Abstract
Stapedotomy with implantation of an alloplastic prosthesis is a well-established therapy for the treatment of otosclerosis. Since the middle of 2008, a new Nitinol prosthesis with memory function and superelastic properties has been available which is expected to make fixation on the long process of the incus much easier. The advantage of this prosthesis is that heat-induced wire crimping is no longer necessary and damage to the incus caused by heat is avoided. Since May 2008, laser-assisted stapedotomy with implantation of a Nitinol prosthesis was performed in 21 patients suffering from otosclerosis. The prostheses used for all patients had a size of 4.5 mm × 0.4 mm. The patient collective consisted of 14 women and 7 men with a mean age of 53.4 years. Pre- and postoperatively, an ENT examination was carried out followed by an audiological evaluation of the hearing result. In addition, the properties of the prosthesis (“proper fitt”, “handling”, and “overall rating”) were evaluated intraoperatively by means of a test protocol. The Nitinol prosthesis was implanted successfully in all 21 patients. The mean air-bone gap for the frequencies from 0.5 to 4 kHz was 9.83 dB postoperatively. Intraoperatively, the fit of the prosthesis was rated as “good to very good”, the handling as “good” and the overall rating of the system was “good to very good”. Our patient collective showed good postoperative hearing results. Due to simple intraoperative handling, especially placing the Nitinol prosthesis in position, the critical work step of crimping is no longer necessary.
Keywords: Otosclerosis, Stapedotomy, Nitinol, Air-bone gap
Introduction
With an incidence of 1–2% of the white population, otosclerosis is among the most common causes of acquired hearing impairment. A bony obliteration of the oval window in a patient who had already lost his hearing was described for the first time in the 18th century. In 1894, Politzer introduced the term otosclerosis as an entity, but it was only in 1956 that otosclerosis was successfully treated by stapedectomy for the first time by Shea [1]. He used a prosthesis developed by his friend Harry Treace, which was made of the “brand-new Teflon material” [2, 3]. The technique developed by Shea continues to be valid to the present day; however, the less invasive stapedotomy has its benefits [4]. With this method, micro-drills or various lasers are used to perforate the stapes footplate [5–7]. Not only the surgery technique but also the prostheses available to the surgeon have continued to evolve since the Teflon prosthesis developed by Treace. Apart from Teflon, various other materials such as titanium, gold, platinum or special steel are employed [8, 9]. Not only are there different options when it comes to material, the prostheses available on the market, too, come in different varieties, with different types of prostheses often leading to the same postoperative hearing results [5, 10]. The main demands on a stapes prosthesis are good bio-tolerance, simple intraoperative handling and good sound transmission [11].
Notwithstanding continuous development of both the operation technique and the prostheses, some work steps that may have a significant impact on the operation result continue to be difficult and critical. Especially the safe fixation of the prosthesis on the long process of the incus is one of the most important and difficult parts of the operation on the success of which a good and lasting postoperative hearing result depends [12, 13].
Many prostheses are fastened by what is called “crimping” [14]. New types of prostheses such as the “Titanium Clip-Piston à Wengen” or the “Soft CliP Piston”, both of which prostheses are made of titanium, are simply slipped over the long process of the incus like a kind of clothes peg and are held in place by the tension of the prosthesis itself. Crimping is therefore no longer necessary [15, 16].
In the ongoing search for the perfect prosthesis from the perfect material, which mainly aims at simplifying the step of crimping, prostheses made of Nitinol (Nickel Titanium Naval Ordnance Laboratory) are a promising start. This nickel titanium alloy consists of 55% nickel and 45% titanium, has a mass of 6.5 g/cm³, and is the most widely-known of the “shape memory alloys”. Thanks to its shape memory, superelasticity, and good damping capacity, Nitinol is a highly interesting material for the development of alloplastic prostheses.
Depending on the temperature, Nitinol can assume two different structures. After deformation, Nitinol can reassume its default shape (defined at production) when heated. Depending on the production process, superelasticity is another outstanding property of Nitinol. Conventionally used prosthesis materials such as titanium only allow a pseudoelastic deformation of ~1%. With a deformation of 8%, Nitinol achieves nearly the elastic properties of natural materials such as hair, bones, and sinews, some of which allow form changes of up to 10% [17, 18].
