Abstract
Background
Preoperative screening for nasal S. aureus carriage, followed by eradication treatment of identified carriers with nasal mupirocine ointment and chlorhexidine soap was highly effective in preventing deep-seated S. aureus infections. It is unknown how cost-effectiveness of this intervention is affected by suboptimal S. aureus screening. We determined cost-effectiveness of different preoperative S. aureus screening regimes.
Methods
We compared different screening scenarios (ranging from treating all patients without screening to treating only identified S. aureus carriers) to the base case scenario without any screening and treatment. Screening and treatment costs as well as costs and mortality due to deep-seated S. aureus infection were derived from hospital databases and prospectively collected data, respectively.
Results
As compared to the base case scenario, all scenarios are associated with improved health care outcomes at reduced costs. Treating all patients without screening is most cost-beneficial, saving €7339 per life year gained, as compared to €3330 when only identified carriers are treated. In sensitivity analysis, outcomes are susceptible to the sensitivity of the screening test and the efficacy of treatment. Reductions in these parameters would reduce the cost-effectiveness of scenarios in which treatment is based on screening. When only identified S. aureus carriers are treated costs of screening should be less than €6.23 to become the dominant strategy.
Conclusions
Preoperative screening and eradication of S. aureus carriage to prevent deep-seated S. aureus infections saves both life years and medical costs at the same time, although treating all patients without screening is the dominant strategy, resulting in most health gains and largest savings.
Introduction
Deep surgical site infections caused by Staphylococcus aureus are an important complication of surgical procedures, associated with increased morbidity and mortality and considerable incremental health care costs. It is estimated that around 80% of such infections are caused by strains already colonizing the patient at the time of surgery, most notably in the anterior nares [1]. In a multi-centre double-blind placebo-controlled trial, preoperative screening for nasal S. aureus carriage, followed by S. aureus eradication treatment of identified carriers with nasal mupirocine ointment and chlorhexidine gluconate soap, all within one week before surgery, was associated with 79% and 55% reductions in deep-seated and superficial S. aureus infections, respectively [2]. Yet, screening all patients preoperatively with PCR-based rapid diagnostic tests and providing timely treatment to identified carriers will be an enormous logistical – and costly – challenge. The cost-effectiveness of this intervention has not been determined and it is unknown how this will be affected by suboptimal screening. The aim of this study was, therefore, to quantify costs and effects of this intervention using different screening scenarios.
Methods
We performed a cost-effectiveness analysis from the societal perspective and restricted our analyses to deep-seated prosthetic joint and deep-seated cardio surgical infections (such as mediastinitis), as the intervention is most relevant for these types of infections. Cost and mortality related to deep surgical site infections were derived from the hospital databases of the UMC Utrecht, one of the participating centres of the recently published multi-centre trial. The UMC Utrecht is a tertiary medical centre with 1012 beds, in which around 200 prosthetic joint implantations and 1,000 cardiopulmonary surgical procedures are performed annually. Infectious complications of these interventions, as well as all costs associated, have been prospectively monitored from 2001 on by the department of hospital hygiene and infection control. From this database we calculated costs for patients readmitted because of a postoperative surgical site infection, which included the number of hospital admission days, surgical procedures, and diagnostic procedures (mainly radiological and microbiological) (Table 1). We intentionally restricted cost estimates to the costs associated with readmission for deep surgical infections in order to not to include other non-associated costs. Although we might have missed episodes that were readmitted to other hospitals, we believe this number to be low and such cases were unlikely to influence the calculated cost per episode. We assessed hospital mortality of patients with deep-seated S. aureus prosthetic joint and cardio surgical infections and quantified the average number of expected life years at the time of death using life tables from Statistics Netherlands (Table 2). We did not adjust life expectancy for comorbidities. Therefore, life expectancies are overestimated, which implies that the calculated savings per life year are rather conservative. Institutional review board approval was not required as monitoring postoperative and other hospital associated infections is part of the regular infection control program conducted by the department of hospital hygiene and infection control.
