Abstract
The aim of this study was to evaluate the outcome of joint arthroplasty in obese and non-obese patients. We reviewed 2,026 consecutive primary total hip and 535 primary total knee arthroplasties performed for osteoarthritis. Patients were separated into two groups according to their body mass index (BMI): non-obese (BMI < 30) and obese (BMI ≥ 30). Their survivorships were compared. Case controlled studies were performed with 134 hip and 50 knee arthroplasties in obese patients. Each was matched individually with a control and their outcome compared. Log rank tests for equality of survival showed no difference in the survival for hip and knee arthroplasty at 11 and ten years, respectively. The obese group had significantly lower postoperative hip and knee scores at latest follow-up, especially in the range of motion. Overall patient satisfaction scores were comparable. There were no significant differences in the radiographic analysis of both hip and knee implants. Revision was used as an end point for the survival analysis. Functional scores (Harris hip score and Hospital for Special Surgery knee score), satisfaction for surgery and radiographic features were used as outcome measures for comparison. The mid-term survival of total hip and knee arthroplasty is not adversely affected by obesity. Despite lower clinical scores, the obese patients were satisfied with the results of their surgery and have an equivalent mid-term survival rate. It would be unreasonable to deny patients arthroplasty surgery purely on the basis of a BMI indicating obesity.
Introduction
There is an increasing awareness of the rise in obesity levels and it has been described as now reaching epidemic proportions. Obesity is defined by The World Health Organisation [1] as having a body mass index (BMI) in excess of 30 kg/m2 and the impact that this will have on the health of future generations remains the subject of much debate. Australian data from National Health Surveys (NHS) has revealed an increase in the overall percentage of adults classified as obese from 11.1% in 1995 to 16.4% in 2005 [2]. This suggests that more than a third of the population here will be obese by 2015. These numbers are even more striking in the 55–64 age group as they show the highest combined rates of overweight and obesity—79% of males and 58% of females. Based on these data from the NHS, it has been estimated that over 52% of all people with osteoarthritis were in this age bracket and amongst this population 43% were obese [3]. The effect of this will have a significant impact on health economics. A more recent Australian report had estimated the economic cost of osteoarthritis due to obesity would reach AUD$5.7 billion in 2008 (from AUD$2 billion in 2005) including the net financial cost as well as cost of lost well-being [4]. A North American unit demonstrated that this trend has meant that the percentage of their patients having hip and knee arthroplasty who are classified as obese has risen from 24.3% in 1990 to 51.0% in 2005 [5]. Their average BMI during this same time period rose from 27.8 to 31.3. A recent study from the United Kingdom demonstrated a significant correlation between a lower age at joint replacement surgery and an increasing BMI [6]. It is a reasonable assumption that this increased load will result in greater forces across the implant–bone interface and could lead to premature wear, loosening of the prosthesis and hence increased failure rates. Therefore, it is clear that there is a real need to determine the role that obesity will play on the survival and outcome of arthroplasty.
The aim of our study was to investigate the mid-term survival, clinical and radiological outcome of patients with high BMI undergoing primary arthroplasty surgery, and to review the recent literature of arthroplasty in obese patients.
Materials and methods
We evaluated 2,026 consecutive primary total hip replacements (THR) and 535 consecutive primary total knee replacements (TKR) between 1995 and 2006. All procedures took place in a single institution and surgery was performed by one of two senior arthroplasty surgeons. All patients had a diagnosis of osteoarthritis, received cementless implants and then followed a standardised postoperative regime.
The patient’s BMI was calculated at their pre-operative assessment [weight (kg) / height2 (m)]. Patients were then separated into non-obese (BMI < 30) and obese (BMI ≥ 30) groups. No individual was lost to follow -up with regard to implant survival, and all were included in the survival study. A case controlled study was subsequently performed retrospectively on the prospectively collected data on all obese patients with a suitable match, with a minimum of two years follow-up. One hundred and thirty-four THR cases were individually matched for age (within one year), side, surgeon, acetabular component, bearing configuration and the time to their latest follow-up (within one year). Fifty TKR cases were matched for age (within five years), sex, side, surgeon and time to follow-up (within one year).
