Abstract
Neuroplasticity can be defined as the ability of the nervous system to respond to intrinsic or extrinsic stimuli by reorganizing its structure, function and connections. Major advances in the understanding of neuroplasticity have to date yielded few established interventions. To advance the translation of neuroplasticity research towards clinical applications, the National Institutes of Health Blueprint for Neuroscience Research sponsored a workshop in 2009. Basic and clinical researchers in disciplines from central nervous system injury/stroke, mental/addictive disorders, paediatric/developmental disorders and neurodegeneration/ageing identified cardinal examples of neuroplasticity, underlying mechanisms, therapeutic implications and common denominators. Promising therapies that may enhance training-induced cognitive and motor learning, such as brain stimulation and neuropharmacological interventions, were identified, along with questions of how best to use this body of information to reduce human disability. Improved understanding of adaptive mechanisms at every level, from molecules to synapses, to networks, to behaviour, can be gained from iterative collaborations between basic and clinical researchers. Lessons can be gleaned from studying fields related to plasticity, such as development, critical periods, learning and response to disease. Improved means of assessing neuroplasticity in humans, including biomarkers for predicting and monitoring treatment response, are needed. Neuroplasticity occurs with many variations, in many forms, and in many contexts. However, common themes in plasticity that emerge across diverse central nervous system conditions include experience dependence, time sensitivity and the importance of motivation and attention. Integration of information across disciplines should enhance opportunities for the translation of neuroplasticity and circuit retraining research into effective clinical therapies.
Keywords: neuroplasticity, retraining, therapeutics, clinical assessment
Introduction
Twenty-seven leading scientists participated in a 2009 workshop sponsored by the National Institutes of Health Blueprint for Neuroscience Research, organized to promote opportunities for the translation of neuroplasticity and circuit retraining research into effective clinical therapies. Included were experts in neurotrauma and stroke, mental and addictive disorders, paediatric and developmental disorders and neurodegeneration and ageing. The participants identified cardinal examples of human neuroplasticity in these conditions, underlying biological substrates and mechanisms, promising interventions for promoting adaptive neuroplastic changes and measures for evaluating neuroplastic capacity and monitoring circuit engagement and reorganization. The current report surveys neuroplastic adaptations across clinical phenotypes and highlights a number of broad themes and potential future directions that may produce therapeutic interventions to reduce disability across a range of conditions (Fig. 1).
Figure 1.
Conceptual overview of the relationship between clinical phenotypes, neuroplasticity, therapeutic interventions and assessment of function.
Neuroplasticity can be broadly defined as the ability of the nervous system to respond to intrinsic and extrinsic stimuli by reorganizing its structure, function and connections; can be described at many levels, from molecular to cellular to systems to behaviour; and can occur during development, in response to the environment, in support of learning, in response to disease, or in relation to therapy. Such plasticity can be viewed as adaptive when associated with a gain in function (Cohen et al., 1997) or as maladaptive when associated with negative consequences such as loss of function or increased injury, points illustrated by animal models and some human studies (Nudo, 2006). Also, adaptive plasticity should be distinguished from compensatory behaviours, which are behaviours that arise from mechanisms different from those operative in the distributed neural networks that typically support behaviour prior to disease onset (Levin et al., 2009).
Examples of neuroplasticity in the clinical context
Injury: stroke, trauma and spinal cord injury
Among syndromes of human CNS injury, an area in which neuroplasticity has been extensively studied, is motor recovery after stroke. Motor deficits are present in a majority of patients with stroke (Rathore et al., 2002), and the degree of motor recovery can vastly influence whether or not the stroke proves disabling. This is perennially a problem of major proportions—by some estimates, 55–75% of stroke survivors still have functional limitations and reduced quality of life months after the infarct (Levin et al., 2009).
Studies of motor recovery after stroke illustrate the principle that many forms of neuroplasticity can be ongoing in parallel. Injury to a region of the motor network can result in spontaneous intra-hemispheric changes, such as in representational maps, e.g. the hand area can shift dorsally to invade the shoulder region (Nudo et al., 1996; Muellbacher et al., 2002) or face region (Weiller et al., 1993; Cramer and Crafton, 2006). At the same time, the inter-hemispheric balance can shift such that the uninjured hemisphere has supranormal activity in relation to movement (Chollet et al., 1991; Murase et al., 2004). Focal injury results in diffuse adaptive changes (Brion et al., 1989), including changes in the connections between network nodes (Grefkes et al., 2008; Sharma et al., 2009b). The molecular basis of such spontaneous adaptive changes includes a host of growth-related processes that evolve over time (Nudo, 1999; Cramer and Chopp, 2000; Carmichael et al., 2005; Wieloch and Nikolich, 2006). Similar results have been described in post-stroke recovery from non-motor deficits such as neglect (Corbetta et al., 2005) and language (Rosen et al., 2000; Saur et al., 2006), though these rely on networks that are differently distributed as compared with the motor system (Raymer et al., 2008). Cognitive recovery after stroke has been less studied and might be more influenced by diaschisis, i.e. the remote depression of function in non-injured tissue (Munoz-Cespedes et al, 2005; Baillieux et al., 2010). Restorative and rehabilitation post-stroke therapies produce a range of brain events (Buma et al., 2010) that in many instances are similar to those arising during spontaneous recovery from stroke, such as a return to a normal degree of laterality (Fig. 2). Other changes can be unique to therapy, such as new projections from neurons on the undamaged side of the brain to denervated areas of the midbrain and spinal cord (Chen et al., 2002a). In some cases, the behavioural significance of such changes is understood—a shift in inter-hemispheric balance towards the uninjured hemisphere is the sign of a distressed system. In other cases, the exact behavioural significance of a pattern of post-stroke plasticity remains unclear, such as the direction of somatotopic map shift after focal cortical injury. As such, biomarkers of adaptive plasticity (Milot and Cramer, 2008), such as those derived from transcranial magnetic stimulation and functional MRI (Fig. 2), often have to be narrowly defined in relation to the targeted outcome. For example, a measure of brain plasticity after stroke might have very different significance at different time points or after different therapies (Dobkin, 2005). Other factors suggest the need for cautious interpretation of brain plasticity measures after stroke. In some cases, a stroke can affect brain function in ways outside of study hypotheses. For example, in a patient with stroke, functional MRI of the language system might be affected by reduced attention; or transcranial magnetic stimulation, by abnormal resting tone or by excess force execution. Interpretation of functional neuroimaging data always requires great care—after stroke this is all the more true, as multiple brain systems and behaviours are often affected (Krakauer, 2006).
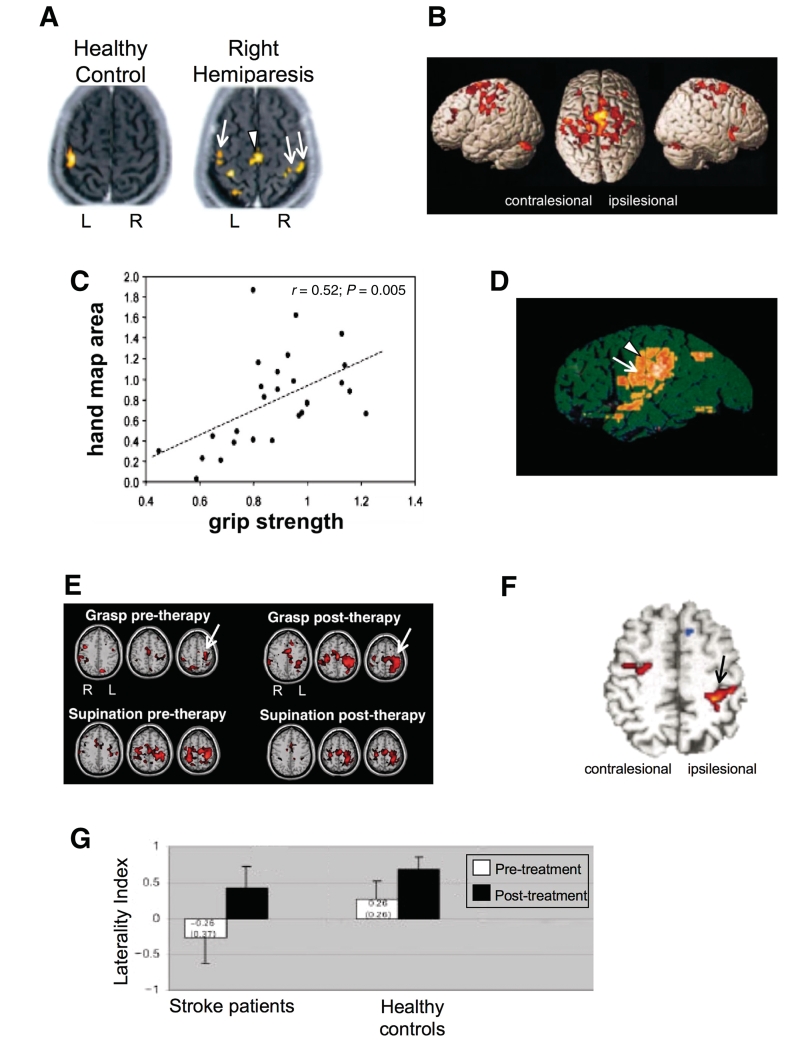
Figure 2.
Studies of the upper extremity motor system after stroke illustrate a number of forms of brain plasticity. (A–D) Brain plasticity associated with spontaneous recovery. Several patterns of change arise spontaneously during the weeks following stroke onset. Laterality is reduced. Normally, unilateral arm movement is associated with activity mainly in the contralateral hemisphere, but after a stroke, activity is often seen in both hemispheres. Activity also increases in multiple brain areas throughout the motor network. These two points are demonstrated in A by Fujii and Nakada, (2003), who used functional MRI and found that right hand grasping movements produced predominantly left motor cortex activation in a healthy control; but in a typical patient with right hemiparesis, these movements were associated with a shift in motor cortex laterality towards the right hemisphere (double arrow) as well as increased recruitment of left dorsal premotor cortex (single arrow) and bilateral supplementary motor area (arrowhead). These patterns occur along a gradient. Thus, in general, the poorer the behavioural outcome, the more these two mechanisms are invoked. For example, (B) shows data from Ward et al. (2003). Across 20 patients, those with poorer recovery were more likely to recruit a number of bilateral motor-related brain regions over and above those seen in the control group during a functional MRI grip task by the paretic hand, whereas patients with more complete recovery were more likely to have a normal pattern of brain activation. Consistent with this (C), a poorer behavioural outcome is associated with a smaller volume of excitable motor cortex. Thickbroom et al. (2004), who used transcranial magnetic stimulation, found a linear relationship between the paretic hand's grip strength and the size of its motor cortex map, each measure expressed as a ratio of values from the contralesional side. Another pattern of spontaneous post-stroke plasticity is a shift in the location of primary sensorimotor cortex activity. A number of patterns of map reorganization have been described after stroke; for the upper extremity motor representational map, a posterior or a ventral shift has been described most often. In (D), Weiller et al. (1993), using a PET measure of regional cerebral blood flow, demonstrated that in patients with capsular infarct such as the case depicted, motor cortex activity extended from the hand area (arrowhead) ventrally into the face area (arrow). (E–G) Brain plasticity associated with treatment-induced recovery. A number of training paradigms have been introduced to patients in the chronic, plateau phase of stroke. Behavioural gains in the affected arm in this context are in general associated with an increase in the volume of activity and excitability of motor cortex, as well as an increase in laterality, back towards normal, i.e. with a greater predominance of activity in stroke-affected motor cortex rather than bilateral activation. In (E), Takahashi et al. (2008), using serial functional MRI scans across 3 weeks of robot-based physiotherapy in patients with stroke affecting the left brain, found that therapy centred around right (paretic) hand grasping movements was associated with a >20-fold increase in left (stroke-affected) sensorimotor cortex (arrow); some specificity of treatment effect was apparent given absence of significant change in the map for supination, a similar but non-rehearsed task. Similar results have been described across treatment modalities. (F) Tardy et al. (2006) found that the stimulant methylphenidate improved motor performance in the paretic hand, which was paralleled by increased functional MRI activation in sites that included stroke-affected primary sensorimotor cortex (arrow). Laterality also changes with treatment. (G) Carey et al. (2002), using functional MRI, found that training of the paretic finger was associated with an increase in the primary sensorimotor cortex laterality index during performance of the trained movement. The laterality index varies from +1 (all sensorimotor cortex activation is contralateral to movement) to –1 (all activation is ipsilateral to movement). Prior to therapy, the value for stroke patients was –0.26. After therapy, the value increased to +0.43, reflecting a shift of activation towards the stroke-affected hemisphere during paretic finger movement, and matching more closely the values observed in treated healthy control subjects.
Similar forms of adaptive neuroplasticity have been described following other forms of acute CNS injury such as traumatic brain injury (Munoz-Cespedes et al., 2005; Belanger et al., 2007) and spinal cord injury (Topka et al., 1991; Cramer et al., 2005; Rosenzweig et al., 2010). Interestingly, after spinal cord injury, treatment-induced brain plasticity can be measured in the absence of behavioural change (Cramer et al., 2007b). Such data provide insight into the status of motor cortex function and might be helpful for stratifying patients for treatments, such as stem cell injections aimed at restoring voluntary motor control in patients with dense plegia after spinal cord injury. The similarity of plasticity mechanisms across divergent forms of CNS injury suggests that plasticity, as with development, uses a limited repertoire of events across numerous contexts.
Another principle is that not all plasticity has a positive impact on clinical status—in some cases, plasticity might have negative consequences. For example, new onset epilepsy is a common complication of cerebral trauma, often arising months to years after the insult. This delayed onset suggests that progressive changes in the brain, such as axonal sprouting and the formation of new connections, produce alterations in neuronal signalling and disinhibition that result in the induction of seizures (Prince et al., 2009). Other examples suggestive of maladaptive plasticity include chronic pain and allodynia following injury to a limb (such as amputation) or to CNS (dorsal spinal cord or thalamus), dystonia after various CNS injuries and autonomic dysreflexia after spinal cord injury (Karl et al., 2001). Thus, recovery from trauma or disease may reflect both adaptive and maladaptive neuroplasticity, which can occur simultaneously.
Neuropsychiatric disorders
Brain plasticity in the setting of neuropsychiatric disorders shows some similarities with that found in the setting of CNS injury such as stroke, but also shows a number of important differences. In both settings, plasticity has been described as part of the adaptation to pathology. However, the nature of the CNS pathology in neuropsychiatric disorders results in additional forms of altered brain structure and function. Mental and addictive disorders do not result from specific localizable lesions in the nervous system, in contrast to the relatively well-defined lesions that occur in stroke and trauma. Instead, these disorders are characterized by abnormalities in the distributed limbic, prefrontal and frontostriatal neural circuits that underlie motivation, perception, cognition, behaviour, social interactions and regulation of emotion (Beauregard et al., 2001). Also in contrast to stroke and trauma, the onset of mental and addictive disorders is usually insidious; the course of illness tends to be chronic or recurring/episodic; recovery in most of these disorders is slow when present; and relapse rates are high, with each episode of illness increasing the likelihood of future episodes (Patten, 2008; Robinson and Berridge, 2008). Expression of these illnesses drives change in key neural systems in the direction of ever more dysfunctional patterns underlying thoughts, emotions and complex behaviours. An important point, therefore, is that CNS plasticity, while a mechanism for achieving therapeutic gains in neuropsychiatric disorders (below) as in other settings, also has a large influence on disease pathogenesis in these disorders (Sullivan and Pfefferbaum, 2005).
