Abstract
We evaluated the results of patients with Gustilo types II, IIIA and IIIB open tibial fractures managed early with the Ilizarov external fixator (IEF). Sixty patients (51 males, nine females; age range 20–62 years; mean age 32.8 years) with type II (11 patients), type IIIA (13) and type IIIB (36) tibial diaphyseal fractures underwent emergency debridement and minimal bone fixation (with external fixator), followed by definite fixation with the IEF after three to five days. Average duration of the hospital stay was 8.6 days. All fractures united with an average union time of 21.1 weeks (standard deviation [SD] 3.18) in type II, 21.7 weeks (SD 3.57) in IIIA and 24. 9 weeks (SD 5.14) in IIIB fractures. The difference between union time in type II and IIIA was not significant (p > 0.05), but that between IIIA (and also type II) and IIIB was significant (p < 0.05). The healing index in patients who underwent lengthening was 1.5 months/cm. The wounds in 27 patients were managed by delayed primary closure, in 19 patients with second intent (all IIIB), in 11 patients with skin grafting (mostly type IIIB fractures) and in three patients with musculocutaneous flaps. The most common complications of the procedure were pin tract infection and pain at the fracture site. Most of the patients were able to achieve good knee and ankle range of motion. Early application of the Ilizarov fixator constitutes an excellent management of open tibial fractures, especially types II, IIIA and IIIB, due to good functional and radiological results. Despite the technical difficulties and some complications (which are mostly minor) IEF may be the preferred method in open tibial fractures, especially types II and III.
Introduction
The tibia is the most commonly fractured long bone. Owing to its location and the tenuous soft tissue coverage, open fractures are more common in the tibia than in any other bone [1]. Open tibial fractures are showing an increasing trend due to road traffic accidents and firearm injuries. The situation is all the more alarming in developing countries such as India where the industrial safety norms are ignored and the traffic management is poor.
Despite its frequency, the ideal management of open tibial fractures remains controversial. Modern day management of this injury has focussed on thorough debridement and immediate bony stabilisation with tissue cover to enable early mobilisation and restoration of optimum function [2]. Plate fixation and the conventional half-pin fixators are associated with high rates of non-union and the need for secondary procedures [3]. In the developed countries, primary debridement and intramedullary nailing is now increasingly becoming the preferred treatment of these fractures. However, in developing countries such as India, where the patients present late to the hospitals and adequate facilities (in terms of manpower and theatre facilities) are not always available, the situation is different. In our hospital, as in most centres in the less developed regions, open tibial fractures have been traditionally managed by external fixators. The high rate of failure associated with this management protocol made us to look to the Ilizarov external fixator (IEF) as an alternative. IEF is a step forward in the management of open tibial fractures in the settings where patients present late, have bone loss, and facilities for emergency nailing are not available. The IEF is a minimally invasive method which permits effective wound management, early weight bearing and bone lengthening. This study looks at the role of early IEF as definitive management in open tibial fractures in a developing country.
Materials and methods
The hospital-based prospective study of compound tibial diaphyseal fractures managed with early Ilizarov external fixator (IEF) was carried out in the Bone & Joint Hospital of the Govt. Medical College, Srinagar between July 2004 and August 2007. The study protocol was approved by the Hospital Ethics Committee and an informed consent was obtained from all patients. Gustilo-Anderson types II, IIIA and IIIB fractures presenting within 72 hours of injury were included. Polytrauma patients, types I and IIIC fractures, fractures with metaphyseal and articular involvement, and patients with fractures or injuries which precluded early mobilisation were excluded. Sixty-four patients underwent the procedure of whom four were lost to follow-up before assessment of union could be carried out. Fifty-one males and nine females (male:female ratio 5.67:1), who underwent the procedure and completed a minimum follow-up of 18 months, were included in the study. The age of the patients ranged from 20 years to 62 years (mean age 32.8 years), with patients between 20 and 39 years comprising 82% of the cases. The right side was involved in 28 and the left side in 32 patients (1:0.875). Road traffic accident was the most common mode of injury (41 patients), followed by blast injury and firearm injury (six each). Fall from trees was the causative factor in five patients and two patients sustained the injury due to a direct forceful blow by iron rods. Thirty three (55%) patients reported to our hospital within 24 hours of the injury, 18 (30%) between 24 and 48 hours and nine patients (15%) between 48–72 hours. Morphology of the fractures was classified according to the modified Gustilo-Anderson classification (Table 1). The Gustilo-Anderson classification has been the most widely used system and is generally accepted as the primary classification system for open fractures. This classification system takes into consideration the energy of the fracture injury, soft tissue damage, and the degree of contamination. Types I and II are essentially low-energy fractures, while type I has a wound size of 1 cm and that of type II is more than 1 cm. The classification system has been modified since the original classification to allow a more accurate prognosis for more severe injuries (i.e. type III injuries) [4]. In our series, type IIIB fractures were the most common, comprising 36 patients (60%), followed by type IIIA with 13 patients (21.7%) and type II with 11 patients (18.3%). The middle one-third of tibia was fractured in 27 patients (45%), the lower third in 21 (35%) and the upper third in 12 patients (20%).
