Abstract
Identification and management of chronic lumbar spine instability is a clinical challenge for manual physical therapists. Chronic lumbar instability is presented as a term that can encompass two types of lumbar instability: mechanical (radiographic) and functional (clinical) instability (FLI). The components of mechanical and FLI are presented relative to the development of a physical therapy diagnosis and management. The purpose of this paper is to review the historical framework of chronic lumbar spine instability from a physical therapy perspective and to summarize current research relative to clinical diagnosis in physical therapy.
Keywords: Diagnosis, Hypermobility, Low back pain, Physical examination, Segmental instability
The topic of chronic instability of the lumbar spine is subject to much debate as to the exact nature of the problem, the correlation with symptoms, or the relevance to patient management. Understanding the associated history may assist clinicians in better understanding current methods used to establish the diagnosis. The purposes of this paper are to review the historical framework of chronic lumbar spine instability from a physical therapy perspective and summarize current research relative to clinical diagnosis. In particular, we endeavour to determine whether there are data to support the two concepts of mechanical and functional chronic lumbar instability and we explore the clinically oriented examination findings relevant to the constructs of chronic lumbar instability by examining relevant clinical diagnostic elements and the best clinical tests.
Historical Perspective
The concept of instability of the lumbar spine was first presented by Barr1 in 1951 when he espoused the view that the degenerative disc was responsible for a proportion of the genesis of low back pain. The loss of disc height was thought to decrease restraint of passive stabilizers resulting in increased movement of vertebral segments. The loss of disc height subsequently decreased space between lumbar facet joints and adjacent vertebral bodies, placing additional stress on articular cartilage. Augmented contact coupled with increased segmental motion was thought to adversely affect the joints and contribute to low back pain.2–4 Orthopaedic surgeons had already been using fusion to treat low back pain caused by lumbar disc degeneration, but this model further reinforced the rationale for lumbar fusion to treat low back pain.
Although the use of therapeutic exercise for low back pain was described in the literature in the early 1950s, a mathematical model of spine muscle function was not discussed until 1977. Muscle function around the lumbar spine of a weight lifter was calculated using a mathematical model developed by Farfan and Gracovetsky.5 Based on the model, it was suggested that the passive structures of the lumbar spine were better designed to resist compression and much less resistant to segmental shear forces5. Co-contraction of the abdominal wall and back extensor muscles provided stability against shear forces in the lumbar spine under load. This work provided additional rationale for physical therapists that muscle contractions could be used to increase stability of the lumbar spine.
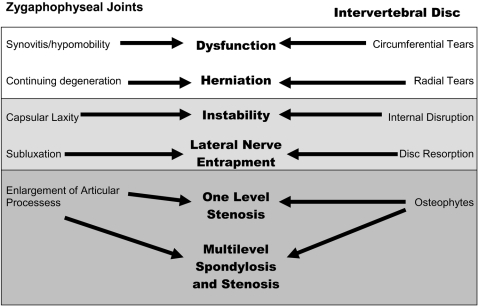
In 1982, the International Society of the Study of the Lumbar Spine held a conference on lumbar instability that included a number of experts from medicine and physical therapy. In the keynote address, Kirkaldy-Willis6 presented his concept of the degenerative cascade of the spine (Fig. 1). He proposed that discussions of instability at the conference should be directed toward three goals: agreement on the definition of instability, how instability could be diagnosed, and how treatment could be initiated based on the severity of instability.
Figure 1.
The degenerative cascade based on Kirkaldy-Willis and Farfan.20 The white section is the dysfunction stage, the light grey is the instability stage, and the dark grey is the stabilization stage.
During this conference, Pope and Panjabi7 defined instability, from a biomechanical perspective, as a loss of stiffness in the spine. Stiffness was defined as the amount of motion within a system relative to a load applied to the structure. This would allow comparison of different responses in adjacent spinal segments to similar load applications, which they conjectured might be difficult to study in vivo. The loss of stiffness was thought to allow increased motion to occur at each vertebral segment. Flexion and extension radiographs could be used to identify and quantify increased end-range motion at lumbar spinal segments.
