Before the onset of myopia, children's near work activities did not differ from those of emmetropes. Those who became myopic had fewer sports and outdoor activity hours than emmetropes had, before, at, and after myopia onset.
Abstract
Purpose.
To investigate visual activities before and after the onset of juvenile myopia.
Methods.
The subjects were 731 incident myopes (−0.75 D or more myopia on cycloplegic autorefraction in both meridians) and 587 emmetropes (between −0.25 and +1.00 D) in the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) Study. Parents supplied visual activity data annually. Data from myopic children 5 years before through 5 years after myopia onset were compared to data from age-, sex-, and ethnicity-matched models of children who remained emmetropic.
Results.
Hours per week spent reading or using a computer/playing video games did not differ between the groups before myopia onset; however, hours per week for both activities were significantly greater in myopes than in emmetropes at onset and in 4 of the 5 years after onset by 0.7 to 1.6 hours per week. Hours per week spent in outdoor/sports activities were significantly fewer for children who became myopic 3 years before onset through 4 years after onset by 1.1 to 1.8 hours per week. Studying and TV watching were not significantly different before myopia onset.
Conclusions.
Before myopia onset, near work activities of future myopic children did not differ from those of emmetropes. Those who became myopic had fewer outdoor/sports activity hours than the emmetropes before, at, and after myopia onset. Myopia onset may influence children's near work behavior, but the lack of difference before onset argues against a major causative role for near work. Less outdoor/sports activity before myopia onset may exert a stronger influence on development than near work.
An association between near work and juvenile-onset myopia has long been theorized, but data in support of the association have shown small effects. Conflicting results have also been reported among studies and within individual studies using various measures of near work,1–4 leaving the issue unresolved. For example, the Singapore Cohort Study of Risk Factors for Myopia (SCORM) reported a significant difference in the number of books read per week by high myopes compared with low myopes and nonmyopes; however, the number of hours of reading per day did not differ among the three groups.1 An earlier cross-sectional report from the Orinda Longitudinal Study of Myopia (OLSM) found that more time was spent in near work (diopter-hours) by myopic children.3 Interestingly, while both SCORM and OLSM reported significant associations between various forms of near work and myopia in cross-sectional analyses of prevalent myopes, neither found any significantly increased risk of myopia onset associated with any form of near work in longitudinal analyses.5,6 The question arises as to whether children's near work activities change near or at the time of myopia onset, with different levels of activity for the premyope compared with that of the prevalent myope. There has not been a year-by-year longitudinal analysis of visual activity data before and after the onset of myopia. This question is relevant because selecting a single point in time, while informative, may miss pertinent information or a trend that depends on the time point(s) selected. Recent work showing less outdoor/sports activity in those who become myopic and in those whose myopia progresses makes assessing visual activity in this manner informative.6–8
Using methodology that we have applied in studying ocular component growth and myopia,9,10 we investigated differences in the visual activity profile between data from myopes and emmetropes before, at, and after the onset of myopia, by using growth curve models.
Methods
The subjects were 6- to 14-year-old participants in the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) Study between 1989 and 2005. The CLEERE Study is a multicenter, observational cohort study of ocular component development and risk factors for juvenile-onset myopia in children of different ethnicities. The OLSM (Orinda, CA) became CLEERE in 1997, with the addition of sites enrolling African-American (Eutaw, AL), Asian (Irvine, CA), and Hispanic (Houston, TX) children. In 2000, a site was added to test and enroll Native-American children (Tucson, AZ). Each affiliated university's institutional review board approved the protocol and informed consent documents in accordance with the tenets of the Declaration of Helsinki. In addition to parental consent, the children provided assent.
Ethnic group identity was supplied by a parent on a medical history form at enrollment in the study by choosing among six categories (based on NIH categories): American Indian or Alaskan Native; Asian or Pacific Islander; black, not of Hispanic origin; Hispanic; white, not of Hispanic origin; and other or unknown. For the purposes of these analyses, those children whose parents designated them as other were excluded (one emmetrope and seven myopes).
Visual activity data were obtained annually with a questionnaire that asked the parent, “During the school year, how many hours per week (outside of regular school hours) would you estimate that this child (1) studies or reads for school assignments; (2) reads for fun (pleasure); (3) watches TV; (4) uses a computer/plays video games; or (5) engages in outdoor/sports activities?”
Reported times exceeding 82 hours per week across all five activities were deleted (data for 15 emmetrope visits and 39 myope visits). We assumed that 82 hours during a week outside of school were not reasonably available to a child. (This maximum value was calculated as follows: 168 [24 hours × 7 days] possible hours per week, and assumed 30 hours per week were spent in school [6 hours × 5 days], and 56 were spent sleeping [7 days × 8 hours], which leaves 82 hours for other activities.) Diopter-hours were also calculated as a comprehensive near work exposure, defined as: 3 × hours of reading + 3 × hours of studying + 2 × video/computer hours + hours watching TV.3 Refractive error measurements were made by certified study personnel with one autorefractor (model R-1; Canon USA, Lake Success, NY; no longer manufactured), from 1989 to 2000, and with another (WR 5100-K; Grand Seiko Co., Hiroshima, Japan), from 2001 to 2005. For cycloplegic autorefraction, subjects fixated on a reduced Snellen target through a +4.00-D Badal lens in primary gaze. The Badal lens allows the subjects to fixate on an in-focus target during autorefraction, despite having removed their refractive correction for the measurement. The Badal system allows for the correction of either hyperopic or myopic refractive errors while keeping the retinal image size of the target constant. These features promote subject cooperation and limit the stimulus to any residual accommodation.
For a subject with grade 1 or 2 iris color,11 testing was performed 30 minutes after 1 drop of proparacaine 0.5% and 2 drops of tropicamide 1.0%. When a subject had dark iris color greater than grade 2, testing was performed 30 minutes after 1 drop of proparacaine 0.5% and 1 drop each of tropicamide 1.0% and cyclopentolate 1.0%.12 Ten autorefractor measurements were made according to a standard protocol.13
Emmetropes were defined as children with refractive error between −0.25 D and +1.00 D (exclusive) in both meridians at all study visits. Myopia was defined as −0.75 D or more in both principal meridians at one or more study visits. Children who fell into neither category were excluded, to allow for clear comparisons between well-delineated groups. Prevalent myopes (i.e., those who were myopic before study enrollment and those who did not have an observed myopia onset visit) were also excluded.