Mental and addictive disorders are known to have a strong neurodevelopmental component and are associated with polygenic risk factors. However, their clinical trajectories are also experience dependent, and so heavily influenced by environmental and experiential phenomena such as stress, exposure to substance use, psychological trauma, social attachments, internal representations of self and other sociocultural influences such as the degree of early stress and of nurturing (Grossman et al., 2003; Leonardo and Hen, 2008). Prefrontal cortical association areas are particularly noteworthy in relation to clinical expression of neuropsychiatric disorders. These areas play a role in many of these environmental and experiential phenomena, as well as in social cognition, cognitive appraisal and impulse control, and are highly plastic (Lewis, 2009; Goto et al., 2010), late to myelinate (Yakovlev and Lecours, 1967) and modifiable by individual cognitive and affective experiences. Recent evidence provides further support for this at the cellular level, with prefrontal cortical neurons demonstrating synaptic plasticity and showing lasting changes in neural activity associated with divergent cognitive processes (Goto et al., 2010).
Because it is difficult to establish valid animal models for most human psychiatric illnesses, evidence for the specific role that plasticity mechanisms play in disease expression remains speculative, although compelling in a number of cases. For example, animal studies show that long-term potentiation of hippocampal–prefrontal synapses is driven by levels of mesocortical dopaminergic activity, with acute stress serving as an environmental determinant of long-term potentiation at these cortical synapses (Jay et al., 2004). The ‘kindling model’ suggests that heightened neural sensitivity to specific triggers reflects plasticity in N-methyl-d-aspartate receptor functioning in addiction (Post and Weiss, 1996) and in other neuropsychiatric disorders (Grossman et al., 2003). Also, putative schizophrenia risk genes such as those related to DISC-1, dysbindin, brain-derived neurotrophic factor and the N-methyl-d-aspartate receptor, are involved in regulating neuroplasticity, and it is possible that alterations in their expression may contribute to the abnormal patterns of cortical connectivity observed in schizophrenia (Balu and Coyle, 2011). Disturbances in dorsolateral prefrontal cortex circuitry are especially prominent in schizophrenia and may reflect direct pathology, as well as developmental plastic changes secondary to underlying disease elsewhere in the brain (Lewis and Gonzalez-Burgos, 2008). Plasticity in neuropsychiatric disease can also arise as a consequence of therapy, as in the maladaptive plasticity occurring in the form of tardive dyskinesia, associated with many antipsychotic medications, particularly first-generation drugs.
A noteworthy exception regarding the paucity of valid animal models in psychiatry is found in the addictive disorders, where a rich array of models is available for study (Shaham et al., 2003; Guo et al., 2006; Ninkovic and Bally-Cuif, 2006). An emerging synthesis from such studies is that drug abuse represents a rigid and stereotyped behavioural repertoire driven by maladaptive plasticity in subcortical reward circuitry, one that is highly resistant to reversal, making it difficult to establish new behaviours to compete with drug seeking (Kalivas, 2008; Koob and Volkow, 2010). Disruption of prefrontal regulation of subcortical limbic neural circuitry (Robinson and Kolb, 2004; Goto and Grace, 2008) and frontostriatal neural circuitry (Koob and LeMoal, 2006) is seen. Prefrontal control mechanisms are thus hijacked by subcortical reward systems in order to support the drug-seeking behaviour, with a loss of adaptive flexibility; free of inhibitory modulation imposed by prefrontal cortex, drug abuse comes under the control of evolutionarily older regions that execute fixed responses to environmental stimuli. These circuit level shifts may be explained by neuroplastic changes at the cellular level, such as loss of glutamate homoeostasis in the nucleus accumbens and loss of synaptic plasticity in striatal spiny neurons, which affect the tone of perisynaptic metabotropic glutamate receptors that are critical for long-term potentiation (Kalivas et al., 2009) and long-term depression (Kalivas et al., 2009).
At least some aspects of treatment-induced behavioural improvement in psychiatric and addictive illnesses are accompanied by plastic changes in the brain. For example, 2 years of social skills group therapy plus cognitive remediation for early schizophrenia is accompanied by significant grey matter increases in left hippocampus and left amygdala, the extent of which correlate with the degree of improved cognition (Eack et al., 2010). Deep brain stimulation that disrupts focal pathological activity in limbic-cortical circuits can reverse symptoms of treatment-resistant depression, and these antidepressant effects are associated with plasticity in downstream limbic and cortical sites (Mayberg et al., 2005). Sustained alcohol abstinence results in improvements in frontal white matter integrity (Gazdzinski et al., 2010). At the cellular level, increased hippocampal neurogenesis, potentially reflective of reparative events and thus plasticity, has been demonstrated in animal models with antidepressant medications, electroconvulsive therapy and stress reduction techniques such as environmental enrichment and exercises (Sahay and Hen, 2007). These initial findings suggest that successful treatment of mental disorders induces meaningful plasticity at the cellular level, as well as in the structure and function of frontal–subcortical neural systems.
Paediatric and developmental disorders
Paediatric congenital and acquired disorders superimpose injury on a developing nervous system that has a unique capacity for certain forms of plasticity. Injury to the developing brain can modify synaptic mechanisms, change neuronal activity, interfere with normal development and plasticity, or alter the range of activities and experiences to which a child is exposed during development. The timing of an insult, particularly with respect to age (Gardner et al., 1955; Chen et al., 2002b; Staudt, 2010) or to developmental critical periods (Cohen et al., 1999; Eyre, 2007; Jacobs et al., 2007; Johnston et al., 2009; Sharma et al., 2009a) can strongly influence the ultimate impact on plasticity and function. Many forms of neuroplasticity are at their maximum during early developmental stages that are exclusive to the developing brain. For example, cross-modal plasticity, defined as the ability of sensory maps to reorganize across afferent modalities when normal input is deprived, has been described in humans who have sustained an early neural insult (Pascual-Leone and Torres, 1993). Shifts in function from one side of the brain to the other can occur at a grand scale, with much more favourable behavioural effects in children than in adults. After large injury to a dominant left hemisphere, the right hemisphere often shows moderate to good control of language or right body movements in a child with very early insult (Staudt et al., 2002; de Bode et al., 2005), but poor control in an adult with stroke. Note too that early brain injury can impair subsequent plasticity (Failor et al., 2010).
Several hypotheses concerning the interaction of development with neuroplasticity have emerged. For example, a greater propensity for large-scale neuroplasticity in the paediatric age range (Kennard, 1942) has been hypothesized to be attributable to the overabundance of neuronal cells and synaptic connections that characterize early postnatal development, which then undergo pruning through a discrete period of experience-dependent competition. Other developmental events, such as maturation of inhibition, extracellular matrix and myelination, might also account for the closure of developmental critical periods with their unique forms of plasticity. Many of these hypotheses require further study.
Plasticity during development can also be adaptive or maladaptive. Two cardinal examples of adaptive plasticity in relation to development are the age-dependent recovery of language and motor functions following hemispherectomy for intractable epilepsy and the ability to benefit from a cochlear implant in early childhood. After hemispherectomy, the shift of language and motor functions to the non-removed hemisphere is remarkable, but highly dependent on age, with the greatest potential for reorganization seen in children under 6 years of age (Gardner et al., 1955; Chen et al., 2002b); interpretation of such plasticity measures must bear in mind that they arise in the setting of an atypical brain at baseline. Congenitally deaf children appear to benefit most from cochlear implants within the first 3.5 years of life, a time during which the central auditory pathways show maximal plasticity. Recent research shows that the latency of the early (P1) component of the cortical auditory evoked potential falls within the normal range for age among children who receive an implant by 3.5 years of age. In contrast, those who receive implants after 7 years of age show abnormal cortical responses even years after receiving the implant (Sharma et al., 2002, 2009a).
Maladaptive plasticity has been described in the setting of early sensory deprivation, which often results in an aberrant neural organization. Within the auditory system, the lack of typical experience imposed by deafness results in a failure of proper development of projections from secondary back to primary auditory areas, which weakens important feedback loops (Sharma et al., 2009a). It is likely that this decoupling makes secondary areas more available to other modalities (Kral et al., 2006). In the visual system, congenital cataracts or other optical problems that limit visual input disadvantage corresponding sensory fibres in their competition for space in the visual cortex, resulting in permanent visual deficits such as amblyopia (Awaya, 1987).
Early-onset diseases of the nervous system often affect specific cell types or neurotransmitter systems, which are reiterated across multiple brain regions and functional domains, and which are important modulators of neuroplasticity. For example, Down syndrome is associated with a general deficit of cholinergic function, several motor disorders involve alterations of dopaminergic circuitry, and epilepsy may involve deficits in GABAergic function. Likewise, hormonal (e.g. thyroid disease) and metabolic (e.g. phenylketonuria) disorders can have diffuse effects on the developing brain. Fortunately, some of these effects can be prevented with early detection and treatment. One of the most surprising findings of recent years comes from animal studies that suggest that many genetic developmental defects, including those that affect neural plasticity, can largely or completely be reversed in adult life by reversing the biochemical defect (Ehninger et al., 2008); such findings indicate that therapy may be effective in cases where it had been thought not to be so.
Neurodegeneration and ageing
Neuroplastic changes in neurodegeneration and ageing have been described, may represent pathogenic or compensatory responses, and are likely of functional consequences, at least in their earlier stages (Prvulovic et al., 2005; Palop et al., 2006; O'Brien et al., 2009). Generally speaking, neurodegenerative diseases are characterized by progressive declines in behavioural and neural function, often manifest through a pathogenic process in a maladaptive cycle. Important new research reveals that pathological molecules can directly influence neuroplasticity at the synaptic level. For example, amyloid-beta dimers, when purified from post-mortem tissue from patients with Alzheimer's disease and injected into rodents, can affect synaptic plasticity, thus establishing a possible cellular mechanism for pathology-induced plasticity in brain circuits (Shankar et al., 2008). While data derived from animal studies and human post-mortem tissue support an inverse correlation between synaptic plasticity and pathological burden (DeKosky et al., 1996), thereby suggesting that decreased plasticity may further exacerbate pathology, the direct effects of these processes in living patients have yet to be demonstrated.
Another perspective on neuroplasticity with degenerative diseases is that, with increasing pathology over time, compensatory mechanisms may fail or perhaps even become pathogenic via their effects on vulnerable neuronal populations, thereby destabilizing networks (Palop et al., 2006). Neurophysiological evidence of increased association cortex responsiveness in the early stages of Alzheimer's disease might reflect dynamic compensation for the impaired transmission of signals from primary cortex processing centres (Fernandez et al., 2007). However, over time, such compensatory activity might have detrimental consequences, possibly mediated by excitotoxic mechanisms. Similar ideas have been advanced in other neurodegenerative conditions; for example, in Huntington's disease, the high frequency of synaptic activation required to maintain medium-sized spiny neurons in an excitable state might render these cells more susceptible to cellular stress (Milnerwood and Raymond, 2010). Clarification of whether changes in neural activity are compensatory or pathogenic may hold implications for treatment, as some network dysfunctions may be reversible. Normalization of network activity might help prevent progressive neuronal loss (Palop et al., 2006).
Changes associated with neurodegenerative diseases can be superimposed on declines and reduced plasticity associated with normal ageing (Gould et al., 2006; Mahncke et al., 2006; Hertzog et al., 2009). Such age-related changes include reductions in processing speed, working memory and peripheral nervous system functions, which may be associated with changes in brain volume, white matter integrity, regional brain activation patterns and cellular function (Park and Reuter-Lorenz, 2009). Indeed, ageing may alter the genetic control of key plastic events, such as axonal sprouting after injury (Li et al., 2010). A traditional view is that ageing-related declines are a direct consequence of adverse changes in brain structure and function. An alternative view holds that such declines result, in part, from reduced engagement in cognitively demanding and stimulating tasks, degraded sensory input and/or weakened neuromodulatory control (Mahncke et al., 2006; Hertzog et al., 2009), thus opening possibilities for preventive interventions targeted towards driving brain plasticity. As people with prior neurological impairment from stroke or cerebral palsy age, their experience- and activity-induced plasticity that led to improved daily functioning may decline due to modest degradation in networks that retain less reserve than in those of healthy people.
The capacity of cognitive reserve may underlie the differential effects of neuroplasticity in ageing and the vulnerability to the detrimental effects of neurodegenerative diseases (La Rue, 2010). For instance, the common observation that the same burden of Alzheimer pathology may not impair patients' cognitive functions to the same extent is often taken as evidence of greater cognitive reserve in less impaired individuals. The effects of pathology may be clinically silent inasmuch as they are associated with the maintenance of a stable behavioural phenotype. Such adaptive plasticity might play a useful role in compensation for ageing effects (Cabeza et al., 2002; Park and Reuter-Lorenz, 2009) and may also be amenable to facilitatory interventions involving drugs (Floel et al., 2008) or non-invasive brain stimulation (Hummel et al., 2010). Moreover, recent animal studies demonstrate the profound effects that environmental enrichment can have on brain function, possibly inducing adaptive neuroplasticity and reducing key histopathological markers of neurodegeneration (Lazarov et al., 2005). However, it remains to be determined whether these strategies can be translated into treatments targeting the functional declines seen in neurodegenerative diseases.
Selected examples of neuroplasticity-based interventions
A number of promising interventions targeted towards promoting neuroplasticity are highlighted below. The examples are meant to be illustrative, rather than exhaustive. In many cases, these interventions represent application of neuroscience knowledge to rehabilitation techniques. Examples include appreciation of learning theory, Hebbian principles, task-specific training, social influences, mechanisms of verbal encoding and the interplay across brain modalities (such as influence of deafferentation on motor function). Such interventions are increasingly being applied mindful of overarching principles of neuroplasticity (Kleim and Jones, 2008). For example, plasticity after injury is often experience dependent. Thus, interventions that aim to promote plasticity can be expected to have maximum impact when coupled with optimal training and experience. Note that measuring the impact of such experiences on behavioural outcomes might require use of domain-specific measures (Cramer et al., 2007a). For example, recovery of language in a patient with post-stroke aphasia is influenced by optimal language therapy (Bhogal et al., 2003); this language recovery is better detected with a scale that is sensitive to the language domain as compared with a global scale of overall status. Also, plasticity can be time-sensitive, occur with considerable specificity, vary with the nature of the environment and be strongly influenced by the extent of concomitant training. Salience, motivation and attention can be critical modulators of plasticity (Woldag and Hummelsheim, 2002; Nithianantharajah and Hannan, 2006; Kleim and Jones, 2008). Skills training illustrates a direct example of harnessing neuroplasticity to achieve clinical gains; training on selected skills has been found to improve behavioural outcomes in parallel with increased brain plasticity, in the setting of numerous forms of CNS disease. The extent to which outcomes can be improved on the backbone of such training and plasticity depends on availability of sufficient residual neural resources, regardless of the type or duration of the neurological insult (Riley et al., 2011). A major challenge, as discussed below, is to match the right patients with the right training approach.
The pursuit of neuroplasticity-based interventions benefits from strong collaborations between basic and clinical researchers (Hachinski et al., 2010), from preclinical investigations to clinical trials. For example, clinical scientists can better understand the limitations and assumptions in the animal models; basic researchers, in turn, can return to the lab to ask pivotal questions upon informed review of early phase human studies. Such an approach stands to provide the best understanding of plasticity mechanisms, from genes to molecules to cells to networks to behaviour.
