Abstract
OBJECTIVE:
The objective was to describe the characteristics of pediatric discharges associated with long-term mechanical ventilation (LTMV) compared with those with complex chronic conditions (CCCs), and evaluate trends over time in health care utilization for the discharges associated with LTMV.
METHODS:
The Kids' Inpatient Database, compiled by the Agency for Healthcare Research and Quality, was used. Routine newborn care was excluded. Discharges associated with LTMV were identified by using the International Classification of Diseases, Ninth Revision, code v46.1x and compared with discharges associated with CCCs in 2006 using simple regression and χ2 analyses. Trends in LTMV-associated discharges from 2000 to 2006 were assessed using variance-weighted least squares regression.
RESULTS:
In 2006, there were an estimated 7812 discharges associated with LTMV. Compared with discharges for children with CCCs, LTMV discharges had significantly higher mortality, longer lengths of stay, higher mean charges, more emergency department admissions, and more discharges to long-term care. From 2000 to 2006, there was a 55% increase in the number of LTMV discharges and a concurrent 70% increase in aggregate hospital charges. The majority of LTMV discharges occurred in children 4 years old and younger, and ∼50% of the aggregate charges were for children younger than 1 year.
CONCLUSIONS:
Discharges for children associated with LTMV require substantively greater inpatient resource use than other children with CCCs. As the number of discharges and associated aggregate charges increase over time, additional research must examine patterns of care for specific clinical subgroups of LTMV, especially children aged 4 years and younger.
Keywords: mechanical ventilation, respiratory failure, utilization, hospitalization, Kids' Inpatient Database
WHAT'S KNOWN ON THIS SUBJECT:
Children dependent on long-term mechanical ventilation are a diverse group who experience respiratory failure due to a variety of chronic conditions. Previous state-based analyses estimated a prevalence of 6 to 14 per 100 000 children but did not focus on age differences.
WHAT THIS STUDY ADDS:
The rate of hospital discharges for children dependent on long-term mechanical ventilation has grown to 173.6 per 100 000 nonnewborn pediatric discharges in 2006. Young children and infants consume the highest proportion of health care resources and should be an area of additional study.
The frequency of inpatient care has increased for all children with complex chronic conditions (CCCs) over the last decade.1 A subgroup of this population with substantial technologic dependence are children dependent on long-term mechanical ventilation (LTMV). Over the last 3 decades, technologic improvements in LTMV care have extended the survival of many children with severe airway and/or respiratory disease.2–4 Despite these widely recognized advances, there has been no national characterization of changes in hospitalized care over time for children with LTMV dependence.
State-level, cross-sectional studies have attempted to estimate the prevalence of children requiring LTMV but with variable case-finding methods and results.5–7 These studies provided state and regional (via referral) estimates of the burden of illness, but they cannot be used to derive national figures. They offered a limited evaluation of health care utilization of their population of children requiring LTMV.
The length of the initial hospitalization for children dependent on LTMV has generally declined from >1 year to several months.2–4,8–15 A significant proportion of that time has been attributed to finding suitable home nursing care.2,3 Despite this improvement, frequent admissions occur, with up to 40% of children dependent on LTMV requiring acute care hospitalizations in a 6-month time period and up to one third of patients living in acute or long-term care facilities.5,16,17
The objective of this analysis was to describe the characteristics of hospitalized children dependent on LTMV compared with other children with CCCs. We hypothesized that LTMV-dependent children would have greater resource utilization per child than other children with CCCs. We described the national trends in hospitalizations for LTMV-dependent children for the years 2000 to 2006 in terms of (1): age distributions; (2) primary insurance status; (3) discharge disposition; and (4) inpatient health care utilization, as reflected in length of stay (LOS) and hospital charges.
