Abstract
Background
Unexplained symptoms are associated with depression and anxiety. This association is largely based on cross-sectional research of symptoms experienced by patients but not of symptoms presented to the GP.
Aim
To investigate whether unexplained symptoms as presented to the GP predict mental disorders.
Design and setting
Cross-sectional and longitudinal analysis of data from a practice-based research network of GPs, the Transition Project, in the Netherlands.
Method
All data about contacts between patients (n = 16 000) and GPs (n = 10) from 1997 to 2008 were used. The relation between unexplained symptoms episodes and depression and anxiety was calculated and compared with the relation between somatic symptoms episodes and depression and anxiety. The predictive value of unexplained symptoms episodes for depression and anxiety was determined.
Results
All somatoform symptom episodes and most somatic symptom episodes are significantly associated with depression and anxiety. Presenting two or more symptoms episodes gives a five-fold increase of the risk of anxiety or depression. The positive predictive value of all symptom episodes for anxiety and depression was very limited. There was little difference between somatoform and somatic symptom episodes with respect to the prediction of anxiety or depression.
Conclusion
Somatoform symptom episodes have a statistically significant relation with anxiety and depression. The same was true for somatic symptom episodes. Despite the significant odds ratios, the predictive value of symptom episodes for anxiety and depression is low. Consequently, screening for these mental health problems in patients presenting unexplained symptom episodes is not justified in primary care.
Keywords: anxiety; depression; mental health; primary care; somatisation; symptoms, unexplained
INTRODUCTION
People experience many symptoms, but they only present a small minority of about 10% to a physician: the so-called ‘iceberg phenomenon’.1,2 Many (about one-third to three-quarters) of the symptoms presented to a physician are not explained by organic pathology.3,4 These symptoms remain ‘medically unexplained’. Patients presenting with unexplained symptoms are classified in a spectrum ranging from a single unexplained symptom of short duration to functional syndromes (such as fibromyalgia and chronic fatigue syndrome) to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) diagnosis of undifferentiated somatoform disorder or even somatisation disorder.
The relation between unexplained symptoms on the one hand and mental health problems on the other has been addressed in several studies in primary care. Results of these studies are not congruent. Jackson and Passamonti showed that ‘the majority of patients whose symptom remained unexplained did not have underlying mood, anxiety, or somatoform disorder’.5 Other research has demonstrated that (1) patients with medically unexplained symptoms had higher scores for depression or anxiety compared with patients with medically explained symptoms;6 (2) the more symptoms patients have, the higher the prevalence of depression or anxiety disorder;7 and (3) unexplained symptoms are frequently accompanied by psychiatric disorders.8 For conditions at the severe side of the somatoform spectrum, de Waal et al showed that patients with somatoform disorders in primary care were 3.3 times more likely to be diagnosed with a depressive or anxiety disorder.9 Research on US primary care attendees also demonstrated a considerable overlap (more than 50% of the cases) of depression, anxiety, and somatisation.10 Based on these results, some researchers advocate screening for depression and anxiety in patients with unexplained symptoms.11
Many GPs perceive medically unexplained symptoms as the presentation of psychological distress,12 or as a manifestation of personality problems or psychiatric illness.13 However, patients often do not agree with their physicians about the (psychological) aetiology of the unexplained symptoms.14 Consequently, the question remains whether the GP should enquire about mental health problems in patients who present unexplained symptoms. The Dutch multidisciplinary guideline for somatoform complaints and disorders advocates diagnostic enquiry for anxiety and depressive disorder as the next step following history taking and physical examination.15
In most studies, the assessment of experienced symptoms has been performed with self-administered questionnaires about all experienced symptoms before the patient entered the consultation room. It remains unknown which symptom(s) the patient presented to the doctor. In the light of the iceberg phenomenon, this might not be adequate as it does not deal with the difference between experienced and presented symptoms.
How this fits in
Unexplained symptoms are associated with depression and anxiety. Therefore, screening patients with unexplained symptoms for depression and anxiety has been advocated. However, the predictive value of unexplained symptoms for anxiety and depression is low. Consequently, screening for these mental health problems in patients presenting unexplained symptom episodes is not justified in primary care.
Therefore, the aim of this study is to investigate whether unexplained symptoms as presented to the GP predict mental disorders. The research questions are:
are mental health problems associated with unexplained symptoms that are presented to the GP?
how often are unexplained symptoms episodes followed by a mental health problem?
METHOD
Data source
Data generated by a practice-based research network, the Transition Project, were analysed.16 The project currently consists of 10 Dutch GPs who routinely code each episode of care according to the International Classification of Primary Care (ICPC) in an episode structure.17,18 An episode of care is defined as ‘a health problem of an individual from the first encounter until the completion of the last encounter for it with a health care provider’. The structure of the ICPC is based on the description of episodes of care. Within this ongoing project, all contacts between GPs and patients have been registered since 1985. An episode of care is defined as ‘a health problem in an individual from the first encounter until the completion of the last encounter for it with a healthcare provider’.18 For all episodes of care, the GPs register the patient’s reason for encounter (RFE), the physician’s diagnosis (episode title), and the physician’s intervention. Also, for each episode of care, GPs indicate its status: ‘new’ (start) or ‘old’ (follow-up). The RFE should be recognised by the patient as an acceptable description of the request for care presented by the patient. The RFE, all interventions, and the diagnostic labels for each encounter are classified with the ICPC (Figure 1).19 The episode title (the diagnosis) could be modified, for example when fatigue (RFE) turns out to be caused by a iron deficiency anemia (episode title). Medically unexplained symptoms, or rather symptom episodes, are very frequently encountered in the Transition Project: about one-third (36.7%) of the symptom presentations remain coded as a symptom.20 When the GP does not find a cause for a presented symptom, the symptom is classified as a symptom diagnosis according to the rules of the ICPC (Box 1).