The analysis described here is similar to that presented in previous papers on ocular component growth curve modeling and in our “before and after myopia onset” papers.9,10,14 By using the data of those subjects identified as emmetropic, we modeled individual growth curves as a function of age. Mixed-modeling methodology was used to determine the function of age that best described the shape of the growth curve. As an example, a model of the change in hours per week with age requires a constant functional form across subjects, while allowing each subject to have individual model parameters. Different transformations of age (i.e., age, age2, ln[age]) were considered. The structure of the variance–covariance matrix in these models was specified to describe the nature of the correlated, longitudinal observations. Maximum-likelihood methods were used to determine the model parameters.15
The data from the emmetropic subjects for each activity variable were modeled as a function of age using a variety of candidate functions to find the best fit (48 candidate functions, 24 models as a function of age with two different variance–covariance matrices: compound symmetry and unstructured). The variance–covariance matrix was selected by assessing whether compound symmetry is appropriate or the matrix should be unstructured. In the resulting models, β0 is the y-intercept, and β1, β2, and β3 are slope parameters. The best-fitting model was determined as the model with the lowest Akaike information criterion (AIC).16 Overall model effectiveness was judged by the model χ2. If the model χ2 P value was <0.05, the model explained more than could be attributed to chance. After determination of the model, sex and ethnicity were included in the mixed linear regression models (SAS 9.1; SAS Institute, Cary, NC).17 Significant interactions between age, sex, and ethnicity (P < 0.01) were retained in the final models. These models provided estimates of visual activity for emmetropes of any age, sex, or ethnicity. The estimates from the growth curve models are referred to in this article as emmetropes and represent all emmetrope data presented, unless specifically identified as unmodeled, raw data, as in Table 4.
Table 4.
Unmodeled, Raw Mean Reported Visual Activity Hours per Week by Age for the Emmetropic Subjects
| Age at Last Birthday (y) | Reading |
Studying |
Using Computer |
Watching TV |
Outdoor/Sports Activities |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| 6 | 108 | 2.8 (2.7) | 106 | 3.0 (3.8) | 104 | 2.9 (4.9) | 109 | 8.9 (7.2) | 107 | 10.5 (8.1) |
| 7 | 130 | 3.0 (3.2) | 132 | 3.6 (3.2) | 128 | 2.2 (3.4) | 131 | 7.5 (5.7) | 131 | 8.7 (6.7) |
| 8 | 186 | 3.7 (4.0) | 187 | 4.4 (3.8) | 169 | 2.5 (3.0) | 187 | 7.4 (5.6) | 186 | 10.6 (7.5) |
| 9 | 180 | 3.6 (3.8) | 181 | 4.8 (4.1) | 179 | 2.9 (3.4) | 180 | 7.1 (6.0) | 179 | 8.9 (7.0) |
| 10 | 220 | 3.5 (3.7) | 220 | 5.5 (4.8) | 217 | 3.1 (4.0) | 220 | 7.2 (6.0) | 217 | 8.3 (6.7) |
| 11 | 258 | 3.5 (3.4) | 260 | 7.1 (5.7) | 232 | 2.8 (3.2) | 259 | 8.4 (7.4) | 259 | 8.6 (6.3) |
| 12 | 252 | 3.9 (4.1) | 252 | 7.2 (5.7) | 249 | 3.4 (4.6) | 253 | 8.4 (5.9) | 249 | 8.6 (6.6) |
| 13 | 258 | 3.3 (4.0) | 260 | 7.3 (5.6) | 254 | 3.2 (4.9) | 260 | 8.2 (6.3) | 261 | 8.6 (7.3) |
| 14 | 101 | 3.2 (3.7) | 100 | 5.4 (4.7) | 100 | 3.0 (3.5) | 99 | 8.5 (7.8) | 99 | 7.4 (7.1) |
For clarity, throughout the paper we refer to those subjects in whom myopia eventually developed as the became-myopic group. For inclusion in the became-myopic group, a myopic subject had to have at least one nonmyopic visit before myopia onset. The year the subject first met the myopia criterion was designated as year 0, or onset. The first study year before onset was −1, and the first year after onset was +1. For each study visit, the age, sex, and ethnicity of each myopic subject were used to calculate a matching estimated age-, sex-, and ethnicity-matched emmetrope value from the relevant emmetrope regression model.9 The mean difference between the became-myopic data and the matched emmetrope data were compared by using a mixed model that accounted for study visit. Additional models were computed to examine the effect of ethnicity and study visit on the mean difference. The significance of post hoc comparisons between visits was designated as P < 0.01, as a tradeoff between the number of comparisons that were made and the high statistical power from the large sample size.
Pearson's correlation coefficient was used to assess the correlation between various visual activity variables. In the became-myopic group, this correlation was determined for each visit relative to myopia onset. Given that emmetrope visits do not have an age of onset, the correlation coefficients were calculated with respect to age.
Results
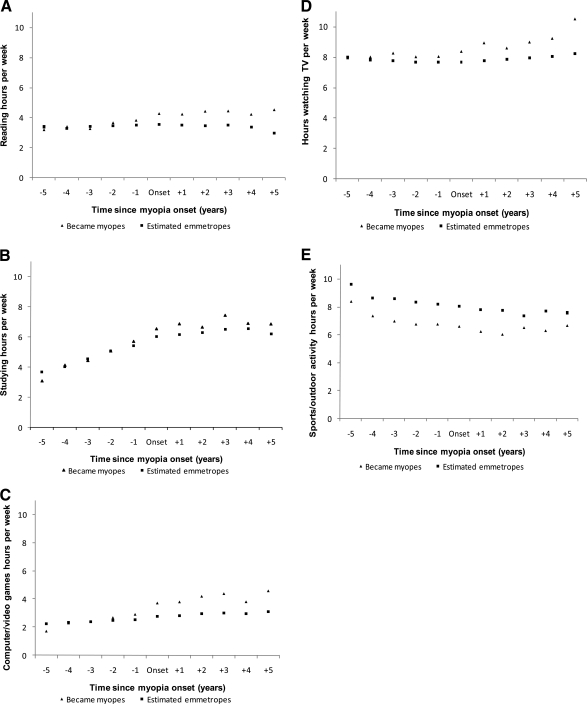
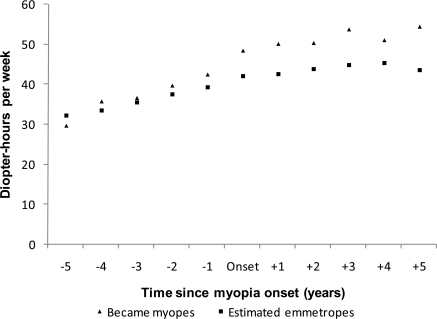
Of the CLEERE subjects (N = 4929), 3600 were excluded: 367 prevalent myopes; 8 who had an ethnicity of other; and 3225 who did not meet the narrow refractive error group criteria used for emmetropes. The remaining 1329 met the criteria for emmetropes (n = 597) or were became-myopic subjects (n = 732). Of these eligible subjects, 11 did not have any available visual activity data, leaving 587 subjects who were emmetropes and 731 who became myopic. Subjects were not required to have visual activity data at every visit to be included in the analyses. Table 1 shows the demographic and study visit information for both groups, and Table 2 presents the number of myopic subjects by age of onset. Table 3 shows the best-fitting models by activity derived from the emmetropes data. The different models indicate that participation in the various visual activities was not uniform (i.e., the pattern of how subjects read for pleasure differed over time compared with how they watched TV). Therefore, a different model was needed for each visual activity. The most common function of age was the cubic function, which was the best-fit model for study hours, TV hours, and diopter-hours. The more meaningful comparisons are between the became-myopic subjects before and after the onset of myopia. Table 4 presents the unmodeled, raw means by age for those subjects who were emmetropic. Figures 1 and 2 present the averages for the estimated emmetropes and the became-myopic subjects by time relative to onset.
