Abstract
Increasing attention is being paid to the importance of built environment characteristics for participation, especially among people with various levels of impairment or activity limitations. The purpose of this research was to examine the role of specific characteristics in the urban environment as they interact with underlying impairments and activity limitations to either promote or hinder participation in life situations. Using data from the Chicago Community Adult Health Study (2001–2003) in the United States, we used logistic regression to examine the effect of built environment characteristics on three indicators of participation (interpersonal interaction, obtaining preventive health care, and voting) among adults age 45+ (N=1225). We examined effects across two levels of spatial scale: the census tract and block group. One in five adults reported difficulty walking 2–3 blocks unaided, but their odds of engaging in regular interpersonal interaction was 45% higher when they lived in areas with higher residential security. For the thirty-six percent of adults who reported visual impairment, and the odds of obtaining preventive health care were over 20% lower when living in an area with heavy traffic. Residing in an area with a high proportion of streets in poor condition was associated with 60% lower odds of voting among those with underlying difficulty with mobility activities. Results varied across levels of spatial scale. Simple changes in urban built environments may facilitate the full participation of all persons in society.
Keywords: aging, disability, built environment, interpersonal interaction, USA
Disability is an umbrella term encompassing impairments, activity limitations and participation restrictions, which are all dynamically influenced by environmental and individual factors (World Health Organization, 2001). Disability continues to be a major health and social issue, particularly within the context of an aging population. While evidence indicates that the prevalence of disability has been declining since the 1990s (Crimmins 2004; Freedman et al. 2004; Freedman, Martin and Schoeni 2002; Manton and Gu 2001), recent data suggest that disability has begun to increase for all but the oldest Americans (Martin et al. 2010; Seeman et al. 2010). Yet, disability is not necessarily a feature of aging nor an inevitable response to the onset or progression of a health problem. As pointed out by the sociologist Saad Nagi (1965), one of the early pioneers in this field, “disability is the expression of a physical or mental limitation in a social context”.
While the role of environmental factors for impairments and activity limitations has been the subject of several studies (e.g. Clarke and George 2005; Clarke et al. 2008; Clarke, Ailshire and Lantz 2009; Yang et al. 1997), the concept of participation (defined as involvement in a life situation (WHO, 2001)) has only recently received attention in the field of disability (Gray et al. 2008; Rimmer et al. 2004; Jette et al. 2005; Hollingsworth and Gray, 2010). Questions remain about how to best conceptualize this construct in relation to environmental factors (Whiteneck and Dijkers 2009). The intent of this paper is to use data from a representative survey of 1225 Chicago adults to understand the dynamics of participation using measures of social interaction, obtaining healthcare, and voting. The aim here is to better understand the interrelationship between impairments and activity limitations as they interact with characteristics in the built environment to influence participation.
Models of Disability
Models of disability (Nagi 1965; Verbrugge and Jette 1994), and the framework on functioning issued by the World Health Organization (WHO, 2001), have increasingly incorporated contingency in the disability pathway by explicitly recognizing the role of contextual factors. The International Classification of Functioning, Disability and Health (WHO, 2001) (known as the ICF) is based on the biopsychosocial model of health and belongs to the family of international classifications developed by the WHO. While health conditions are classified primarily in ICD-10, the ICF provides a framework to collect a wide range of information about health, functioning, and disability, using standardized uniform common language. In 2001 the World Health Assembly endorsed the ICF for international use and urged member states to use the ICF in research, surveillance, and reporting.
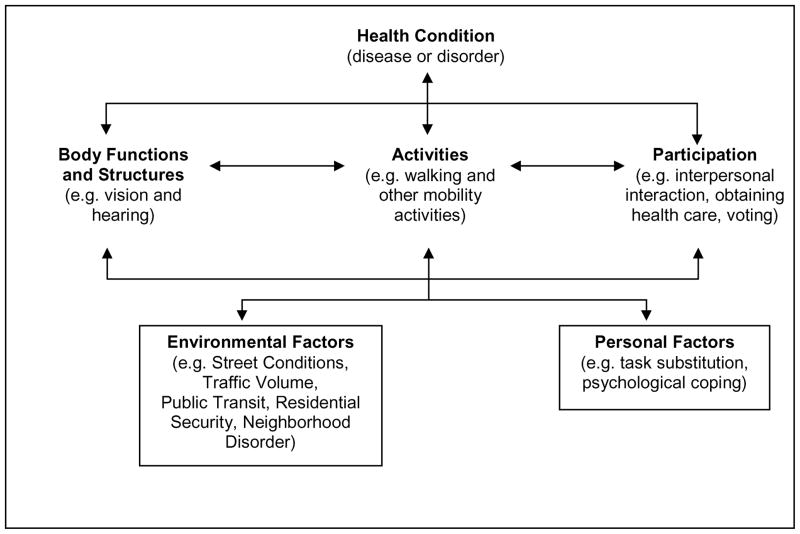
The ICF (Figure 1) is a conceptual framework that incorporates functioning at three levels: the level of the body (e.g. mental, emotional, physiological, or anatomical structures or functions), the level of the individual (e.g. activities such as mobility, self care, general tasks), and at the level of society (participation in life situations and social roles) (Jette and Badley 2000). Difficulty in functioning at these three levels is represented by impairments, activity limitations, and participation restrictions. For example, an individual with arthritis may experience pain (impairment in sensory functions) that leads to difficulty in walking (activity limitation), which may restrict his or her involvement in life situations, such as meeting with close friends (participation restriction). The ICF also incorporates environmental and personal factors that can impede or enhance a person’s functioning at these three levels. Environmental factors are classified under five broad headings: products and technology; natural environment and human-made changes to the environment; support and relationships; attitudes; services, systems and policies (WHO 2001). In this research we focus on the modifying effect of the urban built environment in the pathway between impairments or activity limitations and participation (restrictions).
Figure 1.
Interactions between the Components of the ICF Model (adapted from WHO, 2001)
The interactive role of the built environment for disability can be illustrated by comparing two individuals who have sustained a stroke. Although they both have a severe right hemiparesis and can no longer drive, they may have very different levels of independence and participation. For instance, one person may live close to an accessible public transit system, with connections to local stores and services to permit the accomplishment of day-to-day activities (e.g. shopping and banking) and social interaction. The other person may live in a more suburban community with limited sidewalks and crosswalks, and the nearest bus stop is four blocks away. As a consequence, the second person will experience considerable problems with daily activities and social isolation even though he or she has the same underlying health condition. As emphasized by Nagi (1991, p.315), “characteristics of the environment and the degree to which it is free from, or encumbered with, physical and sociocultural barriers” can lead to very different patterns and levels of independence and participation in those with identical types of impairments or activity limitations.
The Built Environment in the Disablement Process
There has been considerable attention to the role of environmental factors for physical activity and obesity (e.g. Diez Roux et al. 2007; Morenoff et al. 2008; Morland, Wing and Diez Roux 2002), and a growing body of literature has examined the importance of the environment for disability. For example, poor street conditions, heavy traffic, and excessive noise have been shown to be associated with the onset of difficulty with movement related activities (e.g. standing in place, lifting heavy objects, climbing stairs) up to three years later (Balfour and Kaplan 2002; Schootman et al. 2006). Uneven sidewalks and sidewalk obstacles (i.e. stones and other debris) are responsible for the vast majority of outdoor falls among older adults (Li et al. 2006), and data from the city of Chicago indicate that poor street conditions are associated with a four-fold higher odds of walking difficulty among adults with underlying lower extremity weakness (Clarke et al. 2008). Results from nationally representative panel data in the United States have shown that living in neighborhoods characterized by more motorized travel is associated with a 50% higher odds of mobility limitations over time (Clarke, Ailshire, and Lantz 2009).
Research is also increasingly focusing on the consequences of the environment for participation, especially from the perspective of community-based rehabilitation (e.g. Hollingsworth and Gray, 2010). While performance of an activity takes place at the individual level, participation is performance at the societal level through the fulfillment of social roles (Whiteneck and Dijkers 2009; WHO 2001). Barriers in the built environment may have consequences for participation if adults with underlying impairments or activity limitations become fearful of walking outside on their own, with spillover effects on social isolation (Debnam et al. 2002), the ability to carry out daily activities (e.g. shopping, banking) (Clarke and George 2005; Keysor et al. 2010), and nursing home admission (Cohen, Tell and Wallack 1986; Gill, Allore and Han 2006; Jette et al. 1992). More than half of adults with disability (impairments and/or activity limitations) do not engage in any leisure-time physical activity in part because of barriers related to the built and natural environment (Rimmer et al. 2004). Moreover, people with movement-related impairments and mobility limitations are less likely to receive cancer screening and other preventive health services (Chevarley et al. ; Iezzoni et al. 2000; Ramirez et al. 2005), and anecdotal reports indicate that this is partly due to physical barriers either within or leading up to health care facilities (Andriacchi 1997; Gans, Mann and Becker 1993).
