Abstract
Dislocation of the elbow associated with radial head and coronoid fracture, the so-called “terrible triad” of the elbow, is challenging to treat and has a history of complicated outcomes. However, advances in the knowledge of elbow kinematics combined with improved implants and surgical techniques during the past few years have led to the development of standard surgical protocols. This review article analyses the results in 137 elbow triad injuries of five studies treated using the current protocols. These include fixation of the coronoid fracture, repair or replacement the radial head, and repair of the lateral ligament complex, reserving medial collateral ligament repair and application of hinged external fixation for patients with residual instability. Treatment of these demanding injuries appeared effective in the majority of cases, i.e. with an average of 31 months of follow-up, overall flexion arc was 111.4°, averaged flexion was 132.5° with forearm rotation of 135.5°, Mayo elbow performance score was 85.6 points, and Broberg-Morrey score was 85 points. Nevertheless, the patient should be informed about the incidence of complications including joint stiffness, ulnar nerve symptoms or post-traumatic arthritis.
Introduction
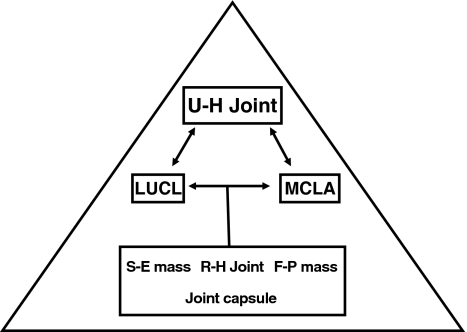
Fracture dislocations of the elbow are difficult injuries to manage [1–5], and historically have had a consistently poor outcome. The terrible triad of the elbow consists of a combination of an elbow dislocation, a radial head fracture, and a coronoid process fracture. This situation almost always renders the elbow unstable, making surgical fixation necessary. The primary goal of surgical fixation is to obtain a stable joint that permits early motion. The knowledge of elbow biomechanics (Fig. 1) and the patho-anatomy of this injury has improved during recent years, and new implants have been developed, thereby allowing the development of a systematic approach for treatment [6]. Most cases are managed surgically. Thus, open reduction and internal fixation of the coronoid fracture and/or repair of the anterior capsule, repair or replacement the radial head, and repair of the lateral ligament complex is the treatment of choice. Repair of the medial collateral ligament and/or application of a hinged external fixation are reserved for patients who demonstrate residual instability after standard treatment.
Fig. 1.
Elements for elbow stability. U-H ulno-humeral, LUCL lateral ulnar collateral ligament, MCLA anterior band of medial collateral ligament, S-E supinator-extensor, R-H radio-humeral, F-P flexor-pronator
The purpose of this review was to evaluate the injury patterns, treatments applied and outcomes obtained in patients with elbow terrible triads treated by current surgical protocols and define the key aspects in the management of these complex injuries.
Material and methods
An electronic search was conducted using the EMBASE and MEDLINE databases. Three different searches were performed in each database. Search keywords included elbow, fracture, dislocation, complex dislocation and terrible triad. Only papers in English were included. Articles were considered eligible if they met the following inclusion criteria: the target population consisted of adult patients with the “terrible triad” pattern of injury of the elbow, the treatment applied was based on current surgical protocols for these injuries, and the outcome was described adequately using validated assessment tools. Case reports, review papers, expert opinion articles, editorials, letters to the editor, publications on congress proceedings, manuscripts with incomplete documentation of outcomes, details of the applied treatment, or unpublished series were excluded (Fig. 2).
Fig. 2.
Search strategy
The combined search produced 3,036 articles. The titles and abstracts were each reviewed to identify those of interest for in-depth review. Twenty-one articles from EMBASE [1, 7–26] and 21 from MEDLINE [1, 8–12, 14–16, 18–21, 27–34] were identified and reviewed, and their bibliographies were also reviewed to look for other potential articles for inclusion.
Of 42 manuscripts initially selected based on the search strategy of this study, five met the inclusion criteria [8, 9, 16, 20, 33].
The Methods and Results sections of these manuscripts were then reviewed. Data regarding study demographics and methodology were extracted and placed in table form (Table 1). Data extracted from the articles were further analysed for type of injury and surgical treatment applied, functional outcomes at final follow-up and postoperative complications.
Table 1.