Gertzbein et al.8 provided evidence that in mildly and moderately degenerated spinal segments, motion was not thought to be excessive but rather erratic. Only 33% of cadaveric spines with mild and moderate degeneration spinal segments demonstrated excessive range of motion based on flexion and extension radiographs. Compared to control spines, mildly and moderately degenerated spinal segments demonstrated changes in the instantaneous axis of rotation throughout flexion and extension. Identification and quantification of this motion in vivo was thought to be more difficult to obtain.
A subjective evaluation of instability from a manual physical therapist’s perspective was provided by Paris.9 He proposed a distinction between lumbar instability and hypermobility, which he defined as excessive movement at a joint given the subject’s age and activity. Since flexion and extension X-rays were not helpful in identifying instability, Paris proposed that they might be helpful in identifying hypermobility. Instability was defined as aberrant (erratic) motion during movement (shake, catch, or hitch; sharp angulation; uncoordinated muscle contraction) or the presence of palpable defect both in standing and in prone. He described hypermobility as a quantitative measure and instability as a qualitative measure. Thus, the defining difference between instability and hypermobility was the presence of what has been termed ‘aberrant movement’.
Panjabi presented his concept of spinal stability in two articles in the early 1990s.10,11 This article discussed the idea that stability of various joints in the body is maintained by a combination of the structural (passive) system, muscular (active) system, and the neural control system.10 The interplay between these systems was thought to be necessary for neuromuscular control of spinal segments and disruption might lead to a lack of segmental control. Panjabi suggested that loss of osseoligamentous integrity would result in lack of stability of the spine if the muscular and neural control systems were unable to adequately compensate. The ability of the patient to maintain an efficient coordination between these systems would allow him or her to function without undue stress on the tissues in the body.10–12
Literature Search Process
A literature search was undertaken to review the published work on instability since the publication of the symposium papers in 1985. In particular, literature was screened for the association with the questions posted previously. The first search used the MESH terms lumbar, vertebrae AND instability, joint in PubMed. The retrieved articles were saved in a Reference ManagerTM database. In order to find all relevant articles, multiple searches were performed. The second search was performed in CINAHL with lumbar vertebrae AND instability. The results were combined in the database to look at the presence of duplicates. A third search was performed in PubMed using the MESH terms ((((Lumbosacral Region [Mesh] OR Lumbar Vertebrae [Mesh])) AND Joint Instability [Mesh]) AND (Diagnosis [Mesh] OR diagnosis [Subheading] OR Diagnosis, Differential [Mesh] OR radiography [Subheading])). This returned 296 citations, which were combined in Reference Manager to determine the presence of duplicates.
A fourth search used the MESH terms ((((Lumbosacral Region [Mesh] OR Lumbar Vertebrae [Mesh])) AND Joint Instability [Mesh]) AND (Diagnosis [Mesh] OR diagnosis [Subheading] OR Diagnosis, Differential [Mesh] OR radiography [Subheading])) AND Physical Therapy (Specialty) [Mesh]. This returned only one article. This was added to the database. A link-out was performed in PubMed and returned 171 citations. The citations were combined in Reference Manager, and duplicates were identified and deleted. Surgical or post-surgical references were also eliminated. A second author (MM) scanned the same references to determine appropriateness for inclusion in the literature review.
The articles were then assessed as to whether the authors had used a method of statistical analysis to determine the presence of instability relative to a radiological standard (flexion–extension films). This resulted in fewer than 50 articles being included in the review of the diagnosis of instability as most articles were surgical reports or narrative reviews describing the current literature.
Are There Data to Support the Two Concepts of Chronic Lumbar Instability?