METHODS
Study Design and Setting
This was a serial cross-sectional analysis of pediatric discharges in 2000, 2003, and 2006 that used the Healthcare Cost and Utilization Project's (HCUP) Kids' Inpatient Database (KID), as compiled by the Agency for Healthcare Research and Quality.18 KID is a nationally representative database that samples 80% of pediatric discharges and 10% of uncomplicated births to increase the power to detect and evaluate rare conditions. Discharges are weighted based on the sampling scheme to permit inferences for a nationally representative population. In 2006, KID contained deidentified information for ∼7.6 million weighted discharges from 3739 hospitals in 38 states. Readmissions are not identified in this data set. HCUP provides additional sampling and weighting details.19 Because of significant changes in data set sampling between 1997 and subsequent years, the present analysis used KID in years 2000, 2003, and 2006.20
Identification of Sample
Hospitalizations for patients 0 to 20 years old at admission were included for each year. Pediatric patients dependent on LTMV represent a heterogeneous group of underlying neurologic, respiratory, and often multiorgan system disorders, linked by a common technology. Therefore, for these analyses, children dependent on LTMV were identified using International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis code v46.1x (dependence on a respirator) rather than a specific illness or organ system diagnosis. This ICD-9-CM definition is not limited to either invasive or noninvasive mechanical support. Before 2004, the diagnosis code v46.1 was used for dependence on a respirator. In 2004, it was stratified into 4 subcategories, including v46.11 (dependence on a respirator). The 2006 analysis was limited to v46.11, because no discharges contained the diagnosis codes v46.12 to v46.14. ICD-9-CM diagnosis codes 518.83 and 518.84 (chronic and acute-on-chronic respiratory failure) were not used because they do not require dependence on mechanical support. Overall, we believe that this case identification strategy improves on those used previously, because it is neither equipment specific nor dependent on a set of specific underlying diagnoses that may not capture all clinical situations in which LTMV was used.
To describe the clinical population captured by the ICD-9-CM diagnosis code v46.1x, the 20 most frequently used diagnosis-related group (DRG) codes for LTMV-dependent discharges in 2006 are delineated in Appendix 1. DRGs were further grouped as a medical versus surgical admission and into disease categories. The rates of discharge in these groups are compared from 2000 to 2006 in Appendix 2.
Discharges characteristics were compared for children dependent on LTMV with those with CCCs in 2006. The presence of at least 1 CCC was defined using ICD-9-CM diagnosis codes in 9 categories of illness, as previously defined.21 Approximately 30% of the LTMV-dependent discharges did not have a corresponding CCC diagnosis code but were included in the CCC group to facilitate comparisons. The limitations of identifying children based on ICD-9-CM–defined CCCs, especially in the presence of technologic dependence, has been discussed previously.1 Proportions of discharges within each CCC category for children dependent on LTMV compared with all CCC-related discharges for 2006 are shown in Appendix 3.
Discharge Variables
The following patient characteristics were used to facilitate comparisons: age at admission, primary insurance type (payer), and average income quartile for the zip code of the patient's residence. Age was grouped into categories based on HCUP-reporting practices: younger than 1 year, 1 to 4 years, 5 to 9 years, 10 to 14 years, and 15 years and older. Primary payers were grouped into public sources (Medicaid and Medicare), private sources, and other types (including self-pay, no charge, and other sources). Additional demographic information (eg, age in days/months, race/ethnicity, secondary payers) were also available in KID but were missing for >20% of cases or otherwise inconsistent across data years, and were therefore not used.
KID contains hospital characteristics, including bed size (small, medium, and large), urban versus rural, teaching status, and census region (Northeast, South, Midwest, and West). Because of significant variation in the type of pediatric facility in the National Association of Children's Hospitals and Related Institutions definition of children's units within a general hospital,19 this variable was dichotomized to include all pediatric facilities and freestanding children's hospitals compared with other hospitals without dedicated pediatric facilities.
Health Care Utilization and Outcome Variables
Discharge-level information such as LOS, source of admission (emergency department or hospital transfer), and discharge disposition were included. Discharge disposition was grouped as death in hospital, routine discharge (ie, without nursing support), transfer to another facility (eg, skilled nursing or long-term care), home health care (eg, home nursing care or hospice), and other (eg, against medical advice, transfer to a short-term hospital, discharge alive/location unknown).
Total charges reflected the total facility fees reported for each discharge record (not including professional fees). Total charges were missing in <5% of discharges. To estimate aggregate charges for various groups that include missing charges, HCUP imputes the missing charges based on the mean total charge for the DRG listed for the hospitalization.20 Although this method is feasible, we determined that total charges as reflective of a single DRG for this population were inadequate. LOS and corresponding charges are often strongly influenced by prolonged periods of inpatient stability and the time necessary to arrange home care services that are not reflected in the DRG code.17 In addition, younger children can have longer LOS due to differences in underlying diagnoses and longer periods of stability judged clinically necessary before home discharge. Therefore, missing total charge values were treated as missing at random and estimated using multiple imputation (a regression technique that estimates the missing value using known variables). Age, LOS, and DRG were included as covariates in the imputation analysis. All charges were converted to 2009 US dollars using the medical consumer price index.22 Multiple imputation of total charges was performed with Stata 10.1 (Stata Corp, College Station, TX) using imputation by chained equations.23
Data Analysis
Statistical comparisons were performed using Stata 10.1. All analyses were weighted by Agency for Healthcare Research and Quality–specified discharge values to obtain nationally representative estimates. Differences in patient characteristics for LTMV discharges versus discharges with at least 1 CCC were assessed using simple regression and χ2 tests.