Demographic data
| Author | Journal | Year | Level of evidence | Number of patients | Male | Female | Age, years (range) | Follow-up, months (range) |
|---|---|---|---|---|---|---|---|---|
| Pugh et al. | J Bone Joint Surg Am | 2004 | IV | 36 | 22 | 14 | 41.4 (13–76) | 34 (20–65) |
| Egol et al. | Bulletin NYU Hosp Joint Dis | 2007 | IV | 29 | 15 | 14 | 53 (28–79) | 27 (12–105) |
| Forthman et al. | J Hand Surg | 2007 | IV | 22 | 14 | 8 | 48.1 (24–75) | 29 (12–46) |
| Lindenhovius et al. | J Hand Surg | 2008 | III | 18 | 12 | 6 | 47 (22–76) | 29 (10–53) |
| Zeiders et al. | J Bone Joint Surg Am | 2008 | IV | 32 | n/a | n/a | n/a | 36 (12–60) |
n/a not available
Type of injury
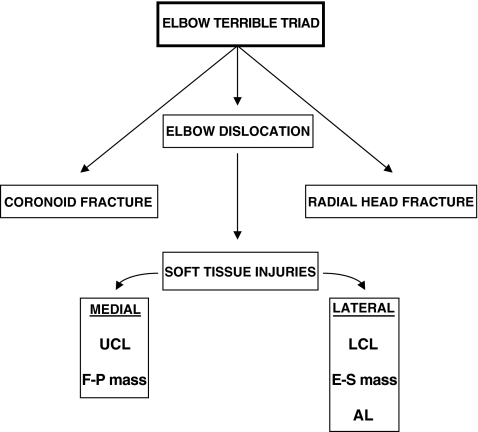
The term "terrible triad of the elbow" refers to an elbow dislocation associated with a radial head and coronoid process fracture (Fig. 3). However, there is a huge spectrum of injuries that can be included. According to the literature reviewed, most of the cases are male adults with types II or III radial head fractures (Mason classification) and type I coronoid fractures (Regan-Morrey classification). Although the Regan-Morrey classification for coronoid fractures has been widely used, the classification described by O’Driscoll et al. [35] has recently gained popularity.
Fig. 3.
Anatomical structures affected in the “terrible triad injury” of the elbow. UCL ulnar collateral ligament, F-P flexor-pronator, LCL lateral collateral ligament, E-S extensor-supinator, AL annular ligament
Soft tissues injuries must also be taken into account. The lateral collateral ligament, medial collateral ligament and anterior capsule are usually torn, and these structures are important determinants of elbow stability [36].
As a result of high energy trauma, associated injuries are often found. These injuries must be suspected to avoid mistakes in diagnosis. In elbow triads, attention is usually focussed on the dislocated elbow but there should be a high index of suspicion for ipsilateral wrist fractures (radius, scaphoid), proximal ulna fractures, radial neck fractures, capitelum fractures, or contralateral upper limb fractures (Table 2).
Table 2.
Associated injuries
| Associated Injuries | Number of patients |
|---|---|
| Wrist fracture (distal radius, scaphoid) | 6 |
| Proximal ulna fracture | 2 |
| Capitellum fracture | 1 |
| Radial neck fracture | 3 |
| Contralateral upper limb fracture | 9 |
| Others (acetabulum) | 1 |
| Total | 22 |
In order to achieve good results, it is important to clearly define the injury and make a preoperative treatment strategy. Plain radiographs of the elbow and wrist must be obtained (Fig. 4a–b), but in the majority of cases a computed tomography scan is mandatory (Fig. 5).
Fig. 4.

Elbow radiographs showing elbow dislocation, radial head fracture and type I coronoid fracture (confirmed by computed tomography). a Anteroposterior view. b Lateral view
Fig. 5.

Computed tomography showing a type II (Regan-Morrey) coronoid fracture
Surgical treatment
Treatment delay
The goal in the treatment of elbow triads is to achieve a stable joint that allows early motion, in order to prevent joint stiffness. The majority of cases reported in the papers reviewed were treated during the first week after the injury.
Before surgery, it is important to define the type of the injury and prepare for any possible intraoperative complications. Thus, all the potentially necessary material must be readied and available (screws, suture anchors, transtibial tunnel guide from the anterior cruciate ligament reconstruction instruments for coronoid fixation, plates, prosthesis, external fixators, etc.).
Surgical approach and treatment strategy
In a recent paper, Mathew et al. [6] described an algorithm for the surgical management of elbow triads.
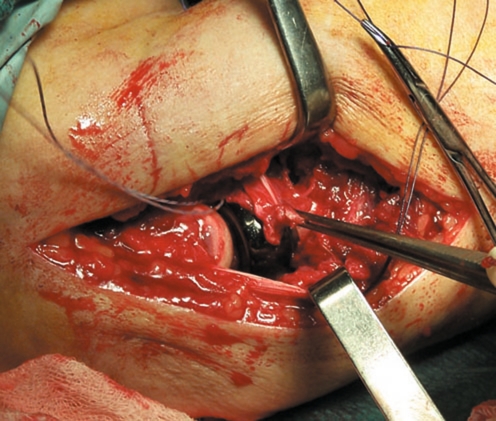
There are several ways to approach the elbow surgically. According to the recent literature, use of the unique posterior approach seems to be used most often. It allows access to both aspects lateral and medial of the elbow. However, lateral and medial approaches can also be used according to the surgeon preferences (Fig. 6). With respect to the articles reviewed, most of the surgeons employed the posterior approach, but lateral or combined approaches were also performed (Table 3).
