Abstract
OBJECTIVE
While prior studies describe the clinical presentation of patients requiring paramedic out-of-hospital endotracheal intubation (ETI), limited data characterize the underlying medical conditions or comorbidities. We sought to characterize the medical conditions and comorbidities of patients receiving successful paramedic out-of-hospital ETI.
METHODS
We used Pennsylvania statewide EMS clinical data, including all successful ETIs performed during 2003–2005. Using multiple imputation triple-match algorithms, we probabilistically linked EMS ETI to statewide death and hospital admission data. Each hospitalization record contained one primary and up to eight secondary diagnoses, classified according to the International Classification of Diseases, Clinical Modification, ninth edition (ICD-9-CM). We determined the proportion of patients in each major ICD-9-CM diagnostic group and subgroup. We calculated the Charlson Comorbidity Index for each patient. Using binomial proportions with confidence intervals, we analyzed the data and combined imputed results using Rubin's method.
RESULTS
Across the imputed sets, we linked 25,733 (77.7% linkage) successful ETI to death or hospital records; 56.3% died before and 43.7% survived to hospital admission. Of the 14,479 deaths before hospital admission, most (92.7%, 95% CI: 92.5–93.3%) presented to EMS in cardiac arrest. Of the 11,255 hospitalized patents, the leading primary diagnoses were circulatory diseases (32.0%, 30.2–33.7%), respiratory diseases (22.8%, 21.9–23.7%), and injury or poisoning (25.2%; 22.7–27.8%). Prominent primary diagnosis subgroups included: asphyxia and respiratory failure (15.2%), traumatic brain injury and skull fractures (11.3%), acute myocardial infarction and ischemic heart disease (10.9%), poisoning, drug and alcohol disorders (6.7%), dysrhythmias (6.7%), hemorrhagic and non-hemorrhagic stroke (5.9%), acute heart failure and cardiomyopathies (5.6%), pneumonia and aspiration (4.9%), and sepsis, septicemia and septic shock (3.2%). Most of the admitted ETI patients had a secondary circulatory (70.8%), respiratory (61.4%), or endocrine, nutritional or metabolic secondary diagnosis (51.4%). The mean Charlson Index score was 1.6 (95% CI: 1.5–1.7).
CONCLUSIONS
The majority of successful paramedic ETI occur on patients with cardiac arrest, circulatory and respiratory conditions. Injury, poisoning and other conditions compromise smaller but important portions. ETI patients have multiple comorbidities. These findings may guide the systemic planning of paramedic airway management care and education.
Keywords: Emergency Medical Services, Paramedics, Intubation Intratracheal, Comorbidities
INTRODUCTION
Endotracheal intubation (ETI) is a key intervention performed by paramedics in the United States.1–9 Prior studies indicate that the most frequent episodes of out-of-hospital ETI occur in patients suffering cardiac arrest, with the remaining ETIs occurring in patients with a range of undifferentiated non-arrest medical and trauma conditions.10–12 However, we know little about the medical conditions associated with paramedic ETI. This information is important because different medical conditions may require unique airway management or ventilation strategies. For example, patients with traumatic brain injury may merit drug-facilitated ETI.13,14 Patients with acute heart failure may respond to non-invasive ventilation with continuous positive airway pressure (CPAP).15,16 Furthermore, coexisting medical comorbidities may complicate airway management and ventilatory strategies as well as the outcomes of these patients.
An improved systemic understanding of the medical conditions and comorbidities associated with paramedic ETI could aid EMS system planning, helping medical directors to identify the range of strategies and training curricula needed for paramedic airway management. We sought to describe the medical conditions and comorbidities of patients receiving successful paramedic out-of-hospital ETI.
METHODS
Study Design
The Institutional Review Boards of the University of Alabama at Birmingham and University of Pittsburgh approved the study. In this retrospective analysis, we linked Commonwealth of Pennsylvania statewide EMS, hospital discharge and death data to determine the hospital discharge diagnoses of patients receiving successful out-of-hospital ETI.
Study Setting
This study included patients receiving out-of-hospital care in the Commonwealth of Pennsylvania. EMS care in Pennsylvania encompasses a range of practice settings including dense urban population centers (for example, Philadelphia and Pittsburgh), extensive suburban and remote rural areas. Care configurations include independent private and municipal agencies providing both local and regional EMS care. There are 11 independent air medical services across the Commonwealth.
Pennsylvania EMS rescuers work in both volunteer and career capacities. EMS roles in Pennsylvania include first responders, emergency medical technicians, paramedics, prehospital registered nurses and EMS physicians. Advanced life support (ALS) vehicles may have one or two ALS rescuers. Only EMS paramedics, nurses and physicians perform out-of-hospital ETI. Paramedics comprise over 90% of Pennsylvania ALS rescuers. All air medical rescuers may use neuromuscular-blockade assisted (rapid-sequence) ETI. Only select ground EMS units are permitted to use ETI facilitated by sedatives-only; ground EMS units are not permitted to perform neuromuscular-blockade assisted (rapid-sequence) ETI
Sources of Data
For this study we used three sources of data: 1) Pennsylvania Emergency Medical Services Patient Care Report (PAEMS) data, 2) Pennsylvania Health Care Cost Containment Council hospital discharge data set (PHC4), and 3) Pennsylvania Death Registry (PA Death). We used data for the three-year period January 1, 2003 through December 31, 2005.
PAEMS is a database of all Pennsylvania EMS patient care incidents. EMS agencies in Pennsylvania use electronic medical record systems that transmit patient care data to a central database. EMS services without computer access must submit patient care reports using computer scan forms. PAEMS follows the National Highway Traffic Safety Administration standards for EMS data collection and reporting. The data describe patient characteristics, nature and severity of illness, injury patterns, administered drugs, procedures and interventions, and information regarding the EMS service and out-of-hospital rescuers delivering care.17
PHC4 contains demographic, diagnostic and clinical information for all hospital discharges in the Commonwealth of Pennsylvania.18 Using standard reporting software, hospitals provide basic demographic (patient age, sex), clinical (the date, time, and location of hospital admission, the discharge status and hospital length of stay) and diagnostic information. The data base contains a primary and up to eight secondary discharge diagnoses, defined using the International Classification of Diseases, Clinical Modification, ninth edition (ICD-9-CM). PHC4 does not include patients dying in the Emergency Department (ED) prior to hospital admission.