Figure 1.
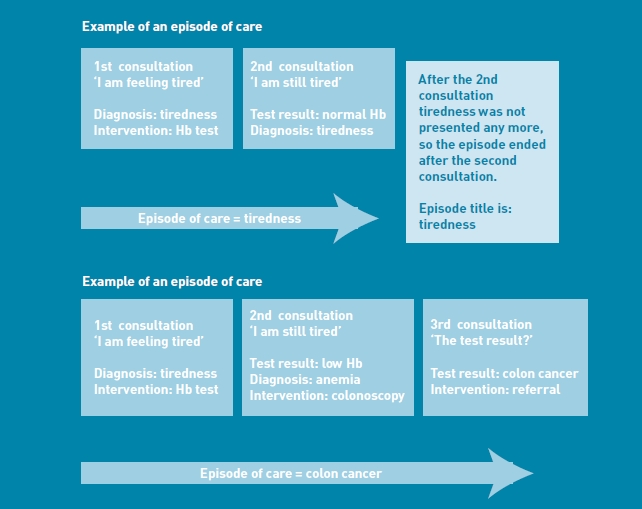
Examples of the relation between consultation and episode of care. Episode title is the name (physician’s diagnosis) given to the episode of care. Hb = haemoglobin.
Box 1.
Concepts in the Transition Project
Reason for encounter
The primary care provider asks for the reason for encounter (RFE) and quotes this as stated by the patient without making any judgments as to the correctness or accuracy of that reason. The RFE should be understood and agreed on between the patient and the provider and should be recognised by the patient as an acceptable description. A patient can have more than one RFE.
Episode title (physician’s diagnosis)
After history taking and physical examination, the physician makes a diagnosis. The diagnosis is the physician’s point of view. Coding health problems should be at the highest level of diagnostic refinement for which the user can be confident, and which meets the inclusion criteria for that category. The diagnostic labels can be on a symptom level or on a disease level.
Episode of care (see Figure 1)
The full spectrum of problems (including organic, psychological, and social) managed by the provider are recorded in the form of episodes of care. The definition of an episode of care is a health problem or disease from its first presentation to a healthcare provider until the completion of the last encounter for that same health problem. So, an episode of care has a RFE, mainly defined by the patient, and an episode title, mainly defined by the physician. If the episode consists of three contacts, then the episode title (for all three contacts in that episode) is the diagnostic label at the end of the episode. The diagnostic labels in this study are labels attributed at the end of the episode. Changes in the diagnostic label during the episode are relatively infrequent, especially in symptom episodes (episodes of care in which the highest classifiable code is a symptom, not a disease).
Example
When the physician codes the episode of care as a symptom episode, this does not mean that the patient had a complaint about only one symptom within this episode. In a patient with the RFE ‘tiredness’, the physician takes the patient’s history and examines the patient. During history taking the patient appears also to suffer from dizziness, trembling, and fatigued legs. The physician judges these complaints to belong to each other and chooses to label that episode with the episode title ‘tiredness’.
The reliability of the registration is high, as the participating GPs use well-defined diagnostic criteria.21 Moreover, the electronic system warns in a case of error and inconsistency.
Population
Between 1997 and 2008 the participating GPs had on average 16 000 enlisted patients. The registration period for the enlisted patients ranged from 1 to 11 years. Encounters with all patients aged 15 years and older were included in this study.
Procedure
For all analyses, two groups of symptoms were compared: first, symptoms generally seen as part of the ‘somatoform construct’, and second, symptoms mostly explained by somatic causes.
Unexplained symptoms
Unexplained symptoms are symptoms generally known as symptoms infrequently caused by organic disease. The following 13 unexplained symptoms, which are frequently presented to the GP, were examined: chest symptoms (L04), shortness of breath (R02), palpitations (K04), abdominal pain (D01), nausea (D09), constipation D12), headache (N01), muscle pain (L18), low back complaints (L02), fainting (A06), dizziness (N17), disturbances of sleep P06), and tiredness (A04). These symptoms constitute the Patient Health Questionnaire (PHQ-15), a scale specifically developed for the detection of somatoform disorders in primary care.22 From the original 15 symptoms in this questionnaire two symptoms were left out, as these were only weakly associated with somatoform disorders (menstrual problems, sexual pain/problems).22
Somatic symptoms
Somatic symptoms are symptoms generally known as symptoms that are commonly caused by organic disease. For both research questions, a control group of symptoms that are mostly of somatic origin was used: lymph gland enlargement (B02), localised abdominal pain (D06), diarrhoea (D11), red eye (F02), swollen ankles (K07), shoulder symptoms (L08), hand/finger symptoms (L12), hip symptoms (L13), tingling fingers/toes/feet (N05), cough (R05), throat symptoms (R21), pruritus (S02), and urinary frequency (U02). Generally, these symptoms are not considered to be related with mental health problems.
Mental health problems
The research also studied how often the 13 unexplained symptoms and the somatic symptoms predicted mental health problems (that is, anxiety disorder [P74] and depressive disorder [P76]). The definitions according to the ICPC criteria are for depression: fundamental disturbance in affect and mood towards depression; mood, energy, and activity are simultaneously lowered, together with an impaired capacity for enjoyment, interest, and concentration; sleep and appetite are usually disturbed; and self-esteem and confidence are decreased. The diagnosis includes depressive neurosis/psychosis, mixed anxiety and depression, reactive depression, and puerperal or postnatal depression. Acute stress reactions are excluded.