Fig. 6.
Intraoperative photograph. Lateral approach to the elbow and radial head replacement, with reconstruction of the annular ligament. Note the suture anchor placed for the coronoid and anterior capsule attachment
Table 3.
Treatment modalities
| Author | Delay in treatment, days (range) | Surgical approach | Radial head fracture | Coronoid fracture | LCL repair | LCM repair | External fixator | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Posterior | Lateral | Lateral and Medial | Screws | Partial excision | Conservative | Prosthesis | Allograft | Screw | Capsular repair | No treatment | |||||
| Pugh et al. | 4.5 (0–17) | 8 | 26 | 2 | 13 | – | 3 | 20 | – | 18 | 18 | – | 36 | 6 | 2 |
| Egol et al. | 10 (1–36) | – | 29 | – | 8 | 3 | 3 | 15 | – | 5 | – | 24 | 29 | n/a | 13 |
| Forthman et al. | 7 (1–24) | 22 | – | – | 1 | – | – | 20 | 1 | 4 | 22 | – | 22 | n/a | – |
| Lindenhovius et al. | 6 (1–13) | 18 | – | – | 1 | – | – | 17 | – | 2 | 18 | – | n/a | n/a | – |
| Zeiders et al. | n/a | 32 | – | – | 7 | – | 6 | 18 | – | – | 32 | – | 32 | 12 | 21 |
LCL lateral collateral ligament, MCL medial collateral ligament, n/a not available
The coronoid fragment should be fixed first. After that, the radial head should be fixed or replaced, and then the lateral collateral ligament should be repaired. Intraoperative testing under fluoroscopy must show a stable and congruent joint; if not, the medial collateral ligament should be repaired. If the elbow continues to be unstable, a hinge external fixator should be applied.
If a congruent ulnohumeral joint cannot be obtained, all the previous steps should be re-evaluated.
Some authors have suggested that stability is adequate when the elbow can be extended to 45° without dislocation [37]. Others maintain that to be confident that the elbow is stable, it should be possible to extend the elbow nearly completely without redislocation [38]. Prolonged dislocation or subluxation of the elbow should be avoided, as it can damage the articular surfaces and/or lead to attenuation of the collateral ligaments requiring more complex reconstructive procedures [39].
Radial head fracture
The radial head is an important secondary stabiliser against valgus loading and posterior translation. As the medial collateral ligament is usually torn in this injury, the radial head takes on a more important role as a stabilizing structure against valgus stress.
Given the relatively young age of the patients that usually sustain these injuries, the radial head fracture should be fixed if possible. Some authors have described radial head excision for fragments <25% of the head fractures if the elbow remains stable after coronoid fixation [2, 20]. If joint instability remains, a radial head prosthesis must be used. Usually, fractures that involve more than one-third the articular surface of the radial head with >2 millimetres of displacement and any sizable comminution are replaced. For better biomechanical and biological compatibility, metal radial head implants are preferable to silicone implants [40–42].
Radial head replacement was the treatment applied in the majority of the cases in the articles reviewed (Table 3).
Coronoid fracture
Repair of a coronoid fragment is important to achieve elbow congruency and stability. Larger fragments clearly affect elbow stability. However, small fragments involving 10% of the coronoid process have been shown to have little effect on stability in cadaveric studies [43]. Whether small coronoid fragments should always be fixed remains debatable. For fractures of the tip of the coronoid, capsular repair or suture anchors can be used to prevent posterior displacement of the ulna.
Small coronoid fragments are often difficult to distinguish from fragments of the radial head. Given that these fractures are so small, it is not clear whether the substantial decrease in elbow stability can be ascribed entirely to them. The anterior aspect of the capsule is attached to this fragment [44], but anterior capsular disruption occurs with most posterior dislocations of the elbow. At a minimum, it is clear that the associated fracture of the coronoid can be a marker for diminished elbow stability. When there is doubt about the presence of a coronoid fragment, computed tomography imaging with three-dimensional reconstruction should be obtained.
The surgical management of coronoid fragments may vary according to the type of injury. For large fragments, internal fixation with screws should be performed. Fractures that involve the medial facet of the coronoid process may be best addressed by a medial exposure and fixation with a plate and screws.
With respect to the papers reviewed, Egol et al. did not repair the coronoid fragment. In the other papers, capsular repair, coronoid fixation or both were performed (Table 3).
