Abstract
Recent studies have linked expression of lectin-like ox-LDL receptor 1 (OLR1) to tumorigenesis. We analyzed microarray data from Olr1 knockout (KO) and wild type (WT) mice for genes involved in cellular transformation and evaluated effects of OLR1 over-expression in normal mammary epithelial cells (MCF10A) and breast cancer cells (HCC1143) in terms of gene expression, migration, adhesion and transendothelial migration. Twenty-six out of 238 genes were inhibited in tissues of OLR1 KO mice; the vast majority of OLR1 sensitive genes contained NF-κB binding sites in their promoters. Further studies revealed broad inhibition of NF-kB target genes outside of the transformation-associated gene pool, with enrichment themes of defense response, immune response, apoptosis, proliferation, and wound healing. Transcriptome of Olr1 KO mice also revealed inhibition of de novo lipogenesis, rate-limiting enzymes fatty acid synthase (Fasn), stearoyl-CoA desaturase (Scd1) and ELOVL family member 6 (Elovl6), as well as lipolytic phospholipase A2 group IVB (Pla2g4b). In studies comparing MCF10A and HCC1143, the latter displayed 60% higher OLR1 expression. Forced over-expression of OLR1 resulted in upregulation of NF-κB (p65) and its target pro-oncogenes involved in inhibition of apoptosis (BCL2, BCL2A1, TNFAIP3) and regulation of cell cycle (CCND2) in both cell lines. Basal expression of FASN, SCD1 and PLA2G4B, as well as lipogenesis transcription factors PPARA, SREBF2 and CREM, was higher in HCC1143 cells. Over-expression of OLR1 in HCC1143 cells also enhanced cell migration, without affecting their adherence to TNFα-activated endothelium or transendothelial migration. On the other hand, OLR1 neutralizing antibody inhibited both adhesion and transmigration of untreated HCC1143 cells. We conclude that OLR1 may act as an oncogene by activation of NF-kB target genes responsible for proliferation, migration and inhibition of apoptosis and de novo lipogenesis genes.
Introduction
OLR1, a lectin-like scavenger receptor, is highly conserved in mammals [1] and it is capable of recognizing several ligands including the protein moiety of oxidized-LDL (ox-LDL), advanced glycation end-products, gram-positive and gram-negative bacteria and apoptotic cells [2]. OLR1 is primarily expressed in vascular cells and vasculature-rich organs [3], and its activation by a wide range of stimuli indicative of dyslipidemia, inflammation and damage initiates several signaling cascades including MAPKs, other protein kinases as well as transcription factors NF-κB and AP-1 [4], [5].
Overexpression of OLR1 has been shown in cellular components of atherosclerotic lesions [6]. Deletion of Olr1 in Ldlr knockout (KO) mice results in much smaller atherosclerotic lesions associated with a drastic reduction of inflammation in the aortic wall [7]. Olr1 abrogation also attenuates angiotensin II-induced hypertension [8]. Similarly, abrogation of Olr1 reduces the extent of ischemia/reperfusion injury [9].
An association between obesity and atherosclerotic disease states in humans is well established [10], [11]. Associations with obesity have been found for various cancers, including breast and prostate neoplasms [12], [13], suggesting a mechanistic overlap in the pathobiology of atherogenesis and tumorigenesis. Recently, Olr1, acting through NF-κB mediated inflammatory signaling, was strongly implicated in carcinogenesis [14].
The focus of the present study was to further elucidate role of OLR1 as an oncogene based on the premise that as a sensor of dyslipidemia and a molecule involved in NF-kB activation, OLR1 may be a link between dyslipidemia and cancer. The first part of the study was based on microarray analysis of wild-type (WT) and olr1 KO mice. The second part defines the relationship between olr1 and apoptosis and lipogenesis genes in breast cancer cell line HCC1143 and migration and adhesion of these cells.
Results
Comparison of OLR1 KO and transformation transcriptomes
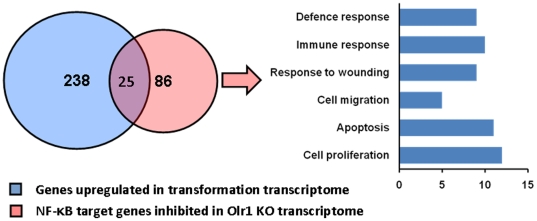
The principal findings from the analysis of microarray data from the hearts of wild-type (WT) and Olr1 KO from our group have been reported elsewhere [15]. An additional analysis against the overlapping set of genes (n = 238) found to be upregulated during transformation of two isogenic cell types [14] revealed that 26 genes from this list were inhibited in the Olr1 KO transcriptome by at least 20% (Table 1). Among these were various components of immune response (Isg20, C1s, S1r, Ifrd1) and a number of transcription factors including well-known oncogenes (JunB, Rel, Irf2, Crem). Promoter analysis of resulting set of genes [16] identified their enrichment for NF-κB binding sites (p<0.03) which were located within 500 nucleotides proximal to transcriptional start sites in all but one (C1s) Olr1 sensitive genes (n = 25, Fig. 1).