Table 1. Direct health care costs of patients readmitted because of a postoperative surgical site infection between 2001 and 2010.
| Department | ||
| Cardio surgical | Orthopedic | |
| (n = 28) | (n = 25) | |
| Age, mean ± SD, years | 58 ± 16 | 55 ± 15 |
| Male sex (%) | 19 (68) | 13 (52) |
| Surgical interventions, no. (%) | ||
| coronary artery bypass grafting | 20 (71) | 0 |
| heart valve replacement | 3 (11) | 0 |
| total knee or hip prosthesis | 0 | 7 (28) |
| shoulder surgery | 0 | 3 (12) |
| spondylodesis | 0 | 3 (12) |
| other fracture surgery | 0 | 6 (24) |
| other | 5 (18) | 6 (24) |
| Length of hospital stay, total days (median) | 529 (17) | 1597 (48) |
| Total cost of health care, euros (mean/patient) | ||
| surgical procedures | 31,605 (1580)a | 71,695 (2987)b |
| laboratory investigations | 40,149 (1434) | 31,781 (1271) |
| radiological investigations | 9068 (363)c | 5071 (211)b |
| hospitalization days | 150,157 (5363) | 499,728 (19,989) |
| other | 3716 (133) | 17,705 (708) |
| total costs readmissiond | 234,695 (8382) | 625,980 (25,039) |
Missing information on 8 patients.
Missing information on 1 patient.
Missing information on 3 patients.
Costs of antibiotic treatment were not included.
Table 2. Life expectancy of patients with deep-seated postoperative S. aureus infections.
| Characteristic | n = 37a |
| Age, mean ± SD, years | 66 ± 17 |
| Male sex (%) | 19 (51) |
| Hospital department (%) | |
| cardio surgical | 23 (62) |
| orthopedic | 14 (28) |
| Postoperative S. aureus infections, no. (%) | |
| mediastinitis | 18 (49) |
| prosthetic joint infection | 14 (38) |
| other deep-seated infection | 5 (14) |
| In-hospital deaths, no. (%) | 9 (24) |
| Expected survival, mean, years | |
| survivors | 19.83 |
| survivors, discounted | 9.54 |
| non survivors | 15.83 |
| non survivors, discounted | 9.29 |
17 patients (46%) are included in estimate of the cost of a postoperative surgical site infection.
Parameters used in the model are listed in Table 3. The incidence of deep-seated S. aureus infections in S. aureus carriers was 4.4% and was assumed to be three to six times lower (1.5% to 0.7%) among non-carriers [3]–[5]. In order to be conservative in our estimates of cost-effectiveness, we have used a six times lower incidence in our calculations. The relative risk of deep-seated S. aureus infections after mupirocin-chlorhexidine treatment was 0.21 compared to placebo [2]. Sensitivity and specificity of the rapid diagnostic test was considered 0.97 and 0.99, respectively [2], [6].
Table 3. Parameters used in cost-effectiveness analysis.
| Parameter | Value | Reference |
| No. of patients colonized with S. aureus, % | 18.5 | [2] |
| Incidence of deep-seated S. aureus infections among S. aureus carriers, % | 4.4 | [2] |
| Incidence of deep-seated S. aureus infections among non-carriers, % | 0.7-1.5 | [2] |
| Cost of screening, € | 63.90 | [7] |
| Sensitivity of screening test | 0.97 | [2]-[5] |
| Specificity of screening test | 0.99 | [6] |
| Cost of treatment, € | 15.94 | [8] |
| Relative risk of deep-seated S. aureus infections due to intervention, % | 0.21 | [2] |
| Cost of deep-seated surgical site infection, € | 17,820 | UMC Utrecht |
| Hospital mortality among patients with deep-seated S. aureus infection, % | 24 | UMC Utrecht |
| Life expectancy of non-survivors of deep-seated S. aureus infection, years | 15.83 | UMC Utrecht |
| Life expectancy of non-survivors of deep-seated S. aureus infection, discounted, years | 9.29 | UMC Utrecht |
The calculated costs of the screening strategy included material and labour costs (real-time PCR assay and conventional culture costs as determined by the Dutch Healthcare Authority) [7]. We assumed 5 minutes extra working time for nurses (the average nurse wage was valued at €26.45 per hour based on gross salary including taxes and social premiums). Costs of mupirocin ointment 2% and chlorhexidine gluconate soap (40 mg per millilitre) for 5 days were calculated according to the pharmaceutical reference pricing system [8]. The reference year for cost computations was 2009. Costs related to postoperative surgical site infection have been adapted to 2009 using the consumer price index as determined by Statistics Netherlands. Effects (life years gained) were discounted at 3%, as recommended in the U.S.A. [9]; costs were not discounted, as all costs are made in one year. Costs were expressed in Euros (1 Euro = 1.43 US dollars, December 2009).
