Abstract
Currently, large levels of practice variability exist regarding the clinical deactivation of trigger points. Manual physical therapy has been identified as a potential means of resolving active trigger points; however, to date the ideal treatment approach has yet to be elucidated. The purpose of this clinical trial was to compare the effects of two manual treatment regimens on individuals with upper trapezius trigger points. Sixty patients, 19–38 years of age with non-specific neck pain and upper trapezius trigger points, were randomized into one of two, 4 week physical therapy programs. One group received muscle energy techniques while the second group received an integrated neuromuscular inhibition technique (INIT) consisting of muscle energy techniques, ischemic compression, and strain–counterstrain (SCS). Outcomes including a visual analog pain scale (VAS), the neck disability index (NDI), and lateral cervical flexion range of motion (ROM) were collected at baseline, 2 and 4 weeks after the initiation of therapy. Results revealed large pre–post-effect sizes within the INIT group (Cohen’s d = 0.97, 0.94 and 0.97). Additionally, significantly greater improvements in pain and neck disability and lateral cervical flexion ROM were detected in favor of the INIT group (0.29–0.57, 0.57–1.12 and 0.29–0.57) at a 95% CI respectively. The findings of this study indicate the potential benefit of an integrated approach in deactivating upper trapezius trigger points. Further research should be performed to investigate the long-term benefits of the current treatment approach.
Keywords: Integrated neuromuscular inhibition technique, Ischemic compression, Muscle energy technique, Strain–counterstrain, Trigger points
Neck pain is a common disorder with a reported 6 month prevalence rate of 54%.1 With up to 37% of individuals developing persistent symptoms, neck pain is a condition that places a large economic burden on the health care system.2 In the majority of cases, the pathoanatomical source of an individual’s pain cannot be identified and are therefore defined as non-specific in nature.3 Although there are many potential contributing factors to non-specific neck pain, one area that has received little scientific emphasis is the trigger point (TrP).
Although, the etiology of TrP development is currently unknown, recent studies have hypothesized that the pathogenesis results from the overloading and injury of muscle tissue, leading to involuntary shortening of localized fibers.4,5 The areas of stressed soft tissue receive less oxygen, glucose, and nutrient delivery, and subsequently accumulate high levels of metabolic waste products. The end result of this cascade of events is the creation of altered tissue status, pain, and the development of TrPs.4,5 TrPs have been found to frequently occur in individuals with mechanical neck pain as compared to their age matched controls.6 TrPs have been associated with hyperalgesia and limited range of motion (ROM) and are therefore clinically important to identify as these possess the potential to restrict functional activies.7 Identification is accomplished through the recognition of a pattern of clinical signs on physical examination. Signs that may include the presence of a taut band in a skeletal muscle, the presence of a tender spot within the taut band, a palpable or visible local twitch response upon palpation, and/or needle inspection of the TrP (called a jump sign), the presence of a typical referred pain pattern, and restricted ROM of the affected tissues.8,9
TrPs have the potential to create pain, limit ROM and restrict functional activities and should therefore be addressed as part of a comprehensive physical therapy program. Currently, a large variety of both manual and non-manual interventions exist for the deactivation of TrPs. Non-manual interventions may include botulism toxin injections, dry needling, acupuncture, and ethyl chloride spray and stretch techniques. Manual approaches may include muscle energy techniques (METs), strain–counterstrain (SCS), myofascial release, proprioceptive neuromuscular facilitation, and ischemic compression.10 Owing to the heterogeneity of the existing clinical trials examining non-manual and manual techniques on TrP deactivation, the evidence currently does not exceed the moderate level. Trials examining manual techniques suggest that such approaches may be effective; however, the extent of the effectiveness beyond placebo is currently unknown.11 Thus, to date the ideal manual physical therapy approach to treat active TrPs has not been identified.
As stated, METs have been recommended as a means of managing TrPs.12,13 METs are a commonly utilized method for achieving tonus release (inhibition) in a muscle before stretching. The approach involves the introduction of an isometric contraction to the affected muscle producing post-isometric relaxation through the influence of the Golgi tendon organs (autogenic inhibition). It may also be applied to the antagonistic muscle group producing reciprocal inhibition in the offending agonistic muscle(s).13,14 Fryer and Fossum15 have hypothesized that the sequence of muscle and joint mechanoreceptor activation evokes firing of local somatic efferents. This in turn leads to sympatho-excitation and activation of the periaqueductal gray matter, which plays a role in the descending modulation of pain. Owing to stimulation of mechanoreceptors, simultaneous gating of the nociceptive impulses takes place in the dorsal horn of the spinal cord.
