Abstract
BACKGROUND
Homeless people have high rates of hospitalization and emergency department (ED) use. Obtaining adequate food is a common concern among homeless people and may influence health care utilization.
OBJECTIVE
We tested the hypothesis that food insufficiency is related to higher rates of hospitalization and ED use in a national sample of homeless adults.
DESIGN
We analyzed data from the 2003 Health Care for the Homeless (HCH) User Survey.
PARTICIPANTS
Participants were 966 adults surveyed at 79 HCH clinic sites throughout the US. The study sample was representative of over 436,000 HCH clinic users nationally.
MEASURES
We determined the prevalence and characteristics of food insufficiency among respondents. Using multivariable logistic regression, we examined the association between food insufficiency and four past-year acute health services utilization outcomes: (1) hospitalization for any reason, (2) psychiatric hospitalization, (3) any ED use, and (4) high ED use (≥4 visits).
RESULTS
Overall, 25% of respondents reported food insufficiency. Among them, 68% went a whole day without eating in the past month. Chronically homeless (p = 0.01) and traumatically victimized (p = 0.001) respondents were more likely to be food insufficient. In multivariable analyses, food insufficiency was associated with significantly greater odds of hospitalization for any reason (AOR 1.59, 95% CI 1.07, 2.36), psychiatric hospitalization (AOR 3.12, 95% CI 1.73, 5.62), and high ED utilization (AOR 2.83, 95% CI 1.32, 6.08).
CONCLUSIONS
One-fourth of homeless adults in this national survey were food insufficient, and this was associated with increased odds of acute health services utilization. Addressing the adverse health services utilization patterns of homeless adults will require attention to the social circumstances that may contribute to this issue.
KEY WORDS: homelessness, food insufficiency, health services utilization
INTRODUCTION
Homeless people have high rates of hospitalization and emergency department (ED) use, far exceeding the utilization rates in the US general population.1–3 Understanding the factors related to this has important policy implications. Competing demands for food are common among homeless individuals and may influence health care utilization patterns.4–6 Homeless people who do not get enough food to eat may postpone or forego needed medical care until later stages of illness,6–9 choose to buy food over medications,10–12 or have difficulty managing health conditions and adhering to treatment plans.13–15 In some cases, homeless people may use health services in order to get food.16 However, the relationship between lack of food and health care utilization among homeless adults has not been examined at a national level.
Recent evidence has documented mounting deficits in emergency food supplies in many US cities,17 making the threat of food shortages a more pressing reality among poor Americans. The experience of lacking food exists on a spectrum and has been variously labeled food insecurity, food insufficiency, and hunger. Food insecurity exists whenever the availability of nutritionally adequate and safe foods or the ability to acquire acceptable foods in socially acceptable ways is limited or uncertain.18 This definition encompasses both quantity and quality domains. Food insufficiency relates exclusively to inadequate quantity of food intake and therefore represents a more severe phenomenon than food insecurity.19,20 Hunger refers to discomfort, illness, weakness, or pain caused by prolonged, involuntary lack of food,21 and can be viewed as a physical consequence of food insufficiency.
Our specific aims were to describe the prevalence and characteristics of food insufficiency among homeless adults, and to determine the relationship between food insufficiency and utilization of acute health services among homeless adults. We hypothesized that food insufficiency would be associated with higher rates of hospitalization for any reason, psychiatric hospitalization, and emergency department use.
METHODS
Data Source
We performed a secondary analysis of the 2003 Health Care for the Homeless (HCH) User Survey, the first nationally representative survey of people using clinical services provided by the federally funded HCH program. The HCH program serves homeless individuals through grantees in all states, the District of Columbia, and Puerto Rico.22 The HCH User Survey was administered by Research Triangle Institute (RTI) International in collaboration with the Health Resources and Services Administration (HRSA) Bureau of Primary Health Care.
Participants and Setting
A three-stage sampling design was used to conduct the survey.23 Of 131 HCH grantees that had been in operation for at least 1 year, 30 were sampled using a geographically stratified probability proportional to size (PPS) technique. Interviews were conducted in-person by RTI field staff at a PPS sample of 79 clinic sites operated by the 30 grantees. The target population was people receiving face-to-face services from an HCH provider. Individuals were eligible if they had received such services at least once in the year prior to the visit in which the survey was administered, since the reference period for many of the questions was 12 months. Participants were selected consecutively with a goal of 33 interviews per grantee. Respondents provided informed consent, and the study was approved by the RTI International institutional review board.
Of 1,444 selected individuals, 1,017 completed the interview, yielding a response rate of 70%. We confined our analysis to the 966 respondents who were aged 18 or older. Analysis weights were applied to obtain estimates that were representative of the target population of 436,171 adult HCH clinic users nationally.
Main Predictor
Participants were asked the food sufficiency item presented in the Text Box. This question is very similar to that developed by the US Department of Agriculture and adapted for use in the Third National Health and Nutrition Examination Survey (NHANES).19,24 Consistent with convention, we defined food insufficiency as “sometimes” or “often” not getting enough to eat.20,24–27 This single item has undergone cognitive testing and validation in diverse populations, including low-income individuals; responses have been found to correlate with nutrient intake and food supplies.19,24–30 We used respondents’ self-reported number of meals per day, days going without eating in the past month, and days going hungry in the past month to internally validate this single item measure of food insufficiency in our study sample.