The purpose of this work was to examine the role of certain characteristics in the urban built environment as they interact with underlying impairments and activity limitations either to promote or hinder the participation of adults in society. Using existing data from a large representative survey of American adults in the city of Chicago, and mapping variables to ICF categories, we focus on three broad aspects of participation: interpersonal interaction; engaging in political life and citizenship (i.e. voting); and obtaining preventive health care. We examine how participation differs in adults with impairments in vision and hearing, and among those with limitations in walking and other mobility activities (Figure 1). Consistent with the ICF, we hypothesize that observed characteristics in the surrounding environment (i.e. heavy traffic, poor street conditions, low residential security, lack of public transit, as well as indicators of neighborhood social disorder) may impede participation among those who have visual or hearing impairment, or movement-related activity limitations, simply because such characteristics create obstacles that make it more difficult for people with these impairments or activity limitations to get out into the community for the purposes of interacting with others, voting, or obtaining health care. We anticipate that some aspects of participation (e.g. interpersonal interaction) may be more sensitive to characteristics in the respondent’s more proximate neighborhood environment (e.g. US Census block group, which is a cluster of residential blocks with about 1500 people on average), while other aspects, such as voting, may be more dependent on the makeup of the larger surrounding area (e.g. US Census tract, averaging about 4000 people). We investigate these differences by empirically examining effects across both levels of spatial scale for each outcome variable. Our focus is less on the conceptualization and measurement of participation as a construct (a topic of growing interest in the literature (Dijkers 2010; Noreau et al. 2004; Perenboom and Perenboom 2003; Whiteneck and Dijkers 2009)) than on the dynamics between the environment and individual impairments/limitations as they shape participation in society and social roles.
Methods
Data
The data source for this research is the Chicago Community Adult Health Study, which was conducted in 2002 through face-to-face interviews with a multi-stage representative sample of 3,105 adults aged 18 and over, living in the city of Chicago, and stratified into 343 neighborhood clusters previously defined by the Project on Human Development in Chicago Neighborhoods (Sampson, Raudenbush et al. 1997). The response rate for this study was 72%, one of the highest in a major American city in recent decades (Galea and Tracy 2007). All study procedures were reviewed and approved by the University of Michigan’s Institutional Review Board and study participants gave informed consent. For our purposes we restrict our analyses to 1225 adults age 45 and over (40% of the sample) in order to focus on the age group most at risk for health-related impairments and activity limitations (National Center for Health Statistics, 2006). The weighted sample matches the 2000 Census population estimates for the city of Chicago in terms of age, race/ethnicity and gender.
Measures of the Urban Built Environment
The Chicago Community Adult Health Study was specifically designed to examine the relationship between neighborhoods and health, and observational data were collected on the city block around each respondent’s residence through the method of systematic social observation (SSO) (Raudenbush and Sampson 1999; Sampson and Raudenbush 1999). SSO is a direct observational method that capitalizes on the interviewer’s visits to the homes. While walking around the residential block where each respondent lives, the survey interviewer characterizes these small respondent-centered neighborhoods using a standardized instrument. On average, observations for each street were completed in about 15 minutes (one hour for each block). Inter-rater reliability of this method was demonstrated using a subsample of 80 blocks in a pilot study conducted in 2001 where two raters made separate, independent observations of the same block at the same time. Observed (percentage) agreement ranged from .78 to 1.00 (Kappa =.27 to .91).
Using multilevel item response models, observations at the block face or street level are aggregated up to characterize the larger neighborhood area of the block group and census tract (approximately 1500 persons and 4000 persons, respectively). For the purposes of our research, we focus on five characteristics of the urban environment that may hinder or facilitate participation in those with underlying impairments or activity limitations. Specifically, we use an indicator of the quality of the streets and sidewalks (percent of streets in the block group or census tract that are in very poor condition, defined as many sizeable cracks, potholes, or broken curbs). Volume of traffic was assessed according to the percent of streets with heavy traffic (defined as a steady stream of cars). We also include a variable to indicate whether there is a public transit line (Chicago Transit Authority (CTA) line) within 500 meters of the respondent’s residence.
An index of neighborhood physical and social disorder (Raudenbush and Sampson 1999) is derived from observations of the block faces with respect to the presence of graffiti, garbage, litter or broken glass, cigarette butts, empty beer/liquor bottles, abandoned cars, and drug-related paraphernalia or condoms on sidewalks or in street gutters. We also include a measure of residential security based on the presence of neighborhood crime watch signs and security warning signs. For each construct, the presence of these items on block faces was used to create multilevel item response models that weight less common, but more discriminating, items more heavily than more prevalent or common items (Raudenbush and Sampson 1999). Because the presence of an item is dichotomous, the overall measures are expressed on a logit scale (ranging from negative to positive) with a high score indicating a high presence of disorder or residential security. Convergent validity of the scales has been demonstrated when compared against census measures of concentrated poverty as well as crime reports (Raudenbush and Sampson 1999). Cronbach’s alpha for the security and disorder scales are .72 and .94, respectively.
Individual Measures
We use three indicators of participation. Interpersonal interaction is assessed by the frequency of getting together with friends, neighbors and relatives, either going out together or visiting in each others’ homes. We use a binary variable to contrast those who get together at least once per month with those who interact with others only rarely (less than once per month) or never. Use of preventive health care is a dichotomous variable indicating whether the respondent had a physical exam, blood pressure check, and cholesterol check in the past two years. Finally, we included a dummy variable to indicate whether the respondent had voted in the last federal and/or mayoral election.
Impairments and activity limitations included self-reported visual impairment assessed through two questions asking about trouble seeing well enough to recognize a friend across the street, and difficulty seeing well enough to read a newspaper (even with glasses, on a scale ranging from 0 to 3 (none, a little, some, a great deal) and averaged across the two measures to create an index of visual impairment). Hearing impairment is similarly assessed with two questions asking about difficulty hearing and understanding words in a normal conversation, and hearing well enough to carry on a conversation in a noisy room (even with a hearing aid, on a scale from 1 (none) to 4 (a great deal), and averaged across the two questions). Respondents were also asked about their level of difficulty walking 2–3 blocks without help (dichotomized according to whether they reported any difficulty vs. none). A separate composite measure of difficulty with other mobility activities was created by averaging the reported level of difficulty with seven activities (stooping, kneeling, climbing stairs, getting up from a chair, moving a heavy object, lifting or carrying, standing up from a kneeling position) as well as one item related to domestic activity (doing heavy housework), all assessed on a five point scale (no difficulty, some difficulty, a lot of difficulty, unable to do without help, cannot do at all). We use a binary variable in our analyses to contrast those who report no (or only some) difficulty (mean score ranges from 0–1.5) with those who have a lot of difficulty or are unable to perform these activities (mean score greater than 1.5).
Individual Controls
We control for key sociodemographic and health factors that could account for the relationships between impairments/activity limitations and participation, and could also differentially select people into areas with different urban characteristics. Sociodemographic factors (or in terms of the ICF: personal factors) include age, gender, marital status, race/ethnicity, and socioeconomic position (SEP). Age is represented by two dummy variables contrasting older adults (age 60 to 69) and very old adults (age 70 plus) with middle-age adults (age 45 to 59). Gender is a dummy variable coded 1 for males and 0 for females. Marital status is captured by three dummy variables contrasting divorced/separated, widowed, and never married, with married respondents. We also use a dummy variable to indicate whether or not the respondent lived alone. Race/ethnicity is categorized according to three dummy variables contrasting Black, Hispanic, and other race/ethnicity (including Native American, Asian, or Pacific Islander) with Whites. Socioeconomic position is assessed through the respondent’s level of education, classified as less than high school, high school diploma, or college degree. Household income is captured with two dummy variables contrasting those with annual incomes less than $15,000 and $15,000–$40,000 with those whose annual incomes are over $40,000. A dummy variable indicates missing data on income.
We also control for underlying health status using an index of self-reported chronic health problems that sums the number of medically diagnosed health conditions (e.g. heart attack, stroke, arthritis, diabetes, peripheral artery disease), current cigarette smoking and body mass index (weight in kilograms/height in meters squared). Cognitive function is a composite index derived from 26 items measuring orientation to time and place, attention and concentration (serially subtracting 3 from 20), and short term memory (immediate and delayed recall of 10 nouns). A summary score is created by totaling the number of correct answers, with a higher score indicating higher cognitive function. For models examining preventive health care, we include a dummy variable to control for whether the respondent has health insurance (e.g. Medicare, Medicaid, Medigap, VA, HMO, PPO) and a dummy variable to indicate whether respondents could rely on someone to take them to the doctor if needed.