Ischemic compression is another manual therapy technique which is frequently employed as a means of deactivating TrPs. It involves applying direct sustained digital pressure to the TrP with sufficient force over dedicated time duration, to slow down the blood supply and relieve the tension within the involved muscle. The pressure is gradually applied, maintained and the gradually released.16,17 One proposed mechanism for the benefit of ischemic compression was explained by Hou et al.17 Hou and colleagues17 suggested that pain and muscle spasm relief from direct digital pressure may result from the reactive hyperemia produced in the area, or from the spinal reflex mechanism.
SCS has also been utilized in the manual treatment of TrPs. This approach involves identification of the active TrPs, followed by the application of pressure until a nociceptive response is produced. The area is then positioned in such a manner as to reduce the tension in the affected muscle and subsequently the pain in the TrP. When the position of ease/pain reduction is attained, the stressed tissues are felt to be at their most relaxed and a local reduction of tone is produced.12
Chaitow18 feels that the combination of MET, ischemic compression and SCS produces the most effective, targeted approach to TrP release. This method is termed the integrated neuromuscular inhibition technique (INIT).19 He has suggested that the benefit of the technique lies in its multifaceted approach. The INIT approach allows for delivery of the techniques in a single coordinated manner. Although randomized clinical trials exist studying the efficacy of ischemic compression and SCS in neck pain and chronic myofascial pain syndromes, there is a lack of evidence regarding the integration of these techniques in individuals with non-specific neck pain.16,20,21 For this reason, additional research examining the effectiveness of this regimen was warranted. The purpose of this study was to compare the effect of two commonly used treatment approaches, MET, and the INIT, in deactivating upper trapezius TrPs as measured by an improvement in pain, ROM, and disability.
Methods
A single blinded, randomized controlled trial (RCT) was conducted between June 2007 and April 2008 in an outpatient clinic in Dhamtari, India. Subjects were referred by their health care providers as well as recruited via advertisements in local newspapers and health magazines. The study population consisted of individuals between 18 and 55 years of age, suffering from non-specific neck pain, defined as non-articular or non-systemic as per the referring physician. Subjects were required to have neck pain of less than 3 months duration as well as active TrPs in the upper trapezius muscle, defined as a tender nodule in a taut band that referred pain beyond the area of contact. The study was approved by the ethical committee at Escorts Physiotherapy College (Dhamtari, India). All subjects provided informed consent before enrollment in the study.
Subjects were excluded if their neck symptoms were related to a motor vehicle collision or significant trauma, if there were signs of serious pathology (e.g. malignancy, infection, inflammatory disorder, or fracture), if there were signs of cervical spinal cord compromise (e.g. diffuse sensory abnormality, diffuse weakness, hyperreflexia, or the presence of clonus), two or more signs of nerve root involvement (e.g. dermatomal sensation changes, myotomal weakness, or diminished/absent tendon jerk reflexes), a history of neck surgery during the previous 12 months, and a history of cervical degenerative joint disease as per radiographs, endocrine disorders, and autoimmune conditions (e.g. rheumatoid arthritis, fibromyalgia, etc.), or if they had received trigger point injections in the upper trapezius muscle within the past 6 months.
Before randomization, subjects completed several self-report outcome measures. A visual analog scale (VAS) was used to grade their level of neck pain. The VAS is a 10 cm long horizontal line with polar descriptors of no pain and worst pain possible. Subjects indicated their pain by placing a vertical line at the point that represented their current level of symptoms. The VAS is a reliable and valid outcome measure and has been used extensively in neck pain research.16,18,22 The participant’s functional status was assessed by means of the neck disability index (NDI). The NDI is a 10-item questionnaire which has shown to be a valid and reliable measure of disability in individuals with neck pain (ICC = 0.70–0.89).23 The NDI is scored from 0–50 points (0–100%) in which higher scores correspond to greater levels of disability. Using this system, a score of 5–14 points (10–28%) is considered to constitute mild disability, 15–24 points (30–48%) is considered to constitute moderate disability, 25–38 points (50–68%) is considered to constitute severe disability, and scores above 34 points (68%) indicate complete disability.23
Following completion of the self-report measures, subjects underwent a baseline clinical examination to include screening tests aimed at ruling out specific causes of neck pain that would exclude the individual from the study.5 Cervical lateral flexion motion was assessed using a cervical range of motion (CROM) goniometer.24 Subjects were asked to sit upright and laterally flex their head towards one side. The motion was stopped once the available ROM was completed and care was taken to disallow shoulder elevation. Once the degree of lateral flexion was recorded, the motion was repeated towards the opposite side. The cervical CROM device has demonstrated good to excellent inter-rater reliability (ICC = 0.73–0.89).24 All recordings were taken by an independent observer and the examining therapist was kept blinded to the records.