Table 1.
Characteristics of Emmetropic and Became-Myopic Subjects
| Emmetropes n (%) | Became Myopes n (%) | |
|---|---|---|
| Sex | ||
| Female | 270 (46.0) | 409 (56.0) |
| Male | 317 (54.0) | 322 (44.0) |
| Ethnicity | ||
| African American | 108 (18.4) | 101 (13.8) |
| Asian | 51 (8.7) | 169 (23.1) |
| Hispanic | 105 (17.9) | 214 (29.3) |
| Native American | 103 (17.6) | 67 (9.2) |
| White | 220 (37.5) | 180 (24.6) |
| Study visits with activity data, n | ||
| 1 | 171 (29.1) | 21 (2.9) |
| 2 | 117 (19.9) | 55 (7.5) |
| 3 | 127 (21.6) | 81 (11.1) |
| 4 | 45 (7.7) | 101 (13.8) |
| 5 | 52 (8.9) | 148 (20.3) |
| 6 | 42 (7.2) | 122 (16.7) |
| 7 | 16 (2.7) | 100 (13.7) |
| 8 | 17 (2.9) | 102 (14.0) |
| 9 | 0 (0.0) | 1 (0.1) |
Table 2.
Frequency of Became-Myopic Subjects by Age of Onset
| Age of Onset (y) | n (%) |
|---|---|
| 6 | 1 (0.1) |
| 7 | 36 (4.9) |
| 8 | 82 (11.2) |
| 9 | 102 (13.9) |
| 10 | 140 (19.1) |
| 11 | 118 (16.1) |
| 12 | 120 (16.4) |
| 13 | 83 (11.3) |
| 14 | 43 (5.9) |
| 15 | 6 (0.8) |
Table 3.
Best-Fitting Emmetrope Model by Visual Activity
| Visual Activity Variable | Model |
|---|---|
| Reading for pleasure | Hours = β0 + β1 × age2 + β2 × age |
| Studying | Hours = β0 + β1 × age3 + β2 × age2 +β3 × age |
| Computer/video games | Hours = β0 + β1 × age |
| Watching TV | Hours = β0 + β1 × age3 + β2 × age2 +β3 × age |
| Outdoor/sports activities | Hours = β0 + β1 × age−1 |
| Diopter-hours | Hours = β0 + β1 × age3 + β2* age2 +β3 × age |
Figure 1.
Unmodeled, raw means for the number of hours engaged in (A) reading, (B) studying, (C) using a computer/playing video games, (D) watching TV, and (E) outdoor/sports activities per week by the myopic subjects and the emmetropic subjects.
Figure 2.
Unmodeled, raw means for the diopter-hours per week of the myopic subjects and the emmetropic subjects.
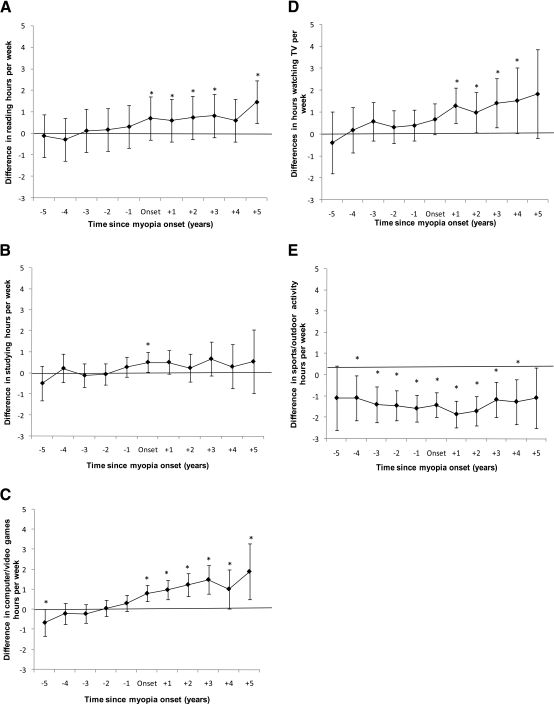
The mean differences (±99% confidence intervals [CI]) in hours per week between the became-myopic children and the emmetropes for each activity are shown in Table 5. The corresponding mean differences and 99% CIs are also plotted in Figures 3 and 4. The sample sizes listed in Table 5 represent the smallest n across all visual activities at a given time point. For example, at onset, the sample size ranged from 615 to 625 myopic children, with 102 subjects having no visual activity data at onset.
Table 5.