For anxiety, the ICPC criteria are: clinically significant anxiety that is not restricted to any particular contextual situation; and it manifests as a panic disorder (recurrent attacks of severe anxiety not restricted to any particular situation, with/without physical symptoms) or as a disorder in which generalised and persistent anxiety, not related to any particular situation, occurs with variable physical symptoms. Anxiety, neurosis, and panic disorder are included, and anxiety with depression (classified as depression) and anxiety not otherwise specified (classified as symptom: feeling anxious/nervous/tense) are excluded.
Analysis
The unit of analysis was the episode title (the diagnosis). The dependent variables were the incidence and prevalence of anxiety (P74) and depression (P76). ‘Encounter-based’ incidence/prevalence rates and ‘total’ incidence/prevalence rates are distinguished. Encounter-based rates are based on diagnoses realised in face-to-face contacts between the patient and physician. Total rates include encounter-based rates and rates of diagnoses that result from specialist letters and telephone consultations for medication. Encounter-based rates were chosen for this research, as the study was primarily interested in the predictive values of symptoms presented in consultations.
Two different views on the analysis were used: cross-sectional and prospective. The period of 1997 to 2008 was analysed in 1-year and 4-year time frames. There were no significant differences between these time frames. One-year data from 2007 are presented and 4-year data from 2004 to 2008. Differences in rates were examined with c2 tests. For the calculation of odds ratios (ORs), logistic regression adjusted for age and sex was used; P values <0.05 were considered statistically significant. In all analyses, ORs for somatoform and somatic symptoms were performed.
A multilevel analysis with between-doctor variation as a variable was not performed because of the low effect of of this source of variation found in earlier research.23
Cross-sectional analyses
Within time frames of 1 year, the database was examined, for each patient, for the occurrence of a mental health problem in a given year. If this patient had a mental problem during this year, the database was examined for the occurrence of the predefined somatoform and somatic symptoms. The procedure was repeated for each year between 1997 and 2008. The ORs (with 95% confidence intervals) were calculated for the chance that a patient with a mental health problem (that is, anxiety disorder or depressive disorder) had presented with one of 13 selected symptom episodes or one of the 13 somatic symptom episodes during that year. Furthermore, the relation between mental health episodes and the number of symptom episodes was analysed, also with ORs. Within a time frame of 4 years, the relation of the duration of symptom episodes and mental health problems was analysed: ORs were calculated for the association between mental health problems and short (<3months) or long (>3months) symptom episodes. Patients had to be registered in the practice for at least 2 years. For all cross-sectional analyses, patients with the somatoform symptom episodes and the somatic symptom episodes were compared. From each patient, only one episode has been included in the analyses, except for the analyses with 1-year time frames (re-analysis with patients counted only once did not show relevant differences; data not shown).
Prospective analyses
The positive predictive value of a symptom diagnosis for a new mental health problem in a period of 3 months after the symptom diagnosis was calculated.24,25
RESULTS
Between 1997 and 2008 there were 419 056 family-physician–patient face-to-face encounters with 10 GPs in about 16 000 enlisted patients from patients aged ≥15 years.
The year prevalence of the ‘unexplained’ symptom episodes ranged from 0.4% (abdominal pain) to 4.8% (low back pain); the total year prevalence of these symptom episodes was 23.1%. The year prevalence of the ‘somatic’ symptom episodes varied between 0.2% and 2.9% (Table 1). The encounter-based year prevalence of anxiety and depressive disorder was 5.8 per 1000 patients per year for anxiety disorder and 22.2 for depressive disorder. The registered total prevalence was respectively 11.9 per 1000 patients per year for anxiety disorder and 45.8 for depressive disorder.
Table 1.
Numbers of episodes 1997–2008 and 1-year prevalence percentages of ‘unexplained’ and ‘somatic’ symptoms
| Unexplained symptoms |
Somatic symptoms |
||||
|---|---|---|---|---|---|
| Number of episodes between 1997 and 2008 | 1-year prevalence (%) | Number of episodes between 1997 and 2008 | 1-year prevalence | ||
| Tiredness | 5179 | 3.8 | Lymph gland enlargement | 571 | 0.4 |
| Fainting | 939 | 0.7 | Localised abdominal pain | 2888 | 2.1 |
| Abdominal pain | 582 | 0.4 | Diarrhoea | 865 | 0.6 |
| Nausea | 681 | 0.5 | Red eye | 350 | 0.3 |
| Constipation | 2741 | 2.0 | Swollen ankles | 1524 | 1.1 |
| Palpitations | 1288 | 0.9 | Shoulder symptoms | 2397 | 1.7 |
| Low back complaint | 6625 | 4.8 | Hand/finger symptoms | 1480 | 1.1 |
| Chest symptoms | 3367 | 2.5 | Hip symptoms | 1164 | 0.9 |
| Muscle pain | 1358 | 1.0 | Tingling fingers/toes/feet | 335 | 0.2 |
| Headache | 2353 | 1.7 | Cough | 3998 | 2.9 |
| Dizziness | 2035 | 1.5 | Throat symptoms | 2294 | 1.7 |
| Disturbances of sleep | 3661 | 2.7 | Pruritus | 1378 | 1.0 |
| Shortness of breath | 1008 | 0.7 | Urinary frequency | 856 | 0.6 |
| Total | 31 817 | 23.1 | Total | 20100 | 14.6 |
Results of cross-sectional analyses
All but three symptom episodes, regardless of whether somatoform or somatic, had significant relations with mental health episodes. Somatoform symptom episodes showed slightly higher associations with anxiety disorder and depressive disorder in comparison with somatic symptoms. The symptom episodes nausea, constipation, sleep disturbances, and shortness of breath had ORs ≥3 for depressive disorder. Generalised abdominal pain, nausea, palpitations, and muscle pain had ORs ≥3 for anxiety disorder (Table 2). Ten out of 13 somatic symptom episodes showed statistically significant associations for anxiety disorder or depressive disorder. Only two ‘somatic’ symptom episodes — swollen ankles and diarrhoea — had an OR ≥3 for depressive disorder (Table 3).
