Abstract
Adherence to highly active antiretroviral therapy (HAART) medication regimens is vital to maintaining suppression of human immunodeficiency virus (HIV), but persons with HIV face many challenges to adhering consistently to HIV medication regimens. This is particularly true for persons who live in geographically-isolated areas or who have significant levels of cognitive compromise. A videophone-based version of Reynolds’ HAART CARE (HC) telephone intervention for medication adherence was pilot-tested with 23 persons living with HIV residing in both urban and non-urban communities. The purpose of the pilot study was to evaluate the feasibility and acceptance of an adherence improvement intervention administered via videophones. Furthermore, the feasibility and acceptability of conducting HIV pill counts through videophones were assessed. The videophone version of HC produced significant increases in self-reported rates of medication adherence and was generally well-received by interventionists and participants. Pill counts conducted via videophone were also well-accepted by participants. Self-reported adherence levels were higher than videophone-based pill count adherence levels. Challenges to the use of videophones included the requirement that only analog landlines be used, poor quality of video and audio transmissions, and high cost for equipment. Methods to overcome these challenges are discussed.
Keywords: videophone, HIV, HAART, adherence
Introduction
HIV medication adherence interventions
Adherence to highly active antiretroviral therapy (HAART) is vital to maintaining the suppression of human immunodeficiency virus (HIV). Initially, adherence rates of 95% or greater were recommended to promote beneficial clinical outcomes.1 However, recent studies suggest that the relationship between HIV medication adherence and viral suppression is more complex than originally presumed.2–6 For example, Bangsberg3 found that a mean adherence rate as low as 54% might still result in HIV viral suppression if a patient was taking a “potent” HIV medication regimen. Despite the complex relationship that characterizes HIV medication adherence and viral suppression, Bangsberg and colleagues recommend that practitioners encourage their HIV-infected patients on HAART to strive for 100% adherence.3 Recommending dissimilar rates for different regimens might lead to confusion among many patients.
Many HIV medication adherence interventions have been tested since the introduction of antiretroviral therapies. Most adherence-related interventions have been conducted using an “in-person” format, either in clinics (one-on-one or in small groups) or in a person’s home.7–14 This approach may not be feasible for persons with HIV who cannot or will not readily attend clinics or who live in rural areas.
To overcome these barriers, some adherence interventions, such as Reynolds’ HAART Care (HC),15,16 have been conducted via telephone. Others have examined the utility of a web-based HIV medication adherence intervention – as part of a comprehensive virtual support system for persons living with HIV.17
In the current study, it was conjectured that an intervention such as HC delivered via analog videophones would create an “in-person” adherence intervention that could reach HIV-infected persons in their homes, even those living in rural areas.
Analog videophones were chosen for testing in the current study because they can be used in households with “plain old telephone service” (POTS) – that is, analog videophones do not require high speed internet access. Other televideo services, such as web-based videoconferencing services and broadband videophones, do require high speed internet access. When this study commenced in 2007, approximately 47% of Americans had high speed internet at home. However, only 28% of persons with household incomes under $20,000 per year had high speed internet access during this same time period.18 This was an important consideration for the current study, because many HIV positive individuals have lower household income levels.19
Methods of monitoring HIV medication adherence
Many assessment methodologies have been used to measure medication adherence in HIV and non-HIV-related research.
Self-reported medication adherence
Self-reported medication adherence is the least expensive and most logistically feasible method. Self-reported adherence is typically collected in an interview format, either in person or via telephone, although some researchers have collected self-reported adherence via online questionnaires.20 While self-reports are inexpensive and logistically practical, participants often over-report medication adherence in this method.20,21 In addition, self-reported medication adherence may not be well-suited for persons with memory problems or other cognitive deficits, which often are seen in persons with HIV.22 In fact, while some of the medical problems associated with HIV/AIDS have decreased over time, psychological and neurocognitive disorders produced by HIV/AIDS have remained problematic since the emergence of the disease.17 For example, in a study of 141 HIV positive individuals, a 39%–41% incidence of cognitive deficits was found, as defined by −2.0 standard deviations on two or more neuropsychological measures.23 It should be noted that this study of 141 HIV positive individuals excluded persons who were already diagnosed with AIDS dementia complex (ADC). The prevalence of ADC and/or cognitive deficits in persons living with HIV is an important factor to consider when developing HIV adherence interventions.
