Abstract
Objective
To examine gender and age differences in Attention-Deficit/Hyperactivity Disorder (ADHD) symptom endorsement in a large community-based sample.
Method
Families with four or more full siblings ascertained from Missouri birth records completed telephone interviews regarding lifetime DSM-IV ADHD symptoms and the Strengths and Weaknesses of ADHD-Symptoms and Normal-behavior (SWAN) questionnaire for current ADHD symptoms. Complete data were available for 9380 subjects aged 7 to 29 years. Lifetime and current DSM-IV-like ADHD diagnoses were assigned by the DSM-IV symptom criterion. Linear regression was used to examine sex and age effects on SWAN ADHD symptom scores. Logistic regression was used to examine sex and age effects on specific ADHD diagnoses. Fractional polynomial graphs were used to examine ADHD symptom count variations across age.
Results
Overall prevalence of current DSM-IV-like ADHD was 9.2% with a male:female ratio of 2.28:1. The prevalence of DSM-IV-like ADHD was highest in children. Gender differences in DSM-IV-like ADHD subtype prevalences were highest in adolescents. On average, individuals with lifetime DSM-IV-like ADHD diagnoses had elevated current ADHD symptoms even as adolescents or adults.
Conclusions
Lower male:female ratios than reported in some clinic-based studies suggest that females are under-diagnosed in the community. Although they may no longer meet the full symptom criterion, young adults with a history of lifetime DSM-IV-like ADHD maintain higher levels of ADHD symptoms compared to the general population. The use of age-specific diagnostic criteria should be considered for DSM-V and ICD-11.
Keywords: ADHD, prevalence, subtypes, sex differences, adult
Introduction
Attention-Deficit/Hyperactivity Disorder (ADHD) is one of the most common neurodevelopmental disorders in the pediatric population.1 Though one of the most researched psychiatric disorders in childhood, its prevalence in the population remains controversial. Early reports from the community-based Great Smoky Mountains Study estimated a relatively low ADHD prevalence, in the range of 1–2% for children 9 to 13 years old.2 DSM-IV-TR estimates prevalence at 3–7% in school aged children,1 the CDC at 7.8% among children aged 4–17 years,3 while other reports cite prevalence estimates ranging from 2–18% in community samples. 4–6 This variability may be due to methodological issues, such as differences in diagnostic criteria, sample ascertainment, developmental stages, tools of assessment, and rater bias. Some recent population-based studies that do not use DSM-IV criteria have reported prevalence of ADHD either close to DSM-IV estimates 7 or much higher.8 In a recent review, Rowland and colleagues conclude that lack of large population-based epidemiologic studies limits the understanding of this disorder and that further studies are needed to ascertain the true prevalence of ADHD in the community.9
As in children, prevalence estimates for adult ADHD are controversial. The prevalence of ADHD in adults is estimated at 2–7%, and 4% is generally accepted. 10, 11 Faraone and colleagues estimate that the prevalence of adult ADHD at age 25 ranges from 1.2% for full threshold DSM-IV diagnosis, to 3.2% for partial remission cases. 12 Some researchers argue that the DSM is not sufficiently sensitive to developmental variations in symptom expression, making it difficult for ADHD children to meet criteria as they age.13, 14 In addition, a recent longitudinal study of ADHD in twins 15 finds that the five year stability of DSM-IV based ADHD subtypes is poor, changing with the transitions from childhood to adolescence and from adolescence to adulthood. The authors emphasize the need for age-specific diagnostic criteria for ADHD subtypes.
In addition to age differences, there are clear gender differences with respect to the prevalence of ADHD, its subtypes, and endorsement of specific DSM-IV ADHD symptoms. Males are generally more likely to be diagnosed with ADHD than females, with a male to female ratio of approximately 4:1 in community samples.16 In the DSM-IV field trials, the sex ratio varied across subtypes.17 Studies exploring gender differences in prevalence and characteristics of ADHD provide inconsistent findings depending on the type of sample used.18–20 Gaub and Carlson suggest ascertainment in clinic settings may mask gender differences, because females in such settings are underrepresented and severely affected due to referral bias.20 Another review recommended a stronger focus on females in ADHD research, and more attention to ADHD subtypes in the study of gender differences.21 In a population-based Australian sample, Graetz and colleagues found the male:female prevalence ratio did not differ across ADHD subtypes, but there were gender differences in co-occurring problems and symptom-specific impairment.8 In contrast, Biederman and colleagues’ small study of non-referred subjects with ADHD (siblings of ADHD probands) did not reveal any gender differences in impairment, psychiatric comorbidity, or ADHD subtypes. 22
Previous work thus supports the importance of large population-based studies to ascertain the prevalence of ADHD symptoms and diagnoses in the community, and to aid in the definition of possible age- and gender-specific diagnostic criteria. The present study investigates the prevalence of ADHD symptoms and DSM-IV symptom-criterion-based diagnoses in a large, non-referred, community-based sample, taking age and gender into account. Because we are not requiring the DSM-IV age-of-onset and impairment criteria for our current DSM-IV-like ADHD diagnoses, we expect our reported prevalences to be somewhat higher than the prevalence of pure DSM-IV ADHD. However, our large, community-based sample allows us to examine the relative prevalence of DSM-IV-like ADHD diagnoses for non-referred individuals within various sex and age groups.
Method
This paper examines age and gender effects on lifetime DSM-IV-like ADHD prevalence (from telephone screening interviews of parents), and current DSM-IV-like ADHD prevalence (parent-report questionnaire). The study protocol was approved by the Washington University Human Studies Committee, and all respondent parents provided informed consent.