Mediators of Neighborhood Characteristics
We examine a number of variables that could potentially mediate the effects of neighbourhood characteristics on participation in order to better understand the mechanisms by which the urban environment facilitates or impedes participation in those with underlying impairments and activity limitations. We use subjective reports from the respondents about fear of walking (based on a question about whether respondents are afraid to walk alone at night in their neighbourhood) and perceived violence (based on respondent reports of gang fights, robberies, use of weapons in their neighbourhood) hypothesizing that these fears may operate as mediators of residential security and/or neighbourhood social disorder. Similarly, perceptions of dangerous traffic, perceived noise, perceptions of poor air quality, and a composite index of physical hazards in one’s neighborhood (derived from perceptions of noise, poor air quality, traffic danger, toxic substances, and the presence of rats/mice/roaches) may mediate some of the effects of street conditions and traffic volume on participation.
Statistical Analyses
For each of the three measures of participation, we use binary logistic regression, and examine the effects at two levels of spatial scale, the census tract and block group. Single level logistic models are conducted for analyses at the block group level (average 1.5 observations per group, range 1–7) and multi-level logistic models are conducted for analyses at the level of the census tract to account for the clustering within tracts (2.4 observations per tract, range 1–12). Single level models were conducted in SAS Version 9.2 and multi-level models were run using HLM 6.08 (Raudenbush and Bryk 2002). For ease of interpretation, measures of the urban environment were standardized (mean of zero, standard deviation of one). All analyses were weighted by post-stratification sample weights to account for the sampling design as well as differential coverage and non-response across neighbourhood clusters.
Results
Descriptive Statistics
On average, respondents in this sample are 60 years of age, with over half (54.3%) between the ages of 45 and 59, and 23% age 70 and over. The sample is well balanced in terms of gender (43.9% male), race/ethnicity (42.7% white, 35.8% black, 18.5% Hispanic, 3% other race/ethnicity), and marital status (50.3% married). Almost a third (30.4%) of these adults have less than a high school education and one in five report annual household incomes below $15,000. On average, these adults report 2 (standard deviation=1.8) chronic health conditions, and a third report visual or hearing impairment. One fifth of these adults (19.4%) report difficulty walking 2–3 blocks unaided and 10% have difficulty with other mobility activities. On average, cognitive function is in the upper middle range of the 26 point scale (mean score=14.5, standard deviation=3.9). Roughly 1 in 5 adults are current smokers (21%), and respondents have an average BMI around 29 (standard deviation=6.5). Just over 12 percent of these Chicago adults have no health insurance.
In terms of participation, three-quarters (77.6%) of respondents interact with friends, neighbors, and relatives at least once per month. Almost 80 percent voted in a previous election and half (50.2%) had obtained preventive health services in the past 2 years. On average, 8 percent of the streets in these residential blocks are in poor condition, and 15 percent of the streets are characterized by heavy traffic. Signs of neighborhood disorder are relatively low (mean score of −2.7 (standard deviation=1.7), scale ranges from −7.3 to 2.2 on the logit scale) and average residential security (mean score=−.8, standard deviation=.9) falls in the upper midrange of the logit scale (range −3.1 to 1.7). One fifth (18.4%) of respondents live within 500 meters of a CTA public transit line.
Interpersonal Interaction
Table 1 presents the logistic regression coefficients and odds ratios from the binary logistic regression models for the three measures of participation. The top panel shows the results for interpersonal interaction at the block group level (reference group is never or rarely engaging in social interaction with friends, neighbors or relatives). We did not find any effects of neighborhood characteristics at the larger tract level on interpersonal interaction, indicating that more proximate characteristics in one’s immediate environment are more salient for interpersonal interaction than characteristics in the wider neighborhood area. Individuals with visual impairment and those who report difficulty walking 2–3 blocks have significantly lower odds of interpersonal interaction (first column of Table 1). Higher levels of neighborhood social disorder are associated with 25 percent lower odds of interpersonal interaction (second column of Table 1), but living in a block group with heavy traffic is associated with greater interpersonal interaction (perhaps because these areas also tend to have more public transit stops (not captured by our measure of proximity to CTA lines) or cafes and restaurants that facilitate interaction).
Table 1.
Binary Logistic Regression Models for Participation by Impairment/Activity Limitations and Built Environment Characteristics
| Impairment/Activity Limitation | Urban Environment | Impairment/Activity Limitation x Environment | ||||
|---|---|---|---|---|---|---|
| Coeff. | OR (95% CI) | Coeff. | OR (95% CI) | Coeff. | OR (95% CI) | |
| Model for Interpersonal Interaction1 | ||||||
| Intercept | 1.64*** | 1.29*** | 1.69*** | |||
| Impairments/Activity Limitations | ||||||
| Visual Impairment | −.22* | .81 (.68–.96) | −.24** | .78 (.65–.94) | ||
| Hearing Impairment | −.09 | .91 (.77–1.1) | −.08 | .93 (.78–1.1) | ||
| Difficulty with Mobility Activities | −.07 | .93 (.56–1.5) | −.23 | .80 (.48–1.3) | ||
| Any Difficulty Walking 2–3 blocks | −.65*** | .52 (.35–.77) | −.55** | .58 (.39–.86) | ||
| Built Environment Characteristics | ||||||
| Streets in Poor Condition | −.05 | .95 (.83–1.1) | −.01 | .99 (.86–1.1) | ||
| Heavy Traffic | .23** | 1.3 (1.1–1.5) | .23** | 1.3 (1.1–1.5) | ||
| Neighborhood Social Disorder | −.28*** | .75 (.65–.88) | −.23** | .79 (.68–.93) | ||
| Residential Security | .03 | 1.0 (.9–1.2) | −.06 | .94 (.79–1.1) | ||
| Public Transit Line Nearby | −.09 | .91 (.64–1.3) | −.12 | .89 (.61–1.3) | ||
| Impairment x Environ Interactions | ||||||
| Walking Difficulty x Res Security | .32* | 1.4 (1.0–1.9) | ||||
|
| ||||||
| Model for Obtaining Health Care2 | ||||||
| Intercept | .08 | .01 | .05 | |||
| Impairments/Activity Limitations | ||||||
| Visual Impairment | −.30*** | .74 (.63–.87) | −.32*** | .73 (.61–.86) | ||
| Hearing Impairment | .09 | 1.1 (.93–1.3) | .10 | 1.1 (.94–1.3) | ||
| Difficulty with Mobility Activities | −.09 | .92 (.57–1.5) | −.12 | .89 (.55–1.4) | ||
| Any Difficulty Walking 2–3 blocks | −.33 | .72 (.50–1.0) | −.33 | .72 (.50–1.0) | ||
| Built Environment Characteristics | ||||||
| Streets in Poor Condition | −.01 | .99 (.88–1.1) | .01 | 1.0 (.89–1.1) | ||
| Heavy Traffic | −.05 | .95 (.85–1.1) | .03 | 1.0 (.89–1.2) | ||
| Neighborhood Social Disorder | −.21*** | .82 (.72–.92) | −.17** | .85 (.74–.96) | ||
| Residential Security | .03 | 1.0 (.91–1.2) | .03 | 1.0 (.91–1.2) | ||
| Public Transit Line Nearby | .04 | 1.0 (.77–1.4) | .02 | 1.0 (.75–1.4) | ||
| Impairment x Environ Interactions | ||||||
| Visual Impairment x Heavy Traffic | −.20* | .82 (.68–.97) | ||||
|
| ||||||
| Model for Voting3 | ||||||
| Intercept | 1.23*** | 1.46*** | 1.33*** | |||
| Impairments/Activity Limitations | ||||||
| Visual Impairment | −.10 | .91 (.73–1.1) | −.12 | .89 (.72–1.1) | ||
| Hearing Impairment | .18 | 1.2 (.94–1.5) | .19 | 1.2 (.95–1.5) | ||
| Difficulty with Mobility Activities | −.63 | .53 (.26–1.1) | −.62 | .54 (.27–1.1) | ||
| Any Difficulty Walking 2–3 blocks | .54 | 1.7 (.98–3.0) | .58 | 1.8 (.99–3.2) | ||
| Built Environment Characteristics | ||||||
| Streets in Poor Condition | .22* | 1.2 (1.0–1.5) | .28** | 1.3 (1.1–1.6) | ||
| Heavy Traffic | .18 | 1.2 (.98–1.4) | .17 | 1.2 (1.0–1.3) | ||
| Neighborhood Social Disorder | −.13 | .88 (.69–1.1) | −.14 | .86 (.67–1.1) | ||
| Residential Security | .08 | 1.1 (.93–1.3) | .10 | 1.1 (.92–1.3) | ||
| Public Transit Line Nearby | −.35 | .71 (.44–1.2) | −.36 | .70 (.44–1.1) | ||
| Impairment x Environ Interactions | ||||||
| Mobility Difficulty x Street Conditions | −.66** | .52 (.31–.87) | ||||
p<.05
p<.01
p<.001 (two-tailed tests) OR = odds ratio CI = confidence interval
Reference group is never or rarely engaging in interpersonal interaction; single level model at block group level
Reference group is no preventive health care (no cholesterol check, no blood pressure exam, and no physical exam) in past 2 years; single level model at block group level
Reference group is not voting in past mayoral or federal elections; multilevel model at tract level
The third column of Table 1 reports the results from models that test for interaction effects between an individual’s impairment or activity limitation and the surrounding neighborhood characteristics. We found a significant interaction effect between walking difficulty and residential security (other combinations of impairment and environmental factors were also tested but no other significant interaction effects were found). For adults who report no difficulty walking 2–3 blocks, residential security has no effect on interpersonal interaction. But for adults who experience walking difficulty, living in a block group with greater residential security (one standard deviation above the mean) is associated with significantly higher odds of interpersonal interaction than for adults with difficulty walking who live in a block group with lower residential security.