In 1986, Enatsu carried out the first tests using Nitinol stapes prostheses in cats. In 1997, Kasano repeated similar studies and additionally examined the biocompatibility of the Nitinol prostheses under the microscope. He did not find any progressive bone resorption caused by Nitinol [19].
Since 2004, middle-ear prostheses made of Nitinol have been available for everyday clinical use for the first time. In case of the so-called Smart™ Piston, the bracket is made of Nitinol and makes use of the temperature-dependent shape memory of the alloy. After the prosthesis is placed in position at the long process of the incus, automatic crimping is induced by heat. For this purpose, a CO2, Argon, or KTP laser and bipolar forceps or battery-powered heating units are available. The postoperative hearing results are comparable to those achieved with a conventional prosthesis [20–25].
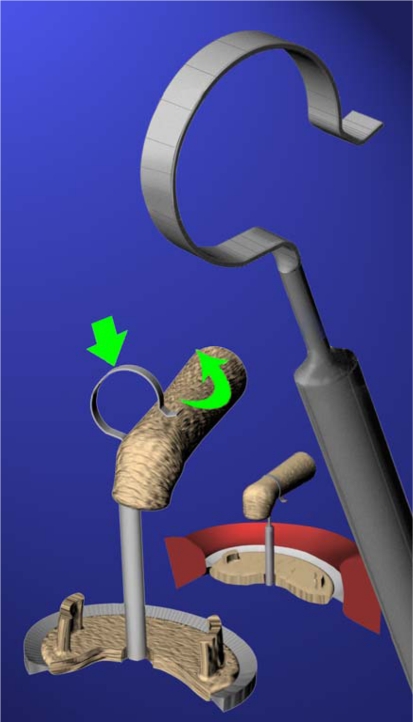
Since the middle of 2008 yet another Nitinol prosthesis (Self-Crimping Super Elastic NITINOL Piston, Audio Technologies, Italy) has been available on the market (Figs. 1, 2). This prosthesis makes use of the superelasticity of Nitinol as a result of which only minimal pressure of ~4 mg is necessary when slipping it on over the long process of the incus. Due to this property of the material, the Nitinol band loop fits snugly around the long process of the incus without further crimping and without application of heat.
Fig. 1.
Self-Crimping Super Elastic NITINOL Piston and animation of fixation to the long process of the incus (by kind permission of Audio Technologies, distributed by Spiggle & Theis Medizintechnik GmbH)
Fig. 2.
Self Crimping Super Elastic NITINOL Piston positioned at small alligator jaws forceps
In the present study we want to present our first results after implantation of the new Self-Crimping Super Elastic NITINOL Piston as alloplastic prosthesis in the surgical treatment of otosclerosis and evaluate the material properties of the prosthesis.
Materials and Methods
Since May 2008, 21 patients suffering from otosclerosis were treated with the Self-Crimping Super Elastic NITINOL Piston (Audio Technologies, Italy, distributed by Spiggle & Theis Medizintechnik GmbH, Germany). Prostheses with the size 0.4 mm × 4.5 mm were used for all patients, the pistons of all the prostheses were made of Nitinol.
The patient collective consisted of 14 women and 7 men with an age distribution of 37–62 years (mean age 53.4 years). The implantation was carried out 10 times on the right and 11 times on the left side.
In addition to an ENT medical status with ear microscopy, a tympanogram, a speech audiogram, a stapedius reflex test, tests according to Weber and Rinne, and an X-ray picture according to Schüller were performed.
The audiometric data was evaluated using the sound threshold audiogram carried out preoperatively and 6 weeks postoperatively. The absolute hearing thresholds and the air-bone gaps were compared.
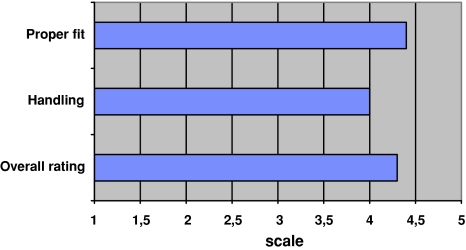
In addition, the properties of the prostheses were evaluated using a test protocol including items such as “proper fit”, “handling” and “overall rating” which could be rated on a 1–5 scale (1 = very poor; 5 = very good). All operations as well as the evaluation of the properties of the prostheses by means of the test protocol were carried out by the senior author.