Non-invasive brain stimulation
Several forms of non-invasive brain stimulation have been examined as a means to change brain function and thereby promote neuroplasticity (Webster et al., 2006; Plow et al., 2009). Chief among these is transcranial magnetic stimulation. Introduced in the mid-1980s, transcranial magnetic stimulation uses an extracranial magnetic coil to induce current in the cerebral cortex (Wagner et al., 2007). Although transcranial magnetic stimulation activates a mixed population of inhibitory and excitatory cortical interneurons, in general, continuous trains of low frequency (<1 Hz) repetitive transcranial magnetic stimulation or theta burst transcranial magnetic stimulation lead to suppression of cortical excitability in healthy subjects, while intermittent, bursting high frequency (>1 Hz) trains of repetitive transcranial magnetic stimulation or intermittent theta burst transcranial magnetic stimulation lead to facilitation (Wagner et al., 2007). Transcranial magnetic stimulation can be applied specifically and selectively to defined cortical regions, particularly when guided by neuroimaging and physiological measures (Neggers et al., 2004; Kleim et al., 2007). Transcranial direct current stimulation uses two scalp electrodes to induce low-amplitude direct currents strong enough to penetrate the brain and modify membrane potentials, thereby influencing neuronal excitability, but without triggering the depolarization of neurons (Wagner et al., 2007). Both techniques can produce effects that are ‘offline’, i.e. that endure beyond the period of stimulation (Fregni and Pascual-Leone, 2007; Reis et al., 2009). The optimal stimulation paradigms and the best means of behavioural reinforcement require further study.
Several strategies build on the basic capacity of stimulation to modulate brain activity. Combination therapies, such as adding concomitant pharmacological or peripheral nerve stimulation, have the potential to further drive Hebbian plasticity (Conforto et al., 2010) and are under study. Also, combination with imagery or behavioural intervention has the potential to increase the efficacy of neuromodulation (Edwards et al., 2009). Another set of approaches builds on the model that, following stroke, cortical excitability is decreased in the ipsilesional hemisphere as a result of increased transcallosal inhibition from the contralesional hemisphere and increased in the contralesional hemisphere (Murase et al., 2004; Nowak et al., 2009). Building on this model, enhancing excitability of the affected hemisphere using high-frequency repetitive transcranial magnetic stimulation or suppressing the contralesional hemisphere via low-frequency repetitive transcranial magnetic stimulation or cathodal transcranial direct current stimulation appears in initial studies to promote gains in motor function, at least among patients with mild to moderate impairment (Fregni and Pascual-Leone, 2007). Promising initial results have also been reported with this approach in the treatment of other neurological domains, such as aphasia (Martin et al., 2004).
The ability of repetitive transcranial magnetic stimulation to induce electrical stimulation in cortex and the hypothesis that it might produce anti-depressant effects similar to electroconvulsive therapy has resulted in several studies on its efficacy for depression. Daily prefrontal transcranial magnetic stimulation for several weeks has been shown to have significant antidepressant effects, but additional work is needed to optimize protocols and establish and improve effect sizes (O'Reardon et al., 2007; Padberg and George, 2009). Importantly, repetitive transcranial magnetic stimulation effects have been shown to spread to distal anatomically connected structures across specific networks, including deeper striatal and limbic structures (Speer et al., 2009). Thus, cortical stimulation might induce plastic changes in cortex directly or indirectly by modifying activity in basal ganglia networks. A key principle in neuroplasticity is the value of coupling a plasticity-promoting intervention with behavioural reinforcement; further efforts in this regard might maximize the impact of repetitive transcranial magnetic stimulation on depression.
The ability of repetitive transcranial magnetic stimulation to induce changes in cortical function has also been examined in schizophrenia. The left temporoparietal cortex is one of several regions whose overactivity is associated with the perception of external voices in hallucinating patients. Low-frequency stimulation of temporoparietal cortex has been used experimentally to inhibit cortical excitability and thereby quell severe, treatment-resistant auditory hallucinations with some success (Hoffman et al., 2007; Stanford et al., 2008; Bagati et al., 2009; Vercammen et al., 2009). However, these studies are characterized by small sample sizes and some methodological inconsistencies, making it difficult—at this point in time—to compare study findings and draw definitive conclusions about the precise mechanisms and utility of low-frequency repetitive transcranial magnetic stimulation for the treatment of hallucinations.
Deep brain stimulation
Like transcranial magnetic stimulation, deep brain stimulation uses electrical stimulation to induce neuroplasticity and produce behavioural changes, although with deep brain stimulation, electrical current is provided through implanted electrodes. Stimulation parameters such as frequency, intensity and pulse width are programmable and can be optimized (Denys and Mantione, 2009). Two generally hypothesized mechanisms of action are that deep brain stimulation creates a functional lesion via inhibition within the stimulated region and, alternatively, that deep brain stimulation activates the neuronal network connected to the stimulated region, leading to modulation of pathological network activity (Johnson et al., 2008). The former mechanism is more consistent with the immediate effects of some applications of deep brain stimulation (e.g. effects on motor function in Parkinson's disease), while the latter may be more consistent with deep brain stimulation-induced gradual effects (e.g. circuit retraining) as seen in neuropsychiatric disorders.
Following increased use of deep brain stimulation in Parkinson's disease and reports of its effects on emotion, interest in its application to severe, treatment-resistant mental disorders has grown. A challenge in using deep brain stimulation for disorders of mood, thought and behaviour is the identification of appropriate and optimal stimulation sites. Although a primate model (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine, also known as MPTP) has been useful for defining a stimulation site in Parkinson's disorder, animal models have generally been of limited value in psychiatry. Human neuroimaging and prior lesioning studies have thus been very useful in identifying putative deep brain stimulation targets that may be appropriate for treating psychiatric disorders (Greenberg et al., 2010b). In mood and anxiety disorders, human neuroimaging studies have generally highlighted prefrontal cortex, subcallosal cingulate cortex (Brodmann area 25), hippocampus and amygdala as dysregulated. Preliminary studies of deep brain stimulation targeting the subcallosal cortex (Brodmann area 25) and its adjacent white matter tracts have shown promise in treating depression, suggesting that disruption of the pathological limbic-cortical circuit may ameliorate treatment-resistant depression (Mayberg et al., 2005; Lozano et al., 2008). Similar response rates have also been shown with stimulation of both the nucleus accumbens and anterior limb of the internal capsule (Malone et al., 2009; Bewernick et al., 2010), findings that also require further study.
Deep brain stimulation is also showing promise as a potential treatment for refractory obsessive-compulsive disorder, thought to involve overactivity of cortico-striatal-limbic circuits. Deep brain stimulation produced substantial behavioural improvements in at least half of the 60 subjects with obsessive–compulsive disorder studied over 10 years (Denys and Mantione, 2009). The most common target in obsessive–compulsive disorder has been the internal capsule (Greenberg et al., 2010a) extending into the ventral striatum, based on positive experiences with gamma capsulotomy and functional neuroimaging findings. Use in the related Tourette's syndrome is more limited, but has targeted the medial thalamus and the globus pallidus internus, the latter based on studies in hyperkinetic states such as dystonia and dyskinesias of Parkinson's disease (Larson, 2008).
As with many forms of plasticity, behavioural gains depend on continued therapeutic exposure. Thus, while improvement in depression and obsessive-compulsive disorder symptoms are progressive over months of chronic deep brain stimulation, they worsen progressively with termination of stimulation, although some metabolic changes linger after chronic deep brain stimulation (Lujan et al., 2008). This supports the contention that deep brain stimulation can induce some long-term neuroplastic changes in neuropsychiatric disorders. Whether durable changes that survive ongoing stimulation are possible remains to be established.
Other forms of invasive brain stimulation are under study. Activity-dependent stimulation is a promising new modality for inducing plasticity. An electronic circuit that used neural activity recorded at one cortical site to trigger stimuli delivered at another site in freely behaving primates produced long-term changes in neural connections (Jackson et al., 2006). The conditioning effects depended on the delay between the recorded action potentials and the stimuli, indicating a spike-timing dependent Hebbian plasticity. Negative findings have been described in a phase III trial of a different form of stimulation, epidural. Epidural motor cortex stimulation combined with physiotherapy was not found to be superior to physiotherapy alone for improvement of upper extremity motor deficits in patients with chronic stroke (Levy et al., 2008).
Neuropharmacology
The cellular and molecular events that underlie neuroplasticity occur on the backbone of specific neurochemical processes that are accessible and vulnerable to pharmacological interventions (Floel and Cohen, 2010). Pharmacotherapies can increase neuroplasticity through molecular manipulation of numerous cellular and synaptic pathways, such as HDAC inhibitors, mTOR inhibitors and trkB agonists (Vecsey et al., 2007; Potter et al., 2010). They appear to be especially promising when used to augment circuit-specific training, i.e. to enhance experience-dependent neuroplasticity. One clear example is the ability of d-cycloserine to significantly augment the effects of exposure/extinction therapy for anxiety disorders by facilitating the activation of N-methyl-d-aspartate glutamate receptors (Ressler et al., 2004). The systems and behavioural level responses to treatments that promote neuroplasticity have been well reviewed elsewhere (Buonomano and Merzenich, 1998; Strangman et al., 2005; Hodics et al., 2006; Penner et al., 2006; Frewen et al., 2008; Rosser and Floel, 2008; Swart et al., 2009). A number of studies have provided mechanistic insights into these pharmacological effects. For example, Pariente et al. (2001), using functional MRI, found that administration of fluoxetine to patients with stroke improved motor function in parallel with increased activation in the ipsilesional motor cortex.
Many of the above principles of plasticity extend to pharmacological approaches. For example, pharmacological targets can vary over time, and plasticity can change with experience and environment (Woldag and Hummelsheim, 2002; Nithianantharajah and Hannan, 2006; Kleim and Jones, 2008). In some cases, a drug has larger effects on plasticity and behavioural gains when paired with specific activities, such as with animal models of motor deficits after CNS injury (Feeney et al., 1982; Garcia-Alias et al., 2009), or with combined use of medication and cognitive-behavioural psychotherapy in the treatment of human depression (DeRubeis et al., 2008). It is important to note that the molecular mechanisms that support plasticity also have pharmacological vulnerabilities. Behavioural gains induced by plasticity-promoting pharmacological interventions can be lost, for example, with N-methyl-d-aspartate blockade or increased GABAergic tone. Indeed, many classes of drugs can retard neuroplasticity (Feeney et al., 1982; Butefisch et al., 2000) and possibly reduce behavioural gains (Goldstein and Sygen in Acute Stroke Study Investigators, 1995; Lazar et al., 2003).
Physical training and exercise
Following injury to the brain or spinal cord that induces motor deficits, many physical rehabilitation interventions have been reported to induce functional improvements. Constraint-induced movement therapy for the arm and hand (Wolf et al., 2007), body weight-supported treadmill training (Dobkin et al., 2006; Duncan et al., 2007), robotic devices (Volpe et al., 2008; Hidler et al., 2009; Housman et al., 2009; Lo et al., 2010), behavioural shaping, bilateral arm training (Lin et al., 2010) and task-oriented physical therapy (Jonsdottir et al., 2010) are all examples of interventions that have led to improved recovery following stroke. In some cases, functional neuroimaging studies have provided insights into mechanisms of treatment effects; for example, constraint-induced movement therapy of the upper extremity has been associated with an enlarged motor cortex map for the hand (Sawaki et al., 2008) as well as with bilateral increases in sensorimotor grey matter (Gauthier et al., 2008). However, the more complex training interventions, such as the use or robotic devices and treadmill locomotor training, generally have not improved outcomes more than conventional task related and strengthening therapies that also aim to optimize activity-dependent plasticity. Likewise, among patients with incomplete spinal cord injury, training through robotic-assisted and body weight-supported techniques have improved walking only to a similar degree as standard over-ground training (Dobkin, 2007). Further research is needed to better understand how these therapies can be coordinated and optimized, especially across diverse patient groups with varied functional limitations. Practice strategies include increased repetition, sensory priming, visualization, modulation of attentional valence and reward, contextual interference, variable demand and intensity levels, blocked versus intermittent practice and various forms of feedback (Kwakkel et al., 1999; Subramanian et al., 2010). Although these practice paradigms may enhance both skills and declarative learning in healthy subjects, their additive benefits for patients with impaired movement or cognition has been difficult to demonstrate. Note that physical rehabilitation training is not only a stand-alone therapy, but serves as an adjunct to other forms of therapy such as pharmacological and behavioural.
Aerobic exercise is a specific extension of activity-based therapies for promoting plasticity. Although the benefits of aerobic exercise in preventing or reversing cognitive and neural deterioration have yet to be fully investigated, substantial human and preclinical data support the utility of such exercise for promoting brain plasticity and improving CNS function in many conditions (Cotman and Berchtold, 2002; Hillman et al., 2008), including normal ageing and early dementia. Aerobic exercise is associated with increased neurogenesis and angiogenesis, as well as the production of neurotrophic molecules such as brain-derived neurotrophic factor and other growth factors involved in neuroprotection and the promotion of cell survival, neurite outgrowth and synaptic plasticity (Cotman and Berchtold, 2002; Gomez-Pinilla et al., 2002; Farmer et al., 2004; Kramer and Erickson, 2007; Rhyu et al., 2010). In humans, neuroimaging studies have described a range of anatomic and functional correlates of such effects (Dustman et al., 1990; Colcombe et al., 2003; Pereira et al., 2007; Pontifex et al., 2009; Pajonk et al., 2010). Furthermore, these plasticity-promoting strategies are able to produce clinically significant changes. For example, aerobic exercise programmes lasting even just a few months significantly benefit cognitive functioning in both healthy ageing and early dementia, may be of benefit in schizophrenia (Colcombe et al., 2004; Kramer and Erickson, 2007), and have been shown to increase brain volume in a variety of regions (Colcombe et al., 2006; Pajonk et al., 2010) and to enhance brain network functioning (Colcombe et al., 2004).
Cognitive training
Cognitive training can be thought of as a direct extension of physical therapy to the non-motor aspects of the human brain and so has been examined across a number of disease conditions. However, the complexities of the distributed neural systems that underlie human behavioural syndromes introduce unique challenges for the design of effective interventions. In depression and anxiety disorders, a long tradition of evidence-based cognitive-behaviour therapy is based on the principle of identifying and modifying top-down responses to maladaptive cognition, affect and behaviour (Beck, 2005; Walkup et al., 2008). Evidence suggests that, as individuals learn to modify their cognitive representations and behavioural responses to distressing stimuli, widespread changes occur in frontal cognitive control systems and in limbic system activation (Goldapple et al., 2004; Kennedy et al., 2007; Farb et al., 2010).
New neuroscience-driven approaches to cognitive training are emerging and directly build on decades of animal research that have identified principles of harnessing plasticity mechanisms in the adult brain (Nudo et al., 1996; Buonomano and Merzenich, 1998). For example, the cognitive deficits of schizophrenia—particularly in verbal learning and memory—are associated with illness severity and predict long-term functioning, but do not respond to currently available medications. Vinogradov et al. (2008), guided by an understanding of the neurobiology of schizophrenia, performed a double-blind randomized controlled trial of intensive computerized cognitive training exercises that focus on the components of auditory and verbal processing that underlie verbal encoding. This intervention was associated with improved verbal memory in patients, as well as magnetoencephalographic evidence of increased amplitude of the M100 response to auditory stimuli, indicating plasticity in auditory cortex (Dale et al., 2010). These findings require replication with a larger, preferably multi-site, study. Another cognitive-based, neuroscience-driven training approach aims to stimulate specific dysfunctional circuits, possibly in association with pharmacological intervention, in order to restore the integrity of frontostriatal circuitry in addiction (Packard, 2009).
