ Res. 2005;96:1064–1071. doi: 10.1161/01.RES.0000168210.10358.f4. [DOI] [PubMed] [Google Scholar]
- 13.Blendea MC, Jacobs D, Stump CS, McFarlane SI, Ogrin C, Bahtyiar G, Stas S, Kumar P, Sha Q, Ferrario CM, Sowers JR. Abrogation of oxidative stress improves insulin sensitivity in the Ren-2 rat model of tissue angiotensin II overexpression. Am J Physiol Endocrinol Metab. 2005;288:E353–E359. doi: 10.1152/ajpendo.00402.2004. [DOI] [PubMed] [Google Scholar]
- 14.Wei Y, Sowers JR, Nistala R, Gong H, Uptergrove GM, Clark SE, Morris EM, Szary N, Manrique C, Stump CS. Angiotensin II induced NADPH oxidase activation impairs insulin signaling in skeletal muscle cells. J Biol Chem. 2006;281:35137–35146. doi: 10.1074/jbc.M601320200. [DOI] [PubMed] [Google Scholar]
- 15.Wei Y, Whaley-Connell AT, Chen K, Habibi J, Uptegrove GM, Clark SE, Stump CS, Ferrario CM, Sowers JR. NADPH oxidase contributes to vascular inflammation, insulin resistance, and remodeling in the transgenic (mRen2) rat. Hypertension. 2007;50:384–391. doi: 10.1161/HYPERTENSIONAHA.107.089284. [DOI] [PubMed] [Google Scholar]
- 16.Um SH, Frigerio F, Watanabe M, Picard F, Joaquin M, Sticker M, Fumagalli S, Allegrini PR, Kozma SC, Auwerx J, Thomas G. Absence of S6K1 protects against age- and diet-induced obesity while enhancing insulin sensitivity. Nature. 2004;431:200–205. doi: 10.1038/nature02866. [DOI] [PubMed] [Google Scholar]
- 17.Khamzina L, Veilleux A, Bergeron S, Marette A. Increased activation of the mammalian target of rapamycin pathway in liver and skeletal muscle of obese rats: possible involvement in obesity-linked insulin resistance. Endocrinology. 2005;146:1473–1481. doi: 10.1210/en.2004-0921. [DOI] [PubMed] [Google Scholar]
- 18.Um SH, D'Alessio D, Thomas G. Nutrient overload, insulin resistance, and ribosomal protein S6 kinase 1, S6K1. Cell Metab. 2006;3:393–402. doi: 10.1016/j.cmet.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 19.Tremblay F, Krebs M, Dombrowski L, Brehm A, Bernroider E, Roth E, Nowotny P, Waldhäusl W, Marette A, Roden M. Overactivation of S6 kinase 1 as a cause of human insulin resistance during increased amino acid availability. Diabetes. 2005;54:2674–2684. doi: 10.2337/diabetes.54.9.2674. [DOI] [PubMed] [Google Scholar]
- 20.Tremblay F, BrÛlé S, Um SH, Li Y, Masuda K, Roden M, Sun XJ, Brebs M, Polakiewicz RD, Thomas G, Marette A. Identification of IRS-1 Ser-1101 as a target of S6K1 in nutrient- and obesity-induced insulin resistance. Proc Natl Acad Sci USA. 2007;104:14056–14061. doi: 10.1073/pnas.0706517104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mayer CM, Belsham DD. Central insulin signaling is attenuated by long-term insulin exposure via insulin receptor substrate-1 serine phosphorylation, proteasomal degradation, and lysosomal insulin receptor degradation. Endocrinology. 2010;151:75–84. doi: 10.1210/en.2009-0838. [DOI] [PubMed] [Google Scholar]
- 22.Zhang J, Gao Z, Yin J, Quon MJ, Ye J. S6K directly phosphorylates IRS-1 on Ser-270 to promote insulin resistance in response to TNF-(alpha) signaling through IKK2. J Biol Chem. 2008;283:35375–35382. doi: 10.1074/jbc.M806480200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adochio R, Leitner JW, Hedlund R, Draznin B. Rescuing 3T3-L1 adipocytes from insulin resistance induced by stimulation of Akt-mammalian target of rapamycin/p70 S6 kinase (S6K1) pathway and serine phosphorylation of insulin receptor substrate-1: effect of reduced expression of p85α subunit of phosphatidylinositol 3-kinase and S6K1 kinase. Endocrinology. 2009;150:1165–1173. doi: 10.1210/en.2008-0437. [DOI] [PubMed] [Google Scholar]