Two scenarios were compared to the base case scenario, in which none of the patients will be screened or treated for S. aureus carriage. In scenario 1, it is aimed to screen all patients and only identified S. aureus carriers receive eradication treatment, as in the study by Bode et al [2]. Yet, preoperative screening and allocating treatment within one week before surgery may not be achievable in all patients, for which estimates of 15% have been reported [10], [11]. Therefore, in scenario 2 not only identified S. aureus carriers but also patients that could not be screened receive eradication treatment. In each scenario, proportions of patients screened were varied from 0% (making scenario 1 identical to base case, and treating all patients in scenario 2) to 100% (making scenario 1 and 2 identical). For each of the scenarios total number of S. aureus infections prevented, costs per infection prevented and costs per life year gained were determined. In sensitivity analyses, we explored which uncertain variables in the model were of most influence on the cost-effectiveness of screening strategies.
Results
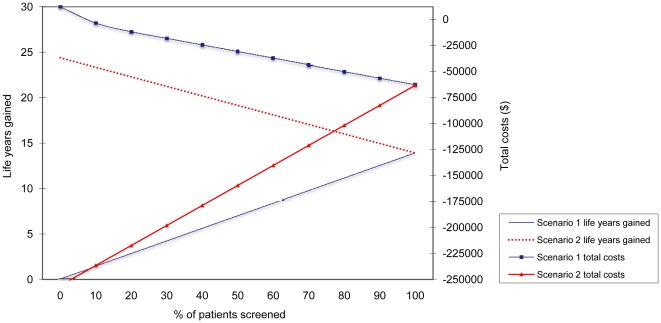
Without screening and treatment (base case) there will be 14 deep-seated postoperative S. aureus infections with 3 patients succumbing from the infection per 1000 procedures, incidence 1.4% (Table 4). Despite large cost differences between scenarios 1 and 2, both scenarios are associated with improved health outcomes and cost savings, compared to the base case scenario without screening and treatment (Figure 1). Yet, the scenario with all patients treated without screening (scenario 2 with 0% of patients screened) clearly is most cost-effective with highest health gains (24 discounted life years) and highest cost savings (€178,970) per 1000 patients. These positive results are explained by the avoidance of screening costs and from the higher efficacy of the intervention, as carriers are not missed and non-carriers, though with a lower infection risk, are also treated.
Table 4. Cost-analysis of different strategies per 1000 patients undergoing prosthetic joint or cardiopulmonary surgery.
| Parameter | Base case Scenario | Scenario 1 (identified S. aureus carries are treated: 100% screened) | Scenario 1 (identified S. aureus carries are treated: 85% screened) | Scenario 2 (identified S. aureus carries and non-screened patients are treated: 85% screened) | Scenario 2 (identified S. aureus carries and non-screened patients are treated: 0% screened) |
| No. of patients screened | 0 | 1000 | 850 | 850 | 0 |
| No. of patients treated | 0 | 185 | 153 | 303 | 1000 |
| No. of deep-seated S. aureus infection | 14 | 7 | 9 | 7 | 3 |
| No. of deaths due to deep-seated S. | |||||
| aureus infection | 3 | 2 | 2 | 2 | 0.7 |
| No. of life years gained, discounted | -31 | 14 | 12 | 15 | 24 |
| Cost per infection prevented, € | NA | 10,395 | 10,703 | 8518 | 1457 |
| Cost per life year gained, € | 7993 | -3330 | -3192 | -4172 | -7339 |
| Total costs saved due to infection | |||||
| prevention, € | -246,722 | 47,746 | 37,737 | 64,583 | 178,970 |
Figure 1. Effect of suboptimal adherence to preoperative S. aureus screening on total costs and life years gained (discounted) per 1000 patients for scenario 1 (only identified S. aureus carriers are treated) and scenario 2 (identified S. aureus carriers and non-screened patients are treated).
Note the negative costs on the y-axis representing cost-savings.
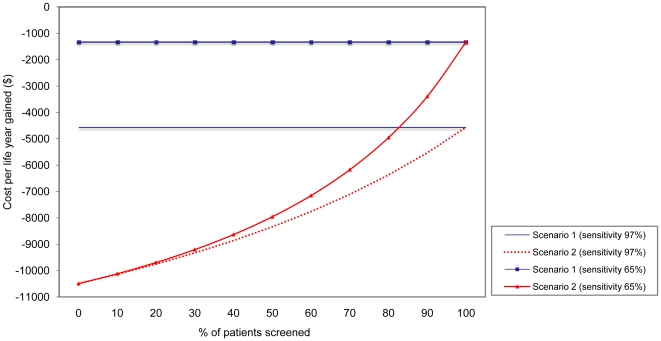
If test sensitivity of the PCR-based screening test is 65%, as was reported for the test used in the multi-center trial [6], the intervention would be less beneficial (and save €930 per life year gained) in scenario 1 (Figure 2). In scenario 2 (non-screened patients will all be treated) the effect of test sensitivity on costs per life year gained decreases with less patients being screened.