Soft tissue injuries
The characteristic soft-tissue injury patterns seen in association with unstable elbow dislocations and fracture-dislocations have been described previously [29].
In elbow triads, the lateral collateral ligament is always torn. This ligament plays an important role in the varus stability of the elbow, especially the ulnar band, and should always be repaired. The ligament is most often detached from its insertion on the lateral epicondyle so suture anchors or transosseous sutures can be used to repair it. It is not rare for the origin of the extensor supinator muscles to be torn as well and should also be repaired because of its contribution in the dynamic stabilisation of the elbow. Defects in soft-tissue planes created by the trauma can be used to perform the surgical approach.
The lateral collateral ligament and the origin of flexor pronator muscles can be also torn. If necessary, they should be repaired. Repair of the lateral collateral ligament is described in all the studies reviewed (Table 3).
Repair of the medial collateral ligament is performed if residual instability persists.
Dynamic external fixator
After repairing all the structures, the elbow must be tested for stability. If appropriate stability is not obtained, a dynamic external fixator should be applied to allow early motion in a safe range.
An external fixator was applied in 36 of 137 patients reviewed in this study, so an external fixator should always be prepared and ready for use in case of instability.
Static external fixation or transfixation of the ulnohumeral joint can be reasonable alternatives if hinged external fixation is not possible. While excessive immobilisation can lead to a stiff elbow, this problem can be treated with a high degree of success with operative capsular release [45, 46], but chronic subluxation or dislocation of the elbow may lead to irreparable articular injury.
Postoperative care
After surgical repair, a stable and congruent joint must be obtained (Fig. 7a–b), and on the first days of the postoperative period active and active-assisted range of motion exercises including both flexion and extension can be initiated as tolerated. Some authors argue that active elbow motion following surgical repair enhances stability through the recruitment of muscle groups that act as dynamic stabilisers of the elbow [20].
Fig. 7.
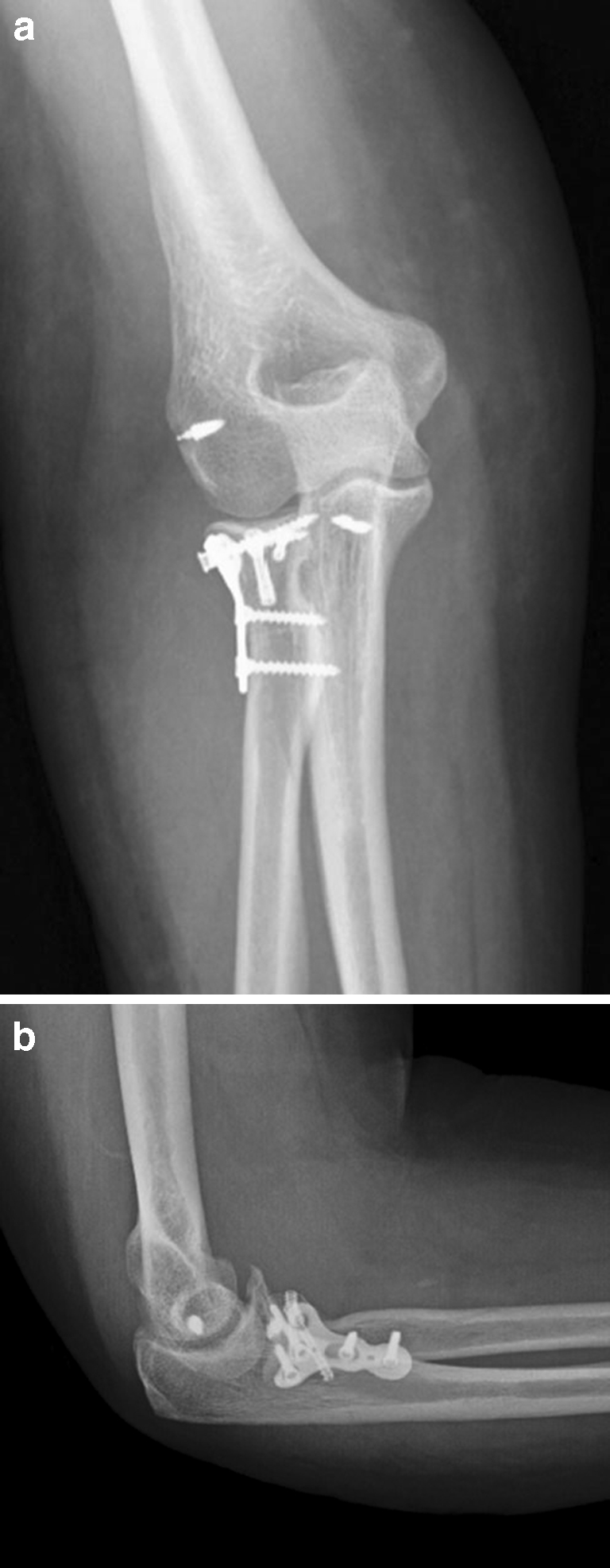
Postoperative radiographs showing joint congruency. a Anteroposterior view. b Lateral view
Functional outcomes
The functional outcomes are detailed in Tables 4 and 5.