PA Death contains demographic and clinical information on all deaths in the Commonwealth of Pennsylvania, including the date, time, location and attributed reason for death.19
Linkage of Data Sets
Because the three data sets (PAEMS, PHC4, PA Death) did not have unique patient identifiers (for example, name, social security number, date of birth, medical record number, etc.), we connected patient records using probabilistic linkage. Probabilistic linkage compares the values from several data fields to estimate the probability that pairs of records represent the same person or event.20–23 Many medical research studies have used probabilistic linkage.24–30
We previously described the details and results of the record linking process.10 To facilitate linkage, we limited PAEMS to successful ETI cases, and we limited PHC4 to patients 1) admitted through the Emergency Department and 2) admitted to an intensive care unit or discharged with a diagnosis of mechanical ventilation (ICD-9p 96.7–96.72), cardiopulmonary arrest (ICD-9-CM 427.4–427.5) or respiratory arrest (ICD-9-CM 799.1).
The probabilistic linking process used combinations of the following variables: date and time of encounter, patient age, patient sex, patient race, receiving hospital facility, EMS agency location and patient geographic location (minor civil division). Since an EMS patient might appear in both the PHC4 and PA Death data sets, we used a “triple match” algorithm to resolve these overlapping linkages.31
A customary practice in probabilistic linkage is to retain only record pairs with predicted match weights over an a priori fixed threshold (-e.g., match probability >0.90).32 However, this approach often results in low match rates and may inadvertently exclude true matches just below the defined threshold. To avoid this outcome, we used a multiple imputation procedure, creating a series of linked data sets based upon the probability distribution of match weights.31 Using this technique we created five probability linked data sets. We conducted separate analyses on each probability linked data set and combined the estimates using Rubin's method.33,34
We linked patient records for the period January 1, 2003 – December 31, 2005. We performed record linkage using Linksolv, version 6 (Strategic Matching Inc., Morrisonville, New York).
Selection of Patients
We included patients reported as receiving successful out-of-hospital ETI by ALS rescuers. The PAEMS data set does not contain information on unsuccessful ETIs. Rescuers define and report ETI success; there are no statewide protocols for independent confirmation by a second rescuer or physician. The PAEMS cannot identify instances where initial ETI failure was followed by successful supraglottic airway placement.
Outcomes
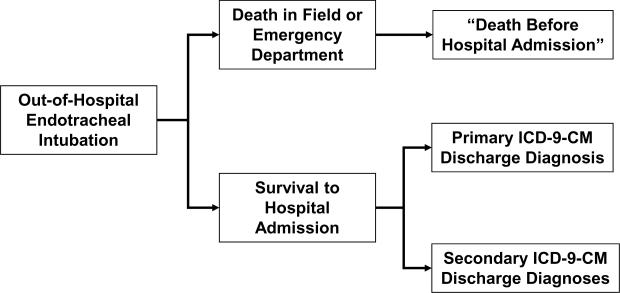
The outcomes of this study were the patient primary and secondary medical conditions. We determined and classified the outcomes differently for patients dying before hospital admission and those admitted to the hospital. (Figure)
FIGURE.
Overview of medical condition classification. We classified patients dying in the field or ED as “Death Before Hospital Admission.” For patients surviving to hospital admission, we determined the primary and secondary medical conditions from the primary and secondary ICD-9-CM discharge diagnosis codes. Each hospitalized patient had one primary and up to 8 secondary diagnoses. ETI = Endotracheal Intubation. ED = Emergency Department. ICD-9-CM = International Classification of Diseases, Clinical Modification, ninth edition.
We classified patients dying in the field or Emergency Department as “Death Before Hospital Admission.” Patients dying before hospital admission do not appear in the hospital discharge data set and therefore do not have assigned ICD-9-CM discharge diagnosis codes. Due to the inconsistency of death reports and their use of the different ICD-10 classification system, we opted not to use the “reason for death” data appearing in the PA Death data set.
For patients surviving to hospital admission, we determined the primary and secondary medical conditions from ICD-9-CM hospital discharge diagnosis codes appearing in the PHC4 data set. At the completion of a patient's hospital course, hospital personnel typically assign diagnosis codes (International Classification of Diseases, ninth edition (ICD-9)) reflecting the medical conditions associated with the patient's hospitalization, as well as the patient's comorbidities. Hospitals typically use this information to support billing efforts. PHC4 contains the primary and up to eight secondary ICD-9-CM diagnosis codes for each hospitalization.
To examine the concurrent medical conditions of the study population, we also calculated Charlson comorbidity index scores for each hospitalized patient.35 The Charlson index is a widely used system for characterizing patient comorbidities, drawing upon information regarding 17 chronic medical conditions (myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, rheumatologic disease, peptic ulcer disease, liver disease, diabetes, hemiplegia or paraplegia, renal disease, cancer, and acquired immunodeficiency disease syndrome (AIDS)). Each condition receives a different weight (1, 2 or 6 points). The total Charlson score consists of the sum of the individual weighted scores and ranges from 0–37, reflecting increasing risks of one-year mortality. For example, a patient with a history of myocardial infarction has Charlson Score of 1, corresponding to 10% probability of death within one year.36 For example, a patient with a history of myocardial infarction and leukemia has Charlson Score of 2, corresponding to 19% probability of death within one year. In scientific analyses, authors typically categorize the Charlson score as 0, 1, 2 or ≥3. Deyo, et al. adapted the Charlson index for use with ICD-9-CM administrative data sets.37
Primary Data Analysis
We grouped the primary and secondary discharge diagnoses of admitted ETI patients according to major ICD-9-CM disease categories. (Table) We opted to group the cases using the ICD-9-CM system due to the wide recognition of this method.