Table 1. A list of transformation related genes influenced by Olr1 deletion in mice.
| Gene | REFSEQ ID | Symbol | Fold change | P value |
| Inhibited | ||||
| interferon-stimulated protein | NM_020583 | Isg20 | −3.26 | 0.007 |
| matrix metallopeptidase 3 | NM_0011135271 | Mmp3 | −2.05 | 0.014 |
| reticuloendotheliosis oncogene | NM_009044 | Rel | −2.02 | 0.011 |
| complement component 1, s subcomponent | NM_144938 | C1s | −1.76 | 0.008 |
| complement component 1, r subcomponent | NM_023143, | C1r | −1.61 | 0.001 |
| suppressor of cytokine signaling 3 | NM_007707 | Socs3 | −1.57 | 0.003 |
| Jun-B oncogene | NM_008416 | Junb | −1.56 | 0.0009 |
| interferon regulatory factor 2 | NM_008391 | Irf2 | −1.51 | 0.044 |
| fibroblast activation protein | NM_007986 | Fap | −1.44 | 0.005 |
| synaptosomal-associated protein 23 | NM_009222 | Snap23 | −1.41 | 0.033 |
| N-myc (and STAT) interactor | NM_001141949 | Nmi | −1.41 | 0.0019 |
| cAMP responsive element modulator | NM_013498 | Crem | −1.40 | 0.043 |
| pentraxin related gene | NM_008987 | Ptx3 | −1.38 | 0.052 |
| MAPK kinase kinase 7 interacting protein 2 | NM_138667 | Map3k7ip2 | −1.37 | 0.041 |
| TNF receptor superfam. member 21 | NM_178589 | Tnfrsf21 | −1.35 | 0.011 |
| Acetylglucosamine (GlcNAc) transferase | NM_139144 | Ogt | −1.35 | 0.002 |
| Ras-GTPase-activating protein SH3-domain binding protein 1 | NM_013716 | G3bp1 | −1.35 | 0.003 |
| Rho family GTPase 3 | NM_028810 | Rnd3 | −1.31 | 0.013 |
| interferon-related developmental regulator 1 | NM_013562 | Ifrd1 | −1.29 | 0.026 |
| oxidation resistance 1 | NM_130885 | Oxr1 | −1.29 | 0.003 |
| solute carrier family 2 member 3 | NM_011401 | Slc2a3 | −1.28 | 0.044 |
| annexin A7 | NM_009674 | Anxa7 | −1.28 | 0.001 |
| karyopherin (importin) alpha 2 | NM_010655 | Kpna2 | −1.27 | 0.014 |
| prostaglandin-endoperoxide synthase 1 | NM_008969 | Ptgs1 | −1.26 | 0.031 |
| lectin, galactose binding, soluble 8 | NM_018886 | Lgals8 | −1.20 | 0.014 |
| Stimulated | ||||
| ser (or cys) peptidase inhibitor, clade. E, memb 2 | NM_009255 | Serpine2 | 1.26 | 0.018 |
| succinate dehydrogenase complex, subunit C | NM_025321 | Sdhc | 1.29 | 0.017 |
| E26 avian leukemia oncogene 2, 3′ domain | NM_011809 | Ets2 | 1.35 | 0.001 |
| NF-κ light polypeptide gene enhancer in B-cells inhibitor, alpha | NM_010907 | Nfkbia | 1.36 | 0.002 |
| GTP binding protein 2 | NM_001145979 | Gtpbp2 | 1.41 | 0.008 |
| mitogen-activated protein kinase kinase kinase 5 | NM_008580 | Map3k5 | 1.51 | 0.005 |
| SRY-box containing gene 4 | NM_009238 | Sox4 | 1.54 | 0.007 |
Figure 1. Olr1 deletion results in broad inhibition of NF-κB target genes.
A diagram depicting a set of overlapping genes between transformation and Olr1 KO transcriptomes. From the set of 238 genes upregulated during transformation, 26 genes were found to be inhibited in Olr1 KO mice. Vast majority of these genes carried NF-κB sites in their proximal promoter sequences. In total, 86 NF-κB target genes were found to be inhibited in Olr1 KO mice with enrichment for regulation of apoptosis (p = 0.0002), proliferation (p = 0.00003), wound healing (p = 0.0002), defense response (p = 0.0011), immune response (p = 0.0003) and cell migration (p = 0.0009).
OLR1 deletion results in a broad inhibition of NF-κB target genes
Further search for NF-κB regulated genes using a list compiled from available web based databases and the literature revealed that inhibition of the p65 subunit observed in the Olr1 KO transcriptome was complemented with upregulation of inhibitory Ikbα subunit (1.36 fold, p = 0.002, Table 1) and accompanied by significant downregulation of several (n = 61) NF-κB target genes (Table 2). The combined set of Olr1 sensitive NF-κB target genes displayed enrichment for regulation of apoptosis (p = 0.0002), proliferation (p = 0.00003), wound healing (p = 0.0002), defense response (p = 0.0011), immune response (p = 0.0003) and cell migration (p = 0.0009) (Figure 1). Among the genes involved in apoptosis (n = 11) and cellular proliferation (n = 12), 6 and 5, respectively, were negative regulators (David Bioinformatics Database, 17).
Table 2. NF-κB target genes outside of transformation pool significantly inhibited in Olr1 knockout mice (more than 1.2-fold).