Surgery was performed via enaural approach with a relieving incision according to Heermann after administration of general anesthesia. The stapedius tendon and the posterior limb were cut through with multiple individual pulses of the CO2 laser (capacity 2 W, pulse duration 50 ms). Establishment of a perforation of the stapes footplate with a diameter of ~600 μm was also carried out using a CO2 laser with single-shot technique (capacity 20 W, pulse duration 50 ms), according to the description by Jovanovic [6].
The prosthesis was then inserted in accordance with the manufacturer’s instructions. At the end of the operation, silicone strips and a tamponade of the meatus were inserted for 1 week.
On the first postoperative day, the air-bone gap was checked in all patients. After removal of the threads and the tamponade of the meatus 7 days postoperative, pure-tone audiometric testing was carried out. In addition, 6 weeks postoperative another pure-tone audiometric examination was performed at our clinic.
The statistical evaluation of our results was carried out using Excel and SPSS 17.0.
Results
In 21 patients suffering from otosclerosis, stapedotomy was performed using a CO2 laser with single shot technique. In all patients, the Nitinol piston was successfully implanted; the average incision-to-suture time was 55.32 min. Intraoperatively no complications occurred, neither were any persistent complications such as infections, inner ear deafness, or persistent vertigo noted postoperatively.
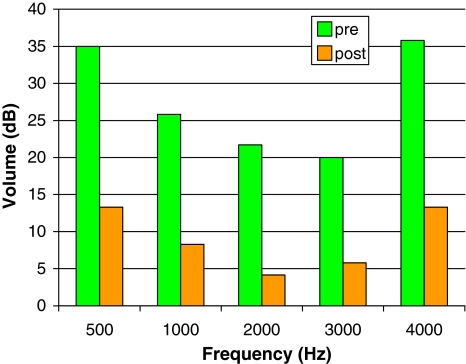
The preoperative auditory diagnostic showed an average air-bone gap in the five main frequencies (0.5–4 kHz) of 27.67 dB (Fig. 3), the absolute hearing threshold in the frequency range 0.5–4 kHz on average reached 61.0 dB (Fig. 4).
Fig. 3.
Average pre- and postoperative (green = preoperative, orange = postoperative) air-bone gap in dB with different frequencies in Hz
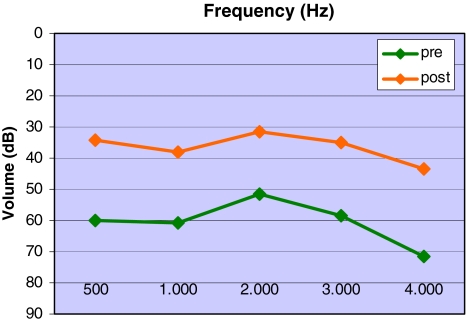
Fig. 4.
Average pre- and postoperative (green = preoperative, orange = postoperative) hearing threshold in dB with different frequencies in Hz
Postoperatively, in the main frequency range of 0.5–4 kHz, an average hearing threshold of 42.33 dB was noted (Fig. 4). The mean air-bone gap for the frequency range from 0.5 to 4 kHz was 9.83 dB postoperatively (Fig. 3). Postoperatively, the air-bone gap in the four main frequencies (0.5–4 kHz) was 15–20 dB in 6.7% of patients, 10–15 dB in 15.2% and under 10 dB in 78.0% of patients. That means that in 78.0% of patients a reduction of the air-bone gap down to 10 dB and less was achieved while a reduction to under 20 dB was achieved in 100% of all operated patients.
The postoperative hearing results were gathered during the pure-tone audiometric tests performed 6 weeks postoperative and other tests carried out at a later time at our out-patient department. The longest monitoring period currently is 15 months. In none of the patients the results have deviated from the results 6 weeks postoperative.
Using the test protocol, the prostheses inserted by the surgeon have been given the following ratings: the fit of the prosthesis was rated as “good to very good” (equivalent to a score of 4.3), the handling as “good” (a score of 4.0) and the overall rating of the system was “good to very good” (a score of 4.4) (Fig. 5).