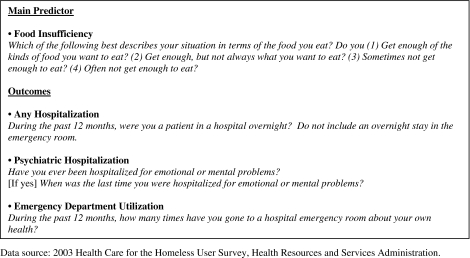
Text Box. Survey Questions Used to Define the Main Predictor and Study Outcomes.
Covariates
Sociodemographic variables included age (18–49 vs. ≥50 years,31,32), gender, self-reported race/ethnicity (categorized as white non-Hispanic, black non-Hispanic, Hispanic, and other), geographic region (Northeast, South, Midwest, or West), educational attainment (high school diploma or higher vs. less than high school completion), veteran status, employment (any past-year work for pay), and insurance status (insured vs. uninsured).
Homeless-specific characteristics included chronic homelessness, defined as being homeless for at least 1 year or having had four episodes of homelessness in one’s lifetime. This definition is similar to that used by the US Department of Housing and Urban Development.33 We also considered past-year physical or sexual assault while homeless, since victimized individuals appear to use health services at higher rates.3,34
Substance abuse variables included illicit drug use or problem alcohol use in the preceding year. Past-year drug use was defined as any past-year use of illicit or non-prescribed controlled substances, or any past-year drug treatment. Past-year problem alcohol use was defined as consuming ≥5 drinks on a single occasion in the past month,35 consuming ≥3 drinks on a typical day of drinking in the past month,36 or any past-year alcohol treatment. Comorbid psychiatric illness was defined as having had “any serious personal or emotional problems” in the past year, using a question adapted from the mental health domain of the 1995 National Health Interview Survey Year 2000 Objectives Supplement.37
To assess medical comorbidity, we used a summary measure (0, 1, ≥2) of the following medical conditions, chosen based on clinical importance: hypertension, diabetes, cardiovascular disease (coronary artery disease or stroke), obstructive lung disease (asthma or chronic obstructive pulmonary disease), HIV infection, cancer, liver disease, kidney disease, and arthritis or chronic joint pain. General health status was dichotomized as fair/poor vs. excellent/very good/good.
Given the potential relationship between food deprivation and overweight,38–42 we used self-reported height and weight to calculate body mass index (BMI). Overweight was defined as having a BMI of 25–29.9 kg/m2, and obesity was defined as having a BMI≥30 kg/m2.43 We validated these measures by comparing the frequency distributions of overweight and obesity to those found in the HCH Visit Survey, a separate chart abstraction study conducted in an independent sample of HCH visits.23
Main Outcome Measures
Our study outcomes were four self-reported measures of past-year acute health services use: (1) hospitalization for any reason, (2) psychiatric hospitalization, (3) any emergency department (ED) use, and (4) high ED use (≥4 visits). The survey questions used to define these outcomes are presented in the Text Box. The definition for high ED use was derived from a prior survey of homeless and marginally housed individuals in which the 8% of respondents who used the ED four or more times in 1 year accounted for 55% of ED visits among those surveyed.3
Statistical Analysis
Chi-square tests were used to determine the unadjusted relationships between categorical variables. We then constructed four multivariable logistic regression models to determine the adjusted relationship between food insufficiency and each health services use outcome, controlling for potential confounders. Candidate covariates were chosen based on prior hypotheses and literature review. In order to obtain stable estimates of effect and avoid model overfitting,44,45 only covariates associated with the respective outcomes at a univariate significance level of p < 0.20 were included in the final multivariable models.
In the principal analyses, participants with missing data for a model variable were excluded from any analysis involving the variable. Item non-response was negligible for the utilization outcomes (≤0.3%) and minimal for model covariates (≤2.4%). Thirty-one adults (3.6%) had missing or indeterminate responses for the food insufficiency item; we assessed the impact of this in two ways. First, we re-ran all models using a food insufficiency missing indicator variable. Next, we performed sensitivity analyses in which all respondents with missing data for food insufficiency were first assumed to be food insufficient and then subsequently assumed to be food sufficient. In all cases, the final multivariable results were unchanged.
Due to the complex sampling design of the survey, all analyses were performed using SAS-Callable SUDAAN, Release 10.0 (Research Triangle Park, NC), in conjunction with SAS 9.2 (Cary, NC). We used weights developed by RTI that incorporated: (1) sampling probability to account for the survey design, (2) adjustment for non-response to reduce bias in the study estimates, and (3) post-stratification adjustment to better reflect the target population of HCH clinic users nationally based on HRSA Uniform Data System estimates. Results were considered significant at p < 0.05.