Refill dates and quantity of pills dispensed from pharmacies
Refill dates and quantity of pills dispensed from pharmacies have also been used to assess HIV adherence rates.24 However, this approach cannot be used if a participant is enrolled in an automatic refill program and assumes that pills are actually taken prior to receiving a refill. It is not uncommon for participants to set aside pills they did not take or throw them away to conceal the fact that they did not take their pills as prescribed.
Medication event monitoring system© (mems)
The Medication Event Monitoring System© (MEMS) is a common measure of medication adherence in HIV adherence research.20 In the MEMS approach, a special cap is placed on top of a standard pill bottle, and it electronically records when the bottle has been opened. MEMS provide researchers with an excellent source of objective adherence data. However, this technology is very expensive and assumes that medications are taken as prescribed whenever when a pill cap is opened.
Unannounced in-person pill counts
Unannounced in-person pill counts are increasingly thought to be one of the most valid and reliable methods of HIV pill counts.25 However, this method is expensive and many participants deny assessors permission to enter into their homes to conduct pill counts. Unannounced in-person pill counts may be best suited for areas of high population density, given the logistical challenges of procuring such pill counts in low population density areas.
Telephone-based pill counts
Kalichman and colleagues have also tested the use of telephone-based pill counts.26 Compared to in-person pill counts, telephone-based pill counts are more cost effective and are more feasible for HIV-infected persons in geographically-isolated areas. Ultimately, however, there is no way to verify visually the pill counts in this method. It is plausible that videophones could be used to conduct pill counts in persons’ homes, thus providing a “visual verification” of the pill counts.
Project ASPIRE
This report describes the “formative phase” of an ongoing study called Project ASPIRE (Adherence Spaced Retrieval Intervention with Remote Enhancement), funded by the National Institute of Mental Health (Grant #R34 MH085246, C. Camp, PI). The formative phase of the study tested the feasibility and acceptability of delivering a one-on-one HIV medication adherence intervention via videophone to HIV-infected persons in urban and nonurban areas. It targeted persons both with and without cognitive impairment (the definition of “cognitive impairment” for the purposes of this study is provided below). A secondary aim of Project ASPIRE was to develop protocols for conducting pill counts via videophone and to assess the feasibility and acceptability of videophone-based pill counts.
Methods
Participants
Participants were recruited through AIDS service organizations in urban, rural, and suburban communities, primarily in the Greater New York City Area (urban) and Ohio (nonurban). Participants were compensated up to US$200 for their complete participation. All recruitment procedures and materials used in this study were approved by two Institutional Review Boards (IRB) – the Menorah Park IRB in Beachwood, Ohio and the Innovative Designs in Environments for an Aging Society (IDEAS) IRB in Kirtland, Ohio.
Participants were divided into two groups based on the size of the community in which they lived. “Urban” communities were those with a population of at least 100,000, and “nonurban” communities were suburban and rural towns with populations of less than 100,000 residents.
Study inclusion criteria were: (1) living with HIV infection or acquired immunodeficiency syndrome (AIDS); (2) being on HAART; (3) aged 18 years or older; (4) self-reported rates of medication adherence of 75% or less over the past four days or self-reported “chronic problems” with adherence at the screening interview; and (5) having access to an analog telephone line.