TABLE.
Discharge diagnoses of patients receiving out-of-hospital endotracheal intubation, Commonwealth of Pennsylvania 2003–2005. Percentages reflect estimates for each imputed set, combined by Rubin's method. Each hospital record contained one primary discharge diagnosis and up to eight secondary discharge diagnoses.
| ICD-9-CM Diagnosis Category | Primary Diagnosis (All ETI Patients, n=25,733) | Primary Diagnosis (Admitted Patients Only, n=11,255) | Secondary Diagnoses (Admitted Patients Only, n=11,255) |
|---|---|---|---|
| n (%; 95% CI) | n (%; 95% CI) | n (%; 95% CI) | |
| Patient Not Admitted to Hospital (Died Before Hospital Admission) | 14,488 (56.3; 51.3–61.2) | N/A (N/A) | N/A (N/A) |
| 001–139.9 Infectious and Parasitic Diseases | 389 (1.5; 1.2–1.9) | 394 (3.5; 3.0–3.9) | 1,373 (12.2; 11.4–12.9) |
| 003.1, 022.3, 031.2, 038–038.9, 040.82, 422.92, 449, 659.3, 670.20–670.24, 673.3, 771.81, 771.83, 785.52, 790.7, 995.90–995.94 | 360 (1.4; 1.0–1.8) | 360 (3.2; 2.7–3.7) | 912 (8.1; 7.2–9.1) |
| Sepsis, Septicemia, Bacteremia and Septic Shock | |||
| 140–239.9 Neoplasms (-e.g., Cancers, Tumors and Malignancies) | 157 (0.6; 0.4–0.8) | 158 (1.4; 1.1–1.7) | 608 (5.4; 4.8–6.0) |
| 240–279.9 Endocrine, Nutritional and Metabolic Diseases, and Immunity Disorders | 180 (0.7; 0.5–0.8) | 169 (1.5; 1.3–1.7) | 5,785 (51.4; 50.1–52.7) |
| 250–250.9, 251.0–251.2 - Diabetic, Hyperglycemic and Hypoglycemic Conditions | 90 (0.35; 0.28–0.43) | 90 (0.8; 0.6–1.0) | 2,094 (18.6; 17.9–19.4) |
| 280–289.9 Diseases of the Blood and Blood-Forming Organs | 31 (0.12; 0.06–0.17) | 34 (0.3; 0.1–0.4) | 1,801 (16.0; 15.3–16.7) |
| 290–319.9 Mental Disorders (including alcohol and drug-related disorders) | 67 (0.26; 0.18–0.33) | 68 (0.6; 0.4–0.7) | 3,084 (27.4; 25.6–29.2) |
| 320–359.9 Diseases of the Nervous System | 206 (0.8; 0.5–1.1) | 203 (1.8; 1.3–2.3) | 2,307 (20.5; 17.1–24.0) |
| 345–345.91, 649.40–649.44, 779.0, 780.3–780.39 | 79 (0.7; 0.6–0.8) | 169 (1.5; 1.3–1.8) | 968 (8.6; 8.0–9.3) |
| Epilepsy, Seizures and Convulsions | |||
| 348.1–348.39, 349.82 - Anoxic Brain Injury and Encephalopathy | 45 (0.4; 0.2–0.7) | 113 (1.0; 0.5–1.4) | 1,249 (11.1; 7.5–14.7) |
| 360–389.9 Diseases of the Sense Organs (-e.g, Eyes, Ears) | 10 (0.04; 0.01–0.07) | 11 (0.10; 0.03–0.17) | 315 (2.8; 2.5–3.2) |
| 390–459.9 Diseases of the Circulatory System | 3,603 (14.0; 11.7–16.3) | 3,602 (32.0; 30.2–33.7) | 7,969 (70.8; 68.2–73.4) |
| 410–414.9 - Acute Myocardial Infarction and Ischemic Heart Disease | 1,235 (4.8; 3.9–5.6) | 1,227 (10.9; 10.0–11.8) | 2,994 (26.6; 25.6–27.6) |
| 415.1–415.19 - Pulmonary Embolism | 28 (0.25; 0.18–0.33) | 68 (0.6; 0.4–0.7) | 68 (0.6; 0.4–0.7) |
| 426–427.9 - Dysrhythmias | 746 (2.9; 2.2–3.6) | 754 (6.7; 5.8–7.6) | 3,658 (32.5; 29.3–35.7) |
| 425, 425.1–425.2, 425.4–425.9, 428–428.9 | 643 (2.5; 2.2–2.7) | 630 (5.6; 5.1–6.1) | 2,668 (23.7; 22.6–24.8) |
| Acute Heart Failure and Cardiomyopathies | |||
| 430–432.9 - Hemorrhagic Stroke | 360 (1.4; 1.2–1.7) | 371 (3.3; 2.9–3.6) | 101 (0.9; 0.7–1.0) |
| 433.0–437.9 - Thrombotic and Other Strokes | 124 (1.1; 0.8–1.4) | 293 (2.6; 2.1–3.0) | 326 (2.9; 2.4–3.3) |
| 460–519.9 Diseases of the Respiratory System | 2,573 (10.0; 8.7–11.3) | 2,566 (22.8; 21.9–23.7) | 6,911 (61.4; 59.7–63.2) |
| 464–466.19, 480–488.9, 507–507.8, 510–510.9, 513–513.1 | 540 (2.1; 1.8–2.5) | 552 (4.9; 4.4–5.3) | 2,364 (21.0; 20.1–22.0) |
| Pneumonia, Aspiration Pneumonitis and Other Infections | |||
| 490–493.92 - Asthma, COPD and Chronic Bronchitis | 257 (1.0; 0.8–1.1) | 248 (2.2; 1.9–2.5) | 1,317 (11.7; 11.1–12.4) |
| 518.5, 518.81–518.85, 799.0–799.1 - Asphyxia and Respiratory Failure | 1,698 (6.6; 5.8–7.5) | 1,711 (15.2; 14.5–15.9) | 3,928 (34.9; 33.1–36.7) |