RESULTS
Respondent Characteristics
Fifty-eight percent of respondents were male, and 20% were 50 years of age or older (Table 1). One in five reported being physically or sexually assaulted in the past year, and 35% of respondents were chronically homeless. The distribution of overweight (28%) and obesity (30%) was very similar to that documented in the HCH Visit Survey (29% obese, 31% overweight).23
Table 1.
Characteristics of the Study Sample
| Overall | Food insufficiency* | |||
|---|---|---|---|---|
| Total, N = 966 % (SE)† | Yes, N = 235 % (SE)† | No, N = 700 % (SE)† | P value‡ | |
| Sociodemographics | ||||
| Age, ≥50 years | 19.5 (1.3) | 16.0 (2.5) | 20.1 (1.7) | 0.25 |
| Sex, male | 58.2 (4.5) | 58.5 (9.5) | 57.7 (4.3) | 0.93 |
| Race | 0.01 | |||
| White, non-Hispanic | 39.2 (4.2) | 44.7 (7.6) | 37.9 (6.0) | |
| Black, non-Hispanic | 38.1 (5.8) | 25.9 (5.3) | 43.6 (7.1) | |
| Hispanic | 16.1 (2.6) | 22.9 (7.0) | 14.4 (2.1) | |
| Other | 5.3 (1.2) | 6.6 (2.5) | 4.1 (1.4) | |
| Region | 0.88 | |||
| Northeast | 15.9 (3.3) | 16.1 (4.5) | 16.3 (3.2) | |
| South | 17.2 (5.8) | 21.3 (9.9) | 16.6 (5.4) | |
| Midwest | 43.3 (8.4) | 39.9 (11.2) | 45.5 (7.7) | |
| West | 23.7 (9.0) | 22.7 (8.9) | 21.6 (8.2) | |
| High school diploma or higher | 58.7 (2.7) | 49.5 (4.0) | 61.4 (3.2) | 0.01 |
| Veteran | 11.5 (1.1) | 11.8 (2.9) | 11.3 (1.1) | 0.88 |
| Employed, past year | 54.5 (3.7) | 54.1 (4.2) | 55.3 (4.2) | 0.75 |
| Uninsured | 59.5 (5.4) | 61.6 (6.3) | 59.6 (5.6) | 0.73 |
| Homeless characteristics | ||||
| Chronically homeless | 35.3 (3.2) | 45.5 (6.2) | 31.7 (3.5) | 0.01 |
| Physical/sexual assault, past year | 20.1 (2.8) | 37.5 (7.1) | 14.5 (1.9) | 0.001 |
| Mental health | ||||
| Serious emotional problems, past year | 55.6 (3.5) | 59.8 (8.6) | 54.7 (3.6) | 0.57 |
| Alcohol/drug problem, past year | 65.3 (4.3) | 67.8 (6.0) | 67.0 (4.6) | 0.90 |
| Physical health | ||||
| Fair/poor health status | 47.9 (2.6) | 53.2 (4.6) | 45.0 (3.4) | 0.18 |
| Medical comorbidities§ | 0.23 | |||
| 0 | 22.2 (2.5) | 16.5 (4.5) | 24.9 (2.9) | |
| 1 | 31.2 (2.5) | 27.1 (6.4) | 32.9 (2.4) | |
| ≥2 | 45.9 (4.0) | 56.4 (10.0) | 42.3 (3.2) | |
| Overweight/obese║ | 57.7 (4.5) | 51.0 (8.8) | 62.0 (3.5) | 0.09 |
Data source: 2003 Health Care for the Homeless User Survey, Health Resources and Services Administration
SE, standard error
*Defined as ‘sometimes’ or ‘often’ not getting enough food to eat. Thirty-one adults (3.6%) had missing or indeterminate responses for the food insufficiency item
†Percentages are weighted using analysis weights provided by Research Triangle Institute, International. Percentages are expressed as a function of column totals and may not sum to 100 within categories because of rounding or item non-response.
‡P value for chi-square test comparing food insufficient and food sufficient respondents on each characteristic
§Medical comorbidities included hypertension, diabetes, cardiovascular disease (coronary artery disease or stroke), obstructive lung disease (asthma or COPD), HIV infection, cancer, kidney disease, liver disease, and arthritis or chronic joint problems
║Defined as body mass index ≥25 kg/m2
Food insufficiency
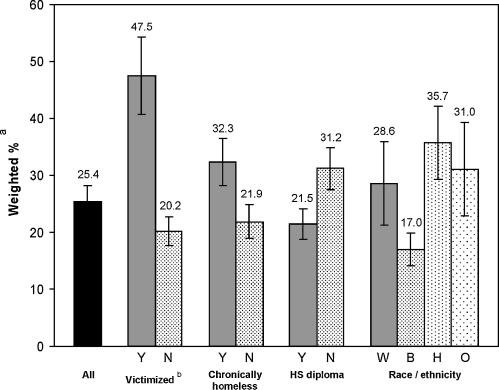
Prevalence Twenty-five percent of respondents reported sometimes or often not getting enough food to eat (Fig. 1). The prevalence of food insufficiency was 32% among chronically homeless adults and 48% among respondents who had been physically or sexually assaulted in the past year.