In our unit, patient demographics, operative details and the results of clinical and radiographical assessments are prospectively collected and recorded as part of routine arthroplasty follow-up. The assessing surgeons are unaware of any particular study. Clinical outcome was assessed using the modified Harris hip score (HHS) and the Hospital for Special Surgery knee rating score (HSSKS), which are validated scoring systems to reflect the functional ability of the joints. In addition, postoperative range of motion was separately evaluated along with a satisfaction with surgery question scored on a visual analogue scale out of a maximum of 10. Radiographs of hips and knees were sequentially and prospectively evaluated by an independent surgeon blinded to the patients BMI and who were not involved in the initial surgery. The TKR’s were scored for osteolysis, radiolucent lines and alignment. The THR’s were evaluated for radiolucent lines, osteolytic lesions, acetabular inclination, as well as the presence of femoral cortical hypertrophy, stress shielding, endosteal spot welds, the degree of bony ingrowth and alignment.
Data analysis was performed using the SPSS software (SPSS Inc., Chicago, Illinois, USA). Results were compared using a combination of the paired two tailed t-tests, Fisher’s exact test and the Chi square test with a significance level set at 0.05. Survival data were investigated with a log rank test for equality of survivorship with Kaplan-Meier curves generated using revision for any reason as the end point.
Results
The demographic details of all 2026 THR’s and 535 TKR’s are illustrated in Table 1. The mean age of the obese patients undergoing arthroplasty in our population was an average five years younger (p < 0.001). There was no significant difference in the proportions of males and females undergoing THR but in the TKR patients there was a significantly higher proportion of females in the obese group (p < 0.05). The mean BMI of all patients undergoing a TKR was higher those having a THR (p < 0.001).
Table 1.
Demographic details for all hip and knee arthroplasty patients
| Demographic | All patients | Non-obese | Obese | ||||
|---|---|---|---|---|---|---|---|
| THR | TKR | THR | TKR | THR | TKR | ||
| Total, n | 2,026 | 535 | 1,612 | 382 | 414 | 153 | |
| Male | 47% | 39% | 47% | 42% | 48% | 30% | |
| Female | 53% | 61% | 53% | 58% | 52% | 70% | |
| Mean age (y) | 67 | 71 | 68 | 72 | 63 | 67 | |
| SD age (y) | 10.3 | 9.0 | 9.9 | 8.4 | 10.0 | 9.6 | |
| Mean follow-up (y) | 6.3 | 9.2 | 6.4 | 9.2 | 6.1 | 9.4 | |
| SD follow-up (y) | 2.5 | 2.5 | 2.5 | 2.4 | 2.6 | 2.5 | |
| Mean BMI | 26.8 | 28.0 | 25.0 | 25.2 | 33.8 | 34.5 | |
| SD BMI | 4.7 | 5.2 | 2.8 | 2.7 | 3.6 | 4.0 | |
THR total hip replacements, TKR total knee replacements, SD standard deviation, BMI body mass index
The case-controlled study patient details are shown in Table 2 and the clinical score results in Tables 3 and 4. There were significant differences in the total HHS and HSSKS, in the non-obese group showing higher mean total scores (p < 0.001, p < 0.05). With regards to the THR group, there were significantly better scores for the non-obese in all the individual score parameters apart from pain. In addition, the independently assessed range of motion also showed significant better hip flexion, adduction and internal rotation in the non-obese group. There was no difference in abduction or external rotation. In the TKR group, the scores for the non-obese were significantly better in the range of motion and functional score components. Independently assessed knee flexion was also significantly better in the non-obese. There was no statistical difference in the patients reported overall satisfaction with surgery for either THR or TKR.
Table 2.