As a part of a molecular epidemiology study of inattentive ADHD, we ascertained a representative sample of families from Missouri birth records, each with four or more full siblings age seven years and older and at least two siblings aged seven to 17 years. Assessment of the families consisted of a telephone screener interview where trained interviewers asked the best informant parent (usually the mother) about lifetime impairment at home and school from the 18 ADHD symptoms for each sibling in the family, followed by mailed questionnaires. Research staff conducting the screening interviews had a minimum of a bachelor’s degree in psychology or a related field and underwent about 80 hours of training. A later stage of the study required collection of DNA samples from both parents. Thus, families were excluded if one of the biological parents was unavailable (i.e., deceased (n=301) or in prison (n=54)). Families were also excluded if the family was known to have twins or if neither parent understood enough English to complete the screener interview. Individual children were excluded if adopted, not a full sibling, in prison, or deceased. The protocol did not allow interviewers to specifically ask about the presence of medical diagnoses, but individual children were excluded if the parent volunteered information that a child had mental retardation, autism, Down’s syndrome, a major medical illness, or major hearing impairment (n=202 for all sibling exclusions).
Out of 11,925 families contacted, 3,422 families refused to participate, 2,227 families were ineligible and 5,276 families completed the screener. Demographic data and socioeconomic status variables (based on the 2000 U.S. census data for postal zip codes) were available for a subset of study responders and refusers (Supplement 1).
For the current analyses, we used data from the parent-report screening interview (for lifetime ADHD symptoms) and Strengths and Weaknesses of ADHD-symptoms and Normal-behavior (SWAN) questionnaires (current ADHD symptoms) on offspring aged 7–29 years. Parents who completed the telephone screening on their children were asked to complete the SWAN questionnaires by mail. The interview questions regarding lifetime DSM-IV ADHD symptoms were derived from the ADHD section of the Missouri Assessment of Genetics Interview for Children (MAGIC), which has excellent inter-rater reliability for DSM-IV ADHD diagnoses.23 Each lifetime symptom was counted as positive only if it caused impairment at home or school. The SWAN was used to collect parental reports quantifying expression of the child’s 18 DSM-IV ADHD symptoms within the past month. The SWAN contains 18 reworded items based on the SNAP rating scale. The items are rated on a seven-point scale (−3 to +3). Positive scores indicate parental report of worse than average ADHD symptoms, whereas negative scores indicate better than average behavior.24 Compared to other ADHD assessments, the SWAN scale provides a more continuous distribution due to its seven-point rating range.24–26 From the 5,276 families who completed the screener, there were 22,581 individuals with complete data on sex, age at screener, and screener ADHD items. Of those, 9,445 subjects had complete age, screener and SWAN data. There was a time gap of only a few months between the screener interview and the SWAN, but because the exact age at time of assessment seems more critical for current than lifetime symptoms, SWAN age was used for the main analyses. The total sample included very few individuals under age 7 or over age 29, so we limited our main analyses to individuals aged seven to 29 years at the time of the SWAN.
The current main analysis of differences in prevalence of ADHD symptoms and DSM-IV-like ADHD diagnoses as a function of age and gender includes 9380 subjects with complete demographic, SWAN and screener data and aged seven to 29 years at the time of SWAN questionnaire. For comparison purposes, we also analyzed the demographic characteristics and lifetime DSM-IV-like ADHD subtype prevalence for the 22,356 individuals with complete screener data who were aged seven to 29 years at the time of the screening interview. Demographic characteristics of the larger sample with screener data and the final study sample with both SWAN and screener data are displayed in Supplement 2. The overall sample consists of an approximately equal number of males and females. The final study sample was 97.93% Caucasian, 1.54% African-American, and 0.53% others (as determined from birth record data).
Data Analysis
The sample was divided by age into three subgroups – children (7–12 years), adolescents (13–17 years) and young adults (18–29 years). Given the biological changes that occur during puberty, it is sensible to examine adolescents separately from children and young adults. All SWAN item scores were averaged to obtain a total ADHD symptoms score. We also calculated average inattention (items 1–9) and average hyperactive-impulsive (items 10–18) scores. These scores serve as continuous measures of ADHD severity, but do not directly allow identification of discrete ADHD diagnostic categories by DSM-IV criteria. This requires the use of a specific cut-off to determine whether a symptom is considered positive. On a seven-point scale (−3 to +3) of the SWAN, we considered a score of 1 or higher to be positive (present). This cut-off reflects the fact that, on average, parents rate their children as having above-average behavior (negative score), rather than “average” behavior (zero). Mean scores on individual SWAN items ranged between −0.54 and −1.15. For each item, the 50th percentile was at either 0 or −1 (usually −1), and the 75th percentile was at 0. Item scores of 1 (“slightly below average”) were between the 90th and 95th percentile (most often at 95th), and scores of 2 (“below average”) were between the 95th and 99th percentile (most often at 99th). Young and colleagues also suggest use of a SWAN item cutoff indicating “slightly below” average or worse behavior, 27 which is equivalent to our cutoff of 1 or higher. To obtain current DSM-IV-like ADHD subtype diagnoses, we applied the DSM-IV symptom criterion to symptom counts derived from the SWAN. Similarly, we used the 18 binary lifetime ADHD symptom items (from MAGIC-based telephone screener) to determine lifetime DSM-IV-like ADHD diagnoses.
We calculated the prevalence of each DSM-IV-like ADHD subtype and male to female prevalence ratios for each age group. Differences in the quantitative subscale scores were analyzed across sex and age group using one-way ANOVA. Within each of the three age groups, linear regression analyses were done to examine the effects of sex and age on each quantitative SWAN score, and logistic regressions were performed to examine the effects of sex and age on current and lifetime DSM-IV-like ADHD diagnoses. For all regression analyses, we adjusted the standard errors for family clustering of data. Finally, we used fractional polynomial regression 28 graphs to examine how current mean ADHD symptom counts vary with age for males and females with various lifetime ADHD subtypes. Statistical analyses were carried out using SAS version 9.1 (SAS Institute, Cary, NC) and STATA version 9.2 (College Station, TX).
Results
The overall prevalence of current DSM-IV-like ADHD (any subtype) is estimated to be 9.2% (11.7% in children, 9.7% in adolescents and 6.4% in adults). DSM-IV-like predominantly inattentive ADHD emerged as the most prevalent current and lifetime diagnostic subtype for each age group, followed by combined type. Lifetime prevalences were similar for the total screener sample (n=22,356) compared to the screener plus SWAN subsample (n=9380) in each of the three age groups. Table S3 presents current and lifetime prevalences of the DSM-IV-like ADHD subtypes in children, adolescents and young adults based on the SWAN and screener interview respectively (Supplement 3).