Mechanical
A number of studies published since the symposium have focused on the relevance of radiographic findings, including X-rays and magnetic resonance imaging (MRI), for the diagnosis for mechanical instability. The use of flexion–extension X-rays is relatively common, but the ability to identify instability has had mixed findings.13–15 The use of side-bending X-rays is thought to provide minimal additional information related to the amount of angular motion and instability.14
The use of MRI to assist in diagnosing lumbar spine dysfunction has increased in the past two decades. The degree of disc degeneration, using standard MRI, is not thought to correlate with the amount of angulation (> 15°) or segmental instability (> 3 mm translation).16 Findings have differed when dynamic MRI is used to examine motion in a standing position.17 The degree of disc and facet joint degeneration has a positive association with excessive translational motion while the degree of facet joint degeneration has a negative association with excessive angular motion.17 These findings are similar to a previous study that indicated that zygapophyseal (facet) joint oedema was associated with the presence of instability on flexion–extension radiographs.18 Other spine pathology such as annular tears (+LR = 6.26, −LR = 0.83) or traction spurs (+LR = 6.58, −LR = 0.89) identified using standard MRI has also been associated with segmental instability (> 3 mm translation) on X-ray.19 It does appear that with more severe disc degeneration (grade V), there is a lesser amount of excessive angular and translational motion when compared to lower grades of disc degeneration.17 This lends support to Kirkaldy-Willis’s proposed degenerative cascade restabilization phase.20
Functional
Video fluoroscopy has been used to analyse segmental motion of the lumbar spine in individuals without low back pain and in individuals who could be classified in the stabilization treatment-based classification.21 All individuals with low back pain also had a positive prone instability test. Individuals with low back pain who met stabilization classification criteria demonstrated aberrant motion in the sagittal plane during lumbar extension, indicating that individuals with stabilization classification low back pain may have altered structural integrity, stiffness, and/or neuromuscular control during mid-range motions. These individuals may exhibit altered control or lack of stability in the neutral zone as previously described by Panjabi.11
Recently an intraoperative measurement system has been developed to obtain in vivo measurements of vertebral segment displacement during the application of a controlled load to produce motion.22 Results indicated that individuals with spondylolisthesis have decreased segmental stiffness and a greater neutral zone size than individuals without low back pain. Although neutral zone size varied in degenerative segments and indicated that not all spondylolytic segments were unstable, individuals with degenerative changes must control a larger neutral zone size with less available stiffness to adequately control spinal motion. This is in agreement with a previous in vitro study that demonstrated that individuals with degenerative changes (disc degeneration) also demonstrate increases in neutral zone size.23
Clinically Oriented Examination Findings Relevant to the Constructs of Chronic Lumbar Instability
Construct of instability
Terminology associated with a diagnosis of instability may be further clouded depending on the perspective of the medical professional (orthopaedic surgeon versus physical therapist). Using established terminology from the extremities may help decrease confusion. Individuals with chronic ankle instability have been described in different groups as having mechanical and functional ankle instability.24 Regardless of the affected region, mechanical instability refers to disruption of the passive stabilizers and decreased structural integrity while functional instability refers to a lack of neuromuscular control of the joint during activities.24 We propose the designation of chronic lumbar instability (CLI), which would include the subcategories of mechanical lumbar instability (MLI) and functional lumbar instability (FLI). Diagnosis of mechanical instability of the lumbar spine is based on imaging findings or posterior–anterior (PA) mobility assessment as discussed previously and, potentially, can be addressed via surgical stabilization (lumbar fusion) or physical therapy. Functional instability may be better addressed via physical therapy as the problem is more likely related to decreases in neuromuscular control of the lumbar vertebral segments during function. It may be important to assess CLI to determine the presence of MLI and FLI as patients may present with a combination. Individuals with MLI may or may not have FLI. As previously proposed by Paris, hypermobility can be present indicating MLI but the presence of aberrant movement may indicate FLI.9
Clinical tests for instability
Certain subjective and objective examination findings may be used to identify lumbar spine clinical instability. A Delphi survey was conducted of physical therapists who were either board-certified in orthopaedics with the American Physical Therapy Association or Fellows in the American Academy of Manual Physical Therapists to determine consensus regarding the existence of specific examination criteria for the identification of lumbar spine clinical instability.25 Consistent subjective measures included a history of painful locking or catching during spinal motion, pain on return from forward bending, pain during transitional activities, pain with sudden or trivial activities, problems with unsupported sitting, or pain that worsens with sustained positions. Respondents consistently identified the following objective findings as the strongest predictors of clinical lumbar instability: muscle dysfunction, motor control abnormalities, and strength losses.