Demographics of the hip and knee case controlled study groups
| Demographics | THR | TKR | |||
|---|---|---|---|---|---|
| Non-obese | Obese | Non-obese | Obese | ||
| Total number, n | 134 | 134 | 50 | 50 | |
| Male | 57 | 57 | 12 | 12 | |
| Female | 77 | 77 | 38 | 38 | |
| Mean age | 64 | 64 | 69 | 69 | |
| SD age | 8.0 | 8.0 | 5.5 | 5.9 | |
| Age range | 44–79 | 43–79 | 51–81 | 55–81 | |
| Mean follow-up | 5.1 | 5.1 | 7.4 | 7.2 | |
| SD follow-up | 1.6 | 1.6 | 1.9 | 1.9 | |
| Range follow-up | 2–10.3 | 2–10.1 | 3.5–12.0 | 3.1–11.5 | |
| Mean BMI | 25.0 | 33.4 | 25.2 | 34.1 | |
| SD BMI | 2.6 | 2.9 | 3.2 | 3.8 | |
| BMI range | 18–29.9 | 30–47.8 | 18–29.9 | 30–46.7 | |
THR total hip replacements, TKR total knee replacements, SD standard deviation, BMI body mass index
Table 3.
Postoperative clinical scores for the hip case controlled groups
| Harris hip score | Non-obese | Obese | Significance |
|---|---|---|---|
| Total | 93.2 | 89.9 | p < 0.001 |
| Pain | 42.3 | 41.8 | ns |
| Function | 31.0 | 29.6 | p = 0.006 |
| Activities | 11.7 | 10.6 | p < 0.001 |
| Range of motion | 8.2 | 7.9 | p = 0.020 |
| Hip flexion | 122 | 113 | p < 0.001 |
| Abduction | 32.5 | 31.0 | ns |
| Adduction | 25.2 | 23.2 | p = 0.011 |
| External rotation | 23.6 | 24.7 | ns |
| Internal rotation | 14.0 | 11.2 | p = 0.008 |
| Satisfaction score/10 | 9.3 | 9.0 | ns |
Reproduced with permission and copyright of the British Editorial Society of Bone and Joint Surgery [Jackson MP, Sexton SA, Yeung E, et al.: The effect of obesity on the mid-term survival and clinical outcome of cementless total hip replacement. J Bone Joint Surg Br 91(10): 1296–1300, 2009]
Table 4.
Postoperative clinical scores for the knee case-controlled groups
| Hospital for Special Surgery score | Non-obese | Obese | Significance |
|---|---|---|---|
| Total | 87.4 | 83.8 | p < 0.05 |
| Pain | 27.3 | 26.8 | ns |
| Function | 16.7 | 15 | p < 0.01 |
| Examination | 29.2 | 29.1 | ns |
| Range of motion | 14.6 | 13.4 | p < 0.01 |
| Maximum knee flexion | 120° | 112° | p < 0.05 |
| Satisfaction score /10 | 9.4 | 8.8 | ns |
Radiographic analysis also revealed no significant differences between the two groups in the evaluation of the appearances of the hip and knee implants.
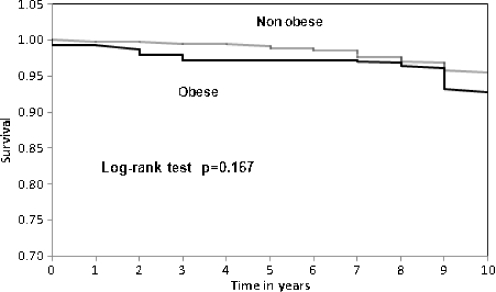
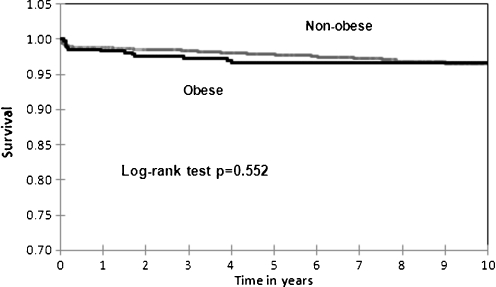
There were 82 deaths during the follow-up period, and 13 revisions for all reasons in the TKR group. KM survival analysis comparing the two groups with the end point as revision for any reason showed no significant difference between the groups (log rank test p = 0.167; Fig. 1). This demonstrates a cumulative estimated survival rate at ten years of 96.4% in the obese (standard error 1.6) and 98% in the non-obese (standard error 0.7) groups. The analysis of the patients with THR at ten years is shown in Fig. 2. With the end point as revision for any reason it showed no significant differences between the groups (log rank test p = 0.552). The estimated chance of THR implant survival at 11 years for the non-obese group is 95.2% (standard error 1.4) and for the obese 96.7% (standard error 0.9).
