Abstract
Introduction:
This review explores whether smoking prevalence in addiction treatment samples exceeds that shown in epidemiological data for persons with alcohol or other drug use disorders and whether smoking may have decreased over time in the addiction treatment population as it has done in the general population.
Methods:
English language papers published between 1987 and 2009 were searched electronically. Forty papers reporting smoking prevalence for addiction treatment samples in the United States were identified, and key predictor variables were abstracted. Random logistic models were used to assess relationships between each individual predictor (year, treatment modality, primary drug treated, government status, and public/private funding status) and smoking prevalence.
Results:
The lowest smoking prevalence aggregated for studies reported in any single year was 65%, well above epidemiological estimates reported among those with alcohol use and drug use disorders. The odds of smoking were higher in methadone maintenance programs (odds ratio [OR] = 2.25, CI = 1.08, 4.68) as compared with outpatient programs. No other variables in the model were significant. Reanalysis omitting recent studies that may represent outliers or confounding with type of treatment showed a small but significant decrease in smoking over time (OR = 0.9891, CI = 0.9888, 0.9893).
Conclusions:
The very high smoking rates reported in addiction treatment samples warrant significant, organized, and systemic response from addiction treatment systems, from agencies that fund and regulate those systems, and from agencies concerned with tobacco control.
Introduction
Population-based tobacco control efforts have reduced adult smoking prevalence in the United States from 40% in 1964 to 20.6% currently (Centers for Disease Control and Prevention [CDC], 2009a; Department of Health Education and Welfare, 1964). The benefits of this achievement are not spread evenly, however, as people living in poverty, those with lower education, and persons with mental health diagnoses continue to smoke at high rates. As smoking prevalence decreases in the general population but remains high in subgroups, these subgroups bear a disproportionate burden of smoking-related illness and also frame new targets for both smoking cessation intervention and tobacco control.
One population with elevated smoking prevalence includes those with substance use disorders. A developed literature indicates that smokers with other addictions smoke more heavily (Hays et al., 1999; J. Hughes, 2002; J. R. Hughes, 1996; Kozlowski, Jelinek, & Pope, 1986; Marks, Hill, Pomerleau, Mudd, & Blow, 1997; Sobell, 2002), are less successful in their attempts to quit smoking (Bobo, Gilchrist, Schilling, Noach, & Schinke, 1987; Drobes, 2002; Joseph, Nichol, & Anderson, 1993; Kozlowski, Skinner, Kent, & Pope, 1989; Sobell, 2002; Zimmerman, Warheit, Ulbrich, & Auth, 1990), and are more likely to die from smoking-related causes than from other substance-related causes (Hser, McCarthy, & Anglin, 1994; Hurt et al., 1996).
The National Comorbidity Study (NCS) was a national sample (n = 8,098) of noninstitutionalized U.S. persons aged 15–54 years, designed to estimate national prevalence of mental illness. NCS data reported smoking prevalence of 56.1% among persons with past-month alcohol disorders and 67.9% among those with substance use disorders (Lasser et al., 2000). The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) is a general population survey (N = 43,093) including noninstitutionalized U.S adults and weighted to be representative of the larger U.S population. NESARC data show that smoking prevalence is 34.5% among those with alcohol disorders and 52.4% among those with substance use disorders (Grant, Hasin, Chou, Stinson, & Dawson, 2004).
Smoking prevalence may be even higher among those who seek treatment for their alcohol or other drug addiction. Current literature cites smoking prevalence among addiction treatment clients as ranging between 49% and 98% (Schroeder, 2009), with many studies reporting ranges of 75%–90% (Gorelick, Simmons, Carriero, & Tashkin, 1997; Kalman, 1998; Kozlowski et al., 1989; Lai, Lai, Page, & McCoy, 2000; Patkar, Sterling, Leone, Lundy, & Weinstein, 2002; Sees & Clark, 1993; Sullivan & Covey, 2002). Papers reporting these estimates often rely on two or three other papers, and there is at present no systematic review of papers reporting smoking prevalence among those in addiction treatment.
Approximately 4 million persons received addiction treatment in 2008 (Substance Abuse and Mental Health Services Administration [SAMHSA], 2009). That smoking should be treated in addiction treatment systems is recommended in Tobacco Dependence Clinical Guidelines (Fiore et al., 2008), in the scientific literature (Hahn, Warnick, & Plemmons, 1999; Kalman, Kim, DiGirolamo, Smelson, & Ziedonis, 2010; McCool, Richter, & Choi, 2005; Walsh, Bowman, Tzelepis, & Lecathelinais, 2005) and in position statements promulgated by the American Public Health Association (2003), the American Society of Addiction Medicine (2008), and National Association of Alcoholism and Drug Abuse Counselors (n.d.), the association for addiction professionals. Nevertheless, the integration of tobacco dependence treatment into addiction programs remains modest. Richter, Choi, McCool, Harris, and Ahluwalia (2004), surveying all U.S. outpatient methadone clinics, found that 18% had offered group or individual smoking cessation counseling and 12% had prescribed nicotine replacement therapy in the past thirty days. Fuller et al. (2007), surveying directors and staff in nearly 400 treatment units, found that 31% of programs offered smoking cessation intervention. Last, Friedmann, Jiang, and Richter (2008) reported, in a national sample of outpatient programs, that 41% offered smoking cessation intervention.
A small number of systems interventions have been initiated to address tobacco dependence in addiction treatment. Beginning in 1999, the Veterans Administration (VA) system implemented smoking cessation guidelines in all health care services, including addiction treatment. Implementation is supported by clinician reminders embedded in electronic medical records, program monitoring measured against national targets, and program director incentives (Sherman, 2008). In 1999, New Jersey included a smoke-free grounds provision in licensure standards for residential addiction treatment facilities. The policy required that staff may not use tobacco during working hours and that assessment and treatment of tobacco dependence must be provided to clients (Williams et al., 2005). In 2005, Colorado adopted a constitutional amendment increasing tobacco taxes and earmarking funds for intervention with populations having high smoking prevalence, including persons in drug treatment. One effect has been to orient the largest drug treatment provider in the State (Signal Behavioral Health) toward addressing smoking in its service population (Toussaint, VanDeMark, Silverstein, & Stone, 2009). In 2008, New York implemented a policy requiring all state-supported programs to have smoke-free grounds, no evidence of smoking among staff, and provision of tobacco dependence service for all clients who request it (New York State Office of Alcoholism and Substance Abuse Tobacco Independence Initiative, 2009). These efforts reflect an increasing recognition of the need to address tobacco dependence in addiction treatment. However, such systematic efforts are few, their effectiveness is generally undocumented, and most programs do not address tobacco.
A systematic review of smoking prevalence in addiction treatment may be helpful in drawing attention to smoking in this population and directing resources and policies to address tobacco dependence. This review explores whether smoking prevalence in addiction treatment samples exceeds that shown in epidemiological data for persons with alcohol or other drug use disorders and whether smoking may have decreased over time in the addiction treatment population as it has in the general population. The review also investigates whether smoking prevalence differs by type of treatment, by primary drug for which samples are being treated, and by government status or public/private funding status of programs.
Methods
Article Identification and Selection
Published papers reporting smoking prevalence for addiction treatment samples were searched using PubMed, PsychINFO, and the Alcohol and Alcohol Problems Science Database (an archived database specific to alcohol-related research). Search terms varied by database but included tobacco, smoking, nicotine, clients, patients, self-report, addiction, substance-related disorders, and substance abuse treatment. Results were limited to articles published in English between 1987 and 2009 to capture an approximate twenty-year period for review and because we were aware of papers reporting these data in the early 1990s but not before that time.