Figure 1.
Prevalence of food insufficiency among all adult respondents (n = 966) and in selected demographic subgroups. Data source: 2003 Health Care for the Homeless User Survey, Health Resources and Services Administration. Abbreviations: Y = yes, N = no, W = white, B = black, H = Hispanic, O = other, HS = high school. aPercentages are weighted using analysis weights provided by Research Triangle Institute, International. Tick marks indicate the bounds of one standard error. bPhysically or sexually assaulted in the past year.
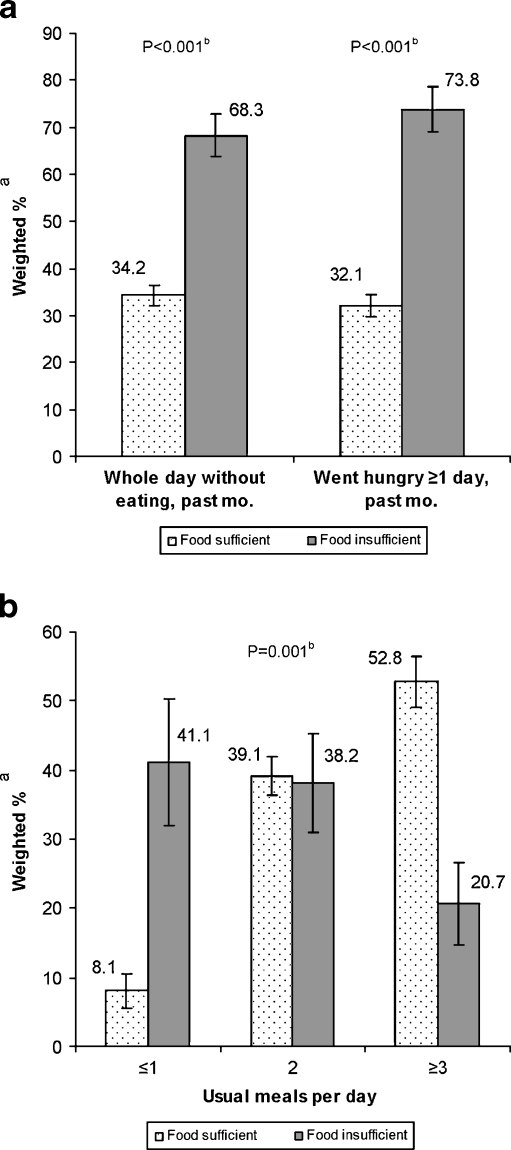
Internal Validation Food insufficient respondents were significantly more likely than food sufficient respondents to go a whole day without eating (68% vs. 34%, p < 0.001) and to go hungry for at least 1 day in the past month (74% vs. 32%, p < 0.001) (Fig. 2a). Food insufficient respondents reported consuming significantly fewer meals than food sufficient respondents; over 40% consumed one or less per day (Fig. 2b).
Figure 2.
Food intake and hunger characteristics of food insufficient vs. food sufficient respondents. Panel a Going without eating and going hungry, past month. Panel b Usual daily meal consumption. Data source: 2003 Health Care for the Homeless User Survey, Health Resources and Services Administration. a Percentages are weighted using analysis weights provided by Research Triangle Institute, International. Tick marks indicate the bounds of one standard error. b P value for chi-square test.
Characteristics Food insufficient respondents were less likely than food sufficient respondents to be black and to have attained a high school diploma (Table 1). Chronic homelessness and past-year victimization were significantly more common among food insufficient respondents.
Health Services Use
Any Hospitalization Overall, 35% of respondents reported being hospitalized in the past year. In unadjusted analyses, food insufficient respondents had higher rates of hospitalization than food sufficient respondents (46% vs. 30%, p = 0.02) (Table 2). After adjusting for insurance status, medical comorbidity, and other potential confounders in the multivariable model, this association remained significant [adjusted odds ratio (AOR) 1.59, 95% CI 1.07, 2.36].
Table 2.