The prevalences of current inattentive and combined DSM-IV-like ADHD subtypes were significantly higher in males than females within each age group (Table 1). However, for the hyperactive-impulsive DSM-IV-like ADHD subtype, the difference was statistically significant only in children. The ratios of DSM-IV-like inattentive and combined type ADHD prevalences in males versus females fell approximately between 2:1 and 3:1 and were highest in adolescents. For the predominantly hyperactive-impulsive subtype, the male: female ratio was about 2:1 in children, but was lower in adolescents and adults.
Table 1.
Gender differences in current DSM-IV-like ADHD subtype prevalence
| ADHD subtype** | Males | Prevalence in Males (%) | Females | Prevalence in Females (%) | M:F ratio | χ2 | p |
|---|---|---|---|---|---|---|---|
| Overall samplea | |||||||
| Overall ADHD | 606 | 12.58 | 252 | 5.52 | 2.28:1 | 140.60 | <0.0001 |
| Inattentive | 405 | 8.41 | 174 | 3.81 | 2.21:1 | 85.40 | <0.0001 |
| Hyperactive-Impulsive | 70 | 1.45 | 35 | 0.77 | 1.88:1 | 9.97 | 0.0016 |
| Combined | 131 | 2.72 | 43 | 0.94 | 2.89:1 | 40.65 | <0.0001 |
|
| |||||||
| Childrenb | |||||||
| Overall ADHD | 217 | 15.69 | 99 | 7.49 | 2.09:1 | 43.97 | <0.0001 |
| Inattentive | 133 | 9.62 | 64 | 4.84 | 1.99:1 | 22.77 | <0.0001 |
| Hyperactive-Impulsive | 35 | 2.53 | 16 | 1.21 | 2.09:1 | 6.53 | 0.011 |
| Combined | 49 | 3.54 | 19 | 1.44 | 2.46:1 | 12.20 | 0.0005 |
|
| |||||||
| Adolescentsc | |||||||
| Overall ADHD | 249 | 13.75 | 90 | 5.38 | 2.56:1 | 69.26 | <0.0001 |
| Inattentive | 177 | 9.77 | 66 | 3.95 | 2.47:1 | 45.47 | <0.0001 |
| Hyperactive-Impulsive | 21 | 1.16 | 11 | 0.66 | 1.76:1 | 2.40 | 0.12 |
| Combined | 51 | 2.82 | 13 | 0.78 | 3.62:1 | 20.03 | <0.0001 |
|
| |||||||
| Adultsd | |||||||
| Overall ADHD | 140 | 8.63 | 63 | 4.01 | 2.15:1 | 28.62 | <0.0001 |
| Inattentive | 95 | 5.86 | 44 | 2.80 | 2.09:1 | 17.90 | <0.0001 |
| Hyperactive-Impulsive | 14 | 0.86 | 8 | 0.51 | 1.69:1 | 1.46 | 0.22 |
| Combined | 31 | 1.91 | 11 | 0.70 | 2.73:1 | 9.01 | 0.002 |
Note: Statistically significant p-values (<0.05) are shown in bold.
Current DSM-IV-like ADHD subtypes based on the Strengths and Weaknesses of ADHD-symptoms and Normal-behavior scale (SWAN).
Overall sample – Subjects in age-range of 7–29.99 years (total=9380, males = 4816, females =4564 )
Children - Subjects in age-range of 7 to 12.99 years (total=2704, males =1383, females =1321 )
Adolescents - Subjects in age-range of 13 to 17.99 years (total=3483, males =1811, females =1672 )
Adults - Subjects in age-range of 18 to 29.99 years (total=3193, males=1622, females=1571)
Mean quantitative SWAN subscale scores varied by age group and sex, with statistically significant higher scores in males and in subjects with younger age for total, inattentive and hyperactive/impulsive scales (Supplement 4).
In children, adolescents and adults, linear regression analyses showed that the quantitative hyperactive-impulsive, inattentive, and total SWAN scores (created by averaging the appropriate SWAN items) were significantly higher in males compared to females, and tended to decrease with older age. The effect of age on mean total and hyperactive-impulsive SWAN scores was significant in children and adolescents but not in adults. In contrast, the effect of age on the SWAN inattentive subscore was significant only in adults (Supplement 5).
Logistic regression analyses, controlling for age and familial clustering, indicate higher likelihood of current DSM-IV-like ADHD subtype diagnoses in males compared to females. However, the gender effect was not statistically significant for the hyperactive-impulsive subtype in adolescents or adults. The odds ratio indicating the effect of male gender on DSM-IV-like ADHD subtype diagnosis was highest for combined type ADHD. A similar pattern of male predominance was seen with the lifetime diagnosis of DSM-IV-like ADHD based on screener items in children, adolescents and adults (Supplement 5).
When all DSM-IV-like ADHD subtypes were considered together, age did not have a statistically significant effect on current DSM-IV-like ADHD diagnosis among children or adolescents, but younger age was associated with current ADHD diagnosis in adults. Also, age sometimes had a significant effect on the likelihood of a specific DSM-IV-like ADHD subtype for individuals in a particular age group. For example, older age was significantly associated with current inattentive subtype diagnosis in children, while younger age was associated with current inattentive subtype diagnosis in adults. Also, younger age was associated with current combined subtype in adolescents. Older age at screener was a significant predictor of screener-based lifetime DSM-IV-like ADHD diagnosis in children, and younger age at screener was a significant predictor of screener-based lifetime DSM-IV-like ADHD diagnosis in adults (supplemental digital content, table S5). Of note, one might expect prevalence of parent-reported lifetime diagnosis to continue increasing with age since there is more chance of exhibiting a lifetime symptom the longer a subject has been alive. However, a decrease in parent-reported lifetime prevalence with increasing age might be observed in adults if the parents are more likely to forget about their adult children’s past symptoms over time.