- 24.Standley PR, Zhang F, Sowers JR. Insulin attenuates vasopressin-induced calcium transients and a voltage-dependent calcium response in rat vascular smooth muscle cells. J Clin Invest. 1991;88:1230–1236. doi: 10.1172/JCI115426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muniyappa R, Xu R, Ram JL, Sowers JR. Inhibition of Rho protein stimulates iNOS expression in rat vascular smooth muscle cells. Am J Physiol Heart Circ Physiol. 2000;278:H1762–H1768. doi: 10.1152/ajpheart.2000.278.6.H1762. [DOI] [PubMed] [Google Scholar]
- 26.Ren J, Samson WK, Sowers JR. Insulin-like growth factor 1 as a cardiac hormone: physiological and pathophysiological implications in heart disease. J Mol Cell Cardiol. 1999;31:2049–2061. doi: 10.1006/jmcc.1999.1036. [DOI] [PubMed] [Google Scholar]
- 27.Ren J, Sowers JR, Walsh MF. Reduced contractile response to insulin and IGF-I in ventricular myocytes from genetically obese Zucker rats. Am J Physiol Heart Circ Physiol. 2000;279:H1708–H1714. doi: 10.1152/ajpheart.2000.279.4.H1708. [DOI] [PubMed] [Google Scholar]
- 28.McDowell SA, McCall E, Matter WF. Phosphoinositide 3-kinase regulates excitation-contraction coupling in neonatal cardiomyocytes. Am J Physiol Heart Circ Physiol. 2004;286:H796–H805. doi: 10.1152/ajpheart.00546.2003. [DOI] [PubMed] [Google Scholar]
- 29.Isenovic ER, Muniyappa R, Sowers JR. Role of PI3-kinase in isoproterenol and IGF-1 induced eNOS activity. Biochem Biophys Res Commun. 2001;285:954–958. doi: 10.1006/bbrc.2001.5246. [DOI] [PubMed] [Google Scholar]
- 30.Shioi T, McMullen JR, Tarnavski O, Converso K, Sherwood MC, Manning WJ, Izumo S. Rapamycin attenuates load-induced cardiac hypertrophy in mice. Circulation. 2003;107:1664–1670. doi: 10.1161/01.CIR.0000057979.36322.88. [DOI] [PubMed] [Google Scholar]
- 31.Diniz GP, Carneiro-Ramos MS, Barreto-Chaves MLM. Angiotensin type 1 receptor mediates thyroid hormone-induced cardiomyocyte hypertrophy through the Akt/GSK-3β/mTOR signaling pathway. Basic Res Cardiol. 2009;104:653–667. doi: 10.1007/s00395-009-0043-1. [DOI] [PubMed] [Google Scholar]
- 32.Hafizi S, Wang X, Chester AH, Yacoub MH, Proud CG. ANG II activates effectors of mTOR via PI3-K signaling in human coronary smooth muscle cells. Am J Physiol Heart Circ Physiol. 2004;287:H1232–H1238. doi: 10.1152/ajpheart.00040.2004. [DOI] [PubMed] [Google Scholar]
- 33.Montagnani M, Ravichandran LV, Chen H, Esposito DL, Quon MJ. Insulin receptor substrate-1 and phosphoinositide-dependent kinase-1 are required for insulin-stimulated production of nitric oxide in endothelial cells. Mol Endocrinol. 2002;16:1931–1942. doi: 10.1210/me.2002-0074. [DOI] [PubMed] [Google Scholar]
- 34.Isenovic ER, Jacobs DB, Kedees MH, Sha Q, Gick G, Sowers JR. Angiotensin II regulation of the Na+ pump involves the phosphatidylinositol-3 kinase and p42/44 mitogen-activated protein kinase signaling pathways in vascular smooth muscle cells. Endocrinology. 2004;145:1151–1160. doi: 10.1210/en.2003-0100. [DOI] [PubMed] [Google Scholar]