Least-Squares Mean Difference between Became-Myopic Hours and Estimated Emmetropic Hours Adjusted for Age, Ethnicity, and Sex
| Time Since Onset (y) | n | Reading | Studying Mean | Computer/Video Games | Watching TV | Outdoor/Sports Activities | Diopter-Hours |
|---|---|---|---|---|---|---|---|
| −5 | 127 | −0.12 (−0.81 to 0.58) | −0.48 (−1.31 to 0.35) | −0.66 (−1.31 to −0.007) | −0.39 (−1.80 to 1.02) | −1.08 (−2.60 to 0.43) | −2.25 (−7.36 to 2.85) |
| −4 | 228 | 0.29 (−0.24 to 0.82) | 0.23 (−0.45 to 0.90) | −0.21 (−0.74 to 0.32) | 0.19 (−0.85 to 1.24) | −1.08 (−2.13 to −0.02) | 3.24 (−0.71 to 7.18) |
| −3 | 340 | −0.12 (−0.57 to 0.32) | −0.11 (−0.68 to 0.46) | −0.21 (−0.68 to 0.25) | 0.59 (−0.29 to 1.47) | −1.39 (−2.23 to 0.54) | 0.92 (−2.38 to 4.21) |
| −2 | 478 | 0.17 (−0.22 to 0.57) | −0.05 (−0.54 to 0.44) | 0.06 (−0.34 to 0.46) | 0.33 (−0.43 to 1.08) | −1.44 (−2.13 to −0.74) | 1.33 (−1.54 to 4.20) |
| −1 | 566 | 0.31 (−0.07 to 0.68) | 0.29 (−0.19 to 0.76) | 0.32 (−0.08 to 0.71) | 0.40 (−0.31 to 1.11) | −1.57 (−2.20 to −0.93) | 3.05 (0.33 to 5.76) |
| Onset | 615 | 0.70 (0.31 to 1.18) | 0.52 (0.04 to 1.00) | 0.81 (0.40 to 1.22) | 0.68 (−0.03 to 1.39) | −1.42 (−2.00 to −0.83) | 6.10 (3.39 to 8.81) |
| 1 | 458 | 0.76 (0.24 to 1.08) | 0.52 (−0.04 to 1.08) | 0.98 (0.49 to 1.48) | 1.31 (0.51 to 2.10) | −1.84 (−2.47 to −1.21) | 6.62 (3.53 to 9.72) |
| 2 | 340 | 0.74 (0.22 to 1.74) | 0.25 (−0.40 to 0.91) | 1.24 (0.67 to 1.82) | 1.00 (0.09 to 1.91) | −1.70 (−2.39 to −1.01) | 5.63 (2.04 to 9.22) |
| 3 | 216 | 0.82 (0.18 to 1.47) | 0.68 (−0.13 to 1.48) | 1.49 (0.77 to 2.22) | 1.43 (0.30 to 2.56) | −1.16 (−1.99 to −0.33) | 7.62 (3.19 to 12.06) |
| 4 | 116 | 0.60 (−0.25 to 1.44) | 0.31 (−0.74 to 1.36) | 1.02 (0.05 to 2.00) | 1.54 (0.04 to 3.04) | −1.26 (−2.32 to −0.20) | 6.76 (0.94 to 12.57) |
| 5 | 55 | 1.46 (0.31 to 2.61) | 0.55 (−0.97 to 2.07) | 1.90 (0.50 to 3.29) | 1.84 (−0.20 to 3.88) | −1.08 (−2.51 to 0.36) | 9.82 (1.73 to 17.90) |
Data are the mean (99% CI). Significant differences are shown in bold.
Figure 3.
Difference between became-myopic subjects and emmetropes for the number of hours engaged in (A) reading, (B) studying, (C) using a computer/playing video games, (D) watching TV, and (E) outdoor/sports activities per week with 99% CI (*significant difference between groups). CIs that do not include 0 indicate a statistically significant difference at α = 0.01 between the two refractive error groups.
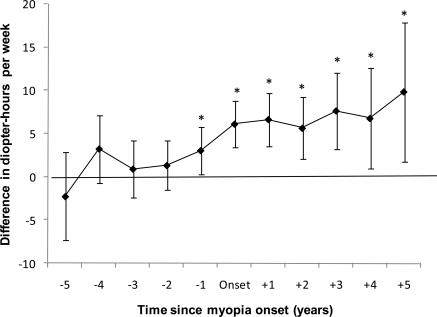
Figure 4.
Difference between became-myopic subjects and estimated emmetropes in the number of diopter-hours per week, with 99% CI (*significant difference between groups). CIs that do not include 0 indicate a statistically significant difference at α = 0.01 between the two refractive error groups.
Hours spent per week reading for pleasure, studying, and using a computer/playing video games were not significantly different between the became-myopic and emmetrope groups before the onset of myopia but became so at onset for each activity. For these activities, those children who became myopic performed more hours per week than those in the corresponding emmetrope models. For reading for pleasure, these differences occurred at onset through the third year after onset and then again in the fifth year after onset (Fig. 3A). These differences averaged 0.7 hours to 1.5 more hours per week spent reading by the became-myopic group. Statistically significant differences in the means for studying appeared at onset only (Fig. 3B). Similar to hours spent reading, those who became myopic spent significantly more hours on the computer/playing video games than the emmetropes, beginning at onset and continuing through the fifth year after onset (Fig. 3C). There was also a significant difference in the fifth year before onset that was in the opposite direction. The mean differences were between 0.8 and 1.9 more hours per week spent on computer/video game activity in the became-myopic group. Hours per week spent watching TV were not significantly different between the became-myopic and emmetropes group until the year after the onset of myopia through 4 years after onset. Those who became myopic watched more TV, by an average of 1.0 to 1.5 hours per week (Fig. 3D).
The difference for the outdoor/sports activity hours per week was significant beginning 4 years before onset and continuing through 4 years after onset, with those subjects who became myopic having fewer outdoor/sports activity hours than the emmetropes by 1.1 to 1.8 hours per week (Fig. 3E). When near work was analyzed as an aggregate in diopter-hours, became-myopic subjects performed more diopter-hours of near work from 1 year before through 5 years after myopia onset, with the difference more than doubling at the time of myopia onset compared with 1 year before (Fig. 4). The mean difference was 3.0 more diopter-hours per week in the became-myopic group 1 year before the onset of myopia, an increase of 1.7 diopter-hours per week over the prior year. More consistent with the results for the activities taken separately, differences between groups were greater at onset and after onset, from 5.6 to 9.8 diopter-hours per week.
The six visual activity variables are presented by ethnic group in Table 6 with a summary of differences for each ethnic group presented. Available data vary depending on ethnic group. African Americans (n = 11) had too small a sample size at 5 years before onset to permit meaningful analysis, while Native Americans had sufficient data only from 3 years before onset through 2 years after.
Table 6.