For 4,031 papers identified, abstracts were reviewed by six raters using three criteria: (a) The publication dealt with clients in alcohol and/or drug treatment, (b) client-level data were collected, and (c) tobacco use was mentioned. Abstracts meeting all criteria were coded for inclusion. Following rater training, all raters independently rated the same set of 30 abstracts. Interrater reliability for the inclusion/exclusion was calculated using Stata (generalized κ = 0.83, p < .001). Each rater then rated a unique set of 300 abstracts, followed by a second measure of interrater reliability (generalized κ = 0.79, p < .001). The rating team reviewed five abstracts where there was disagreement and then reviewed all remaining abstracts.
Of the abstracts reviewed, 179 met inclusion criteria. One author (EP) reviewed each full article for any of four exclusions: (a) a review paper (not primary data), (b) did not report smoking prevalence for an addiction treatment sample, (c) participant selection included smokers only, and (d) reported on an adolescent sample. Also excluded were reports on screening, brief intervention, and referral to treatment conducted in medical settings (e.g., Bernstein, Bernstein, & Levenson, 1997; Fleming, Barry, Manwell, Johnson, & London, 1997; Manwell, Fleming, Mundt, Stauffacher, & Barry, 2000), one paper where sample size was not reported (Trudeau, Isenhart, & Silversmith, 1995), and three where samples overlapped with other papers (Joseph, 1993; Joseph et al., 1993; Patkar et al., 2003).
Data Analysis
Of 61 papers remaining, 33 reported studies within the United States and 28 reported studies outside the United States. Non-U.S. papers represented 21 countries, so the number from any single country was small. For this reason, the review focused on 33 papers reporting on smoking in U.S. adult addiction clinics. Bibliographies of these papers were reviewed, and nine eligible papers were added to analysis (N = 42 papers).
Year of publication, number of participants, number of smokers, and smoking prevalence were recorded for each paper. For papers using repeated measures, we used smoking prevalence from the first or baseline data collection only. For papers reporting on intervention studies, we used prevalence from the baseline or pretest data. Each article was categorized by treatment modality (outpatient, inpatient, and methadone maintenance), and primary drug treated (alcohol, alcohol and other drugs, cocaine/crack, and opiate/narcotic). Because smoking may be lower among patients entering privately funded programs and following Knudsen, Studts, Boyd, and Roman (2010), each article was classified on two dichotomous dimensions (government/nongovernment and public/private funding). Program Web sites were consulted, and authors were contacted for additional information when needed. Government programs were those operated by agencies like the VA or Departments of Public Health. Nongovernment programs may receive government funds but are generally operated by separate (for profit or nonprofit) agencies. Government programs are publicly funded, but nongovernment programs may have public funding or private funding or a combination of both. Where papers drew clients from two modalities (Cicero, Lynskey, Todorov, Inciardi, & Surratt, 2008; Cottler, Robins, & Helzer, 1989; Gorelick et al., 1997; Sees & Clark, 1993), they were coded to whichever category represented more than half of patients involved in the article. The same rule was applied where clinics reported both public and private funding.
Smoking rate was calculated for treatment modality, primary drug treated, and government status and public/private funding. To assess change over time, prevalence was calculated for all studies reported in each year from 1987 to 2009 and graphed against CDC adult smoking rates in the same time period (CDC, 2009b). Annual prevalence estimates included from one to four papers per year except for years when no papers were found (1987, 2004, and 2009). Random logistic models were used to assess univariate relationships between each individual predictor (year, treatment modality, primary drug treated, government status, and public/private funding) and smoking prevalence and then to assess multivariate relationship of these variables to smoking in the presence of all other variables.
National Survey on Drug Use and Health Analysis
National Survey on Drug Use and Health (NSDUH) is a national annual survey of drug use among noninstitutionalized persons aged 12 years and above (SAMHSA, 2009). Following procedures used by Tsoh, Chu, Mertens, and Weisner (2010) using the online NSDUH database (U.S. Department of Health and Human Services, 2009) and for the period 2000–2009, we identified respondents who had received treatment for drug or alcohol use in the past year (variable TXILLALC) and the proportion in this group who reported any cigarette use in the past month (variable CIGMON). This gives an estimate of smoking prevalence, by year, among those who had received drug or alcohol treatment. The Cochran–Armitage trend test was used to assess whether smoking prevalence in the NSDUH data may show change over time, and the slope in percent change per year was estimated using a linear regression over the ten years of data.
Results
Papers included in the review are summarized in Table 1. The type of treatment represented included inpatient (48% of papers), outpatient (31%), and methadone maintenance (21%). The primary drugs treated in these programs were coded as cocaine (24%), alcohol (21%), alcohol and other drugs combined (31%), and opiate/narcotic (24%). Nearly two thirds (64%) were nongovernment programs, and the same proportion were publicly funded.
Table 1.
U.S. Addiction Treatment Studies by Year, with Sample Size, Smoking Prevalence, and Predictor Variables (N = 42)
| Author & year | N | Smoking prevalence (%) | Modality | Primary drug treated | Government’t status | Funding source |
| Burling and Ziff (1988) | 140 | 90.7 | Inpatient | Alcohol or drug | Yes | Public |
| Finlayson, Hurt, Davis, and Morse (1988) | 216 | 66.7 | Inpatient | Alcohol | No | Private |
| Cottler et al. (1989)a | 32 | 84.4 | Inpatient | Alcohol or drug | No | Private |
| Joseph, Nichol, Willenbring, Korn, and Lysaght (1990) | 407 | 76.7 | Inpatient | Alcohol or drug | Yes | Public |
| Natali, Curtis, Suarez, and Millman (1991) | 52 | 94.2 | Inpatient | Alcohol | Yes | Public |
| Stark and Campbell (1991) | 238 | 81.9 | Methadone maintenance | Opiate/narcotic | No | Public |
| Abrams et al. (1992) | 163 | 68.1 | Outpatient | Alcohol | No | Private |
| Chakko et al. (1992) | 52 | 92.3 | Inpatient | Cocaine | Yes | Public |
| Orleans and Hutchinson (1993) | 118 | 66.1 | Inpatient | Alcohol | No | Private |
| Sees and Clark (1993) | 272 | 82.4 | Methadone maintenance | Alcohol or drug | Yes | Public |
| Hser et al. (1994) | 405 | 84.4 | Inpatient | Opiate/narcotic | Yes | Public |
| Sterling, Gottheil, Weinstein, Kurtz, and Menduke (1994) | 29 | 89.7 | Outpatient | Cocaine | No | Public |
| Fleming et al. (1995) | 1,098 | 65.0 | Inpatient | Alcohol | No | Private |