Fig. 1.
Kaplan-Meier survival curve for the knee arthroplasty in obese and non-obese groups. Reproduced with permission and copyright of the British Editorial Society of Bone and Joint Surgery [Jackson MP, Sexton SA, Walter WL, et al.: The impact of obesity on the mid-term outcome of cementless total knee replacement. J Bone Joint Surg Br 91(8):1044–8, 2009]
Fig. 2.
Kaplan-Meier survival curve for the hip arthroplasty in obese and non-obese groups. Reproduced with permission and copyright of the British Editorial Society of Bone and Joint Surgery [Jackson MP, Sexton SA, Yeung E, et al.: The effect of obesity on the mid-term survival and clinical outcome of cementless total hip replacement. J Bone Joint Surg Br 91(10):1296–1300, 2009]
Discussion
Total hip and knee arthroplasty has proved to be a reliable and successful procedure for thousands of individuals over the last few decades. Recent figures have shown that the prevalence of osteoarthritis and obesity are increasing in the younger age group [2, 3, 7]. There also appears to be an association between both the presence and the degree of obesity with the relative risk of subsequent hip arthroplasty [8]. A more recent study has shown more specifically that the adiposity is a good measure in predicting the risk of joint arthroplasty, especially in the knee [9].
We have demonstrated, in the largest survival analysis to date, that there is no significant difference between the non-obese and obese groups in midterm survival with both groups of patients achieving over 95% survival rates at 11 years. We believe this to be an important result as it strengthens the opinion that the obese patient should not be denied surgery purely on the basis of their obesity. There are two other studies that have looked at the longer-term survival of hips in obese patients. Haverkamp et al. reported no influence of obesity on the ten-year survival rates for cemented THR [10]. McLaughlin and Lee studied cementless THRs followed for a mean of 14.5 years and noted no differences in outcome [11]. However, both these studies were performed on relatively small groups of 411 and 260 patients, respectively. Survival studies in TKR, however, have shown rather varied results. Spicer et al. found that the ten-year survival figures and revision rates between obese and non-obese had been similar [12], whilst a demographic study with a ten-year follow up found a significant decrease in survival in an obese group [13]. A study by Foran et al. revealed similar implant survival between obese and non-obese groups up to 60–80 months, after which survival of the obese group was significantly decreased [14]. The same group also published results of a longer-term study in which the survival figures up to 14 years were comparable; but after that there were more failures in the obese group, though this was not statistically significant [15].
We were able to review a large group of obese and non-obese patients who were closely matched to reduce potential confounding variables. The results show that the obese patients achieved a lower clinical score and range of movement after surgery. In the hip replacement group, all final components of the HHS were significantly reduced in the obese apart from pain. The post surgical HSS knee score, function and range of movement for the TKR group were also shown to be significantly lower in the obese group. It is reasonable to assume that this difference of reduced range of motion is secondary to the soft tissue apposition occurring in extreme positions. This reduced range of motion is likely to have an impact on the function and activity scores. Despite these, however, the overall satisfaction with surgery is equivalent. This finding is supported by a recent study which has a similar conclusion that despite a lower clinical score, patients are still very satisfied with the procedure in the long term [16]. Apart from physical limitation, obesity has also been shown to have broad associations with conditions detrimental to health which may adversely influence the functional score. These include depression, chronic fatigue, insomnia and pain [17]. The reasons for the effect on the hip and knee score after surgery are therefore not entirely clear and it is likely to be a complex relationship.
