Abstract
BACKGROUND:
Physician advice increases quit rates 1% to 3% above unassisted quit rates among adults, an increase sufficient to be ranked as a high-priority, evidence-based preventive service. However, there is little research on the potential impact of physician advice on adolescent smoking.
OBJECTIVE:
The purpose of this study was to examine the association between recalled physician communication and adolescents' attitudes toward smoking, knowledge about smoking, intentions to smoke, tobacco use, and quitting behaviors.
METHODS:
This study was a retrospective observational study of 5154 students (82.9% black, 17.1% white) from an urban, mid-South school system. Outcome variables included adolescents' self-rated attitudes toward smoking, knowledge about smoking, intentions to smoke, tobacco use, and quitting behaviors.
RESULTS:
Physician advice and the combination of screening and advice were associated with healthier attitudes about smoking. Physician screening and advice were also associated with a more accurate knowledge regarding tobacco-related damage. Among current smokers, recalled physician advice was also associated with reduced intentions to smoke in 5 years. Importantly, advised teens were more likely to plan to quit smoking in 6 months. Furthermore, teens who were screened by their physician reported significantly more quit attempts than those who were neither screened nor advised (P = .007).
CONCLUSIONS:
Physician's tobacco-related interactions with adolescents seemed to positively impact their attitudes, knowledge, intentions to smoke, and quitting behaviors. Brief physician interventions have the potential to be a key intervention on a public health level through the prevention, cessation, and reduction of smoking and smoking-related disease.
Keywords: smoking, adolescent, counseling, physician's role
WHAT'S KNOWN ON THIS SUBJECT:
Previous research has shown that physician advice against smoking has sufficient impact among adults to be ranked as a high-priority, evidence-based preventive service. However, little research has explored the potential benefits of physician advice against smoking among adolescents.
WHAT THIS STUDY ADDS:
This study examines the relationship between physician communications regarding smoking and adolescent tobacco use. The study is unique in that (1) it examines a range of tobacco use behaviors; and (2) it explores potential benefits for young nonsmokers as well as smokers.
Every day, ∼1000 adolescents in the United States become daily smokers.1 Fortunately, many teens who smoke make multiple quit attempts,2,3 but the odds of unaided success are low, with quit rates for teens ranging from 6.2% to 12.2%.4,5
Considerable research has evaluated cessation programs for adolescents who smoke. However, these programs have been plagued by recruitment difficulties and attrition.2 Even when recruitment and retention have been adequate, cessation rates for teen smokers have not improved significantly.6
Given these discouraging results, researchers have noted the potential importance of physicians' advice to adolescents. Previous research has shown that physician advice has sufficient impact among adults to be ranked as a high-priority, evidence-based preventive service.7 In fact, a Cochrane review found that brief physician advice to quit smoking produced 1% to 3% increases in adult cessation above unassisted quitting rates.8 Furthermore, annual physician advice has preventive cost savings comparable to those conveyed by annual influenza immunizations and biyearly mammograms.7 The advantages of physician intervention include time efficiency, cost efficiency,7,9,10 and accessibility.11–13
The Agency for Healthcare Research and Quality has developed clinical practice guidelines for the treatment of tobacco use and dependence, recognizing physician advice as a key public health intervention.9 These guidelines (“the 5 A's”) require physicians to ask about smoking status, advise patients to quit, assess whether patients are ready to quit, assist the patient with quitting, and arrange follow-up visits to avoid relapses. The Committee on Substance Abuse added “anticipation” to the beginning of this model for physicians' interactions with young people,14 a step designed to encourage physicians to provide preventive advice.
Given the success of physician advice with adults, surprisingly little research has explored its benefits for adolescents. Adolescent smoking differs significantly from that of adults2; thus, one would not necessarily expect physician interventions to have similar benefits for teenagers. Most research in this area has simply explored the frequency of physician screening and advice to teenagers. For example, 1 study examined the rates of physician intervention with adolescents, as reported by physicians.15 Physicians identified the smoking status of 71% of the adolescents but advised only 2% of all adolescents and 17% of the smokers to avoid tobacco. Other investigators obtained more encouraging results using adolescent reports of physician advice. More than 40% of teenagers reported being screened, and rates of advising ranged from 33% to 42%.13,16 Notably, 79% of adolescents said they would admit their smoking to their physicians,16 and young smokers preferred to receive smoking cessation services from physicians rather than from other professionals.17
The only study that has examined physician advice and adolescent quit attempts was conducted by Shelley et al.13 Results from this cross-sectional study indicated that physician advice increased the odds of a quit attempt among teenagers. However, the study did not examine the relationship between physician advice and the behavior of nonsmokers. In addition, the effects of physician communication on related variables (eg, knowledge about tobacco, intentions to smoke) were not explored. Our retrospective observational study is unique in that (1) it examines a range of smoking behaviors; and (2) it explores the benefits of physician advice for young nonsmokers as well as smokers.