Figure 2. Effect of suboptimal adherence to preoperative S. aureus screening and test sensitivity on cost per life year gained (discounted) per 1000 patients for different screening scenarios.
Scenario 1 is treatment of S. aureus carriers identified by screening; scenario 2 is treatment of S. aureus carriers identified by screening plus treatment of all patients that were not screened. In scenario 1 the life years gained and costs increase, or decrease, at a constant rate resulting in an invariable cost per life years gained. Note the negative costs on the y-axis representing cost-savings.
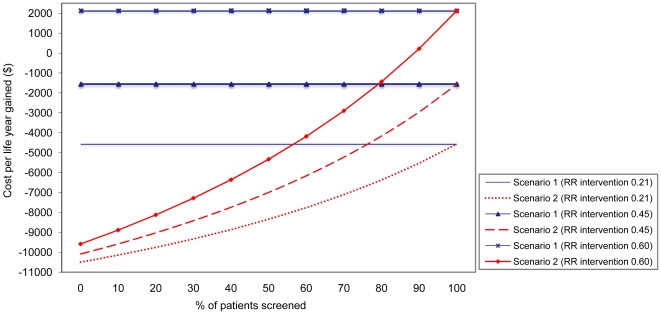
We have assumed that the relative risk of deep-seated S. aureus infections after eradication treatment was 0.21 compared to placebo. However, if the effect of the intervention is lower, health outcomes and cost savings are less (Figure 3), and when the relative risk with eradication is less than, respectively, 0.53 and 0.62 for scenario 1 and 2, the intervention is no longer cost-saving.
Figure 3. Effect of suboptimal adherence to preoperative S. aureus screening and treatment effectiveness on cost per life year gained (discounted) per 1000 patients for different screening scenarios.
Scenario 1 is treatment of S. aureus carriers identified by screening; scenario 2 is treatment of S. aureus carriers identified by screening plus treatment of all patients that were not screened. In scenario 1 the life years gained and costs increase, or decrease, at a constant rate resulting in an invariable cost per life years gained. Note the negative costs on the y-axis representing cost-savings.
If the proportion of identified S. aureus carriers is higher than 18.5% [1], [11], the cost savings will increase for all scenarios. The largest increase occurs in scenario 1, in which the cost savings per life year gained will increase from €3330 (with 18.5% carriage) to €5039 with 30% carriage, which is still lower than the €7339 per life year gained when all patients are treated without screening.
When only identified S. aureus carriers receive eradication treatment (scenario 1) costs of screening should be less than €6.23 to become the dominant strategy, resulting in more cost-savings than scenario 2 with 0% screening. In scenario 2, when all non-screened patients also receive treatment, the break-even point of the screening costs will decrease with fewer patients being screened. For instance, with 85% of patients being screened treating only identified S. aureus carriers will become the dominant strategy if the costs of screening become less than €50.27 per patient.
Discussion
Although screening for S. aureus carriage followed by short-term eradication therapy among identified carriers is associated with both improved health outcomes and reduced health care costs, treating all patients without previous screening appears to result in more infections prevented, more life years gained and higher savings. The benefits in life years gained and costs saved must be balanced against the risks for selection of mupirocin and/or chlorhexidine resistance by using these agents in patients not colonized with S. aureus.
The current analysis was motivated by our own experiences with implementing preoperative screening for S. aureus carriage in our hospital. A large - and increasing - number of patients is admitted just hours before surgery, with the last out-patient clinic visit frequently weeks before. In such patients preoperative screening and starting treatment is difficult to realize. Furthermore, although the recent clinical trial reported PCR test sensitivity of 97% [2], the sensitivity as reported in literature is much lower (65% to 82%) [6], [12]. Although negative screening results have been associated with lower levels of colonization density [6], possibly reflecting lower infection risks [3], [13], patients potentially benefiting from eradication therapy will be missed in a screen and treat strategy. These aspects did not affect the multi-centre trial as only S. aureus carriers, as identified with PCR-testing, were eligible. Numbers of patients that were not screened were not available from the Bode publication, but in our hospital we estimate that more than 50% of the surgical patients were not screened, due to the before-mentioned reasons. Moreover, the 18.5% incidence of S. aureus carriage in the multi-centre study was lower than previously estimated, probably because of low test sensitivity.