Table 2.
Cross-sectional analysis of data with a time frame of 1 year: association of unexplained symptoms with anxiety disorder and depressive disorder
| Unexplained symptoms | Anxiety disorder | Depressive disorder | ||
|---|---|---|---|---|
| Odds ratio | 95% CI | Odds ratio | 95% CI | |
| Tiredness | 1.85 | 1.53 to 2.23 | 2.85 | 2.61 to 3.12 |
| Fainting | 2.44 | 1.69 to 3.52 | 2.16 | 1.75 to 2.68 |
| Abdominal pain | 4.49 | 3.20 to 6.30 | 1.99 | 1.52 to 2.61 |
| Nausea | 3.08 | 2.23 to 4.26 | 4.24 | 3.60 to 5.00 |
| Constipation | 1.97 | 1.63 to 2.38 | 3.79 | 3.49 to 4.12 |
| Palpitations | 4.7 | 3.74 to 5.89 | 2.49 | 2.11 to 2.94 |
| Low back complaint | 1.72 | 1.47 to 2.02 | 1.7 | 1.56 to 1.86 |
| Chest symptoms | 2.79 | 2.29 to 3.39 | 1.83 | 1.61 to 2.08 |
| Muscle pain | 5.09 | 4.11 to 6.31 | 2.88 | 2.47 to 3.35 |
| Headache | 2.95 | 2.41 to 3.61 | 2.49 | 2.21 to 2.81 |
| Dizziness | 2.62 | 2.07 to 3.31 | 2.25 | 1.96 to 2.59 |
| Disturbances of sleep | 2.55 | 2.23 to 2.92 | 4.08 | 3.82 to 4.36 |
| Shortness of breath | 2.13 | 1.48 to 3.07 | 3.15 | 2.64 to 3.75 |
Table 3.
Cross-sectional analysis with a time frame of 1 year: association of somatic symptoms with anxiety and depressive disorder
| Somatic symptoms | Anxiety disorder | Depressive disorder | ||
|---|---|---|---|---|
| Odds ratio | 95% CI | Odds ratio | 95% CI | |
| Lymph gland enlargement | 2.59 | 1.62 to 4.15 | 0.69 | 0.43 to 1.11 |
| Localised abdominal pain | 1.68 | 1.30 to 2.17 | 2.03 | 1.79 to 2.32 |
| Diarrhoea | 2.66 | 1.98 to 3.59 | 3.02 | 2.58 to 3.55 |
| Red eye | 1.25 | 0.59 to 2.64 | 1.47 | 1.01 to 2.14 |
| Swollen ankles | 1.65 | 1.23 to 2.22 | 3.05 | 2.68 to 3.47 |
| Shoulder symptoms | 1.59 | 1.20 to 2.11 | 1.6 | 1.37 to 1.86 |
| Hand/finger symptoms | 1.94 | 1.39 to 2.71 | 1.84 | 1.53 to 2.22 |
| Hip symptoms | 0.92 | 0.55 to 1.54 | 2.06 | 1.70 to 2.51 |
| Tingling fingers/toes/feet | 2.65 | 1.49 to 4.72 | 2.01 | 1.40 to 2.88 |
| Cough | 1.47 | 1.21 to 1.80 | 1.84 | 1.66 to 2.04 |
| Throat symptoms | 1.56 | 1.17 to 2.09 | 1.56 | 1.34 to 1.83 |
| Pruritus | 2.35 | 1.80 to 3.09 | 2.43 | 2.09 to 2.82 |
| Urinary frequency | 2.42 | 1.66 to 3.51 | 2.47 | 2.01 to 3.03 |
In comparison with short episodes, longer episodes of two unexplained symptoms (dizziness, sleep disturbances) and two somatic symptoms (throat symptoms and swollen ankles) had a statistically significant relation with the occurrence of anxiety or depressive disorder. Patients with these symptom episodes more often have diagnoses of new depression or anxiety. In all other symptom episodes there is no difference in the occurrence of these mental health problems between short and long episodes (Table 4).
Table 4.