Neuroimaging can contribute to cognitive training in a number of ways. Functional brain imaging can help to identify the neural correlates of various core mental processes such as interference control that can be targeted by cognitive training and that are relevant for a number of psychiatric disorders (Dahlin et al., 2008; Persson and Reuter-Lorenz, 2008). Neuroimaging data can also be used as biomarkers, i.e. surrogate markers. A surrogate marker has been defined as ‘a laboratory measurement… used as a substitute for a clinically meaningful endpoint’ (Temple, 1995). For example, changes in functional MRI brain activation have been shown to correlate with functional gains in studies that employed cognitive training in the setting of schizophrenia (Farb et al., 2010; Haut et al., 2010), dyslexia (Temple et al., 2003) and depression (Farb et al., 2010), consistent with observations in studies that employed direct instructional approaches (Aylward et al., 2003; Eden et al., 2004; Keller and Just, 2009). Such imaging biomarkers might prove useful as predictors of clinical outcome, and a number of MRI and PET measures are under study in this regard (Rosenberg and Hillis, 2009). Neuroimaging can also provide molecular insights into treatment mechanism. For example, McNab et al. (2009) found that cognitive training in healthy subjects was associated with changes in the density of cortical dopamine D1 receptors on PET scanning, a finding relevant to the treatment of children with attention deficit disorder (Klingberg et al., 2005). PET has also been used to describe changes in glucose metabolism associated with cognitive-behavioural or pharmacological treatment of depression (Goldapple et al., 2004; Kennedy et al., 2007). Though promising on a number of fronts, a number of issues remain to be addressed to maximize the impact of neuroimaging on cognitive training. Most imaging work has been performed on small samples, with differing approaches across labs, such as in relation to the underlying hypotheses of mechanisms of training-induced change, and further study is needed regarding the validity and reliability of neuroimaging data. Critically important is the question of whether changes in circuit strength demonstrated using neuroimaging are paralleled by meaningful behavioural changes.
The ultimate goal of cognitive training is to improve behaviour by systematically harnessing neuroplasticity and driving adaptive changes in dysfunctional neural systems through carefully designed exercises. Note that cognitive training approaches have particularly broad potential, for example, as part of rehabilitation therapy of patients with focal brain injury such as stroke, where myriad cognitive syndromes exist with few treatment options, as well as in the treatment of numerous neuropsychiatric disorders such as depression and schizophrenia. Systems neuroscience-informed cognitive training appears to be a promising treatment approach for a number of brain disorders. A key future direction for this field will be to maximize the extent to which cognitive training in one domain generalizes to others, and the extent to which such training has a meaningful impact on real-world functioning as well as the subjective experience of the individual (Green and Bavelier, 2008).
Feedback using real-time functional magnetic resonance imaging
A central challenge to creating neuroplastic change is determining how to target plasticity to a particular brain system. Such targeting might be enabled by the ability to monitor changes in brain activation within localized brain regions in real time. Recent advances in neuroimaging and computing have enabled the development of such methods based on functional MRI-based measures of regional brain activation (Cox et al., 1995). These methods now offer the possibility of allowing individuals to view real-time measures of their own regional brain activation (deCharms, 2008). Rapid feedback of regional activation level or of distributed patterns of brain activation might provide a novel means of instructing subjects on how to modulate their own brain function. Goals of such feedback include modulation of activity in specific brain regions in response to intrinsic or extrinsic cues, as well evaluation of the effects of various interventions.
Data suggest that subjects can indeed learn volitional control over a specific brain region. For example, healthy subjects can be taught to control brain activity within the anterior insula (Caria et al., 2007). In another study, both healthy subjects and patients with chronic pain were able to use real time functional MRI training to learn to control activation of brain regions involved in modulation of pain, which was associated with a concomitant decrease in pain perception (deCharms et al., 2005). The long-term goal is to improve patient outcomes by modulating brain activity in those selected neural circuits that are most related to the target symptoms.
Assessing neuroplastic capacity and monitoring circuit reorganization
Although a number of smaller studies appear to promote clinically relevant neuroplasticity, in most cases compelling evidence from large studies or clinical trials is still needed. The fundamental need in harnessing neuroplasticity for clinical applications is to reliably demonstrate behavioural improvements in human populations. This goal would be aided by validation of (i) prognostic indicators to identify those individuals with capacity for neuroplasticity, i.e. those most likely to respond to an intervention; and (ii) surrogate markers of efficacy to assist clinical trials. Numerous probes exist to assess the nervous system in this regard (Endres et al., 2008), many of which have been discussed above. Transcranial magnetic stimulation can provide insight into many cortical functions, inhibitory tone, pharmacological effects and neurophysiology, can produce virtual lesions, and can generate enduring effects on cortical function. PET can measure a multitude of brain functions, perfusion and metabolism and provide specific molecular insights. MRI can provide information on brain structure, function, perfusion, white matter integrity, tractography and network connectivity. Connectivity has been discussed above in relation to stroke (Grefkes et al., 2008; Sharma et al., 2009b), schizophrenia (Balu and Coyle, 2011) and movement disorders (Johnson et al., 2008). Emerging functional connectivity MRI methods provide information about the strength of connections across multiple distributed networks, such as emotion, motor and cognitive, in parallel, and so might be of high value in the future, unifying concepts across divergent conditions related to neuroplasticity.
Regarding predictors, one approach that might be of particular merit is the evaluation of reserve, which can be operationalized as the ability to improve performance given optimized conditions or training. In clinical practice, treatment of many organ systems is defined by a measure of organ structure or function rather than behavioural assessment, such as treatment of hypothyroidism. Also, treatment is often best prescribed when organ function is observed in response to a challenge, such as triage of patients with coronary artery disease in response to exercise or treatment of asthma based on response to methacholine; a random serum cortisol does not have nearly the information as the change in cortisol in response to adrenocorticotropic hormone infusion. These same principles are being extended to studies of therapies that promote neuroplasticity. Thus, measuring function (Cramer et al., 2007c) or injury (Stinear et al., 2007) at baseline or in response to a brief challenge (Koski et al., 2004) have each been found in small studies to have utility for predicting response to subsequent plasticity-promoting therapy.
Surrogate endpoints of clinically relevant neuroplasticity might help establish the clinical utility of therapies under study. This was considered above, where many of the candidate methods for obtaining such measures were described. One important consideration for a surrogate marker is the extent to which the method can be directly translated from animal to human studies, as is the case for some transcranial magnetic stimulation (Oberman et al., 2010) and MRI methodologies (van Meer and Dijkhuizen, 2010). Other points are that a surrogate measure has reduced utility when it is not in the causal pathway of the disease process, when the therapy selectively affects physiology of the surrogate, or when the surrogate measure does not fully capture the net effect of therapy on the clinical outcome (Fleming and DeMets, 1996; Bucher et al., 1999).
Surrogate endpoints are generally easier to measure and standardize and save time compared with most behavioural endpoints. Such markers have proved useful in phase II trials to probe biological activity of a proposed therapy, gain mechanistic insights, guide features of therapy in ways that behavioural assessment cannot, inform the decision of whether or not to proceed to Phase III, or define a target population (Fleming et al., 1994; Milot and Cramer, 2008). In the setting of neuroplasticity, a surrogate marker might be useful to demonstrate that behavioural recovery can be attributed to an anatomical or physiological change of interest (Segal et al., 2006).
Selected issues in the study of clinical neuroplasticity
A number of issues complicate the study of neuroplasticity. Many of these directly impact clinical applications. Disease can affect imaging biomarkers in numerous ways outside of study hypotheses, such as through the influence of increased head motion, reduced attention or concomitant impairments. The caveats expressed above regarding cautious interpretation of functional neuroimaging results in the setting of stroke are likely to extend to many of the neurological conditions characterized by neuroplasticity. Neurological disease and its treatment can affect many factors impacting functional neuroimaging results, either directly or indirectly. Examples include effects on attention, intention, pain threshold, behaviour during the resting state and patient strategy.
Another set of issues pertains to clinical trial design. Crossover studies are not always possible, as an intervention that promotes plasticity changes the brain, perhaps in an enduring way, and so might not allow for an independent assessment of a second intervention after crossover. Concern exists for selection bias. For example, although published multi-site trial data for constraint-induced therapy are impressive, a limited proportion of patients with stroke are eligible (Wolf et al., 2002). Indeed, it is not uncommon for plasticity trials in stroke to screen 40 patients for each one enrolled (Gladstone et al., 2006). The impairments and limitations of those enrolled may not be representative of the overall disease population. Also, in many conditions, plasticity evolves through successive temporal stages and so is time-sensitive; plasticity is in some respects a four-dimensional therapeutic target. This introduces a need to assess behaviour, biomarkers, treatment effects and more at specific time points; for example, plasticity in patients with the same disease can be quite different when assessed early after a CNS insult versus weeks later. The time course of some conditions, particularly developmental or degenerative, suggests a need to observe patients (or therapies) for years to answer a specific question related to neuroplasticity. Plasticity studies are thus particularly vulnerable to effects and biases introduced by subject dropout. However, the use of biomarkers such as imaging might improve this situation (Holland et al., 2009).
Many factors influence plasticity under healthy conditions, and CNS disease only increases the complexity of this situation. As such, a large number of covariates and their interactions sometimes must be considered. Disease strikes the CNS of each patient differently; to this point, C. Miller Fisher used to quip that ‘when it comes to stroke, there isn't a single common Englishman in all of London’. Because of these differences, influences and therapies for neuroplasticity must have a substantial effect size else large study populations are needed. In some settings, multi-site cooperative research study groups may be unavoidable. Studies of plasticity will benefit from stratifying patients and by advances in methods to identify biologically distinct subgroups.
This variability also complicates the generalization of findings. Generalization can be said to occur when therapy-induced changes ‘occur over time, persons, and settings, and the effects of the change… spread to a variety of related behaviours' (Stokes and Baer, 1977). Reduced generalization might limit the therapeutic impact of plasticity-promoting interventions. Krakauer (2006) noted that ‘recovery related to spontaneous biological processes seems to improve performance across a range of tasks whereas recovery mediated by training, like learning in healthy subjects, is more task-specific’. In response to this, some protocols can be designed to maximize generalizability (Carey and Matyas, 2005); for example, variable practice increases generalization of learning to new tasks.
Plasticity in the clinical context discussed is generally experience dependent. Both disease expression and treatment effects are influenced by a wide range of experiences, a fact that complicates study and harnessing of neuroplasticity. Measuring prior experience can be difficult, for example, in the setting of psychosis or dementia. Controlling future experience can be equally difficult, such as for a patient given a stem cell injection, the impact of which will be influenced by amount/type of subsequent rehabilitation therapy. Differences in health-care delivery systems across countries further complicate this issue. Indeed, it can be difficult to simply measure the amount of relevant experience among participants in a clinical trial of a plasticity-promoting therapy. This is not a trivial issue; in one recent, large, multi-centre, randomized, controlled trial of robotic therapy to improve arm function after stroke, 73% of participants were receiving some form of rehabilitation therapy outside of study procedures at the time of enrolment (Lo et al., 2010), and most continued this therapy during the trial. In many ways, the experience that accompanies and shapes a therapy promoting neuroplasticity is akin to the common practice of adding an adjuvant (such as a carrier protein) to achieve maximum efficacy for many vaccines.
As with many other neuroscience areas, translating neuroplasticity findings from animal models to humans can be difficult. Compared with human counterparts, studied animals usually have a younger relative age, more homogenous injury and lower frequency of comorbid conditions. Rodents are often studied but these animals are quadrupeds with prominent reliance on vibrissae, are housed in social conditions that often do not well model the human experience, and have white matter that constitutes 14% of brain volume compared with 50% in humans (Cramer, 2003; Goldberg and Ransom, 2003). The need has been emphasized for direct and enduring interactions between basic and clinical researchers to maximize translational productivity.
Conclusions and future directions
Neuroplasticity plays a significant functional and ameliorative role across a wide spectrum of brain diseases as well as in normal ageing and health. Measures of plasticity can provide insights into disease pathogenesis, improve treatment strategies and help identify substrates of treatment effects.
This report describes a number of principles of neuroplasticity common across several forms of CNS disease. Many forms of neuroplasticity can be ongoing in parallel. Neuroplasticity is often experience dependent, time-sensitive and strongly influenced by features of environment. Motivation and attention can be critical modulators of plasticity. Skills training can improve behavioural outcomes on the backbone of neuroplasticity; in many cases, maintenance of behavioural gains depends on continued therapeutic exposure. Many covariates influence neuroplasticity. Neuroplasticity does not always have a positive impact on behavioural status and can result in negative consequences in some cases. Note too that there are many important differences between CNS disorders in neuroplasticity findings, such as the temporal course and spatial distribution of the CNS disease that incites plasticity, the extent to which ageing effects interact with plasticity, the extent to which plasticity itself directly influences disease pathogenesis, and the degree to which relevant animal models are available for the study of plasticity.
Although a number of promising neuroplasticity-based interventions have been identified or are under study, many questions remain. Some of these have been described above, such as issues related to clinical trial methodology. In many cases, fundamental issues such as optimal therapy parameters and patient population require much more clarification, which might require increased reliance on multi-site research cooperative groups. Directions for future research might include tailoring plasticity-based therapies based on individual patient measurements such as functional status of residual brain circuits or distribution of disease. High-throughput methods are needed to screen potential plasticity-promoting interventions within specific networks. Most commonly, therapies under study to promote neuroplasticity have been examined one at a time, but with greater experience and understanding these therapies can be examined in combination, e.g. task-specific training coupled with stem cell therapy. An understanding of treatment mechanisms at every level will facilitate the development of preventive and therapeutic interventions. Animal models that replicate the complexity of disease mechanisms over time are needed. Ideally, such models will attend to human risk factors such as age, comorbidities and variation in patterns of pathology, and will employ ecologically valid activities. While rodent studies are well suited to investigations of cellular-molecular mechanisms, non-human primate studies may be more appropriate for understanding circuit-level changes. Because underlying biological vulnerabilities are critical for many diseases, databases determining associated genetic polymorphisms (Pearson-Fuhrhop et al., 2009) might facilitate the development of therapies aimed at altering protein functions to regulate neuroplasticity. Improved means to access the brain might allow improved CNS signal measurement as well as increased reliance on direct brain–computer interactions (Kurzweil, 2005).
For many CNS conditions, a deeper understanding of age effects on neuroplasticity is needed. Insight into critical periods, the mechanisms by which they influence circuit development, and the forces that cause them to end may be fruitful for maximizing neuroplasticity-based treatments in adults. Understanding more fully the interaction between ageing and plasticity mechanisms might be particularly useful for reducing disability in older populations.
Valid assessments of circuit engagement and reorganization, including early surrogate markers capable of predicting and monitoring treatment response, are needed. A greater understanding of what these surrogate markers reflect at the cellular–molecular level is critical. Standardization of data collection and publication would facilitate the sharing and accumulation of knowledge across studies and diseases. Through greater sharing of end points and study designs across conditions related to neuroplasticity, a higher understanding can emerge. Parallel studies in animals and humans that explicitly examine relationships between circuit-level and cellular–molecular changes may be particularly helpful. Finally, assessments of outcome should include not only behavioural and neural measurements, but also community function, quality of life, and the subjective experience of the individual.