METHODS
Overview
Data were drawn from the Memphis Health Project, a longitudinal study of smoking in urban, mid-South adolescents.18 The first survey was given in 1994 to a cohort of 6967 seventh grade students and repeated annually for 9 years. Surveys were administered in schools by teachers, using procedures that maximized student confidentiality. Parents notified the research team if they did not want their child to participate, and students provided written assent. The study was approved by the The University of Memphis institutional review board. Procedures are detailed elsewhere.18
Participants
The sample for this report comprised primarily (81%) 11 grade students, along with students from the original cohort who were either retained or advanced an additional year. Of the 7875 eligible students, 65.4% (5154 of 7875) participated. Diminished participation in the original cohort was due to absenteeism (8%), refusal to participate (7.5%), and various other reasons. This report includes data from 5154 adolescents who participated in the 11 grade year.
Measures and Coding of Items of Interest
Demographic variables were measured via self-report.
Physician Communication
Recalled physicians' interventions were measured using adolescent reports of (1) physician screening for tobacco; and (2) physician advice not to smoke. To measure screening, adolescents were asked if their physicians had inquired about whether they smoked. To measure advising, the youth were asked whether their physician advised them not to smoke. No time frame was provided for these questions; thus, there could be sizable variability in when the communication occurred. The 2 measures were used to create an overall measure of physician communication, with the following categories: neither screened nor advised (0); screened only (1); advised only (2); and both screened and advised (3). Thus, higher numbers were associated with more intense intervention.
Social Value
Four questions assessed the extent to which teenagers expected positive social outcomes from smoking,18 with responses measured on 4-point Likert scales. Scores were averaged, producing an overall scale ranging from 0 to 3, with higher scores representing stronger belief in the social benefits of smoking.
Knowledge About Health Risks
Knowledge of the health risks of smoking was measured by using 2 questions. One asked when smoking was dangerous, with 4 response options ranging from “as soon as you start to smoke” to “never.” The second asked students about tobacco-related damage, with response options ranging from “smoking really doesn't hurt your health” to “many people die from smoking.” Responses were coded from 0 to 3, so that higher scores indicated more accurate knowledge.
Intentions Variables
Intention to smoke was measured by 2 questions: “How likely is it that you will smoke cigarettes during the next year?” and “How likely is it that you will smoke cigarettes five years from now?” Responses on a 4-point scale ranged from “very unlikely” (0) to “very likely” (3). Higher scores indicated stronger intentions to smoke.
Tobacco Use
Smoking status was self-reported. Individuals who reported any use of tobacco, past or present, were coded as “ever smokers” (1). Those who had never smoked scored “0.”
Amount of smoking included 6 response options, ranging from “never smoked” (0) to “smoke at least 1 cigarette daily” (5).
Stage of change was assessed with measures of participants' history of and plans for smoking cessation.19 Four categories were included: precontemplation (0), contemplation (1), preparation (2), and action or maintenance (3).
Intentions to quit were assessed by asking “Are you seriously thinking about quitting smoking within the next 6 months?” Response options were “yes” (1) or “no” (0). Quitting status was measured by comparing smokers who had never tried to quit (0) with those with at least 1 attempt (1).
Students were asked to report the number of previous quit attempts. Response options included “never tried to quit” (0), “one time” (1), “two times” (2), and “three times or more” (3).
Relapse status was measured for those with a history of quitting. Those who had quit and were not currently smoking were identified as quitters (1). Those who had quit but resumed smoking were relapsers (0).
Data Analysis
When the dependent variable was categorical, χ2 tests or logistic regression was used. When the dependent variable was continuous, analysis of variance was used. Main effects were explored using Bonferroni tests or Dunnett's C, where appropriate. In addition, trend analyses and 1-way analysis of variances were used for follow-up assessments, with α set at .05.