- 35.Acosta-Jaquez HA, Keller JA, Foster KG, Ekim B, Soliman GA, Feener EP, Ballif BA, Fingar DC. Site-specific mTOR phosphorylation promotes mTORC1-mediated signaling and cell growth. Mol Cell Biol. 2009;29:4308–4324. doi: 10.1128/MCB.01665-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gropler RJ. Methodology governing the assessment of myocardial glucose metabolism by positron emission tomography and fluorine 18-labeled fluorodeoxyglucose. J Nucl Cardiol. 1994;1(2 Pt 2):S4–S14. doi: 10.1007/BF02940063. [DOI] [PubMed] [Google Scholar]
- 37.Dutka DP, Pitt M, Pagano D. Myocardial glucose transport and utilization in patients with type 2 diabetes mellitus, left ventricular dysfunction, and coronary artery disease. J Am Coll Cardiol. 2006;48:2225–2231. doi: 10.1016/j.jacc.2006.06.078. [DOI] [PubMed] [Google Scholar]
- 38.Ouwens DM, Boer C, Fodor M, de Galan P, Heine RJ, Maassen JA. Cardiac dysfunction induced by high-fat diet is associated with altered myocardial insulin signalling in rats. Diabetologia. 2005;48:1229–1237. doi: 10.1007/s00125-005-1755-x. [DOI] [PubMed] [Google Scholar]
- 39.Scognamiglio R, Negut C, De Kreutzenberg SV, Tiengo A, Avogaro A. Postprandial myocardial perfusion in healthy subjects and in type 2 diabetic patients. Circulation. 2005;112:179–184. doi: 10.1161/CIRCULATIONAHA.104.495127. [DOI] [PubMed] [Google Scholar]
- 40.Aasum E, Hafstad AD, Severson DL, Larsen TS. Age-dependent changes in metabolism, contractile function, and ischemic sensitivity in hearts from db/db mice. Diabetes. 2003;52:434–441. doi: 10.2337/diabetes.52.2.434. [DOI] [PubMed] [Google Scholar]
- 41.Sundell J, Knuuti J. Insulin and myocardial blood flow. Cardiovasc Res. 2003;57:312–319. doi: 10.1016/s0008-6363(02)00718-6. [DOI] [PubMed] [Google Scholar]
- 42.Peterson LR, Herrero P, Schechtman KB. Effect of obesity and insulin resistance on myocardial substrate metabolism and efficiency in young women. Circulation. 2004;109:2191–2196. doi: 10.1161/01.CIR.0000127959.28627.F8. [DOI] [PubMed] [Google Scholar]
- 43.Krebs M, Brunmair B, Brehm A, Artwohl M, Szendroedi J, Nowotny P, Roth E, Fürnsinn C, Promintzer M, Anderwald C, Bischof M, Roden M. The Mammalian target of rapamycin pathway regulates nutrient-sensitive glucose uptake in man. Diabetes. 2007;56:1600–1607. doi: 10.2337/db06-1016. [DOI] [PubMed] [Google Scholar]
- 44.Drummond MJ, Bell JA, Fujita S, Dreyer HC, Glynn EL, Volpi E, Rasmussen BB. Amino acids are necessary for the insulin-induced activation of mTOR/S6K1 signaling and protein synthesis in healthy and insulin resistant human skeletal muscle. Clin Nutr. 2008;27:447–456. doi: 10.1016/j.clnu.2008.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fukushima K, Momose M, Kondo C, Kusakabe K, Kasanuki H. Myocardial kinetics of (201)Thallium, (99m)Tc-tetrofosmin, and (99m)Tc-sestamibi in an acute ischemia-reperfusion model using isolated rat heart. Ann Nucl Med. 2007;21:267–273. doi: 10.1007/s12149-007-0019-x. [DOI] [PubMed] [Google Scholar]
- 46.Bove CM, Gilson WD, Scott CD, Epstein FH, Yang Z, Dimaria JM, Berr SS, French BA, Bishop SP, Kramer CM. The angiotensin II type 2 receptor and improved adjacent region function post-MI. J Cardiovasc Magn Reson. 2005;7:459–464. doi: 10.1081/jcmr-200053461. [DOI] [PubMed] [Google Scholar]
- 47.Brillante DG, O'Sullivan AJ, Johnstone MT, Howes LG. Evidence for functional expression of vascular angiotensin II type 2 receptors in patients with insulin resistance. Diabetes Obes Metab. 2008;10:143–150. doi: 10.1111/j.1463-1326.2006.00678.x. [DOI] [PubMed] [Google Scholar]
- 48.Haywood GA, Gullestad L, Katsuya T, Hutchinson HG, Pratt RE, Horiuchi M, Fowler MB. AT1 and AT2 angiotensin receptor gene expression in human heart failure. Circulation. 1997;95:1201–1206. doi: 10.1161/01.cir.95.5.1201. [DOI] [PubMed] [Google Scholar]