| 520–579.9 Diseases of the Digestive System | 437 (1.7; 1.4–1.9) | 428 (3.8; 3.4–4.2) | 1,936 (17.2; 16.2–18.2) |
| 580–629.9 Diseases of the Genitourinary System | 129 (0.5; 0.4–0.6) | 135 (1.2; 1.0–1.4) | 2,881 (25.6; 23.7–27.5) |
| 584–586 - Acute and Chronic Renal Failure | 77 (0.3; 0.2–0.4) | 79 (0.7; 0.6–0.9) | 1,463 (13.0; 10.9–15.1) |
| 680–709.9 Diseases of the Skin and Subcutaneous Tissue (includes cellulitis) | 15 (0.06; 0.02–0.09) | 15 (0.13; 0.06–0.21) | 574 (5.1; 4.6–5.5) |
| 710–739.9 Diseases of the Musculoskeletal System and Connective Tissue | 36 (0.14; 0.09–0.19) | 34 (0.3; 0.2–0.4) | 1,047 (9.3; 8.7–10.0) |
| 740–759.9 Congenital Anomalies | 5 (0.02; 0.000003–0.03) | 5 (0.04; 0.000004–0.07) | 79 (0.7; 0.6–0.9) |
| 760–779.9 Certain Conditions Originating in the Perinatal Period | 3 (0.01; [−0.002]–0.03) | 3 (0.03; [−0.00003]–0.06) | 10 (0.09; 0.04–0.2) |
| 780–799.9 Symptoms, Signs, and Ill-Defined Conditions | 566 (2.2; 2.0–2.4) | 574 (5.1; 4.6–5.7) | 3,433 (30.5; 29.2–31.9) |
| 780.0–780.2, 780.97 - Syncope, Coma and Altered Mental Status | 51 (0.45; 0.36–0.55) | 113 (1.0; 0.8–1.2) | 450 (4.0; 3.6–4.4) |
| 786.5–786.59 - Chest Pain | 113 (1.0; 0.8–1.1) | 248 (2.2; 1.9–2.5) | 1,317 (11.7; 11.1–12.4) |
| 276.5–276.52, 458–458.9, 785.5–785.51, 785.59, 958.4, 995.0, 999.4 | 77 (0.3; 0.2–0.4) | 79 (0.7; 0.5–0.8) | 1,576 (14.0; 12.7–15.2) |
| Shock, Hypovolemia, Dehydration, Hypotension and Anaphylaxis | |||
| 800–999.9 Injury and Poisoning | 2,831 (11.0; 10.6–11.4) | 2,836 (25.2; 22.7–27.8) | 3,084 (27.4; 25.3–29.4) |
| 800–804.9, 850–854.9, 959.0–959.09 - Skull Fractures and Traumatic Brain Injury | 1,287 (5.0; 4.7–5.2) | 1,272 (11.3; 10.0–12.6) | 822 (7.3; 6.2–8.3) |
| 805–806.9, 952–952.9 - Fractures of Spine and Spinal Cord Injuries | 69 (0.27; 0.20–0.33) | 68 (0.6; 0.5–0.8) | 416 (3.7; 3.1–4.3) |
| 807–839.9, 885–887.7, 895–897.7, 900–904.9, 925–929 | 232 (0.9; 0.8–1.0) | 236 (2.1; 1.7–2.4) | 867 (7.7; 6.8–8.6) |
| Other Fractures, Dislocations, Amputations, Crush and Vascular Injuries | |||
| 860–869.9 - Internal Injury of Chest, Abdomen, and Pelvis | 257 (1.0; 0.8–1.1) | 248 (2.2; 1.8–2.6) | 754 (6.7; 5.7–7.7) |
| 940–949.9 - Burns | 49 (0.19; 0.13–0.24) | 45 (0.4; 0.3–0.6) | 45 (0.4; 0.3–0.6) |
| 291–292.9, 303.0–305.9, 960–989.9 - Poisonings, drug and alcohol disorders | 746 (2.9; 2.7–3.2) | 754 (6.7; 5.9–7.5) | 1,891 (16.8; 15.3–18.3) |
In addition to the major ICD-9-CM categories, we also highlighted selected disease subgroups with potential relevance to airway management. We defined a subgroup for sepsis, septicemia, bacteremia and septic shock (003.1, 022.3, 031.2, 038–038.9, 040.82, 422.92, 449, 659.3, 670.20–670.24, 673.3, 771.81, 771.83, 785.52, 790.7, 995.90–995.94). Under endocrine disorders we identified the subgroup with diabetes, hypoglycemia and hyperglycemia conditions (ICD-9-CM 250–250.9, 251.0–251.2). Under neurological disorders we identified epilepsy, seizures and convulsions (ICD-9-CM 345–345.91, 649.40–649.44, 779.0, 780.3–780.39) as well as anoxic brain injury and encephalopathy (348.1–348.39, 349.82).
Circulatory system disease subgroups included myocardial infarction and ischemic heart disease (ICD-9-CM 410–414.9), pulmonary embolism (415.1–415.19), dysrhythmias (425–427.9), congestive heart failure and cardiomyopathies (425, 425.1–425.2, 425.4–425.9, 428–428.9), and hemorrhagic (430–432.9) and thrombotic stroke (433.437.9). Respiratory disease subgroups included pneumonia and influenza (ICD-9-CM 480–488.9), chronic obstructive pulmonary disease and allied conditions (490–496.9), and other respiratory diseases (510–519.9). Among genitourinary disorders we identified acute and chronic renal failure (584–586).