| Boyd and Pohl (1996) | 152 | 80.3 | Inpatient | Cocaine | No | Public |
| Heffner, Rosenberg, Rothrock, Kimber-Riggs, and Gould (1996) | 47 | 78.7 | Outpatient | Alcohol or drug | No | Private |
| Hurt et al. (1996) | 845 | 74.7 | Inpatient | Alcohol | No | Private |
| Roll, Higgins, Budney, Bickel, and Badger (1996) | 186 | 78.0 | Outpatient | Cocaine | No | Public |
| Clemmey, Brooner, Chutuape, Kidorf, and Stitzer (1997) | 179 | 92.2 | Methadone maintenance | Opiate/narcotic | No | Public |
| Gorelick et al. (1997) | 228 | 78.5 | Inpatient | Cocaine | Yes | Public |
| Stuyt (1997) | 348 | 75.9 | Inpatient | Alcohol or drug | No | Private |
| Rustin (1998) | 2,445 | 78.0 | Inpatient | Alcohol or drug | Yes | Public |
| Chatham, Hiller, Rowan-Szal, Joe, and Simpson (1999) | 435 | 94.0 | Methadone maintenance | Opiate/narcotic | No | Public |
| Patten et al. (1999) | 404 | 54.7 | Inpatient | Alcohol | Yes | Public |
| Frosch, Shoptaw, Nahom, and Jarvik (2000) | 355 | 73.5 | Methadone maintenance | Opiate/narcotic | No | Private |
| Hall et al. (2000) | 313 | 62.9 | Outpatient | Cocaine | Yes | Public |
| Clarke, Stein, McGarry, and Gogineni (2001) | 283 | 88.7 | Methadone maintenance | Opiate/narcotic | No | Private |
| Heil, Badger, and Higgins (2001) | 302 | 80.1 | Outpatient | Cocaine | No | Public |
| Moore and Budney (2001)b | 174 | 46.6 | Outpatient | Alcohol or drug | No | Public |
| Richter, Gibson, Ahluwalia, and Schmelzle (2001) | 550 | 76.7 | Methadone maintenance | Opiate/narcotic | No | Private |
| Miles, Kulstad, and Haller (2002)c | 108 | 79.0 | Inpatient | Cocaine | No | Public |
| Patkar, Lundy, Leone, Weinstein, Gotheil, and Steinberg (2002) | 125 | 55.2 | Outpatient | Cocaine | No | Public |
| Gibson et al. (2003)d | 337 | 82.5 | Inpatient | Alcohol or drug | Yes | Public |
| Kohn, Tsoh, and Weisner (2003) | 749 | 52.7 | Outpatient | Alcohol or drug | No | Private |
| Patten et al. (2003) | 813 | 78.4 | Inpatient | Alcohol | No | Private |
| Williams et al. (2005) | 3,472 | 76.6 | Inpatient | Alcohol or drug | Yes | Public |
| Kim et al. (2006) | 92 | 91.3 | Methadone maintenance | Opiate/narcotic | Yes | Public |
| Nahvi et al. (2006) | 389 | 81.2 | Methadone maintenance | Opiate/narcotic | No | Private |
| Patkar et al. (2006) | 168 | 82.7 | Outpatient | Cocaine | No | Public |
| Yadav et al. (2007) | 1,402 | 87.2 | Outpatient | Alcohol | Yes | Public |
| Cicero et al. (2008)ae | 1,408 | 69.4 | Outpatient | Opiate/narcotic | No | Private |
| Graff, Griffin, and Weiss (2008) | 61 | 57.4 | Outpatient | Alcohol or drug | No | Public |
| Rees, Reehlmann, Stewart, and Jones (2008) | 516 | 80.2 | Inpatient | Alcohol or drug | Yes | Public |
Note. aReported in paper as inpatient/outpatient.
Primarily treated marijuana.
The smoking n for Miles et al. (2002) was reported as being 77, however, N = 108 and states 79% smoking prevalence in text and Table 2.
Domiciliary care.
Prescription opiates only not heroin.
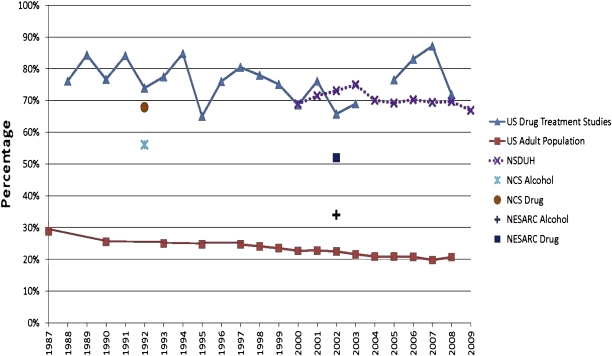
These studies span more than twenty years during which time smoking prevalence in the general population decreased dramatically. To assess whether smoking prevalence in addiction treatment samples may have changed over time, aggregated prevalence rates were calculated for each year. From 1987 through 2009, the smallest sample size, during any year for which data were available, was 32 (in 1989) and the largest sample size was 3,472 (in 2005). Mean number of respondents per year was 1,004.8 (SD = 880.7), and the median was 711.5. The lowest smoking prevalence reported in any single year was 65.0%, the highest was 87.2%, and the median was 76.3%. Annual smoking prevalence in drug treatment studies is shown in Figure 1, together with U.S. adult smoking prevalence and estimates from NESARC, NCS, and NSDUH data.
Figure 1.
Smoking prevalence in 42 U.S. addiction treatment studies, in epidemiological reports, and in the U.S. population. The literature review uncovered no studies from U.S. drug treatment facilities in 2004, giving a break in the topmost line at 2004. National Survey on Drug Use and Health (NSDUH) data (dotted line) are available in 2000–2009. Prior to 2000, NSDUH used a different variable to reflect any drug or alcohol treatment. The individual points reflect epidemiological data, showing rate of smoking among persons with a substance use disorder. National Comorbidity Study (NCS) data were collected in 1991–92, and National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) data were collected in 2001–2002. The bottom line reflects smoking prevalence in the U.S. general population.
Random logistic results are reported in Table 2. Year is a continuous measure reflecting years in which papers were published, with values in the range from 1988 to 2008. Considering the column for unadjusted odds ratio (ORs), smoking prevalence showed no change over time and no differences by primary drug treated, government status, or funding source. Smoking prevalence was higher in methadone maintenance programs when compared with outpatient programs (OR = 2.45, CI = 1.47, 4.10). In the adjusted analysis, the OR for year as a measure of time is not significant, suggesting no change in smoking prevalence across time. Among the remaining variables, only modality is significant such that the odds of smoking are higher in methadone maintenance settings (OR = 2.25, CI = 1.08, 4.68) as compared with outpatient settings. The odds of smoking in methadone maintenance were not different than those in inpatient settings (OR = 1.41, CI = 0.70, 2.83, data not shown). Tests for interactions of source year by modality and source year by primary drug treated were not significant, suggesting that the pattern of smoking prevalence over time did not differ by modality or primary drug treated.
Table 2.
Predictors of Smoking Prevalence across 42 U.S. Addiction Treatment Studies
| Predictor | Smoking rate | Unadjusted normalized |
Adjusted normalized |
||
| OR | 95% Confidence limits | OR | 95% Confidence limits | ||
| Year | 1.00 | (0.96, 1.04) | 1.01 | (0.97, 1.05) | |
| Modality | |||||
| Outpatient | 72% (3,676/5,127) | 1.00 | – | 1.00 | – |
| Inpatient | 76% (9,229/12,177) | 1.49 | (0.98,2.28) | 1.60 | (0.99, 2.59) |
| Methadone maintenance | 83% (2,327/2,793) | 2.45 | (1.47, 4.10) | 2.25 | (1.08, 4.68) |
| Primary drug treated | |||||
| Cocaine | 75% (1,244/1,652) | 1.00 | – | 1.00 | – |
| Alcohol | 74% (3,807/5,111) | 0.78 | (0.43, 1.39) | 0.86 | (0.46, 1.61) |
| Alcohol or drug | 75% (6,759/9,000) | 0.84 | (0.49, 1.44) | 0.75 | (0.44, 1.29) |
| Opiate/narcotic | 79% (3,422/4,334) | 1.51 | (0.85, 2.65) | 1.11 | (0.50, 2.46) |
| Government status | |||||
| No | 73% (6,970/9,560) | 1.00 | – | 1.00 | – |
| Yes | 78% (8,262/10,537) | 1.41 | (0.92, 2.16) | 1.17 | (0.70, 1.96) |
| Funding source | |||||
| Private | 71% (5,265/7,414) | 1.00 | – | 1.00 | – |
| Public | 79% (9,967/12,683) | 0.68 | (0.45, 1.04) | 0.71 | (0.41, 1.20) |
Note. Year is a continuous measure reflecting years in which papers were published, with values in the range from 1988 to 2008. OR = oodds ratio.