Food Insufficiency and Past-Year Health Services Utilization
| (A) Hospitalization | ||||
| Any hospitalization, past year | Psychiatric hospitalization, past year | |||
| % (SE)† | AOR (95% CI)‡ | % (SE)† | AOR (95% CI)§ | |
| Food insufficiency* | ||||
| No | 30.3 (2.5) | 1.00 (Ref.) | 8.9 (1.6) | 1.00 (Ref.) |
| Yes | 46.3 (5.9) | 1.59 (1.07, 2.36) | 25.0 (5.6) | 3.12 (1.73, 5.62) |
| (B) Emergency department (ED) utilization | ||||
| Any ED visits, past year | ≥4 ED visits, past year# | |||
| % (SE)† | AOR (95% CI)║ | % (SE)† | AOR (95% CI)¶ | |
| Food insufficiency* | ||||
| No | 59.7 (3.0) | 1.00 (Ref.) | 13.0 (2.0) | 1.00 (Ref.) |
| Yes | 68.5 (7.3) | 1.20 (0.61, 2.37) | 30.3 (11.0) | 2.83 (1.32, 6.08) |
Data source: 2003 Health Care for the Homeless User Survey, Health Resources and Services Administration
SE, standard error; AOR, adjusted odds ratio; CI, confidence interval; Ref., referent; ED, emergency department
*Defined as ‘sometimes’ or ‘often’ not getting enough food to eat
†Percentages are weighted using analysis weights provided by Research Triangle Institute, International
‡Adjusted for age, race, region, education, insurance status, chronic homelessness, past-year victimization, past-year serious emotional problems, number of medical comorbidities, and overweight/obesity
§Adjusted for age, chronic homelessness, past-year victimization, past-year serious emotional problems, past-year substance abuse, and number of medical comorbidities
║Adjusted for race, region, insurance status, past-year victimization, past-year serious emotional problems, and number of medical comorbidities
¶Adjusted for gender, race, insurance status, past-year victimization, past-year serious emotional problems, past-year substance abuse, fair/poor health status, and number of medical comorbidities
#Comparison group is respondents with 0–3 ED visits
Psychiatric Hospitalization Thirteen percent of respondents reported being hospitalized for mental or emotional problems in the past year. Food insufficient respondents had a nearly three-fold higher unadjusted rate of past-year psychiatric hospitalization than food sufficient respondents (25% vs. 9%, p = 0.003) (Table 2). This association remained significant in the multivariable analysis adjusted for substance abuse, emotional disturbance, victimization history, and other potential confounders (AOR 3.12, 95% CI 1.73, 5.62).
Any ED Use Overall, 62% of respondents reported using the ED at least once in the past year. Food insufficient respondents had non-significantly higher unadjusted rates and adjusted odds of making any ED visit in the past year (69% vs. 60%, p = 0.32; AOR 1.20, 95% CI 0.61, 2.37) (Table 2).
High ED Use Overall, 18% of respondents reported using the ED four or more times in the past year. Food insufficient respondents had a more than two-fold higher unadjusted rate of past-year high ED utilization (30% vs. 13%, p = 0.09; unadjusted OR 2.91, 95% CI 0.83, 10.3) (Table 2). Adjusting for medical comorbidity, substance abuse, victimization history, and other potential confounders in the multivariable model resulted in a relatively unchanged but more precise estimate of effect (AOR 2.83, 95% CI 1.32, 6.08).
DISCUSSION
One-fourth of homeless adults in this study reported not getting enough food to eat. The prevalence of food insufficiency was six times higher than that seen in the US general population, and more than double that seen among impoverished Americans.20 It is very similar to the prevalence among homeless individuals in the 1996 National Survey of Homeless Assistance Providers and Clients.46
Food insufficiency was associated with several markers of vulnerability. Chronic homelessness, a history of physical or sexual assault, and low educational attainment were all more common among food insufficient respondents in comparison to those who reported getting enough to eat. This finding is concordant with prior work demonstrating a high burden of food insecurity among chronically homeless individuals, further disputing the notion that the accumulated “street wisdom” of entrenched homelessness might endow a protective effect against lacking food because of increased knowledge about how to acquire it.4 Instead, the clustering of food, shelter, and safety concerns documented in this study suggests that difficulty in meeting one basic subsistence need predicts difficulties with others.
Food insufficient respondents used acute health services at considerably higher rates than food sufficient individuals. This complements and extends prior evidence demonstrating increased hospital and ED use among food insecure low-income Americans.9 The hospitalization and ED utilization rates among food insufficient adults in our study sample were about five times higher than those seen among adults in the US general population.47 In multivariable analyses adjusted for important confounders, food insufficiency was associated with significantly greater odds of hospitalization for any reason, psychiatric hospitalization, and high emergency department utilization. Although prior evidence has shown higher rates of some chronic diseases among food-deprived individuals,48–50 the associations between food insufficiency and health services utilization were independent of medical comorbidity.
To our knowledge, this is the first national study to document the association between food insufficiency and acute health services utilization among homeless adults. Our findings add to a growing literature supporting the hypothesis that food insufficiency may represent an important non-medical determinant of acute health services use. Several mechanisms are suggested by this body of evidence; the priority of basic subsistence needs over health-related issues forms the foundation of each.
Food insufficient homeless people may postpone treatment at earlier stages of illness until the need is acute,6,51 resulting in crisis-oriented service utilization patterns.7 Indeed, food insufficiency and insecurity have been linked to going without needed health care among both homeless and low-income housed individuals,8,9 suggesting that the pattern of acute utilization seen in this study may have its roots in poor access to other health care services.