The comprehensive radiographic assessment of the THR cohort revealed no significant differences between the obese and non-obese groups. This should mean that we can expect similar long-term survival with good osteo-integration of the cementless implants. In addition, with the predominant use of ceramic bearings, wear debris and aseptic loosening is expected to be minimal [18]. The radiographic analysis of the TKR cohort also demonstrates that there is no difference between patient groups with regards to any findings suggestive of impending implant failure or malalignment, which has been suggested to predispose to aseptic loosening [19]. Again the continued survivorship is expected to remain similar. In the future we may expect more revisions in the obese group secondary to wear due to the increased load, as one study has shown that the odds of stem loosening in THR is increased with weight [20]. However, it has been suggested that there is increased wear in the non-obese due to their trend towards higher activity levels; and that the obese tend to have a much reduced activity level [21] which will counteract any higher joint forces from increased load.
Several studies have examined the early outcomes and peri-operative complication rates in obese and non-obese patients. There is little evidence from these to suggest that the obese patient is at significantly increased risk of early postoperative complications. Moran et al. [22] looked at 800 cemented implants and found no relationship between BMI and complication rates. A large study on 1,207 THRs has, however, found a higher rate of infection independent of medical comorbidities such as diabetes mellitus at a follow up of one year in obese patients [23]. Others have found associations with prolonged wound drainage and infection only in patients with morbid obesity (BMI ≥ 40) with no other significant increases in complications up to one year following surgery [24]. But the study numbers of the obese are all small, and their significance is debatable. One more recent study did show that obesity is associated with an increased risk of postoperative pulmonary embolus (PE) after hip or knee arthroplasty, but there are a number of co-factors amongst those who were diagnosed to have PE [25].
The literature on the clinical and radiographic outcome in relation to obesity is limited. Several short-term follow-up studies have failed to show a significant difference between their non-obese and obese groups in both hip or knee replacements [26, 27]. Moran et al. found a lower HHS in their obese group at six and 18 months but no difference in Short Form 36 scores [22]. A medium-term study (five years) by Andrew et al. reported no differences in their measured clinical outcomes and radiographic analysis of 1,421 cemented hips [28]. They did not perform a survival analysis. This study also has considerable limitations with incomplete data for 25.5% and all the confounding variables attached to a multi-centre trial (different hospitals, surgeons, approaches, acetabular implants, bearings, assessors). Amin et al. showed that the clinical outcome of knee replacement at five years is comparable in obese and non-obese groups [29]. But in the morbidly obese group (BMI > 40), the functional score, complication rate and survivorship were shown to be significantly inferior compared to the non-obese; although the improvement from pre-op to post-op are comparable. However, this result only applies to a very small subset of joint replacement, and the groups were not matched by other co-morbidity; thus the poor outcome may be due to other confounding factors as well as obesity. It is therefore difficult to assess the true impact of obesity on their results.
We do not wish to underestimate the challenges still presented by the obese patient with regard to patient handling, nursing care, surgical exposure and the management of comorbidities. However, our study has shown that there would appear to be no justification to withhold hip and knee arthroplasty surgery because of concerns regarding long-term outcome. The patient can therefore be counselled that despite a lower clinical score, they can expect equivalent implant survival and satisfaction with surgery.
Acknowledgments
Conflict of interest The arthroplasty fellows (first three authors) received grants from a research fund contributed by DePuy (Johnson & Johnson) and Stryker.Dr. Bernard Zicat received royalties for implant design from DePuy (Johnson & Johnson).Dr. William L Walter received royalties and/or payment for intellectual property from Finsbury and Stryker.Dr. William K Walter received royalties and/or payment for intellectual property from DePuy (Johnson & Johnson) and Stryker.
Contributor Information
Eric Yeung, Email: ericyeung259@yahoo.co.uk.
Mark Jackson, Email: mrmark.jackson@btinternet.com.
Shaun Sexton, Email: shaunsexton@doctors.org.uk.