Current research in physical therapy has focused on developing specific and sensitive clinical tests for identification of lumbar spine instability. Segmental instability (flexion/extension radiographs) may be identified in the clinic using segmental mobility testing and lumbar range of motion using an inclinometer. The lack of hypomobility during segmental mobility testing and the presence of increased lumbar range of motion (> 53°) have been shown to be predictive (+LR = 12.8; 95% CI = 0.79–211.6) of segmental instability (flexion/extension radiographs).26 The likelihood of segmental instability is still high (+LR = 4.3; 95% CI = 1.8–10.6) when only one variable is present. It should be noted that the associated confidence intervals are wide, indicating the need for further studies.
Four tests relevant to physical therapists for identifying FLI include aberrant movement, PA glide, straight leg raise, and the prone instability test. Aberrant motion is a qualitative test, PA glide is quantitative, straight leg raise evaluates neural tissue, and the prone instability test is a pain provocation test. Aberrant motion may be assessed in standing and the subject is asked to flex forward as far as possible and return to standing. Aberrant motion is present if any one of the following is identified: instability catch, painful arc of motion in flexion, painful arc on return from flexion, thigh climbing, or a reversal of lumbopelvic rhythm.27 The reliability for identification of aberrant movement has been described as moderate (kappa = 0.60).27 The straight leg raise is performed with the patient in supine while the examiner passively raises one leg to the maximum tolerated height indicated by the patient. The amount of motion may be quantified by placing an inclinometer on the tibial crest just inferior to the tibial tubercle. The reliability for the straight leg raise has been described as excellent (ICC = 0.94–0.96).28 Individuals with a straight leg raise greater then 91° may also demonstrate other signs and symptoms consistent with chronic lumbar instability.27
Individual segmental stiffness can be assessed using a PA glide of the individual vertebral segment. Recently, a study by Landel et al.29 examined the intertester reliability for the PA glide in the lumbar spine. PA glide demonstrated good reliability (kappa = 0.71) and agreement (82.8%) for identifying the least mobile lumbar vertebral segment, and poor reliability (kappa = 0.29) but good agreement (79.3%) for identifying the most mobile vertebral segment. The validity of a PA glide as a quantitative measure is questionable since there is little agreement when compared to the amount of segmental motion measured using dynamic MRI. It is possible that a PA glide is best at identifying quality of stiffness or resistance to motion. In a physical therapy setting, the use of a PA glide of the vertebral segment and range-of-motion measurements may help predict the presence of MLI when X-rays are not available.26 Individuals who lack hypomobility with PA glide or have lumbar flexion range of motion greater than 53° were 4.3 times (95% CI = 1.8–10.6) more likely to have radiographic instability and 12.8 times (95% CI = 0.79–211.6) more likely when both variables were present.26 No study has examined resistance to motion at lumbar vertebral segments. Resistance to motion at lumbar vertebral segments would be consistent with the concepts of maintenance of spinal stability via the stiffness of the osseoligamentous system and the muscular system.10
The prone instability test uses the PA glide to assess segmental stiffness and pain provocation with muscles in a resting state and during an active contraction.27 The first portion of the test is performed with the patient in prone with the lower extremities in contact with the ground while a PA glide is performed at each lumbar segment to see if pain is produced at that segment. If a painful segment is identified, the second half of the test is performed at that segment in conjunction with active lumbar and hip extension to lift the legs from the ground. The prone instability test is considered positive if pain is provoked in the resting state and eliminated during active muscle contraction. Reliability of the prone instability test has been described as high (kappa = 0.87).27 Recently, spinal stiffness was measured during the application of a PA force when doing either the abdominal drawing in manoeuvre or abdominal bracing in individuals without lumbar spine pathology.30 Both instances increased spinal stiffness greater than resting, but the abdominal brace increased spine stiffness greater than the abdominal drawing in manoeuvre. These findings are consistent with modelling of lumbar spine function during muscular contraction.5