- 49.Rompe F, Artuc M, Hallberg A, Alterman M, Stroder K, Thone-Reineke C, Reichenbach A, Schacherl J, Dahlof B, Bader M, Alenina N, Schwaninger M, Zuberbier T, Funke-Kaiser H, Schmidt C, Schunck WH, Unger T, Steckelings UM. Direct angiotensin II type 2 receptor stimulation acts anti-inflammatory through epoxyeicosatrienoic acid and inhibition of nuclear factor κB. Hypertension. 2010;55:924–931. doi: 10.1161/HYPERTENSIONAHA.109.147843. [DOI] [PubMed] [Google Scholar]
- 50.Simko F, Pechanova O. Remodelling of the heart and vessels in experimental hypertension: advances in protection. J Hypertens. 2010;28(suppl 1):S1–S6. doi: 10.1097/01.hjh.0000388487.43460.db. [DOI] [PubMed] [Google Scholar]
- 51.Steckelings UM, Widdop RE, Paulis L, Unger T. The angiotensin AT2 receptor in left ventricular hypertrophy. J Hypertens. 2010;28(suppl 1):S50–S55. doi: 10.1097/01.hjh.0000388495.66330.63. [DOI] [PubMed] [Google Scholar]
- 52.Bosnyak S, Welungoda IK, Hallberg A, Alterman M, Widdop RE, Jones ES. Stimulation of angiotensin AT2 receptors by the non-peptide agonist, Compound 21, evokes vasodepressor effects in conscious spontaneously hypertensive rats. Br J Pharmacol. 2010;159:709–716. doi: 10.1111/j.1476-5381.2009.00575.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fischer TA, Singh K, O'Hara DS, Kaye DM, Kelly RA. Role of AT1 and AT2 receptors in regulation of MAPKs and MKP-1 by ANG II in adult cardiac myocytes. Am J Physiol. 1998;275(3 Pt 2):H906–H916. doi: 10.1152/ajpheart.1998.275.3.H906. [DOI] [PubMed] [Google Scholar]
- 54.Yan X, Schuldt AJ, Price RL, Amende I, Liu FF, Okoshi K, Ho KK, Pope AJ, Borg TK, Lorell BH, Morgan JP. Pressure overload-induced hypertrophy in transgenic mice selectively overexpressing AT2 receptors in ventricular myocytes. Am J Physiol Heart Circ Physiol. 2008;294:H1274–H1281. doi: 10.1152/ajpheart.00174.2006. [DOI] [PubMed] [Google Scholar]
- 55.Booz GW. Putting the brakes on cardiac hypertrophy: exploiting the NO-cGMP counter-regulatory system. Hypertension. 2005;45:341–346. doi: 10.1161/01.HYP.0000156878.17006.02. [DOI] [PubMed] [Google Scholar]
- 56.Messadi-Laribi E, Griol-Charhbili V, Gaies E, Vincent MP, Heudes D, Meneton P, Alhenc-Gelas F, Richer C. Cardioprotection and kallikrein-kinin system in acute myocardial ischaemia in mice. Clin Exp Pharmacol Physiol. 2008;35:489–493. doi: 10.1111/j.1440-1681.2008.04902.x. [DOI] [PubMed] [Google Scholar]
- 57.Samuelsson AM, Bollano E, Mobini R, Larsson BM, Omerovic E, Fu M, Waagstein F, Holmang A. Hyperinsulinemia: effect on cardiac mass/function, angiotensin II receptor expression, and insulin signaling pathways. Am J Physiol Heart Circ Physiol. 2006;291:H787–H796. doi: 10.1152/ajpheart.00974.2005. [DOI] [PubMed] [Google Scholar]
- 58.Funke-Kaiser H, Reinemund J, Steckelings UM, Unger T. Adapter proteins and promoter regulation of the angiotensin AT2 receptor – implications for cardiac pathophysiology. J Renin Angiotensin Aldosterone Syst. 2010;11:7–17. doi: 10.1177/1470320309343652. [DOI] [PubMed] [Google Scholar]
- 59.Porrello ER, Delbridge LM, Thomas WG. The angiotensin II type 2 (AT2) receptor: an enigmatic seven transmembrane receptor. Front Biosci. 2009;14:958–972. doi: 10.2741/3289. [DOI] [PubMed] [Google Scholar]