The changes in inpatient characteristics over time were described in 2000, 2003, and 2006 for children dependent on LTMV. Discharges characteristics for LTMV-dependent children in each year were described as the rates of discharge per 100 000 pediatric nonroutine newborn discharges. The denominator for pediatric nonroutine newborn discharges was the total number of weighted discharges excluding DRG 391 (routine newborn care). Trends in mean and aggregate charges for all LTMV-dependent discharges and between age categories and payers were described. The statistical significance of all time trends was analyzed by assessing P-for-trend across the 3 study years, using variance-weighted regression for categorical and continuous variables.24,25 Statistically significant (P < .05) interaction terms between categorical values and year were retained in the final models. Changes over time in aggregate charges were controlled for by the increases in overall rate of LTMV-dependent discharges, where appropriate.
RESULTS
Hospital Care, 2006
The 2006 KID contains an estimated 4.5 million discharges after excluding routine newborn (DRG 391) discharges. Of these 4.5 million discharges, 7812 (95% confidence interval [CI]: 6615–9010) estimated discharges were for children dependent on LTMV and 769 770 (95% CI: 709 115–830 429) estimated discharges were related to other children with CCCs. This represents 0.17% and 17%, respectively, of pediatric discharges excluding rou-tine newborns. Aggregate inpatient charges were $1.5 billion for children dependent on LTMV and $44 billion for other CCC-related discharges. This represents 1.5% and 44%, respectively, of the ∼$100 billion for the 4.5 million pediatric nonroutine newborn hospitalizations.
Characteristics of discharges for children dependent on LTMV versus other pediatric CCC-related discharges in 2006 are compared in Table 1. There was an approximately threefold longer LOS for children dependent on LTMV. Children dependent on LTMV were slightly younger on average, chiefly because of a higher proportion of children aged 1 to 4 years. Discharges for LTMV-dependent children were more often reimbursed through public programs.
TABLE 1.
Characteristics of LTMV-Dependent Discharges Versus Other Discharges Related to CCCs in 2006
| LTMV Discharges | CCC Discharges | |
|---|---|---|
| Mean age, ya | 6.2 | 6.7 |
| Mean LOS, db | 26.1 | 9.0 |
| Mean charges per dischargeb,c | $189 522 | $57 195 |
| Aggregate chargesb,c | $1.5 billion | $44 billion |
| Age categories, %b | ||
| <1 y | 26.8 | 37.2 |
| 1–4 y | 29.3 | 15.9 |
| 5–9 y | 13.9 | 11.6 |
| 10–14 y | 11.1 | 12.4 |
| ≥15 y | 18.9 | 22.9 |
| Primary payers, %b | ||
| Public | 61.9 | 46.1 |
| Private | 31.3 | 45.4 |
| Other | 6.8 | 8.4 |
| Income quartile of patient's zip code, %a | ||
| $1–37 999 | 30.9 | 28.5 |
| $38 000–46 999 | 25.5 | 24.3 |
| $47 000–61 999 | 22.5 | 24.1 |
| >$62 000 | 21.1 | 23.1 |
| Admission characteristics, %b | ||
| Admitted from the emergency department | 42.1 | 28.2 |
| Transferred from another hospital | 20.8 | 8.7 |
| Transferred from a nonhospital | 3.6 | 1.1 |
| Other sources (routine) | 33.5 | 62.0 |
| Disposition of patient, %b | ||
| Death in hospital | 6.2 | 1.6 |
| Routine discharge | 49.8 | 84.2 |
| Transfer, nonacute facility (eg, long- term care) | 18.4 | 2.3 |
| Home health care | 19.2 | 7.6 |
| Other | 6.4 | 4.3 |
| Hospital characteristics, % | ||
| Urban hospitalb | 98.7 | 95.9 |
| Large bed sized | 59.7 | 60.7 |
| Teaching hospitalb | 89.5 | 78.4 |
| Any type of pediatric facilityb | 81.1 | 60.4 |
Significant, P < .05.
Significant, P < .001.
Charges converted to 2009 dollars using the medical consumer price index.
Not significant.
LTMV discharges were significantly more likely than discharges with other CCCs to have been admitted through the emergency department or been transferred from another hospital. Although routine discharge disposition predominated for CCC-related stays, discharges for LTMV-dependent children were distinctive for fourfold higher inpatient mortality versus other children with a CCC diagnosis, and substantially higher proportions of transfers to long-term care facilities and home health care.
Differences in the hospital characteristics for LTMV-dependent children versus other children with CCCs are also presented in Table 1. Children dependent on LTMV were significantly more likely to use urban hospitals, teaching hospitals, and pediatric facilities. There were no differences in the distribution of the discharges of LTMV-dependent children versus CCC-related discharges by the hospital's census region (data not shown).