RESULTS
Participant Characteristics
The 5154 participants averaged 16.9 years of age. Almost 56% of the sample was female. The ethnicity of the sample was well matched with that of the local school system, with 82.9% black and 17.1% white. Approximately 23% came from low-income neighborhoods.16
Overall, 54% of these students reported never smoking and 46% had smoked. Among those who smoked at least monthly, 88.2% had made at least 1 attempt to quit. Seventeen percent were precontemplators, 20.3% contemplators, 32.6% in preparation, and 30.1% in the action or maintenance stage (Tables 1 and 2).
TABLE 1.
Characteristics of the Sample Grouped According to Smoking Status
| Categorical Variablesa | Smoking Status, n (%) |
P | |
|---|---|---|---|
| Never Smoker | Ever Smoker | ||
| Gender | <.001 | ||
| Female | 1574 (32.3) | 1177 (24.1) | |
| Male | 1059 (21.7) | 1068 (21.9) | |
| Ethnicity | <.001 | ||
| Black | 2237 (48.7) | 1544 (33.6) | |
| White | 243 (5.3) | 565 (12.3) | |
Percentages represent percentages within the total sample.
χ2 tests were used to examine differences.
TABLE 2.
Tobacco Use Among Smokers
| Level of Smoking | Smoking Status, n (%) |
|
|---|---|---|
| Ever Smokers (n = 2265) | Current Smokersa (n = 681) | |
| Smoked once or twice | 1277 (56.4%) | NA |
| Used to smoke regularly but quit | 307 (13.6) | NA |
| Smoke at least once per month | 126 (5.6%) | 126 (18.5%) |
| Smoke at least once per week | 67 (3.0%) | 67 (9.8%) |
| Smoke 1–6 cigarettes per week | 127 (5.6%) | 127 (18.6%) |
| Smoke at least 1 cigarette daily | 361 (15.9%) | 361 (53.0%) |
NA indicates not applicable.
Current smokers are subsumed in the ever-smoker category and are defined as at least monthly smokers.
According to the adolescents, many students had received neither screening for tobacco use nor advice about smoking from their physician (43.2%). In addition, 14.6% were only screened, and 13.3% were only advised. Less than one third (28.9%) reported being both screened and advised not to smoke.
Social Value
Recalled physician communication, smoking status (never versus ever smoker), and their interaction were used to predict students' perceptions of the social value of smoking. The interaction between smoking status and physician communication was not significant (F[3]4,515 = 1.02; P = .38). However, there was a significant main effect for smoking status (F[1]4,515 = 534.67; P < .001), such that never smokers rated the social value of smoking more negatively than ever smokers (Table 3). In addition, there was a main effect of physician communication (F[3]4,515 = 8.29; P < .001) (Table 4). Follow-up analyses revealed that participants who were advised not to smoke rated the social value of tobacco less than those who received no intervention and those who were simply screened. Similarly, teenagers that were screened and advised had more negative perceptions of the social value of smoking than participants with no intervention or screening only.
TABLE 3.
Descriptive Statistics for Participants Grouped According to Smoking Status
| Variable | Smoking Status, Mean (SD) |
P | |
|---|---|---|---|
| Never Smoker | Ever Smoker | ||
| Social valuea | 0.56 (.57) | 1.04 (0.68) | <.001 |
| Dangerousness of smokingb | 2.53 (.81) | 2.34 (0.90) | <.001 |
| Tobacco-related damageb | 2.63 (.70) | 2.58 (0.72) | .052 |
| Intentions to smoke during the next yeara | 0.12 (.47) | 0.94 (1.16) | <.001 |
| Intentions to smoke cigarettes 5 y from nowa | 0.14 (0.50) | 0.76 (1.00) | <.001 |
| Amount of current smokinga | NA | 0.96 (0.97) | |
| No. of previous quit attemptsb | NA | 1.43 (1.16) | |
NA indicates not applicable.
Lower scores represent better outcomes.
Higher scores represent better outcomes.
TABLE 4.