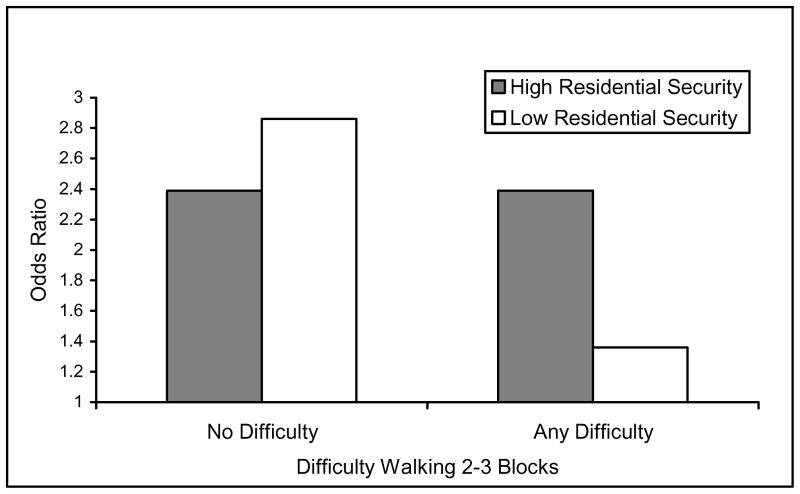
The base model in Table 2 (first column) presents the effects of residential security from Table 1 (final column) calculated for adults with and without walking difficulty. Effects indicate that, for adults who have difficulty walking, the odds of interpersonal interaction are 30 percent higher when they live in an area with higher levels of residential security. The second column adds the individual control variables, which only serves to strengthen the effect of residential security on interpersonal interaction for those who have difficulty walking. Results from these models also indicate significant gender and racial differences in interpersonal interaction, and that better cognitive function is associated with more frequent interpersonal interaction. The final column in Table 2 adds potential mediators to try to explain the effects of residential security on interpersonal interaction for those who have difficulty walking. As expected, fear of walking in one’s neighborhood is strongly associated with less frequent interaction (adjusted OR=.77, 95% CI=.63–.92), but this did not mediate any effects of residential security. Perceived neighborhood violence was not associated with interpersonal interaction over and above fear of walking. Predicted odds ratios are presented in Figure 2a according to levels of walking difficulty and residential security (one standard deviation above and below the mean for high and low residential security, respectively). Adjusting for controls, the odds ratio for interpersonal interaction among those who have difficulty walking is 45% higher in areas with higher residential security than the corresponding odds ratio for those living in areas with lower residential security.
Table 2.
Binary Logistic Regression Model for Interpersonal Interaction1 by Difficulty Walking and Residential Security (at the Block Group Level)
| Base Model | + Controls | + Mediators | ||||
|---|---|---|---|---|---|---|
| Coeff. | OR (95% CI) | Coeff. | OR (95% CI) | Coeff. | OR (95% CI) | |
| Intercept | 1.69*** | 5.4 (4.0–7.3) | .96 | 2.6 (.95–7.2) | .97 | 2.6 (.89–7.9) |
| Effect of Residential Security: | ||||||
| For adults with no difficulty walking | −.06 | .94 (.79–1.1) | −.09 | .91 (.76–1.1) | −.09 | .91 (.76–1.1) |
| For adults with difficulty walking | .26* | 1.3 (1.0–1.7) | .28* | 1.3 (1.0–1.8) | .29* | 1.3 (1.0–1.8) |
| Other Built Environ Characteristics | ||||||
| Streets in Poor Condition | −.01 | .99 (.86–1.1) | .02 | 1.0 (.88–1.2) | .03 | 1.0 (.89–1.2) |
| Heavy Traffic | .23** | 1.3 (1.1–1.5) | .18* | 1.2 (1.0–1.4) | .19* | 1.2 (1.0–1.4) |
| Neighborhood Social Disorder | −.23** | .79 (.68–.93) | −.04 | .96 (.81–1.1) | −.02 | 1.0 (.85–1.2) |
| Public Transit Line Nearby | −.12 | .89 (.61–1.3) | −.19 | .82 (.56–1.2) | −.20 | .82 (.55–1.2) |
| Individual Controls | ||||||
| Age 60–69a | .12 | 1.1 (.76–1.7) | .10 | 1.1 (.74–1.6) | ||
| Age 70+ a | −.03 | .97 (.62–1.5) | −.07 | .93 (.59–1.5) | ||
| Maleb | −.40** | .67 (.49–.92) | −.44** | .64 (.47–.89) | ||
| Blackc | −.59** | .56 (.38–.82) | −.55** | .58 (.39–.85) | ||
| Hispanicc | −.12 | .89 (.56–1.4) | −.07 | .93 (.58–1.5) | ||
| Other Race/Ethnicityc | 2.35 | 10.5 (.83–132) | 2.31 | 10.1 (.79–126) | ||
| Separated/Divorcedd | .04 | 1.0 (.68–1.6) | .06 | 1.1 (.69–1.6) | ||
| Widowedd | .26 | 1.3 (.77–2.2) | .29 | 1.3 (.79 (2.4) | ||
| Never Marriedd | .30 | 1.3 (.78–2.3) | .33 | 1.4 (.80–2.4) | ||
| Lives Alone | .20 | 1.2 (.81–1.9) | .22 | 1.2 (.82–1.9) | ||
| <HS Educatione | −.32 | .73 (.43–1.2) | −.33 | .72 (.43–1.2) | ||
| HS Educatione | −.27 | .76 (.48–1.2) | −.27 | .76 (.49–1.2) | ||
| Income <$15,000f | −.35 | .71 (.43–1.2) | −.34 | .71 (.44–1.2) | ||
| Income $15–40,000f | −.36 | .70 (.45–1.1) | −.35 | .71 (.46–1.1) | ||
| Income missingf | .04 | 1.0 (.66–1.6) | .08 | 1.1 (.69–1.7) | ||
| Current Smoker | .01 | 1.0 (.69–1.5) | −.01 | .99 (.69–1.5) | ||
| Body Mass Index | −.03 | .97 (.83–1.1) | −.06 | .94 (.81–1.1) | ||
| Number of Chronic Conditions | .02 | 1.0 (.93–1.1) | .02 | 1.0 (.93–1.1) | ||
| Cognitive Function | .09*** | 1.1 (1.0–1.1) | .09*** | 1.1 (1.0–1.1) | ||
| Visual Impairment | −.24** | .78 (.65–.94) | −.11 | .90 (.74–1.1) | −.08 | .92 (.75–1.1) |
| Hearing Impairment | −.08 | .93 (.78–1.1) | −.08 | .93 (.77–1.1) | −.06 | .94 (.78–1.1) |
| Difficulty with Mobility Activities | −.23 | .80 (.48–1.3) | −.18 | .83 (.48–1.5) | −.18 | .83 (.48–1.5) |
| Any Difficulty Walking 2–3 Blocks | −.55** | .58 (.39–.86) | −.37 | .69 (.44–1.1) | −.32 | .72 (.46–1.1) |
| Mediators of Residential Security | ||||||
| Fear of walking in neighborhood | −.27** | .77 (.63–.92) | ||||
| Perceived neighborhood violence | −.05 | .95 (.73–1.2) | ||||
Reference group is never or rarely engaging in interpersonal interaction; single level model at block group level HS= high school CI= confidence interval
p<.05
p<.01
p<.001 (two-tailed tests)
Reference group is Age 45–59
Reference group is Female
Reference group is white
Reference group is married
Reference group is college degree or higher (16+ years of education)
Reference group is income $40,000 or higher
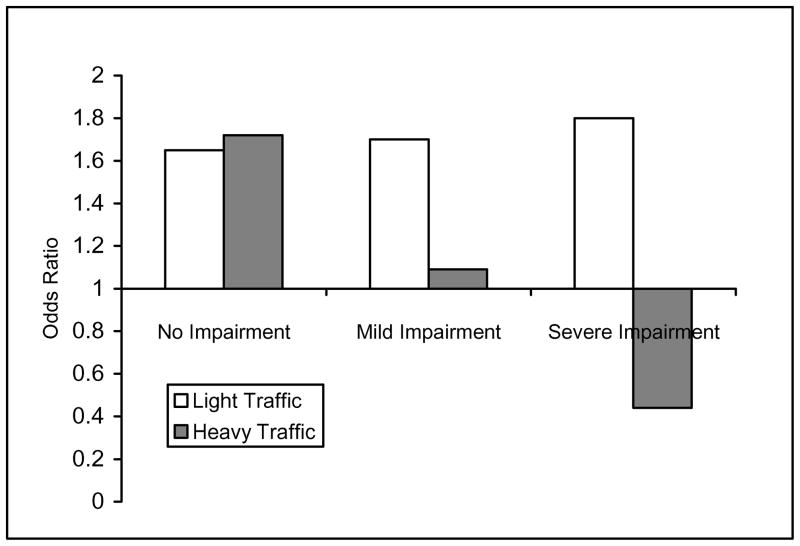
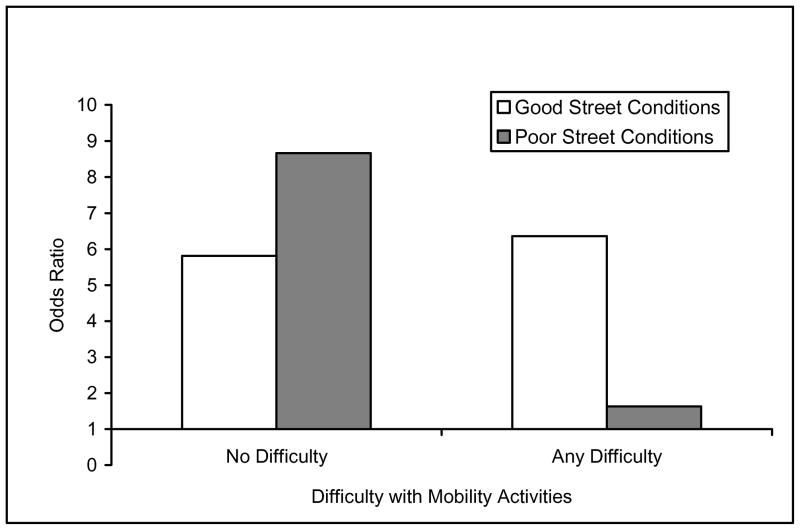
Figure 2.