In addition, at least 50% of participants were expected to evince cognitive impairment (actual percentages are shown below). Two cognitive assessments, the Telephone Adaptation of the Modified Mini-Mental State Exam (T3MS)27,28 and the Verbal Fluency Test (FAS),29,30 were administered to participants via telephone. For the T3MS, a conservative cutoff score of 88 was used to identify participants as being impaired if they had completed nine or more years of education, while a score of 79 indicated impairment for persons with less than nine years of education.28,31 FAS scores that were more than one standard deviation (SD) below the norm for each particular group were considered as evidence of cognitive impairment.
Procedures
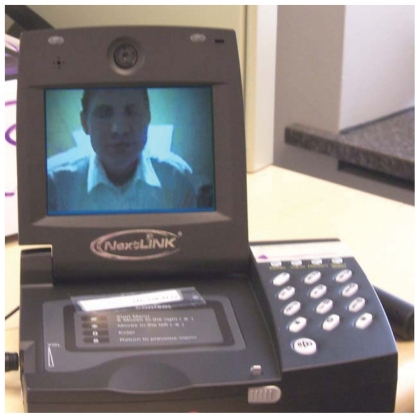
Because the formative phase of Project ASPIRE was to test the acceptability and feasibility of delivering the HC intervention via videophone, all participants received the HC intervention. Upon enrollment in the study, each participant was sent a videophone (see Figure 1) and a “pill counting tray” (see Figure 2). Participants also received easy-to-read, picture-based instructions.
Figure 1.
Videophone used in the study.
Figure 2.
Pill counting tray used for videophone-based pill counts.
Intervention
The intervention tested in the formative phase of Project ASPIRE is an adapted version of Nancy Reynolds’ HC intervention.32 This individualized adherence intervention is guided by self-regulation theory. According to this theory and supporting theoretical and empirical work,33 people attempt to understand their illness (in this case, HIV) by developing a working model or of the disease (in this case, an “HIV representation”): its causes, effects, duration, and treatment. HC suggests that there are many barriers to HIV medication adherence, such as a desire to avoid negative side effects, lack of social support, depression, misconceptions of the disease, poor understanding of the effects of treatment on the disease, stigma, stress, and cognitive limitations, such as forgetting to take one’s medications. The HC intervention addresses each of these possible barriers and attempts to intervene upon factors that contribute to adherence-incompatible perceptions.
In Reynolds’ multicenter AIDS Clinical Trial Group (ACTG) 731, the HC intervention was delivered via regular telephone. Intervention sessions occurred once per week for 12 weeks and then once every other week for four weeks (for a total of 14 sessions). The mean length of each session in Reynolds’ study was eight minutes.8
As modified for Project ASPIRE, the HC protocol asked participants to take part in eight intervention sessions twice per week for four weeks. Each session was expected to be approximately 30 minutes in duration. These changes enabled us to integrate a memory intervention into the HC protocol, a major focus of the next phase of the project.
Assessing medication adherence
Participants were assessed for medication adherence at baseline, at the midpoint of treatment, and at follow-up intervals of one-week and one-, two-, and three-months following treatment, using both self-report and videophone-based pill counts (VBPCs).
Videophone-based pill counts (VBPCs)
Because some participants had cognitive impairments, the pill counting procedure was simplified by selecting a single “anchor” HAART medication (ie, the medication with the most complex regimen) to be assessed during the study. Detailed descriptions of the specifics of conducting VBPCs and the method by which to define “anchor” medications are available from the authors upon request. The information gathered during each VBPC enabled researchers to calculate each participant’s adherence rate. See Table 1 for the formulae used to calculate adherence rates.
Table 1.