| Gene Title | Gene Symbola | Fold change | P value | A | W | P | D | M |
| colony stimulating factor 2 | Csf21,2 | -3.55 | 0.0148 | • | • | |||
| phospholipase A2, group IVB (cytosolic) | Pla2g4b1 | -3.29 | 0.0079 | |||||
| lectin, galactose binding, soluble 3 | Lgals31 | -2.93 | 0.0302 | |||||
| BCL 2 related protein A1a | Bcl2a11,2,3 | -2.90 | 0.0304 | • | ||||
| chitinase 3-like 1 | Chi3l12 | -2.80 | 0.0145 | |||||
| lymphotoxin A | Lta1 | -2.73 | 0.0007 | • | • | • | • | |
| hepcidin antimicrobial peptide | Hamp2 | -2.50 | 0.0518 | • | ||||
| immunoglobulin heavy chain complex | Igh2 | -2.34 | 0.0006 | |||||
| glucosaminyl (N-acetyl) transferase 1, core 2 | Gcnt12 | -2.23 | 0.0216 | |||||
| fos-like antigen 2 | Fosl22 | -2.22 | 0.0012 | • | ||||
| NFκB inhibitor, ε | Nfkbie2 | -2.20 | 0.0321 | |||||
| selectin, platelet | Selp1 | -2.20 | 0.0309 | • | • | • | ||
| complement factor B | Cfb1 | -2.15 | 0.0079 | • | • | |||
| deiodinase, iodothyronine, type II | Dio22 | -2.07 | 0.0039 | |||||
| FBJ osteosarcoma oncogene | Fos2 | -2.03 | 0.0270 | |||||
| interleukin 17A | Il17a2 | -2.00 | 0.0103 | • | • | |||
| thrombospondin 1 | Thbs2 | -1.94 | 0.0146 | • | • | • | ||
| CD3 antigen, gamma polypeptide | Cd3g1 | -1.92 | 0.0020 | • | ||||
| LPS-induced TN factor | Litaf3 | -1.91 | 0.0072 | |||||
| CD48 antigen | Cd481 | -1.77 | 0.0228 | |||||
| prostaglandin E synthase | Ptges2 | -1.61 | 0.0484 | • | ||||
| chemokine (C-X-C motif) ligand 5 | Cxcl51 | -1.60 | 0.0055 | • | • | |||
| HSP90, α (cytosolic), class A member 1 | Hsp90aa12 | -1.59 | 0.0355 | |||||
| CD209f antigen | Cd209f2 | -1.56 | 0.0067 | |||||
| vascular cell adhesion molecule 1 | Vcam11,2 | -1.54 | 0.0007 | |||||
| coagulation factor III | F31 | -1.54 | 0.0111 | • | ||||
| twist gene homolog 1 (Drosophila) | Twist12 | -1.52 | 0.0092 | |||||
| B-cell leukemia/lymphoma 2 | Bcl21,2,3 | -1.52 | 0.0201 | • | • | • | • | • |
| cyclin D2 | Ccnd23 | -1.51 | 0.0161 | • | ||||
| dihydropyrimidine dehydrogenase | Dpyd2 | -1.48 | 0.0062 | |||||
| CASP8 and FADD-like apopt. regulator | Cflar1,2,3 | -1.44 | 0.0544 | • | ||||
| related RAS viral oncogene homolog 2 | Rras23 | -1.43 | 0.0476 | • | ||||
| CD274 antigen | Cd2742 | -1.42 | 0.0273 | • | ||||
| immediate early response 3 | Ier31,2,3 | -1.41 | 0.0250 | |||||
| Fas (TNFRSF6)-assoc. via death domain | Fadd3 | -1.39 | 0.0272 | • | ||||
| TNF, alpha-induced protein 3 | Tnfaip31,2,3 | -1.38 | 0.0520 | |||||
| Kruppel-like factor 10 | Klf103 | -1.38 | 0.0267 | • | • | |||
| NUAK family, SNF1-like kinase, 2 | Nuak22 | -1.37 | 0.0300 | • | ||||
| TNF receptor superfamily, member 21 | Tnfrsf211 | -1.35 | 0.0113 | |||||
| interferon regulatory factor 7 | Irf71,2 | -1.35 | 0.0173 | |||||
| transglutaminase 2, C polypeptide | Tgm21 | -1.31 | 0.0390 | • | • | |||
| CD82 antigen | Cd823 | -1.31 | 0.0308 | |||||
| phosphodiesterase 7A | Pde7a2 | -1.31 | 0.0123 | |||||
| heparanase | Hpse2 | -1.29 | 0.0390 | |||||
| ATP-binding cass., subf. B, memb. 1A | Abcb1a1 | -1.28 | 0.0298 | |||||
| midkine | Mdk2 | -1.27 | 0.0502 | • | ||||
| MAD homolog 7 (Drosophila) | Smad73 | -1.27 | 0.0195 | |||||
| solute carrier family 3, member 2 | Slc3a22 | -1.27 | 0.0355 | |||||
| Proteasome subunit, beta type 9 | Psmb91,2 | -1.25 | 0.0264 | |||||
| cyclin D binding myb-like TF 1 | Dmtf12 | -1.25 | 0.0224 | |||||
| beta-2 microglobulin | B2m1,2 | -1.24 | 0.0007 | • | ||||
| adenosine A1 receptor | Adora11 | -1.23 | 0.0215 | • | • | • | ||
| nuclear receptor subf. 3, gr. C, member 1 | Nr3c12 | -1.22 | 0.0540 | • | ||||
| platelet derived GF, B polypeptide | Pdgfb1,2 | -1.22 | 0.0152 | • | • | |||
| cAMP responsive element bind. protein 3 | Creb32 | -1.21 | 0.0306 |
Legend: (a)- a list of NFkB target genes was compiled from the following web-based databases: 1 - http://bioinfo.lifl.fr/NF-KB/; 2 -http://people.bu.edu/gilmore/nf-kb/target/index.html#cyto; and 3 - http://www.broadinstitute.org/mpr/publications/projects/Lymphoma/FF_NFKB_suppl_revised.pdf. The genes whose expression was significantly altered by OLR1 deletion was analyzed for enrichment themes using DAVID bioinformatic database. The enriched themes included regulation of apoptosis, “A”; Wound healing,“W”; Cell proliferation, “P”; Defense response,“D”; Cell migration, “M”.