Trends in Hospital Care, 2000–2006
Characteristics of discharges for children dependent on LTMV were assessed serially in 2000, 2003, and 2006. The estimated national number of discharges for LTMV-dependent children increased from 5026 in 2000 to 7812 in 2006 (55% increase). Similarly, for LTMV-dependent children, the rate of discharge increased from 113.2 to 173.2 per 100 000 pediatric nonroutine newborn discharges (Table 2).
TABLE 2.
Trends for LTMV-Dependent Discharges From 2000 to 2006
| 2000 | 2003 | 2006 | |
|---|---|---|---|
| LTMV dischargesa | 5026 | 5832 | 7812 |
| Rate of LTMV dischargesa,b | 113.2 | 126.9 | 173.2 |
| Mean LOS, dc | 32.0 | 23.9 | 26.1 |
| Mean charges per dischargec,d | $176 417 | $167 332 | $188 220 |
| Aggregate chargesa,d | $880 million | $980 million | $1.5 billion |
| Age categories (rate)b | |||
| <1 yc | 41.4 | 32.8 | 46.1 |
| 1–4 ya | 24.6 | 36.4 | 50.5 |
| 5–9 ya | 13.5 | 17.4 | 24.0 |
| 10–14 ya | 11.6 | 14.2 | 19.2 |
| ≥15 ya | 21.9 | 25.9 | 32.5 |
| Primary payers (rate)b | |||
| Publica | 58.7 | 72.6 | 107.2 |
| Privatec | 48.3 | 47.0 | 54.1 |
| Othera | 5.8 | 6.9 | 11.8 |
| Disposition of patient (rate)b | |||
| Death in hospitalc | 9.3 | 8.7 | 10.8 |
| Routine dischargee | 56.9 | 68.0 | 86.2 |
| Transfer, nonacute facility (eg, long-term care)a | 17.5 | 20.6 | 31.9 |
| Home health carea | 19.2 | 19.3 | 33.2 |
| Otherc | 10.2 | 9.5 | 11.0 |
Significant change over time, P < .001.
Rates expressed in number of discharges associated with LTMV per 100 000 pediatric nonnewborn discharges.
No significant change over time.
Charges converted to 2009 dollars using Medical Consumer Price Index.
Significant change over time, P < .01.
The increasing number of discharges over time was reflected in an increase in aggregate charges for LTMV-dependent children, from $880 million nationally in 2000 to $1.5 billion in 2006 (70% increase; < .001). When the trend in increased aggregate charges was controlled for, the increase in the rate of discharges for LTMV-dependent children was no longer statistically significant (= .79), suggesting that increasing aggregate charges were chiefly related to the increasing volume of discharges.
Trends in Hospital Utilization According to Patient Age, 2000–2006
Most of the LTMV-dependent discharges (∼55%) each year occurred in children younger than 1 year and between 1 and 4 years old (Table 2). In 2000, the rate of discharge was highest for children younger than 1 year and remained relatively constant over time (time trend, P = .051). In each of the other age categories, from 2000 to 2006 the rate of LTMV discharges increased, with the greatest increase occurring in the 1- to 4-year-old age group.
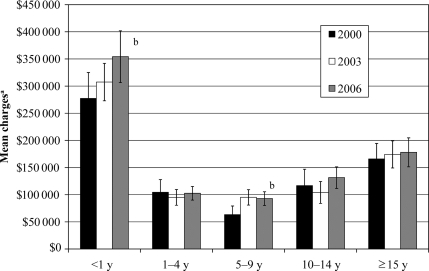
Mean charges by age category in the LTMV population differed significantly from each other (< .001), with the highest mean charges ($278 115 per discharge) in children younger than 1 year (Fig 1). Moreover, there were statistically significant increases in the mean charges for infants younger than 1 year (P = .025) and for children aged 5 to 9 years (P = .009). Mean LOS for children younger than 1 year was longer than other age groups (P < .001), but LOS for each age group did not change over time (P = .15). Aggregate charges increased in each age group. For infants aged younger than 1 year, this is likely due to the increase in mean charges because there is no increase in the rate of discharge. In the other age groups, the increase in aggregate charges was likely due to the increase in rate of discharge, except in the 5- to 9-year-olds, in whom there may be a combined effect. Children aged younger than 1 year continued to have the highest aggregate charges ($740 million in 2006 [∼50% of the aggregate charges for all LTMV-dependent discharges]).
FIGURE 1.