- 60.Yan X, Price RL, Nakayama M, Ito K, Schuldt AJ, Manning WJ, Sanbe A, Borg TK, Robbins J, Lorell BH. Ventricular-specific expression of angiotensin II type 2 receptors causes dilated cardiomyopathy and heart failure in transgenic mice. Am J Physiol Heart Circ Physiol. 2003;285:H2179–H2187. doi: 10.1152/ajpheart.00361.2003. [DOI] [PubMed] [Google Scholar]
- 61.Ali SM, Sabatini DM. Structure of S6 kinase 1 determines whether raptor-mTOR or rictor-mTOR phosphorylates its hydrophobic motif site. J Biol Chem. 2005;280:19445–19448. doi: 10.1074/jbc.C500125200. [DOI] [PubMed] [Google Scholar]
- 62.Manning BD. Balancing Akt with S6K: implications for both metabolic diseases and tumorigenesis. J Cell Biol. 2004;167:399–403. doi: 10.1083/jcb.200408161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hannan RD, Jenkins A, Jenkins AK, Brandenburger Y. Cardiac hypertrophy: a matter of translation. Clin Ex Pharmacol Physiol. 2003;30:517–527. doi: 10.1046/j.1440-1681.2003.03873.x. [DOI] [PubMed] [Google Scholar]
- 64.Chen JK, Chen J, Neilson EG, Harris RC. Role of mammalian target of rapamycin signaling in compensatory renal hypertrophy. J Am Soc Nephrol. 2005;16:1384–1391. doi: 10.1681/ASN.2004100894. [DOI] [PubMed] [Google Scholar]
- 65.Bonegio RG, Fuhro R, Wang Z, Valeri CR, Andry C, Salant DJ, Lieberthal W. Rapamycin ameliorates proteinuria-associated tubulointerstitial inflammation and fibrosis in experimental membranous nephropathy. J Am Soc Nephrol. 2005;16:2063–2072. doi: 10.1681/ASN.2004030180. [DOI] [PubMed] [Google Scholar]
- 66.Iwano M, Neilson EG. Mechanisms of tubulointerstitial fibrosis. Curr Opin Nephrol Hypertens. 2004;13:279–284. doi: 10.1097/00041552-200405000-00003. [DOI] [PubMed] [Google Scholar]
- 67.Lloberas N, Cruzado JM, Franquesa M, Herrero-Fresneda I, Torras J, Alperovich G, Rama I, Vidal A, Grinyo JM. Mammalian target of rapamycin pathway blockade slows progression of diabetic kidney disease in rats. J Am Soc Nephrol. 2006;17:1395–1404. doi: 10.1681/ASN.2005050549. [DOI] [PubMed] [Google Scholar]
- 68.Tao Y, Kim J, Schrier RW, Edelstein CL. Rapamycin markedly slows disease progression in a rat model of polycystic kidney disease. J Am Soc Nephrol. 2005;16:46–51. doi: 10.1681/ASN.2004080660. [DOI] [PubMed] [Google Scholar]
- 69.Yang Y, Wang J, Qin L, Shou Z, Zhao J, Wang H, Chen Y, Chen J. Rapamycin prevents early steps of the development of diabetic nephropathy in rats. Am J Nephrol. 2007;27:495–502. doi: 10.1159/000106782. [DOI] [PubMed] [Google Scholar]
- 70.Lui SL, Tsang R, Chan KW, Zhang F, Tam S, Yung S, Chan TM. Rapamycin attenuates the severity of murine Adriamycin nephropathy. Am J Nephrol. 2009;29:342–352. doi: 10.1159/000166599. [DOI] [PubMed] [Google Scholar]
- 71.Williams MR. Diabetic nephropathy: the proteinuria hypothesis. Am J Nephrol. 2005;25:77–94. doi: 10.1159/000084286. [DOI] [PubMed] [Google Scholar]
- 72.Hayden MR, Whaley-Connell A, Sowers JR. Renal redox stress and remodeling in metabolic syndrome, type 2 diabetes mellitus, and diabetic nephropathy. Am J Nephrol. 2005;25:553–569. doi: 10.1159/000088810. [DOI] [PubMed] [Google Scholar]
- 73.Kim D, Sarbassov D, Ali S, King J, Latek R, Erdjument-Bromage H, Tempst P, Sabatini D. mTOR interacts with raptor to form a nutrient-sensitive complex that signals to the cell growth machinery. Cell. 2002;110:163–175. doi: 10.1016/s0092-8674(02)00808-5. [DOI] [PubMed] [Google Scholar]