Table 4.
Functional results (range of motion)
| Author | Flexion arc | Averaged flexion | Averaged flexion contracture | Forearm rotation | Forearm pronation | Forearm supination |
|---|---|---|---|---|---|---|
| Pugh et al. | 112° ± 11 | 131 ± 11 | 19° ± 9 | 136° ± 16 | n/a | n/a |
| Egol et al. | 109° ± 57 | n/a | n/a | 128° ± 44 | n/a | n/a |
| Forthman et al. | 117° (75–145) | 134° (100–150) | 17° (0–45) | 137° (0–180) | 75° (0–90) | 62°(0–85) |
| Lindenhovius et al. | 119° (75–145) | 135° (120–145) | 17° (0–45) | 141° (70–180) | 78°(45–90) | 63°(20–90) |
| Zeiders et al. | 100° (30–130) | 130° | 12° (0–20) | n/a | n/a | n/a |
n/a not available
Table 5.
Functional results (Broberg-Morrey and Mayo elbow performance [MEPI] scores)
| Author | Broberg-Morrey (scores and results in patients) | MEPI (scores and results in patients) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Score | Excellent | Good | Fair | Poor | Score | Excellent | Good | Fair | Poor | |
| Pugh et al. | n/a | n/a | n/a | n/a | n/a | 88(45–100) | 15 | 13 | 7 | 1 |
| Egol et al. | 77 (33–100) | 3 | 10 | 12 | 4 | 81(45–100) | 7 | 12 | 9 | 1 |
| Forthman et al. | 88 (53–100) | 6 | 11 | 3 | 2 | n/a | n/a | n/a | n/a | n/a |
| Lindenhovius et al. | 90 (64–100) | 5 | 10 | 3 | 0 | 88(65–100) | 6 | 8 | 2 | n/a |
| Zeiders et al. | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
n/a not available
At an average of 31 months of follow-up, overall flexion arc was 111.4°, average flexion 132.5°, forearm rotation 135.5°, Mayo elbow performance (MEPI) score 85.6 points, and the Broberg-Morrey score was 85 points.
Weighted outcomes for the five studies were as follows: flexion arc 110.28°, averaged flexion 131.98°, averaged flexion contracture 16.19°, forearm rotation 134.86°, forearm pronation 76.35°, forearm supination 62.45°, MEPI score 85.55 points, and Broberg-Morrey score 83.90.
According to the MEPI and Broberg-Morrey scores, the outcome in the majority of cases was rated as excellent or good.
Complications and additional procedures
Most of the complications were related to ulnar nerve symptoms, post-traumatic arthritis, elbow stiffness and heterotopic ossification. However, there was no consensus about the routine transposition of the ulnar nerve and the prevention of heterotopic ossifications with the use of postoperative radiotherapy or indometacin. Egol et al. used postoperative radiotherapy (single doses of 700cGy), and Zeidres et al. prescribed indometacin daily for three weeks after surgery.
With respect to post-traumatic arthritis, the majority of patients who developed it had symptoms of mild or moderate joint degeneration (Table 6).
Table 6.
Complications
| Author | Ulnar nerve dysfunction signs | Calcifications | Arthritis | ||||
|---|---|---|---|---|---|---|---|
| Severe | Moderate | Mild | None | Total | |||
| Pugh et al. | – | 26 | 1 | 5 | 8 | 22 | 14 |
| Egol et al. | 3 | 10 | 1 | 3 | 18 | – | 22 |
| Forthman et al. | – | – | – | 1 | 6 | – | 7 |
| Lindenhovius et al. | 4 | – | – | 3 | 9 | – | 12 |
| Zeiders et al. | n/a | 3 | n/a | n/a | n/a | n/a | n/a |
n/a not available
Additional procedures were mainly capsular release, hardware removal and secondary ulnar nerve transposition (Table 7).
Table 7.
Additional procedures
| Author | Additional procedures | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Stiffness | Secondary ulnar nerve transposition | Infection | Forearm synostosis | Instability (external fixation) | Hardware removal | Conversion fixation radial head to prosthesis | Interposition arthroplasty | Total | |
| Pugh et al. | – | – | 1 | 2 | 1 | 4 | – | – | 8 |
| Egol et al. | 2 | – | – | – | 1 | 1 | 2 | – | 6 |
| Forthman et al. | 4 | 4 | – | – | – | – | – | 1 | 9 |
| Lindenhovius et al. | 2 | 3 | 1 | – | – | – | – | – | 6 |
| Zeiders et al. | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
n/a not available
Recommendations
Limitations of this study include level of evidence III and IV of the papers reviewed. Future investigations seem advisable, especially to refine specific indications for type I coronoid fracture fixation, fixation or replacement of the radial head in partial fractures, medial collateral ligament reconstruction and benefits and indications of the hinge external fixation.