Injury subgroups included skull fractures and traumatic brain injury (ICD-9-CM 800–804.9, 850–854.9, 959.0–959.09), spinal fractures and spinal cord injuries (805–806.9, 952–952.9), limb fractures, dislocations, amputations, crush and vascular injuries (807–839.9, 885–887.7, 895–897.7, 900–904.9, 925–929), chest, abdomen and pelvis internal injuries (860–869.9) and burns (940–949.9). We identified all poisonings, drug and alcohol disorders (291–292.9, 303.0–305.9, 960–989.9).
Under symptoms, signs and ill-defined conditions, we identified the subgroup syncope, coma and altered mental status (780.0–780.2, 780.97), chest pain (786.5–786.59), and shock, hypovolemia, dehydration, hypotension and anaphylaxis (276.5–276.52, 458–458.9, 785.5–785.51, 785.59, 958.4, 995.0, 999.4).
We analyzed the data using descriptive statistics. For each of the five imputed match sets, we examined the primary discharge diagnosis, calculating the binomial proportion of cases in each major ICD-9-CM disease category and subgroup. We determined the proportion of each disease category and subgroup relative to all successful ETI as well as to admitted patients only. We analyzed the secondary diagnoses in a similar fashion, examining all eight secondary discharge diagnoses of admitted patients and calculating the proportion of each secondary disease category relative to admitted patients only.
Utilizing the primary and all eight secondary discharge diagnoses, we calculated the Charlson comorbidity index using the Stata “Charlson” module. Combining the primary and secondary diagnoses and the Charlson score allowed estimations from each of the five imputed match sets using Rubin's method, implemented using the Stata “mi” command.33 Because Rubin's method cannot combine medians, we examined the Charlson median and interquartile range for each imputed set separately. We analyzed the data using Stata 11.2 (Stata, Inc., College Station, Texas).
RESULTS
During 2003–2005, 4,846 rescuers performed successful ETI on 33,117 patients. The 33,117 ETI patients included 21,753 with cardiac arrest, 8,162 with medical non-arrest conditions and 3,202 with trauma non-arrest ETI. Across the five imputed probability linked data sets, we matched a mean of 25,733 of 33,117 successful ETI to hospital or death records (mean linkage rate 77.7%).
Of ETI cases matched to hospital and/or death records across the five imputations, a mean of 14,487 (56.3%; 95% CI: 51.3–61.2) died prior to hospital admission. (Table) Most of the deaths prior to hospital admission suffered non-traumatic out-of-hospital cardiac arrest (92.7%, 95% CI: 92.5–93.3%).
Across the five imputations we linked a mean of 11,255 successful ETI to hospitalization records. The mean age was 61 years (95% CI: 60–63), and the cohort was mostly male (56%; 95% CI: 55–57%). Of the hospitalized patients, the leading primary diagnosis groups were circulatory diseases (32.0%, 30.2–33.7%), respiratory diseases (22.8%, 21.9–23.7%), and injury or poisoning (25.2%; 22.7–27.8%), collectively comprising over 80% of the hospitalized cases. Prominent primary diagnosis subgroups included: asphyxia and respiratory failure (15.2%), traumatic brain injury and skull fractures (11.3%), acute myocardial infarction and ischemic heart disease (10.9%), poisoning, drug and alcohol disorders (6.7%), dysrhythmias (6.7%), hemorrhagic and non-hemorrhagic stroke (5.9%), acute heart failure and cardiomyopathies (5.6%), pneumonia and aspiration (4.9%), and sepsis, septicemia and septic shock (3.2%).
Most of the admitted ETI patients had secondary circulatory (70.8%), respiratory (61.4%), or endocrine, nutritional or metabolic secondary diagnoses (51.4%). Combined across the five imputed data sets, the mean Charlson Index score was 1.6 (95% CI: 1.5–1.7). Within each of the five imputed data set, the median Charlson Index score was 1 (IQR: 0–2, min 0, max 11).
DISCUSSION
The diseases afflicting out-of-hospital patients are often unclear on initial field presentation and may require confirmation – or discovery – in the hospital. In the setting of out-of-hospital ETI, knowledge of the pattern of illnesses when the current cause is uncertain is important not only for optimizing the care required by individual patients but also for understanding the spectrum of medical conditions associated with out-of-hospital airway management. Similar to prior studies, we observed that the majority of paramedic ETIs occur on patients with out-of-hospital cardiac arrest.11,12 However, we also found that circulatory and respiratory diseases, injuries and poisonings comprised most of the remaining cases. While our use of hospital discharge diagnoses could be subject to classification bias, this method provided the best available approach, capitalizing on existing data from a large number of cases (over 11,000 hospitalizations after successful out-of-hospital ETI). Prospective ETI case identification and review would have proved logistically prohibitive.
While diagnostic information could influence airway management methods for individual patients, in aggregate they may also guide EMS system planning and education, identifying the relative range and frequency of specific medical conditions associated with paramedic ETI. Medical directors could use this information to define and prioritize airway management options and strategies for EMS agencies. For example, to avoid interruptions in cardiopulmonary resuscitation chest compressions, some EMS practitioners use supraglottic alternate airways (King LT, Combitube) for cardiac arrest airway management; our series suggest that this strategy may have a role in over half of out-of-hospital airway management efforts.38,39 Rapid-sequence intubation is a viable strategy for facilitating ventilation and intracerebral pressure control in traumatic brain injury; our observations suggest a potential role for this approach in approximately 5% of out-of-hospital ETI.14,40,41 As a potential ventilatory management strategy for acute heart failure, asthma and pneumonia, continuous positive airway pressure (CPAP) may play a role in approximately 12% of the patients in this series.15 16
Our study also highlights disease groups that often receive less emphasis in out-of-hospital airway care. For example, those with poisonings, alcohol and drug overdoses received 6.7% of ETI efforts, and hemorrhagic or non-hemorrhagic stroke patients received over 6% of successful ETI efforts. Three percent of successful ETI cases involved sepsis, septicemia, bacteremia or septic shock. These conditions may require specialized airway management approaches. For example, ventilation and intracerebral pressure control are important in the management of stroke patients and may merit pharmacologic assisted intubation or other neuroprotective approaches.14 Given the concerns with the etomidate-induced adrenosuppression, the sepsis, septicemia, bacteremia or septic shock cases may merit ETI facilitated by alternative sedative/induction agents.42,43 These less common yet prominent conditions pose a challenge to medical directors, who must balance the need for specialized airway management strategies against the relatively limited opportunities for application by individual paramedics.