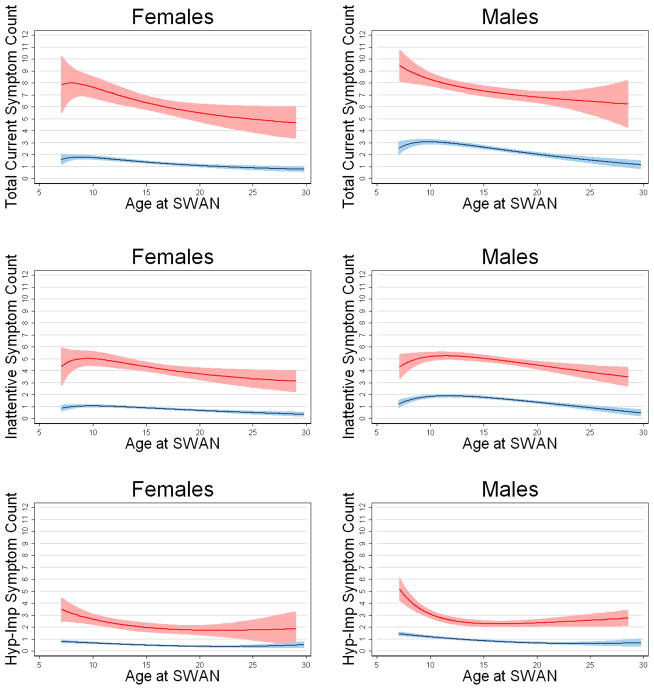
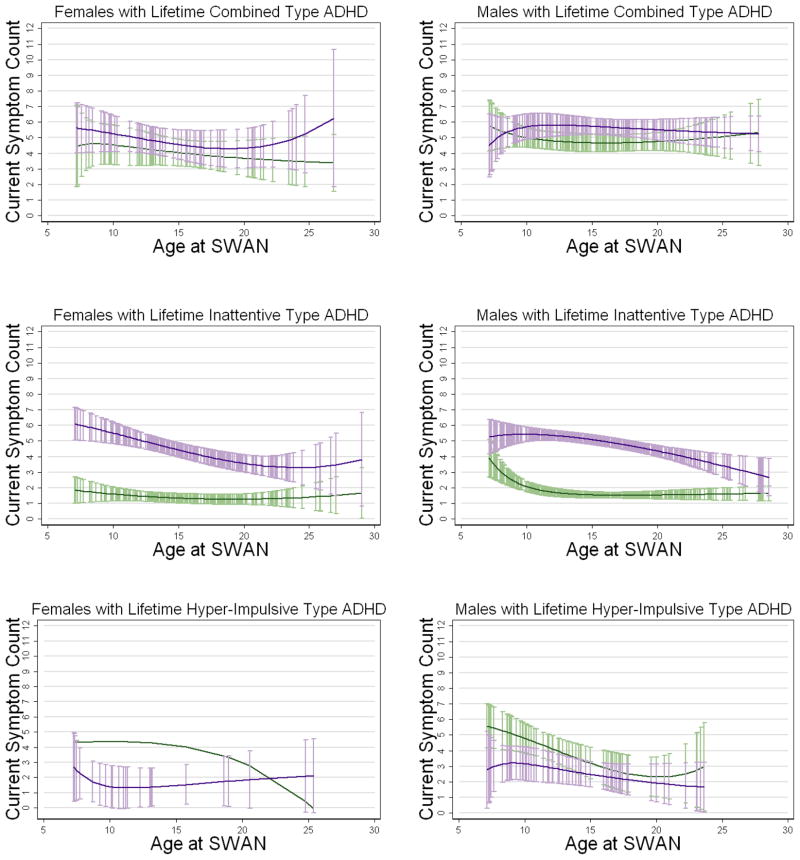
The above linear and logistic regression analyses illustrate how the effect of age on ADHD symptoms and subtypes is not identical within each of the three age groups in this sample. This suggests the effect of age is not linear across development from childhood to young adulthood. Fractional polynomial regression allows us to fit a curve rather than a straight line, so this method is very appropriate when examining the variation in ADHD symptom counts across the entire age range. Figure 1 shows the estimated mean current (SWAN-based) symptom counts by sex and across the age range for all male or female subjects together and for subjects with lifetime DSM-IV-like ADHD diagnoses (screener-based). Although symptom counts are lower at older ages, even older individuals with a lifetime DSM-IV-like ADHD diagnosis have markedly higher current ADHD symptoms than the total sample. Figure 2 shows estimated mean current (SWAN-based) inattentive and hyperactive-impulsive symptom counts by sex and across the age range for individuals with each lifetime (screener-based) DSM-IV-like ADHD subtype. Symptoms appear more persistent across age in subjects with a lifetime diagnosis of DSM-IV-like combined type ADHD compared to other subtypes. Although SWAN-based current symptom counts are clearly elevated for individuals with screener-based lifetime DSM-IV-like ADHD diagnoses, the average individual with a lifetime diagnosis will not meet SWAN-based current ADHD criteria due to falling below the DSM-IV requirement of 6 symptoms in one category.
Figure 1.
Fractional polynomial regression graphs showing estimated current total, inattentive, and hyperactive-impulsive mean ADHD symptom counts by sex and across age for subjects with a lifetime DSM-IV-like ADHD diagnosis (red line) and for total male or female sample (blue line). Current ADHD symptom counts are based on number of items rated 1 or higher on the parent-rated SWAN questionnaire, which asks about symptoms over the past month. Lifetime DSM-IV-like ADHD diagnosis is based on parent responses to questions asking whether their child ever had impairment at home or school from each of the DSM-IV ADHD symptoms. Shaded regions indicate 95% confidence intervals.
Figure 2.