Formulae for calculating adherence rates
| Adherence rate since last pill count = | # of pills taken since last pill count ÷ # of pills should have taken since last pill count |
|---|---|
| # of pills taken since last pill count = | (# of pills counted at last pill count + # of pills from refills since last pill count) – (# of pills thrown away + # of pills given away/sold + # of pills lost + # of pills broken + # of pills taken, but taken too early/late day of THIS pill count) – (# of pills counted from all locations at this pill count) |
| # of pills the person should have taken since the last pill count = | [(# of full days since last pill count) x (# of pills per day)] + (# of pills that should have been taken later in the day at the last pill count) + (# of pills that should have been taken earlier in the day at THIS pill count) |
Follow-up interviews
Follow-up interviews were conducted after the intervention phase of the study at one-week and one-, two-, and three-month intervals. In addition to obtaining adherence estimates, participants provided data on reasons for failing to adhere to medication regimens, such as forgetting, not having their medicines with them while traveling, worries regarding side effects, and stigma/confidentiality concerns. Participants also rated their satisfaction with social support in general, and the extent to which family members and/or friends facilitated their adherence efforts. At the one-week and three-month follow-up interviews, participants also provided information about the acceptability of the videophone.
Results
Thirty-three participants were eligible to take part in the intervention phase of the study; 23 participants (70%) completed at least five of the eight intervention sessions and all follow-up interviews. Data presented are from these 23 participants (12 female, 11 male, Mage = 47.95 years, age range: 28–59 years). Seventy percent of participants had been living with HIV/AIDS for more than 10 years. The urban sample (n = 14) had seven female participants, with a mean age of 50 years (age range: 38–59 years). The “non-urban” sample (n = 9) had five female participants, with a mean age of 45 years (age range: 28–54 years). See Table 2 for demographics and Table 3 for scores on tests of cognitive assessment at baseline.
Table 2.
Demographics (in percentages)
| Sexual orientation* | Racial/Ethnic identity* | Education level* | Income | History of substance abuse | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Heterosexual | Homosexual | Bisexual | African American/Black | White | Other | Less than HS | HS | More than HS | Less than $12,000/year | Alcohol | Drug | |
| Overall (A/= 23) | 77 | 14 | 9 | 70 | 26 | 4 | 23 | 54 | 23 | 50 | 44 | 73 |
| Nonurban | 62 | 38 | 0 | 22 | 67 | 11 | 0 | 62 | 38 | 50 | 44 | 67 |
| Urban (n = 14) | 86 | 0 | 14 | 100 | 0 | 0 | 36 | 50 | 14 | 50 | 43 | 77 |
Note: Chi-square = p < 0.01 for urban vs nonurban comparisons.
Abbreviation: HS, high school.
Table 3.
Mean scores and percentages on tests of cognitive impairment at baseline
| T3MS | FAS | Evidence of overall impairment | |||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| Overall (n = 23) | 89.00 | 8.36 | −0.89 | 1.19 | 81.80% |
| Nonurban (n = 9) | 92.75 | 4.74 | −1.14 | 0.81 | 75.00% |
| Urban (n = 14) | 86.86 | 9.34 | −0.75 | 1.36 | 85.70% |
Abbreviations: FAS, Semantic Fluency Test; T3MS, Telephone Adaption of the Modified Mini-Mental State Exam.
Feasibility of delivering intervention via videophones
Comparisons with Reynolds’ outcomes
Reynolds and colleagues8 reported that 70% of all scheduled phone calls were completed successfully in their multicenter randomized, controlled trial. In the current study, 80.3% of all scheduled intervention videophone calls were completed as scheduled. The mean session length of these completed sessions was 23 minutes. Reynolds’ sample had not yet started HAART before receiving HC or a control condition, but self-reported levels of compliance with recently prescribed non-HAART medications in Reynolds’ sample were high (M = 97% treatment; 98% controls) before starting a HAART regimen. At four and 16 weeks after the start of treatment in Reynolds’ study, mean adherence rates for HAART regimens were reported to be 98% for the treatment group and 97% for the control group. In the current sample, mean HAART adherence was self-reported to be 63% before HC, 91% at mid-treatment, and 92% at 16 weeks after initiation of HC. Dependent t-tests revealed a significant increase in self-reported adherence from baseline to mid-treatment (P < 0.01) and from pre-treatment to 16-week follow-up (P < 0.01), with no difference in adherence rates between mid-treatment and 16-week follow up (suggesting that the increase in adherence was maintained from mid-treatment to 16-week follow up). Urban and nonurban participants reported similar levels of adherence. There were no significant correlations between adherence and the FAS (r = 0.12, P < 0.60) and adherence and the T3MS (r = 0.39, P < 0.08).