Passive accessory intervertebral motion (PAIVM) and passive physiological intervertebral motion (PPIVM) are used by physical therapists to evaluate segmental mobility in the spine. Abbott et al.31 compared assessment of PAIVM mobility and PPIVM mobility in 138 patients who also had flexion/extension radiographs. The authors reported that translation lumbar segmental instability (LSI) was correlated with chronic or recurrent low back pain. PAIVMs were specific for translational LSI (sp = 0.89) but had poor sensitivity (sn = 0.29). The positive likelihood ratio (+LR) of a positive test is 2.52. The authors reported that flexion PPIVMs were highly specific for translational LSI (sp = 0.995) but had very poor sensitivity (sn = 0.05), which results in statistically insignificant likelihood ratios. Extension PPIVMs were more sensitive (sn = 0.16) and the specificity was similar to flexion PPIVM (sp = 0.98), resulting in a +LR of 7.1 for a positive test. Abbott et al. reported that PPIVMs and PAIVMs are specific but not sensitive, yielding +LRs that are moderate at best.
The relevance here for physical therapists is that FLI appears to be related to a loss of segmental stiffness and one of mid-range control of spinal segments during motion (aberrant motion). Teyhen et al.21 used digital video fluoroscopy to compare segmental motion in the lumbar spine between healthy individuals and individuals with low back pain who fit a stabilization treatment-based classification27 and who had a positive prone instability test in L3, L4, or L5 segment. Individuals who fit stabilization classification demonstrated aberrant motion in the sagittal plane during flexion and extension potentially due to altered structural integrity, loss of stiffness, and decreased neuromuscular control during mid-range motions. These findings are similar to the radiographic findings in cadaveric spines reported by Gertzbein et al.8 and are consistent with Panjabi’s model of proposed altered control or lack of stability in the neutral zone.11 Loss of mid-range control and aberrant motion may be difficult to quantify using static measures of stability (X-ray or MRI).8,32 It is possible that FLI and associated decreased mid-range control may eventually degenerate into loss of mechanical stability.
Discussion
The answers to the questions originally posed in this review are present within the literature and shed light on this evolving concept. There is evidence in the radiology literature of hypermobility or MLI during flexion/extension films as well as correlates in static films or studies to indicate excessive motion. The use of PA assessment in identifying hypermobile segments has been reported by two different studies, which may indicate that this test can help identify MLI. The correlation of PPIVMs and PAIVMs to radiographs indicates that the segmental mobility testing may have moderate validity for assessing abnormal motion.
The development of advanced real-time imaging has supported Gertzbein et al.’s8 original cadaveric work reporting altered dynamic motion patterns in FLI. This also corresponds to Paris’9original differentiation between hypermobility, which we define as MLI, and clinical instability, which we define as FLI. The use of the prone instability test may be a way to utilize a clinical test to look for the patient’s ability to stabilize a hypermobile segment and may well indicate the presence of FLI, especially when coupled with the observation of aberrant motion during the examination of lumbar range of motion.
As to whether clinical examination tests are valid in identifying translational lumbar instability can also be found in the literature, there is evidence that PAIVMs and PPIVMs are statistically correlated to radiographic findings. In addition, diagnostic power has been reported with likelihood ratios. However, accessory motion testing seems to be more specific than sensitive and this may limit a therapist’s ability to confidently rule out the presence of radiographic instability. These findings suggest differences in the diagnostic capabilities for determining mechanical and functional instability. It is possible that accessory motion testing is better for evaluating mid-range stiffness and may be more of an indirect measure of FLI versus MLI, which occurs at the end range of motion.