Fractional polynomial graphs showing estimated inattentive (purple line) and hyperactive-impulsive (green line) mean current symptom counts by sex and across age for individuals with a lifetime DSM-IV-like diagnosis of combined, inattentive, or hyperactive-impulsive type ADHD. Current ADHD symptom counts are based on number of items rated 1 or higher on the parent-rated SWAN (Strengths and Weaknesses of ADHD-Symptoms and Normal-behavior) questionnaire, which asks about symptoms over the past month. Lifetime DSM-IV-like ADHD diagnosis is based on parent responses to questions asking whether their child ever had impairment at home or school from each of the DSM-IV ADHD symptoms. Purple and green capped vertical spikes indicate 95% confidence intervals for inattentive symptom count and hyperactive-impulsive symptom count, respectively. The confidence interval for mean hyperactive-impulsive symptom count is not shown in the lower left panel because it interfered with scaling of the graph (confidence interval went below zero at the upper age range).
Discussion
By applying the DSM-IV symptom criterion to dichotomized parent responses on the SWAN, this study estimates prevalence of DSM-IV-like ADHD subtypes in male and female children, adolescents, and young adults in a large community sample. Strengths of this study include the wide age range and large sample size, which provide enough power to examine gender and age differences in great detail. Since our data were selected from the community, they overcome some important limitations of previous studies using clinical samples. However, we cannot report the prevalence of meeting full DSM-IV criteria (due to absence of age-of-onset and impairment data).
In our entire sample of seven to 29 year-old subjects, we found an overall current (SWAN-based) DSM-IV-like ADHD prevalence of 9.2%. This is somewhat higher than the prevalence of 3 to 7% reported in the DSM-IV-TR for school-aged children, even though our total sample includes young adults, who are less likely to be affected than school-aged children. Our prevalence estimates for male (15.7%) and female (7.5%) children aged 7–12 years are slightly lower than those reported in a recent Australian study of 6–13 year old children (18.7% and 8.4%, respectively), 8 and somewhat higher than those from a recent U.S. study of 8–15 year old children (11.8% and 5.4%, respectively).29 The disagreement may be partly due to differences in the age range of study subjects and differences in the diagnostic instruments used. We found the prevalence of DSM-IV-like ADHD was highest in children (11.7%) followed by adolescents (9.7%) and lowest in adults (6.4%). This decrease in prevalence with age is in agreement with many other studies and supports the hypothesis that ADHD symptoms decrease with brain maturation. The findings, however, are also compatible with a lack of age-appropriate symptom criteria for adolescents and adults and with lack of age-adjusted concepts of illness.
We found the overall DSM-IV-like ADHD prevalence ratio for males versus females to be 2.28:1, lower than the usually accepted estimate of 4:1. The ratio was highest for adolescents (2.56:1). Since we used a population-based sample, our results are not subject to clinical referral bias that can lead to under representation of females, and our male:female prevalence ratio is likely more accurate that those obtained from clinical samples. Even though the overall prevalence of DSM-IV-like ADHD decreases with age, the ratio between males and females remains relatively stable. The lower prevalence in females may thus be the result of higher liability toward ADHD in boys than girls,20 the expression of different genes for ADHD in boys versus girls,30 or the requirement of a higher threshold in girls for the level of liability to manifest ADHD as explained by the polygenic multiple threshold model.31 Alternatively, parents may notice more symptoms in males, who tend to have higher levels of disruptive hyperactive-impulsive symptoms.
In our sample, the inattentive subtype of DSM-IV-like ADHD was the most common subtype in both males and females, as found in recent community studies, 8, 18, 29 but not in some clinic-based studies, where the combined subtype is most common.22 It is thus possible that the increased morbidity associated with the combined subtype is responsible for referral bias in clinic-based studies. In addition to producing overestimates of the relative prevalence of combined versus inattentive type ADHD, such referral bias may result in biased estimates of gender differences in the proportion of children with a particular subtype of ADHD. Similar to the DSM-IV field trials,17 we found male:female ratios for children aged 7 to 12 were highest for the combined type, intermediate for the hyperactive-impulsive type, and lowest for the inattentive type. We found the sex differences in inattentive and combined type DSM-IV-like ADHD prevalence were higher in adolescents compared to children and adults. In contrast, the sex ratio for hyperactive-impulsive DSM-IV-like ADHD was highest in children.
In addition to considering DSM-IV-like ADHD subtype prevalences for different sex and age groups, our study also used quantitative measures of DSM-IV ADHD symptoms (SWAN subscale scores and SWAN-based symptom counts). Quantitative SWAN subscale scores (total, inattentive and hyperactive-impulsive) were highest in children and lowest in adults and significantly different across age groups. This supports the consensus that symptoms improve with age. Significantly higher mean subscale scores in males across all age groups suggest the presence of more severe symptoms in males than females.
Figures 1 and 2 illustrate the important finding that symptom counts vary with age in both males and females. Such changes in symptom counts over time are also consistent with the temporal instability of ADHD subtype diagnoses as shown in longitudinal studies.15, 32 Despite having met criteria for DSM-IV-like ADHD at some point in their life, subjects with lifetime DSM-IV-like ADHD do not, on average, have a high enough symptom count to meet criteria for a current diagnosis. However they continue to have significantly elevated symptom counts compared to the total sample. Adults with lifetime DSM-IV-like ADHD may not meet full criteria for DSM-IV ADHD, but appear to have persistent symptoms which may be clinically significant. Our data are consistent with longitudinal studies of ADHD such as the MTA study, which showed persistence of elevated ADHD symptoms during several years of follow-up.33
This study has some limitations. Although we used the DSM-IV ADHD symptom criterion for diagnosis of ADHD and subtypes, we did not apply the age of onset criterion (impairing symptoms before age 7). However, the age-of-onset criterion has questionable validity.34, 35 Parents report later ages of onset when interviewed again after 5 years, leading to the under-diagnosis of ADHD in older age groups.34 Also, we relied only on parent reports of ADHD symptoms, with possible bias related to single informant. However, parent reports of current ADHD symptoms in their child are very reliable36 and are less likely to be subject to treatment effects than teacher reports. Our most important limitation is that we did not require impairment in multiple settings when assigning current or lifetime diagnoses. Screener items were not considered positive unless impairment was present in at least one setting (home or school), and, to some degree, “below average” ratings for current ADHD symptom descriptions on the SWAN may imply impairment relative to peers, but we did not have an acceptable measure of current impairment. Thus, it is not surprising that our prevalence estimates are somewhat inflated compared to studies that follow strict DSM-IV impairment and age of onset criteria.