Figure 2a. Odds Ratios for Interpersonal Interaction by Walking Difficulty and Residential Security*: Chicago Community Adult Health Study, Age 45+
Figure 2b. Odds Ratios for Obtaining Preventive Health Care by Visual Impairment and Traffic Volume*: Chicago Community Adult Health Study, Age 45+
Figure 2c. Odds Ratios for Voting by Mobility Difficulty and Quality of Street Conditions*: Chicago Community Adult Health Study, Age 45+
*Models control for age, gender, race/ethnicity, marital status, living arrangements, education, income, multiple health indicators, cognitive function, heavy traffic, street conditions, public transit lines, and neighborhood social disorder. Predicted values are calculated for a married, white female, age 45–59, with college education, and no chronic health problems (with health insurance for preventive health care model).
Obtaining Preventive Health Care
The second panel of Table 1 presents the results for the logistic regression model for obtaining preventive health care. Similar to interpersonal interaction, built environment effects were only significant at the smaller block group level, not for the larger area of the census tract. Visual impairment is associated with 26% lower odds of having a blood pressure check, cholesterol check, and physical exam in the past two years (OR=.74, 95% CI=.63–.87), but the effects vary by the volume of traffic in one’s block group neighborhood. For adults without visual impairment, traffic volume has no association with preventive health care. But for adults with increasing levels of visual impairment, living in an area with a heavy volume of traffic is associated with significantly lower odds of obtaining preventive health care compared to adults with visual impairment who live in areas with lighter traffic. Among all adults, neighborhood social disorder is associated with lower odds of obtaining preventive health care, but this did not vary according to underlying impairments or activity limitations.
The effects of heavy traffic calculated across different levels of visual impairment are presented in the first column of Table 3. Effects are illustrated for no impairment (score of 0 on the visual impairment index, representing 64% of the sample), mild impairment (score of 1, 23% of the sample), and severe impairment/difficulty seeing even with glasses (score of 3, 4.5% of the sample). Results indicate that for adults with mild and severe visual impairment, the respective odds of obtaining preventive health care are 16% and 44% lower when living in an area of heavy traffic than for similar adults living in areas with lighter traffic. The second column of Table 3 adds the control variables, which results in an increase in the negative effect of heavy traffic across levels of visual impairment. There are also strong gender, education and income disparities in obtaining preventive care, with men, lower educated and lower income adults significantly less likely to have received preventive health care in the past two years (adjusted OR = .62, .59, .53, respectively) even controlling for health insurance, which has a strong effect. After adjusting for individual sociodemographic and socioeconomic factors, neighborhood social disorder is no longer associated with preventive health care suggesting that the unadjusted effect of neighborhood disorder is a function of neighborhood composition. Results did not change when controlling for whether the respondent indicated that he/she could rely on someone to help get to the doctor if needed.
Table 3.
Binary Logistic Regression Model for Obtaining Preventive Health Care1 by Visual Impairment and Volume of Traffic (at the Block Group Level)
| Base Model | + Controls | + Mediators | ||||
|---|---|---|---|---|---|---|
| Coeff. | OR (95% CI) | Coeff. | OR (95% CI) | Coeff. | OR (95% CI) | |
| Intercept | .05 | 1.0 (.82–1.3) | .52 | 1.7 (.64–4.4) | .30 | 1.3 (.46–3.9) |
| Effect of Heavy Traffic: | ||||||
| For adults with no visual impairment | .03 | 1.0 (.89–1.2) | .02 | 1.0 (.87–1.2) | .01 | 1.0 (.87–1.2) |
| For adults with mild visual impairment | −.17* | .84 (.71–.99) | −.22* | .80 (.66–.96) | −.25* | .78 (.64–.95) |
| For adults with severe visual impairment | −.57* | .56 (.35–.93) | −.70** | .50 (.28–.86) | −.76** | .47 (.26–.84) |
| Other Built Environ Characteristics | ||||||
| Streets in Poor Condition | .01 | 1.0 (.89–1.1) | .01 | 1.0 (.88–1.2) | .01 | 1.0 (.88–1.2) |
| Neighborhood Social Disorder | −.17** | .85 (.74–.96) | .05 | 1.0 (.90–1.2) | .03 | 1.0 (.88–1.2) |
| Residential Security | .03 | 1.0 (.91–1.2) | −.02 | .98 (.85–1.1) | −.02 | .98 (.86–1.1) |
| Public Transit Line Nearby | .02 | 1.0 (.75–1.4) | −.04 | .96 (.69–1.3) | −.06 | .94 (.67–1.3) |
| Individual Controls | ||||||
| Age 60–69a | .06 | 1.1 (.76–1.5) | .07 | 1.1 (.76–1.5) | ||
| Age 70+ a | −.29 | .75 (.51–1.1) | −.26 | .77 (.52–1.2) | ||
| Maleb | −.47*** | .62 (.48–.81) | −.47*** | .62 (.48–.81) | ||
| Blackc | −.18 | .83 (.60–1.2) | −.16 | .85 (.61–1.2) | ||
| Hispanicc | −.25 | .78 (.53–1.2) | −.23 | .79 (.54–1.2) | ||
| Other Race/Ethnicityc | .63 | 1.9 (.87–4.1) | .68 | 1.9 (.91–4.3) | ||
| Separated/Divorcedd | −.37* | .69 (.48–.98) | −.38* | .68 (.48–.98) | ||
| Widowedd | −.52* | .60 (.38–.93) | −.53* | .60 (.38–.92) | ||
| Never Marriedd | −.39 | .68 (.44–1.1) | −.41 | .66 (.53–1.0) | ||
| Lives Alone | .31 | 1.4 (.96–1.9) | .30 | 1.3 (.95–1.9) | ||
| <HS Educatione | −.55** | .59 (.38–.87) | −.58** | .65 (.35–.8) | ||
| HS Educatione | −.11 | .90 (.65 (1.3) | −.12 | .88 (.63–1.2) | ||
| Income <$15,000f | −.63** | .53 (.35–.81) | −.64** | .53 (.35–.8) | ||
| Income $15–40,000f | −.30 | .74 (.52–1.1) | −.31 | .73 (.52–1.1) | ||
| Income missingf | −.32 | .73 (.51–1.0) | −.31 | .74 (.52–1.0) | ||
| Current Smoker | −.52** | .60 (.43–.82) | −.52** | .59 (.43–.82) | ||
| Body Mass Index | −.10 | .90 (.79–1.0) | −.11 | .90 (.79–1.0) | ||
| Number of Chronic Conditions | .10* | 1.1 (1.0–1.2) | .10* | 1.1 (1.0–1.2) | ||
| Cognitive Function | .02 | 1.0 (.99–1.1) | .02 | 1.0 (.98–1.1) | ||
| Visual Impairment | −.32*** | .73 (.61–.86) | −.21* | .82 (.67–.98) | −.21* | .81 (.66–.98) |
| Hearing Impairment | .10 | 1.1 (.94–1.3) | .10 | 1.1 (.94–1.3) | .11 | 1.1 (.94–1.3) |
| Difficulty with Mobility Activities | −.12 | .89 (.55–1.4) | −.10 | .90 (.53–1.5) | −.11 | .90 (.52–1.5) |
| Any Difficulty Walking 2–3 Blocks | −.33 | .72 (.50–1.0) | −.25 | .78 (.51–1.2) | −.25 | .78 (.51–1.2) |
| No Health Insurance | −.81*** | .44 (.29–.67) | .77*** | .46 (.30–.69) | ||
| Have Help to get to Doctor Appointments | .03 | 1.0 (.91–1.2) | .03 | 1.0 (.91–1.2) | ||
| Mediators of Heavy Traffic | ||||||
| Perceptions of Traffic Danger | .11 | 1.1 (.85–1.5) | ||||
| Perceived Noise | .04 | 1.0 (.89–1.2) | ||||
| Perceptions of Poor Air Quality | .04 | 1.0 (.87–1.2) | ||||
Reference group is no preventive health care (no cholesterol check, no blood pressure exam, and no physical exam) in past 2 years; single level model at block group level HS= high school
p<.05
p<.01
p<.001 (two-tailed tests)
Reference group is Age 45–59
Reference group is Female
Reference group is white
Reference group is married
Reference group is college degree+
Reference group is $40,000+
The third column of Table 3 adds potential mediators that could explain why heavy traffic is associated with less health care use among those with visual impairment, including individual perceptions of dangerous traffic, noise, and poor air quality (including air particles that may be bothersome for vision), but these variables did not mediate any of the association of heavy traffic on preventive health care for those with visual impairment. Predicted odds ratios are presented in Figure 2b. Adjusting for controls, the odds ratio for obtaining preventive health care among those with increasing visual impairment is 22% lower in areas with heavy traffic than the corresponding odds ratio in areas with lighter traffic volume. However, adults with visual impairment who live in areas with only light traffic (1 standard deviation below the mean) have a similar odds of obtaining preventive health care to those without any visual impairment.