Descriptive Statistics for Participants Grouped According to Physician Communication Status
| Dependent Variable | Physician Communication, Mean (SD) |
|||
|---|---|---|---|---|
| Neither Screened nor Advised | Screened Only | Advised Only | Screened and Advised | |
| Social valuea | 0.82 (0.67) | 0.81 (0.67) | 0.70 (0.64) | 0.72 (0.66) |
| Dangerousness of smokingb | 2.59 (0.71) | 2.58 (0.76) | 2.63 (0.71) | 2.64 (0.67) |
| Tobacco-related damageb | 2.42 (0.87) | 2.43 (0.86) | 2.43 (0.86) | 2.49 (0.84) |
| Intentions to smoke during the next yeara | 0.49 (0.94) | 0.54 (1.00) | 0.39 (0.86) | 0.53 (1.00) |
| Intentions to smoke cigarettes 5 y from nowa | 0.42 (0.81) | 0.47 (0.89) | 0.30 (0.69) | 0.47 (0.88) |
| Amount of current smokinga | 0.78 (0.93) | 0.99 (0.93) | 0.93 (0.97) | 1.15 (1.02) |
| No. of previous quit attemptsb | 1.30 (1.12) | 1.69 (1.13) | 1.43 (1.22) | 1.44 (1.17) |
Lower scores represent better outcomes.
Higher scores represent better outcomes.
Knowledge About Smoking
We first examined participants' knowledge of the dangerousness of smoking. Results indicated no interaction between smoking status and physician communication (F[3]4,768 = 0.86; P = .46). However, the main effect of smoking status was significant (F[1]4,768 = 48.07; P < .001), so that never smokers had more accurate knowledge than ever smokers. Physician communication had a main effect on teenagers' perceptions of the dangers of smoking (F[3]4,768 = 2.71; P = .04). A trend analysis identified a significant linear trend, with knowledge increasing as communication intensity increased (F[1]4,947 = 5.67; P = .02).
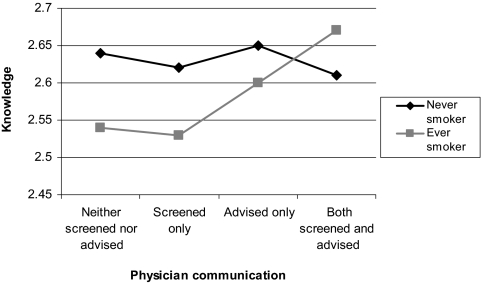
Next we examined students' perceptions about tobacco-related damage. The interaction between smoking status and physician communication was significant (F[3]4,816 = 3.39; P = .02). Follow-up tests were conducted for ever smokers and never smokers separately (Fig 1). Teen-aged smokers became more accurate in their estimates of tobacco-related damage as physicians' interventions increased (F[3]2,228 = 4.60; P = .003). Posthoc analyses indicated that teen-aged smokers who were both screened and advised had more knowledge about the health risks of smoking than smokers who received no intervention or only screening. In contrast, physicians' communication was not associated with never smokers' knowledge. Main effects were not significant.
FIGURE 1.
Knowledge of tobacco-related damage according to smoking status and physician communication. Higher scores indicate more knowledge.
Intentions to Smoke
Intentions to smoke during the next year were examined first. The interaction between smoking status (never versus ever) and physician communication was not significant (F[3]4,790 = 1.42; P = .23), and there was no main effect for communication (F[3]4,790 = 1.16; P = .33). Predictably, never smokers had fewer intentions to smoke than ever smokers (F[1]4,790 = 815.18; P < .001).
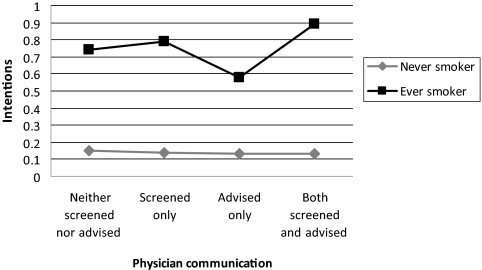
Teenagers' intentions to smoke in 5 years were explored next. A significant interaction between smoking status (never versus ever) and physician communication emerged (F[3]4,765 = 3.65; P = .01). Among smokers, there was a significant cubic component for physician communication (F[1]4,765 = 12.81; P < .001). Smokers had fewer intentions to continue to smoke when they received physician advice (Fig 2). Among never smokers, physician communication was unrelated to intentions. We also found main effects of smoking status and physician communication (F[1]4,765 = 559.30; P < .001 and F[3]4,765 = 3.73; P = .01, respectively). Never smokers had fewer intentions to smoke than ever smokers, and teenagers that had been advised by their doctor had fewer intentions than other teens.