The cutoff we used to indicate symptom presence for individual SWAN items was based on the item score distributions (at the 95th percentile for the majority of items). In further support of our SWAN item cutoff, a recent study examining psychometrics of the SWAN used the same cutoff (slightly below average) to indicate symptom presence.27 Clearly, the proportion of subjects meeting criteria will vary depending on the cutoff used. A cutoff of 2 may seem more consistent with those (between 2.00 and 2.48) suggested for teacher-rated SWAN continuous summary scores by Swanson and colleagues,24 who acknowledge these cutoffs identified less than their expected 5% extreme cases for combined, inattentive, and hyperactive-impulsive ADHD symptoms. If a stricter cutoff of 2 is used in our sample, the resulting estimates are much lower than those reported in most studies of ADHD prevalence (2.74 % for children, 2.81% for adolescents, and 2.16% for adults).
In a supplementary analysis to further assess the effect of using a cutoff of 1 vs. 2 on SWAN items, we examined the agreement between the lifetime (screener-based) and current (SWAN-based) diagnosis for the 7 and 8 year-olds in our sample (n=775). In this young age range we expected most children with lifetime DSM-IV-like ADHD should meet criteria for current DSM-IV-like ADHD. When the SWAN item cutoff of 1 was used for the 775 children in this age range, the lifetime DSM-IV-like ADHD prevalence according the screener was exactly equal to current prevalence based on SWAN (83 individuals, 10.7%); however, the telephone screener and SWAN did not always identify the same individuals as affected (48 met both lifetime and current criteria, 35 met only lifetime criteria, 35 met only current criteria), so agreement between the lifetime and current diagnoses was only poor to moderate (kappa= 0.53 for presence of DSM-IV-like ADHD overall; kappas of 0.43, 0.33, and 0.56 for inattentive, hyperactive-impulsive, and combined subtypes, respectively). Reasons for poor agreement between lifetime and current DSM-IV-like ADHD diagnoses despite the equivalent prevalence estimates could include treatment effects, changes in symptoms that naturally occur in this age range (such as increase in observed inattentive symptoms as academic demands increase and developmental decrease in hyperactive-impulsive symptoms), and differences in parent responses based on the way questions are asked in the screener (questions about presence of ADHD symptoms that cause problems at home and/or school) versus the SWAN (more positive wording with option to rate child anywhere from far above to far below average on each symptom item). If the higher SWAN cutoff of 2 was used, fewer of the 7–8 year-old children with lifetime DSM-IV-like ADHD met criteria for current DSM-IV-like ADHD according to the SWAN, so agreement was worse (kappa=0.26 for ADHD overall; kappas of 0.07, 0.26, and 0.07 for inattentive, hyperactive-impulsive, and combined types, respectively).
Ideally, we would also have liked to determine if the cutoff of 1 for symptom presence on the SWAN identifies individuals with significant impairment. Although we do not have a good measure of current impairment, each lifetime ADHD symptom was only coded as present if the parent reported a history of impairment at home and/or school from that individual symptom. So, we have examined the number of lifetime impairing symptoms for individuals meeting our criteria for current DSM-IV-like ADHD (using a SWAN cutoff of 1 to indicate current ADHD symptom presence). On average, individuals with no current DSM-IV-like ADHD diagnosis had 1.4 ± 2.8 lifetime impairing symptoms. Those meeting our DSM-IV-like criteria for current inattentive, hyperactive-impulsive, and combined type ADHD had mean lifetime impairing symptom counts of 7.9 ± 4.3, 8.0 ± 5.6, and 11.6 ± 5.3, respectively. Thus, we conclude that individuals identified on the basis of SWAN scores of 1 or greater are likely to be substantially impaired by their symptoms.
We separated child and adolescent groups at age 13 partly because of differences in symptoms that may occur during puberty, but we did not include any direct measures of pubertal development, so we cannot determine whether changes in ADHD symptoms correspond to a particular stage of puberty. In the case of depression, 13 is the approximate age where depression becomes more common in females, and pubertal development has been hypothesized to account for this change in the sex ratio for depression. 37 Based on what we know about depression, age 13 is a reasonable guess regarding the age at which puberty may influence a change in ADHD symptoms.
Parents were not asked about medication use for ADHD, which may have resulted in misclassification of some affected subjects who had fewer symptoms due to medication treatment. However, if parents volunteered that their child was taking medication, they were asked to answer screener questions based on their child’s behavior when not taking the medication (there were no such instructions on the SWAN questionnaire). The difference in these instructions for lifetime versus current ADHD symptoms may have contributed to poor agreement between the measures as described above.
The response rate for the SWAN was lower than that of the screener instrument. However, whether we used all screener subjects, or screener plus SWAN subjects, lifetime prevalence rates (based on the screener) were similar.
The families in our study were comparatively larger than the current average family size in the United States, and families in which either parent would be unavailable to provide DNA(i.e., one parent deceased or incarcerated) were excluded. Also, our sample was primarily Caucasian. These issues may limit the generalizability of our results.
The study protocol did not allow interviewers to ask whether the diagnoses of other psychiatric or major medical illnesses were present. Because we did not examine psychiatric comorbidity, the overlap of symptoms between ADHD and other diagnoses (such as mood and anxiety disorders) could lead to some diagnostic misclassification. Study subjects were not seen in-person or directly assessed by a clinician during the screening phase of this study, which further limits the ability to make clinical diagnoses. However, detailed in-person assessment on a subset of this sample is underway.
This study has some important implications for diagnostic nosology. Our findings suggest lower male:female ratios in ADHD diagnoses than previous clinic-based studies. This result is consistent with multiple epidemiological studies.3,7,29 The inattentive subtype emerged as the most prevalent subtype in our study as compared to combined subtype in some clinic-based studies. This implies that females and the inattentive subtype are under-diagnosed and/or under-treated in the community. This represents an important disparity in the delivery of health care to a substantial proportion of affected individuals.