Voting
The final panel of Table 1 presents the results for the logistic regression model for voting in the last mayoral or federal election (not voting is the reference group). Unlike the other two measures of participation, we found significant effects of the urban built environment at the level of the census tract and not at the more proximate block group level, indicating that characteristics in the larger spatial area are more salient for voting in this urban population. An unconditional two level logistic model indicates that 15% of the variance in voting is attributable to differences between census tract neighborhoods (intraclass correlation coefficient = .153). On average a greater proportion of streets in poor condition is associated with a higher odds of voting (second column of Table 1, lower panel), but the effect varies depending on whether one has difficulty with mobility activities (third column of Table 1). A cross-level interaction between the quality of street conditions and mobility activities indicates that the odds of voting are significantly lower among adults who have difficulty with mobility activities when they live in areas characterized by a high proportion of streets in poor condition.
The calculated effects of poor street conditions by mobility difficulty (Table 4, column 1) indicate that the odds of voting are 32 percent lower for adults who have difficulty with mobility activities when they live in areas with poor street conditions. The positive effect of poor street conditions for adults who have no difficulty with mobility activities is attenuated and no longer statistically significant after adjusting for controls (Table 4, column 2). This suggests that other individual characteristics related to both street quality and voting (e.g. age or race) may be confounding this relationship. Adjusting for controls only served to strengthen the effect of poor street conditions on voting behavior among those who have difficulty with mobility activities (adjusted OR=.51). Adding perceived physical hazards does not mediate the effect of street conditions on voting for those with mobility difficulties (final column Table 4). Predicted odds ratios are presented in Figure 2c, illustrating that the odds ratio for voting among adults with mobility difficulties is almost 60% lower for those living in tracts characterized by poor street quality than for similar adults living in areas with better street quality. The odds of voting are similar across people both with and without difficulty with mobility activities when they live in areas characterized by good street quality (one standard deviation below the mean).
Table 4.
Multilevel Logistic Regression Model for Voting1 by Difficulty with Mobility Activities and Quality of Street Conditions (Tract Level)
| Base Model | + Controls | + Mediators | ||||
|---|---|---|---|---|---|---|
| Coeff. | OR (95% CI) | Coeff. | OR (95% CI) | Coeff. | OR (95% CI) | |
| Intercept | 1.33*** | 3.8 (2.3–6.1) | 1.96** | 7.1 (1.9–11.8) | 1.97** | 7.2 (1.5–11.2) |
| Effect of Poor Street Conditions: | ||||||
| For adults with no difficulty with mobility | .28** | 1.3 (1.1–1.6) | .20 | 1.2 (.98–1.5) | .20 | 1.2 (.98–1.5) |
| For adults with mobility difficulty | −.38* | .68 (.41–1.0) | −.68** | .51 (.30–.85) | −.68** | .51 (.30–.85) |
| Other Built Environ Characteristics | ||||||
| Heavy Traffic | .17 | 1.2 (1.0–1.3) | .26* | 1.3 (1.1–1.6) | .26* | 1.3 (1.1–1.6) |
| Neighborhood Social Disorder | −.14 | .86 (.67–1.1) | −.05 | .96 (.71–1.3) | −.05 | .96 (.70–1.3) |
| Residential Security | .10 | 1.1 (.92–1.3) | .02 | 1.0 (.82–1.3) | .02 | 1.0 (.83–1.3) |
| Public Transit Line Nearby | −.36 | .70 (.44–1.1) | −.63* | .53 (.32–.91) | −.63* | .54 (.31–.92) |
| Individual Controls | ||||||
| Age 60–69a | 1.10*** | 3.0 (1.9–4.7) | 1.10*** | 3.0 (1.9–4.7) | ||
| Age 70+ a | 1.79*** | 6.0 (3.3–10.9) | 1.79*** | 6.0 (3.3–10.9) | ||
| Maleb | −.63** | .53 (.36–.79) | −.63 | .53 (.36–.79) | ||
| Blackc | 1.35*** | 3.8 (2.3–6.5) | 1.35*** | 3.8 (2.3–6.5) | ||
| Hispanicc | .06 | 1.1 (.62–1.8) | .06 | 1.1 (.62–1.8) | ||
| Other Race/Ethnicityc | −.75* | .47 (.22–1.0) | −.75* | .47 (.22–1.0) | ||
| Separated/Divorcedd | .34 | 1.4 (.84–2.4) | .34 | 1.4 (.84–2.4) | ||
| Widowedd | −.60 | .55 (.27–1.1) | −.60 | .55 (.27–1.1) | ||
| Never Marriedd | .62 | 1.9 (.93–3.7) | .62 | 1.9 (.93–3.7) | ||
| Lives Alone | .08 | 1.1 (.68–1.7) | .08 | 1.1 (.68–1.7) | ||
| <HS Educatione | −1.69*** | .18 (.10–.36) | −1.69*** | .18 (.10–.36) | ||
| HS Educatione | −.36 | .70 (.40–1.3) | −.36 | .70 (.40–1.3) | ||
| Income <$15,000f | −1.62*** | .20 (.1–..39) | −1.62*** | .20 (.1–..39) | ||
| Income $15–40,000f | −1.07*** | .34 (.19–.61) | −1.07*** | .34 (.19–.61) | ||
| Income missingf | −1.25*** | .29 (.17–.48) | −1.25*** | .29 (.17–.48) | ||
| Current Smoker | .01 | 1.0 (.64–1.6) | .01 | 1.0 (.64–1.6) | ||
| Body Mass Index | .16 | 1.2 (.98–1.4) | .16 | 1.2 (.98–1.4) | ||
| Number of Chronic Conditions | .24*** | 1.3 (1.1–1.4) | .24*** | 1.3 (1.1–1.4) | ||
| Cognitive Function | .01 | 1.0 (.95–1.1) | .01 | 1.0 (.95–1.1) | ||
| Visual Impairment | −.11 | .89 (.72–1.1) | −.09 | .91 (.69–1.2) | −.09 | .91 (.69–1.2) |
| Hearing Impairment | .19 | 1.2 (.95–1.5) | .13 | 1.2 (.87–1.5) | .13 | 1.2 (.87–1.5) |
| Difficulty with Mobility Activities | −.28 | .54 (.27–1.1) | −.79 | .45 (.20–1.0) | −.79 | .45 (.20–1.0) |
| Any Difficulty Walking 2–3 Blocks | .58 | 1.8 (.99–3.2) | −.05 | .95 (.50–1.8) | −.05 | .95 (.50–1.8) |
| Mediators of Poor Street Conditions | ||||||
| Perceived Physical Hazards | −.01 | .99 (.63–1.5) | ||||
Reference group is not voting in past mayoral or federal elections; multilevel model at tract level HS= high school
p<.05
p<.01
p<.001 (two-tailed tests)
Reference group is Age 45–59
Reference group is Female
Reference group is white
Reference group is married
Reference group is college degree or higher (16+ years of education)
Reference group is income $40,000 or higher
Discussion
In this work we extend existing research on the built environment and health (Addy et al. 2004; Berke et al. 2007; Diez Roux et al. 2007; Clarke et al. 2008; Clarke, Ailshire and Lantz 2009; Li et al. 2005; Shumway-Cook et al. 2003) by examining how characteristics in the urban environment can interact with underlying impairments and activity limitations to either promote or hinder the full participation of adults in society. We investigated participation in a large, representative sample of Chicago adults using a broad range of meaningful indicators of engagement in society, specifically interpersonal interaction, voting in government elections, and obtaining preventive health care. We also examined effects across two levels of spatial scale to identify the salience for participation of environmental characteristics in the more immediate versus the more distal neighborhood context.