After the baseline examination was completed, the examining therapist left the room and a second, blinded therapist entered. A sealed, opaque envelope was then opened indicating the treatment group to which the subjects were randomized. A computer-generated randomized block of numbers was performed before the study. *Subjects were randomized to receive either METs or the INIT. The primary outcome measures of pain intensity and cervical lateral flexion as well as the secondary measure of functional status were captured at baseline, 2 and 4 weeks.
Muscle energy technique group
Subjects randomized to the MET group received treatment as per Lewit’s post-isometric relaxation approach.25 The subjects were placed supine and the practitioner stabilized the shoulder on the affected side with one hand, while the ear/mastoid area of the affected side was held by the opposite hand. The head and neck were then side bent towards the contralateral side, flexed, and rotated ipsilaterally, placing the subject just short of their upper trapezius restriction barrier. The subjects then shrugged the involved/stabilized shoulder towards the ear at a submaximal, pain-free, effort (20% of their available strength). The isometric effort was held for 7–10 s while a normal breathing rhythm was maintained. During the relaxation phase, the head and neck were eased into increasing degrees of side bending, flexion and rotation to advance the stretch placed on the muscle. Each stretch was held for 30 s, and this was repeated for three to five repetitions per session (Fig. 1).26
Figure 1.
Example of a muscle energy technique (MET) used in the study.
Integrated neuromuscular inhibition technique group
As the primary focus of the INIT approach is to deactivate specific TrPs, the practitioners first identified the TrPs to be treated within the upper trapezius muscle. The subjects were placed in supine to reduce tension in the upper trapezius muscle. Their arm was positioned in slight shoulder abduction with the elbow bent and their hand resting on their stomach. Using a pincer grasp, the practitioner moved throughout the fibers of the upper trapezius and made note of any active TrPs (Fig. 2). Once the TrPs were identified treatment began. The first technique applied was ischemic compression. The therapist again utilized a pincer grasp, placing the thumb and index finger over the active TrP. Slow, increasing levels of pressure were applied until the tissue resistance barrier was identified. Pressure was maintained until a release of the tissue barrier was felt. At that time, pressure was again applied until a new barrier was felt. This process was repeated until tension/tenderness was unable to be identified or 90 s had elapsed, whichever came first. All identified TrPs were treated (Fig. 3).
Figure 2.
Identification of upper trapezius trigger point by the pincer method.
Figure 3.
Example of an ischemic compression therapy technique used in the study.
Ischemic compression was followed by the application of SCS. Moderate digital pressure was applied to the identified TrP as subjects rated their level of pain on a scale from 1 to 10. If pain was unable to be identified, pressure was increased. If pain was reproduced, the pressure was maintained over the active TrP as the position of ease was identified. The position of ease was often produced through positioning the muscle in a shortened/relaxed position. Ease was defined as the point where a reduction in pain of at least 70% was produced. An example of this was supine lying with the head side bent towards the involved side while the practitioner positioned the ipsilateral arm in flexion, abduction and external rotation to reduce the reported TrP pain. Once the position of ease was identified, it was held for 20–30 s and repeated for three to five repetitions (Fig. 4).
Figure 4.
Example of a positional release therapy technique used in the study.
Lastly, the subjects received MET directed towards the involved upper trapezius. Each isometric contraction was held for 7–10 s and was followed by further contralateral sidebending, flexion, and ipsilateral rotation to maintain the soft tissue stretch. Each stretch was held for 30 seconds and was repeated three to five times per treatment session (Fig. 1)27.
Both groups were treated three times per week for 4 consecutive weeks and were instructed to maintain their normal activities while avoiding any undue stress to the neck.