Food insufficiency may also require that patients make choices between buying food and medications. Food insecurity has been associated with spacing out the frequency of medication use and putting off the purchase of medications in favor of buying food.11 In studies of ED patients, those confronted with these trade-offs between food and medication believed that their choices caused illness, resulting in increased ED use and hospitalization.10,12
Food insufficiency may adversely impact disease self-management and treatment adherence, leading to poorer overall disease control.15 Indeed, homeless diabetics in Toronto reported that inadequate dietary choices were a principal barrier to disease management.14 Among low-income diabetic participants in NHANES, food insecurity was associated with a 40% greater risk of inadequate disease control.49 In a sample of diabetic patients at an urban county hospital, one-third of those with hypoglycemic episodes attributed their episodes to being unable to afford food; of these, one-fourth required ED treatment or hospitalization.52 Among homeless HIV-positive individuals, food insecurity has been associated with lower rates of anti-retroviral treatment adherence and viral load suppression.13
Finally, a portion of acute health services utilization by food insufficient homeless adults might be attributable to an effort to get food through these services. Among homeless ED users in San Francisco, one in eight reported that hunger was the main reason for their visit.16
Limitations
Our study has important limitations. All measures were self-reported and may be subject to bias. The single item measure of food insufficiency may provide a less comprehensive picture of food resources among homeless people than the multi-item US Food Security Survey Module,53 which was not assessed in the HCH User Survey. When deployed simultaneously in other populations, the food insufficiency item and the food security module have shown substantial overlap in identifying limited food access,54,55 and both are correlated with household food supplies.29 Although tested in low-income settings, the food insufficiency item has not been formally validated in the setting of homelessness. We addressed this limitation by internally validating this item against other self-reported measures of food intake and hunger; we found that it correlated well with these measures. Notably, over 30% of food sufficient respondents reported going hungry or going a whole day without eating in the past month. This suggests that homeless people may have a different threshold than those in the general population in defining “enough to eat.” To the extent that such respondents are characterized as food sufficient, our findings likely represent a conservative estimate of food insufficiency and its effect on health services utilization among homeless adults.
The study sample consisted of adults who had used HCH clinic services at least twice in the past year, so the findings may not be generalizable to the homeless population as a whole. Lastly, causality cannot be determined due to the cross-sectional nature of the data. The relationship between food insufficiency and health services utilization was statistically independent of many potential confounding factors; however, reverse causation or unmeasured confounders such as social support and community-level resources may provide alternative explanations. Although we have highlighted several mechanisms by which lacking food may impact health services use, future studies should attempt to clarify these mechanisms and determine whether expanded provision of food services positively impacts patterns of health care utilization in addition to the expected benefits in overall well-being.
CONCLUSION
Lacking food was common and closely correlated with other markers of vulnerability in this national sample of homeless adults. Food insufficient respondents had higher odds of acute health services utilization despite the fact that all respondents had accessed ambulatory care in the prior year. The growing deficit in emergency food supplies makes this finding particularly concerning. Addressing the adverse health services utilization patterns of homeless adults will require attention to the social determinants of this issue. Efforts to provide primary care for homeless persons should be matched by public health and policy initiatives to provide for basic subsistence needs among the very poor.
Acknowledgments
This study was funded by grant number T32HP10251 from the Health Resources and Services Administration of the Department of Health and Human Services to support the Harvard Medical School Fellowship in General Medicine and Primary Care. The views expressed in this publication are the opinions of the authors and do not necessarily reflect the official policies of the US Department of Health and Human Services or the Health Resources and Services Administration, nor does mention of the department or agency imply endorsement by the US government.
A preliminary summary of these findings was presented as a scientific abstract at the Society of General Internal Medicine 33rd Annual Meeting (Minneapolis, MN; April 28–May 1, 2010).
Conflicts of interest None disclosed
REFERENCES
- 1.Martell JV, Seitz RS, Harada JK, Kobayashi J, Sasaki VK, Wong C. Hospitalization in an urban homeless population: the Honolulu Urban Homeless Project. Ann. Intern. Med. 1992;116(4):299–303. doi: 10.7326/0003-4819-116-4-299. [DOI] [PubMed] [Google Scholar]
- 2.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200–206. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- 3.Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: results from a community-based study. Am. J. Public Health. 2002;92(5):778–784. doi: 10.2105/AJPH.92.5.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee BA, Greif MJ. Homelessness and hunger. J. Health Soc. Behav. 2008;49(1):3–19. doi: 10.1177/002214650804900102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stark LR. Barriers to health care for homeless people. In: Jahiel RI, editor. Homelessness: a Prevention-Oriented Approach. Baltimore: Johns Hopkins University Press; 1992. pp. 151–164. [Google Scholar]