Two studies reported smoking prevalence preceding the literature review period. Hser et al. (1994) was a longitudinal follow-up of 405 narcotic users first interviewed in 1974–1975 and Hurt et al. (1996) involved mortality outcomes for persons entering alcohol treatment from 1972 to 1983. Because these cohorts were recruited in the 1970s and because we used only the baseline smoking prevalence, these more dated prevalence rates could affect estimates of change over time. Rerunning the analyses excluding data from these two papers resulted in the same pattern of findings as that reported in Table 2, although the odds of smoking in methadone maintenance no longer reached significance.
Additional analyses were prompted by two observations. First, data for U.S. drug treatment studies (Figure 1) appear to show a downward trend until 2003. Second, smoking prevalence estimates for 2005–2007 may be elevated due to confounding or atypical samples. The 2005 estimate is based on a single large sample of inpatients (Williams et al., 2005). The 2006 estimate is based on three studies, two of which are methadone maintenance samples (Kim, Alford, Malabanan, Holick, & Samet, 2006; Nahvi, Richter, Li, Modali, & Arnsten, 2006). Data in Table 1 show that smoking tends to be higher in methadone maintenance samples compared with outpatient. The 2007 sample (Yadav, Eigenbrodt, Briggs, Williams, & Wiseman, 2007) involves veterans seeking outpatient detoxification, and smoking in this sample (87.2%) may be atypical when compared with other outpatient samples in the data.
Repeating the analysis using only data from 1988 through 2003 resulted in a significant time effect (OR = 0.9891, CI = 0.9888, 0.9893), where the small CI is driven by the large sample size, and suggesting modest decrease in smoking prevalence over time. The slope in these data was 0.7% per year or an approximate 7% decrease over ten years. Given that these analyses yield different findings depending on whether they include data for all years or data for 1988–2003 only, comparison with NSDUH data may be illuminative (Figure 1). Smoking prevalence in NSDUH data from 2000 to 2009, among persons who also reported past year substance abuse treatment, ranged from 68.9% in 2000 to 66.9% in 2009. The trend test showed a significant linear decline over time (p < .0001), and the slope in the NSDUH data reflected an approximate 4% decrease over ten years.
Discussion
Across all studies reviewed, the lowest smoking prevalence for any single year was 65%, well above epidemiological estimates for those with alcohol and drug use disorders as observed in NESARC (Grant et al., 2004) and NCS (Lasser et al., 2000) data. This finding supports, as others have observed (Hahn et al., 1999; J. Hughes, 2002; Hurt et al., 1996; Schroeder & Morris, 2009), that smoking is a prevalent comorbid health risk in this population.
The question of whether smoking prevalence may have decreased over time in the addiction treatment population, as in the general population, requires interpretation. Treatment studies found in later years (2005–2008) represented programs where smoking prevalence tended to be higher and may confound the analysis. Noting that both the earlier treatment data (1987–2003) and the NSDUH data suggested decreasing smoking at similar rates, it seems likely that smoking in addiction treatment populations may be decreasing over time. Furthermore, the decrease in population smoking from 1987 to 2007 is about 8% (CDC, 2009b), while the smoking decrease observed in NSDUH data, multiplied by 20 years, gives a very similar 8% decrease. The leading concern in addiction treatment then is not that there is no decrease in smoking prevalence over time but that the prevalence of smoking is inordinately high.
Other findings offer direction about where to intervene. In the United States, 13,648 programs reported to the National Survey of Substance Abuse Treatment Services (N-SSATS) in 2007, and of these, 1,433 (10.5%) were methadone maintenance programs (SAMHSA, 2008). An estimated 260,000 persons received methadone maintenance therapy for addiction treatment in 2008 (Kleber, 2008), and most of those were smokers. Persons in methadone treatment often have long-term contact with the treating program, offering a platform for tobacco intervention. Although our analysis did not show higher smoking rates in residential as compared with outpatient treatment, residential programs may offer an intervention target because of high smoking rates and secondhand smoke exposure on program campuses. There were 4,716 residential treatment programs reporting to N-SSATS in 2007 (SAMHSA, 2008), representing almost 35% of reporting programs, and serving an estimated 743,000 persons (SAMHSA, 2009). Focusing on these two types of programs alone would bring tobacco intervention to 45% of the N-SSATS programs and to 22% (900,000/4,000,000) of persons receiving treatment each year. Because smoking prevalence is 1.6–2.3 times higher in these programs compared with outpatient programs, smoking policy and cessation interventions in these settings would reach an even larger proportion of all smokers in addiction treatment.
Most addiction treatment in the United States is provided in the public sector (Mechanic, Schlesinger, & McAlpine, 1995). Public programs are funded through Center for Substance Abuse Treatment (CSAT) block grants allocated to Single State Agencies (SSAs) responsible for addiction treatment. States, and sometimes individual counties, add to block grant funds (Guydish & Claus, 2002). In the public sector, CSAT and individual SSAs bear responsibility for access and quality of addiction treatment, including whether programs address tobacco. State addiction treatment systems in New Jersey, New York, Indiana, Oregon, and Utah now have tobacco initiatives in planning or implementation stages (Indiana Tobacco Prevention and Cessation, 2010; New York State Office of Alcoholism and Substance Abuse Services, 2008; Oregon Department of Human Services, 2010; Utah Division of Substance Abuse and Mental Health, n.d.; Williams et al., 2005). The only findings reported from these efforts to date are those from New Jersey where, one year after the policy was implemented, all residential programs provided some tobacco intervention, about half had adopted smoke-free grounds, and 41% of smokers were smoke-free during their residential stay (Williams et al., 2005).
This review includes only programs where client smoking prevalence was reported and may not be representative of all treatment programs. Nevertheless, it includes the most complete compilation of such studies reported to date and should reasonably represent the literature concerning smoking rates in U.S. adult addiction treatment. The aggregation of multiple studies by year offers only a blunt measure of annual smoking prevalence. These estimates are based on few reports per year and subject to differing proportions of programs where smoking prevalence may be relatively higher (e.g., methadone maintenance) or lower (e.g., outpatient). Annual estimates of smoking derived from this review ranged from 65% to 87% and converged with estimates derived from NSDUH data (from 66.9% to 75.0%). Literature review data reflect smoking among person recruited from addiction treatment settings, while NSDUH data reflect past-month smoking among population samples who reported receiving any addiction treatment in the past year. About half of those who report receiving addiction treatment in 2008 received such treatment in specialty clinics (SAMHSA, 2009), so that literature review data and NSDUH data capture overlapping, but not the same, samples.