Time Points at Which the Difference between Became-Myopic Hours and Emmetropic Hours Were Significantly Different from 0, Overall and Within Ethnic Group
| Reading | Studying | Computer/Video Games | TV | Outdoor/Sports Activities | Diopter-Hours | |
|---|---|---|---|---|---|---|
| Overall | 0, +1, +2, +3, +5 | 0 | −5*, 0, +1, +2, +3, +4, +5 | +1, +2, +3, +4 | −4, −3, −2, −1, 0, +1, +2, +3, +4 | −1, 0, +1, +2, +3, +4, +5 |
| African American | +3 | +1 | −4* | +1 | ||
| Asian | 0 | +1* | −2, −1, 0, +1, +2, +3, +4 | |||
| Hispanic | +2 | −1, 0, +1, +2 | 0, +1, +2, +3 | −3, 0, +1, +2, +3, +4 | −4, −1, +1, +2 | −4, −3, −2, −1, 0, +1, +2, +3 |
| Native American | −1 | −1* | ||||
| White | +2, +3 | 0, +1, +2, +3, +4 | −3, −2, −1, 0, +1, +2, +3 | 0, +1, +2, +3 |
0 = onset.
Direction of the difference was opposite to the overall effect.
As can be seen, significant differences between the became-myopes and emmetropes were not seen to the same extent among the ethnic groups when compared with the sample at large. The Hispanic subgroup showed slightly more difference between became-myopes and emmetropes in the number of hours studying per week than the sample overall and was reasonably consistent with the overall findings for computer/video games, TV, outdoor/sports activity, and diopter-hours. Differences within the white subgroup were similar to the overall results on computer/video games, outdoor/sports activity, and diopter-hours. The outdoor/sports activity results for the Asian subgroup were also similar to the overall findings. The remaining ethnic group comparisons showed little evidence of difference between the became-myopes and emmetropes.
Correlations between activities were explored to look for evidence of tradeoff behavior—that is, whether one activity (i.e., reading) was substituted for another activity (i.e., outdoor/sports activities). Outdoor/sports activity hours per week did not correlate negatively with any of the other visual activity variables and consistently correlated positively with television hours only (correlations in the range of 0.30 to 0.40) across time points relative to myopia onset. Comparison of correlations between became-myopes and emmetropes showed a similar lack of significance between activities across age and visit. The level of one activity, therefore, did not appear to substitute for another.
Discussion
Outdoor/sports activity was significantly different between the subjects who became myopic and the emmetropes, with the difference present as early as 4 years before myopia onset. In contrast, each of the other individual activities became significantly different either at onset or after onset. Diopter-hours were significantly greater in became-myopic children 1 year before onset, but the difference was small compared with the differences seen at onset and after onset. If increased near work is important as a cause of myopia, 1 year yields only a small window of time for the purpose of predicting myopia. For example, differences in refractive error and axial length between those who became myopic and emmetropes were seen earlier before onset.10 Became-myopic subjects began to diverge from emmetropes 3 years before myopia onset (as defined by −0.75 D or more in each principal meridian) for axial length and 4 years before reaching this criterion for refractive error. Hispanic children may be the one exception in which near work activity has some predictive utility. It should be noted that recruitment efforts targeted a given ethnicity at a single site. Therefore, our results related to ethnicity may not be representative across the United States, and some of what has been attributed to ethnicity may in fact be related to region or site instead.
The magnitude of the difference between the became-myopes and the emmetropes for outdoor/sports hours was small. Given that the protective effect of outdoor/sports activity has been found in several studies, it may be that small differences are a potent factor in inhibiting the onset of myopia. For example, in children with two myopic parents, performing sports or outdoor activity in the highest quartile (over 14 hours per week) compared with the lowest quartile (0–5 hours per week) reduced the probability of myopia onset from 0.60 to 0.20, respectively.6 This difference is similar to the statistically significant associations for physical activity and myopia progression in a cohort study of university students.8 Dirani et al.18 found a significantly lower odds ratio for both outdoor leisure activities and outdoor sports activities in an analysis of the SCORM, unlike an earlier SCORM analysis that found no association with outdoor activity.5 They credit the use of a more detailed survey that contained multiple questions, although our single question about each activity yielded a similar result. Reports from Saw et al. (IOVS 2008;49:ARVO E-Abstract 1551) and Rose et al.19 indicate that the protective effect may not arise from any specific physical activity so much as simply being outdoors. Because our question did not distinguish indoor from outdoor sports, it is possible that indoor sports were included by parents in this estimate. If the actual association is outdoor exposure and the indoor sports were unrelated as reported in other papers, it would be anticipated to attenuate the result toward the null.
Reported seasonal effects on myopia progression lend credence to the visual implications of outdoor experiences, although perhaps not in the way originally proposed.20,21 For example, Fulk et al.20 found that most children had slower myopic progression in the summer. Goss and Rainey21 also found that myopia progression in children during the 6 months that include summer was slower by half compared with the 6 months that include school attendance.
The distance viewing that accompanies being outdoors is a potential explanation for the preventive association of outdoor/sports activities. Brief exposures to distance stimuli or minimal defocus powerfully counteract the elongating effects of hyperopic defocus or deprivation in several animal species including the tree shrew,22,23 chick,24,25 and monkey.26 These studies provide evidence that perhaps distance clarity is the “stop” signal for growth, requiring only minutes or a few hours of clarity to offset the risk of a much longer exposure to a “grow” signal.
Retinal levels of dopamine increase during the day and decrease at night in a circadian rhythm, indicating a potential correlation with light exposure.27 Dopamine has been postulated to be related to eye growth, suggesting that more outdoor exposure could affect dopamine levels and therefore eye elongation, as shown in animal studies of form deprivation.28–31 Light-induced change in retinal dopamine levels remains a potential explanation for the inhibitory effects on refractive development associated with outdoor exposure.
Some individual visual activities did not differ between the became-myopes and emmetropes until the onset of myopia (for reading, studying and computer/video games hours) or 1 year after onset (for TV hours). Of these four activities, three of these (reading, computer/video games, and TV) had the most robust associations, continuing to differ between the two groups as long as 3 to 5 years after onset. Differences after onset but not before onset lead to the question of whether there is a change in behavior in response to myopia development. Is a child more likely to opt for indoor activities after beginning to wear glasses? This hypothesis is consistent with two existing cross-sectional studies that have described increased amounts of near work activities among those already myopic compared with those who are not, but found no increased risk before onset.5,6 Unfortunately, the literature does not address behavior in myopes or behavior changes in relation to wearing glasses.
As stated in our previous paper6 and in a SCORM report,32 the hypothesis that increased reading represents a corresponding decrease in outdoor/sports activities is not supported by CLEERE data; that is, there does not appear to be a substitution of reading for outdoor/sports activity, either before or after myopia onset, as evidenced by the lack of negative correlation between outdoor/sports activity and any of the near work activities. This result is supported by a report from Harrison and Narayan,33 who reported that students who spent 1 to 2 hours per week in sports and 1 to 2 hours in other activities (such as club activities) had increased rather than decreased odds of studying 3 or more hours per week.