- 6.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am. J. Public Health. 1997;87(2):217–220. doi: 10.2105/AJPH.87.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elvy A. Access to care. In: Brickner PW, Scharer LK, Conanan B, Elvy A, Savarese M, editors. Health Care of Homeless People. New York: Springer; 1985. pp. 223–231. [Google Scholar]
- 8.Baggett TP, O’Connell JJ, Singer DE, Rigotti NA. The unmet health care needs of homeless adults: a national study. Am J Public Health. Jul;100(7):1326-1333. [DOI] [PMC free article] [PubMed]
- 9.Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J. Gen. Intern. Med. 2006;21(1):71–77. doi: 10.1111/j.1525-1497.2005.00278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Biros MH, Hoffman PL, Resch K. The prevalence and perceived health consequences of hunger in emergency department patient populations. Acad. Emerg. Med. 2005;12(4):310–317. doi: 10.1111/j.1553-2712.2005.tb01949.x. [DOI] [PubMed] [Google Scholar]
- 11.Sullivan AF, Clark S, Pallin DJ, Camargo CA, Jr. Food security, health, and medication expenditures of emergency department patients. J Emerg Med. Mar 7 2009. [DOI] [PMC free article] [PubMed]
- 12.Kersey MA, Beran MS, McGovern PG, Biros MH, Lurie N. The prevalence and effects of hunger in an emergency department patient population. Acad. Emerg. Med. 1999;6(11):1109–1114. doi: 10.1111/j.1553-2712.1999.tb00112.x. [DOI] [PubMed] [Google Scholar]
- 13.Weiser SD, Frongillo EA, Ragland K, Hogg RS, Riley ED, Bangsberg DR. Food insecurity is associated with incomplete HIV RNA suppression among homeless and marginally housed HIV-infected individuals in San Francisco. J. Gen. Intern. Med. 2009;24(1):14–20. doi: 10.1007/s11606-008-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hwang SW, Bugeja AL. Barriers to appropriate diabetes management among homeless people in Toronto. CMAJ. 2000;163(2):161–165. [PMC free article] [PubMed] [Google Scholar]
- 15.Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. Jul 1;363(1):6-9. [DOI] [PubMed]
- 16.Rodriguez RM, Fortman J, Chee C, Ng V, Poon D. Food, shelter and safety needs motivating homeless persons’ visits to an urban emergency department. Ann. Emerg. Med. 2009;53(5):598–602. doi: 10.1016/j.annemergmed.2008.07.046. [DOI] [PubMed] [Google Scholar]
- 17.Hunger and Homelessness Survey: A Status Report on Hunger and Homelessness in America’s Cities: A 27-City Survey. Washington, DC: The United States Conference of Mayors; 2009. [Google Scholar]
- 18.Core indicators of nutritional state for difficult-to-sample populations. J Nutr. Nov 1990;120 Suppl 11:1559-1600. [DOI] [PubMed]
- 19.Briefel RR, Woteki CE. Development of food sufficiency questions for the Third National Health and Nutrition Examination Survey. J. Nutr. Educ. 1992;24:24S–28S. [Google Scholar]
- 20.Alaimo K, Briefel RR, Frongillo EA, Jr, Olson CM. Food insufficiency exists in the United States: results from the third National Health and Nutrition Examination Survey (NHANES III) Am. J. Public Health. 1998;88(3):419–426. doi: 10.2105/AJPH.88.3.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wunderlich GS, Norwood JL, editors. Committee on National Statistics, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press; 2006. Food insecurity and hunger in the United States: an assessment of the measure. Panel to review the US Department of Agriculture’s measurement of food insecurity and hunger. [Google Scholar]
- 22.Bureau of Primary Health Care, Health Resources and Services Administration. Bureau of Primary Health Care Section 330 Grantees Uniform Data System (UDS), Calendar Year 2007 Data: Health Care for the Homeless Rollup Report: US Department of Health and Human Services; 2008.
- 23.Greene J, Fahrney K, Byron M. Health Care for the Homeless User/Visit Surveys, RTI Project Number 07147.021. Research Triangle Park, NC: RTI International; 2004. [Google Scholar]
- 24.Carlson S, Briefel RR. The USDA and NHANES food sufficiency question as an indicator of hunger and food insecurity. Paper presented at: Conference on Food Security Measurement and Research. 1995; Washington, DC
- 25.Rose D, Oliveira V. Nutrient intakes of individuals from food-insufficient households in the United States. Am. J. Public Health. 1997;87(12):1956–1961. doi: 10.2105/AJPH.87.12.1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Basiotis PP. Validity of the self-reported food sufficiency status item in the US Department of Agriculture Food Consumption Surveys. Paper presented at: Annual Meeting of the American Council in the Consumer Interest, 1992; Toronto, Canada.
- 27.Cristofar SP, Basiotis PP. Dietary intake and selected characteristics of women age 19–50 years and their children age 1–5 years by reported perception of food sufficiency. J. Nutr. Educ. 1992;24:53–58. [Google Scholar]
- 28.Alaimo K, Olson CM, Frongillo EA. Importance of cognitive testing for survey items: an example from food security questionnaires. J. Nutr. Educ. 1999;31(5):269–275. doi: 10.1016/S0022-3182(99)70463-2. [DOI] [Google Scholar]
- 29.Kaiser LL, Melgar-Quinonez H, Townsend MS, et al. Food insecurity and food supplies in Latino households with young children. J. Nutr. Educ. Behav. 2003;35(3):148–153. doi: 10.1016/S1499-4046(06)60199-1. [DOI] [PubMed] [Google Scholar]
- 30.Rose D, Oliveira V. Validation of a Self-reported Measure of Household Food Insufficiency with Nutrient Intake Data. Technical bulletin 1863. Washington, DC: US Department of Agriculture, Economic Research Service; 1997. [Google Scholar]
- 31.Gelberg L, Linn LS, Mayer-Oakes SA. Differences in health status between older and younger homeless adults. J. Am. Geriatr. Soc. 1990;38(11):1220–1229. doi: 10.1111/j.1532-5415.1990.tb01503.x. [DOI] [PubMed] [Google Scholar]
- 32.Garibaldi B, Conde-Martel A, O’Toole TP. Self-reported comorbidities, perceived needs, and sources for usual care for older and younger homeless adults. J. Gen. Intern. Med. 2005;20(8):726–730. doi: 10.1111/j.1525-1497.2005.0142.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Defining Chronic Homelessness: a Technical Guide for HUD Programs. Office of Community Planning and Development, Office of Special Needs Assistance Programs, US Department of Housing and Urban Development. Washington, DC 2007.