Over half of the admitted patients receiving field ETI had secondary circulatory, respiratory, or endocrine, nutrition or metabolic conditions (for example, hypoglycemia and electrolyte abnormalities). The mean Charlson Index score of 1.6 exhibited by these patients indicate a population with a moderate number of comorbidities.35 These observations underscore the need for ETI strategies that accommodate the presence of multiple comorbidities. For example, select patients may have reduced pulmonary reserve, limiting their tolerance of repeated or prolonged intubation efforts. Other patients may not be able to tolerate sedation-facilitated intubation using full unadjusted doses of medications. Our findings also highlight that studies of paramedic ETI must account for the confounding effect of comorbidities and severity of illness.3,8,44,45 Prior studies have used out-of-hospital variables or the Mediqual Severity of Illness Index to adjust for severity of illness, but these approaches have not been independently validated.3,10,46 The observed comorbidities in this series highlight the need for risk adjustment strategies specific to the out-of-hospital ETI population.
LIMITATIONS
Because the study data sets did not contain unique identifiers, we relied on probabilistic record linkage, which represented the best approach given the inherent data set limitations. Using multiple imputation methods with the available variables, our study achieved a linkage rate of 77.7%, which is compares favorably with prior efforts that achieved linkage on the order of 45–70%.47–49 While linkage rates can be higher with a greater number of variables, we were limited to the variables available across the PAEMS, PHC4 and PA Death data sets.23,32
Our study evaluated out-of-hospital ETI practice in Pennsylvania only. Although we drew upon a large number of ETI, different patterns may exist in other US regions. Medical directors must compare these findings with the characteristics of their individual practice setting. We did not have data on ETI or other complications, such as bleeding, vomiting, tube misplacement, inadvertent hyperventilation or prolonged ETI efforts.40,50–52 We used administrative data based upon rescuer clinical reports. While paramedic clinical care reports may be subject to recall and reporting bias, these factors would not have changed the results of the study.
PAEMS contained reportedly successful ETI only. Up to 15% of out-of-hospital ETI efforts may fail.11,12 We were unable to determine the discharge diagnoses of patients experiencing failed ETI efforts. The PAEMS data set did not have data on other performance parameters such as number of attempts or the contingency use of a supraglottic airway. The study data originated from 2000–2005. Since this time the Commonwealth of Pennsylvania implemented select airway protocol changes (for example, the mandatory use of waveform capnography) but none that would have changed the findings of the current study.
Despite maximizing linkage with multiple imputation methods, we still lack clinical information on non-linked cases. We used administrative EMS, hospital and death records, which may be subject to reporting bias. Medical record personnel at individual hospitals assigned discharge primary and secondary diagnoses, a process primarily designed for financial purposes.
While this analysis posits a connection between initial clinical presentation and final hospital diagnoses, a direct association may not always exist. For example, a patient with an initial presentation of cellulitis may later die from aspiration pneumonia and sepsis. We surmised that the majority of deaths before hospitalization consisted of those experiencing non-traumatic cardiac arrest. However, approximately 30% of out-of-hospital arrest patients survive to hospital admission; in this analysis, these patients would have likely received a primary discharge diagnosis other than cardiopulmonary arrest.53 The data sets could not ascertain the diagnoses of patients dying in the field or the emergency department.
CONCLUSION
The majority of paramedic ETI occurs on patients with cardiac arrest, circulatory and respiratory conditions. Injury, poisoning and other conditions compromise smaller portions of the paramedic ETI pool, and many patients have multiple comorbidities. These findings may guide the systemic planning of paramedic airway management care and education.
ACKNOWLEDGEMENTS
This study was supported by National Heart, Lung and Blood Institute grant R21-HL084528. Dr. Wang received support from Clinical Scientist Development Award K08-HS013628 from the Agency for Health Care Research and Quality, Rockville, Maryland. The funders had no direct role in the design or execution of the study or the composition of the resulting manuscript. The authors declare no financial or other conflicts of interest.
