Abstract
Coexistence of chronic lymphocytic leukemia (CLL) with myelofibrosis is a rare association with only isolated case reports in the literature. We report an unusual case of CLL in which the cause of anemia was coexistent myelofibrosis. In a case of CLL presenting with refractory anemia, besides common causes like autoimmune hemolytic anemia and marrow infiltration, other causes like myelofibrosis should be searched for.
Keywords: CLL, Myelofibrosis
Coexistence chronic lymphocytic leukemia (CLL) with myelofibrosis is a rare association, though CLL has been described to occur with solid tumors [1–3]. When these two coexist, either CLL may precede or follow idiopathic myelofibrosis [2, 3]. Very unusually both may be diagnosed simultaneously [4]. A 60-year-male presented with fatigue and breathlessness of 6 months duration. On examination pallor, bilateral axillary lymphadenopathy and moderate splenomegaly were present. His hemogram revealed hemoglobin of 4.9 g/dl, corrected reticulocyte count of 0.5%, mean corpuscular volume of 80 fl, total leucocyte count 8,400/μl (neutrophils—34, lymphocytes—62 (including 16% atypical cells), monocytes—02, eosinophils—20), absolute lymphocyte count of 5000/μl, platelet count of 1.7 × 105/μl and erythrocyte sedimentation rate of 56 mm first hour. Normocytic normochromic anemia along with erythroblastemia, tear drop cells and smudge cells were seen in the peripheral blood smear. Serum electrolytes, renal and liver function tests and fasting blood sugar did not show any abnormality. Chest X-ray was normal. Splenomegaly was seen on ultrasound of abdomen. Immunophenotyping showed dim positivity for CD19 and CD25, moderately strong positivity for CD23, CD20, CD38 and lambda chain positive cells. In addition, dual CD19 and CD5 positivity were seen. CD22, CD11c, CD103 and FMC7 were negative, consistent with the diagnosis of CLL. His direct and indirect Coomb’s test was negative. Trephine biopsy was done to ascertain the cause of anemia, which showed hypercellular marrow with a non-erythroid: erythroid ratio of 9:1. There was diffuse infiltration by atypical lymphoid cells. In addition, areas of fibroblastic proliferation were noted (Fig 1). Reticulin was grade 3 (Bauermeister grading system) [5]. However, Masson’s trichrome stain failed to reveal true collagen. A final diagnosis of chronic lymphocytic leukemia with myelofibrosis was made. He was found negative for JAK2 mutation. Patient was started on prednisolone 60 mg/day with tapering dose. He has responded with hemoglobin of 9.5 g/dl and no requirement of blood transfusion.
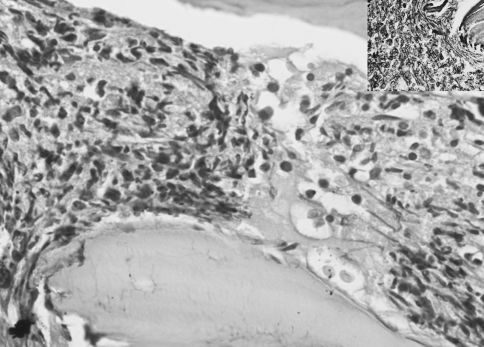
Fig. 1.
Photomicrograph showing monomorphic population of atypical lymphoid cells in the bone marrow trephine biopsy along with areas of fibroblastic proliferation and crushing artefact. Inset shows reticulin stain showing grade III fibrosis. H & E, ×400
Initial presentation of CLL with myelofibrosis is extremely unusual and remains a subject of anecdotal case reports [1–3]. Secondary myelofibrosis occurs in 20–30% of CLL cases, but usually does not manifest clinically [3]. Kimura et al. have suggested that the marrow fibrosis occurs by the secretion of IL-1 alpha from the CLL cells causing growth stimulation of marrow fibroblasts [1]. A review of literature revealed anecdotal case reports of co-existent CLL with myelofibrosis [4]. Possible pathogenetic mechanisms for the development of CLL and myelofibrosis include: (1) a bilineage manifestation of a pluripotent stem cell proliferation, (2) independent proliferations of two distinct cell lines under a common leukemogenic stimulus or (3) an accidental association [3]. Fibrosis of the marrow also indicates an aggressive clinical course [4].
We present a very rare case in which dual hematological malignancy CLL and myelofibrosis were simultaneously detected at presentation with only a singular case report earlier [4]. Thus, in a case of CLL presenting with refractory anemia, causes like myelofibrosis should be considered for in addition to autoimmune hemolytic anemia and marrow infiltration. However, in absence of JAK2 mutation we cannot say for sure whether the myelofibrosis was idiopathic or secondary.
Conflict of interest
No financial support has been received from any institution or companies.
References
- 1.Kimura A, Hyodo H, Nakata Y, Kuramoto A. Chronic lymphocytic leukemia associated with bone marrow fibrosis: possible role of interleukin 1 alpha in the pathogenesis. Am J Hematol. 1993;43:47–50. doi: 10.1002/ajh.2830430111. [DOI] [PubMed] [Google Scholar]
- 2.Böhm J, Schaefer HE, Fisch P. Coincidence of chronic idiopathic myelofibrosis and chronic lymphocytic leukaemia. A rare phenomenon. Pathologe. 2002;23:480–485. doi: 10.1007/s00292-002-0578-5. [DOI] [PubMed] [Google Scholar]
- 3.Nieto HL, Sánchez JMR, Arguelles HA, Barroso MLB, González BG. A case of chronic lymphocytic leukemia overwhelmed by rapidly progressing idiopathic myelofibrosis. Haematologica. 2000;85:973–977. [PubMed] [Google Scholar]
- 4.Zylberait D, Audebert AA, Grolleau Y, Krulik M, Hervouet D, Debray J. Two cases of agnogenic myeloid metaplasia associated with chronic lymphocytic leukemia. Nouv Rev Fr Hematol. 1981;23:111–113. [PubMed] [Google Scholar]
- 5.Bauermeister DE. Quantitation of bone marrow reticulin—a normal range. Am J Clin Pathol. 1971;56:24–31. doi: 10.1093/ajcp/56.1.24. [DOI] [PubMed] [Google Scholar]