Finally, the answer to the first question, are there data to support two concepts of lumbar instability, e.g. radiographic (mechanical) and clinical (functional), would also seem to be yes, with preliminary evidence to indicate two components of chronic lumbar instability, which may include of MLI and FLI. MLI is likely to be related to an increase in end range of motion while FLI appears to be related to a loss of segmental stiffness and one of mid-range spinal segmental control during motion (aberrant motion). It is important to note that individuals with MLI may or may not have symptoms associated with FLI depending on the function of stabilizing muscles. Therapists can use various components of the subjective and objective examination in order to differentiate MLI and FLI, allowing them to make evidence-based recommendations for intervention. Physical therapy interventions may best address FLI.
The ability to accurately identify relevant signs and symptoms and develop a supportable clinical diagnosis may assist in improving current interventions to address chronic lumbar instability. Future studies should be directed towards developing clinical tools that are specific and sensitive so as to improve manual therapists’ ability to develop a clinical picture of patient spinal mobility and control during motion and function.
References
- 1.Barr JS. Low-back and sciatic pain: results of treatment. J Bone Joint Surg Am 1951;33-A: 633–49 [PubMed] [Google Scholar]
- 2.Lettin AW. Diagnosis and treatment of lumbar instability. J Bone Joint Surg Br 1967;49-B: 520–9 [PubMed] [Google Scholar]
- 3.Morgan FP, King T. Primary instability of lumbar vertebrae as a common cause of low back pain. J Bone Joint Surg Br 1957;39-B: 6–22 [DOI] [PubMed] [Google Scholar]
- 4.Macnab I. The traction spur: An indicator of segmental instability. J Bone Joint Surg Am 1971;53: 663–70 [PubMed] [Google Scholar]
- 5.Farfan HF, Gracovetsky S. The nature of instability. Spine (Phila Pa 1976) 1984;9: 714–9 [DOI] [PubMed] [Google Scholar]
- 6.Dupuis PR, Yong-Hing K, Cassidy JD, Kirkaldy-Willis WH. Radiologic diagnosis of degenerative lumbar spinal instability. Spine (Phila Pa 1976) 1985;10: 262–76 [DOI] [PubMed] [Google Scholar]
- 7.Pope MH, Panjabi M. Biomechanical definitions of spinal instability. Spine (Phila Pa 1976) 1985;10: 255–6 [DOI] [PubMed] [Google Scholar]
- 8.Gertzbein SD, Seligman J, Holtby R, Chan KH, Kapasouri A, Tile M, et al. Centrode patterns and segmental instability in degenerative disc disease. Spine (Phila Pa 1976) 1985;10: 257–61 [DOI] [PubMed] [Google Scholar]
- 9.Paris S. Physical signs of instability. Spine (Phila Pa 1976) 1985;10: 277–9 [DOI] [PubMed] [Google Scholar]
- 10.Panjabi MM. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord 1992;5: 383–9 [DOI] [PubMed] [Google Scholar]
- 11.Panjabi MM. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord 1992;5: 390–6 [DOI] [PubMed] [Google Scholar]
- 12.Comerford MJ, Mottram SL. Movement and stability dysfunction: contemporary developments. Man Ther 2001;6: 15–26 [DOI] [PubMed] [Google Scholar]
- 13.Soini J, Antti-Poika I, Tallroth K, Konttinen YT, Honkanen V, Santavirta S. Disc degeneration and angular movement of the lumbar spine: comparative study using plain and flexion–extension radiography and discography. J Spinal Disord 1991;4: 183–7 [DOI] [PubMed] [Google Scholar]
- 14.Pitkanen M, Manninen H. Sidebending versus flexion–extension radiographs in lumbar spinal instability. Clin Radiol 1994;49: 109–14 [DOI] [PubMed] [Google Scholar]