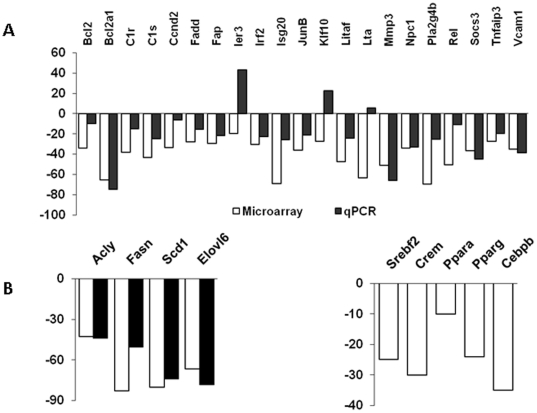
OLR1 deletion suppresses lipogenesis genes
The microarray findings were validated for select genes using quantitative real-time PCR. For most of the tested genes, the transcriptional shifts in Olr1 KO observed in microarrays were confirmed (Figure 2A). In addition, Olr1 deletion resulted in inhibition of key enzymes for lipogenesis (Figure 2B), including ATP citrate lyase (Acly), acetyl-Coenzyme A carboxylase alpha (Acaca), fatty acid synthase (Fasn), stearoyl-CoA Desaturase 1 (Scd1) and ELOVL family member 6 (Elovl6). It is of interest that none of the Olr1-sensitive lipid metabolism related genes carried NF-κB binding sites in their promoters. This suggests that the effects of Olr1 on lipogenesis may be independent from its NF-κB signaling arm. On the other hand, several lipid metabolism transcription factors, including sterol regulatory element binding factor 2 (Srebf2), cAMP responsive element modulator (Crem), peroxisome proliferator activated receptors alpha and gamma (Ppara and Pparg), as well as CCAAT/enhancer binding protein (C/EBP) beta, were found to be downregulated in Olr1 KO mice (Figure 2B).
Figure 2. qPCR validation of microarray data.
A. qPCR validation of select genes from overlapping set (from Table 1); B. Expression of lipogenesis genes and transcription factors in olr1 KO mice. White bars – microarray data; black bars – qPCR data. All P values<0.05.
Effects of OLR1 overexpression in normal epithelial and cancer cells
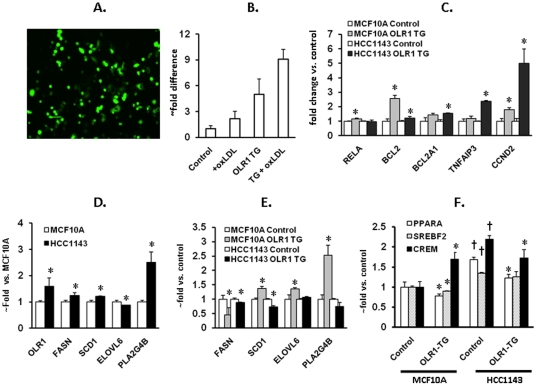
Transfection of MCF10A and HCC1143 cells with OLR1 expression vector resulted in 5 to 8-fold increase of OLR1 expression, which falls within the range OLR1 upregulation. In epithelial cells exposed to ox-LDL [18]. This led to modest upregulation of RELA (p65) and significant increases in RNA message for BCL2, BCL2A1, TNFAIP3 and CCND2 (Figure 3B). Compared to MCF10A cells, HCC1143 cells displayed increased basal levels of OLR1 (59%, p<0.05), FASN (24%, p<0.03), SCD1 (21%, p<0.01) and PLA2G4B (153%, p<0.01) (Figure 3C). The response from lipogenesis genes to OLR1 transfection varied in these cell lines (Figure 3D). In MCF10A cells, over-expression of OLR1 significantly stimulated transcription of SCD1 (37%, p<0.02), ELOVL6 (38%, p<0.05) and PLA2G4B (153%, p<0.02) concomitant with upregulation of CREM, whereas in HCC1143 cells CREM transcription declined and SCD1 and PLA2G4B were inhibited compared with control cultures transfected with empty vector.
Figure 3. Effects of OLR1 overexpression on transcription of genes involved in apoptosis, proliferation and lipogenesis in MCF10a and HCC1143 cells.
These cells were transfected with either empty vector or OLR1 cDNA (Origene, Rockville, MD) using Lipofectamine 2000 (Invitrogen). Transfection efficiency (70–80%) was evaluated using GFP vector. RNA was extracted 48 hours post-transfection, converted into cDNA and the expression of genes was determined by quantitative PCR. A. Efficiency of transfection (cells transfected with GFP vector). B. Quantitative PCR plot. Note the enhancement of OLR1 expression in both control and OLR1-transfected cultures in response to ox-LDL. C. Expression of genes involved in apoptosis and proliferation. In order to stimulate OLR1 associated signaling requiring OLR1-ligand interaction, OLR1 transfected cells were treated with 40 µg/ml ox-LDL for 24 hours; graphs represent comparison with untreated control cells transfected with empty vector; D. Basal expression of OLR1, PLA2G4B and lipogenesis genes in normal human mammary epithelial cells (MCF10A) and breast cancer cells (HCC1143); E. Expression of OLR1, PLA2G4B and lipogenesis genes in MCF10a and HCC1143 cells transfected with OLR1 treated according to the protocol described above. F. Expression of lipogenesis transcription factors in MCF10a and HCC1143 cells transfected with OLR1 and treated according to the protocol described above. All experiments were conducted in triplicates. (*) p<0.05 compared to respective control; (†) – p<0.05 compared to MCF10A.