William Walter, Email: bill.walter@hipknee.com.au.
Bernard Zicat, Email: bzicat@sogm.com.au.
William Walter, Email: wkwalter@sogm.com.au.
References
- 1.World Health Organisation (2006). Obesity and overweight. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/index.html. Accessed September 2009
- 2.Australian Bureau of Statistics (2006) National health survey 2004–2005. Available from: http://www.aihw.gov.au/publications/aus/ah06/ah06-c07.pdf. Accessed September 2009
- 3.Access Economics (2006) The economic costs of obesity. Report for Diabetes Australia, Canberra. Available from: www.accesseconomics.com.au/publicationsreports/showreport.php?id=102. Accessed September 2009
- 4.Access Economics (2008) The growing cost of obesity in 2008: three years on. Canberra: Diabetes Australia. Available from: www.accesseconomics.com.au/publicationsreports/showreport.php?id=172. Accessed September 2009
- 5.Fehring TK, Odum SM, Griffin WL, Bohannon Mason J, McCoy TH (2007) The obesity epidemic. It’s effect on total joint arthroplasty. J Arthroplasty 22(6)suppl 2:71–76 [DOI] [PubMed]
- 6.Changulani M, Kalairajah Y, Peel T, Field RE. The relationship between obesity and the age at which hip and knee replacement is undertaken. J Bone Joint Surg Br. 2008;90-B:360–363. doi: 10.1302/0301-620X.90B3.19782. [DOI] [PubMed] [Google Scholar]
- 7.Harms S, Larson R, Sahmoun AE, Beal JR. Obesity increases the likelihood of total joint replacement surgery among younger adults. Int Orthop. 2007;31(1):23–26. doi: 10.1007/s00264-006-0130-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bourne R, Mukhi S, Zhu N, Keresteci M, Marin Role of obesity on the risk for total hip or knee arthroplasty. Clin Orth. 2007;465:185–188. doi: 10.1097/BLO.0b013e3181576035. [DOI] [PubMed] [Google Scholar]
- 9.Wang Y, Simpson JA, Wluka AE, Teichtah AJ, English DR, Giles GG, Graves S, Cicuttini FM. Relationship between body adiposity measures and risk of primary knee and hip replacement for osteoarthritis: a prospective cohort study. Arthitis Res Ther. 2009;11(2):R31. doi: 10.1186/ar2636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haverkamp D, Man HR, Jong PT, Stralen RA, Marti RK. Is the long-term outcome of cemented THA jeopardized by patients being overweight? Clin Orth. 2008;466:1162–1168. doi: 10.1007/s11999-008-0129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McLaughlin JR, Lee KR. The outcome of total hip replacement in obese and non-obese patients at 10 to 18 years. J Bone Joint Surg Br. 2006;88-B:1286–1292. doi: 10.1302/0301-620X.88B10.17660. [DOI] [PubMed] [Google Scholar]
- 12.Spicer DD, Pomeroy DL, Badenhausen WE, Schaper LA, Jr, Curry JI, Suthers KE, Smith MW. Body mass index as a predictor of outcome in total knee replacement. Int Orthop. 2001;25(4):246–249. doi: 10.1007/s002640100255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vazquez-Vela Johnson G, Worland RL, Keenan J, Norambuena N.Patient demographics as a predictor of the 10 year survival rate in primary total knee replacement J Bone Joint Surg Br 2008903360–363. 10.1302/0301-620X.90B3.1978218310761 [DOI] [Google Scholar]
- 14.Foran JRH, Mont MA, Etienne G, Jones LC, Hungerford DS. The outcome of total knee arthroplasty in obese patients. J Bone Joint Surg. 2004;86-A(8):1609–1615. doi: 10.2106/00004623-200408000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Foran JRH, Mont MA, Rajadhyaksha AD, Jones LC, Etienne G, Hungerford DS. Total knee arthroplasty in obese patients. A comparison with a matched control group. J Arthroplasty. 2004;19(7):817–824. doi: 10.1016/j.arth.2004.03.017. [DOI] [PubMed] [Google Scholar]