Data analysis
Baseline characteristics including means and standard deviations (SD) were described. The mean differences with SD for the outcome measures of pain, lateral neck flexion, and neck disability were calculated for the time periods of baseline to 2 weeks, and baseline to 4 weeks. A one-way analysis of variance (ANOVA) was used to assess the between-group differences for all three outcome measures (pain intensity, neck disability, and lateral cervical flexion) at each follow-up period. An a priori alpha level equal to 0.05 was used. A one-tailed hypothesis was generated favoring the INIT group. The minimum required sample size was calculated as 21 subjects per group; 30 subjects were included per group to increase the statistical power of the analysis. The power of the sample was calculated as 0.92. This calculation was performed to determine a 7.5 point difference on the NDI at 4 weeks. All data were analysed with SPSS version 14.0. Effect sizes were calculated using Cohen’s d for comparative outcomes at 2 and 4 weeks.
Results
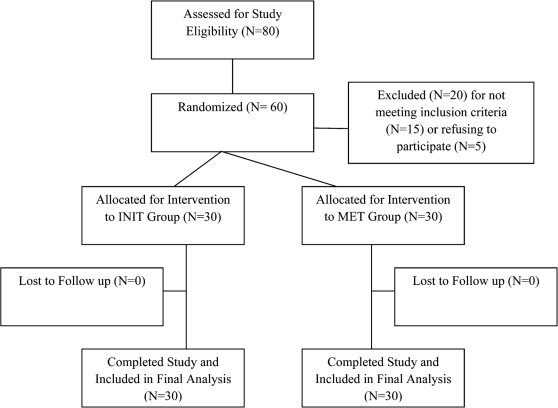
Eighty subjects were screened for eligibility. Fifteen subjects failed to meet the criteria for study participation while five subjects selected not to participate and did not sign the informed consent form. Sixty subjects remained and were randomized (Fig. 5). Thirty subjects were randomized to receive METs, with mean age 28 years (SD = 10 years), and 30 subjects received INIT, with mean age 27 years (SD = 8 years). All 60 subjects completed the study and were included in the analysis. The baseline characteristics were found to be similar between groups (P > 0.05); however, the subjects in the MET group were significantly older than those receiving INIT (P < 0.01) (Table 1).
Figure 5.
Study inclusion flow chart. INIT = integrated neuromuscular inhibition technique; MET = muscle energy technique.
Table 1. Baseline characteristics of the sample.
| Variable | MET | INIT |
| Gender | 12 male | 13 male |
| 18 female | 17 female | |
| Age (years) | 28.2 (4.78) | 27.6 (4.28) |
| Lateral flexion (°) | 24.8 (1.39) | 24.73 (1.41) |
| VAS | 8.2 (0.66) | 8.36 (0.55) |
| Neck disability | 42.9 (6.01) | 42.96 (6.09) |
Note: MET = muscle energy technique; INIT = integrated neuromuscular inhibition technique. All values represent the mean with standard deviation (SD).
Both groups demonstrated significant levels of improvement in pain intensity (P < 0.01), lateral cervical flexion (P < 0.01), and neck disability at the 2 and 4 week follow-up points (P < 0.01). The between-group analysis indicated that there was significantly greater improvement in pain, functioning, and lateral flexion favoring the group receiving the INIT at both the 2 and 4 week follow-up points (P < 0.05) (Table 2).
Table 2. Between-group change scores from baseline to 2 and 4 weeks .
| Variable | At 2 weeks |
P value/Cohen’s d | At 4 weeks |
P value/Cohen’s d | ||
| Change score MET, mean/SD (95% CI) | Change score INIT, mean/SD (95% CI) | Change score MET, mean/SD (95% CI) | Change score INIT, mean/SD (95% CI) | |||
| Lateral flexion (°) | 27.65/1.59 (0.87–2.34) | 30.71/1.42 (0.29–0.32) | <0.01/0.94 | 29.33/1.72 (1.32–1.84) | 34.44/1.2 (0.10–0.73) | <0.01/0.97 |
| VAS | 7.03/0.69 (0.35–0.88) | 6.46/0.55 (0.09–0.55) | <0.01/0.92 | 6.10/0.68 (0.21–0.31) | 5.28/0.47 (0.29–0.57) | <0.01/0.97 |
| Neck disability index* | 37.7/6.32 (0.51–0.85) | 33.04/5.05 (0.24–0.29) | <0.01/0.79 | 31.88/4.4 (0.07–0.91) | 27.19/3.7 (0.57–1.12) | <0.01/0.94 |
Note: VAS = visual analog scale. All values are expressed as mean with standard deviation (SD) and 95% CI. P value and Cohen’s d reflects between-groups changes.