Over-expression of OLR1 facilitates wound healing, but has no effect on adhesion
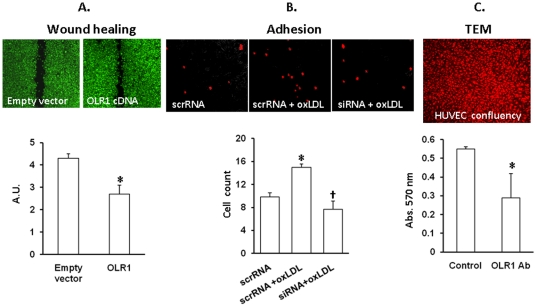
It has been reported that inhibition of OLR1 using siRNAs resulted in reduction of tumor growth in vivo and cancer cell migration in vitro [14]. In order to evaluate effects of OLR1 upregulation, we transfected HCC1143 cells with either empty plasmid or OLR1 expression vector and tested migration in a wound healing assay (Figure 4A). Over-expression of OLR1 was confirmed using qPCR. Cells with upregulated OLR1 bridged the wounds much faster than control cultures (p<0.001). In contrast, adhesion and transendothelial migration of OLR1 transfected cancer cells did not differ from control values (not shown).
Figure 4. Phenotypic consequences of OLR1 overexpression or inhibition.
A. Wound healing assay. Upper panel - representative images of wound healing assay performed using HCC1143 cells transfected with either empty plasmid or OLR1 cDNA vector; Lower panel – graph depicting the distance between edges of the wound after 36 hours of incubation. (*) – p<0.01; B. Adhesion assay. Upper panel- representative images of adherent non-transfected HCC1143 cells loaded with CellTracker Red CMTX (Invitrogen, Carlbad, CA) and applied to non-activated or activated (50 µg/ml oxLDL, 4 hrs) confluent HUVECs transfected with OLR1 Silencer or scrambled siRNA. Lower panel - graph depicting the number of adherent cells averaged from multiple fields of view in triplicate cultures. (*) – p<0.05 compared to non-activated control (“scrRNA”); (†) - p<0.05 compared to scrambled RNA; C. Colorimetric transendothelial migration assay. Upper panel – verification of the confluence of HUVECs on the membranes by staining cells with CellTracker Red CMTX. Lower panel – absorbance values of stain extracted from the cells migrated through TNFα-activated endothelial monolayer in presence of OLR1 neutralizing antibody or human IgG (Control).
However, basal adhesion and transendothelial migration of non-transfected HCC1143 cells were significantly attenuated when OLR1 was inhibited or neutralized in endothelial cells using siRNA or pre-treating cells with OLR1 neutralizing antibody (Figure 4BC).
Discussion
This study suggests multiple potential links between OLR1 and susceptibility to cancer. First, the microarray database in the mice with Olr1 abrogation exhibited a marked reduction in expression of NF-kB target genes involved in cellular transformation [14], as well as genes related to lipogenesis. Second, over-expression of OLR1 in a human cancer cell line showed significant upregulation of several genes with oncogenic properties and a significant increase in cell migration.
Our microarray analysis showed that the vast majority of genes reported to be upregulated during cell transformation (but inhibited in Olr1 KO mice) carried NF-kB binding sites in their promoters (Table 1). Furthermore, a significant portion of NF-kB target genes outside of the transformation-related pool, especially those involved in regulation of apoptosis, proliferation and migration, were also down-regulated in the Olr1 KO transcriptome (Table 2). In the mouse Olr1 KO microarray, both B-cell leukemia/lymphoma 2 related protein A1 (Bcl2a1) and Bcl2 were transcriptionally inhibited. Bcl2a1 is an upstream negative regulator of the mitochondriocentric mode of apoptosis via prevention of cytochrome c release into the cytoplasm, which is required for initiation of the apoptotic cascade. It has been reported that enhanced synthesis of BCL2A1 and BCL-XL are the underlying cause of about 1000-fold greater resistance of subsets of chronic lymphocytic leukemia cells [19]. TNFα-induced protein 3 (TNFAIP3) is a key regulator of inflammation and immunity involved in the development of various autoimmune diseases and it also desensitizes cells from TNFα-induced cytotoxicity and was shown to be anti-apoptotic in breast cancer MCF7S1 cells [20]. Inhibition of TNFAIP3 compromises growth and survival of glioblastoma stem cells via inhibition of cell cycle progression and NF-κB activity, and increases survival of mice bearing glioblastome xenografts [21].
We observed a significant reduction of Ccnd2 message in Olr1 KO mice and its multi-fold upregulation in OLR1 transgenic HCC1143 cells. Cyclin D2 is a highly conserved regulator of cyclin-dependent kinases 4 and 6 responsible for of G1/S transition. This gene is epigenetically silenced in the majority of breast cancers [22]. Its overexpression in LNCaP cells results in an impediment to proliferation and increased apoptosis [23]. In addition, Olr1 deletion appeared to compromise the entire technological chain of de novo lipogenesis, including synthesis of saturated C16 and C18 fatty acids (Fasn and Elovl6), and their conversion into MUFAs (Scd1). Many cancers, including those involving prostate and breast [24], [25], rely almost exclusively on de novo synthesis regardless of nutritional availability. The switch to de novo lipogenesis occurs early and is a prerequisite for efficient transformation. Novel effects of OLR1 on lipid metabolism could account for much of its reported pro-oncogenic activity. For example, the expression level of FASN positively correlates with poor cancer prognosis [26], its genomic amplification is a common occurrence in some cancers [27], and its over-expression promotes transformation of epithelial cells [28]. Similarly, over-expression of SCD1 has been observed in several types of cancers, including mammary cancer [29]; its upregulation is associated with transformation and its knock-down results in decreased cell proliferation, a loss of anchorage-independent growth and impaired apoptosis [30]. It is of note that compared to MCF10A cells, over-expression of OLR1 in HCC1143 cells did not evoke the expected activation of lipogenesis genes. This may be explained by maximally increased basal expression of these genes in HCC1143 cells at baseline (Figure 3D).