According to the recent literature about the management of elbow triads and the outcomes reported in this study, the following recommendations have been made when treating elbow triads:
Computed tomography with three dimensional reconstructions can be helpful in obtaining an appropriate diagnosis of the type of injury.
All potential material needed for reconstruction must be prepared (screws, suture anchors, plates, prosthesis, external fixators, etc.) prior to surgery.
A posterior skin incision is most widely used. It allows access to both medial and lateral aspects of the elbow.
Anterior ulnar nerve transposition can prevent postoperative ulnar nerve dysfunction symptoms.
Repair the structures from deep to superficial—coronoid process, radial head and lateral collateral ligament—using the different methods available depending on the type of injury.
Try to preserve the radial head; if not possible, a metallic radial head arthroplasty should be performed.
Assess the stability after reconstruction. If the elbow dislocates in 30–45° degrees of extension, repair the medial collateral ligament. If it persists, a dynamic external fixator must maintain stability.
Assess articular congruency. If the joint is not congruent, repeat the previous steps from point 5.
The goal of the surgery is to obtain a stable joint that allows early motion, which must be started a few days postoperatively, avoiding varus stress.
A functional elbow can be expected when using these current protocols, with an average flexion of approximately 110°.
Additional procedures may be necessary, especially for joint stiffness, removal material or ulnar nerve symptoms. Arthritis can develop but will usually be tolerated.
Acknowledgments
The authors appreciate the contribution of Mrs. Teresa M. de la Torre Aragones and Mrs. Rocio Galvez Lazcano (Infanta Leonor Hospital Library) in obtaining some of the manuscripts reviewed in this paper.
Conflict of interests The authors declare that they have no conflict of interests.
References
- 1.Ring D, Jupiter JB, Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am. 2002;84-A:547–551. doi: 10.2106/00004623-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 2.McKee MD, Pugh DM, Wild LM, Schemitsch EH, King GJ. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. Surgical technique. J Bone Joint Surg Am. 2005;87(Suppl 1):22–32. doi: 10.2106/JBJS.D.02933. [DOI] [PubMed] [Google Scholar]
- 3.Schneeberger AG, Sadowski MM, Jacob HA. Coronoid process and radial head as posterolateral rotatory stabilizers of the elbow. J Bone Joint Surg Am. 2004;86-A:975–982. doi: 10.2106/00004623-200405000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Rodriguez-Martin J, Pretell-Mazzini J, Cecilia-Lopez D, Resines-Erasun C. Medial complex elbow dislocation: an unusual pattern of injury. J Orthop Trauma. 2010;24:e21–24. doi: 10.1097/BOT.0b013e3181ad629d. [DOI] [PubMed] [Google Scholar]
- 5.Sharma H, Sibinski M, Sherlock DA. Outcome of lateral humeral condylar mass fractures in children associated with elbow dislocation or olecranon fracture. Int Orthop. 2009;33:509–514. doi: 10.1007/s00264-007-0463-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mathew PK, Athwal GS, King GJ. Terrible triad injury of the elbow: current concepts. J Am Acad Orthop Surg. 2009;17:137–151. doi: 10.5435/00124635-200903000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Chell J, Harris N. Salvage of the head of the radius after fracture-dislocation of the elbow. J Bone Joint Surg Br. 1999;81:745–746. doi: 10.1302/0301-620X.81B5.9453. [DOI] [PubMed] [Google Scholar]
- 8.Egol KA, Immerman I, Paksima N, Tejwani N, Koval KJ. Fracture-dislocation of the elbow functional outcome following treatment with a standardized protocol. Bull NYU Hosp Jt Dis. 2007;65:263–270. [PubMed] [Google Scholar]
- 9.Forthman C, Henket M, Ring DC. Elbow dislocation with intra-articular fracture: the results of operative treatment without repair of the medial collateral ligament. J Hand Surg Am. 2007;32:1200–1209. doi: 10.1016/j.jhsa.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 10.Frankle MA, Koval KJ, Sanders RW, Zuckerman JD. Radial head fractures associated with elbow dislocations treated by immediate stabilization and early motion. J Shoulder Elbow Surg. 1999;8:355–360. doi: 10.1016/S1058-2746(99)90160-X. [DOI] [PubMed] [Google Scholar]