Function measured with the neck disability index (score range: 0–50 with higher score indicating greater disability).
Calculated effect sizes at 2 weeks revealed a large treatment effect favoring the INIT group for VAS scores, NDI, and lateral flexion with effect sizes of 0.94, 0.92, and 0.79 respectively. At 4 weeks, INIT still demonstrated a large treatment effect compared to MET only providing magnitude measures of 0.97 (lateral flexion), 0.97 (VAS), and 0.94 (NDI).
Discussion
The results of the present study have been reported using the CONSORT guidelines for RCTs.27 The results indicate that METs may be a viable option for addressing active TrPs in the upper trapezius muscle; however, the addition of ischemic compression and SCS to the METs, INIT, produced significantly greater results. Subjects receiving INIT reduced their pain levels by a mean VAS of 1.18 mm compared to the individuals that received the MET in isolation. INIT also reduced the participant’s neck disability by a mean change of 5.85 points compared to 5.82 points for those that received MET. Lastly lateral cervical side bending ROM was significantly improved by a mean change of 3.73° for the subjects receiving INIT and 1.68° for those receiving MET. The results indicate significant between-group differences for VAS and NDI studies favoring the INIT approach over the MET approach for subjects with non-specific neck pain presenting with active TrPs in the upper trapezius muscle.
Our results agree with previously published trials on this subject indicating the ability of METs to affect TrPs.28–30 Chaitow and Delaney28 noticed a consistent reduction of TrP pain with the post-isometric relaxation approach (MET) at a 4 week follow-up. Goldenburg29 and Delany30 reported decreased pain intensity following the application of an osteopathic treatment package which included MET as a major element. Blanco and collegues31 identified the benefit of the post-isometric relaxation approach (MET) on latent masseter muscle TrPs as demonstrated by an improvement in active mouth opening (P < 0.01).
In the present study, the MET approach proved to be effective in improving all three outcome measures; however, the INIT was found superior versus MET only in its ability to improve pain, lateral flexion, and neck disability. These results again agree with previous research in this area as reports have indicated the benefit of such an approach in reducing pain and significantly improving functional status.32,33 Rubin et al.32 randomized subjects with identified TrPs into three groups, osteopathic manipulative treatment (OMT) (SCS and MET) plus medication, OMT plus placebo, and a placebo only. The group receiving OMT and medication demonstrated the largest improvement in quality of life and reduction of TrP tenderness. Owing to the combination of non-manual and manual interventions, the true identification of the benefit produced from the manual therapy component of the treatment is difficult. The current RCT did not involve non-manual therapy interventions, thus allowing for a stronger indication of the influence of manual therapy on the outcome measures studied.
The benefit of the INIT approach over the MET may lie in the addition of direct ischemic compression and subsequent tissue relaxation (SCS).34 According to Travell,5 ischemic compression decreases the sensitivity of painful nodules in muscle. Simons35 proposed that local pressure may equalize the length of sarcomeres in the involved TrP and consequently decrease the pain. Additionally, the subsequent tissue relaxation created by attaining a position of TrP ease (SCS) has been proposed as a mechanism of facilitating ‘unopposed arterial filling’ which allows for a reduction of tone in the tissues involved. This reduction in local tone further results in modification of neural reporting and improved local circulation. These changes ultimately facilitate a resetting of the neural reporting structures, resulting in a more normal resting length, enhanced circulation, and decreased pain.36
The exact mechanism by which ischemic compression and SCS contribute to the deactivation of TrPs is currently unknown and further research is required in this area. However, the current lack of understanding of the mechanisms of resolution should not preclude the pursuit of treatment for this condition. The combined treatment program of the INIT approach has demonstrated superiority to METs in isolation and should therefore be considered as a viable option for active upper trapezius TrPs. Despite the current findings, the best approach to treatment of TrPs has yet to be identified and further research is warranted to compare other manual physical therapy interventions to the INIT approach.