Fig. 5.
Average evaluation of prosthesis properties from the test protocol. Rated on a 1–5 scale (1 = very poor; 5 = very good)
Discussion
Currently, a number of different types of prostheses are available for implantation of a stapes prosthesis in the framework of a stapedotomy. Most prostheses are fastened to the long process of the incus with a loop by means of so-called “crimping” 14]. Crimping is the most difficult step during stapedotomy, since too tight fastening of the loop on the long process of the incus may cause reduction of the blood supply, which may lead to a risk of erosion or even necrosis of the incus process. Damage of the process of the incus has been described several times in literature and has been subject to controversy [13, 26]. Excessive crimping or insufficiently tight fastening of the prosthesis both result in the same poor hearing results for the patient. The potential effects on the process of the incus vary strongly and may even cause full-blown necrosis of the incus process, which in some cases may occur as late as after 10 years [27, 28].
In recent years, efforts have been made to simplify the method of fixing the prosthesis to the long process of the incus with the help of improved prostheses. In 2000, Daniel à Wengen for the first time used a prosthesis which is fixed to the long process of the incus simply by slipping it on carefully and which is held in place by the tension of the prosthesis itself [16, 29]. With this so-called clip prosthesis, crimping is no longer necessary. The prosthesis was further developed by Eiber and Schimanski until it reached the form of the Soft CliP Piston [15].
Apart from the design of the prosthesis as such, enhanced bio-materials have been used in the development of the prosthesis, which also aim at simplifying crimping. One of the materials used is Nitinol, the most widely known of the “shape memory alloys”. Thanks to its shape memory, superelasticity and good damping capacity, Nitinol is particularly well-suited for the development of alloplastic prostheses. Depending on the temperature, Nitinol can assume two different structures. After deformation, Nitinol can reassume its default shape (defined at production) when heated. Superelasticity is another outstanding property of Nitinol.
In the present study, we used a Nitinol prosthesis with superelastic properties. Thanks to this superelasticity, only minimal pressure is required so slip the prosthesis over the long process of the incus, and the Nitinol band fits snugly around the long process of the incus without further crimping.
The high concentration of nickel justifies the question as to any intolerance reactions and allergies. Following implantation, Nitinol forms a titanium oxide layer similar to the surfaces of pure titanium prostheses. This oxide layer largely prevents the discharge of nickel into the surrounding tissue [30, 31]. In many studies, both in vitro and in vivo, it was possible to show that nickel concentration was slightly increased in some cases but never reached toxic levels.
So far in our study, 21 patients have been treated successfully with the self-crimping superelastic Nitinol piston. Intra- or postoperative complications have not occurred. The postoperative hearing results after implantation of the prosthesis can be compared with the results after insertion of a crimping prosthesis such as the K-Piston, or the Clip prosthesis according to à Wengen, or the Soft-CliP-Piston. The evaluation of the test protocols has shown good to very good results for proper fit and handling of the prosthesis as well as the overall rating of the prosthesis system by the surgeon. However, although intraoperative handling is simple, the positioning of the prosthesis requires a sufficient degree of experience on the part of the stapes surgeon.
Due to the superelasticity of the prosthesis, it is not possible to adjust the prosthesis to anatomical variations by making minimal changes to the shape of the prosthesis. Therefore, according to our experience until now, the use of a superelastic Nitinol prosthesis cannot be recommended in case of very narrow anatomical conditions, e.g. an overhanging facial nerve.
The longest postoperative monitoring period so far has amounted to 15 months. Therefore, further testing of the hearing results of our patients is important because only these results will show if the new Nitinol prosthesis can guarantee good and firm hold to the long process of incus.
A summary of the results after insertion of a nickel titanium piston with memory properties during operative repair of otosclerosis was presented on 21/05/2009 at the 80th Annual Meeting of the Annual Meeting of the German Society of Oto-Rhino-Laryngology, Head and Neck Surgery in Rostock.