Workshop participants
Workshop co-chairs: Steven C. Cramer, University of California, Irvine; Mriganka Sur, MIT, Judith Rumsey, NIMH. Adult trauma and stroke working group: Bruce Dobkin, UCLA and Daofen Chen, NINDS (co-chairs); Leonardo G. Cohen, NINDS; Eberhardt E. Fetz, University of Washington; Ramona Hicks, NINDS; Bryan Kolb, University of Lethbridge; Alvaro Pascual-Leone, Harvard; Nicholas Schiff, Weill Cornell. Mental and addictive disorders working group: Charles O'Brien, University of Pennsylvania, and Steven J. Grant and Minda Lynch, NIDA (co-chairs); Christopher deCharms, Omneuron, Inc.; Suzanne Haber, University of Rochester; Peter Kalivas, Medical University of South Carolina; Helen S. Mayberg, Emory; Patricia Reuter-Lorenz, University of Michigan; Sophia Vinogradov, University of California San Francisco; Pediatric and developmental disorders working group: Terence D. Sanger, University of Southern California and Ralph Nitkin, NICHD (co-chairs); Guinevere F. Eden, Georgetown; Patrick S. McQuillen and Michael Stryker, University of California at San Francisco; Anu Sharma, University of Colorado at Boulder; Lana Shekim, NIDCD. Neurodegenerative and ageing working group: John Trojanowski, University of Pennsylvania and Wen Chen, NIA (co-chairs); Judy Cameron, Oregon Health and Science University; Charles J. Duffy, University of Rochester; Emad Eskandar, Harvard/Massachusetts General Hospital; Arthur F. Kramer, University of Illinois; John Matochik, NIAAA; Michael M. Merzenich, University of California at San Francisco; Edith V. Sullivan, Stanford; ad-hoc National Institutes of Health members: Rosemarie Filart, NCRR; Michelle Freund and Michael Huerta, NIMH.
Acknowledgements
This work is based on a workshop sponsored by the National Institutes of Health Blueprint for Neuroscience Research and held in April, 2009. The views expressed herein do not necessarily represent the official views of the National Institutes of Health, the U.S. Department of Health and Human Services, or any other agency of the United States Government.
Conflict of interest: Steven Cramer has received grant support from GlaxoSmithKline, Stem Cell Therapeutics and Panasonic and has received consulting income from GlaxoSmithKline, Stem Cell Therapeutics, Pfizer, Photothera, Allergan and Asubio. Christopher deCharms is an employee and stockholder in Omneuron, Inc., a research company that develops neuroimaging approaches for diagnosing and treating neurologic and psychiatric diseases. Helen S. Mayberg holds intellectual property in the field of deep brain stimulation for depression and is a consultant for St Jude Medical. Charles O'Brien has served as a consultant in the past year to Gilead, Alkermes, Reckitt and Embera. Alvaro Pascual-Leone serves on the medical advisory board for Nexstim, Neuronix, Neosync and Starlab.
References
- Awaya S. Stimulus deprivation amblyopia in humans. In: Reinecke R, editor. Strabismus. New York: Grune and Stratton; 1987. [Google Scholar]
- Aylward EH, Richards TL, Berninger VW, Nagy WE, Field KM, Grimme AC, et al. Instructional treatment associated with changes in brain activation in children with dyslexia. Neurology. 2003;61:212–9. doi: 10.1212/01.wnl.0000068363.05974.64. [DOI] [PubMed] [Google Scholar]
- Bagati D, Nizamie SH, Prakash R. Effect of augmentatory repetitive transcranial magnetic stimulation on auditory hallucinations in schizophrenia: randomized controlled study. Aust N Z J Psychiatry. 2009;43:386–92. doi: 10.1080/00048670802653315. [DOI] [PubMed] [Google Scholar]
- Baillieux H, De Smet HJ, Dobbeleir A, Paquier PF, De Deyn PP, Marien P. Cognitive and affective disturbances following focal cerebellar damage in adults: a neuropsychological and SPECT study. Cortex. 2010;46:869–79. doi: 10.1016/j.cortex.2009.09.002. [DOI] [PubMed] [Google Scholar]
- Balu DT, Coyle JT. Neuroplasticity signaling pathways linked to the pathophysiology of schizophrenia. Neurosci Biobehav Rev. 2011;35:848–70. doi: 10.1016/j.neubiorev.2010.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauregard M, Levesque J, Bourgouin P. Neural correlates of conscious self-regulation of emotion. J Neurosci. 2001;21:RC165. doi: 10.1523/JNEUROSCI.21-18-j0001.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT. The current state of cognitive therapy: a 40-year retrospective. Arch Gen Psychiatry. 2005;62:953–9. doi: 10.1001/archpsyc.62.9.953. [DOI] [PubMed] [Google Scholar]
- Belanger HG, Vanderploeg RD, Curtiss G, Warden DL. Recent neuroimaging techniques in mild traumatic brain injury. J Neuropsychiatry Clin Neurosci. 2007;19:5–20. doi: 10.1176/jnp.2007.19.1.5. [DOI] [PubMed] [Google Scholar]
- Bewernick BH, Hurlemann R, Matusch A, Kayser S, Grubert C, Hadrysiewicz B, et al. Nucleus accumbens deep brain stimulation decreases ratings of depression and anxiety in treatment-resistant depression. Biol Psychiatry. 2010;67:110–6. doi: 10.1016/j.biopsych.2009.09.013. [DOI] [PubMed] [Google Scholar]
- Bhogal S, Teasell R, Speechley M. Intensity of aphasia therapy, impact on recovery. Stroke. 2003;34:987–93. doi: 10.1161/01.STR.0000062343.64383.D0. [DOI] [PubMed] [Google Scholar]
- Brion J-P, Demeurisse G, Capon A. Evidence of cortical reorganization in hemiparetic patients. Stroke. 1989;20:1079–84. doi: 10.1161/01.str.20.8.1079. [DOI] [PubMed] [Google Scholar]
- Bucher H, Guyatt G, Cook D, Holbrook A, McAlister F. Users' guides to the medical literature: XIX. Applying clinical trial results. A. How to use an article measuring the effect of an intervention on surrogate end points. Evidence-Based Medicine Working Group. JAMA. 1999;282:771–8. doi: 10.1001/jama.282.8.771. [DOI] [PubMed] [Google Scholar]
- Buma FE, Lindeman E, Ramsey NF, Kwakkel G. Functional Neuroimaging Studies of Early Upper Limb Recovery After Stroke: A Systematic Review of the Literature. Neurorehabil Neural Repair. 2010;24:589–608. doi: 10.1177/1545968310364058. [DOI] [PubMed] [Google Scholar]
- Buonomano DV, Merzenich MM. Cortical plasticity: from synapses to maps. Annu Rev Neurosci. 1998;21:149–86. doi: 10.1146/annurev.neuro.21.1.149. [DOI] [PubMed] [Google Scholar]
- Butefisch C, Davis B, Wise S, Sawaki L, Kopylev L, Classen J, et al. Mechanisms of use-dependent plasticity in the human motor cortex. Proc Natl Acad Sci USA. 2000;97:3661–5. doi: 10.1073/pnas.050350297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabeza R, Anderson N, Locantore J, McIntosh A. Aging gracefully: compensatory brain activity in high-performing older adults. Neuroimage. 2002;17:1394–402. doi: 10.1006/nimg.2002.1280. [DOI] [PubMed] [Google Scholar]
- Carey J, Kimberley T, Lewis S, Auerbach E, Dorsey L, Rundquist P, et al. Analysis of fMRI and finger tracking training in subjects with chronic stroke. Brain. 2002;125:773–88. doi: 10.1093/brain/awf091. [DOI] [PubMed] [Google Scholar]
- Carey LM, Matyas TA. Training of somatosensory discrimination after stroke: facilitation of stimulus generalization. Am J Phys Med Rehabil. 2005;84:428–42. doi: 10.1097/01.phm.0000159971.12096.7f. [DOI] [PubMed] [Google Scholar]
- Caria A, Veit R, Sitaram R, Lotze M, Weiskopf N, Grodd W, et al. Regulation of anterior insular cortex activity using real-time fMRI. Neuroimage. 2007;35:1238–46. doi: 10.1016/j.neuroimage.2007.01.018. [DOI] [PubMed] [Google Scholar]
- Carmichael ST, Archibeque I, Luke L, Nolan T, Momiy J, Li S. Growth-associated gene expression after stroke: evidence for a growth-promoting region in peri-infarct cortex. Exp Neurol. 2005;193:291–311. doi: 10.1016/j.expneurol.2005.01.004. [DOI] [PubMed] [Google Scholar]
- Chen P, Goldberg D, Kolb B, Lanser M, Benowitz L. Inosine induces axonal rewiring and improves behavioral outcome after stroke. Proc Natl Acad Sci USA. 2002a;99:9031–6. doi: 10.1073/pnas.132076299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R, Cohen L, Hallett M. Nervous system reorganization following injury. Neuroscience. 2002b;111:761–73. doi: 10.1016/s0306-4522(02)00025-8. [DOI] [PubMed] [Google Scholar]
- Chollet F, DiPiero V, Wise R, Brooks D, Dolan R, Frackowiak R. The functional anatomy of motor recovery after stroke in humans: A study with positron emission tomography. Ann Neurol. 1991;29:63–71. doi: 10.1002/ana.410290112. [DOI] [PubMed] [Google Scholar]
- Cohen LG, Celnik P, Pascual-Leone A, Corwell B, Falz L, Dambrosia J, et al. Functional relevance of cross-modal plasticity in blind humans. Nature. 1997;389:180–3. doi: 10.1038/38278. [DOI] [PubMed] [Google Scholar]
- Cohen LG, Weeks RA, Sadato N, Celnik P, Ishii K, Hallett M. Period of susceptibility for cross-modal plasticity in the blind. Ann Neurol. 1999;45:451–60. doi: 10.1002/1531-8249(199904)45:4<451::aid-ana6>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Colcombe SJ, Erickson KI, Raz N, Webb AG, Cohen NJ, McAuley E, et al. Aerobic fitness reduces brain tissue loss in aging humans. J Gerontol A Biol Sci Med Sci. 2003;58:176–80. doi: 10.1093/gerona/58.2.m176. [DOI] [PubMed] [Google Scholar]
- Colcombe SJ, Erickson KI, Scalf PE, Kim JS, Prakash R, McAuley E, et al. Aerobic exercise training increases brain volume in aging humans. J Gerontol A Biol Sci Med Sci. 2006;61:1166–70. doi: 10.1093/gerona/61.11.1166. [DOI] [PubMed] [Google Scholar]
- Colcombe SJ, Kramer AF, Erickson KI, Scalf P, McAuley E, Cohen NJ, et al. Cardiovascular fitness, cortical plasticity, and aging. Proc Natl Acad Sci USA. 2004;101:3316–21. doi: 10.1073/pnas.0400266101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conforto AB, Ferreiro KN, Tomasi C, dos Santos RL, Moreira VL, Marie SK, et al. Effects of somatosensory stimulation on motor function after subacute stroke. Neurorehabil Neural Repair. 2010;24:263–72. doi: 10.1177/1545968309349946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbetta M, Kincade MJ, Lewis C, Snyder AZ, Sapir A. Neural basis and recovery of spatial attention deficits in spatial neglect. Nat Neurosci. 2005;8:1603–10. doi: 10.1038/nn1574. [DOI] [PubMed] [Google Scholar]
- Cotman CW, Berchtold NC. Exercise: a behavioral intervention to enhance brain health and plasticity. Trends Neurosci. 2002;25:295–301. doi: 10.1016/s0166-2236(02)02143-4. [DOI] [PubMed] [Google Scholar]
- Cox RW, Jesmanowicz A, Hyde JS. Real-time functional magnetic resonance imaging. Magn Reson Med. 1995;33:230–6. doi: 10.1002/mrm.1910330213. [DOI] [PubMed] [Google Scholar]
- Cramer S. Clinical issues in animal models of stroke and rehabilitation. Ilar J. 2003;44:83–4. doi: 10.1093/ilar.44.2.83. [DOI] [PubMed] [Google Scholar]
- Cramer S, Chopp M. Recovery recapitulates ontogeny. Trends Neurosci. 2000;23:265–71. doi: 10.1016/s0166-2236(00)01562-9. [DOI] [PubMed] [Google Scholar]
- Cramer SC, Crafton KR. Somatotopy and movement representation sites following cortical stroke. Exp Brain Res. 2006;168:25–32. doi: 10.1007/s00221-005-0082-2. [DOI] [PubMed] [Google Scholar]
- Cramer SC, Koroshetz WJ, Finklestein SP. The case for modality-specific outcome measures in clinical trials of stroke recovery-promoting agents. Stroke. 2007a;38:1393–5. doi: 10.1161/01.STR.0000260087.67462.80. [DOI] [PubMed] [Google Scholar]
- Cramer SC, Lastra L, Lacourse MG, Cohen MJ. Brain motor system function after chronic, complete spinal cord injury. Brain. 2005;128:2941–50. doi: 10.1093/brain/awh648. [DOI] [PubMed] [Google Scholar]
- Cramer SC, Orr EL, Cohen MJ, Lacourse MG. Effects of motor imagery training after chronic, complete spinal cord injury. Exp Brain Res. 2007b;177:233–42. doi: 10.1007/s00221-006-0662-9. [DOI] [PubMed] [Google Scholar]
- Cramer SC, Parrish TB, Levy RM, Stebbins GT, Ruland SD, Lowry DW, et al. Predicting functional gains in a stroke trial. Stroke. 2007c;38:2108–14. doi: 10.1161/STROKEAHA.107.485631. [DOI] [PubMed] [Google Scholar]
- Dahlin E, Neely AS, Larsson A, Backman L, Nyberg L. Transfer of learning after updating training mediated by the striatum. Science. 2008;320:1510–2. doi: 10.1126/science.1155466. [DOI] [PubMed] [Google Scholar]
- Dale CL, Findlay AM, Adcock RA, Vertinski M, Fisher M, Genevsky A, et al. Timing is everything: neural response dynamics during syllable processing and its relation to higher-order cognition in schizophrenia and healthy comparison subjects. Int J Psychophysiol. 2010;75:183–93. doi: 10.1016/j.ijpsycho.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bode S, Firestine A, Mathern GW, Dobkin B. Residual motor control and cortical representations of function following hemispherectomy: effects of etiology. J Child Neurol. 2005;20:64–75. doi: 10.1177/08830738050200011101. [DOI] [PubMed] [Google Scholar]
- deCharms RC. Applications of real-time fMRI. Nat Rev Neurosci. 2008;9:720–9. doi: 10.1038/nrn2414. [DOI] [PubMed] [Google Scholar]
- deCharms RC, Maeda F, Glover GH, Ludlow D, Pauly JM, Soneji D, et al. Control over brain activation and pain learned by using real-time functional MRI. Proc Natl Acad Sci USA. 2005;102:18626–31. doi: 10.1073/pnas.0505210102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeKosky ST, Scheff SW, Styren SD. Structural correlates of cognition in dementia: quantification and assessment of synapse change. Neurodegeneration. 1996;5:417–21. doi: 10.1006/neur.1996.0056. [DOI] [PubMed] [Google Scholar]
- Denys D, Mantione M. Deep brain stimulation in obsessive-compulsive disorder. Prog Brain Res. 2009;175:419–27. doi: 10.1016/S0079-6123(09)17527-1. [DOI] [PubMed] [Google Scholar]