FIGURE 2.
Intentions to smoke in 5 years according to smoking status and physician communication. Higher scores indicate stronger intentions to smoke.
Current Smoking
To identify current smokers, we selected adolescents who reported smoking at least once a month. We then explored whether physician communication was related to the amount of current smoking, using smokers only. There was a significant main effect of physician communication on current smoking (F[3]695 = 6.40; P < .001. The effect was linear, so that as physician intervention increased in intensity, so did the amount smoked (F[1]695 = 12.62; P < .001) (Table 3). One possible explanation is that physicians may increase the intensity of their communication about tobacco once they learn that a teenager smokes.
Quit Attempts
Logistic regression was used to predict plans to quit smoking, with physician communication serving as the independent variable. The lowest level of intervention (no screening, no advice) served as the referent. Results revealed that adolescents who were advised to stop smoking were 1.76 times more likely to plan to quit than those that were neither asked nor advised (P = .04).
We also found that physician communication was associated with the number of quit attempts (F[3]851 = 4.08; P = .007). Follow-up tests indicated that teenagers who were screened by their physicians made more quit attempts than those who received no intervention.
There was no evidence of an association between physician communication and stage of change or the odds of maintaining successful smoking cessation (both comparisons, P > .05).
DISCUSSION
The present study is the first, to our knowledge, to examine the relationship between physician communication and a spectrum of tobacco-related variables in teenagers, including expectations about social reinforcement from smoking, knowledge of the effects of smoking, intentions to smoke, tobacco use, intentions to quit, attempts to quit, and success in quitting. Our study is also novel in its focus on the potential impact of physician communication on both smokers and nonsmokers.
Results suggest that physician intervention affects a range of attitudes, beliefs, and behaviors. For example, regardless of whether they were smokers, teenagers who reported conversations with physicians about tobacco were less likely to believe that smoking would improve their social standing. Furthermore, when physicians screened and advised youth about tobacco, the adolescents were more knowledgeable about its dangers, particularly if they smoked. Intentions to smoke in 5 years were lower among smokers who discussed their habit with their physician. Similarly, adolescent smokers who were advised by their physician were more likely to plan on quitting. Finally, those who talked with their physicians made more quit attempts than those who did not.
Taken together, these data suggest that physician communication has an impressive effect on tobacco use. However, these correlational findings might simply indicate that adolescents who smoke less have greater recall of physician communications about smoking. In this case, one might expect that light smokers would report more physician discussions about smoking than heavy smokers. Alternately, physicians might communicate more with teenagers who are less likely to smoke.
Our data argue against both of these alternate interpretations. We found, in fact, that physicians provided more intensive interventions for those who smoked more. Thus, physicians seemed to detect which teenagers were more at risk for smoking—and were more likely to take time to discuss tobacco use with them. Given that physician communication was associated with less belief in the social value of smoking, better knowledge of health risks, fewer intentions to smoke, more intentions to quit, and more quit attempts, it seems likely that physicians' interactions with teenagers do impact their beliefs and behavior in a positive way.
Little attention has been paid to the potential for physicians to reduce smoking onset. Our results suggested that physician communication can help nonsmokers as well as smokers. For example, the benefits of physician interventions on knowledge and perceptions of the social value of smoking were similar for both groups of teenagers. Conversely, physician communication had no impact on nonsmokers' intentions to smoke. Additional research is needed to explore ways in which physicians may decrease smoking onset.
Surprisingly, we obtained different results when we explored the relationship of physician communication with intentions to smoke in 1 year versus 5 years. Physician advice was not associated with reduced intentions to smoke in 1 year, but it did predict fewer intentions to smoke in 5 years. Perhaps physician communication serves to prime adolescents to consider eventual quitting.
There were a number of weaknesses in our study. Each construct was assessed by few items, but the questions were culled from similar investigations16,18 and the items behaved as expected. Another limitation is the lack of biochemical validation of smoking. However, studies of this kind have been shown to produce sufficiently valid self-reported smoking rates, especially when confidentiality is assured.16 Third, our sample consisted largely of black participants. Although representation of minorities is important because smoking is more harmful to blacks, it also limits the study's generalizability.20 Fourth, our design is correlational in nature, leaving the causal mechanisms of observed differences murky. Finally, our measure of physician communication was based on student recall.