Footnotes
Presented at: National Association of EMS Physicians Annual Meeting, Jacksonville, Florida, January 2009
REFERENCES
- 1.Wang HE, Yealy DM. Out-of-hospital endotracheal intubation: where are we? Ann Emerg Med. 2006;47:532–41. doi: 10.1016/j.annemergmed.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 2.Hubble MW, Brown L, Wilfong DA, Hertelendy A, Benner RW, Richards ME. A meta-analysis of prehospital airway control techniques part I: orotracheal and nasotracheal intubation success rates. Prehosp Emerg Care. 2010;14:377–401. doi: 10.3109/10903121003790173. [DOI] [PubMed] [Google Scholar]
- 3.Wang HE, Peitzman AB, Cassidy LD, Adelson PD, Yealy DM. Out-of-hospital endotracheal intubation and outcome after traumatic brain injury. Ann Emerg Med. 2004;44:439–50. doi: 10.1016/j.annemergmed.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 4.Egly J, Custodio D, Bishop N, et al. Assessing the impact of prehospital intubation on survival in out-of-hospital cardiac arrest. Prehosp Emerg Care. 2011;15:44–9. doi: 10.3109/10903127.2010.514090. [DOI] [PubMed] [Google Scholar]
- 5.Hanif MA, Kaji AH, Niemann JT. Advanced airway management does not improve outcome of out-of-hospital cardiac arrest. Acad Emerg Med. 2010;17:926–31. doi: 10.1111/j.1553-2712.2010.00829.x. [DOI] [PubMed] [Google Scholar]
- 6.Thomas S, Judge T, Lowell MJ, et al. Airway management success and hypoxemia rates in air and ground critical care transport: a prospective multicenter study. Prehosp Emerg Care. 2010;14:283. doi: 10.3109/10903127.2010.481758. [DOI] [PubMed] [Google Scholar]
- 7.Gausche M, Lewis RJ, Stratton SJ, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: a controlled clinical trial. JAMA. 2000;283:783–90. doi: 10.1001/jama.283.6.783. [DOI] [PubMed] [Google Scholar]
- 8.Studnek JR, Thestrup L, Vandeventer S, et al. The association between prehospital endotracheal intubation attempts and survival to hospital discharge among out-of-hospital cardiac arrest patients. Acad Emerg Med. 2010;17:918–25. doi: 10.1111/j.1553-2712.2010.00827.x. [DOI] [PubMed] [Google Scholar]
- 9.Davis DP, Koprowicz KM, Newgard CD, et al. The Relationship between Out-of-Hospital Airway Management and Outcome among Trauma Patients with Glasgow Coma Scale Scores of 8 or Less. Prehosp Emerg Care. 2011;Early Online:1–9. doi: 10.3109/10903127.2010.545473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang HE, Balasubramani GK, Cook LJ, Lave JR, Yealy DM. Out-of-hospital endotracheal intubation experience and patient outcomes. Ann Emerg Med. 2010;55:527–37. doi: 10.1016/j.annemergmed.2009.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang HE, O'Connor RE, Schnyder ME, Barnes TA, Megargel RE. Patient status and time to intubation in the assessment of prehospital intubation performance. Prehosp Emerg Care. 2001;5:10–8. doi: 10.1080/10903120190940254. [DOI] [PubMed] [Google Scholar]
- 12.Wang HE, Kupas DF, Paris PM, Bates RR, Yealy DM. Preliminary experience with a prospective, multi-centered evaluation of out-of-hospital endotracheal intubation. Resuscitation. 2003;58:49–58. doi: 10.1016/s0300-9572(03)00058-3. [DOI] [PubMed] [Google Scholar]
- 13.Ochs M, Davis D, Hoyt D, Bailey D, Marshall L, Rosen P. Paramedic-performed rapid sequence intubation of severely head-injured patients. Ann Emerg Med. 2002 doi: 10.1067/mem.2002.126397. [DOI] [PubMed] [Google Scholar]
- 14.Wang HE, Davis DP, O'Connor RE, Domeier RM. Drug-assisted intubation in the prehospital setting (resource document to NAEMSP position statement) Prehosp Emerg Care. 2006;10:261–71. doi: 10.1080/10903120500541506. [DOI] [PubMed] [Google Scholar]
- 15.Thompson J, Petrie DA, Ackroyd-Stolarz S, Bardua DJ. Out-of-hospital continuous positive airway pressure ventilation versus usual care in acute respiratory failure: a randomized controlled trial. Ann Emerg Med. 2008;52:232–41. doi: 10.1016/j.annemergmed.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 16.Hubble MW, Richards ME, Jarvis R, Millikan T, Young D. Effectiveness of prehospital continuous positive airway pressure in the management of acute pulmonary edema. Prehosp Emerg Care. 2006;10:430–9. doi: 10.1080/10903120600884848. [DOI] [PubMed] [Google Scholar]
- 17.Spaite D, Benoit R, Brown D, et al. Uniform Prehospital Data Elements and Definitions: A Report From the Uniform Prehospital Emergency Medical Services Data Conference. Ann Emerg Med. 1995;25:525–31. doi: 10.1016/s0196-0644(95)70271-7. [DOI] [PubMed] [Google Scholar]
- 18.Pennsylvania Health Care Cost Containment Council [Accessed March 20, 2008];2008 www.phc4.org.
- 19.Pennsylvania Department of Health, Division of Vital Records [Accessed March 20, 2008];Death Records. 2008 http://www.dsf.health.state.pa.us/health/cwp/view.asp?a=168&Q=202275.
- 20.Fellegi I, Sunter A. A theory for record linkage. J Am Stat Assoc. 1969;64:1183–210. [Google Scholar]
- 21.Jaro MA. Probabilistic linkage of large public health data files. Stat Med. 1995;14:491–8. doi: 10.1002/sim.4780140510. [DOI] [PubMed] [Google Scholar]
- 22.Newcombe H, Kennedy J. Record Linkage. Comun Assoc Computing Machinery. 1962;5:563–6. [Google Scholar]
- 23.Newgard CD. Validation of probabilistic linkage to match de-identified ambulance records to a state trauma registry. Acad Emerg Med. 2006;13:69–75. doi: 10.1197/j.aem.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 24.Cercarelli LR, Rosman DL, Ryan GA. Comparison of accident and emergency with police road injury data. J Trauma. 1996;40:805–9. doi: 10.1097/00005373-199605000-00021. [DOI] [PubMed] [Google Scholar]
- 25.Overpeck MD, Hoffman HJ, Prager K. The lowest birth-weight infants and the US infant mortality rate: NCHS 1983 linked birth/infant death data. Am J Public Health. 1992;82:441–4. doi: 10.2105/ajph.82.3.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Henderson J, Goldacre MJ, Graveney MJ, Simmons HM. Use of medical record linkage to study readmission rates. BMJ. 1989;299:709–13. doi: 10.1136/bmj.299.6701.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goldacre MJ, Simmons H, Henderson J, Gill LE. Trends in episode based and person based rates of admission to hospital in the Oxford record linkage study area. BMJ. 1988;296:583–5. doi: 10.1136/bmj.296.6621.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Henderson J, Goldacre MJ, Griffith M. Hospital care for the elderly in the final year of life: a population based study. BMJ. 1990;301:17–9. doi: 10.1136/bmj.301.6742.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Newman TB, Brown AN. Use of commercial record linkage software and vital statistics to identify patient deaths. J Am Med Inform Assoc. 1997;4:233–7. doi: 10.1136/jamia.1997.0040233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cook LJ, Knight S, Olson LM, Nechodom PJ, Dean JM. Motor vehicle crash characteristics and medical outcomes among older drivers in Utah, 1992–1995. Ann Emerg Med. 2000;35:585–91. [PubMed] [Google Scholar]
- 31.McGlincy MH. A Bayesian record linkage methodology for multiple imputation of missing links. ASA Proceedings of the Joint Statistical Meetings; Alexandria, Virginia: American Statistical Association; 2004. pp. 4001–8. [Google Scholar]
- 32.Cook LJ, Olson LM, Dean JM. Probabilistic record linkage: relationships between file sizes, identifiers and match weights. Methods Inf Med. 2001;40:196–203. [PubMed] [Google Scholar]
- 33.Rubin DB, Schenker N. Multiple imputation in health-care databases: an overview and some applications. Stat Med. 1991;10:585–98. doi: 10.1002/sim.4780100410. [DOI] [PubMed] [Google Scholar]
- 34.Little RJA, Rubin DB. Statistical analysis with missing data. 2nd ed. Wiley; Hoboken, N.J.: 2002. [Google Scholar]
- 35.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 36.Soapnote [Accessed February 22, 2011];Charlson Comorbidity Index. http://www.soapnote.org/elder-care/charlson-comorbidity-index/.