Conclusions
Main findings from this review are that smoking prevalence among persons in addiction treatment is much higher than in the general population, higher than that reported in epidemiological samples of persons with substance use disorders, and highest among persons enrolled in methadone maintenance and inpatient addiction treatment. These findings point to the need for systemic tobacco dependence intervention in addiction treatment. Such intervention can occur, for example, as treatment systems consider how to embrace tobacco dependence as a comorbid condition on par with other addictions. State licensing, regulatory, and financing agencies may develop strategies to incentivize and support programs in addressing tobacco dependence. CSAT, as the primary funder of addiction treatment, could orient treatment toward tobacco dependence through grant mechanisms as it has done historically on other areas such as pregnant and perinatal women, criminal justice populations, HIV testing and counseling, and adolescent treatment. Finally, as time goes on and as population smoking decreases, tobacco control efforts may have greater impact if directed to populations where smokers are found in large numbers and for whom tobacco control efforts to date have shown limited impact.
Funding
This work was supported by the National Institute on Drug Abuse (NIDA; R01 DA020705) by the California–Arizona research node of the NIDA Clinical Trials Network (U10 DA015815) and by the NIDA San Francisco Treatment Research Center (P50 DA009253). The manuscript was not reviewed by the sponsor (NIDA) prior to submission.
Declaration of Interests
None declared.
References
- Abrams DB, Rohsenow DJ, Niaura RS, Pedraza M, Longabaugh R, Binkoff JA, et al. Smoking and treatment outcome for alcoholics. Behavior Therapy. 1992;23:283–297. doi:10.1016/S0005-7894(05)80386-7. [Google Scholar]
- American Public Health Association. 2003–10 smoking cessation within substance abuse and/or mental health treatment settings. Association News, 2003 Policy Statements. 2003:19–20. [Google Scholar]
- American Society of Addiction Medicine. Public policy statement on nicotine addiction and tobacco (formerly nicotine dependence and tobacco) Chevy Chase, MD: Author; 2008. [Google Scholar]
- Bernstein E, Bernstein J, Levenson S. Project ASSERT: An ED-based intervention to increase access to primary care, preventive services, and the substance abuse treatment system. Annals of Emergency Medicine. 1997;30:181–189. doi: 10.1016/s0196-0644(97)70140-9. doi:10.1016/S0196-0644(97)70140-9. [DOI] [PubMed] [Google Scholar]
- Bobo JK, Gilchrist LD, Schilling RF, II, Noach B, Schinke SP. Cigarette smoking cessation attempts by recovering alcoholics. Addictive Behaviors. 1987;12:209–215. doi: 10.1016/0306-4603(87)90030-x. doi:10.1016/0306-4603(87)90030-X. [DOI] [PubMed] [Google Scholar]
- Boyd CJ, Pohl J. Nicotine and alcohol abuse in African American women who smoke crack cocaine. Journal of Substance Abuse. 1996;8:463–469. doi: 10.1016/s0899-3289(96)90007-3. doi:10.1016/SO899-3289(96)90007-3. [DOI] [PubMed] [Google Scholar]
- Burling TA, Ziff DC. Tobacco smoking: A comparison between alcohol and drug abuse inpatients. Addictive Behaviors. 1988;13:185–190. doi: 10.1016/0306-4603(88)90010-x. doi:0306-4603(88)90010-X [pii] [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Cigarette smoking among adults and trends in smoking cessation—United States, 2008. Morbidity and Mortality Weekly Report. 2009a;58:1227–1232. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 1965–2007. 2009b. Trends in current cigarette smoking among high school students and adults, United States. Retrieved from http://www.cdc.gov/tobacco/data_statistics/tables/trends/cig_smoking/index.htm. [Google Scholar]
- Chakko S, Fernandez A, Mellman TA, Milanes FJ, Kessler KM, Myerburg RJ. Cardiac manifestations of cocaine abuse: A cross-sectional study of asymptomatic men with a history of long-term abuse of “crack” cocaine. Journal of the American College of Cardiology. 1992;20:1168–1174. doi: 10.1016/0735-1097(92)90374-v. doi:0735-1097(92)90374-V [pii] [DOI] [PubMed] [Google Scholar]
- Chatham LR, Hiller ML, Rowan-Szal GA, Joe GW, Simpson DD. Gender differences at admission and follow-up in a sample of methadone maintenance clients. Substance Use & Misuse. 1999;34:1137–1165. doi: 10.3109/10826089909039401. doi:10.3109/10826089909039401. [DOI] [PubMed] [Google Scholar]
- Cicero TJ, Lynskey M, Todorov A, Inciardi JA, Surratt HL. Co-morbid pain and psychopathology in males and females admitted to treatment for opioid analgesic abuse. Pain. 2008;139:127–135. doi: 10.1016/j.pain.2008.03.021. doi:10.1016/j.pain.2008.03.021. [DOI] [PubMed] [Google Scholar]
- Clarke JG, Stein MD, McGarry KA, Gogineni A. Interest in smoking cessation among injection drug users. American Journal on Addictions. 2001;10:159–166. doi: 10.1080/105504901750227804. doi:10.1080/105504901750227804. [DOI] [PubMed] [Google Scholar]
- Clemmey P, Brooner R, Chutuape MA, Kidorf M, Stitzer M. Smoking habits and attitudes in a methadone maintenance treatment population. Drug and Alcohol Dependence. 1997;44:123–132. doi: 10.1016/s0376-8716(96)01331-2. doi:10.1016/s0376-8716(96)01331-2. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Robins LN, Helzer JE. The reliability of the CIDI-SAM: A comprehensive substance abuse interview. British Journal of Addiction. 1989;84:801–814. doi: 10.1111/j.1360-0443.1989.tb03060.x. doi:10.1111/j.1360-0443.1989.tb03060.x. [DOI] [PubMed] [Google Scholar]
- Department of Health Education and Welfare. Washington, DC: U.S. Government Printing Office; 1964. Smoking and health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. [Google Scholar]
- Drobes DJ. Cue reactivity in alcohol and tobacco dependence. Alcoholism: Clinical and Experimental Research. 2002;26:1928–1929. doi: 10.1097/01.ALC.0000040983.23182.3A. doi:10.1097/01.ALC.0000040983.23182.3A. [DOI] [PubMed] [Google Scholar]
- Finlayson RE, Hurt RD, Davis LJ, Jr., Morse RM. Alcoholism in elderly persons: A study of the psychiatric and psychosocial features of 216 inpatients. Mayo Clinic Proceedings. 1988;63:761–768. doi: 10.1016/s0025-6196(12)62355-6. [DOI] [PubMed] [Google Scholar]
- Fiore M, Jaén C, Baker T, Bailey W, Benowitz N, Currie S, et al. Rockville, MD: U.S. Department of Health and Human Services; 2008. Clinical practice guideline. Treating tobacco use and dependence: 2008 update. [Google Scholar]
- Fleming MF, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice for problem alcohol drinkers: A randomized controlled trial in community-based primary care practices. Journal of the American Medical Association. 1997;277:1039–1045. doi:10.1001/jama.1997.03540370029032. [PubMed] [Google Scholar]