Reynolds and colleagues reported a 67% satisfaction rate with general social support at baseline. Post-treatment social support was not reported in the Reynolds’ study. In the current study, 89% of participants stated that they were satisfied with their general social support at baseline and at the three-month follow up. In the current study, 57% of participants stated that they received at least some help from family or friends with their adherence efforts baseline, compared to 67% at the three-month follow-up. This difference was not significant (P = 0.43).
Barriers to using videophones
One barrier to conducting the HC intervention over videophones was finding people who had analog telephone lines. Many potential participants had only a cell phone, while others had a digital phone service, which is incompatible with analog videophones. In fact, approximately 15% of persons interested in the study could not participate because they did not have analog telephone landlines. Some participants and interventionists felt that the quality of the video signal was poor and detrimentally affected the quality of intervention sessions. Another problem to the use of videophones is their prohibitive cost. Each videophone used in this study cost approximately $1700.
Acceptability of videophone-based intervention
In general, videophones were well-accepted by participants and interventionists, even though some people felt that the video and audio quality was poor. All 23 participants stated that they would “be willing to use a videophone again in the future” and that they “felt comfortable using the videophone.” Twenty participants (87%) stated that they found it “easy to use the videophone.” Seventeen participants (73.9%) said that they “liked the videophones.” Four out of five interventionists said that they would be willing to use videophones again in the future and that they felt comfortable using videophones.
Feasibility and acceptability of conducting pill counts via videophone
After a considerable amount of in-house pilot testing, the study team developed a videophone-based pill counting protocol that was efficient and well-accepted by participants. Most pill counts lasted 15–30 minutes. No participants withdrew from the study due to the burden of conducting pill counts. Participants with an education level as low as 8–11 years, T3MS scores as low as 68, and FAS scores as low as −2.29 SD were able to complete successfully pill counts.
VBPC adherence data and correlations with self-reported adherence data
Videophone-based pill count adherence rates calculated after treatment were combined into a composite score for each participant. This composite score was required due to data missing for most participants at some point during post-treatment. Videophone-based adherence rates improved from 60% before HC to 82% at post-treatment, though this change was not statistically significant. There were no significant differences between videophone-based pill count adherence levels of the urban and nonurban groups.
For a subset of 17 participants, all of whom had complete data for all time points, self-reported adherence rates were not correlated with VBPC adherence rates, suggesting that participants may have had little insight into their actual adherence rates. However, self-reported adherence rates at baseline were correlated with self-reported post-treatment adherence rates (r = 0.65, P < 0.01), and the two VBPC adherence rates were correlated with one another (r = 0.60, P < 0.05).
Discussion
As HIV infection is increasingly transformed to a chronic, albeit manageable, disease, cost-effective and more readily accessible interventions that can intervene upon and assess medication adherence in persons with HIV are urgently needed. Videophone technology appears to be an efficacious way by which to deliver adherence-improvement interventions to persons living with HIV/AIDS. In addition, pill counts conducted with videophones can provide more objective information regarding levels of adherence than self-report. This may be especially critical when working with persons who have cognitive impairment.