Study limitations
The present study is not without limitations. The absence of a true no-treatment control group makes it difficult to differentiate between the treatment effect and the natural course of the disorder, thus threatening the internal validity of the study. The INIT group received a multimodal approach as compared to control group who received MET only. The authors recognize the potential for attention bias as the INIT group was treated for a greater amount of time each session. Generalizability of the findings is limited by the short-term follow-up used in this study and a longer period of follow-up is recommended to determine the lasting effects of this approach. Lastly, although the current treatment program produced statistically significant reductions in pain and disability, the results may not be clinically meaningful as per recent evidence indicating a higher level of change required for clinically meaningful results.37
Conclusion
In patients with non-specific neck pain, an integrated approach (INIT) to the treatment of TrPs has proven to be more beneficial in relieving pain, reducing stiffness, and improving functional ability as compared to METs in isolation. The results of this clinical trial contribute to the growing body of evidence supporting the use of manual physical therapy in individuals with active TrPs. Further research is warranted with variable competing interventions such as cervical and thoracic thrust manipulations. Longer follow-up periods are recommended as well as the investigation of whether the INIT approach produces clinically meaningful outcomes.
References
- 1.Douglass AB, Bope ET. Evaluation and treatment of posterior neck pain in family practice. J Am Board Fam Pract 2004;17: S13–22 [DOI] [PubMed] [Google Scholar]
- 2.Cote P, Cassidy JD, Carroll LJ, Kristman V. The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain 2004;112: 267–73 [DOI] [PubMed] [Google Scholar]
- 3.Borghouts JA, Koes BW, Bouter LM. The clinical course and prognostic factors of non-specific neck pain: a systematic review. Pain 1998;77: 1–13 [DOI] [PubMed] [Google Scholar]
- 4.Mense S, Simons DG, Russell IJ. Muscle pain: understanding its nature, diagnosis and treatment. Philadelphia, PA: Lippincott Williams & Wilkins; 2000 [Google Scholar]
- 5.Travell J, Simons DG. Myofascial pain and dysfunction. The trigger point manual. The lower extremities. 1st ed. Vol. II Baltimore, MD: Lippincott Williams & Wilkins; 1999 [Google Scholar]
- 6.Nachemson A, Waddell G, Norlund AI. Epidemiology of neck and low back pain. Nachemson AL, Johnsson E, (eds.) Neck and back pain, the scientific evidence of causes, diagnosis, and treatment. Philadelphia, PA: Lippincott Williams & Wilkins; 2000, 165–87 [Google Scholar]
- 7.Harden RN, Bruehl SP, Gass S, Niemiec C, Barbick B. Signs and symptoms of the myofascial pain syndrome: a national survey of pain management providers. Clin J Pain 2000;16: 64–72 [DOI] [PubMed] [Google Scholar]
- 8.Simons DG, Travell J, Simons LS. Myofascial pain and disfunction. Travel J, Simons D, (eds.), The trigger point manual. 2nd ed. Vol. 1 Baltimore, MD: Lippincott Williams & Wilkins, 1999, 1–8 [Google Scholar]
- 9.Fernandez-de-las Penas C, Sohrbeck Campo M, Fernandez Carnero J, Miangolarra Page JC. Manual therapies in myofascial trigger point treatment: a systematic review. J Bodyw Mov Ther 2005;9: 27–34 [Google Scholar]
- 10.Alvarez D, Rockwell P. Trigger points: diagnosis and management. Am Fam Physician 2002;65: 653–60 [PubMed] [Google Scholar]
- 11.Rickards LD. The effectiveness of non-invasive treatments for active myofascial trigger point pain: a systematic review of the literature. Int J Osteopath Med 2006;9: 120–36 [Google Scholar]
- 12.Chaitow L. Muscle energy techniques. Edinburgh: Churchill Livingstone; 2001 [Google Scholar]
- 13.Niel-Asher S. The concise book of trigger points. Chichester: Lotus Publishing; 2005 [Google Scholar]
- 14.Kuchera WA, Kuchera ML. Osteopathic principles in practice. Kirksville, MO: Kirksville College of Osteopathic Medicine Press; 1992 [Google Scholar]