- Fleming MF, Wilk A, Kruger J, Kropp S, Manwell L, Desnoyers P. Hospital-based alcohol and drug specialty consultation service: Does it work? Southern Medical Journal. 1995;88:275–282. doi: 10.1097/00007611-199503000-00006. [DOI] [PubMed] [Google Scholar]
- Friedmann PD, Jiang L, Richter KP. Cigarette smoking cessation services in outpatient substance abuse treatment programs in the United States. Journal of Substance Abuse Treatment. 2008;34:165–172. doi: 10.1016/j.jsat.2007.02.006. doi:10.1016/j.jsat.2007.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frosch DL, Shoptaw S, Nahom D, Jarvik ME. Associations between tobacco smoking and illicit drug use among methadone-maintained opiate-dependent individuals. Experimental and Clinical Psychopharmacology. 2000;8:97–103. doi: 10.1037//1064-1297.8.1.97. doi:10.1037//1064-1297.8.1.97. [DOI] [PubMed] [Google Scholar]
- Fuller BE, Guydish J, Tsoh J, Reid MS, Resnick M, Zammarelli L, et al. Attitudes toward the integration of smoking cessation treatment into drug abuse clinics. Journal of Substance Abuse Treatment. 2007;32:53–60. doi: 10.1016/j.jsat.2006.06.011. doi:10.106/j.jsat.2006.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson G, Rosenheck R, Tullner JB, Grimes RM, Seibyl CL, Rivera-Torres A, et al. A national survey of the oral health status of homeless veterans. Journal of Public Health Dentistry. 2003;63:30–37. doi: 10.1111/j.1752-7325.2003.tb03471.x. doi:10.1111/j.1752-7325.2003.tb03471.x. [DOI] [PubMed] [Google Scholar]
- Gorelick DA, Simmons MS, Carriero N, Tashkin DP. Characteristics of smoked drug use among cocaine smokers. American Journal on Addictions. 1997;6:237–245. doi:10.3109/10550499709136991. [PubMed] [Google Scholar]
- Graff FS, Griffin ML, Weiss RD. Predictors of dropout from group therapy among patients with bipolar and substance use disorders. Drug and Alcohol Dependence. 2008;94:272–275. doi: 10.1016/j.drugalcdep.2007.11.002. doi:10.1016/j.drugalcdep.2007.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61:1107–1115. doi: 10.1001/archpsyc.61.11.1107. doi:10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- Guydish J, Claus RE. Improving publicly-funded drug abuse treatment systems: The target cities initiative. Journal of Psychoactive Drugs. 2002;34:1–6. doi: 10.1080/02791072.2002.10399930. [DOI] [PubMed] [Google Scholar]
- Hahn EJ, Warnick TA, Plemmons S. Smoking cessation in drug treatment programs. Journal of Addictive Diseases. 1999;18:89–101. doi: 10.1300/J069v18n04_08. doi:10.1300/J069v18n04_08. [DOI] [PubMed] [Google Scholar]
- Hall GW, Carriero NJ, Takushi RY, Montoya ID, Preston KL, Gorelick DA. Pathological gambling among cocaine-dependent outpatients. American Journal of Psychiatry. 2000;157:1127–1133. doi: 10.1176/appi.ajp.157.7.1127. doi:10.1176/appi.ajp.157.7.1127. [DOI] [PubMed] [Google Scholar]
- Hays JT, Schroeder DR, Offord KP, Croghan IT, Patten CA, Hurt RD, et al. Response to nicotine dependence treatment in smokers with current and past alcohol problems. Annals of Behavioral Medicine. 1999;21:244–250. doi: 10.1007/BF02884841. doi:10.1007/bf02884841. [DOI] [PubMed] [Google Scholar]
- Heffner KP, Rosenberg H, Rothrock N, Kimber-Riggs K, Gould C. Recreational drug use concurrent with abuse or dependence on other psychoactive substances. Journal of Substance Abuse Treatment. 1996;13:499–504. doi: 10.1016/s0740-5472(96)00190-0. doi:S0740547296001900 [pii] [DOI] [PubMed] [Google Scholar]
- Heil SH, Badger GJ, Higgins ST. Alcohol dependence among cocaine-dependent outpatients: Demographics, drug use, treatment outcome and other characteristics. Journal of Studies on Alcohol. 2001;62:14–22. doi: 10.15288/jsa.2001.62.14. [DOI] [PubMed] [Google Scholar]
- Hser YI, McCarthy WJ, Anglin MD. Tobacco use as a distal predictor of mortality among long-term narcotics addicts. Preventive Medicine. 1994;23:61–69. doi: 10.1006/pmed.1994.1009. doi:10.1006/pmed.1994.1009. [DOI] [PubMed] [Google Scholar]
- Hughes J. Do smokers with current or past alcoholism need different or more intensive treatment? Alcoholism: Clinical and Experimental Research. 2002;26:1934–1935. doi: 10.1097/01.ALC.0000041282.57396.30. doi:10.1097/01.ALC.0000041282.57396.30. [DOI] [PubMed] [Google Scholar]
- Hughes JR. Treating smokers with current or past alcohol dependence. American Journal of Health Behavior. 1996;20:286–290. [Google Scholar]
- Hurt RD, Offord KP, Croghan IT, Gomez-Dahl L, Kottke TE, Morse RM, et al. Mortality following inpatient addictions treatment. Role of tobacco use in a community-based cohort. Journal of the American Medical Association. 1996;275:1097–1103. doi: 10.1001/jama.275.14.1097. doi.1001/jama.1996/03530380039029. [DOI] [PubMed] [Google Scholar]
- Indiana Tobacco Prevention and Cessation. 2010. Policy change in behavioral health care and addiction treatment facilities. Retrieved from http://www.in.gov/itpc/files/MI_SUD_TF_Policy.pdf. [Google Scholar]
- Joseph AM. Nicotine treatment at the drug dependency program of the Minneapolis VA Medical Center. A researcher's perspective. Journal of Substance Abuse Treatment. 1993;10:147–152. doi: 10.1016/0740-5472(93)90039-5. doi:10.1016/0740-5472(93)90039-5. [DOI] [PubMed] [Google Scholar]
- Joseph AM, Nichol KL, Anderson H. Effect of treatment for nicotine dependence on alcohol and drug treatment outcomes. Addictive Behaviors. 1993;18:635–644. doi: 10.1016/0306-4603(93)90017-4. doi:10.1016/0306-4603(93)90017-4. [DOI] [PubMed] [Google Scholar]
- Joseph AM, Nichol KL, Willenbring ML, Korn JE, Lysaght LS. Beneficial effects of treatment of nicotine dependence during an inpatient substance abuse treatment program. Journal of the American Medical Association. 1990;263:3043–3046. doi:10.1001/jama.1990.03440220067031. [PubMed] [Google Scholar]
- Kalman D. Smoking cessation treatment for substance misusers in early recovery: A review of the literature and recommendations for practice. Substance Use & Misuse. 1998;33:2021–2047. doi: 10.3109/10826089809069815. doi:10.3109/10826089809069815. [DOI] [PubMed] [Google Scholar]
- Kalman D, Kim S, DiGirolamo G, Smelson D, Ziedonis D. Addressing tobacco use disorder in smokers in early remission from alcohol dependence: The case for integrating smoking cessation services in substance use disorder treatment programs. Clinical Psychology Review. 2010;30:12–24. doi: 10.1016/j.cpr.2009.08.009. doi:10.1016/j.cpr.2009.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim TW, Alford DP, Malabanan A, Holick MF, Samet JH. Low bone density in patients receiving methadone maintenance treatment. Drug and Alcohol Dependence. 2006;85:258–262. doi: 10.1016/j.drugalcdep.2006.05.027. doi:10.1016/j.drugalcdep.2006.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleber HD. Methadone maintenance 4 decades later: Thousands of lives saved but still controversial. Journal of the American Medical Association. 2008;300:2303–2305. doi: 10.1001/jama.2008.648. doi:10.1001/jama.2008.648. [DOI] [PubMed] [Google Scholar]