As most of the genes upregulated in OLR1-TG HCC1143 cells are functionally pleiotropic, we evaluated the cumulative outcome of their upregulation on wound healing, adhesion and transendothelial migration assays (Figure 4). Notably, the migration of cells was seen to almost double the control value in cells with over-expression of OLR1, strongly suggesting a role for this molecule in breast cancer growth. On the other hand, presentation of OLR1 on the surface of cancer cells did not seem to be essential for adhesion to activated endothelial cells or for transendothelial migration. The level of OLR1 in endothelial cells, however, appears to be important, as addition of neutralizing OLR1 antibody to the medium or inhibition of OLR1 transcription significantly impaired adhesion and transendothelial migration in non-transfected cancer cells. This is indicative of OLR1 as a possible mechanism of cancer cell-endothelium interactions, as tumor cells are characterized by abundance of OLR1 ligand phophatidylserine on the cellular membranes [31].
In summary, our data from multiple approaches in transgenic mice and human normal epithelial and cancer cell lines suggest that OLR1 has several pro-oncogenic actions based on: a) activation of NF-κB signaling pathway resulting in inhibition of apoptosis and stimulation of proliferation; b) activation of de novo lipogenesis, and c) more efficient adhesion and transendothelial migration due to upregulation of OLR1 in endothelium. We believe these data strongly suggest that OLR1 may function as a link between obesity and susceptibility to breast cancer.
Materials and Methods
Animals
C57BL/6 mice were obtained from Jackson Laboratories. The homozygous Olr1 KO mice were developed on C57BL/6 background as described previously [17]. The Olr1 KO mice showed total absence of Olr1 as determined by RT PCR and immunostaining, and the binding of oxLDL to the vascular intima was completely absent in these animals. All animals received humane care in compliance with the Public Health Service Policy on Humane Care and Use of Laboratory Animals published by the National Institutes of Health. The present studies were approved by UAMS Animal Care and Usage Committee approval number 2484, dated November 2007.
Microarray Analysis
Total RNA of heart was extracted from WT mice and Olr1 KO mice. Microarray analysis was performed by Affymetrix Mouse Genome GenChip 430 2.0 gene expression array (Affymetrix Inc. Santa Clara, CA) and analyzed using Affymetrix Microarray Analysis Suite (MAS) 5.0 to assess the quality of RNA and hybridization. A log base 2 transformation was applied to the data before the arrays were normalized. All values from each array were normalized to the 75th percentile value of the array, which was arbitrarily set at intensity minimum >100. For gene expression annotation, EASE (as described in http://apps1.niaid.nih.gov/David) analysis was performed on significant genes identified by one sample t-test. In addition, Gene Ontology (GO) terms http://www.geneontology.org) for biological processes and cellular component were identified as proposed by the GO Consortium. All microarray data is MIAME compliant and that the raw data has been deposited in a MIAME compliant database (ArrayExpress) as detailed on the MGED Society website http://www.mged.org/Workgroups/MIAME/miame.html (accession number E-MTAB-473).
Reagents and cell lines
All reagents, unless stated otherwise, were purchased from Sigma (St. Louis, MO). Human breast cancer cell line HCC1143 was a kind gift of Dr. A. Basnakian (University of Arkansas for Medical Sciences, Little Rock AR). Mammalian expression vector (pCMV5-XL5) with human OLR1 cDNA were obtained from Origene (Rockville, MD). Silencer Select Validated siRNA to OLR1 (s9843) was purchased from Invitrogen (Carlsbad, CA). Cells were cultured using standard RPMI 1640 growth medium supplemented with fetal bovine serum (10%) and ampicillin/streptomycin. High TBAR ox-LDL (90 nmoles MDA/mg Protein) was purchased from Biomedical Technologies Inc. (Stoughton, MA). Human IgG was purchased from Abcam (Cambridge, MA).
Real-Time Quantitative PCR
Cells were transfected with either empty vector or OLR1 expression vector. The efficiency of transfection was confirmed in parallel experiments with GFP carrying plasmid. Part of the transfected cultures (all in triplicates) was treated with oxLDL (40 µg/ml) for 24 hours before harvesting and RNA extraction. RT qPCR was performed using the Applied Biosystems 7900 real-time PCR system. qPCR specific primers were designed using Probe-Finder (http://www.roche-appliedscience.com) web-based software. All qPCR reactions were carried out in a final volume of 15 µl containing 1× of SYBR Green PCR Master Mix (Applied Biosystems, Carlsbad, CA), 300 nM of each gene specific primers, 100 ng cDNA, in sterile deionized water. The standard cycling condition was 50°C for 2 min, 90°C for 10 min, followed by 40 cycles of 95°C for 15 s and 62°C for 1 min. The results were analyzed using SDS 2.3 relative quantification manager software. The comparative threshold cycles values were normalized for GAPDH reference genes. qPCR was performed in triplicate to ensure quantitative accuracy.
Transfection protocol
Cells were transfected with either empty vector or OLR1 cDNA constructs (Origene, Rockville, MD) using lipofectamine 2000 (Invitrogen, Carlsbad, CA) in accordance with manufacturer's instructions with minor modifications. In preliminary experiments, we determined that higher transfection efficiency is achieved by applying a 2∶1 ratio of DNA to lipofectamine in relation to the proposed concentration of DNA recommended in the general protocol. Using these conditions, we routinely observed 70–80% transfection efficiency. Transfection of HUVECs with OLR1 Silencer (s9843) or scrambled siRNA (Invitrogen, Carlsbad, CA) was carried out using lipofectamine 2000 according to manufacturer's instructions. Cells we used in adhesion experiments 48 hours post-transfection and inhibition of OLR1 transcription was verified by quantitative RT PCR.