- 34.Koss MP, Koss PG, Woodruff WJ. Deleterious effects of criminal victimization on women’s health and medical utilization. Arch. Intern. Med. 1991;151(2):342–347. doi: 10.1001/archinte.151.2.342. [DOI] [PubMed] [Google Scholar]
- 35.NIAAA Council Approves Definition of Binge Drinking. NIAAA Newsletter. Vol Winter. Rockville, MD: US Department of Health & Human Services; 2004. p. 3. [Google Scholar]
- 36.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Test: Guidelines for Use in Primary Care, Second Edition. Document No. WHO/MSD/MSB/01.6a: World Health Organization; 2001.
- 37.Data File Documentation, National Health Interview Survey of Topics Related to the Year 2000 Health Objectives, 1995. Hyattsville, MD: National Center for Health Statistics; 1997. [Google Scholar]
- 38.Townsend MS, Peerson J, Love B, Achterberg C, Murphy SP. Food insecurity is positively related to overweight in women. J. Nutr. 2001;131(6):1738–1745. doi: 10.1093/jn/131.6.1738. [DOI] [PubMed] [Google Scholar]
- 39.Dietz WH. Does hunger cause obesity? Pediatrics. 1995;95(5):766–767. [PubMed] [Google Scholar]
- 40.Martin KS, Ferris AM. Food insecurity and gender are risk factors for obesity. J. Nutr. Educ. Behav. 2007;39(1):31–36. doi: 10.1016/j.jneb.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 41.Olson CM. Nutrition and health outcomes associated with food insecurity and hunger. J. Nutr. 1999;129(2S Suppl):521S–524S. doi: 10.1093/jn/129.2.521S. [DOI] [PubMed] [Google Scholar]
- 42.Basiotis PP, Lino M. Food insufficiency and prevalence of overweight among adult women. Nutrition Insights. 2002(26).
- 43.Centers for Disease Control and Prevention. Overweight and Obesity: Defining Overweight and Obesity. 2010; http://www.cdc.gov/obesity/defining.html. Accessed December 29, 2010.
- 44.Cepeda MS, Boston R, Farrar JT, Strom BL. Comparison of logistic regression versus propensity score when the number of events is low and there are multiple confounders. Am. J. Epidemiol. 2003;158(3):280–287. doi: 10.1093/aje/kwg115. [DOI] [PubMed] [Google Scholar]
- 45.Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996;49(12):1373–1379. doi: 10.1016/S0895-4356(96)00236-3. [DOI] [PubMed] [Google Scholar]
- 46.Burt MR. Urban Institute. Homelessness: Programs and the People They Serve: Findings of the National Survey of Homeless Assistance Providers and Clients: Technical Report. Washington, DC: US Department of Housing and Urban Development, Office of Policy Development and Research; 1999. [Google Scholar]
- 47.Medical Expenditure Panel Survey, MEPSnet Query Tools. Agency for Healthcare Research and Quality, Rockville, MD; 2003. http://www.meps.ahrq.gov/mepsweb. Accessed December 29, 2010.
- 48.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999-2002. J. Gen. Intern. Med. 2007;22(7):1018–1023. doi: 10.1007/s11606-007-0192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. Feb;140(2):304-310. [DOI] [PMC free article] [PubMed]
- 50.Vozoris NT, Tarasuk VS. Household food insufficiency is associated with poorer health. J. Nutr. 2003;133(1):120–126. doi: 10.1093/jn/133.1.120. [DOI] [PubMed] [Google Scholar]
- 51.Schlossstein E, St Clair P, Connell F. Referral keeping in homeless women. J. Community Health. 1991;16(6):279–285. doi: 10.1007/BF01324513. [DOI] [PubMed] [Google Scholar]
- 52.Nelson K, Brown ME, Lurie N. Hunger in an adult patient population. JAMA. 1998;279(15):1211–1214. doi: 10.1001/jama.279.15.1211. [DOI] [PubMed] [Google Scholar]
- 53.Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Security. Alexandria, VA: US Department of Agriculture, Food and Nutrition Service; 2000. [Google Scholar]
- 54.Hamilton WL, Cook JT, Thompson WW, et al. Household Food Security in the United States in 1995. Alexandria, VA: US Department of Agriculture, Food and Consumer Service; 1997. [Google Scholar]
- 55.Cohen B, Ohls J, Andrews M, et al. Food Stamp Participants’ Food Security and Nutrient Availability: Final Report. Alexandria, VA: US Department of Agriculture, Food and Nutrition Service; 1999. [Google Scholar]