Our results also underscore the need to include the expected severity and number of symptoms based on a patient’s age in a clinical diagnosis of ADHD. Although DSM-IV-TR does instruct clinicians to consider age-appropriateness of symptoms when determining symptom presence vs. absence, this may not adequately address the issue of changes in symptom presentation with age. A lower symptom count cut-off may be appropriate when diagnosing ADHD symptoms in adolescents or adults.
We suggest the development of a nomogram-based approach to determine the possible presence of ADHD based on age norms for the 18 DSM-IV ADHD symptoms. As for height, weight or body mass index (BMI) charts, such a screening approach is straightforward, easy to implement during an office visit and unlikely to miss the “true cases”. We acknowledge that selection of an exact percentile cutoff for “abnormal” ADHD symptom counts (or continuous symptom scores) is necessarily arbitrary because such cutoffs will not perfectly separate those with impairment from those without. So, while nomograms can be used to determine whether someone has a higher number of symptoms (or more severe symptoms) than expected in the population, the presence of functional impairment still needs to be considered when making a diagnosis and deciding whether treatment is indicated. Using the current DSM-IV symptoms as the basis for a nomogram-based approach would avoid the issues of what are appropriate “adult” ADHD symptoms and focus on core concepts of deficits which interfere with functioning across the life span.
Supplementary Material
Acknowledgments
This work was supported by award numbers R01-MH-067921 (PI-RDT), R01-MH-083823 (PI-AAT), and K08-MH-080287(PI-AMR) from the National Institute of Mental Health (NIMH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH or the National Institutes of Health.
Footnotes
This paper is dedicated to the senior author, Dr. Richard Todd, who died from complications of leukemia on August 22, 2008. Dr. Todd was principal investigator on the study described here. He was heavily involved in supervising the data analysis and writing of this paper, even until a few days before his death. Dr. Todd was a brilliant scientist, an excellent mentor, and a highly valued colleague.
Disclosure: Drs. Ramtekkar, Reiersen, Todorov, and Todd report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.APA. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 2.Costello EJ, Farmer EM, Angold A, Burns BJ, Erkanli A. Psychiatric disorders among American Indian and white youth in Appalachia: the Great Smoky Mountains Study. Am J Public Health. 1997;87:827–832. doi: 10.2105/ajph.87.5.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CDC. Mental Health in the United States: Prevalence of Diagnosis and Medication Treatment for Attention-Deficit/Hyperactivity Disorder --- United States, 2003. CDC MMWR. 2005;34:842–847. [PubMed] [Google Scholar]
- 4.Brown RT, Freeman WS, Perrin JM, et al. Prevalence and assessment of attention-deficit/hyperactivity disorder in primary care settings. Pediatrics. 2001;107:E43. doi: 10.1542/peds.107.3.e43. [DOI] [PubMed] [Google Scholar]
- 5.Elia J, Ambrosini PJ, Rapoport JL. Treatment of attention-deficit-hyperactivity disorder. N Engl J Med. 1999;340:780–788. doi: 10.1056/NEJM199903113401007. [DOI] [PubMed] [Google Scholar]
- 6.Goldman LS, Genel M, Bezman RJ, Slanetz PJ. Diagnosis and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Council on Scientific Affairs, American Medical Association. JAMA. 1998;279:1100–1107. doi: 10.1001/jama.279.14.1100. [DOI] [PubMed] [Google Scholar]
- 7.Cuffe SP, Moore CG, McKeown RE. Prevalence and correlates of ADHD symptoms in the national health interview survey. J Atten Disord. 2005;9:392–401. doi: 10.1177/1087054705280413. [DOI] [PubMed] [Google Scholar]
- 8.Graetz BW, Sawyer MG, Baghurst P. Gender differences among children with DSM-IV ADHD in Australia. J Am Acad Child Adolesc Psychiatry. 2005;44:159–168. doi: 10.1097/00004583-200502000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Rowland AS, Lesesne CA, Abramowitz AJ. The epidemiology of attention-deficit/hyperactivity disorder (ADHD): a public health view. Ment Retard Dev Disabil Res Rev. 2002;8:162–170. doi: 10.1002/mrdd.10036. [DOI] [PubMed] [Google Scholar]
- 10.Resnick RJ. Attention deficit hyperactivity disorder in teens and adults: they don’t all outgrow it. J Clin Psychol. 2005;61:529–533. doi: 10.1002/jclp.20117. [DOI] [PubMed] [Google Scholar]
- 11.Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716–723. doi: 10.1176/appi.ajp.163.4.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36:159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- 13.Barkley RA. Advancing age, declining ADHD. Am J Psychiatry. 1997;154:1323–1325. doi: 10.1176/ajp.154.9.1323b. [DOI] [PubMed] [Google Scholar]
- 14.Faraone SV, Biederman J, Spencer T, et al. Attention-deficit/hyperactivity disorder in adults: an overview. Biol Psychiatry. 2000;48:9–20. doi: 10.1016/s0006-3223(00)00889-1. [DOI] [PubMed] [Google Scholar]
- 15.Todd RD, Huang H, Todorov AA, et al. Predictors of stability of attention- deficit/hyperactivity disorder subtypes from childhood to young adulthood. J Am Acad Child Adolesc Psychiatry. 2008;47:76–85. doi: 10.1097/chi.0b013e31815a6aca. [DOI] [PubMed] [Google Scholar]