- 15.Fryer G, Fossum C. Therapeutic mechanisms underlying muscle energy approaches. Cephalalgia 2008;28: 264–7518254895 [Google Scholar]
- 16.Gemmel H, Miller P, Nordstrom H. Immediate effect of ischaemic compression and trigger point pressure release on neck pain and upper trapezius trigger point: a randomized controlled trial. Clin Chiropract 2008;11: 30–6 [Google Scholar]
- 17.Hou CR, Tsai LC, Cheng KF, Chung KC, Hong CZ. Immediate effects of various physical therapeutic modalities on cervical myofasical pain and trigger point sensitivity. Arch Phys Med Rehabil 2002;83: 1406–14 [DOI] [PubMed] [Google Scholar]
- 18.Chaitow L. Modern neuromuscular techniques. Edinburgh: Churchill Livingstone; 1996 [Google Scholar]
- 19.Chaitow L. Neuro-muscular technique. Wellingborough: Thorsons; 1982 [Google Scholar]
- 20.Hanten W, Olson S, Butts N, Nowicki A. Effectiveness of a home program of ischemic pressure followed by sustained stretch for treatment of myofascial trigger points. Phys Ther 2000;80: 997–1003 [PubMed] [Google Scholar]
- 21.Dardzinski JA, Ostrov BE, Hamann LS. Myofascial pain unresponsive to standard treatment. Successful use of a strain and counterstrain technique with physical therapy. J Clin Rheumatol 2000;6: 169–74 [DOI] [PubMed] [Google Scholar]
- 22.Fernandez-de-las-Penas CF, Alonso-Blanco C, Miangolarra JC. Myofascial trigger points in subjects presenting with mechanical neck pain: a blinded, controlled study. Man Ther 2007;1: 29–33 [DOI] [PubMed] [Google Scholar]
- 23.Vernon H, Mior S. The neck disability index – a study of reliability and validity. J Manipulative Physiol Ther 1991;14: 409–15 [PubMed] [Google Scholar]
- 24.Youdas JW, Carey JR, Garrett TR. Reliability of measurements of cervical spine range of motion-comparison of three methods. Phys Ther 1991;71: 98–106 [DOI] [PubMed] [Google Scholar]
- 25.Chaitow L. Muscle energy techniques. 3rd ed. Edinburgh: Churchill livingstone, 2003 [Google Scholar]
- 26.Travell J, Simons D. Myofascial pain and dysfunction – the trigger point manual. Baltimore, MD: Lippincott Williams & Wilkins; 1992 [Google Scholar]
- 27.Moher D, Schultz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel randomized trials. JAMA 2001;285: 1987–91 [DOI] [PubMed] [Google Scholar]
- 28.Chaitlow L, Delany J. Clinical application of neuromuscular techniques. Vol. 1 The upper body. Amsterdam: Elsevier; 2008 [Google Scholar]
- 29.Goldenberg D. Fibromyalgia, chronic fatigue syndrome and myofascial pain syndrome. Curr Opin Rheumatol 1993;5: 199–208 [DOI] [PubMed] [Google Scholar]
- 30.Delany JP. Foundational platform of NMT. FSMTA Convention 2007:08 [Google Scholar]
- 31.Blanco CR, de las Peñas CF, Xumet JEH, Algaba CP, Rabadán MF, de la Quintana MCL. Changes in active mouth opening following a single treatment of latent myofascial trigger points in the masseter muscle involving post-isometric relaxation or strain/counterstrain. J Bodyw Mov Ther 2005:10: 197–205 [Google Scholar]
- 32.Rubin BR, Gamber RG, Cortez CA, Wright TJ, Shores J, Davis G. Treatment options in fibromyalgia syndrome. J Am Osteopath Assoc 1990;90: 844–5 [Google Scholar]
- 33.Gamber RG, Shores JH, Russo DP, Jimenez C, Rubin BR. Osteopathic manipulative treatment in conjunction with medication relieves pain associated with fibromyalgia syndrome: results of a randomized clinical pilot project. J Am Osteopath Assoc 2002:102: 321–5 [PubMed] [Google Scholar]
- 34.Chaitow L. INIT in treatment of pain and trigger points. Br J Osteopathy 1994:13: 17–21 [Google Scholar]
- 35.Simons DG. Understanding effective treatments of myofascial trigger points. J Bodyw Mov Ther 2002;6: 81–8 [Google Scholar]
- 36.Jones LH. Strain and counterstrain. Colorado Springs, CO: The American Academy of Osteopathy; 1981 [Google Scholar]
- 37.Young BA, Walker MJ, Strunce JB, Boyles RE, Whitman JM, Childs JD. Responsiveness of the neck disability index in patients with mechanical neck disorders. Spine J 2009;9: 802–8 [DOI] [PubMed] [Google Scholar]