Cross-sectional analysis in a time frame of 4 years (2004–2008): relation of duration of episodes and the presence of a mental health episode
| Episodes | Number of short episodes | Number of long episodes | Number of episodes with depression or anxiety | Odds ratio (95% CI) |
|---|---|---|---|---|
| Somatoform | ||||
| Tiredness | 881 | 119 | 116 | 0.711 (0.41 to 1.23) |
| Fainting | 238 | 19 | 25 | 0.892 (0.19 to 4.23) |
| Abdominal pain | 116 | 9 | 9 | 0.592 (0.06 to 5.48) |
| Nausea | 201 | 17 | 35 | 0.604 (0.18 to 2.00) |
| Constipation | 465 | 192 | 62 | 0.736 (0.42 to 1.30 |
| Palpitations | 267 | 58 | 33 | 0.970 (0.38 to 2.48) |
| Low back complaint | 1179 | 254 | 118 | 0.824 (0.51 to 1.32) |
| Chest symptoms | 735 | 54 | 50 | 1.168 (0.35 to 3.90) |
| Muscle pain | 302 | 49 | 35 | 0.652 (0.25 to 1.71) |
| Headache | 440 | 75 | 64 | 0.528 (0.27 to 1.01) |
| Dizziness | 448 | 60 | 32 | 0.357 (0.14 to 0.90) |
| Disturbances of sleep | 447 | 205 | 81 | 0.560 (0.34 to 0.91) |
| Shortness of breath | 236 | 16 | 33 | Too few long episodes |
| Somatic | ||||
| Lymph gland enlargement | 129 | 7 | 10 | Too few long episodes |
| Localised abdominal pain | 634 | 80 | 71 | 0.991 (0.46 to 2.16) |
| Diarrhoea | 290 | 32 | 28 | 0.713 (0.23 to 2.23) |
| Red eye | 101 | 2 | 9 | Too few long episodes |
| Swollen ankles | 218 | 90 | 22 | 0.328 (0.13 to 0.81) |
| Shoulder symptoms | 440 | 91 | 37 | 1.404 (0.53 to 3.74) |
| Hand/finger symptoms | 362 | 52 | 35 | 0.565 (0.23 to 1.38) |
| Hip symptoms | 281 | 34 | 27 | 0.879 (0.25 to 3.14) |
| Tingling fingers/toes/feet | 93 | 6 | 11 | 0.215 (0.03 to 1.44) |
| Cough | 949 | 107 | 112 | 0.690 (0.38 to 1.24) |
| Throat symptoms | 488 | 41 | 44 | 0.264 (0.12 to 0.60 |
| Pruritus | 251 | 56 | 30 | 2.050 (0.59 to 7.11) |
| Urinary frequency | 301 | 22 | 34 | 0.477 (0.12 to 1.89) |
Short episodes = ≤3 months. Long episodes = >3 months.
The number of symptoms episodes presented to the GP showed a clear relation with the presence of anxiety or depressive disorder. Presenting two or more symptom episodes gives a five-fold increase of the risk of anxiety or depressive disorder. However, there was no difference between somatoform symptom episodes and somatic symptom episodes in relation to the number of presented episodes (Table 5, only data from 2007 are presented).
Table 5.
Cross-sectional analysis in a time frame of 1 year (2007): percentages of patients with/without anxiety or depression in patients presenting with different numbers of symptom episodes
| Number of symptom episodes | Number of patients | No depression or anxiety, %, | Depression or anxiety, % |
|---|---|---|---|
| Somatoform symptoms | |||
| 0 | 8447 | 98.83 | 1.17 |
| 1 | 1357 | 96.61 | 3.39 |
| ≥2 | 335 | 94.03 | 5.92 |
| Somatic symptoms | |||
| 0 | 8782 | 98.54 | 1.46 |
| 1 | 1156 | 97.66 | 2.34 |
| ≥2 | 201 | 95.02 | 4.98 |
Results of prospective analyses
The positive predictive value of all symptom episodes for anxiety and depression was very limited. Values varied between zero and 1.2% (Tables 6 and 7). For anxiety, the post-test odds (posterior chance) roughly remained unchanged with respect to the pretest odds (prior chance) for somatoform symptom episodes. The somatoform symptom episode ‘palpitations’ tripled the risk of anxiety. Somatic symptom episodes generally reduced the risk for a new episode of anxiety. The risk of depressive disorder was not raised by somatoform symptom episodes, or by somatic symptom episodes.
Table 6.
Prospective analysis of patient data (1997–2008) with symptom episodes followed by an anxiety episode within 3 months: positive and negative predictive values of unexplained and somatic symptoms for anxiety disorder
| Positive | Negative | |||
|---|---|---|---|---|
| Symptoms | Pretest, % | Post-test, % | predictive value, % | predictive value, % |
| Somatoform | ||||
| Tiredness | 0.004 | 0.003 | 0.003 | 0.996 |
| Fainting | 0.004 | 0.004 | 0.004 | 0.997 |
| Abdominal pain | 0.004 | 0.004 | 0.004 | 0.997 |
| Nausea | 0.004 | 0.007 | 0.007 | 0.997 |
| Constipation | 0.004 | 0.003 | 0.003 | 0.996 |
| Palpitations | 0.004 | 0.013 | 0.012 | 0.997 |
| Low back complaint | 0.004 | 0.001 | 0.001 | 0.996 |
| Chest symptoms | 0.004 | 0.004 | 0.004 | 0.997 |
| Muscle pain | 0.004 | 0.002 | 0.002 | 0.996 |
| Headache | 0.004 | 0.004 | 0.004 | 0.997 |
| Dizziness | 0.004 | 0.004 | 0.004 | 0.997 |
| Disturbances of sleep | 0.004 | 0.008 | 0.008 | 0.997 |
| Shortness of breath | 0.004 | 0.006 | 0.006 | 0.997 |
| Somatic | ||||
| Lymph gland enlargement | 0.004 | 0.002 | 0.002 | 0.996 |
| Localised abdominal pain | 0.004 | 0.002 | 0.002 | 0.996 |
| Diarrhoea | 0.004 | 0.004 | 0.004 | 0.997 |
| Red eye | 0.004 | 0.000 | 0.000 | 0.996 |
| Swollen ankles | 0.004 | 0.001 | 0.001 | 0.996 |
| Shoulder symptoms | 0.004 | 0.002 | 0.002 | 0.996 |
| Hand/finger symptoms | 0.004 | 0.001 | 0.001 | 0.996 |
| Hip symptoms | 0.004 | 0.002 | 0.002 | 0.996 |
| Tingling fingers/toes/feet | 0.004 | 0.003 | 0.003 | 0.997 |
| Cough | 0.004 | 0.002 | 0.002 | 0.996 |
| Throat symptoms | 0.004 | 0.004 | 0.004 | 0.997 |
| Pruritus | 0.004 | 0.002 | 0.002 | 0.996 |
| Urinary frequency | 0.004 | 0.003 | 0.003 | 0.997 |
Positive predictive value: the chance that a patient consulting the GP with a symptom has anxiety (incidence). Negative predictive value: the chance that a patient who does not present the symptom episode does not have anxiety disorder.