- 37.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 38.Garza AG, Gratton MC, Salomone JA, Lindholm D, McElroy J, Archer R. Improved patient survival using a modified resuscitation protocol for out-of-hospital cardiac arrest. Circulation. 2009;119:2597–605. doi: 10.1161/CIRCULATIONAHA.108.815621. [DOI] [PubMed] [Google Scholar]
- 39.Bobrow BJ, Clark LL, Ewy GA, et al. Minimally interrupted cardiac resuscitation by emergency medical services for out-of-hospital cardiac arrest. JAMA. 2008;299:1158–65. doi: 10.1001/jama.299.10.1158. [DOI] [PubMed] [Google Scholar]
- 40.Davis DP, Dunford JV, Poste JC, et al. The impact of hypoxia and hyperventilation on outcome after paramedic rapid sequence intubation of severely head-injured patients. J Trauma. 2004;57:1–8. doi: 10.1097/01.ta.0000135503.71684.c8. [DOI] [PubMed] [Google Scholar]
- 41.Davis DP, Hoyt DB, Ochs M, et al. The effect of paramedic rapid sequence intubation on outcome in patients with severe traumatic brain injury. J Trauma. 2003;54:444–53. doi: 10.1097/01.TA.0000053396.02126.CD. [DOI] [PubMed] [Google Scholar]
- 42.Jabre P, Combes X, Lapostolle F, et al. Etomidate versus ketamine for rapid sequence intubation in acutely ill patients: a multicentre randomised controlled trial. Lancet. 2009;374:293–300. doi: 10.1016/S0140-6736(09)60949-1. [DOI] [PubMed] [Google Scholar]
- 43.Walls RM, Murphy MF. Clinical controversies: etomidate as an induction agent for endotracheal intubation in patients with sepsis: continue to use etomidate for intubation of patients with septic shock. Ann Emerg Med. 2008;52:13–4. doi: 10.1016/j.annemergmed.2008.01.344. [DOI] [PubMed] [Google Scholar]
- 44.Wang HE, Bogucki S, Cone DC. Out-of-hospital endotracheal intubation: Are observational data useful? Acad Emerg Med. 2010;17:987–8. doi: 10.1111/j.1553-2712.2010.00864.x. [DOI] [PubMed] [Google Scholar]
- 45.Arslan Hanif M, Kaji AH, Niemann JT. Advanced airway management does not improve outcome of out-of-hospital cardiac arrest. Acad Emerg Med. 2010;17:926–31. doi: 10.1111/j.1553-2712.2010.00829.x. [DOI] [PubMed] [Google Scholar]
- 46.Wang HE, Cook LJ, Chang CC, Yealy DM, Lave JR. Outcomes after out-of-hospital endotracheal intubation errors. Resuscitation. 2009;80:50–5. doi: 10.1016/j.resuscitation.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 47.Boyle MJ. The experience of linking Victorian emergency medical service trauma data. BMC Med Inform Decis Mak. 2008;8:52. doi: 10.1186/1472-6947-8-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Coutinho RG, Coeli CM, Faerstein E, Chor D. Sensitivity of probabilistic record linkage for reported birth identification: Pro-Saude Study. Rev Saude Publica. 2008;42:1097–100. [PubMed] [Google Scholar]
- 49.Guenther E, Knight S, Olson LM, Dean JM, Keenan HT. Prediction of child abuse risk from emergency department use. The Journal of pediatrics. 2009;154:272–7. doi: 10.1016/j.jpeds.2008.07.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Garza AG, Gratton MC, Coontz D, Noble E, Ma OJ. Effect of paramedic experience on orotracheal intubation success rates. J Emerg Med. 2003;25:251–6. doi: 10.1016/s0736-4679(03)00198-7. [DOI] [PubMed] [Google Scholar]
- 51.Wang HE, Lave JR, Sirio CA, Yealy DM. Paramedic intubation errors: isolated events or symptoms of larger problems? Health Aff (Millwood) 2006;25:501–9. doi: 10.1377/hlthaff.25.2.501. [DOI] [PubMed] [Google Scholar]
- 52.Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emerg Med. 2001;37:32–7. doi: 10.1067/mem.2001.112098. [DOI] [PubMed] [Google Scholar]
- 53.Grasner JT, Meybohm P, Fischer M, et al. A national resuscitation registry of out-of-hospital cardiac arrest in Germany-a pilot study. Resuscitation. 2009;80:199–203. doi: 10.1016/j.resuscitation.2008.10.008. [DOI] [PubMed] [Google Scholar]