Wound healing assay
Wound healing assay was performed to determine cell migration, according to the following protocol: Cells were cultured to confluence in 24-well plates, and two separate scratch wounds were made in every well using a sterile 200 µl pipette tip. Cells lifted in the process of scratching were gently removed by washing in PBS, then fresh growth medium was added. Pictures were taken at 10× magnification every 12 hours and the final picture after 36 hours of incubation was taken after loading the cells with calcein AM (Invitrogen, Carlsbad, CA).
Adhesion assay
Human umbilical vein endothelial cells (HUVECs) were grown to confluence in 12-well plates and activated by exposure to oxLDL (50 µg/ml) for 4 hrs. Breast cancer cells HCC1143 were labeled with CellTracker Red CMTX (Invitrogen, Carlsbad, CA) according to manufacturer's instructions and added on to endothelial monolayer at concentration of 105 cells per well. Plates were incubated for 1 hour in a CO2 incubator and then gently washed 3 times with growth medium to remove non-adherent cells. The number of cells attached to endothelium was counted in several fields of view in triplicate cultures using fluorescent microscope.
Colorimetric transendothelial migration assay
The transmigration potential of HCC1143 cells was evaluated using QCM Tumor Cell Transendothelial Migration Assay (Millipore, Billerica, MA) according to manufacturer's instructions. Briefly, HUVECs were seeded on fibronectin-coated cell culture inserts at high density (pore size 8 µm), cultured until reaching 100% confluence and activated by exposure to 20 ng/ml TNFα.overnight. Breast cancer cells HCC1143 were added. (1×105 per insert) to the monolayer and incubated in the cell incubator for 6 hours. Upon completion of the incubation period, growth medium and cells were gently swabbed from the interior of inserts The extent of transmigration was evaluated by measuring the amount of stain extracted from transmigrated cells on the outer surface of the membrane (absorbance at 570 nm) using a plate reader.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: The authors have no support or funding to report.
References
- 1.Xie Q, Matsunaga S, Niimi S, Ogawa S, Tokuyasu K, et al. Human lectin-like oxidized low-density lipoprotein receptor-1 functions as a dimer in living cells. DNA Cell Biol. 2004;23:111–117. doi: 10.1089/104454904322759920. [DOI] [PubMed] [Google Scholar]
- 2.Mehta JL, Chen J, Hermonat PL, Romeo F, Novelli G. Lectin-like oxidized low- Density lipoprotein receptor-1 (OLR1): A critical player in the development of atherosclerosis and related disorders. Cardiovasc Res. 2006;69:36–45. doi: 10.1016/j.cardiores.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 3.Yamanaka S, Zhang XY, Miura K, Kim S, Iwao H. The human gene encoding the lectin-type oxidized LDL receptor (OLR1) is a novel member of the natural killer gene complex with a unique expression profile. Genomics. 1998;1998;54:191–199. doi: 10.1006/geno.1998.5561. [DOI] [PubMed] [Google Scholar]
- 4.Li D, Mehta JL. Ox-LDL induces apoptosis in human coronary artery endothelial cells: role of PKC, PTK, bcl-2, and Fas. Am J Physiol. 1998;275:H568–H576. doi: 10.1152/ajpheart.1998.275.2.H568. [DOI] [PubMed] [Google Scholar]
- 5.Li D, Saldeen T, Romeo F, Mehta JL. Oxidized LDL upregulates angiotensin II type 1 receptor expression in cultured human coronary artery endothelial cells: the potential role of transcription factor NF-kappaB. Circulation. 2000;102:1970–1976. doi: 10.1161/01.cir.102.16.1970. [DOI] [PubMed] [Google Scholar]
- 6.Chen M, Kakutani M, Minami MM, Kataoka H, Kume N, et al. Increased expression of lectin-like oxidized low density lipoprotein receptor-1 in initial atherosclerotic lesions of Watanabe Heritable Hyperlipidemic rabbits. Arterioscler Thromb Vasc Biol. 2000;20:1107–1115. doi: 10.1161/01.atv.20.4.1107. [DOI] [PubMed] [Google Scholar]
- 7.Mehta JL, Sanada N, Hu CP, Chen J, Dandapat A, et al. Deletion of OLR1 reduces atherogenesis in LDLR knockout mice fed high cholesterol diet. Circ Res. 2007;100:1634–1642. doi: 10.1161/CIRCRESAHA.107.149724. [DOI] [PubMed] [Google Scholar]
- 8.Hu C, Dandapat A, Sun L, Marwali MR, Inoue N, et al. Modulation of angiotensin II-mediated hypertension and cardiac remodeling by OLR1 deletion. Hypertension. 2008;52:552–562. doi: 10.1161/HYPERTENSIONAHA.108.115287. [DOI] [PubMed] [Google Scholar]
- 9.Hu C, Chen J, Dandapat A, Fujita Y, Inoue N, et al. OLR1 abrogation reduces myocardial ischemia-reperfusion injury in mice. J Mol Cell Cardiol. 2008;44:76–83. doi: 10.1016/j.yjmcc.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 10.Mathieu P, Lemieux I, Després JP. Obesity, inflammation, and cardiovascular risk. Clin Pharmacol Ther. 2010;2010;87:407–16. doi: 10.1038/clpt.2009.311. [DOI] [PubMed] [Google Scholar]
- 11.Brinkley TE, Kume N, Mitsuoka H, Phares DA, Hagberg J. Elevated soluble lectin-like oxidized LDL receptor-1 (sOLR1) levels in obese postmenopausal women. Obesity (Silver Spring) 2008;16:1454–1456. doi: 10.1038/oby.2008.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cleary MP, Grossmann ME, Ray A. Effect of obesity on breast cancer development. Vet Pathol. 2010;2010;47:202–213. doi: 10.1177/0300985809357753. [DOI] [PubMed] [Google Scholar]