Mean charges according to age category from 2000 to 2006. a Charges corrected to 2009 US$ using the medical consumer price index. b Statistically significant change in mean charges over time, P < .05. Statistically significant differences in mean charges according to each age category, P < .001.
Trends in Primary Payers, 2000–2006
The distribution of reimbursement according to primary payer categories also shifted significantly from 2000 to 2006 for children dependent on LTMV. The rate of discharges reimbursed by public payers (Medicaid and Medicare) increased from 58.7 to 107.2 per 100 000 pediatric nonroutine newborn discharges (83% increase, Table 2), which contrasted sharply with a virtually unchanged rate of discharges reimbursed by private insurers (P = .32). There was a 105% increase in the aggregate charges billed to public insurers from 2000 to 2006 ($420 million to $860 million; P < .001). Private insurers saw a 25% increase in aggregate total charges, from 2000 to 2006 ($400 million to $500 million; P < .001).
Discharge Disposition, 2000–2006
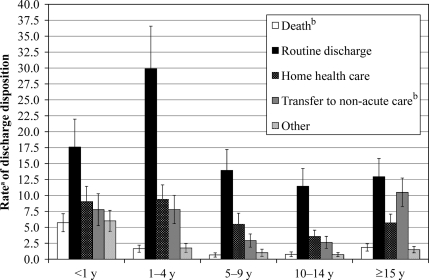
Inpatient care of LTMV-dependent children was additionally complicated by mechanisms of discharge disposition. LTMV-dependent discharges had high rates of in-hospital mortality, long-term care, and home health care. The rate of in-hospital mortality was unchanged during the study period, at ∼10 per 100 000 pediatric nonroutine newborn discharges (P = .32). The increased rates of discharge in the other categories generally reflected proportional increases due to overall LTMV discharge rate (Table 2). When discharge disposition was compared across different age categories, there were significantly higher rates of mortality in infants younger than 1 year and of discharges to other nonacute care facilities (eg, long-term care facilities) for teenagers 15 years of age or older. These differences are presented in Fig 2 for the year 2006.
FIGURE 2.
Rate of discharge disposition according to age category in 2006. a Rate expressed in number of discharges associated with LTMV per 100 000 nonroutine newborn pediatric discharges. b Statistically significant differences in disposition according to age category, P < .05.
DISCUSSION
This is the first study to describe the inpatient characteristics and health care utilization for LTMV-dependent children using a nationally representative sample. Our analysis indicates that discharges for children dependent on LTMV and their inpatient health care expenditures have steadily increased in the past decade. Discharges for children dependent on LTMV also use a disproportionately high amount of health care resources, strikingly higher than other children with CCCs. Such trends are critically important to understand as we anticipate future growth in this group of patients and their health care needs.
Consistent with evidence from previous state-level studies,5–7 this nationally representative sample indicated a 55% increase in the number of discharges from 2000 to 2006. Importantly, this increase in the number of discharges corresponds to a 70% increase in aggregate charges, to $1.5 billion (1.5% of aggregate nonroutine newborn inpatient care charges). This increase in aggregate charges has occurred without significant changes in the inpatient LOS, overall mean charges, and inpatient mortality rate over time; that is, the intensity of inpatient resource utilization has remained relatively flat whereas the sheer number of hospitalizations has increased.
The increasing rate of discharge for LTMV-dependent children, coupled with their long LOS, translates to a substantial increase over time in the number of bed-days for these patients, which often occur in the PICU. This has occurred while overall admissions for children with CCCs account for an increased proportion (41% in 2006) of the delivery of critical care services.26 In the United Kingdom, 12% of PICU beds were occupied with children dependent on LTMV during a winter respiratory season.28 The growth in health care resource utilization by all children with CCCs, and especially those who require LTMV, should inform discussions regarding resource allocation and training for all types of health care providers who care for these children and their families.
Because of the substantial health care needs of children dependent on LTMV, it is not surprising that two thirds of inpatient care is reimbursed through public coverage (particularly Medicaid) that provide support for specific medical disabilities, compared with approximately half for other children with CCCs. Since 2000, there has been an increase in the proportion of all pediatric discharges (including routine newborn care, publicly available from HCUP) charged to public programs, from 36% in 2000% to 45% in 2006.27 This 9 percentage-point increase for all pediatric discharges represents a 25% relative increase (compared with 83% in LTMV-dependent discharges) in the rate of discharges charged to public sources. The increasing overall inpatient charges, the increasing rate at which public payers reimburse these charges, and the significant outpatient resource utilization suggested by this analysis will further burden already strained public payers.