One in five adults reported difficulty walking 2–3 blocks unaided, and their odds of engaging in regular interpersonal interaction was almost 50% lower than those without difficulty walking. However, residential security operated as a facilitator, increasing the odds of interpersonal interaction among adults who have difficulty walking. For people for whom it may take a little more time to walk to a friend’s or neighbor’s house, neighborhood security may be more salient, particularly in the evening hours. However, subjective measures of perceived fear and violence in one’s neighborhood did not mediate this effect suggesting that other elements of neighborhood security not captured by the measures in our data may be operating here (e.g. street lighting, police presence).
Visual impairment has received comparatively little attention in the built environment literature. Yet 36% of our sample reported some difficultly with vision, and traffic volume was inversely associated with the use of preventive health care among people with visual impairment. On the other hand, the odds of obtaining preventive health care were equivalent among those with and without visual impairment when living in areas with only light traffic. When visual impairment poses a problem for driving, adults may have to rely more on public transit for their transportation needs, and negotiating streets and traffic crossings may be particularly hazardous where there is a heavy volume of traffic. However, attempts to explain this effect through respondent’s subjective perception of traffic danger (or other hazards associated with traffic) were not successful. Built environment barriers to obtaining health care (both within and leading up to health care institutions) have been identified as a concern in the literature (Iezzoni et al. 2000; Iezzoni et al. 2002), and our work further contributes to this research by identifying heavy traffic volume as a factor associated with reduced health care use among people with visual impairment. Further work should investigate the mechanisms by which heavy traffic may operate as a barrier in this population with a view to developing strategies to promote access to health care among those with visual impairments.
Voting, as an indicator of participation in political life and citizenship, is highly meaningful in a democratic society. Yet our results indicate that barriers in the built environment may operate as obstacles for people who have difficulty moving around, and are associated with a decreased capacity to exercise their right to vote. Living in an area with streets in good condition acts as a leveler for voting behavior among those with and without difficulty with mobility activities, but residing in an area with a high proportion of streets in poor condition is associated with 60% lower odds of voting among those with underlying difficulty with mobility activities. Broken curbs and streets in disrepair are likely to be associated with more obstacles (e.g. rubble, uneven pavement) for pedestrians navigating along sidewalks and crossing streets, and are liable to be particularly problematic for those who have difficulty with mobility.
The fact that we found built environment effects operating at different levels of spatial scale (census track versus block group) underscores the importance of considering different definitions of “neighborhood” when examining the role of the built environment. Our results illustrate that interpersonal interaction and obtaining health care are more responsive to characteristics in the immediate urban environment, while characteristics in a larger geographic area are more salient for getting to a polling station.
Limitations
This study is limited to a geographically defined sample in an urban setting. Measures of impairments and activity limitations were based on self-report and we focused on a very narrow set of self-report measures of participation. We did not gather data on the mechanism by which people voted in previous elections, and environmental factors may be less relevant for those who voted by mail (e.g. absentee ballots). Measures pertain to current difficulty with an activity or current impairment, and relationships with participation may vary depending on the length of time an individual has been living with an impairment or limitation, particularly if he or she adopts strategies to minimize their influence or restructure their surroundings (Whiteneck and Dijkers 2009). A lack of data on the duration of these impairments and activity limitations may also attenuate the association with voting and obtaining health care if participation occurred prior to the onset of these limitations and impairments. Cross-sectional data preclude an understanding of the prospective association between neighborhood design and participation. However, our capacity to examine the impact of the built environment on levels of participation was considerably enhanced by using independent observational measures to capture the more detailed neighborhood characteristics that people encounter in their day-to-day lives. Further studies in other settings using the ICF as a framework would contribute to a more comprehensive understanding of the complex issues faced by people with impairments and activity limitations living in different built and social environments.
In summary, the level of participation among people with visual impairment and limitations in walking and other mobility activities varies by characteristics in the urban environment. Poor street conditions, heavy traffic, and low residential security are negatively associated with interpersonal interaction, obtaining health care, and voting in government elections. Although we were not successful in identifying mediating variables that might explain these associations, the results suggest that simple changes in urban built environments may facilitate the full participation of all persons in society. Understanding the dynamic interplay of real-world factors that influence participation is essential to understanding the broad health-related impacts of chronic disease or conditions (Jette et al. 2005). Participation is a key outcome of rehabilitation programs and of other medical and social service programs that support persons who are engaging in family, community and society to a lesser extent than they may wish (Dijkers 2010). Our results emphasize the importance of looking at the environment as one factor that can interact with a person’s underlying impairments or activity limitations to either limit or facilitate engagement in society. As argued by Whiteneck and Dijkers (2009; p. S24) “modern medicine can still not eliminate many activity limitations, but at least in theory, with the right assistive devices, personal assistance, social support, policies, and environment, people with disability can fully participate in society”.
Acknowledgments
This publication was supported by Grant Number K01EH000286-01 from the Centers for Disease Control and Prevention (CDC), and by NIH/NICHHD Grant RO1HD050467. The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of the sponsors. An earlier version of this paper was presented at the annual meeting of the American Public Health Association, Philadelphia, PA, November 9, 2009. We thank James S. House for helpful comments on the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Addy CL, Wilson DK, Kirtland KA, Ainsworth BE, Sharpe P, Kimsey D. Associations of perceived social and physical environmental supports with physical activity and walking behavior. American Journal of Public Health. 2004;94:440–443. doi: 10.2105/ajph.94.3.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andriacchi R. The Internal Medicine Perspective1. American Journal of Physical Medicine & Rehabilitation. 1997;76:17–20. doi: 10.1097/00002060-199705001-00005. [DOI] [PubMed] [Google Scholar]
- Balfour JL, Kaplan GA. Neighborhood environment and loss of physical function in older adults: Evidence from the Alameda County Study. American Journal of Epidemiology. 2002;155:507–515. doi: 10.1093/aje/155.6.507. [DOI] [PubMed] [Google Scholar]
- Berke EM, Koepsell TD, Moudon AV, Hoskins RE, Larson EB. Associations of the built environment with physical activity and obesity in older persons. American Journal of Public Health. 2007;97:486–492. doi: 10.2105/AJPH.2006.085837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chevarley FM, Thierry JM, Gill CJ, Ryerson AB, Nosek MA. Health, preventive health care, and health care access among women with disabilities in the 1994–1995 National Health Interview Survey, Supplement on Disability. Women’s Health Issues. 2006;16:297–312. doi: 10.1016/j.whi.2006.10.002. [DOI] [PubMed] [Google Scholar]
- Clarke P, Ailshire JA, Bader M, Morenoff JD, House JS. Mobility Disability and the Urban Built Environment. Am J Epidemiol. 2008;168:506–513. doi: 10.1093/aje/kwn185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P, Ailshire JA, Lantz P. Urban built environments and trajectories of mobility disability: Findings from a national sample of community-dwelling American adults (1986–2001) Social Science & Medicine. 2009;69:964–970. doi: 10.1016/j.socscimed.2009.06.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P, George LK. The role of the built environment in the Disablement Process. American Journal of Public Health. 2005;95:1933–1939. doi: 10.2105/AJPH.2004.054494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen MA, Tell EJ, Wallack SS. Client-related risk factors of nursing home entry among elderly adults. Journals of Gerontology. 1986;41:785–792. doi: 10.1093/geronj/41.6.785. [DOI] [PubMed] [Google Scholar]