Table 7.
Prospective analysis of patient data (1997–2008) with symptom episodes followed by a depressive episode within 3 months: positive and negative predictive values of unexplained and somatic symptoms for depressive disorder
| Positive | Negative | |||
|---|---|---|---|---|
| Symptoms | Pretest, % | Post-test, % | predictive value, % | predictive value, % |
| Somatoform | ||||
| Tiredness | 0.014 | 0.014 | 0.014 | 0.986 |
| Fainting | 0.014 | 0.014 | 0.014 | 0.986 |
| Abdominal pain | 0.014 | 0.010 | 0.010 | 0.986 |
| Nausea | 0.014 | 0.021 | 0.021 | 0.986 |
| Constipation | 0.014 | 0.014 | 0.014 | 0.986 |
| Palpitations | 0.014 | 0.012 | 0.012 | 0.986 |
| Low back complaint | 0.014 | 0.007 | 0.007 | 0.986 |
| Chest symptoms | 0.014 | 0.005 | 0.005 | 0.986 |
| Muscle pain | 0.014 | 0.008 | 0.008 | 0.986 |
| Headache | 0.014 | 0.011 | 0.011 | 0.986 |
| Dizziness | 0.014 | 0.009 | 0.009 | 0.986 |
| Disturbances of sleep | 0.014 | 0.026 | 0.025 | 0.986 |
| Shortness of breath | 0.014 | 0.015 | 0.014 | 0.986 |
| Somatic | ||||
| Lymph gland enlargement | 0.014 | 0.005 | 0.005 | 0.986 |
| Localised abdominal pain | 0.014 | 0.008 | 0.008 | 0.986 |
| Diarrhoea | 0.014 | 0.013 | 0.013 | 0.986 |
| Red eye | 0.014 | 0.005 | 0.005 | 0.986 |
| Swollen ankles | 0.014 | 0.013 | 0.012 | 0.986 |
| Shoulder symptoms | 0.014 | 0.009 | 0.009 | 0.986 |
| Hand/finger symptoms | 0.014 | 0.006 | 0.006 | 0.986 |
| Hip symptoms | 0.014 | 0.005 | 0.005 | 0.986 |
| Tingling fingers/toes/feet | 0.014 | 0.000 | 0.000 | 0.986 |
| Cough | 0.014 | 0.008 | 0.008 | 0.986 |
| Throat symptoms | 0.014 | 0.007 | 0.007 | 0.986 |
| Pruritus | 0.014 | 0.007 | 0.007 | 0.986 |
| Urinary frequency | 0.014 | 0.013 | 0.013 | 0.986 |
Positive predictive value: the chance that a patient consulting the GP with a symptom has depression (incidence). Negative predictive value: the chance that a patient who does not present the symptom episode does not have depressive disorder.
DISCUSSION
Summary
The study showed that unexplained symptoms do have a statistically significant relation with anxiety and depression. The ORs of this association ranged from 1.7 to 5.1. Somatic symptoms were also associated with anxiety and depression but the ORs were slightly lower (range 0.69 to 3.02). Generally, there was no association between the duration of a symptom episode and the presence of anxiety or depression. The number of somatoform symptom episodes was clearly related with anxiety or depression: the more episodes, the more depression/anxiety. The same was true for somatic symptoms. The risk of depression/anxiety was 3–4 times higher in patients with two or more symptom episodes compared with patients without symptom episodes. However, in general, the predictive value for anxiety or depression was low — somatoform as well as somatic symptom episodes have low predictive values. In conclusion, patients presenting with symptoms — especially patients with two or more symptom episodes — do have a higher risk of anxiety or depression episodes. However, symptom episodes are only rarely followed by an anxiety or depression episode. Patients presenting unexplained symptoms do not differ from patients presenting somatic symptoms with respect to the occurrence of anxiety or depression.
Strengths and limitations
Several characteristics make the study valid. First, the data originate from a morbidity registration system with established reliability.21 Second, the data reflect real-life practice with presented instead of experienced morbidity. Obviously, episodes of care only reflect problems that have led to a demand for care (consulting the GP). Only a minority of symptoms that people experience result in the actual contacting of a healthcare professional.26 Third, to assess the association of unexplained symptoms and mental health problems, both cross-sectional and prospective analyses were used. Fourth, in the ICPC, the physician has to have clear indications for the diagnosis of a mental problem. The patient has to give these clues; the mere existence of one or more unexplained symptoms in itself is insufficient to diagnose a mental health problem. So, the diagnosis of a mental health problem is an assessment with mutual approval by physician and patient, which is more relevant than a diagnosis solely based on psychiatric assessment tools. Fifth, the congruence of applying ICPC depression criteria and DSM-IV criteria in routine general practice is considerable.27
One of the limitations of the study might be the low prevalence of depression and anxiety, which raises the question of under-recognition or underdiagnosis of depression or anxiety by the GPs participating in the Transition Project. If these GPs underdiagnose depression or anxiety, then the study findings of low predictive values for depression might be seriously biased. However, the prevalences of anxiety and depression are of the same order of magnitude as in two other large encounter-based Dutch primary care studies.28,29 In the authors’ view, the prevalence of depression and anxiety in the Transition project data therefore reflect the ‘true’ encounter-based prevalence of these disorders in patients visiting their GP because of a need for help for these disorders.