Importantly, among the discharges associated with LTMV, total health care utilization is affected strongly, and differently, by age. All ages, except for children younger than 1 year, have had significant increases in the rate of discharge from 2000 to 2006. Meanwhile, this youngest age group has consistently constituted a substantial proportion of LTMV-dependent discharges. Chronic respiratory failure in infancy likely continues to be a mix of rare central nervous system and neuromuscular diseases, premature lung disease, and complex congenital malformations.9,29 This age group has the longest hospital stays and the highest mean hospital charges, which account for ∼50% of the overall aggregate charges for LTMV-dependent children.
This analysis has several limitations that must be considered when interpreting these results. KID is a deidentified discharge data source limited to what is coded in administrative data and cannot be used to identify specific patients; therefore, readmission cannot be determined. We have identified discharges associated with LTMV using the ICD-9-CM code v46.1x (dependence on a respirator), which may underestimate the total number of discharges associated with LTMV because it is a nonreimbursable v-code and may either be omitted with variation in coding practices or truncated during HCUP's data collection process. We have also chosen not to exclude discharges associated with transfer between acute care hospitals. This strategy may potentially duplicate the number of discharges for a particular patient but is a more complete representation of total inpatient health care utilization at the national level. In addition, we felt that it was important to describe the number of transfers in this population, as they are a significant part of the care of technologically dependent children.
CONCLUSIONS
LTMV-dependent children use a disproportionate share of inpatient health care resources compared with other pediatric discharges and even compared with discharges related to other CCCs. In recent years, there has been significant growth in the number of discharges for children dependent on LTMV, especially among children aged 1 to 4 years, with concurrent growth in health care expenditures for all LTMV-dependent children. The inpatient charges are disproportionately and progressively reimbursed by public payers over time. This study provides baseline inpatient health care utilization trends at the national level that may be used as the basis for additional examination of care trends for the LTMV population, especially young children and infants.
ACKNOWLEDGMENT
Dr Benneyworth was supported by a training grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (T32 HD07534).
APPENDIX 1.
Twenty Most Frequent DRG Codes for LTMV-Dependent Discharges in 2006 (Total Percentage Described: 67.18%)
| Code | DRG Name (Version 24) | LTMV Discharges, % | 95% CI |
|---|---|---|---|
| 565 | Respiratory system diagnosis with ventilatory support >96 h | 16.0 | 14.1–17.9 |
| 566 | Respiratory system diagnosis with ventilatory support <96 h | 10.3 | 9.2–11.4 |
| 541 | Extracorporeal membrane oxygenation or tracheostomy with mechanical ventilation >96 h for non-head and neck diagnoses with major operating room procedure | 8.3 | 6.9–9.7 |
| 542 | Tracheostomy with mechanical ventilation >96 h for non-head and neck diagnoses without major operating room procedure | 4.9 | 4.2–5.5 |
| 386 | Extreme immaturity or respiratory distress syndrome, neonate | 2.6 | 1.8–3.5 |
| 26 | Seizure and headache, age 0–17 y | 2.5 | 2.0–3.0 |
| 385 | Neonates, died or transferred to another acute care facility | 2.2 | 1.7–2.8 |
| 91 | Simple pneumonia and pleurisy, age 0–17 y | 2.2 | 1.6–2.8 |
| 298 | Nutritional and miscellaneous metabolic disorders, age 0–17 y | 2.0 | 1.6–2.4 |
| 34 | Other diseases of the nervous system with complications | 1.8 | 1.3–2.2 |
| 98 | Bronchitis and asthma, age 0–17 y | 1.8 | 1.2–2.4 |
| 3 | Craniotomy, age 0–17 y | 1.7 | 1.2–2.1 |
| 101 | Other respiratory system diagnosis with complications | 1.6 | 1.1–2.1 |
| 76 | Other respiratory system operating room procedure with complications | 1.6 | 1.1–2.1 |
| 468 | Extensive operating room procedure unrelated to principal diagnosis | 1.5 | 1.1–1.9 |
| 190 | Other digestive system diagnosis, age 0–17 Y | 1.4 | 1.0–1.8 |
| 417 | Septicemia, age 0–17 y | 1.3 | 0.9–1.7 |
| 144 | Other circulatory system diagnosis with Complications | 1.2 | 0.9–1.6 |
| 184 | Esophagitis, gastrointestinal, and miscellaneous digestive tract disorders, age 0–17 y | 1.2 | 0.9–1.6 |
| 70 | Otitis media and upper respiratory tract infection, age 0–17 y | 1.1 | 0.8–1.4 |
APPENDIX 2.