There are several potential areas for bias in these data. The first is that the responses are elicited from the parents rather than the children. Given the ages of these children, the parents are the most reliable source of information, as other studies in myopia and other research areas indicate. Saw et al.5,34 also used parent-reported data from their baseline visit, while the Sydney Myopia Study used subject-reported data from the baseline visit.35,36 There is, of course, the concern that parents may not know what their children are doing outside of school hours. One would suspect that parents' inability to track their children's activities would be truer of older children than of younger children. We posited in an earlier paper6 that there may be some differential recall bias, because parents often transport their children to sporting activities and therefore might be more likely to remember hours engaged in sports.
It is possible that using computer/playing video games may differ across the study, by virtue of the length of this longitudinal study. This is a valid observation that affects longitudinal studies of all kinds. A look at some of the literature may indicate that a large difference over the past 10 years in the type of game used (increase in hand-held games) versus the time spent (less than an hour among those playing) and in the increased number of children engaging in this activity.37 The reported data over time in the CLEERE Study indicate an upward trend over the course of the study, with the increase being no more than 1.5 hours on average per group; however, this increase occurs in both those who became myopic and the emmetropes, leaving the difference between the two groups relatively unbiased over time.
Another limitation is related to there being only one administration of the survey per year, as opposed to multiple administrations per year. Most studies lack longitudinal visual activity data, making it difficult to determine what activities are currently performed. Perhaps the more pertinent problem is activities during summer vacation versus during the school year. Deng et al.38 presented data that parents reported on the time children spent in various visual activities during both the school year and summer. Their results showed that decreased outdoor activity was seen in myopes during the school year compared with nonmyopes, but myopes did not differ from nonmyopes in the time spent reading, studying, or on the computer. During the summer there was no significant difference between myopes and nonmyopes for any visual activity.
Another potential issue deals with the recall bias that may be involved with the use of questionnaires. Other options that have been used in myopia research include diaries and the experience sampling method (ESM), where subjects carried pagers and responded by calling in to report their visual activity when paged.39,40The biggest drawbacks to either of these methods are the burden on the respondent and the complex logistics.
Rah et al.39 used the ESM to quantify children's daily visual activities. In comparison to a questionnaire completed by the children, the ESM responses differed only in the amount of time spent in conversation. When comparing parents' responses to ESM, differences were found in conversation time and chores time. The sample was small, however, and so some comparisons had low statistical power.
Saw et al.40 compared 4 days of diaries completed by parents within a few weeks of a baseline clinic visit with questionnaire responses. They reported data from four different times of year. A small sample was pilot tested for reliability, and they found that total near work (a sum of the near work variables) had an ICC of 0.87, although the ICC for total weekend near work hours was lower (0.33). Otherwise, TV hours had the lowest ICC (0.47), with reading and writing together at 0.97, and video games at 0.80. Comparing the interview using the questionnaire to the diary showed an ICC for total near work of 0.50 and for reading and writing of 0.55. The remaining ICCs were in the range of 0.67 (TV hours) to 0.90 (computer hours). The questions asked were similar to those in the CLEERE survey, with the exception of separating computer and video games, breaking out weekday from weekend, and attempting to include examination and vacation time. The relation between the time the diaries were completed and the questionnaire is unclear, as the 4 days of diaries were completed within a few weeks of the questionnaires. How this correlated to four different points in the year was not specified.
An additional potential source of bias may arise from the use of a brief questionnaire as opposed to a more comprehensive one. In addition to the variation of the CLEERE questionnaire that Saw et al. used, the Sydney Myopia Study35,36 had a baseline questionnaire that asked detailed physical activity questions on the amount of time per day spent in various activities. For the near work activities, information per day was solicited by choosing one of four check boxes: none; less than 1 hour; 1 to 2 hours; and 3 or more hours. While the benefits of parsing out sports from being outdoors are definitely an advantage of a detailed questionnaire, one would assume that the likelihood of finding any association would increase using a more general question. A significant finding might result from the pooling of multiple items. It would seem less likely that there would be an absence of an association that in fact exists.
Follow-up of our emmetropes with necessary data was shorter than that of myopes and therefore may have affected the growth curves. Data were available across the entire age range for the emmetropes, so the modeling applied should lead to robust results. Some of the follow-up problems were intrinsic to the study design, where there was a staggered entry of subjects during the initiation of the study and a cutoff at eighth grade,13 meaning that some of the identified emmetropes had the opportunity for only three visits (those enrolled as sixth graders). In addition, the older emmetropic subjects (at entry) were probably more likely to remain emmetropic. It could be that emmetropes had a lack of incentive to continue to participate. There were approximately 260 13-year-old emmetropes and approximately 100 14-year-old emmetropes who were included in the analysis. These subjects represent the eighth graders. The strict definition of emmetropia made it more likely to exclude subjects when small measurement variability occurred. Although this criterion limited the sample size, we do not believe that it introduced a systematic bias.
Conclusions
An evaluation of the association between visual activity variables before, at, and after myopia onset in a cohort of children failed to show evidence of a relationship between near visual activities and the development of myopia. Outdoor exposure may exert a strong preventive effect against the onset of myopia.
Appendix A: The CLEERE Study Group (as of July 2009)
Clinical Centers
Franklin Primary Health Center, Inc.
Sandral Hullett (Principal Investigator, 1997–2006), Robert N. Kleinstein (Co-investigator, 1997–2006), Janene Sims (Optometrist, 1997–2001 and 2004–2006), Raphael Weeks (Optometrist, 1999–2006), Sandra Williams (Study Coordinator, 1999–2006), LeeAndra Calvin (Study Coordinator, 1997–1999), and Melvin D. Shipp (Co-investigator, 1997–2004).
University of California, Berkeley School of Optometry, Berkeley, CA.
Nina E. Friedman (Principal Investigator, 1999–2001), Pamela Qualley (Study Coordinator, 1997–2001), Donald O. Mutti (Principal Investigator, 1996–1999), and Karla Zadnik (Optometrist, 1996–2001).
University of Houston College of Optometry, Houston, TX.
Ruth E. Manny (Principal Investigator, 1997–2006), Suzanne M. Wickum (Optometrist, 1999–2006), Ailene Kim (Optometrist, 2003–2006), Bronwen Mathis (Optometrist, 2002–2006), Mamie Batres (Study Coordinator, 2004–2006). Sally Henry (Study Coordinator, 1997–1998), Janice M. Wensveen (Optometrist, 1997–2001), Connie J. Crossnoe (Optometrist, 1997–2003), Stephanie L. Tom (Optometrist, 1999–2002), Jennifer A. McLeod (Study Coordinator, 1998–2004), and Julio C. Quiralte (Study Coordinator, 1998–2005).