- 11.Harrington IJ, Sekyi-Otu A, Barrington TW, Evans DC, Tuli V. The functional outcome with metallic radial head implants in the treatment of unstable elbow fractures: a long-term review. J Trauma. 2001;50:46–52. doi: 10.1097/00005373-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Judet T. Results of acute excision of the radial head in elbow radial head fracture-dislocations. J Orthop Trauma. 2001;15:308–309. doi: 10.1097/00005131-200105000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Jupiter JB, Ring D. Treatment of unreduced elbow dislocations with hinged external fixation. J Bone Joint Surg Am. 2002;84-A:1630–1635. doi: 10.2106/00004623-200209000-00017. [DOI] [PubMed] [Google Scholar]
- 14.Kalicke T, Muhr G, Frangen TM. Dislocation of the elbow with fractures of the coronoid process and radial head. Arch Orthop Trauma Surg. 2007;127:925–931. doi: 10.1007/s00402-007-0424-6. [DOI] [PubMed] [Google Scholar]
- 15.Lill H, Korner J, Rose T, Hepp P, Verheyden P, Josten C. Fracture-dislocations of the elbow joint-strategy for treatment and results. Arch Orthop Trauma Surg. 2001;121:31–37. doi: 10.1007/s004020000180. [DOI] [PubMed] [Google Scholar]
- 16.Lindenhovius AL, Jupiter JB, Ring D. Comparison of acute versus subacute treatment of terrible triad injuries of the elbow. J Hand Surg Am. 2008;33:920–926. doi: 10.1016/j.jhsa.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 17.McKee MD, Bowden SH, King GJ, Patterson SD, Jupiter JB, Bamberger HB, Paksima N. Management of recurrent, complex instability of the elbow with a hinged external fixator. J Bone Joint Surg Br. 1998;80:1031–1036. doi: 10.1302/0301-620X.80B6.8536. [DOI] [PubMed] [Google Scholar]
- 18.Nalbantoglu U, Kocaoglu B, Gereli A, Aktas S, Guven O. Open reduction and internal fixation of Mason type III radial head fractures with and without an associated elbow dislocation. J Hand Surg Am. 2007;32:1560–1568. doi: 10.1016/j.jhsa.2007.09.016. [DOI] [PubMed] [Google Scholar]
- 19.Popovic N, Gillet P, Rodriguez A, Lemaire R. Fracture of the radial head with associated elbow dislocation: results of treatment using a floating radial head prosthesis. J Orthop Trauma. 2000;14:171–177. doi: 10.1097/00005131-200003000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Pugh DM, Wild LM, Schemitsch EH, King GJ, McKee MD. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am. 2004;86-A:1122–1130. doi: 10.2106/00004623-200406000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Ring D, Hannouche D, Jupiter JB. Surgical treatment of persistent dislocation or subluxation of the ulnohumeral joint after fracture-dislocation of the elbow. J Hand Surg Am. 2004;29:470–480. doi: 10.1016/j.jhsa.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 22.Ruch DS, Triepel CR. Hinged elbow fixation for recurrent instability following fracture dislocation. Injury. 2001;32(Suppl 4):SD70–SD78. doi: 10.1016/s0020-1383(01)00113-9. [DOI] [PubMed] [Google Scholar]
- 23.Sanchez-Sotelo J, Romanillos O, Garay EG. Results of acute excision of the radial head in elbow radial head fracture-dislocations. J Orthop Trauma. 2000;14:354–358. doi: 10.1097/00005131-200006000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Stavlas P, Gliatis J, Polyzois V, Polyzois D. Unilateral hinged external fixator of the elbow in complex elbow injuries. Injury. 2004;35:1158–1166. doi: 10.1016/j.injury.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 25.Yu JR, Throckmorton TW, Bauer RM, Watson JT, Weikert DR. Management of acute complex instability of the elbow with hinged external fixation. J Shoulder Elbow Surg. 2007;16:60–67. doi: 10.1016/j.jse.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 26.Zilkens C, Graf M, Anastasiadis A, Smajic S, Muhr G, Kalicke T. Treatment of acute and chronic elbow instability with a hinged external fixator after fracture dislocation. Acta Orthop Belg. 2009;75:167–174. [PubMed] [Google Scholar]
- 27.Jeon IH, Oh CW, Kyung HS, Park BC, Kim PT, Ihn JC. Functional outcome after operative treatment of eight type III coronoid process fractures. J Trauma. 2005;59:418–423. doi: 10.1097/01.ta.0000174734.23193.e0. [DOI] [PubMed] [Google Scholar]