All of our participants, even those with evidence of cognitive impairment, were able to install and utilize videophones when we could talk them through the process over a regular phone line. However, we found it was necessary to supplement our verbal instructions with picture-based instructions. The participant’s ability to refer to pictures of items such as “telephone splitters” and “telephone jacks” was vital to the successful installation and use of videophones. Study staff found that it was important to be patient with, and encouraging of, participants as they attempted to install and operate videophones. Research staff concluded that the installation process was more effective if short sentences and simple vocabulary were used during the instructional period and if they prompted participants with questions throughout the installation period (eg, “So, which jack is the cord plugged into now?”). After videophones were installed, participants had relatively few problems understanding the proper use of the videophone.
Nonetheless, future research on this topic should attempt to address and resolve potential difficulties associated with the prohibitive costs of videophones. As videophone technology increases in sophistication and as more areas of the United States receive state-of-the-science broadband capacity, perhaps some of these issues will be resolved.
In the meantime, the provision of inexpensive laptops ($300–$400) and mobile broadband internet access, which would enable participants to use Skype or a similar technology, is one potential solution to address cost dilemmas in the immediate future. Indeed, it might even be more cost-effective to permit participants to keep laptops provided to them as opposed to purchasing numerous videophones (some of which malfunction or are not returned after their scheduled use). Permitting participants to keep laptops would provide several benefits. It would act as an incentive to take part in the study (videophones had to be returned, which was an added expense and logistical challenge for the project), and help in other ways (eg, making available automatic email reminders, HIV education materials online, etc.) All of this could be achieved at a much lower cost than using current videophone technology. As mentioned earlier, some researchers have already begun to pilot test the use of a web-based HIV medication adherence intervention.17 Additional research in web-based televideo is warranted, especially given the encouraging preliminary results of this study.
The current study has several limitations worthy of comment. First, the sample was a relatively small convenience sample. Second, biologic data (eg, HIV viral load and CD4 cell counts) were not collected in this study; future research on videophone-administered adherence interventions should examine results using more objective immunologic measures. Third, all participants were recruited through AIDS service organizations and, as such, had access to at least some medical and mental health care supportive services; the adherence needs of persons who are not connected with these types of supportive services may be even greater.
In spite of these limitations, this is perhaps the first study to show that the adherence efforts of persons living with HIV/AIDS can be enhanced through interventions delivered using videophone technology. Not only did the intervention show potential to improve adherence in this geographically-diverse group, but the videophone provided a more objective methodology by which to assess participant adherence (ie, videophone-based pill counts). The promising results observed in this pilot study clearly warrant additional research on the topic of administering adherence improvement interventions to persons living with HIV/AIDS through the rapidly evolving technology of videophone systems.
Footnotes
Disclosure
The research projects discussed in this article were funded by Grant #R34 MH085246, (C Camp, PI) from the National Institute of Mental Health, and by Grant #R01 MH078749-04 from the National Institute of Mental Health and National Institute of Nursing Research (Heckman, PI).
References