A second limitation is that the prospective analyses did not include an analysis of the predictive value of two or more somatoform or two or more somatic symptom episodes. The reason for this was that there were too few patients with two or more new somatoform and somatic symptom episodes in the Transition Project.
Comparison with existing literature
Previous studies demonstrated much higher prevalence rates of anxiety or depressive disorder.4,5 For example, Jackson and Passamonti found a prevalence of 29% of patients having a depressive or anxiety disorder,5 and Kroenke found a prevalence of anxiety of 18% and of depressive disorder of 26%.4 With these prevalence rates, ORs of 3–5 in primary care patients with unexplained symptoms are generally sufficient to justify screening for these disorders. However, both studies assessed symptoms as well as psychiatric morbidity with a questionnaire relying on recall of experienced complaints. The present data reflect everyday practice more accurately, as they reflect complaints and disorders presented by patients to their GP. In an earlier study, the authors looked at the ecology model for mental health problems, and found the same distribution.26 Presented mental health problems are considerably lower than those of screen-based data of experienced mental health problems. This is in line with the model of ‘ecology of medical care’ and the way this works out for mental health problems.30
Implications for practice and research
This study has shown that unexplained symptoms do have a statistically significant relation with anxiety and depressive disorder, and that somatic symptoms also have such a relation with these mental health problems. Due to the relatively high prevalence of symptom episodes, neither somatoform nor somatic symptoms predict anxiety or depressive disorder. Screening for anxiety and depression in patients presenting with somatoform symptom episodes in general practice is not justified because of the low incidence of those affective disorders following somatoform symptom episodes in the clinical population of the current study. However, there is ample evidence of a link between persistent unexplained symptoms and child abuse, maltreatment, and other forms of violence.31 Future research should therefore aim to identify patients who merit a simple ‘medical’ management and patients who are in need of a more elaborate conversation about disadvantageous life experiences. Further studies could also be directed at the relation of depression and anxiety and presenting combinations of symptoms. Finally, in the light of the generalist working style of the GP, the authors do not consider the distinction between somatoform and somatic symptoms relevant as this distinction might lead to false conclusions.
Acknowledgments
We would like to thank the following GPs for their contribution to the Transition Project: P Dijksterhuis, A Groen, J de Haan, A Honselaar-de Groot, D Janssen, G Polderman, T Polman, K Stolp, N Valken, and M Woerdeman.
Ethical approval
Ethical approval was not required.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Demers RY, Altamore R, Mustin H, et al. An exploration of the dimensions of illness behavior. J Fam Pract. 1980;11(7):1085–1092. [PubMed] [Google Scholar]
- 2.van de Lisdonk EH. Perceived and presented morbidity in general practice. A study with diaries in four general practices in The Netherlands. Scand J Prim Health Care. 1989;7(2):73–78. doi: 10.3109/02813438909088650. [DOI] [PubMed] [Google Scholar]
- 3.Kroenke K, Mangelsdorff AD. Common symptoms in ambulatory care: incidence, evaluation, therapy and outcome. Am J Med. 1989;86(3):262–266. doi: 10.1016/0002-9343(89)90293-3. [DOI] [PubMed] [Google Scholar]
- 4.Kroenke K. Somatization in primary care: it’s time for parity. Gen Hosp Psychiatry. 2000;22(3):141–143. doi: 10.1016/s0163-8343(00)00082-7. [DOI] [PubMed] [Google Scholar]
- 5.Jackson JL, Passamonti M. The outcomes among patients presenting in primary care with a physical symptom at 5 years. J Gen Intern Med. 2005;20(11):1032–1037. doi: 10.1111/j.1525-1497.2005.0241.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duddu V, Husain N, Dickens C. Medically unexplained presentations and quality of life: a study of a predominantly South Asian primary care population in England. J Psychosom Res. 2008;65(4):311–317. doi: 10.1016/j.jpsychores.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 7.Kroenke K, Spitzer RL, Williams JB, et al. Physical symptoms in primary care. Predictors of psychiatric disorders and functional impairment. Arch Fam Med. 1994;3(9):774–779. doi: 10.1001/archfami.3.9.774. [DOI] [PubMed] [Google Scholar]
- 8.Katon WJ, Walker EA. Medically unexplained symptoms in primary care. J Clin Psychiatry. 1998;59(suppl 20):15–21. [PubMed] [Google Scholar]
- 9.de Waal MWM, Arnold IA, Eekhof JAH, van Hemert AM. Somatoform disorders in general practice. Prevalence, functional impairment and comorbidity with anxiety and depressive disorders. Br J Psychiatry. 2004;184:470–476. doi: 10.1192/bjp.184.6.470. [DOI] [PubMed] [Google Scholar]