Strengths of our analysis include the fact that both costs and mortality due to deep-seated postoperative S. aureus infections were based on detailed prospectively determined data. Yet, we still had to make assumptions on several parameter values, which deserve comments. For instance, the S. aureus infection rate among non-carriers was estimated to be three to six times lower than among carriers based on published data [2], [5]. We have used a six times lower incidence in our calculations, which is a conservative estimate as a higher incidence of infection would result in increased savings. Also, the intervention was considered equally effective in S. aureus carriers and non-carriers. Since the overwhelming majority of S. aureus infections are from endogenous origin, this assumption seems not unlikely. Yet, a lower efficacy of treatment in non-identified carriers would make any strategy that includes screening less cost-effective. Furthermore, we assumed that all patients with deep-seated infections that died in our hospital (i.e., 24%, all cardiosurgical patients) succumbed because of the infection. Others though have estimated attributable mortality due to serious S. aureus infections to range from 7–20% [14], [15]. With lower mortality rates the number of life years gained would become lower, but the relative differences between the different scenarios would not change. We also limited our analyses to deep-seated infections, as we had most accurate cost data for this category of infection and the effect of the intervention was most pronounced for these infections in the recently published trial [2]. Real-life cost-effectiveness is assumed to be more beneficial than reported in this paper, as we disregard the effects of screen and treat strategies on superficial infections. Only direct health care costs were included in our analysis. As the average age of patients dying from nosocomial S. aureus infections in our hospital was almost 70, inclusion of indirect costs associated with productivity losses is not thought to have a large influence on our estimates.
Widespread use of mupirocine and chlorhexidine might increase the risk of resistance of S. aureus, as resistance for both agents has been reported. However, overall resistance rates for both agents are still low, despite widespread use in the last decades. Some S. aureus strains carry the plasmid-born qacA/B genes which code for multidrug efflux pumps and increase minimum bactericidal concentrations (MBCs) to chlorhexidine [16]. Although presence of these genes have been associated with reduced efficacy of a chlorhexidine-based decolonization strategy to prevent MRSA transmission in a British ICU [17], MBCs usually remain below concentrations to treat patients and the clinical significance of these qacA/B genes remains unclear [18]. Yet, whether treatment in the absence of S. aureus colonization increases the risk of resistance to mupirocine and chlorhexidine (for instance through selection of plasmid-born resistance in coagulase-negative staphylococci) is unknown. Yet, based on the cost-effectiveness of decolonization to prevent deep-seated postoperative S. aureus infections, we conclude that the benefits of treating non-detected or non-screened patients outweigh the future risks of reduced effectiveness due to widespread resistance to antiseptics and mupirocine. Surveillance cultures will be necessary for early detection of emerging resistance.
Acknowledgments
We thank Ms T. Hopmans who calculated the cost of postoperative surgical site infection in the UMC Utrecht.
Footnotes
Competing Interests: M.J.M.B. reports receiving advisory board fees from Ipsat Therapies, 3M, Cepheid and Novartis; consulting fees from Novartis, 3M and Bayer; lecture fees from Cepheid, Kimberly-Clark and Pfizer. All other authors: none to declare.
Funding: M.J.M.B. was supported by the Netherlands Organization for Scientific Research (VICI NWO Grant 918.76.611). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Wertheim HF, Melles DC, Vos MC, van Leeuwen W, van Belkum A, et al. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect Dis. 2005;5:751–762. doi: 10.1016/S1473-3099(05)70295-4. [DOI] [PubMed] [Google Scholar]
- 2.Bode LG, Kluytmans JA, Wertheim HF, Bogaers D, Vandenbroucke-Grauls CM, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med. 2010;362:9–17. doi: 10.1056/NEJMoa0808939. [DOI] [PubMed] [Google Scholar]
- 3.Luzar MA, Coles GA, Faller B, Slingeneyer A, Dah GD, et al. Staphylococcus aureus nasal carriage and infection in patients on continuous ambulatory peritoneal dialysis. N Engl J Med. 1990;322:505–509. doi: 10.1056/NEJM199002223220804. [DOI] [PubMed] [Google Scholar]
- 4.Nouwen J, Schouten J, Schneebergen P, Snijders S, Maaskant J, et al. Staphylococcus aureus carriage patterns and the risk of infections associated with continuous peritoneal dialysis. J Clin Microbiol. 2006;44:2233–2236. doi: 10.1128/JCM.02083-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perl TM, Cullen JJ, Wenzel RP, Zimmerman MB, Pfaller MA, et al. Intranasal mupirocin to prevent postoperative Staphylococcus aureus infections. N Engl J Med. 2002;346:1871–1877. doi: 10.1056/NEJMoa003069. [DOI] [PubMed] [Google Scholar]
- 6.Choudhurry RS, Melles DC, Eadie K, Vos M, Wertheim HF, et al. Direct detection of human Staphylococcus aureus carriage in the nose using the Lightcycler Staphylococcus kit. J Microbiol Methods. 2006;65:354–356. doi: 10.1016/j.mimet.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 7.Dutch Healthcare Authority. Medisch specialistische behandelingen en bijbehorende tarieven, CI-1094-b2. Available: http://www.nza.nl/regelgeving/tarieven/. Accessed 2010 January 10.