Trends in DRG Groups for LTMV-Dependent Discharges, 2000–2006
| 2000 | 2003 | 2006 | |
|---|---|---|---|
| Rate of medical dischargea,b | 76.8 | 87.5 | 119.3 |
| Rate of surgical dischargesa,b | 36.4 | 39.4 | 53.9 |
| DRG group (rate)a | |||
| Respiratory diseaseb | 47.0 | 56.5 | 77.5 |
| Related to prematurityc | 16.2 | 9.1 | 10.0 |
| Neurologic diseaseb | 7.6 | 9.7 | 14.1 |
| Respiratory tract infectionsc | 7.1 | 9.1 | 10.4 |
| Gastrointestinal/renalb | 6.9 | 9.7 | 12.3 |
| Cardiovascular diseasec | 6.2 | 5.7 | 8.3 |
| Infectious diseaseb | 5.6 | 7.1 | 11.8 |
| Orthopedicd | 2.4 | 2.8 | 4.8 |
| Traumac | 1.9 | 2.1 | 2.9 |
| Malignancyc | 1.2 | 1.0 | 1.3 |
| Otherb | 11.2 | 14.2 | 19.6 |
Rates expressed in number of discharges associated with LTMV per 100 000 pediatric nonnewborn discharges.
Significant change over time, P < .001.
No significant change over time.
Significant change over time, P < .01.
APPENDIX 3.
Proportion Differences in Each CCC Group in 2006
| Condition Group | LTMV Discharges, % (95% CI) | CCC Discharges, % (95% CI) |
|---|---|---|
| Neurologica | 36.8 (34.2–39.4) | 20.2 (19.5–21.0) |
| Respiratorya | 22.6 (20.0–25.2) | 8.1 (7.7–8.5) |
| Cardiovasculara | 19.6 (17.7–21.5) | 28.5 (27.7–29.4) |
| Genetica | 19.6 (17.9–21.2) | 13.7 (13.4–14.1) |
| Metabolicb | 4.8 (3.7–5.9) | 6.1 (5.8–6.3) |
| Malignancya | 3.1 (2.4–3.8) | 19.5 (18.4–20.6) |
| Hematologic/immunologica | 2.7 (1.9–3.4) | 9.2 (8.6–9.8) |
| Renala | 2.1 (1.6–2.7) | 6.3 (6.1–6.5) |
| Gastrointestinala | 2.0 (1.5–2.5) | 5.2 (5–5.4) |
| ≥2 CCC diagnosesa | 30.1 (27.4–32.9) | 14.6 (14.1–15.1) |
| No CCC diagnosis | 24.7 (22.3–27.0) | — |
Significant, P < .001.
Not significant.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
Funded by the National Institutes of Health (NIH).
- CCC
- complex chronic condition
- LTMV
- long-term mechanical ventilation
- LOS
- length of stay
- HCUP
- Healthcare Cost and Utilization Project
- KID
- Kids' Inpatient Database
- ICD-9-CM
- International Classification of Diseases, Ninth Revision, Clinical Modification
- DRG
- diagnosis-related group
- CI
- confidence interval
REFERENCES
- 1. Simon TD, Berry J, Feudtner C, et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126(4):647–655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. DeWitt PK, Jansen MT, Ward SL, Keens TG. Obstacles to discharge of ventilator-assisted children from the hospital to home. Chest. 1993;103(5):1560–1565 [DOI] [PubMed] [Google Scholar]
- 3. Edwards EA, O'Toole M, Wallis C. Sending children home on tracheostomy dependent ventilation: pitfalls and outcomes. Arch Dis Child. 2004;89(3):251–255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. O'Brien JE, Dumas HM, Haley SM, et al. Clinical findings and resource use of infants and toddlers dependent on oxygen and ventilators. Clin Pediatr (Phil). 2002;41(3):155–162 [DOI] [PubMed] [Google Scholar]
- 5. Graham RJ, Fleegler EW, Robinson WM. Chronic ventilator need in the community: a 2005 pediatric census of Massachusetts. Pediatrics. 2007;119(6). Available at: www.pediatrics.org/cgi/content/full/119/6/e1280 [DOI] [PubMed] [Google Scholar]
- 6. Gowans M, Keenan HT, Bratton SL. The population prevalence of children receiving invasive home ventilation in Utah. Pediatr Pulmonol. 2007;42(3):231–236 [DOI] [PubMed] [Google Scholar]
- 7. Downes JJ, Boroughs DS, Dougherty J, Parra M. A statewide program for home care of children with chronic respiratory failure. Caring. 2007;26(9):16–18, 20, 22–23 passim [PubMed] [Google Scholar]
- 8. Frates RC, Jr, Splaingard ML, Smith EO, Harrison GM. Outcome of home mechanical ventilation in children. J Pediatrics. 1985;106(5):850–856 [DOI] [PubMed] [Google Scholar]
- 9. Schreiner MS, Downes JJ, Kettrick RG, Ise C, Voit R. Chronic respiratory failure in infants with prolonged ventilator dependency. JAMA. 1987;258(23):3398–3404 [PubMed] [Google Scholar]