Nonetheless, this investigation suggests important areas for research. Randomized controlled trials in which the behavior of physicians is manipulated would clarify causal direction. Studies that use objective measures of physician behavior are also needed. Additional work should determine the potential benefits of each type of physician intervention. Our findings broadly suggest that both screening and advice produce more benefit than no intervention or screening alone. It would also be helpful to explore the time frame within which physician communication is effective. Finally, studies are needed to determine the sequence of changes that occurs in attitudes, knowledge, and behavior. Previous research has suggested that changes in attitudes and knowledge are precursors to behavior change.21–23 In fact, Bruvold24 suggested that attitudes may be harder to improve than knowledge and behavior. Nonetheless, negative attitudes toward smoking and knowledge of health risks have been identified as key motivators for smoking cessation.25,26 In this study, attitudes, knowledge, and behavior seemed responsive to physician communication. Understanding the sequence of changes teenagers experience after receiving advice might help researchers design more thoughtful intervention programs.
Most smoking cessation interventions for adolescents have shown poor results.6 For this reason, the cumulative impact of physician advice, a relatively simple intervention with wide reach, may be of great importance for public health. Physicians are not currently advising adolescents at desirable levels, but research has shown that they value being treated as partners in helping adolescents to quit.27 By measuring the effects of brief screening and advice carefully, it may be easier to convince health care professionals to add communication about tobacco use to their routine practice with adolescents.
CONCLUSIONS
Physicians' tobacco-related interactions with adolescents seemed to positively impact their attitudes, knowledge, intentions to smoke, and quitting behaviors. Brief physician interventions have the potential to be a key intervention on a public health level through the prevention, cessation, and reduction of smoking and smoking-related disease.
ACKNOWLEDGMENTS
This study was supported by National Heart, Lung, and Blood Institute grant HL50723 and a Centers of Excellence grant awarded by the State of Tennessee to the Department of Psychology, University of Memphis.
Footnotes
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
Funded by the National Institutes of Health (NIH).
REFERENCES
- 1. Substance Abuse and Mental Health Services Administration Results from the 2008 National Survey on Drug Use and Health: National Findings. Rockville, MD: Office of Applied Studies, NSDUH Series H-36, HHS Publication No. SMA 09–4434; 2009 [Google Scholar]
- 2. Centers for Disease Control and Prevention Preventing Tobacco Use Among Young People: A Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1994 [Google Scholar]
- 3. Bancej C, O'Loughlin J, Platt RW, Paradis G, Gervais A. Smoking cessation attempts among adolescent smokers: a systematic review of prevalence studies. Tob Control. 2007;16(6):e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention (CDC) High school students who tried to quit smoking cigarettes—United States, 2007. MMWR Morb Mortal Wkly Rep. 2009;58(16):428–431 [PubMed] [Google Scholar]
- 5. Sussman S, Sun P, Dent CW. A meta-analysis of teen cigarette smoking cessation. Health Psychol. 2006;25(5):549–557 [DOI] [PubMed] [Google Scholar]
- 6. Grimshaw GM, Stanton A. Tobacco cessation interventions for young people. Cochrane Database Syst Rev. 2006;(4):. Available at: http://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD003289/pdf_fs.html Accessed June 9, 2009 [DOI] [PubMed]
- 7. Solberg LI, Maciosek MV, Edwards NM, Khanchandani HS, Goodman MJ. Repeated tobacco-use screening and intervention in clinical practice: health impact and cost effectiveness. Am J Prev Med. 2006;31(1):62–71 [DOI] [PubMed] [Google Scholar]
- 8. Stead LF, Bergson G, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2008;(2):. Available at: http://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD000165/pdf_fs.html Accessed June 9, 2009 [DOI] [PubMed]