- 8.College voor Zorgverzekeringen. Houten: Bohn Stafleu van Loghum; 2010. Farmacotherapeutisch Kompas 2010. [Google Scholar]
- 9.Gold MR, Siegel JE, Russell LB, Weinstein MC. New York: Oxford University Press; 1996. Cost-effectiveness in health and medicine. [Google Scholar]
- 10.Kluytmans JA, Mouton JW, VandenBergh MF, Manders MJ, Maat AP, et al. Reduction of surgical-site infections in cardiothoracic surgery by elimination of nasal carriage of Staphylococcus aureus. . Infect Control Hosp Epidemiol. 1996;17:780–785. doi: 10.1086/647236. [DOI] [PubMed] [Google Scholar]
- 11.Hacek DM, Robb WJ, Paule SM, Kudrna JC, Stamos VP, et al. Staphylococcus aureus nasal decolonization in joint replacement surgery reduces infection. Clin Orthop Relat Res. 2008;466:1349–1355. doi: 10.1007/s11999-008-0210-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andriesse GI, van Rijen M, Bogaers D, Bergmans AM, Kluytmans JA. Comparison of two PCR-based methods and conventional culture for the detection of nasal carriage of Staphylococcus aureus in pre-operative patients. Eur J Clin Microbiol Infect Dis. 2009;28:1223–1226. doi: 10.1007/s10096-009-0770-0. [DOI] [PubMed] [Google Scholar]
- 13.White A. Increased infection rates in heavy nasal carriers of coagulase-positive staphylococci. Antimicrob Agents Chemother (Bethesda) 1963;161:667–670. [PubMed] [Google Scholar]
- 14.Noskin GA, Rubin RJ, Schentag JJ, Kluytmans J, Hedblom EC, et al. National trends in Staphylococcus aureus infection rates: impact on economic burden and mortality over a 6-year period (1998-2003). Clin Infect Dis. 2007;45:1132–1140. doi: 10.1086/522186. [DOI] [PubMed] [Google Scholar]
- 15.Karra R, McDermott L, Connelly S, Smith P, Sexton DJ, et al. Risk factors for 1-year mortality after postoperative mediastinitis. J Thorac Cardiovasc Surg. 2006;132:537–543. doi: 10.1016/j.jtcvs.2006.04.037. [DOI] [PubMed] [Google Scholar]
- 16.Smith K, Gemmell CG, Hunter IS. The association between biocide tolerance and the presence or absence of qac genes among hospital-acquired and community-acquired MRSA isolates. J Antimicrob Chemother. 2008;61:78–84. doi: 10.1093/jac/dkm395. [DOI] [PubMed] [Google Scholar]
- 17.Batra R, Cooper BS, Whiteley C, Patel AK, Wyncoll D, et al. Efficacy and limitation of a chlorhexidine-based decolonization strategy in preventing transmission of methicillin-resistant Staphylococcus aureus in an intensive care unit. Clin Infect Dis. 2010;50:210–217. doi: 10.1086/648717. [DOI] [PubMed] [Google Scholar]
- 18.Vali L, Davies SE, Lai LL, Dave J, Amyes SG. Frequency of biocide resistance genes, antibiotic resistance and the effect of chlorhexidine exposure on clinical methicillin-resistant Staphylococcus aureus isolates. J Antimicrob Chemother. 2008;61:524–532. doi: 10.1093/jac/dkm520. [DOI] [PubMed] [Google Scholar]