- DeRubeis RJ, Siegle GJ, Hollon SD. Cognitive therapy versus medication for depression: treatment outcomes and neural mechanisms. Nat Rev Neurosci. 2008;9:788–96. doi: 10.1038/nrn2345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobkin BH. Rehabilitation and functional neuroimaging dose-response trajectories for clinical trials. Neurorehabil Neural Repair. 2005;19:276–82. doi: 10.1177/1545968305281892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobkin BH. Confounders in rehabilitation trials of task-oriented training: lessons from the designs of the EXCITE and SCILT multicenter trials. Neurorehabil Neural Repair. 2007;21:3–13. doi: 10.1177/1545968306297329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobkin B, Apple D, Barbeau H, Basso M, Behrman A, Deforge D, et al. Weight-supported treadmill vs over-ground training for walking after acute incomplete SCI. Neurology. 2006;66:484–93. doi: 10.1212/01.wnl.0000202600.72018.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan PW, Sullivan KJ, Behrman AL, Azen SP, Wu SS, Nadeau SE, et al. Protocol for the Locomotor Experience Applied Post-stroke (LEAPS) trial: a randomized controlled trial. BMC Neurol. 2007;7:39. doi: 10.1186/1471-2377-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dustman RE, Emmerson RY, Ruhling RO, Shearer DE, Steinhaus LA, Johnson SC, et al. Age and fitness effects on EEG, ERPs, visual sensitivity, and cognition. Neurobiol Aging. 1990;11:193–200. doi: 10.1016/0197-4580(90)90545-b. [DOI] [PubMed] [Google Scholar]
- Eack SM, Hogarty GE, Cho RY, Prasad KM, Greenwald DP, Hogarty SS, et al. Neuroprotective effects of cognitive enhancement therapy against gray matter loss in early schizophrenia: results from a 2-year randomized controlled trial. Arch Gen Psychiatry. 2010;67:674–682. doi: 10.1001/archgenpsychiatry.2010.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eden GF, Jones KM, Cappell K, Gareau L, Wood FB, Zeffiro TA, et al. Neural changes following remediation in adult developmental dyslexia. Neuron. 2004;44:411–22. doi: 10.1016/j.neuron.2004.10.019. [DOI] [PubMed] [Google Scholar]
- Edwards DJ, Krebs HI, Rykman A, Zipse J, Thickbroom GW, Mastaglia FL, et al. Raised corticomotor excitability of M1 forearm area following anodal tDCS is sustained during robotic wrist therapy in chronic stroke. Restor Neurol Neurosci. 2009;27:199–207. doi: 10.3233/RNN-2009-0470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehninger D, Li W, Fox K, Stryker MP, Silva AJ. Reversing neurodevelopmental disorders in adults. Neuron. 2008;60:950–60. doi: 10.1016/j.neuron.2008.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endres M, Engelhardt B, Koistinaho J, Lindvall O, Meairs S, Mohr JP, et al. Improving outcome after stroke: overcoming the translational roadblock. Cerebrovasc Dis. 2008;25:268–78. doi: 10.1159/000118039. [DOI] [PubMed] [Google Scholar]
- Eyre JA. Corticospinal tract development and its plasticity after perinatal injury. Neurosci Biobehav Rev. 2007;31:1136–49. doi: 10.1016/j.neubiorev.2007.05.011. [DOI] [PubMed] [Google Scholar]
- Failor S, Nguyen V, Darcy DP, Cang J, Wendland MF, Stryker MP, et al. Neonatal cerebral hypoxia-ischemia impairs plasticity in rat visual cortex. J Neurosci. 2010;30:81–92. doi: 10.1523/JNEUROSCI.5656-08.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farb NA, Anderson AK, Mayberg H, Bean J, McKeon D, Segal ZV. Minding one's emotions: mindfulness training alters the neural expression of sadness. Emotion. 2010;10:25–33. doi: 10.1037/a0017151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer J, Zhao X, van Praag H, Wodtke K, Gage FH, Christie BR. Effects of voluntary exercise on synaptic plasticity and gene expression in the dentate gyrus of adult male Sprague-Dawley rats in vivo. Neuroscience. 2004;124:71–9. doi: 10.1016/j.neuroscience.2003.09.029. [DOI] [PubMed] [Google Scholar]
- Feeney D, Gonzalez A, Law W. Amphetamine, Halperidol, and experience interact to affect the rate of recovery after motor cortex injury. Science. 1982;217:855–7. doi: 10.1126/science.7100929. [DOI] [PubMed] [Google Scholar]
- Fernandez R, Kavcic V, Duffy CJ. Neurophysiologic analyses of low- and high-level visual processing in Alzheimer disease. Neurology. 2007;68:2066–76. doi: 10.1212/01.wnl.0000264873.62313.81. [DOI] [PubMed] [Google Scholar]
- Fleming T, DeMets D. Surrogate end points in clinical trials: are we being misled? Ann Intern Med. 1996;125:605–13. doi: 10.7326/0003-4819-125-7-199610010-00011. [DOI] [PubMed] [Google Scholar]
- Fleming TR, Prentice RL, Pepe MS, Glidden D. Surrogate and auxiliary endpoints in clinical trials, with potential applications in cancer and AIDS research. Stat Med. 1994;13:955–68. doi: 10.1002/sim.4780130906. [DOI] [PubMed] [Google Scholar]
- Floel A, Cohen LG. Recovery of function in humans: cortical stimulation and pharmacological treatments after stroke. Neurobiol Dis. 2010;37:243–51. doi: 10.1016/j.nbd.2009.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floel A, Garraux G, Xu B, Breitenstein C, Knecht S, Herscovitch P, et al. Levodopa increases memory encoding and dopamine release in the striatum in the elderly. Neurobiol Aging. 2008;29:267–79. doi: 10.1016/j.neurobiolaging.2006.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fregni F, Pascual-Leone A. Technology insight: noninvasive brain stimulation in neurology-perspectives on the therapeutic potential of rTMS and tDCS. Nat Clin Pract Neurol. 2007;3:383–93. doi: 10.1038/ncpneuro0530. [DOI] [PubMed] [Google Scholar]
- Frewen PA, Dozois DJ, Lanius RA. Neuroimaging studies of psychological interventions for mood and anxiety disorders: empirical and methodological review. Clin Psychol Rev. 2008;28:228–46. doi: 10.1016/j.cpr.2007.05.002. [DOI] [PubMed] [Google Scholar]
- Fujii Y, Nakada T. Cortical reorganization in patients with subcortical hemiparesis: neural mechanisms of functional recovery and prognostic implication. J Neurosurg. 2003;98:64–73. doi: 10.3171/jns.2003.98.1.0064. [DOI] [PubMed] [Google Scholar]
- Garcia-Alias G, Barkhuysen S, Buckle M, Fawcett JW. Chondroitinase ABC treatment opens a window of opportunity for task-specific rehabilitation. Nat Neurosci. 2009;12:1145–51. doi: 10.1038/nn.2377. [DOI] [PubMed] [Google Scholar]
- Gardner W, Karnosh L, McClure C, Gardner A. Residual function following hemispherectomy for tumor and for infantile hemiplegia. Brain. 1955;78:487–502. doi: 10.1093/brain/78.4.487. [DOI] [PubMed] [Google Scholar]
- Gauthier LV, Taub E, Perkins C, Ortmann M, Mark VW, Uswatte G. Remodeling the brain: plastic structural brain changes produced by different motor therapies after stroke. Stroke. 2008;39:1520–5. doi: 10.1161/STROKEAHA.107.502229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazdzinski S, Durazzo TC, Mon A, Yeh PH, Meyerhoff DJ. Cerebral white matter recovery in abstinent alcoholics–a multimodality magnetic resonance study. Brain. 2010;133:1043–53. doi: 10.1093/brain/awp343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gladstone DJ, Danells CJ, Armesto A, McIlroy WE, Staines WR, Graham SJ, et al. Physiotherapy coupled with dextroamphetamine for rehabilitation after hemiparetic stroke: a randomized, double-blind, placebo-controlled trial. Stroke. 2006;37:179–85. doi: 10.1161/01.STR.0000195169.42447.78. [DOI] [PubMed] [Google Scholar]
- Goldapple K, Segal Z, Garson C, Lau M, Bieling P, Kennedy S, et al. Modulation of cortical-limbic pathways in major depression: treatment-specific effects of cognitive behavior therapy. Arch Gen Psychiatry. 2004;61:34–41. doi: 10.1001/archpsyc.61.1.34. [DOI] [PubMed] [Google Scholar]
- Goldberg MP, Ransom BR. New light on white matter. Stroke. 2003;34:330–2. doi: 10.1161/01.str.0000054048.22626.b9. [DOI] [PubMed] [Google Scholar]
- Goldstein L Sygen in Acute Stroke Study Investigators. Common drugs may influence motor recovery after stroke. Neurology. 1995;45:865–71. doi: 10.1212/wnl.45.5.865. [DOI] [PubMed] [Google Scholar]
- Gomez-Pinilla F, Ying Z, Roy RR, Molteni R, Edgerton VR. Voluntary exercise induces a BDNF-mediated mechanism that promotes neuroplasticity. J Neurophysiol. 2002;88:2187–95. doi: 10.1152/jn.00152.2002. [DOI] [PubMed] [Google Scholar]
- Goto Y, Grace AA. Limbic and cortical information processing in the nucleus accumbens. Trends Neurosci. 2008;31:552–8. doi: 10.1016/j.tins.2008.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goto Y, Yang CR, Otani S. Functional and dysfunctional synaptic plasticity in prefrontal cortex: roles in psychiatric disorders. Biol Psychiatry. 2010;67:199–207. doi: 10.1016/j.biopsych.2009.08.026. [DOI] [PubMed] [Google Scholar]
- Gould RL, Arroyo B, Brown RG, Owen AM, Bullmore ET, Howard RJ. Brain mechanisms of successful compensation during learning in Alzheimer disease. Neurology. 2006;67:1011–7. doi: 10.1212/01.wnl.0000237534.31734.1b. [DOI] [PubMed] [Google Scholar]
- Green CS, Bavelier D. Exercising your brain: a review of human brain plasticity and training-induced learning. Psychol Aging. 2008;23:692–701. doi: 10.1037/a0014345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg BD, Gabriels LA, Malone DA, Jr, Rezai AR, Friehs GM, Okun MS, et al. Deep brain stimulation of the ventral internal capsule/ventral striatum for obsessive-compulsive disorder: worldwide experience. Mol Psychiatry. 2010a;15:64–79. doi: 10.1038/mp.2008.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg BD, Rauch SL, Haber SN. Invasive circuitry-based neurotherapeutics: stereotactic ablation and deep brain stimulation for OCD. Neuropsychopharmacology. 2010b;35:317–36. doi: 10.1038/npp.2009.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grefkes C, Nowak DA, Eickhoff SB, Dafotakis M, Kust J, Karbe H, et al. Cortical connectivity after subcortical stroke assessed with functional magnetic resonance imaging. Ann Neurol. 2008;63:236–46. doi: 10.1002/ana.21228. [DOI] [PubMed] [Google Scholar]
- Grossman AW, Churchill JD, McKinney BC, Kodish IM, Otte SL, Greenough WT. Experience effects on brain development: possible contributions to psychopathology. J Child Psychol Psychiatry. 2003;44:33–63. doi: 10.1111/1469-7610.t01-1-00102. [DOI] [PubMed] [Google Scholar]
- Guo Y, Weller P, Allard J, Usuka J, Masjedizadeh M, Wu SY, et al. Understanding our drugs and our diseases. Proc Am Thorac Soc. 2006;3:409–12. doi: 10.1513/pats.200601-014AW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hachinski V, Donnan GA, Gorelick PB, Hacke W, Cramer SC, Kaste M, et al. Stroke: working toward a prioritized world agenda. Stroke. 2010;41:1084–99. doi: 10.1161/STROKEAHA.110.586156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haut KM, Lim KO, Macdonald A., 3rd Prefrontal Cortical Changes Following Cognitive Training in Patients with Chronic Schizophrenia: Effects of Practice, Generalization, and Specificity. Neuropsychopharmacology. 2010;35:1850–9. doi: 10.1038/npp.2010.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hertzog C, Kramer AF, Wilson RS, Lindenberg U. Enrichment effects on adult cognitive development: Can the functional capacity of older adults be preserved and enhanced? Psychol Sci Public Int. 2009;9:1–65. doi: 10.1111/j.1539-6053.2009.01034.x. [DOI] [PubMed] [Google Scholar]
- Hidler J, Nichols D, Pelliccio M, Brady K, Campbell DD, Kahn JH, et al. Multicenter randomized clinical trial evaluating the effectiveness of the Lokomat in subacute stroke. Neurorehabil Neural Repair. 2009;23:5–13. doi: 10.1177/1545968308326632. [DOI] [PubMed] [Google Scholar]
- Hillman CH, Erickson KI, Kramer AF. Be smart, exercise your heart: exercise effects on brain and cognition. Nature Reviews Neuroscience. 2008;9:58–65. doi: 10.1038/nrn2298. [DOI] [PubMed] [Google Scholar]
- Hodics T, Cohen LG, Cramer SC. Functional imaging of intervention effects in stroke motor rehabilitation. Arch Phys Med Rehabil. 2006;87:S36–42. doi: 10.1016/j.apmr.2006.09.005. [DOI] [PubMed] [Google Scholar]
- Hoffman RE, Hampson M, Wu K, Anderson AW, Gore JC, Buchanan RJ, et al. Probing the pathophysiology of auditory/verbal hallucinations by combining functional magnetic resonance imaging and transcranial magnetic stimulation. Cereb Cortex. 2007;17:2733–43. doi: 10.1093/cercor/bhl183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland D, Brewer JB, Hagler DJ, Fennema-Notestine C, Dale AM. Subregional neuroanatomical change as a biomarker for Alzheimer's disease. Proc Natl Acad Sci USA. 2009;106:20954–9. doi: 10.1073/pnas.0906053106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Housman SJ, Scott KM, Reinkensmeyer DJ. A randomized controlled trial of gravity-supported, computer-enhanced arm exercise for individuals with severe hemiparesis. Neurorehabil Neural Repair. 2009;23:505–14. doi: 10.1177/1545968308331148. [DOI] [PubMed] [Google Scholar]
- Hummel FC, Heise K, Celnik P, Floel A, Gerloff C, Cohen LG. Facilitating skilled right hand motor function in older subjects by anodal polarization over the left primary motor cortex. Neurobiol Aging. 2010;31:2160–8. doi: 10.1016/j.neurobiolaging.2008.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson A, Mavoori J, Fetz EE. Long-term motor cortex plasticity induced by an electronic neural implant. Nature. 2006;444:56–60. doi: 10.1038/nature05226. [DOI] [PubMed] [Google Scholar]
- Jacobs R, Harvey AS, Anderson V. Executive function following focal frontal lobe lesions: impact of timing of lesion on outcome. Cortex. 2007;43:792–805. doi: 10.1016/s0010-9452(08)70507-0. [DOI] [PubMed] [Google Scholar]
- Jay TM, Rocher C, Hotte M, Naudon L, Gurden H, Spedding M. Plasticity at hippocampal to prefrontal cortex synapses is impaired by loss of dopamine and stress. Neurotoxicity Research. 2004;6:223–244. doi: 10.1007/BF03033225. [DOI] [PubMed] [Google Scholar]
- Johnson MD, Miocinovic S, McIntyre CC, Vitek JL. Mechanisms and targets of deep brain stimulation in movement disorders. Neurotherapeutics. 2008;5:294–308. doi: 10.1016/j.nurt.2008.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston MV, Ishida A, Ishida WN, Matsushita HB, Nishimura A, Tsuji M. Plasticity and injury in the developing brain. Brain Dev. 2009;31:1–10. doi: 10.1016/j.braindev.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonsdottir J, Cattaneo D, Recalcati M, Regola A, Rabuffetti M, Ferrarin M, et al. Task-oriented biofeedback to improve gait in individuals with chronic stroke: motor learning approach. Neurorehabil Neural Repair. 2010;24:478–85. doi: 10.1177/1545968309355986. [DOI] [PubMed] [Google Scholar]
- Kalivas PW. Addiction as a pathology in prefrontal cortical regulation of corticostriatal habit circuitry. Neurotox Res. 2008;14:185–9. doi: 10.1007/BF03033809. [DOI] [PubMed] [Google Scholar]