Conclusions and Clinical Relevance
Due to simple intraoperative handling, especially in placing the new Nitinol prosthesis in position, the critical work step of crimping is no longer necessary. Fixation of the prosthesis does not have to be induced by heat. Very good postoperative hearing results are achieved while the rate of intraoperative complications is low. However, the positioning of the prosthesis requires a sufficient degree of experience on the part of the stapes surgeon. In order to allow a precise evaluation of the results it is planned to increase the size of the patient collective and to gather long-term results.
Conflict of interest
None.
References
- 1.Shea JJ., Jr Fenestration of the oval window. Ann Otol Rhinol Laryngol. 1958;67(4):932–951. doi: 10.1177/000348945806700403. [DOI] [PubMed] [Google Scholar]
- 2.Shea JJ., Jr A personal history of stapedectomy. Am J Otol. 1998;19(5 Suppl):S2–S12. [PubMed] [Google Scholar]
- 3.Shea JJ., Jr Forty years of stapes surgery. Am J Otol. 1998;19(1):52–55. [PubMed] [Google Scholar]
- 4.House HP, Hansen MR, Al Dakhail AA, House JW. Stapedectomy versus stapedotomy: comparison of results with long-term follow-up. Laryngoscope. 2002;112(11):2046–2050. doi: 10.1097/00005537-200211000-00025. [DOI] [PubMed] [Google Scholar]
- 5.Hausler R. General history of stapedectomy. Adv Otorhinolaryngol. 2007;65:1–5. doi: 10.1159/000098661. [DOI] [PubMed] [Google Scholar]
- 6.Jovanovic S, Schonfeld U, Scherer H. “One shot” CO2 laser stapedotomy. HNO. 2006;54(11):842–850. doi: 10.1007/s00106-005-1375-2. [DOI] [PubMed] [Google Scholar]
- 7.Vincent R, Sperling NM, Oates J, Jindal M. Surgical findings and long-term hearing results in 3,050 stapedotomies for primary otosclerosis: a prospective study with the otology-neurotology database. Otol Neurotol. 2006;27(8 Suppl 2):S25–S47. doi: 10.1097/01.mao.0000235311.80066.df. [DOI] [PubMed] [Google Scholar]
- 8.Tange RA, Grolman W, Dreschler WA. Gold and titanium in the oval window: a comparison of two metal stapes prostheses. Otol Neurotol. 2004;25(2):102–105. doi: 10.1097/00129492-200403000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Tange RA, Bruijn AJ, Grolman W. Experience with a new pure gold piston in stapedotomy for cases of otosclerosis. Auris Nasus Larynx. 1998;25(3):249–253. doi: 10.1016/S0385-8146(98)00008-X. [DOI] [PubMed] [Google Scholar]
- 10.Causse JB, Causse JR, Parahy C. Stapedotomy technique and results. Am J Otol. 1985;6(1):68–71. [PubMed] [Google Scholar]
- 11.Jahnke K Dost P, Schrader M (1999) Biocompatibility studies of implants for reconstructive middle ear surgery. In: Yanagihara N, Suzuki JI (eds) Symposium on transplants in otology, Venice, Italy
- 12.Minovi A, Probst G, Dazert S. Current concepts in the surgical management of otosclerosis. HNO. 2009;57(3):273–286. doi: 10.1007/s00106-009-1888-1. [DOI] [PubMed] [Google Scholar]
- 13.Kwok P, Fisch U, Strutz J, May J. Stapes surgery: how precisely do different prostheses attach to the long process of the incus with different instruments and different surgeons? Otol Neurotol. 2002;23(3):289–295. doi: 10.1097/00129492-200205000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Huettenbrink KB, Beutner D. A new crimping device for stapedectomy prostheses. Laryngoscope. 2005;115(11):2065–2067. doi: 10.1097/01.mlg.0000177988.05547.aa. [DOI] [PubMed] [Google Scholar]
- 15.Bast F, Schrom T. First experiences with the new soft-clip piston as an alloplastic prosthesis during stapedotomy. Laryngorhinootologie. 2009;88(5):304–308. doi: 10.1055/s-0028-1100384. [DOI] [PubMed] [Google Scholar]