Southern California College of Optometry, Fullerton, CA.
Susan A. Cotter (Principal Investigator, 2004–2006, Optometrist, 1997–2004), Julie A. Yu (Principal Investigator, 1997–2004; Optometrist 2005–2006), Raymond J. Chu (Optometrist, 2001–2006), Carmen N. Barnhardt (Optometrist 2004–2006), Jessica Chang (Optometrist, 2005–2006), Kristine Huang (Optometrist, 2005–2006), Rebecca Bridgeford (Study Coordinator, 2005–2006), Connie Chu (Optometrist, 2004–2005), Soonsi Kwon (Optometrist, 1998–2004), Gen Lee (Study Coordinator, 1999–2003), John Lee (Optometrist, 2000–2003), Robert J. Lee (Optometrist, 1997–2001), Raymond Maeda (Optometrist, 1999–2003), Rachael Emerson (Study Coordinator, 1997–1999), and Tracy Leonhardt (Study Coordinator, 2003–2004).
University of Arizona, Department of Ophthalmology and Vision Science, Tucson, AZ.
J. Daniel Twelker (Principal Investigator, 2000–present), Dawn Messer (Optometrist, 2000–present), Denise Flores (Study Coordinator, 2000–2007), Rita Bhakta (Optometrist, 2000–2004), Katie Garvey (Optometrist, 2005–2008), and Amanda Mendez Roberts (Optometrist, 2008–present).
Resource Centers
Chairman's Office, The Ohio State University College of Optometry, Columbus, OH.
Karla Zadnik (Chairman, 1997–present) and Jodi M. Malone (Study Coordinator, 1997–present).
Videophakometry Reading Center, The Ohio State University College of Optometry, Columbus, OH.
Donald O. Mutti (Director, 1997–present), Huan Sheng (Reader, 2000–2006), Holly Omlor (Reader, 2003–2006), Meliha Rahmani (Reader, 2004-present), Jaclyn Brickman (Reader, 2002–2003), Amy Wang (Reader, 2002–2003), Philip Arner (Reader, 2002–2004), Samuel Taylor (Reader, 2002–2003), Myhanh T. Nguyen (Reader, 1998–2001), Terry W. Walker (Reader, 1997–2001), Vidhya Subramanian (Reader, 2006–2009), Elizabeth Perry (2010), and Austen Tanner (2009–present).
Optometry Coordinating Center, The Ohio State University College of Optometry, Columbus, OH.
Lisa A. Jones-Jordan (Director, 1997–present), Linda Barrett (Data Entry Operator, 1997–2007), John Hayes (Biostatistician, 2001–2007), G. Lynn Mitchell (Biostatistician, 1998–present), Melvin L. Moeschberger (Consultant, 1997-present), Loraine Sinnott (Biostatistician, 2005–present), Pamela Wessel (Program Coordinator, 2000-present), and Julie N. Swartzendruber (Program Coordinator, 1998–2000).
Project Office, National Eye Institute, Rockville, MD.
Donald F. Everett
Executive Committee
Karla Zadnik (Chairman), Lisa A. Jones-Jordan, Robert N. Kleinstein, Ruth E. Manny, Donald O. Mutti, J. Daniel Twelker, and Susan A. Cotter.
Footnotes
Supported by National Eye Institute/National Institutes of Health Grants U10-EY08893 and R24-EY014792, the Ohio Lions Eye Research Foundation, the E. F. Wildermuth Foundation, the Knights Templar Eye Foundation, and Research to Prevent Blindness.
Disclosure: L.A. Jones-Jordan, None; G.L. Mitchell, None; S.A. Cotter, None; R.N. Kleinstein, None; R.E. Manny, None; D.O. Mutti, None; J.D. Twelker, None; J. R. Sims, None; K. Zadnik, None
References
- 1. Saw SM, Chua WH, Hong CY, et al. Nearwork in early-onset myopia. Invest Ophthalmol Vis Sci. 2002;43:332–339 [PubMed] [Google Scholar]
- 2. Hepsen IF, Evereklioglu C, Bayramlar H. The effect of reading and near-work on the development of myopia in emmetropic boys: a prospective, controlled, three-year follow-up study. Vision Res. 2001;41:2511–2520 [DOI] [PubMed] [Google Scholar]
- 3. Mutti DO, Mitchell GL, Moeschberger ML, Jones LA, Zadnik K. Parental myopia, near work, school achievement, and children's refractive error. Invest Ophthalmol Vis Sci. 2002;43:3633–3640 [PubMed] [Google Scholar]
- 4. Saw SM, Hong CY, Chia KS, Stone RA, Tan D. Nearwork and myopia in young children. Lancet. 2001;357:390. [DOI] [PubMed] [Google Scholar]
- 5. Saw SM, Shankar A, Tan SB, et al. A cohort study of incident myopia in Singaporean children. Invest Ophthalmol Vis Sci. 2006;47:1839–1844 [DOI] [PubMed] [Google Scholar]
- 6. Jones LA, Sinnott LT, Mutti DO, Mitchell GL, Moeschberger ML, Zadnik K. Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci. 2007;48:3524–3532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rose KA, Morgan IG, Smith W, Burlutsky G, Mitchell P, Saw SM. Myopia, lifestyle, and schooling in students of chinese ethnicity in Singapore and Sydney. Arch Ophthalmol. 2008;126:527–530 [DOI] [PubMed] [Google Scholar]
- 8. Jacobsen N, Jensen H, Goldschmidt E. Does the level of physical activity in university students influence development and progression of myopia?—a 2-year prospective cohort study. Invest Ophthalmol Vis Sci. 2008;49:1322–1327 [DOI] [PubMed] [Google Scholar]
- 9. Mutti DO, Mitchell GL, Hayes JR, et al. Accommodative lag before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2006;47:837–846 [DOI] [PubMed] [Google Scholar]
- 10. Mutti DO, Hayes JR, Mitchell GL, et al. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2007;48:2510–2519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Seddon JM, Sahagian CR, Glynn RJ, Sperduto RD, Gragoudas ES. Evaluation of an iris color classification system. The Eye Disorders Case-Control Study Group. Invest Ophthalmol Vis Sci. 1990;31:1592–1598 [PubMed] [Google Scholar]
- 12. Kleinstein RN, Mutti DO, Manny RE, Shin JA, Zadnik K. Cycloplegia in African-American children. Optom Vis Sci. 1999;76:102–107 [DOI] [PubMed] [Google Scholar]