- Crimmins EM. Trends in the health of the elderly. Annual Review of Public Health. 2004;25:79–98. doi: 10.1146/annurev.publhealth.25.102802.124401. [DOI] [PubMed] [Google Scholar]
- Debnam K, Harris J, Morris I, Parikh S, Shirey L. Durham County Socially Isolated Older Adults: An Action-Oriented Community Diagnosis. University of North Carolina at Chapel Hill School of Public Health, Department of Health Behavior and Health Education; 2002. [Google Scholar]
- Diez Roux AV, Evenson KR, McGill AP, Brown DG, Moore L, Brines S, Jacobs DR. Availability of recreational resources and physical activity in a sample of adults. American Journal of Public Health. 2007;97:493–499. doi: 10.2105/AJPH.2006.087734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dijkers MP. Issues in the Conceptualization and Measurement of Participation: An Overview. Archives of Physical Medicine and Rehabilitation. 2010;91:S5–S16. doi: 10.1016/j.apmr.2009.10.036. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Crimmins EM, Schoeni RF, Spillman BC, Aykan H, Kramanow E, Land K, Lubitz J, Manton KG, Martin LG, Shinbeg D, Waidmann T. Resolving inconsistencies in trends in old-age disability: report from a technical working group. Demography. 2004;41:417–441. doi: 10.1353/dem.2004.0022. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Martin LG, Schoeni RF. Recent trends in disability and functioning among older adults in the United States: A systematic review. Journal of the American Medical Association. 2002;288:3123–3146. doi: 10.1001/jama.288.24.3137. [DOI] [PubMed] [Google Scholar]
- Galea S, Tracy M. Participation Rates in Epidemiologic Studies. Annals of Epidemiology. 2007;17:643–653. doi: 10.1016/j.annepidem.2007.03.013. [DOI] [PubMed] [Google Scholar]
- Gans BM, Mann NR, Becker BE. Delivery of primary care to the physically challenged. Archives of Physical Medicine and Rehabilitation. 1993;74:S15–S19. [PubMed] [Google Scholar]
- Gill TM, Allore HG, Han L. Bathing disability and the risk of long-term admission to a nursing home. Journals of Gerontology: Biological Sciences and Medical Sciences. 2006;61A:821–825. doi: 10.1093/gerona/61.8.821. [DOI] [PubMed] [Google Scholar]
- Gray DB, Hollingsworth HH, Stark S, Morgan KA. A subjective measure of environmental facilitators and barriers to participation for people with mobility limitations. Disability and Rehabilitation. 2008;30:434–457. doi: 10.1080/09638280701625377. [DOI] [PubMed] [Google Scholar]
- Hollingsworth H, Gray DB. Structural Equation Modeling of the Relationships between Participation in Leisure Activities and Community Environments by People with Mobility Impairments. Archives of Physical Medicine and Rehabilitation. 2010;91:1174–1181. doi: 10.1016/j.apmr.2010.04.019. [DOI] [PubMed] [Google Scholar]
- Iezzoni LI, McCarthy EP, Davis RB, Siebens H. Mobility impairments and use of screening and preventive services. Am J Public Health. 2000;90:955–961. doi: 10.2105/ajph.90.6.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iezzoni LI, Davis RB, Soukup J, O’Day B. Satisfaction with quality and access to health care among people with disabling conditions. Int J Qual Health Care. 2002;14:369–381. doi: 10.1093/intqhc/14.5.369. [DOI] [PubMed] [Google Scholar]
- Jette AM, Badley E. Conceptual issues in the measurement of work disability. In: Mathiowetz N, Wunderlich GS, editors. Committee to Review the Social Security Administration’s Disability Decision Process Research. Committee on National Statistics, National Research Council, National Academies Press; 2000. [Google Scholar]
- Jette Alan M, Branch LG, Sleeper LA, Feldman HR, Sullivan LM. High-risk profiles for nursing home admission. Gerontologist. 1992;32:634–640. doi: 10.1093/geront/32.5.634. [DOI] [PubMed] [Google Scholar]
- Jette AM, Keysor J, Coster W, Ni P, Haley S. Beyond Function: Predicting Participation in a Rehabilitation Cohort. Archives of Physical Medicine and Rehabilitation. 2005;86:2087–2094. doi: 10.1016/j.apmr.2005.08.001. [DOI] [PubMed] [Google Scholar]
- Keysor JJ, Jette AM, LaValley MP, Lewis CE, Torner JC, Nevitt MC, Felson DT. Community Environmental Factors Are Associated With Disability in Older Adults With Functional Limitations: The MOST Study. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2010;65A:393–399. doi: 10.1093/gerona/glp182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F, Fisher KJ, Brownson RC, Bosworth M. Multilevel modelling of built environment characteristics related to neighbourhood walking activity in older adults. J Epidemiol Community Health. 2005;59:558–564. doi: 10.1136/jech.2004.028399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W, Keegan THM, Sternfeld B, Sidney S, Quesenberry CP, Kelsey JL. Outdoor falls among middle-aged and older adults: A neglected public health problem. American Journal of Public Health. 2006;96:1192–1200. doi: 10.2105/AJPH.2005.083055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manton KG, Gu X. Changes in the prevalence of chronic disability in the United States black and non-black population above age 65 from 1982 to 1999. Proceedings of the National Academy of Sciences. 2001;98:6354–6359. doi: 10.1073/pnas.111152298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin LG, V, Freedman A, Schoeni RF, Andreski PM. Trends in Disability and Related Chronic Conditions Among People Ages Fifty To Sixty-Four. Health Aff. 2010;29:725–731. doi: 10.1377/hlthaff.2008.0746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morenoff JD, Diez Roux AV, Hansen B, Osypuk T. Residential Environments and Obesity: How Can Observational Studies Inform Policy Interventions? In: House J, Kaplan G, Schoeni R, Pollock H, editors. Making Americans Healthier: Social and Economic Policy as Health Policy. New York: Russell Sage Foundation; 2008. pp. 309–343. [Google Scholar]
- Morland K, Wing S, Diez Roux AV. The contextual effect of the local food environment on residents’ diets. American Journal of Public Health. 2002;82:1761–1767. doi: 10.2105/ajph.92.11.1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagi S. Institute of Medicine, Disability in America: Toward a National Agenda for Prevention. Washington, D.C: National Academy Press; 1991. Disability concepts revisited: Implications for prevention. [Google Scholar]
- Nagi S. Some conceptual issues in disability and rehabilitation. In: Sussman MB, editor. Sociology and Rehabilitation. Washington, D.C: American Sociological Association; 1965. pp. 100–113. [Google Scholar]
- National Center for Health Statistics. Health, United States, 2006. Hyattsville, MD: 2006. [Google Scholar]
- Noreau L, Desrosiers J, Robichaud L, Fougeyrollas P, Rochette A, Viscogliosi C. Measuring social participation: reliability of the LIFE-H in older adults with disabilities. Disability and Rehabilitation. 2004;26:346. doi: 10.1080/09638280410001658649. [DOI] [PubMed] [Google Scholar]
- Perenboom RJM, Perenboom Measuring participation according to the International Classification of Functioning, Disability and Health (ICF) Disability and Rehabilitation. 2003;25:577. doi: 10.1080/0963828031000137081. [DOI] [PubMed] [Google Scholar]
- Ramirez A, Farmer GC, Grant D, Papachristou T. Disability and Preventive Cancer Screening: Results from the 2001 California Health Interview Survey. Am J Public Health. 2005;95:2057–2064. doi: 10.2105/AJPH.2005.066118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Heirarchical Linear Models: Applications and Data Analysis Methods. Thousand Oaks: Sage Publications; 2002. [Google Scholar]
- Raudenbush SW, Sampson RJ. Ecometrics: Toward a Science of Assessing Ecological Settings, With Application to the Systematic Social Observation of Neighborhoods. Sociological Methodology. 1999;29:1–41. [Google Scholar]
- Rimmer JH, Riley B, Wang E, Rauworth A, Jurkowski J. Physical activity participation among persons with disabilities: Barriers and facilitators. American Journal of Preventive Medicine. 2004;26:419–425. doi: 10.1016/j.amepre.2004.02.002. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW. Systematic social observation of public spaces: A new look at disorder in urban neighborhoods. American Journal of Sociology. 1999;105:603–651. [Google Scholar]
- Schootman M, Andresen EM, Wolinsky FD, Malmstron TK, Miller JP, Miller DK. Neighborhood conditions and risk of incident lower-body functional limitations among middle-aged African Americans. American Journal of Epidemiology. 2006;163:450–458. doi: 10.1093/aje/kwj054. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Merkin SS, Crimmins EM, Karlamangla AS. Disability Trends Among Older Americans: National Health and Nutrition Examination Surveys, 1988–1994 and 1999–2004. Am J Public Health. 2010;100:100–107. doi: 10.2105/AJPH.2008.157388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shumway-Cook A, Patla A, Stewart A, Ferrucci L, Ciol MA, Guralnik J. Environmental Components of Mobility Disability in Community-Living Older Persons. Journal of the American Geriatrics Society. 2003;51:393–398. doi: 10.1046/j.1532-5415.2003.51114.x. [DOI] [PubMed] [Google Scholar]
- Verbrugge LM, Jette AM. The disablement process. Social Science and Medicine. 1994;38:1–4. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Whiteneck G, Dijkers MP. Difficult to Measure Constructs: Conceptual and Methodological Issues Concerning Participation and Environmental Factors. Archives of Physical Medicine and Rehabilitation. 2009;90:S22–S35. doi: 10.1016/j.apmr.2009.06.009. [DOI] [PubMed] [Google Scholar]
- World Health Organization. International Classification of Functioning, Disability and Health. Geneva, Switzerland: 2001. [Google Scholar]
- Yang JJ, Mann WC, Nochajski S, Tomita MR. Use of assistive devices among elders with cognitive impairment: A follow-up study. Topics in Geriatric Rehabilitation. 1997;13:13–31. [Google Scholar]