- 1.Paterson DL, Swindells S, Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- 2.Bangsberg DR, Perry S, Charlebous ED, et al. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15:1181–1183. doi: 10.1097/00002030-200106150-00015. [DOI] [PubMed] [Google Scholar]
- 3.Bangsberg DR. Less than 95% adherence to nonnucleoside reversetranscriptase inhibitor therapy can lead to viral suppression. Clin Infect Dis. 2006;43:939–941. doi: 10.1086/507526. [DOI] [PubMed] [Google Scholar]
- 4.Bangsberg DR, Deeks SG. Is average adherence to HIV antiretroviral therapy enough? J Gen Intern Med. 2002;17:812–813. doi: 10.1046/j.1525-1497.2002.20812.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bangsberg DR, Moss AR, Deeks SG. Paradoxes of adherence and drug resistance to HIV antiretroviral therapy. J Antimicrob Chemother. 2004;53:696–699. doi: 10.1093/jac/dkh162. [DOI] [PubMed] [Google Scholar]
- 6.Weiser SD, Guzman D, Riley ED, Clark R, Bangsberg DR. Higher rates of viral suppression with nonnucleoside reverse transcriptase inhibitors compared to single protease inhibitors are not explained by better adherence. HIV Clinical Trials. 2004;5:278–287. doi: 10.1310/LNHD-K1R7-HQP5-HJCQ. [DOI] [PubMed] [Google Scholar]
- 7.Parsons JT, Rosof E, Punzalan JC, Di Maria L. Integration of motivational interviewing and cognitive behavioral therapy to improve HIV medication adherence and reduce Substance use among HIV-positive men and women: results of a pilot project. AIDS Patient Care STDs. 2005;19:31–39. doi: 10.1089/apc.2005.19.31. [DOI] [PubMed] [Google Scholar]
- 8.McPherson-Baker S, Malow RM, Penedo F, Jones DL, Schneiderman N, Klimas NG. Enhancing adherence to combination antiretroviral therapy in non-adherent HIV-positive men. AIDS Care. 2000;12:399–404. doi: 10.1080/09540120050123792. [DOI] [PubMed] [Google Scholar]
- 9.Jones DL, Ishii M, LaPerriere A, et al. Influencing medication adherence among women with AIDS. AIDS Care. 2003;15:463–474. doi: 10.1080/0954012031000134700. [DOI] [PubMed] [Google Scholar]
- 10.Jones D, McPherson-Baker S, Lydston D, et al. Efficacy of a group medication adherence intervention among HIV positive women: the SMART/EST Women’s Project. AIDS Behav. 2007;11:79–86. doi: 10.1007/s10461-006-9165-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murray MD, Young J, Hoke S, et al. Pharmacist intervention to improve medication adherence in heart failure: A randomized trial. Ann Intern Med. 2007;146:714–725. doi: 10.7326/0003-4819-146-10-200705150-00005. [DOI] [PubMed] [Google Scholar]
- 12.Rigsby MO, Rosen MI, Beauvais JE, et al. Cue-dose training with monetary reinforcement: pilot study of an antiretroviral adherence intervention. J Gen Intern Med. 2000;15:841–847. doi: 10.1046/j.1525-1497.2000.00127.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Remien RH, Stirratt MJ, Dolezal C, et al. Couple-focused support to improve HIV medication adherence: a randomized controlled trial. AIDS. 2005;19:807–814. doi: 10.1097/01.aids.0000168975.44219.45. [DOI] [PubMed] [Google Scholar]
- 14.Neundorfer MM, Camp CJ. Cognitive impairment in midlife in older persons living with HIV/AIDS: Pilot results of a cognitive clinical intervention to improve medication adherence. Adult Development and Aging News. 2005 Spring;:7–10. [Google Scholar]
- 15.Reynolds NR, Testa MA, Marc LG, et al. Factors influencing medication adherence beliefs and self-efficacy in persons naive to antiretroviral therapy: A multicenter, cross-sectional study. AIDS Behav. 2004;8(2):141–150. doi: 10.1023/B:AIBE.0000030245.52406.bb. [DOI] [PubMed] [Google Scholar]
- 16.Reynolds NR, Testa MA, Su M, et al. AIDS Clinical Trials Groups 731 and 384 Teams. Telephone support to improve antiretroviral medication adherence: A multisite, randomized controlled trial. J Acquir Immune Defic Syndr. 2008;47:62–68. doi: 10.1097/QAI.0b013e3181582d54. [DOI] [PubMed] [Google Scholar]
- 17.Blanch JA, Caceres CT, Nomdedeu M, Rousaud AP, Gomez EA, Garcia F. Telemedicine and HIV. UOC Papers: E-Journal on the Knowledge Society. 2007;4:24–31. [Google Scholar]
- 18.Pew Internet and American Life Project. Home Broadband Adoption 2009. Pew Internet and American Life Project. 2009. Jun 17, [Accessed August 31, 2009]. Available from: http://www.pewinternet.org/Reports/2009/10-Home-Broadband-Adoption-2009.aspx.