- 28.Josefsson PO, Gentz CF, Johnell O, Wendeberg B. Dislocations of the elbow and intraarticular fractures. Clin Orthop Relat Res. 1989;246:126–130. [PubMed] [Google Scholar]
- 29.McKee MD, Schemitsch EH, Sala MJ, O’Driscoll SW. The pathoanatomy of lateral ligamentous disruption in complex elbow instability. J Shoulder Elbow Surg. 2003;12:391–396. doi: 10.1016/S1058-2746(03)00027-2. [DOI] [PubMed] [Google Scholar]
- 30.Pai V. Use of suture anchors for coronoid fractures in the terrible triad of the elbow. J Orthop Surg (Hong Kong) 2009;17:31–35. doi: 10.1177/230949900901700108. [DOI] [PubMed] [Google Scholar]
- 31.Rodgers WB, Kharrazi FD, Waters PM, Kennedy JG, McKee MD, Lhowe DW. The use of osseous suture anchors in the treatment of severe, complicated elbow dislocations. Am J Orthop. 1996;25:794–798. [PubMed] [Google Scholar]
- 32.Terada N, Yamada H, Seki T, Urabe T, Takayama S. The importance of reducing small fractures of the coronoid process in the treatment of unstable elbow dislocation. J Shoulder Elbow Surg. 2000;9:344–346. doi: 10.1067/mse.2000.106082. [DOI] [PubMed] [Google Scholar]
- 33.Zeiders GJ, Patel MK. Management of unstable elbows following complex fracture-dislocations-the “terrible triad” injury. J Bone Joint Surg Am. 2008;90(Suppl 4):75–84. doi: 10.2106/JBJS.H.00893. [DOI] [PubMed] [Google Scholar]
- 34.Geissler WB, Freeland AE. Radial head fracture associated with elbow dislocation. Orthopedics. 1992;15:874–877. doi: 10.3928/0147-7447-19920701-13. [DOI] [PubMed] [Google Scholar]
- 35.O’Driscoll SW, Jupiter JB, Cohen MS, Ring D, McKee MD. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52:113–134. [PubMed] [Google Scholar]
- 36.Micic I, Kim SY, Park IH, Kim PT, Jeon IH. Surgical management of unstable elbow dislocation without intra-articular fracture. Int Orthop. 2009;33:1141–1147. doi: 10.1007/s00264-008-0624-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Morrey BF. Complex instability of the elbow. Instr Course Lect. 1998;47:157–164. [PubMed] [Google Scholar]
- 38.Ring D, Jupiter JB. Fracture-dislocation of the elbow. J Bone Joint Surg Am. 1998;80:566–580. doi: 10.1302/0301-620X.80B4.9165. [DOI] [PubMed] [Google Scholar]
- 39.Ring D, Jupiter JB. Reconstruction of posttraumatic elbow instability. Clin Orthop Relat Res. 2000;370:44–56. doi: 10.1097/00003086-200001000-00006. [DOI] [PubMed] [Google Scholar]
- 40.King GJ, Zarzour ZD, Rath DA, Dunning CE, Patterson SD, Johnson JA. Metallic radial head arthroplasty improves valgus stability of the elbow. Clin Orthop Relat Res. 1999;368:114–125. doi: 10.1097/00003086-199911000-00014. [DOI] [PubMed] [Google Scholar]
- 41.Moro JK, Werier J, MacDermid JC, Patterson SD, King GJ. Arthroplasty with a metal radial head for unreconstructible fractures of the radial head. J Bone Joint Surg Am. 2001;83-A:1201–1211. doi: 10.2106/00004623-200108000-00010. [DOI] [PubMed] [Google Scholar]
- 42.Vanderwilde RS, Morrey BF, Melberg MW, Vinh TN. Inflammatory arthritis after failure of silicone rubber replacement of the radial head. J Bone Joint Surg Br. 1994;76:78–81. [PubMed] [Google Scholar]
- 43.Beingessner DM, Stacpoole RA, Dunning CE, Johnson JA, King GJ. The effect of suture fixation of type I coronoid fractures on the kinematics and stability of the elbow with and without medial collateral ligament repair. J Shoulder Elbow Surg. 2007;16:213–217. doi: 10.1016/j.jse.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 44.Cage DJ, Abrams RA, Callahan JJ, Botte MJ. Soft tissue attachments of the ulnar coronoid process. An anatomic study with radiographic correlation. Clin Orthop Relat Res. 1995;320:154–158. [PubMed] [Google Scholar]
- 45.Cohen MS, Hastings H., 2nd Post-traumatic contracture of the elbow. Operative release using a lateral collateral ligament sparing approach. J Bone Joint Surg Br. 1998;80:805–812. doi: 10.1302/0301-620X.80B5.8528. [DOI] [PubMed] [Google Scholar]
- 46.Mansat P, Morrey BF. The column procedure: a limited lateral approach for extrinsic contracture of the elbow. J Bone Joint Surg Am. 1998;80:1603–1615. [PubMed] [Google Scholar]