- 13.Romieu I, Lajous M. The role of obesity, physical activity and dietary factors on the risk for breast cancer: Mexican experience. Salud Publica Mex. 2009;51(Suppl 2):s172–180. doi: 10.1590/s0036-36342009000800007. [DOI] [PubMed] [Google Scholar]
- 14.Hirsch HA, Iliopoulos D, Joshi A, Zhang Y, Jaeger S, et al. Transcriptional signature and common gene networks link cancer with lipid metabolism and diverse human diseases. Cancer Cell. 2010;2010;17:348–361. doi: 10.1016/j.ccr.2010.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kang BY, Hu C, Ryu S, Khan JA, Biancolell, et al. Genomics of cardiac remodeling in angiotensin II-treated wildtype and OLR1-deficient mice. Physiol Genomics. 2010;42:42–54. doi: 10.1152/physiolgenomics.00009.2010. [DOI] [PubMed] [Google Scholar]
- 16.Zambelli F, Pesole G, Pavesi G. Pscan. Finding over-represented transcription factor binding site motifs in sequences from co-regulated or co-expressed genes. Nucleic Acids Res. 2009;37:W247–W252. doi: 10.1093/nar/gkp464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang DW, Sherman BT, Lempicki RA. Systematic and integrative analysis of large gene lists using DAVID Bioinformatics Resources. Nature Protoc. 2009;4:44–57. doi: 10.1038/nprot.2008.211. [DOI] [PubMed] [Google Scholar]
- 18.Wang R, Ding G, Liang W, Chen C, Yang H. Role of LOX-1 and ROS in oxidized low-density lipoprotein induced epithelial-mesenchymal transition of NRK52E_. Lipids Health Dis. 2010;9:120. doi: 10.1186/1476-511X-9-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vogler M, Butterworth M, Majid A, Walewska RJ, Sun, et al. Concurrent up-regulation of BCL-XL and BCL2A1 induces approximately 1000-fold resistance to ABT- 737 in chronic lymphocytic leukemia. Blood. 2009;2009;113:4403–4413. doi: 10.1182/blood-2008-08-173310. [DOI] [PubMed] [Google Scholar]
- 20.Jäättelä M, Mouritzen H, Elling F, Bastholm L. A20 zinc finger protein inhibits TNF and IL-1 signaling. J Immunol. 1996;1996;156:1166–1173. [PubMed] [Google Scholar]
- 21.Hjelmeland AB, Wu Q, Wickman S, Eyler C, Heddlest, et al. Targeting A20 decreases glioma stem cell survival and tumor growth. PLoS Biol. 2010;8:e1000319. doi: 10.1371/journal.pbio.1000319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Evron E, Umbricht CB, Korz D, Raman V, Loeb, et al. Loss of cyclin D2 expression in the majority of breast cancers is associated with promoter hypermethylation. Cancer Res. 2001;61:2782–2787. [PubMed] [Google Scholar]
- 23.Kobayashi T, Nakamura E, Shimizu Y. Restoration of cyclin D2 has an inhibitory potential on the proliferation of LNCaP cells. Biochem Biophys Res Commun. 2009;387:196–201. doi: 10.1016/j.bbrc.2009.06.146. [DOI] [PubMed] [Google Scholar]
- 24.Yang YA, Morin PJ, Han WF, Chen T, Bornman DM, et al. Regulation of fatty acid synthase expression in breast cancer by sterol regulatory element binding protein-1c. Exp Cell Res. 2003;2003;282:132–137. doi: 10.1016/s0014-4827(02)00023-x. [DOI] [PubMed] [Google Scholar]
- 25.Baron A, Migita T, Tang D, Loda M. Fatty acid synthase: a metabolic oncogene in prostate cancer? J Cell Biochem. 2004;2004;91:47–53. doi: 10.1002/jcb.10708. [DOI] [PubMed] [Google Scholar]
- 26.Alo' PL, Visca P, Marci A, Mangoni A, Botti C, et al. Expression of fatty acid synthase (FAS) as a predictor of recurrence in stage I breast carcinoma patients. Cancer. 1996;77:474–482. doi: 10.1002/(SICI)1097-0142(19960201)77:3<474::AID-CNCR8>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 27.Shah US, Dhir R, Gollin SM, Chandran UR, Lewis, et al. Fatty acid synthase gene overexpression and copy number gain in prostate adenocarcinoma. Hum Pathol. 2006;37:401–409. doi: 10.1016/j.humpath.2005.11.022. [DOI] [PubMed] [Google Scholar]
- 28.Migita T, Ruiz S, Fornari A, Fiorentino M, Priolo, et al. Fatty acid synthase: a metabolic enzyme and candidate oncogene in prostate cancer. J Natl Cancer Inst. 2009;101:519–532. doi: 10.1093/jnci/djp030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li J, Ding SF, Habib NA, Fermor BF, Wood CB, et al. Partial characterization of a cDNA for human stearoyl-CoA desaturase and changes in its mRNA expression in some normal and malignant tissues. Int J Cancer. 1994;57:348–352. doi: 10.1002/ijc.2910570310. [DOI] [PubMed] [Google Scholar]
- 30.Fritz V, Benfodda Z, Rodier G, Henriquet C, Iborra F, et al. Abrogation of de novo lipogenesis by stearoyl-CoA desaturase 1 inhibition interferes with oncogenic signaling and blocks prostate cancer progression in mice. Mol Cancer Ther. 2010;9:1740–1754. doi: 10.1158/1535-7163.MCT-09-1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Utsugi T, Schroit AJ, Connor J, Bucana CD, Fidler IJ. Elevated expression of phosphatidylserine in the outer membrane leaflet of human tumor cells and recognition by activated human blood monocytes. Cancer Res. 1991;11:3062–3066. [PubMed] [Google Scholar]