- Knudsen HK, Studts JL, Boyd S, Roman PM. Structural and cultural barriers to the adoption of smoking cessation services in addiction treatment organizations. Journal of Addictive Diseases. 2010;29:294–305. doi: 10.1080/10550887.2010.489446. doi:10.1080/10550887.2010.489446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohn CS, Tsoh JY, Weisner CM. Changes in smoking status among substance abusers: Baseline characteristics and abstinence from alcohol and drugs at 12-month follow-up. Drug and Alcohol Dependence. 2003;69:61–71. doi: 10.1016/s0376-8716(02)00256-9. doi:S0376871602002569 [pii] [DOI] [PubMed] [Google Scholar]
- Kozlowski LT, Jelinek LC, Pope MA. Cigarette smoking among alcohol abusers: A continuing and neglected problem. Canadian Journal of Public Health. 1986;77:205–207. [PubMed] [Google Scholar]
- Kozlowski LT, Skinner W, Kent C, Pope MA. Prospects for smoking treatment in individuals seeking treatment for alcohol and other drug problems. Addictive Behaviors. 1989;14:273–278. doi: 10.1016/0306-4603(89)90058-0. doi:10.1016/0306-4603(89)90058-0. [DOI] [PubMed] [Google Scholar]
- Lai S, Lai H, Page JB, McCoy CB. The association between cigarette smoking and drug abuse in the United States. Journal of Addictive Diseases. 2000;19:11–24. doi: 10.1300/J069v19n04_02. doi:10.1300/J069v19n04_02. [DOI] [PubMed] [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: A population-based prevalence study. Journal of the American Medical Association. 2000;284:2606–2610. doi: 10.1001/jama.284.20.2606. doi:10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- Manwell LB, Fleming MF, Mundt MP, Stauffacher EA, Barry KL. Treatment of problem alcohol use in women of childbearing age: Results of a brief intervention trial. Alcoholism: Clinical and Experimental Research. 2000;24:1517–1524. doi:10.2307/3350312. [PubMed] [Google Scholar]
- Marks JL, Hill EM, Pomerleau CS, Mudd SA, Blow FC. Nicotine dependence and withdrawal in alcoholic and nonalcoholic ever-smokers. Journal of Substance Abuse Treatment. 1997;14:521–527. doi: 10.1016/s0740-5472(97)00049-4. doi:10.1016/S0740-5472(97)00049-4. [DOI] [PubMed] [Google Scholar]
- McCool RM, Richter KP, Choi WS. Benefits of and barriers to providing smoking treatment in methadone clinics: Findings from a national study. American Journal on Addictions. 2005;14:358–366. doi: 10.1080/10550490591003693. doi:10.1080/10550490591003693. [DOI] [PubMed] [Google Scholar]
- Mechanic D, Schlesinger M, McAlpine DD. Management of mental health and substance abuse services: State of the art and early results. Milbank Quarterly. 1995;73:19–55. doi:10.2307/3350312. [PubMed] [Google Scholar]
- Miles DR, Kulstad JL, Haller DL. Severity of substance abuse and psychiatric problems among perinatal drug-dependent women. Journal of Psychoactive Drugs. 2002;34:339–346. doi: 10.1080/02791072.2002.10399974. [DOI] [PubMed] [Google Scholar]
- Moore BA, Budney AJ. Tobacco smoking in marijuana-dependent outpatients. Journal of Substance Abuse. 2001;13:583–596. doi: 10.1016/s0899-3289(01)00093-1. doi:10.1016/S0899-3289(01)00093-1. [DOI] [PubMed] [Google Scholar]
- National Association of Alcoholism and Drug Abuse Counselors. n.d.. Position statement: Nicotine dependence. Retrieved from http://www.naadac.org/index.php?option=com_content&view=article&id=236&Itemid=82. [Google Scholar]
- Nahvi S, Richter K, Li X, Modali L, Arnsten J. Cigarette smoking and interest in quitting in methadone maintenance patients. Addictive Behaviors. 2006;31:2127–2134. doi: 10.1016/j.addbeh.2006.01.006. doi:10.1016/j.addbeh.2006.01.006. [DOI] [PubMed] [Google Scholar]
- Natali C, Curtis JL, Suarez L, Millman EJ. Oral mucosa pigment changes in heavy drinkers and smokers. Journal of the National Medical Association. 1991;83:434–438. [PMC free article] [PubMed] [Google Scholar]
- New York State Office of Alcoholism and Substance Abuse Services. 2008. Tobacco-free services: 2008 title 14 NYCRR part 856. Retrieved from http://www.oasas.state.ny.us/regs/856.cfm. [Google Scholar]
- New York State Office of Alcoholism and Substance Abuse Tobacco Independence Initiative. Vol. 18. Tobacco Free for Recovery; 2009. 100 pioneers profile: Freedom from a deadly addiction. Retrieved from http://smokingcessationleadership.ucsf.edu/newsletter/DEC09.html. [Google Scholar]
- Oregon Department of Human Services. Salem, OR: Addictions and Mental Health Division; 2010. Tobacco freedom, August 17, 2010: Prepared by Richard L. Harris, Assistant Director. [Google Scholar]
- Orleans CT, Hutchinson D. Tailoring nicotine addiction treatments for chemical dependency patients. Journal of Substance Abuse Treatment. 1993;10:197–208. doi: 10.1016/0740-5472(93)90045-4. doi:10.1016/0740-5472(93)90045-4. [DOI] [PubMed] [Google Scholar]
- Patkar AA, Lundy A, Leone FT, Lundy A, Weinstein SP. Tobacco and Alcohol Use and Medical Symptoms Among Cocaine Dependent Patients. Substance Abuse. 2002;23:105–114. doi: 10.1080/08897070209511480. doi:10.1023/A:1015339306326. [DOI] [PubMed] [Google Scholar]
- Patkar AA, Mannelli P, Peindl K, Murray HW, Meier B, Leone FT. Changes in tobacco smoking following treatment for cocaine dependence. American Journal of Drug and Alcohol Abuse. 2006;32:135–148. doi: 10.1080/00952990500479209. doi:10.1080/00952990500479209. [DOI] [PubMed] [Google Scholar]
- Patkar AA, Sterling RC, Leone FT, Lundy A, Weinstein SP. Relationship between tobacco smoking and medical symptoms among cocaine-, alcohol-, and opiate-dependent patients. American Journal on Addictions. 2002;11:209–218. doi: 10.1080/10550490290087974. doi:10.1080/10550490290087974. [DOI] [PubMed] [Google Scholar]
- Patkar AA, Vergare MJ, Thornton CC, Weinstein SP, Murray HW, Leone FT. Nicotine dependence and treatment outcome among African American cocaine-dependent patients. Nicotine & Tobacco Research. 2003;5:411–418. doi: 10.1080/1462220031000094178. doi:10.1080/1462220031000094178. [DOI] [PubMed] [Google Scholar]
- Patten CA, Hurt RD, Offord KP, Croghan IT, Gomez-Dahl LC, Kottke TE, et al. Relationship of tobacco use to depressive disorders and suicidality among patients treated for alcohol dependence. American Journal on Addictions. 2003;12:71–83. doi:10.1080/713869856. [PubMed] [Google Scholar]
- Patten CA, Martin JE, Hofstetter CR, Brown SA, Kim N, Williams C. Smoking cessation following treatment in a smoke-free Navy alcohol rehabilitation program. Journal of Substance Abuse Treatment. 1999;16:61–69. doi: 10.1016/s0740-5472(98)00016-6. doi:S0740547298000166 [pii] [DOI] [PubMed] [Google Scholar]