- Kalivas PW, Lalumiere RT, Knackstedt L, Shen H. Glutamate transmission in addiction. Neuropharmacology. 2009;56(Suppl 1):169–73. doi: 10.1016/j.neuropharm.2008.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karl A, Birbaumer N, Lutzenberger W, Cohen LG, Flor H. Reorganization of motor and somatosensory cortex in upper extremity amputees with phantom limb pain. J Neurosci. 2001;21:3609–18. doi: 10.1523/JNEUROSCI.21-10-03609.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller TA, Just MA. Altering cortical connectivity: remediation-induced changes in the white matter of poor readers. Neuron. 2009;64:624–31. doi: 10.1016/j.neuron.2009.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennard M. Cortical reorganization of motor function. Studies on series of monkeys of various ages from infancy to maturity. Arch Neurol Psychiatr. 1942;48:227–240. [Google Scholar]
- Kennedy SH, Konarski JZ, Segal ZV, Lau MA, Bieling PJ, McIntyre RS, et al. Differences in brain glucose metabolism between responders to CBT and venlafaxine in a 16-week randomized controlled trial. Am J Psychiatry. 2007;164:778–88. doi: 10.1176/ajp.2007.164.5.778. [DOI] [PubMed] [Google Scholar]
- Kleim JA, Jones TA. Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. J Speech Lang Hear Res. 2008;51:S225–39. doi: 10.1044/1092-4388(2008/018). [DOI] [PubMed] [Google Scholar]
- Kleim J, Kleim E, Cramer S. Systematic assessment of training-induced changes in corticospinal output to hand using frameless stereotaxic transcranial magnetic stimulation. Nature Protocols. 2007;2:1675–84. doi: 10.1038/nprot.2007.206. [DOI] [PubMed] [Google Scholar]
- Klingberg T, Fernell E, Olesen PJ, Johnson M, Gustafsson P, Dahlstrom K, et al. Computerized training of working memory in children with ADHD–a randomized, controlled trial. J Am Acad Child Adolesc Psychiatry. 2005;44:177–86. doi: 10.1097/00004583-200502000-00010. [DOI] [PubMed] [Google Scholar]
- Koob GF, LeMoal M. Neurobiology of addiction. London: Academic Press; 2006. [Google Scholar]
- Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35:217–38. doi: 10.1038/npp.2009.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koski L, Mernar T, Dobkin B. Immediate and long-term changes in corticomotor output in response to rehabilitation: correlation with functional improvements in chronic stroke. Neurorehabil Neural Repair. 2004;18:230–49. doi: 10.1177/1545968304269210. [DOI] [PubMed] [Google Scholar]
- Krakauer JW. Motor learning: its relevance to stroke recovery and neurorehabilitation. Curr Opin Neurol. 2006;19:84–90. doi: 10.1097/01.wco.0000200544.29915.cc. [DOI] [PubMed] [Google Scholar]
- Kral A, Tillein J, Heid S, Klinke R, Hartmann R. Cochlear implants: cortical plasticity in congenital deprivation. Prog Brain Res. 2006;157:283–313. doi: 10.1016/s0079-6123(06)57018-9. [DOI] [PubMed] [Google Scholar]
- Kramer AF, Erickson KI. Capitalizing on cortical plasticity: influence of physical activity on cognition and brain function. Trends Cogn Sci. 2007;11:342–8. doi: 10.1016/j.tics.2007.06.009. [DOI] [PubMed] [Google Scholar]
- Kurzweil R. The Singularity Is Near: When Humans Transcend Biology. New York: Penguin Group USA; 2005. [Google Scholar]
- Kwakkel G, Wagenaar R, Twisk J, Lankhorst G, Koetsier J. Intensity of leg and arm training after primary middle-cerebral-artery stroke: a randomised trial. Lancet. 1999;354:191–6. doi: 10.1016/S0140-6736(98)09477-X. [DOI] [PubMed] [Google Scholar]
- La Rue A. Healthy brain aging: role of cognitive reserve, cognitive stimulation, and cognitive exercises. Clin Geriatr Med. 2010;26:99–111. doi: 10.1016/j.cger.2009.11.003. [DOI] [PubMed] [Google Scholar]
- Larson PS. Deep brain stimulation for psychiatric disorders. Neurotherapeutics. 2008;5:50–8. doi: 10.1016/j.nurt.2007.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazar RM, Fitzsimmons BF, Marshall RS, Mohr JP, Berman MF. Midazolam challenge reinduces neurological deficits after transient ischemic attack. Stroke. 2003;34:794–6. doi: 10.1161/01.STR.0000056540.04159.F3. [DOI] [PubMed] [Google Scholar]
- Lazarov O, Robinson J, Tang YP, Hairston IS, Korade-Mirnics Z, Lee VM, et al. Environmental enrichment reduces Abeta levels and amyloid deposition in transgenic mice. Cell. 2005;120:701–13. doi: 10.1016/j.cell.2005.01.015. [DOI] [PubMed] [Google Scholar]
- Leonardo ED, Hen R. Anxiety as a developmental disorder. Neuropharmacol Rev. 2008;33:134–40. doi: 10.1038/sj.npp.1301569. [DOI] [PubMed] [Google Scholar]
- Levin MF, Kleim JA, Wolf SL. What do motor “recovery” and “compensation” mean in patients following stroke? Neurorehabil Neural Repair. 2009;23:313–9. doi: 10.1177/1545968308328727. [DOI] [PubMed] [Google Scholar]
- Levy R, Benson R, Winstein C for the Everest Study Investigators. Cortical Stimulation for Upper-Extremity Hemiparesis from Ischemic Stroke: Everest Study Primary Endpoint Results; International Stroke Conference. New Orleans, LA, 2008. [Google Scholar]
- Lewis DA. Neuroplasticity of excitatory and inhibitory cortical circuits in schizophrenia. Dialogues Clin Neurosci. 2009;11:269–80. doi: 10.31887/DCNS.2009.11.3/dalewis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis DA, Gonzalez-Burgos G. Neuroplasticity of neocortical circuits in schizophrenia. Neuropsychopharmacology. 2008;33:141–65. doi: 10.1038/sj.npp.1301563. [DOI] [PubMed] [Google Scholar]
- Li S, Overman JJ, Katsman D, Kozlov SV, Donnelly CJ, Twiss JL, et al. An age-related sprouting transcriptome provides molecular control of axonal sprouting after stroke. Nat Neurosci. 2010;13:1496–504. doi: 10.1038/nn.2674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin KC, Chen YA, Chen CL, Wu CY, Chang YF. The effects of bilateral arm training on motor control and functional performance in chronic stroke: a randomized controlled study. Neurorehabil Neural Repair. 2010;24:42–51. doi: 10.1177/1545968309345268. [DOI] [PubMed] [Google Scholar]
- Lo AC, Guarino PD, Richards LG, Haselkorn JK, Wittenberg GF, Federman DG, et al. Robot-assisted therapy for long-term upper-limb impairment after stroke. N Engl J Med. 2010;362:1772–83. doi: 10.1056/NEJMoa0911341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozano AM, Mayberg HS, Giacobbe P, Hamani C, Craddock RC, Kennedy SH. Subcallosal cingulate gyrus deep brain stimulation for treatment-resistant depression. Biol Psychiatry. 2008;64:461–7. doi: 10.1016/j.biopsych.2008.05.034. [DOI] [PubMed] [Google Scholar]
- Lujan JL, Chaturvedi A, McIntyre CC. Tracking the mechanism of deep brain stimulation for neuropsychiatric disorders. Front Biosci. 2008;13:5892–904. doi: 10.2741/3124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahncke HW, Bronstone A, Merzenich MM. Brain plasticity and functional losses in the aged: scientific bases for a novel intervention. Prog Brain Res. 2006;157:81–109. doi: 10.1016/S0079-6123(06)57006-2. [DOI] [PubMed] [Google Scholar]
- Malone DA, Jr, Dougherty DD, Rezai AR, Carpenter LL, Friehs GM, Eskandar EN, et al. Deep brain stimulation of the ventral capsule/ventral striatum for treatment-resistant depression. Biol Psychiatry. 2009;65:267–75. doi: 10.1016/j.biopsych.2008.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin P, Naeser M, Theoret H, Tormos J, Nicholas M, Kurland J, et al. Transcranial magnetic stimulation as a complementary treatment for aphasia. Semin Speech Lang. 2004;25:181–91. doi: 10.1055/s-2004-825654. [DOI] [PubMed] [Google Scholar]
- Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, et al. Deep brain stimulation for treatment-resistant depression. Neuron. 2005;45:651–60. doi: 10.1016/j.neuron.2005.02.014. [DOI] [PubMed] [Google Scholar]
- McNab F, Varrone A, Farde L, Jucaite A, Bystritsky P, Forssberg H, et al. Changes in cortical dopamine D1 receptor binding associated with cognitive training. Science. 2009;323:800–2. doi: 10.1126/science.1166102. [DOI] [PubMed] [Google Scholar]
- Milnerwood AJ, Raymond LA. Early synaptic pathophysiology in neurodegeneration: insights from Huntington's disease. Trends Neurosci. 2010;33:513–23. doi: 10.1016/j.tins.2010.08.002. [DOI] [PubMed] [Google Scholar]
- Milot MH, Cramer SC. Biomarkers of recovery after stroke. Curr Opin Neurol. 2008;21:654–9. doi: 10.1097/WCO.0b013e3283186f96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muellbacher W, Richards C, Ziemann U, Wittenberg G, Weltz D, Boroojerdi B, et al. Improving hand function in chronic stroke. Arch Neurol. 2002;59:1278–82. doi: 10.1001/archneur.59.8.1278. [DOI] [PubMed] [Google Scholar]
- Munoz-Cespedes JM, Rios-Lago M, Paul N, Maestu F. Functional neuroimaging studies of cognitive recovery after acquired brain damage in adults. Neuropsychol Rev. 2005;15:169–83. doi: 10.1007/s11065-005-9178-5. [DOI] [PubMed] [Google Scholar]
- Murase N, Duque J, Mazzocchio R, Cohen LG. Influence of interhemispheric interactions on motor function in chronic stroke. Ann Neurol. 2004;55:400–9. doi: 10.1002/ana.10848. [DOI] [PubMed] [Google Scholar]
- Neggers SF, Langerak TR, Schutter DJ, Mandl RC, Ramsey NF, Lemmens PJ, et al. A stereotactic method for image-guided transcranial magnetic stimulation validated with fMRI and motor-evoked potentials. Neuroimage. 2004;21:1805–17. doi: 10.1016/j.neuroimage.2003.12.006. [DOI] [PubMed] [Google Scholar]
- Ninkovic J, Bally-Cuif L. The zebrafish as a model system for assessing the reinforcing properties of drugs of abuse. Methods. 2006;39:262–74. doi: 10.1016/j.ymeth.2005.12.007. [DOI] [PubMed] [Google Scholar]
- Nithianantharajah J, Hannan AJ. Enriched environments, experience-dependent plasticity and disorders of the nervous system. Nat Rev Neurosci. 2006;7:697–709. doi: 10.1038/nrn1970. [DOI] [PubMed] [Google Scholar]
- Nowak DA, Grefkes C, Ameli M, Fink GR. Interhemispheric competition after stroke: brain stimulation to enhance recovery of function of the affected hand. Neurorehabil Neural Repair. 2009;23:641–56. doi: 10.1177/1545968309336661. [DOI] [PubMed] [Google Scholar]
- Nudo R. Recovery after damage to motor cortical areas. Curr Opin Neurobiol. 1999;9:740–7. doi: 10.1016/s0959-4388(99)00027-6. [DOI] [PubMed] [Google Scholar]
- Nudo RJ. Plasticity. NeuroRx. 2006;3:420–7. doi: 10.1016/j.nurx.2006.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nudo R, Wise B, SiFuentes F, Milliken G. Neural substrates for the effects of rehabilitative training on motor recovery after ischemic infarct. Science. 1996;272:1791–4. doi: 10.1126/science.272.5269.1791. [DOI] [PubMed] [Google Scholar]
- O'Brien RJ, Resnick SM, Zonderman AB, Ferrucci L, Crain BJ, Pletnikova O, et al. Neuropathologic studies of the Baltimore Longitudinal Study of Aging (BLSA) J Alzheimers Dis. 2009;18:665–75. doi: 10.3233/JAD-2009-1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Reardon JP, Solvason HB, Janicak PG, Sampson S, Isenberg KE, Nahas Z, et al. Efficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: a multisite randomized controlled trial. Biol Psychiatry. 2007;62:1208–16. doi: 10.1016/j.biopsych.2007.01.018. [DOI] [PubMed] [Google Scholar]
- Oberman L, Fritz I, Najib U, Bashir S, Woollacott I, Gonzalez-Heydrich J, et al. Transcranial magnetic stimulation provides means to assess cortical plasticity and excitability in humans with fragile X syndrome and autism spectrum disorder. Front Synaptic Neurosci. 2010;2:1–8. doi: 10.3389/fnsyn.2010.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Packard MG. Anxiety, cognition, and habit: a multiple memory systems perspective. Brain Res. 2009;1293:121–8. doi: 10.1016/j.brainres.2009.03.029. [DOI] [PubMed] [Google Scholar]
- Padberg F, George MS. Repetitive transcranial magnetic stimulation of the prefrontal cortex in depression. Exp Neurol. 2009;219:2–13. doi: 10.1016/j.expneurol.2009.04.020. [DOI] [PubMed] [Google Scholar]
- Pajonk FG, Wobrock T, Gruber O, Scherk H, Berner D, Kaizl I, et al. Hippocampal plasticity in response to exercise in schizophrenia. Arch Gen Psychiatry. 2010;67:133–43. doi: 10.1001/archgenpsychiatry.2009.193. [DOI] [PubMed] [Google Scholar]
- Palop JJ, Chin J, Mucke L. A network dysfunction perspective on neurodegenerative diseases. Nature. 2006;443:768–73. doi: 10.1038/nature05289. [DOI] [PubMed] [Google Scholar]
- Pariente J, Loubinoux I, Carel C, Albucher J, Leger A, Manelfe C, et al. Fluoxetine modulates motor performance and cerebral activation of patients recovering from stroke. Ann Neurol. 2001;50:718–29. doi: 10.1002/ana.1257. [DOI] [PubMed] [Google Scholar]
- Park DC, Reuter-Lorenz P. The adaptive brain: aging and neurocognitive scaffolding. Annu Rev Psychol. 2009;60:173–96. doi: 10.1146/annurev.psych.59.103006.093656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascual-Leone A, Torres F. Plasticity of the sensorimotor cortex representation of the reading finger in Braille readers. Brain. 1993;116(Pt 1):39–52. doi: 10.1093/brain/116.1.39. [DOI] [PubMed] [Google Scholar]
- Patten SB. Sensitization: the sine qua non of the depressive disorders? Med Hypotheses. 2008;71:872–5. doi: 10.1016/j.mehy.2008.06.040. [DOI] [PubMed] [Google Scholar]
- Pearson-Fuhrhop KM, Kleim JA, Cramer SC. Brain plasticity and genetic factors. Top Stroke Rehabil. 2009;16:282–99. doi: 10.1310/tsr1604-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner IK, Kappos L, Rausch M, Opwis K, Radu EW. Therapy-induced plasticity of cognitive functions in MS patients: insights from fMRI. J Physiol Paris. 2006;99:455–62. doi: 10.1016/j.jphysparis.2006.03.008. [DOI] [PubMed] [Google Scholar]
- Pereira AC, Huddleston DE, Brickman AM, Sosunov AA, Hen R, McKhann GM, et al. An in vivo correlate of exercise-induced neurogenesis in the adult dentate gyrus. Proc Natl Acad Sci USA. 2007;104:5638–43. doi: 10.1073/pnas.0611721104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persson J, Reuter-Lorenz PA. Gaining control: training executive function and far transfer of the ability to resolve interference. Psychol Sci. 2008;19:881–8. doi: 10.1111/j.1467-9280.2008.02172.x. [DOI] [PubMed] [Google Scholar]