- 9. Fiore MC, Jaén CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. Rockville, MD: US Department of Health and Human Services, Public Health Service; 2008 [Google Scholar]
- 10. Westmaas JL, Nath V, Brandon TH. Contemporary smoking cessation. Cancer Control. 2000;7(1):56–62 [DOI] [PubMed] [Google Scholar]
- 11. Centers for Disease Control and Prevention (CDC) Physician and other health-care professional counseling of smokers to quit—United States, 1991. MMWR Morb Mortal Wkly Rep. 1993;42(44):854–857 [PubMed] [Google Scholar]
- 12. Centers for Disease Control and Prevention (CDC) QuickStats: annual rate of visits per person to physician offices, by patient age group—United States, 2003. MMWR Morb Mortal Wkly Rep. 2005;54(48):1238 [Google Scholar]
- 13. Shelley D, Cantrell J, Faulkner D, Haviland L, Healton C, Messeri P. Physician and dentist tobacco use counseling and adolescent smoking behavior: results from the 2000 National Youth Tobacco Study. Pediatrics. 2005;115(3):719–725 [DOI] [PubMed] [Google Scholar]
- 14. Committee on Substance Abuse American Academy of Pediatrics: Tobacco's toll: implications for the pediatrician. Pediatrics. 2001;107(4):794–798 [PubMed] [Google Scholar]
- 15. Thorndike AN, Ferris TG, Stafford RS, Rigotti NA. Rates of US physicians counseling adolescents about smoking. J Natl Cancer Inst. 1999;91(21):1857–1862 [DOI] [PubMed] [Google Scholar]
- 16. Alfano CM, Zbikowski SM, Robinson LA, Klesges RC, Scarinci IC. Adolescent reports of physician counseling for smoking. Pediatrics. 2002;109(3):. Available at: www.pediatrics.org/cgi/content/full/109/3/e47 [DOI] [PubMed] [Google Scholar]
- 17. Jackson AA, Robinson LA, Ali KS, Hum AM. Technology vs. interpersonal contact: adolescent smokers' preferences for smoking cessation formats. Poster presented at: Fourteenth Annual Meeting of the Society for Research on Nicotine and Tobacco; February 29, 2008; Portland, OR Available at: www.srnt.org/conferences/past/2008/pdf/2008_SRNT_Proceedings.pdf Accessed April 19, 2011 [Google Scholar]
- 18. Robinson LA, Klesges RC, Zbikowski SM, Glaser R. Predictors of risk for different stages of adolescent smoking in a biracial sample. J Consult Clin Psychol. 1997;65(4):653–662 [DOI] [PubMed] [Google Scholar]
- 19. Pallonen UE. Transtheoretical measures for adolescent and adult smokers: similarities and differences. Prev Med. 1998;27(5 pt 3):A29–A38 [DOI] [PubMed] [Google Scholar]
- 20. US Department of Health and Human Services Tobacco Use Among US Racial/Ethnic Minority Groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics: A Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1998 [Google Scholar]
- 21. Robinson LA, Emmons KM, Moolchan ET, Ostroff JS. Developing smoking cessation programs for chronically ill teens: lessons learned from research with healthy adolescent smokers. J Pediatr Psychol. 2008;33(2):133–144 [DOI] [PubMed] [Google Scholar]
- 22. Klein JD, Wilson KM. Delivering quality care: adolescents' discussion of health risks with their providers. J Adolesc Health. 2002;30(3):190–195 [DOI] [PubMed] [Google Scholar]
- 23. Robinson LA, Klesges RC, Levy MC, Zbikowski SM. Preventing cigarette use in a bi-ethnic population: results of the Memphis Smoking Prevention Program. Cogn Behav Pract. 1999;6(3):136–143 [Google Scholar]
- 24. Bruvold WH. A meta-analysis of adolescent smoking prevention programs. Am J Public Health. 1993;83(6):872–880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Engels RC, Knibbe RA, de Vries H, Drop MJ. Antecedents of smoking cessation among adolescents: who is motivated to change? Prev Med. 1998;27(3):348–357 [DOI] [PubMed] [Google Scholar]
- 26. Riedel BW, Robinson LA, Klesges RC, Mclain-Allen B. What motivates adolescent smokers to make a quit attempt? Drug Alcohol Depend. 2002;68(2):167–174 [DOI] [PubMed] [Google Scholar]
- 27. McIntosh S, Ossip-Klein DJ, Hazel-Fernandez L, Spada J, McDonald PW, Klein JD. Recruitment of physician offices for an office-based adolescent smoking cessation study. Nicotine Tob Res. 2005;7(3):405–412 [DOI] [PubMed] [Google Scholar]