- Rees AC, Reehlmann DO, Stewart D, Jones G. Banning smoking on a substance abuse treatment unit: Does it deter patients? Journal of the Louisiana State Medical Society. 2008;160:343–347. [PubMed] [Google Scholar]
- Richter KP, Choi WS, McCool RM, Harris KJ, Ahluwalia JS. Smoking cessation services in U.S. methadone maintenance facilities. Psychiatric Services. 2004;55:1258–1264. doi: 10.1176/appi.ps.55.11.1258. [DOI] [PubMed] [Google Scholar]
- Richter KP, Gibson CA, Ahluwalia JS, Schmelzle KH. Tobacco use and quit attempts among methadone maintenance clients. American Journal of Public Health. 2001;91:296–299. doi: 10.2105/ajph.91.2.296. doi:10.2105/AJPH.91.2.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roll JM, Higgins ST, Budney AJ, Bickel WK, Badger GJ. A comparison of cocaine-dependent cigarette smokers and non-smokers on demographic, drug use and other characteristics. Drug and Alcohol Dependence. 1996;40:195–201. doi: 10.1016/0376-8716(96)01219-7. doi:10.1016/0376-8716(96)01219-7. [DOI] [PubMed] [Google Scholar]
- Rustin TA. Incorporating nicotine dependence into addiction treatment. Journal of Addictive Diseases. 1998;17:83–108. doi: 10.1300/J069v17n01_08. doi:10.1300/J069v17n01_08. [DOI] [PubMed] [Google Scholar]
- Schroeder SA. A 51-year-old woman with bipolar disorder who wants to quit smoking. Journal of the American Medical Association. 2009;301:522–531. doi: 10.1001/jama.2008.982. doi:10.1001/jama.2008.982. [DOI] [PubMed] [Google Scholar]
- Schroeder SA, Morris CD. Confronting a neglected epidemic: Tobacco cessation for persons with mental Illness and substance abuse problems. Annual Review of Public Health. 2010;31:297–314. doi: 10.1146/annurev.publhealth.012809.103701. doi:10.1146/annurev.publhealth.012809.103701. [DOI] [PubMed] [Google Scholar]
- Sees KL, Clark HW. When to begin smoking cessation in substance abusers. Journal of Substance Abuse Treatment. 1993;10:189–195. doi: 10.1016/0740-5472(93)90044-3. doi:10.1016/0740-5472(93)90044-3. [DOI] [PubMed] [Google Scholar]
- Sherman SE. A framework for tobacco control: Lessons learnt from Veterans Health Administration. British Medical Journal. 2008;336:1016–1019. doi: 10.1136/bmj.39510.805266.BE. doi:10.1136/bmj.39510.805266.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell MB. Alcohol and tobacco: Clinical and treatment issues. Alcoholism: Clinical and Experimental Research. 2002;26:1954–1955. doi: 10.1097/01.ALC.0000041008.52475.C5. doi:10.1097/01.ALC.0000041008.52475.C5. [DOI] [PubMed] [Google Scholar]
- Stark MJ, Campbell BK. A psychoeducational approach to methadone maintenance treatment: A survey of client reactions. Journal of Substance Abuse Treatment. 1991;8:125–131. doi: 10.1016/0740-5472(91)90003-s. doi:10.1016/0740-5472(91)90003-S. [DOI] [PubMed] [Google Scholar]
- Sterling RC, Gottheil E, Weinstein SP, Kurtz JW, Menduke H. The effect of a no-smoking policy on recruitment and retention in outpatient cocaine treatment. Journal of Addictive Diseases: The Official Journal of the American Society of Addiction Medicine. 1994;13:161–168. doi: 10.1300/j069v13n04_04. doi:10.1300/J069v13n04_04. [DOI] [PubMed] [Google Scholar]
- Stuyt EB. Recovery rates after treatment for alcohol/drug dependence. Tobacco users vs. non-tobacco users. American Journal on Addictions. 1997;6:159–167. doi:10.1111/j.1521-0391.1997.tb00565.x. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Rockville, MD: Office of Applied Studies; 2008. National Survey of Substance Abuse Treatment Services (N-SSATS): 2007. Data on substance abuse treatment facilities. DASIS Series: S-44, DHHS Publication No. (SMA) 08-4348. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Rockville, MD: Office of Applied Studies; 2009. Results from the 2008 National Survey on Drug Use and Health: National findings. NSDUH Series H-36, HHS Publication No. SMA 09-4434. [Google Scholar]
- Sullivan MA, Covey LS. Current perspectives on smoking cessation among substance abusers. Current Psychiatry Report. 2002;4:388–396. doi: 10.1007/s11920-002-0087-5. doi:10.1007/s11920-002-0087-5. [DOI] [PubMed] [Google Scholar]
- Toussaint DW, VanDeMark NR, Silverstein M, Stone E. Exploring factors related to readiness to change tobacco use for clients in substance abuse treatment. Journal of Drug Issues. 2009;39:277–1209. [Google Scholar]
- Trudeau DL, Isenhart C, Silversmith D. Efficacy of smoking cessation strategies in a treatment program. Journal of Addictive Diseases. 1995;14:109–116. doi: 10.1300/J069v14n01_10. doi:10.1300/J069v14n01_10. [DOI] [PubMed] [Google Scholar]
- Tsoh JY, Chu FW, Mertens JR, Weisner CM. Stopping smoking during first year of substance use treatment predicted 9-year alcohol and drug treatment outcomes. Drug and Alcohol Dependence. 2011;114:110–118. doi: 10.1016/j.drugalcdep.2010.09.008. doi:10.1016/j.drugalcdep.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Ann Arbor, MI: Inter-University Consortium for Political and Social Research (distributor); 2009. National Survey on Drug Use and Health, 2008. National Survey on Drug Use and Health (NSDUH) Series. United States Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Office of Applied Studies. [Google Scholar]
- Utah Division of Substance Abuse and Mental Health. Recovery plus tobacco project. n.d.. Retrieved from http://www.dsamh.utah.gov/recovery_plus_tobacco_project.html. [Google Scholar]
- Walsh RA, Bowman JA, Tzelepis F, Lecathelinais C. Smoking cessation interventions in Australian drug treatment agencies: A national survey of attitudes and practices. Drug and Alcohol Review. 2005;24:235–244. doi: 10.1080/09595230500170282. doi:10.1080/09595230500170282. [DOI] [PubMed] [Google Scholar]
- Williams JM, Foulds J, Dwyer M, Order-Connors B, Springer M, Gadde P, et al. The integration of tobacco dependence treatment and tobacco-free standards into residential addictions treatment in New Jersey. Journal of Substance Abuse Treatment. 2005;28:331–340. doi: 10.1016/j.jsat.2005.02.010. doi:10.1016/j.jsat.2005.02.010. [DOI] [PubMed] [Google Scholar]
- Yadav D, Eigenbrodt ML, Briggs MJ, Williams DK, Wiseman EJ. Pancreatitis: Prevalence and risk factors among male veterans in a detoxification program. Pancreas. 2007;34:390–398. doi: 10.1097/mpa.0b013e318040b332. doi:10.1097/mpa.0b013e318040b332. [DOI] [PubMed] [Google Scholar]
- Zimmerman RS, Warheit GJ, Ulbrich PM, Auth JB. The relationship between alcohol use and attempts and success at smoking cessation. Addictive Behaviors. 1990;15:197–207. doi: 10.1016/0306-4603(90)90063-4. doi:10.1016/0306-4603(90)90063-4. [DOI] [PubMed] [Google Scholar]