- 19.Centers for Disease Control and Prevention. Supplement to HIV/AIDS Surveillance Project Demographic and Behavioral Data from a Supplemental HIV/AIDS Behavioral Surveillance Project 1997–2000. CDC: HIV/AIDS Statistics and Surveillance; 2004. [Accessed August 31, 2009]. Available from: http://www.cdc.gov/hiv/topics/surveillance/resources/reports/2004spec_no2/default.htm. [Google Scholar]
- 20.Arnsten JH, Demas PA, Farzadegan H, et al. Antiretroviral therapy adherence and viral suppression in HIV-infected drug users: Comparison of self-report and electronic monitoring. Clin Infect Dis. 2001;33:1417–1423. doi: 10.1086/323201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bangsberg DR, Hecht FM, Charlebois ED, et al. Adherence to protease inhibitors, HIV-1 viral load, and development of drug resistance in an indigent population. AIDS. 2000;14:357–366. doi: 10.1097/00002030-200003100-00008. [DOI] [PubMed] [Google Scholar]
- 22.Brew BJ. AIDS dementia complex. In: Portegies P, Berger JR, editors. Handbook of Clinical Neurology. Volume 85: HIV/AIDS and the Nervous System. Philadelphia: Elsevier Health Sciences; 2007. pp. 79–91. [DOI] [PubMed] [Google Scholar]
- 23.Cysique LA, Maruff P, Brew BJ. Prevalence and pattern of neuropsychological impairment in human immunodeficiency virus-infected/acquired immunodeficiency syndrome (HIV/AIDS) patients across pre- and post-highly active antiretroviral therapy eras: A combined study of two cohorts. J Neurovirol. 2004;10:350–357. doi: 10.1080/13550280490521078. [DOI] [PubMed] [Google Scholar]
- 24.Grossberg R, Gross R. Use of pharmacy refill data as a measure of antiretroviral adherence. Curr HIV/AIDS Rep. 2007;4:187–191. doi: 10.1007/s11904-007-0027-4. [DOI] [PubMed] [Google Scholar]
- 25.Bangsberg DR, Hecht FM, Charlebois ED, Chesney M, Moss A. Comparing objective measures of adherence to HIV antiretroviral therapy: Electronic medication monitors and unannounced pill counts. AIDS Behav. 2001;5:275–281. [Google Scholar]
- 26.Kalichman SC, Amaral CM, Stearns H, et al. Adherence to antiretroviral therapy assessed by unannounced pill counts conducted by telephone. J Gen Intern Med. 2007;22:1003–1006. doi: 10.1007/s11606-007-0171-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48:314–318. [PubMed] [Google Scholar]
- 28.Norton MC, Tschanz JAT, Fan X, et al. Telephone adaptation of the Modified Mini-Mental State Exam (3MS). The Cache County study. Neuropsychiatry Neuropsychol Behav Neurol. 1999;12:270–276. [PubMed] [Google Scholar]
- 29.Benton AL, Hamsher K. Multilingual Aphasia Examination. 2nd ed. Iowa City, IA: AJA Associates Inc; 1976. [Google Scholar]
- 30.Brickman AM, Paul RH, Cohen RA, et al. Category and letter verbal fluency across the adult lifespan: Relationship to EEG theta power. Arch Clin Neuropsychol. 2005;20:561–573. doi: 10.1016/j.acn.2004.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ogrocki PK. Personal communication. Aug, 2007.
- 32.Reynolds NR. The problem of antiretroviral adherence: a self-regulatory model for intervention. AIDS Care. 2003;15:117–124. doi: 10.1080/0954012021000039815. [DOI] [PubMed] [Google Scholar]
- 33.Alonzo AA, Reynolds NR. The structure of emotions during acute myocardial infarction: a model of coping. Soc Sci Med. 1998;46:1099–1110. doi: 10.1016/s0277-9536(97)10040-5. [DOI] [PubMed] [Google Scholar]