- 16.Núñez M, Lozano L, Núñez E, Segur JM, Sastre S, Maculé F, Ortega R, Suso S. Total knee replacement and health-related quality of life: factors influencing long-term outcomes. Arthritis Rheum. 2009;61(8):1062–1069. doi: 10.1002/art.24644. [DOI] [PubMed] [Google Scholar]
- 17.Patterson RE, Frank LL, Kristal AR, White E. A comprehensive examination of health conditions associated with obesity in older adults. Am J Prev Med. Dec. 2004;27(5):385–390. doi: 10.1016/j.amepre.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 18.Lusty PJ, Tai CC, Sew-Hoy RP, Walter WL, Walter WK, Zicat BA. Third-generation alumina-on-alumina ceramic bearings in cementless total hip arthroplasty. J Bone Joint Surg Am. Dec. 2007;89(12):2676–2683. doi: 10.2106/JBJS.F.01466. [DOI] [PubMed] [Google Scholar]
- 19.Werner FW, Ayers DC, Maletsky LP, Rullkoetter PJ. The effect of valgus/varus malalignment on load distribution in total knee replacements. J Biomech. 2005;38:349–355. doi: 10.1016/j.jbiomech.2004.02.024. [DOI] [PubMed] [Google Scholar]
- 20.Röder C, Eggli S, Münger P, Melloh M, Busato A. Patient characteristics differently affect early cup and stem loosening in THA: a case-control study on 7,535 patients. Int Orthop. 2008;32(1):33–38. doi: 10.1007/s00264-006-0291-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McClung CD, Zahiri CA, Higa JK, Amstutz HC, Schmalzried TP. Relationship between body mass index and activity in hip and knee arthroplasty patients. J Orthop Res. 2000;18:35–39. doi: 10.1002/jor.1100180106. [DOI] [PubMed] [Google Scholar]
- 22.Moran M, Walmsley P, Gray A, Brenkel IJ. Does body mass index affect the early outcome of primary total hip arthroplasty? J Arthroplasty. 2005;20(7):866–869. doi: 10.1016/j.arth.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 23.Dowsey MM, Choong PFM. Obesity is a major risk factor for prosthetic infection after primary hip arthroplasty. Clin Orth. 2008;466:153–158. doi: 10.1007/s11999-007-0016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Patel VP, Walsh M, Sehgal B, Preston C, DeWal H, Cesare PE. Factors associated with prolonged wound drainage after primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89-A:33–38. doi: 10.2106/JBJS.F.00163. [DOI] [PubMed] [Google Scholar]
- 25.Memtsoudis SG, Besculides MC, Gaber L, Liu S, González Della Valle A. Risk factors for pulmonary embolism after hip and knee arthroplasty: a population-based study. Int Orthop. 2009;33(6):1739–1745. doi: 10.1007/s00264-008-0659-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chan CLH, Villar RN. Obesity and quality of life after primary hip arthroplasty. J Bone Joint Surg Br. 1996;78-B:78–81. [PubMed] [Google Scholar]
- 27.Deshmukh RG, Hayes JH, Pinder IM. Does body weight influence outcome after total knee arthroplasty? A 1-year analysis. J Arthroplasty. 2002;17(3):315–319. doi: 10.1054/arth.2002.30776. [DOI] [PubMed] [Google Scholar]
- 28.Andrew JG, Palan J, Kurup HV, Gibson P, Murray DW, Beard DJ. Obesity in total hip replacement. J Bone Joint Surg Br. 2008;90-B:424–429. doi: 10.1302/0301-620X.90B4.20522. [DOI] [PubMed] [Google Scholar]
- 29.Amin AK, Patton JT, Cook RE, Brenkel IJ. Does obesity influence the clinical outcome at five years following total knee replacement for osteoarthritis? J Bone Joint Surg Br. 2006;88-B:335–340. doi: 10.1302/0301-620X.88B3.16488. [DOI] [PubMed] [Google Scholar]