- 16.Cantwell DP. Attention deficit disorder: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 1996;35:978–987. doi: 10.1097/00004583-199608000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Lahey BB, Applegate B, McBurnett K, et al. DSM-IV field trials for attention deficit hyperactivity disorder in children and adolescents. Am J Psychiatry. 1994;151:1673–1685. doi: 10.1176/ajp.151.11.1673. [DOI] [PubMed] [Google Scholar]
- 18.Wolraich ML, Hannah JN, Pinnock TY, Baumgaertel A, Brown J. Comparison of diagnostic criteria for attention-deficit hyperactivity disorder in a county-wide sample. J Am Acad Child Adolesc Psychiatry. 1996;35:319–324. doi: 10.1097/00004583-199603000-00013. [DOI] [PubMed] [Google Scholar]
- 19.Carlson CL, Tamm L, Gaub M. Gender differences in children with ADHD, ODD, and co-occurring ADHD/ODD identified in a school population. J Am Acad Child Adolesc Psychiatry. 1997;36:1706–1714. doi: 10.1097/00004583-199712000-00019. [DOI] [PubMed] [Google Scholar]
- 20.Gaub M, Carlson CL. Gender differences in ADHD: a meta-analysis and critical review. J Am Acad Child Adolesc Psychiatry. 1997;36:1036–1045. doi: 10.1097/00004583-199708000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Gershon J. A meta-analytic review of gender differences in ADHD. J Atten Disord. 2002;5:143–154. doi: 10.1177/108705470200500302. [DOI] [PubMed] [Google Scholar]
- 22.Biederman J, Kwon A, Aleardi M, et al. Absence of gender effects on attention deficit hyperactivity disorder: findings in nonreferred subjects. Am J Psychiatry. 2005;162:1083–1089. doi: 10.1176/appi.ajp.162.6.1083. [DOI] [PubMed] [Google Scholar]
- 23.Todd RD, Joyner CA, Heath AC, Neuman RJ, Reich W. Reliability and stability of a semistructured DSM-IV interview designed for family studies. J Am Acad Child Adolesc Psychiatry. 2003;42:1460–1468. doi: 10.1097/00004583-200312000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Swanson JM, Shuck S, Mann M, Carlson C, Hartman K, Sergeant J, Clevenger W, Wasdell M, McCleary R. Categorical and Dimensional Definitions and Evaluations of Symptoms of ADHD: The SNAP and the SWAN rating scales. Retrieved September 25, 2009 from www.adhd.net. [PMC free article] [PubMed]
- 25.Hay DA, Bennett KS, Levy F, Sergeant J, Swanson J. A twin study of attention-deficit/hyperactivity disorder dimensions rated by the strengths and weaknesses of ADHD-symptoms and normal-behavior (SWAN) scale. Biol Psychiatry. 2007;61:700–705. doi: 10.1016/j.biopsych.2006.04.040. [DOI] [PubMed] [Google Scholar]
- 26.Polderman TJ, Derks EM, Hudziak JJ, Verhulst FC, Posthuma D, Boomsma DI. Across the continuum of attention skills: a twin study of the SWAN ADHD rating scale. J Child Psychol Psychiatry. 2007;48:1080–1087. doi: 10.1111/j.1469-7610.2007.01783.x. [DOI] [PubMed] [Google Scholar]
- 27.Young DJ, Levy F, Martin NC, Hay DA. Attention Deficit Hyperactivity Disorder: A Rasch Analysis of the SWAN Rating Scale. Child Psychiatry Hum Dev. 2009;40:543–559. doi: 10.1007/s10578-009-0143-z. [DOI] [PubMed] [Google Scholar]
- 28.Royston P, Altman DG. Regression using Fractional Polynomials of Continuous Covariates: Parsimonius Parametric Modelling. Applied Statistics. 1994;3:429–467. [Google Scholar]
- 29.Froehlich TE, Lanphear BP, Epstein JN, Barbaresi WJ, Katusic SK, Kahn RS. Prevalence, recognition, and treatment of attention-deficit/hyperactivity disorder in a national sample of US children. Arch Pediatr Adolesc Med. 2007;161:857–864. doi: 10.1001/archpedi.161.9.857. [DOI] [PubMed] [Google Scholar]
- 30.Derks EM, Dolan CV, Hudziak JJ, Neale MC, Boomsma DI. Assessment and etiology of attention deficit hyperactivity disorder and oppositional defiant disorder in boys and girls. Behav Genet. 2007;37:559–566. doi: 10.1007/s10519-007-9153-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rhee SH, Waldman ID. Etiology of sex differences in the prevalence of ADHD: an examination of inattention and hyperactivity-impulsivity. Am J Med Genet B Neuropsychiatr Genet. 2004;127:60–64. doi: 10.1002/ajmg.b.20131. [DOI] [PubMed] [Google Scholar]
- 32.Lahey BB, Pelham WE, Loney J, Lee SS, Willcutt E. Instability of the DSM-IV Subtypes of ADHD from preschool through elementary school. Arch Gen Psychiatry. 2005;62:896–902. doi: 10.1001/archpsyc.62.8.896. [DOI] [PubMed] [Google Scholar]
- 33.Molina BS, Hinshaw SP, Swanson JM, et al. The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry. 2009;48:484–500. doi: 10.1097/CHI.0b013e31819c23d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Todd RD, Huang H, Henderson CA. Poor utility of the age of onset criterion for DSM-IV attention deficit/hyperactivity disorder: recommendations for DSM-V and ICD-11. J Child Psychol Psychiatry. 2008;49:942–949. doi: 10.1111/j.1469-7610.2008.01892.x. [DOI] [PubMed] [Google Scholar]
- 35.Rohde LA, Biederman J, Zimmermann H, Schmitz M, Martins S, Tramontina S. Exploring ADHD age-of-onset criterion in Brazilian adolescents. Eur Child Adolesc Psychiatry. 2000;9:212–218. doi: 10.1007/s007870070045. [DOI] [PubMed] [Google Scholar]
- 36.Faraone SV, Biederman J, Milberger S. How reliable are maternal reports of their children’s psychopathology? One-year recall of psychiatric diagnoses of ADHD children. J Am Acad Child Adolesc Psychiatry. 1995;34:1001–1008. doi: 10.1097/00004583-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 37.Angold A, Costello EJ. Puberty and depression. Child Adolesc Psychiatr Clin N Am. 2006;15:919–937. ix. doi: 10.1016/j.chc.2006.05.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.