- 10.Löwe B, Spitzer RL, Williams JB, et al. Depression, anxiety and somatization in primary care: syndrome overlap and functional impairment. Gen Hosp Psychiatry. 2008;30(3):191–199. doi: 10.1016/j.genhosppsych.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 11.Mussell M, Kroenke K, Spitzer RL, et al. Gastrointestinal symptoms in primary care: prevalence and association with depression and anxiety. J Psychosom Res. 2008;64(6):605–612. doi: 10.1016/j.jpsychores.2008.02.019. [DOI] [PubMed] [Google Scholar]
- 12.Wileman L, May C, Chew-Graham CA. Medically unexplained symptoms and the problem of power in the primary care consultation: a qualitative study. Fam Pract. 2002;19(2):178–182. doi: 10.1093/fampra/19.2.178. [DOI] [PubMed] [Google Scholar]
- 13.Reid S, Whooley D, Crayford T, Hotopf M. Medically unexplained symptoms — GPs’ attitudes toward their cause and management. Fam Pract. 2001;18(5):519–523. doi: 10.1093/fampra/18.5.519. [DOI] [PubMed] [Google Scholar]
- 14.Greer J, Halgin R. Predictors of physician-patient agreement on symptom etiology in primary care. Psychosom Med. 2006;68(2):277–282. doi: 10.1097/01.psy.0000203239.74461.db. [DOI] [PubMed] [Google Scholar]
- 15.Multidisciplinary Guideline Medically Unexplained Symptoms and Somatoform Disorders [in Dutch] Houten, The Netherlands: Ladenius Communicatie BV; 2009. Trimbos Instituut/Netherlands Institute of Mental Health and Addiction and Dutch Institute for Healthcare Improvement CBO. [Google Scholar]
- 16.Okkes IM, Oskam SK, Lamberts H. The probability of specific diagnoses for patients presenting with common symptoms to Dutch family physicians. J Fam Pract. 2002;51(1):31–36. [PubMed] [Google Scholar]
- 17.Lamberts H, Wood M. International classification of primary care. Oxford: Oxford University Press; 1987. ICPC. [Google Scholar]
- 18.Lamberts H, Hofmans-Okkes IM. Episode of care: a core concept in family practice. J Fam Pract. 1996;42(2):161–167. [PubMed] [Google Scholar]
- 19.WONCA International Classification Committee. ICPC-2: International Classification of Primary Care, second edition. Prepared by the International Classification Committee of WONCA (WICC); Oxford: Oxford University Press; 1998. [Google Scholar]
- 20.Okkes IM, Oskam SK, Van Boven K, Lamberts H. EFP. Episodes of care in family practice. Epidemiological data based on the routine use of the International Classification of Primary Care (ICPC) in the Transition Project of the Academic Medical Center/University of Amsterdam. (1985–2003) In: Okkes IM, Oskam SK, Lamberts H, editors. ICPC in the Amsterdam Transition Project. CD-Rom. Amsterdam: Academic Medical Center/University of Amsterdam, Department of Family Medicine; 2005. [Google Scholar]
- 21.Lamberts H, Oskam SK, Okkes IM. [The clinical relationship between symptoms and the final diagnosis in general practice, determined by means of posterior probabilities calculated on the basis of the Transition Project] Ned Tijdschr Geneeskd. 2005;149(46):2566–2572. [PubMed] [Google Scholar]
- 22.van Ravesteijn H, Wittkampf K, Lucassen P, et al. Detecting somatoform disorders in primary care with the PHQ-15. Ann Fam Med. 2009;7(3):232–238. doi: 10.1370/afm.985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marinus AMF. Meppel: Krips; 1993. Inter-doctor variation in general practice. PhD thesis. [Google Scholar]
- 24.Bayes FRS. An essay towards solving a problem in the doctrine of changes. Philos Transact. 1763;53:370–418. (communicated by Mr Price in a letter to Mr John Canton) [PubMed] [Google Scholar]
- 25.Vermeulen M. [Roaming through methodology XXXVI. Likelihood ratios and Bayes’ rule] Ned Tijdschr Geneeskd. 2001;145(50):2421–2424. [PubMed] [Google Scholar]
- 26.Van Rijswijk E, Borghuis M, van de Lisdonk E, et al. Treatment of mental health problems in general practice: a survey of psychotropics prescribed and other treatments provided. Int J Clin Pharmacol Ther. 2007;45(1):23–29. doi: 10.5414/cpp45023. [DOI] [PubMed] [Google Scholar]
- 27.Van Weel-Baumgarten EM, van de Bosch WJ, et al. The validity of the diagnosis of depression in general practice: is using criteria for diagnosis as a routine the answer? Br J Gen Pract. 2000;50(453):284–287. [PMC free article] [PubMed] [Google Scholar]
- 28.van der Linden MW, Westert GP, de Bakker DH, Schellevis FG. Tweede Nationale Studie naar ziekten en verrichtingen in de huisartspraktijk: klachten en aandoeningen in de bevolking en in de huisartspraktijk. [The Second Dutch National Survey of General Practice] Utrecht: NIVEL, Rijksinstituut voor Volksgezondheid en Milieu; 2004. [Google Scholar]
- 29.van den Bosch WJHM, Lagro-Janssen ALM, van de Lisdonk EH, editors. Ziekten in de huisartspraktijk. Houten: Reed Business; 2008. [Google Scholar]
- 30.Green LA, Fryer GE, Yawn BP, et al. The ecology of medical care revisited. N Engl J Med. 2001;344(26):2021–2025. doi: 10.1056/NEJM200106283442611. [DOI] [PubMed] [Google Scholar]
- 31.Kirkengen AL. The lived experience of violation: how abused children become unhealthy adults. Bucharest: Zeta Books; 2010. [Google Scholar]