- Plow EB, Carey JR, Nudo RJ, Pascual-Leone A. Invasive cortical stimulation to promote recovery of function after stroke: a critical appraisal. Stroke. 2009;40:1926–31. doi: 10.1161/STROKEAHA.108.540823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pontifex MB, Hillman CH, Polich J. Age, physical fitness, and attention: P3a and P3b. Psychophysiology. 2009;46:379–87. doi: 10.1111/j.1469-8986.2008.00782.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post RM, Weiss SR. A speculative model of affective illness cyclicity based on patterns of drug tolerance observed in amygdala-kindled seizures. Mol Neurobiol. 1996;13:33–60. doi: 10.1007/BF02740751. [DOI] [PubMed] [Google Scholar]
- Potter WB, O'Riordan KJ, Barnett D, Osting SM, Wagoner M, Burger C, et al. Metabolic regulation of neuronal plasticity by the energy sensor AMPK. PLoS ONE. 2010;5:e8996. doi: 10.1371/journal.pone.0008996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince DA, Parada I, Scalise K, Graber K, Jin X, Shen F. Epilepsy following cortical injury: cellular and molecular mechanisms as targets for potential prophylaxis. Epilepsia. 2009;50(Suppl 2):30–40. doi: 10.1111/j.1528-1167.2008.02008.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prvulovic D, Van de Ven V, Sack AT, Maurer K, Linden DE. Functional activation imaging in aging and dementia. Psychiatry Res. 2005;140:97–113. doi: 10.1016/j.pscychresns.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Rathore S, Hinn A, Cooper L, Tyroler H, Rosamond W. Characterization of incident stroke signs and symptoms: findings from the atherosclerosis risk in communities study. Stroke. 2002;33:2718–21. doi: 10.1161/01.str.0000035286.87503.31. [DOI] [PubMed] [Google Scholar]
- Raymer AM, Beeson P, Holland A, Kendall D, Maher LM, Martin N, et al. Translational research in aphasia: from neuroscience to neurorehabilitation. J Speech Lang Hear Res. 2008;51:S259–75. doi: 10.1044/1092-4388(2008/020). [DOI] [PubMed] [Google Scholar]
- Reis J, Schambra HM, Cohen LG, Buch ER, Fritsch B, Zarahn E, et al. Noninvasive cortical stimulation enhances motor skill acquisition over multiple days through an effect on consolidation. Proc Natl Acad Sci USA. 2009;106:1590–5. doi: 10.1073/pnas.0805413106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ressler KJ, Rothbaum BO, Tannenbaum L, Anderson P, Graap K, Zimand E, et al. Cognitive enhancers as adjuncts to psychotherapy: use of D-cycloserine in phobic individuals to facilitate extinction of fear. Arch Gen Psychiatry. 2004;61:1136–44. doi: 10.1001/archpsyc.61.11.1136. [DOI] [PubMed] [Google Scholar]
- Rhyu IJ, Bytheway JA, Kohler SJ, Lange H, Lee KJ, Boklewski J, et al. Effects of aerobic exercise training on cognitive function and cortical vascularity in monkeys. Neuroscience. 2010;167:1239–48. doi: 10.1016/j.neuroscience.2010.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley J, Le V, Der-Yeghiaian L, See J, Newton J, Ward N, et al. Anatomy of Stroke Injury Predicts Gains from Therapy. Stroke. 2011;42:421–6. doi: 10.1161/STROKEAHA.110.599340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson TE, Berridge KC. Review. The incentive sensitization theory of addiction: some current issues. Philos Trans R Soc Lond B Biol Sci. 2008;363:3137–46. doi: 10.1098/rstb.2008.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson TE, Kolb B. Structural plasticity associated with exposure to drugs of abuse. Neuropharmacology. 2004;47(Suppl 1):33–46. doi: 10.1016/j.neuropharm.2004.06.025. [DOI] [PubMed] [Google Scholar]
- Rosen H, Petersen S, Linenweber M, Snyder A, White D, Chapman L, et al. Neural correlates of recovery from aphasia after damage to left inferior frontal cortex. Neurology. 2000;55:1883–94. doi: 10.1212/wnl.55.12.1883. [DOI] [PubMed] [Google Scholar]
- Rosenberg PB, Hillis AE. Biomarkers for Alzheimer's disease: ready for the next step. Brain. 2009;132(Pt 8):2002–4. doi: 10.1093/brain/awp184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenzweig ES, Courtine G, Jindrich DL, Brock JH, Ferguson AR, Strand SC, et al. Extensive spontaneous plasticity of corticospinal projections after primate spinal cord injury. Nat Neurosci. 2010;13:1505–10. doi: 10.1038/nn.2691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosser N, Floel A. Pharmacological enhancement of motor recovery in subacute and chronic stroke. NeuroRehabilitation. 2008;23:95–103. [PubMed] [Google Scholar]
- Sahay A, Hen R. Adult hippocampal neurogenesis in depression. Nat Neurosci. 2007;10:1110–5. doi: 10.1038/nn1969. [DOI] [PubMed] [Google Scholar]
- Saur D, Lange R, Baumgaertner A, Schraknepper V, Willmes K, Rijntjes M, et al. Dynamics of language reorganization after stroke. Brain. 2006;129:1371–84. doi: 10.1093/brain/awl090. [DOI] [PubMed] [Google Scholar]
- Sawaki L, Butler AJ, Xiaoyan L, Wassenaar PA, Mohammad YM, Blanton S, et al. Constraint-induced movement therapy results in increased motor map area in subjects 3 to 9 months after stroke. Neurorehabil Neural Repair. 2008;22:505–13. doi: 10.1177/1545968308317531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Kennedy S, Gemar M, Hood K, Pedersen R, Buis T. Cognitive reactivity to sad mood provocation and the prediction of depressive relapse. Arch Gen Psychiatry. 2006;63:749–55. doi: 10.1001/archpsyc.63.7.749. [DOI] [PubMed] [Google Scholar]
- Shaham Y, Shalev U, Lu L, De Wit H, Stewart J. The reinstatement model of drug relapse: history, methodology and major findings. Psychopharmacology. 2003;168:3–20. doi: 10.1007/s00213-002-1224-x. [DOI] [PubMed] [Google Scholar]
- Shankar GM, Li S, Mehta TH, Garcia-Munoz A, Shepardson NE, Smith I, et al. Amyloid-beta protein dimers isolated directly from Alzheimer's brains impair synaptic plasticity and memory. Nat Med. 2008;14:837–42. doi: 10.1038/nm1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma A, Dorman MF, Spahr AJ. A sensitive period for the development of the central auditory system in children with cochlear implants: implications for age of implantation. Ear Hear. 2002;23:532–9. doi: 10.1097/00003446-200212000-00004. [DOI] [PubMed] [Google Scholar]
- Sharma A, Nash AA, Dorman M. Cortical development, plasticity and re-organization in children with cochlear implants. J Commun Disord. 2009a;42:272–9. doi: 10.1016/j.jcomdis.2009.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma N, Baron JC, Rowe JB. Motor imagery after stroke: relating outcome to motor network connectivity. Ann Neurol. 2009b;66:604–16. doi: 10.1002/ana.21810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speer AM, Benson BE, Kimbrell TK, Wassermann EM, Willis MW, Herscovitch P, et al. Opposite effects of high and low frequency rTMS on mood in depressed patients: relationship to baseline cerebral activity on PET. J Affect Disord. 2009;115:386–94. doi: 10.1016/j.jad.2008.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanford AD, Sharif Z, Corcoran C, Urban N, Malaspina D, Lisanby SH. rTMS strategies for the study and treatment of schizophrenia: a review. Int J Neuropsychopharmacol. 2008;11:563–76. doi: 10.1017/S1461145707008309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staudt M. Reorganization after pre- and perinatal brain lesions. J Anat. 2010;217:469–74. doi: 10.1111/j.1469-7580.2010.01262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staudt M, Grodd W, Gerloff C, Erb M, Stitz J, Krageloh-Mann I. Two types of ipsilateral reorganization in congenital hemiparesis: a transcranial magnetic stimulation and fMRI study. Brain. 2002;125:2222–37. doi: 10.1093/brain/awf227. [DOI] [PubMed] [Google Scholar]
- Stinear CM, Barber PA, Smale PR, Coxon JP, Fleming MK, Byblow WD. Functional potential in chronic stroke patients depends on corticospinal tract integrity. Brain. 2007;130:170–80. doi: 10.1093/brain/awl333. [DOI] [PubMed] [Google Scholar]
- Stokes TF, Baer DM. An implicit technology of generalization. J Appl Behav Anal. 1977;10:349–67. doi: 10.1901/jaba.1977.10-349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strangman G, O'Neil-Pirozzi TM, Burke D, Cristina D, Goldstein R, Rauch SL, et al. Functional neuroimaging and cognitive rehabilitation for people with traumatic brain injury. Am J Phys Med Rehabil. 2005;84:62–75. doi: 10.1097/01.phm.0000150787.26860.12. [DOI] [PubMed] [Google Scholar]
- Subramanian SK, Massie CL, Malcolm MP, Levin MF. Does provision of extrinsic feedback result in improved motor learning in the upper limb poststroke? A systematic review of the evidence. Neurorehabilitation and Neural Repair. 2010;24:113–24. doi: 10.1177/1545968309349941. [DOI] [PubMed] [Google Scholar]
- Sullivan EV, Pfefferbaum A. Neurocircuitry in alcoholism: a substrate of disruption and repair. Psychopharmacology. 2005;180:583–94. doi: 10.1007/s00213-005-2267-6. [DOI] [PubMed] [Google Scholar]
- Swart CM, Stins JF, Beek PJ. Cortical changes in complex regional pain syndrome (CRPS) Eur J Pain. 2009;13:902–7. doi: 10.1016/j.ejpain.2008.11.010. [DOI] [PubMed] [Google Scholar]
- Takahashi CD, Der-Yeghiaian L, Le V, Motiwala RR, Cramer SC. Robot-based hand motor therapy after stroke. Brain. 2008;131:425–37. doi: 10.1093/brain/awm311. [DOI] [PubMed] [Google Scholar]
- Tardy J, Pariente J, Leger A, Dechaumont-Palacin S, Gerdelat A, Guiraud V, et al. Methylphenidate modulates cerebral post-stroke reorganization. Neuroimage. 2006;33:913–22. doi: 10.1016/j.neuroimage.2006.07.014. [DOI] [PubMed] [Google Scholar]
- Temple E, Deutsch GK, Poldrack RA, Miller SL, Tallal P, Merzenich MM, et al. Neural deficits in children with dyslexia ameliorated by behavioral remediation: evidence from functional MRI. Proc Natl Acad Sci USA. 2003;100:2860–5. doi: 10.1073/pnas.0030098100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temple R. A regulatory authority's opinion about surrogate endpoints. In: Nimmo W, Tucker G, editors. Clinical Measurement in Drug Evaluation. New York: J. Wiley; 1995. [Google Scholar]
- Thickbroom GW, Byrnes ML, Archer SA, Mastaglia FL. Motor outcome after subcortical stroke correlates with the degree of cortical reorganization. Clin Neurophysiol. 2004;115:2144–50. doi: 10.1016/j.clinph.2004.04.001. [DOI] [PubMed] [Google Scholar]
- Topka H, Cohen LG, Cole RA, Hallett M. Reorganization of corticospinal pathways following spinal cord injury. Neurology. 1991;41:1276–83. doi: 10.1212/wnl.41.8.1276. [DOI] [PubMed] [Google Scholar]
- van Meer MPA, Dijkhuizen RM. Functional and Structural MR Imaging of Brain Reorganization after Stroke. In: Cramer SC, Nudo RJ, editors. Brain repair after stroke. Cambridge: Cambridge University Press; 2010. [Google Scholar]
- Vecsey CG, Hawk JD, Lattal KM, Stein JM, Fabian SA, Attner MA, et al. Histone deacetylase inhibitors enhance memory and synaptic plasticity via CREB:CBP-dependent transcriptional activation. J Neurosci. 2007;27:6128–40. doi: 10.1523/JNEUROSCI.0296-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vercammen A, Knegtering H, Bruggeman R, Westenbroek HM, Jenner JA, Slooff CJ, et al. Effects of bilateral repetitive transcranial magnetic stimulation on treatment resistant auditory-verbal hallucinations in schizophrenia: a randomized controlled trial. Schizophr Res. 2009;114:172–9. doi: 10.1016/j.schres.2009.07.013. [DOI] [PubMed] [Google Scholar]
- Vinogradov S, Luks TL, Schulman BJ, Simpson GV. Deficit in a neural correlate of reality monitoring in schizophrenia patients. Cereb Cortex. 2008;18:2532–9. doi: 10.1093/cercor/bhn028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volpe BT, Lynch D, Rykman-Berland A, Ferraro M, Galgano M, Hogan N, et al. Intensive sensorimotor arm training mediated by therapist or robot improves hemiparesis in patients with chronic stroke. Neurorehabil Neural Repair. 2008;22:305–10. doi: 10.1177/1545968307311102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner T, Valero-Cabre A, Pascual-Leone A. Noninvasive human brain stimulation. Annu Rev Biomed Eng. 2007;9:527–65. doi: 10.1146/annurev.bioeng.9.061206.133100. [DOI] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. N Engl J Med. 2008;359:2753–66. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward N, Brown M, Thompson A, Frackowiak R. Neural correlates of outcome after stroke: a cross-sectional fMRI study. Brain. 2003;126:1430–48. doi: 10.1093/brain/awg145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster BR, Celnik PA, Cohen LG. Noninvasive brain stimulation in stroke rehabilitation. NeuroRx. 2006;3:474–81. doi: 10.1016/j.nurx.2006.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiller C, Ramsay S, Wise R, Friston K, Frackowiak R. Individual patterns of functional reorganization in the human cerebral cortex after capsular infarction. Ann Neurol. 1993;33:181–9. doi: 10.1002/ana.410330208. [DOI] [PubMed] [Google Scholar]
- Wieloch T, Nikolich K. Mechanisms of neural plasticity following brain injury. Curr Opin Neurobiol. 2006;16:258–64. doi: 10.1016/j.conb.2006.05.011. [DOI] [PubMed] [Google Scholar]
- Woldag H, Hummelsheim H. Evidence-based physiotherapeutic concepts for improving arm and hand function in stroke patients: a review. J Neurol. 2002;249:518–28. doi: 10.1007/s004150200058. [DOI] [PubMed] [Google Scholar]
- Wolf S, Blanton S, Baer H, Breshears J, Butler A. Repetitive task practice: a critical review of constraint-induced movement therapy in stroke. The Neurologist. 2002;8:325–38. doi: 10.1097/01.nrl.0000031014.85777.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf SL, Newton H, Maddy D, Blanton S, Zhang Q, Winstein CJ, et al. The Excite Trial: relationship of intensity of constraint induced movement therapy to improvement in the wolf motor function test. Restor Neurol Neurosci. 2007;25:549–62. [PubMed] [Google Scholar]
- Yakovlev P, Lecours A. The myelogenetic cycles of regional maturation of the brain. In: Minkowski A, editor. Regional development of the brain in early life. Oxford: Blackwell; 1967. pp. 3–65. [Google Scholar]