- 16.Wengen DF. A new self-retaining titanium clip stapes prosthesis. Adv Otorhinolaryngol. 2007;65:184–189. doi: 10.1159/000098805. [DOI] [PubMed] [Google Scholar]
- 17.Stoeckel D, Pelton A, Duerig T. Self-expanding nitinol stents: material and design considerations. Eur Radiol. 2004;14(2):292–301. doi: 10.1007/s00330-003-2022-5. [DOI] [PubMed] [Google Scholar]
- 18.Schillinger M, Sabeti S, Loewe C, Dick P, Amighi J, Mlekusch W, et al. Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery. N Engl J Med. 2006;354(18):1879–1888. doi: 10.1056/NEJMoa051303. [DOI] [PubMed] [Google Scholar]
- 19.Kasano F, Morimitsu T. Utilization of nickel-titanium shape memory alloy for stapes prosthesis. Auris Nasus Larynx. 1997;24(2):137–142. doi: 10.1016/S0385-8146(96)00026-0. [DOI] [PubMed] [Google Scholar]
- 20.Hornung J, Zenk J, Schick B, Wurm J, Iro H. First experiences with a new nickel-titanium piston with a shape memory feature. HNO. 2007;55(2):104–108. doi: 10.1007/s00106-006-1432-5. [DOI] [PubMed] [Google Scholar]
- 21.Brown KD, Gantz BJ. Hearing results after stapedotomy with a nitinol piston prosthesis. Arch Otolaryngol Head Neck Surg. 2007;133(8):758–762. doi: 10.1001/archotol.133.8.758. [DOI] [PubMed] [Google Scholar]
- 22.Rajan GP, Diaz J, Blackham R, Eikelboom RH, Atlas MD, Shelton C, et al. Eliminating the limitations of manual crimping in stapes surgery: mid-term results of 90 patients in the Nitinol stapes piston multicenter trial. Laryngoscope. 2007;117(7):1236–1239. doi: 10.1097/MLG.0b013e31805c9a5c. [DOI] [PubMed] [Google Scholar]
- 23.Knox GW, Reitan H. Shape-memory stapes prosthesis for otosclerosis surgery. Laryngoscope. 2005;115(8):1340–1346. doi: 10.1097/01.mlg.0000172274.73365.11. [DOI] [PubMed] [Google Scholar]
- 24.Hornung JA, Brase C, Bozzato A, Zenk J, Schick B, Iro H. (2009) Retrospective analysis of the results of implanting Nitinol pistons with heat-crimping piston loops in stapes surgery. Eur Arch Otorhinolaryngol 266:25–35 [DOI] [PubMed]
- 25.Babighian G, Fontana M, Caltran S, Ciccolella M, Amadori M, Zen M. The heat-activated stapes prosthesis ‘SMart’ Piston: technique and preliminary results. Adv Otorhinolaryngol. 2007;65:190–196. doi: 10.1159/000098806. [DOI] [PubMed] [Google Scholar]
- 26.Tange RA, Grolman W. An analysis of the air-bone gap closure obtained by a crimping and a non-crimping titanium stapes prosthesis in otosclerosis. Auris Nasus Larynx. 2008;35(2):181–184. doi: 10.1016/j.anl.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 27.Schobel H. Realistic early and late results after otosclerosis surgery and presentation of a technique involving almost no complications. HNO. 2004;52(12):1049–1060. doi: 10.1007/s00106-004-1161-6. [DOI] [PubMed] [Google Scholar]
- 28.Schimanski G. Erosion and necrosis of the long process of the incus after otosclerosis operation. HNO. 1997;45(9):682–689. doi: 10.1007/s001060050142. [DOI] [PubMed] [Google Scholar]
- 29.Grolman W, Tange RA. First experience with a new stapes clip piston in stapedotomy. Otol Neurotol. 2005;26(4):595–598. doi: 10.1097/01.mao.0000178132.89353.54. [DOI] [PubMed] [Google Scholar]
- 30.Zahnert T. Nitinol as a memory-metal for the coupling of stapes prostheses. HNO. 2007;55(3):158–163. doi: 10.1007/s00106-007-1543-7. [DOI] [PubMed] [Google Scholar]
- 31.Shabalovskaya SA. On the nature of the biocompatibility and on medical applications of NiTi shape memory and superelastic alloys. Biomed Mater Eng. 1996;6(4):267–289. [PubMed] [Google Scholar]