- 74.Brennan P, Babbage JW, Thomas G, Cantrell D. p70(s6k) integrates phosphatidylinositol 3-kinase and rapamycin-regulated signals for E2F regulation in T lymphocytes. Mol Cell Biol. 1999;19:4729–4738. doi: 10.1128/mcb.19.7.4729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Harrison DE, Strong R, Sharp ZD, Nelson JF, Astle CM, Flurkey K, Nadon NL, Wilkinson JE, Frenkel K, Carter CS, Pahor M, Javors MA, Fernandez E, Miller RA. Rapamycin fed late in life extends lifespan in genetically heterogeneous mice. Nature. 2009;460:392–395. doi: 10.1038/nature08221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Huang S, Zhang A, Ding G, Chen R. Aldosterone-induced mesangial cell proliferation is mediated by EGF receptor transactivation. Am J Physiol Renal Physiol. 2009;296:F1323–F1333. doi: 10.1152/ajprenal.90428.2008. [DOI] [PubMed] [Google Scholar]
- 77.Xia Z, Abe K, Furusu A, Miyazaki M, Obata Y, Tabata Y, Koji T, Kohno S. Suppression of renal tubulointerstitial fibrosis by small interfering RNA targeting heat shock protein 47. Am J Nephrol. 2008;28:34–46. doi: 10.1159/000108759. [DOI] [PubMed] [Google Scholar]
- 78.Goldfarb M, Rosenberger C, Abassi Z, Shina A, Zilbersat F, Eckardt KU, Rosen S, Heyman SN. Acute-on-chronic renal failure in the rat: functional compensation and hypoxia tolerance. Am J Nephrol. 2006;26:22–33. doi: 10.1159/000091783. [DOI] [PubMed] [Google Scholar]
- 79.Strutz F, Neilson EG. New insights into mechanisms of fibrosis in immune renal injury. Springer Semin Immunopathol. 2003;24:459–476. doi: 10.1007/s00281-003-0123-5. [DOI] [PubMed] [Google Scholar]
- 80.Okada H, Danoff TM, Kalluri R, Neilson EG. Early role of Fsp1 in epithelial-mesenchymal transformation. Am J Physiol. 1997;273:F563–F574. doi: 10.1152/ajprenal.1997.273.4.F563. [DOI] [PubMed] [Google Scholar]
- 81.Strutz F, Zeisberg M, Ziyadeh FN, Yang CQ, Kalluri R, Müller GA, Neilson EG. Role of basic fibroblast growth factor-2 in epithelial-mesenchymal transformation. Kidney Int. 2002;61:1714–1728. doi: 10.1046/j.1523-1755.2002.00333.x. [DOI] [PubMed] [Google Scholar]
- 82.Ha H, Lee HB. Reactive oxygen species and matrix remodeling in diabetic kidney. J Am Soc Nephrol. 2003;14:S246–S249. doi: 10.1097/01.asn.0000077411.98742.54. [DOI] [PubMed] [Google Scholar]
- 83.Kalluri R, Neilson EG. Epithelial-mesenchymal transition and its implications for fibrosis. J Clin Invest. 2003;112:1776–1784. doi: 10.1172/JCI20530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hills CE, Squires PE. TGF-β1-induced epithelial-to-mesenchymal transition and therapeutic intervention in diabetic nephropathy. Am J Nephrol. 2010;31:68–74. doi: 10.1159/000256659. [DOI] [PubMed] [Google Scholar]
- 85.Kreidberg JA, Symons JM. Integrins in kidney development, function, and disease. Am J Physiol Renal Physiol. 2000;279:F233–F242. doi: 10.1152/ajprenal.2000.279.2.F233. [DOI] [PubMed] [Google Scholar]
- 86.Lee DB, Huang E, Ward HJ. Tight junction biology and kidney dysfunction. Am J Physiol Renal Physiol. 2006;290:F20–F34. doi: 10.1152/ajprenal.00052.2005. [DOI] [PubMed] [Google Scholar]
- 87.Jung KY, Dean D, Jiang J, Gaylor S, Griffith WH, Burghardt RC, Parrish AR. Loss of N-cadherin and alpha-catenin in the proximal tubules of aging male Fischer 344 rats. Mech Ageing Dev. 2004;125:445–53. doi: 10.1016/j.mad.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 88.Chen G, Akintola AD, Catania JM, Covington MD, Dean DD, Trzeciakowski JP, Burghardt RC, Parrish AR. doi: 10.1080/15419060701556943. [DOI] [PubMed] [Google Scholar]