- 10. Canlas-Yamsuan M, Sanchez I, Kesselman M, Chernick V. Morbidity and mortality patterns of ventilator-dependent children in a home care program. Clin Pediatr (Phil). 1993;32(12):706–713 [DOI] [PubMed] [Google Scholar]
- 11. Nelson VS, Carroll JC, Hurvitz EA, Dean JM. Home mechanical ventilation of children. Dev Med Child Neurol. 1996;38(8):704–715 [DOI] [PubMed] [Google Scholar]
- 12. Appierto L, Cori M, Bianchi R, et al. Home care for chronic respiratory failure in children: 15 years experience. Paediatr Anaesth. 2002;12(4):345–350 [DOI] [PubMed] [Google Scholar]
- 13. Graf JM, Montagnino BA, Hueckel R, McPherson ML. Pediatric tracheostomies: a recent experience from one academic center. Pediatr Crit Care Med. 2008;9(1):96–100 [DOI] [PubMed] [Google Scholar]
- 14. Spentzas T, Auth M, Hess P, Minarik M, Storgion S, Stidham G. Natural course following pediatric tracheostomy. J Intensive Care Med. 2010;25(1):39–45 [DOI] [PubMed] [Google Scholar]
- 15. Fraser J, Henrichsen T, Mok Q, Tasker RC. Prolonged mechanical ventilation as a consequence of acute illness. Arch Dis Child. 1998;78(3):253–256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dhillon JS, Frewen TC, Singh NC, Speechley KN. Chronic mechanical ventilation-dependent children in Canada. Paediatri Child Health. 1996;1(2):111–116 [Google Scholar]
- 17. Jardine E, O'Toole M, Paton JY, Wallis C. Current status of long term ventilation of children in the United Kingdom: questionnaire survey. BMJ. 1999;318(7179):295–299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. HCUP Kids' Inpatient Database (KID) Healthcare Cost and Utilization Project (HCUP). 2000, 2003 and 2006. Rockville, MD: Agency for Healthcare Research and Quality; Available at: www.hcup-us.ahrq.gov/nisoverview.jsp Accessed November 1, 2009 [Google Scholar]
- 19. Introduction to the KID: 2006. In: HCUP KID Related Reports. Rockville, MD: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project (HCUP); 2008 [Google Scholar]
- 20. Using the KIDS' Inpatient Database (KID) to Estimate Trends, Report #2007–02. In: HCUP Methods Series. Rockville, MD: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project (HCUP); 2009 [Google Scholar]
- 21. Feudtner C, Hays RM, Haynes G, Geyer JR, Neff JM, Koepsell TD. Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics. 2001;107(6). Available at: www.pediatrics.org/cgi/content/full/107/6/e99 [DOI] [PubMed] [Google Scholar]
- 22. Bureau of Labor Statistics Consumer Price Index, 2010. Available at: www.bls.gov/cpi/ Accessed November 5, 2010
- 23. Royston P. Multiple imputation of missing values: further update of ice, with an emphasis an categorical variables. Stata Journal. 2009;9(3):466–477 [Google Scholar]
- 24. Lee JM, Okumura MJ, Freed GL, Menon RK, Davis MM. Trends in hospitalizations for diabetes among children and young adults: United States, 1993–2004. Diabetes Care. 2007;30(12):3035–3039 [DOI] [PubMed] [Google Scholar]
- 25. Weisberg S. Applied Linear Regression. Hoboken, NJ: Wiley-Interscience; 2005 [Google Scholar]
- 26. Odetola FO, Gebremariam A, Davis MM. Comorbid illnesses among critically ill hospitalized children: impact on hospital resource use and mortality, 1997–2006. Pediatr Crit Care Med. 2010;11(4):457–463 [DOI] [PubMed] [Google Scholar]
- 27. HCUPnet Healthcare Cost and Utilization Project (HCUP). 2000–2006. Agency for Healthcare Research and Quality, Rockville, MD: Available at: http://hcupnet.ahrq.gov Accessed May 5, 2010 [PubMed] [Google Scholar]
- 28. Fraser J, Mok Q, Tasker R. Survey of occupancy of paediatric intensive care units by children who are dependent on ventilators. BMJ. 1997;315(7104):347–348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Berry JG, Graham DA, Graham RJ, et al. Predictors of clinical outcomes and hospital resource use of children after tracheotomy. Pediatrics. 2009;124(2):563–572 [DOI] [PMC free article] [PubMed] [Google Scholar]