- 15.Pitkanen MT, Manninen HI, Lindgren KA, Sihvonen TA, Airaksinen O, Soimakallio S. Segmental lumbar spine instability at flexion–extension radiography can be predicted by conventional radiography. Clin Radiol 2002;57: 632–9 [DOI] [PubMed] [Google Scholar]
- 16.Murata M, Morio Y, Kuranobu K. Lumbar disc degeneration and segmental instability: a comparison of magnetic resonance images and plain radiographs of patients with low back pain. Arch Orthop Trauma Surg 1994;113: 297–301 [DOI] [PubMed] [Google Scholar]
- 17.Kong MH, Hymanson HJ, Song KY, Chin DK, Cho YE, Yoon do H, et al. Kinetic magnetic resonance imaging analysis of abnormal segmental motion of the functional spine unit. J Neurosurg Spine 2009;10: 357–65 [DOI] [PubMed] [Google Scholar]
- 18.Schinnerer KA, Katz LD, Grauer JN. MR findings of exaggerated fluid in facet joints predicts instability. J Spinal Disord Tech 2008;21: 468–72 [DOI] [PubMed] [Google Scholar]
- 19.Bram J, Zanetti M, Min K, Hodler J. MR abnormalities of the intervertebral disks and adjacent bone marrow as predictors of segmental instability of the lumbar spine. Acta Radiol 1998;39: 18–23 [DOI] [PubMed] [Google Scholar]
- 20.Kirkaldy-Willis WH, Farfan HF. Instability of the lumbar spine. Clin Orthop Relat Res 1982; 165: 110–23 [PubMed] [Google Scholar]
- 21.Teyhen DS, Flynn TW, Bovik AC, Abraham LD. A new technique for digital fluoroscopic video assessment of sagittal plane lumbar spine motion. Spine 2005;30: E406–13 [DOI] [PubMed] [Google Scholar]
- 22.Hasegewa K, Kitahara K, Hara T, Takano K, Shimoda H. Biomechanical evaluation of segmental instability in degenerative lumbar spondylolisthesis. Eur Spine J 2009;18: 465–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mimura M, Panjabi MM, Oxland TR, Crisco JJ, Yamamoto I, Vasavada A. Disc degeneration affects the multidirectional flexibility of the lumbar spine. Spine (Phila Pa 1976) 1994;19: 1371–80 [DOI] [PubMed] [Google Scholar]
- 24.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train 2002;37: 364–75 [PMC free article] [PubMed] [Google Scholar]
- 25.Cook C, Brismee JM, Sizer PSJr. Subjective and objective descriptors of clinical lumbar spine instability: a Delphi study. Man Ther 2006;11: 11–21 [DOI] [PubMed] [Google Scholar]
- 26.Fritz JM, Piva SR, Childs JD. Accuracy of the clinical examination to predict radiographic instability of the lumbar spine. Eur Spine J 2005;14: 743–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hicks GE, Fritz JM, Delitto A, Mishock J. Interrater reliability of clinical examination measures for identification of lumbar segmental instability. Arch Phys Med Rehabil 2003;84: 1858–64 [DOI] [PubMed] [Google Scholar]
- 28.Waddell G, Somerville D, Henderson I, Newton M. Objective clinical evaluation of physical impairment in chronic low back pain. Spine (Phila Pa 1976) 1992;17: 617–28 [DOI] [PubMed] [Google Scholar]
- 29.Landel R, Kulig K, Fredericson M, Li B, Powers CM. Intertester reliability and validity of motion assessments during lumbar spine accessory motion testing. Phys Ther 2008;88: 43–9 [DOI] [PubMed] [Google Scholar]
- 30.Stanton T, Kawchuk G. The effect of abdominal stabilization contractions on postero-anterior spinal stiffness. Spine 2008;33: 694–701 [DOI] [PubMed] [Google Scholar]
- 31.Abbott JH, McCane B, Herbison P, Moginie G, Chapple C, Hogarty T. Lumbar segmental instability: a criterion-related validity study of manual therapy assessment. BMC Musculoskelet Disord 2005;6: 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gertzbein SD, Seligman J, Holtby R, et al. Centrode characteristics of the lumbar spine as a function of segmental instability. Clin Orthop Relat Res 1986;208: 48–51 [PubMed] [Google Scholar]