- 13. Zadnik K, Mutti DO, Friedman NE, Adams AJ. Initial cross-sectional results from the Orinda Longitudinal Study of Myopia. Optom Vis Sci. 1993;70:750–758 [DOI] [PubMed] [Google Scholar]
- 14. Zadnik K, Mutti DO, Mitchell GL, Jones LA, Burr D, Moeschberger ML. Normal eye growth in emmetropic schoolchildren. Optom Vis Sci. 2004;81:819–828 [DOI] [PubMed] [Google Scholar]
- 15. Hogg R, Tanis E. Probability and Statistical Inference. 2nd ed. New York: Macmillan Publishing Co.; 1983:266 [Google Scholar]
- 16. Bozdogan H. Model selection and Akaike's Information Criteria (AIC): the general theory and its analytical extensions. Psychometrika. 1987;52:345–370 [Google Scholar]
- 17. SAS/STAT User's Guide ver. 9.1 Cary, NC: SAS Institute Inc.; 2002 [Google Scholar]
- 18. Dirani M, Tong L, Gazzard G, et al. Outdoor activity and myopia in Singapore teenage children. Br J Ophthalmol. 2009;93:997–1000 [DOI] [PubMed] [Google Scholar]
- 19. Rose KA, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115:1279–1285 [DOI] [PubMed] [Google Scholar]
- 20. Fulk GW, Cyert LA, Parker DA. Seasonal variation in myopia progression and ocular elongation. Optom Vis Sci. 2002;79:46–51 [DOI] [PubMed] [Google Scholar]
- 21. Goss DA, Rainey BB. Relation of childhood myopia progression rates to time of year. J Am Optom Assoc. 1998;69:262–266 [PubMed] [Google Scholar]
- 22. Shaikh AW, Siegwart JT, Jr, Norton TT. Effect of interrupted lens wear on compensation for a minus lens in tree shrews. Optom Vis Sci. 1999;76:308–315 [DOI] [PubMed] [Google Scholar]
- 23. Norton TT, Siegwart JT, Jr, Amedo AO. Effectiveness of hyperopic defocus, minimal defocus, or myopic defocus in competition with a myopiagenic stimulus in tree shrew eyes. Invest Ophthalmol Vis Sci. 2006;47:4687–4699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Schmid KL, Wildsoet CF. Effects on the compensatory responses to positive and negative lenses of intermittent lens wear and ciliary nerve section in chicks. Vision Res. 1996;36:1023–1036 [DOI] [PubMed] [Google Scholar]
- 25. Napper GA, Brennan NA, Barrington M, Squires MA, Vessey GA, Vingrys AJ. The effect of an interrupted daily period of normal visual stimulation on form deprivation myopia in chicks. Vision Res. 1997;37:1557–1564 [DOI] [PubMed] [Google Scholar]
- 26. Smith EL, 3rd, Hung LF, Kee CS, Qiao Y. Effects of brief periods of unrestricted vision on the development of form-deprivation myopia in monkeys. Invest Ophthalmol Vis Sci. 2002;43:291–299 [PubMed] [Google Scholar]
- 27. Witkovsky P. Dopamine and retinal function. Doc Ophthalmol. 2004;108:17–40 [DOI] [PubMed] [Google Scholar]
- 28. Iuvone PM, Tigges M, Stone RA, Lambert S, Laties AM. Effects of apomorphine, a dopamine receptor agonist, on ocular refraction and axial elongation in a primate model of myopia. Invest Ophthalmol Vis Sci. 1991;32:1674–1677 [PubMed] [Google Scholar]
- 29. McCarthy CS, Megaw P, Devadas M, Morgan IG. Dopaminergic agents affect the ability of brief periods of normal vision to prevent form-deprivation myopia. Exp Eye Res. 2007;84:100–107 [DOI] [PubMed] [Google Scholar]
- 30. Roberts W, Banford R. Evaluation of bifocal correction techniques in juvenile myopia. Optometry Weekly. 1967;58:21–30 [Google Scholar]
- 31. Stone RA, Lin T, Laties AM, Iuvone PM. Retinal dopamine and form-deprivation myopia. Proc Natl Acad Sci U S A. 1989;86:704–706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dirani M, Tong L, Gazzard G, et al. Outdoor activity and myopia in Singapore teenage children. Br J Ophthalmol. 2009;93:997–1000 [DOI] [PubMed] [Google Scholar]
- 33. Harrison PA, Narayan G. Differences in behavior, psychological factors, and environmental factors associated with participation in school sports and other activities in adolescence. J Sch Health. 2003;73:113–120 [DOI] [PubMed] [Google Scholar]
- 34. Saw SM, Tong L, Chua WH, et al. Incidence and progression of myopia in Singaporean school children. Invest Ophthalmol Vis Sci. 2005;46:51–57 [DOI] [PubMed] [Google Scholar]
- 35. Ip JM, Huynh SC, Robaei D, et al. Ethnic differences in the impact of parental myopia: findings from a population-based study of 12-year-old Australian children. Invest Ophthalmol Vis Sci. 2007;48:2520–2528 [DOI] [PubMed] [Google Scholar]
- 36. Ip JM, Saw SM, Rose KA, et al. Role of near work in myopia: findings in a sample of Australian school children. Invest Ophthalmol Vis Sci. 2008;49:2903–2910 [DOI] [PubMed] [Google Scholar]
- 37. Rideout VJ, Foehr UG, Roberts DF. Generation M2: Media in the Lives of 8- to 18-Year Olds. Menlo Park, CA: Kaiser Family Foundation; 2010:20–26 [Google Scholar]
- 38. Deng L, Gwiazda J, Thorn F. Children's refractions and visual activities in the school year and summer. Optom Vis Sci. 2010;87:406–413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rah MJ, Walline JJ, Lynn Mitchell G, Zadnik K. Comparison of the experience sampling method and questionnaires to assess visual activities in pre-teen and adolescent children. Ophthalmic Physiol Opt. 2006;26:483–489 [DOI] [PubMed] [Google Scholar]
- 40. Saw SM, Nieto FJ, Katz J, Chew SJ. Estimating the magnitude of close-up work in school-age children: a comparison of questionnaire and diary instruments. Ophthalmic Epidemiol. 1999;6:291–301 [DOI] [PubMed] [Google Scholar]