Table 1.
Gustilo-Anderson classification
| Type | Wound Description | Other criteria |
|---|---|---|
| I | <1 cm (so-called puncture wounds) | |
| II | 1–10 cm | |
| IIIA | >10 cm, coverage available | Segmental fractures, farm injuries, or any injury occurring in a highly contaminated environment. High-velocity gunshot injuries |
| IIIB | 10 cm, requiring soft tissue coverage procedure | Periosteal stripping |
| IIIC | With vascular injury requiring repair |
Initial resuscitation, splintage and primary care for the wound were provided in the emergency room and swabs taken for culture. Any protruding bone fragments were covered with sterile dressing and obvious foreign material removed. The wound was copiously washed with normal saline (6 litres for types II & IIIA and about 10 litres for type IIIB), and thorough debridement of all devitalised bone and soft tissue was done under anaesthesia. Only stay sutures were applied with a view to cover the bone, if possible. To stabilise the fracture, an external fixator consisting of two Schanz pins, one on either side of the fracture, was applied. In all cases, third-generation cephalosporins and aminoglycosides were administered in the emergency room and used until the culture reports returned. In fractures with gross contamination and farmyard injuries, metronidazole was added.
Definite fixation with the IEF was carried out after three to five days of the initial emergency debridement. To save surgical time, pre-assembled frames were used. Thirty-three patients (55%) were treated on the third day, 22 (37%) on the fourth day and only five patients (8%) on the fifth day. Four Ilizarov rings were used, although in a few cases five rings were required. We used 1.8-mm Ilizarov wires in all patients. The Schanz pins introduced in the initial fixation were also included in the frame, if possible. When removal of loose detached small fragments was necessary or where bone loss existed, bone ends were approximated. This shortening was also helpful in wound closure. However, in patients with bone loss which had gross contamination and presented late (after 48 hours), the bone ends were not approximated. Eleven patients with bone loss of 3 cm or more underwent corticotomy to allow bone lengthening to be done. Wound debridement was done and if the wound condition permitted, the wound was closed. We were able to achieve delayed primary wound closure in 27 patients. The average operating time was 1 hour and 40 minutes; more operating time was needed for the complex fractures and those undergoing corticotomy. Antibiotics were continued for a minimum of five days post-operatively, and further if indicated. The patients and their attendants were taught pin and ring care. On the first post-operative day, knee and ankle mobilisation was started within the limits of pain. All patients were made to stand with support after 24 hours and partial weight bearing commenced within 48 hours progressing to full weight bearing within the limits of pain. Distraction was started on the first post-operative day at a rate of 0.25 mm per day. The patients were discharged after being taught pin site care (cleaning at least twice a day with a providone-iodine solution or alcohol) and distraction methods. The average hospital stay of the patients was 8.6 days (7–13 days).
Patients were followed-up regularly, checking for frame stability, pin site condition, wound condition, knee and ankle range of motion and limb length discrepancy. Radiological and clinical assessment of union was done. Whenever required, adjustments in the frame were made. If in three to six weeks time no callus response was evident, compression at the fracture site was performed. The quality of the regenerate in transported cases was assessed by Fernandez-Estev grading, the frame being removed only after appearance of grade V regenerate in the radiographs. Radiological bony union was accepted when there was evidence of periosteal bridging and obliteration of the fracture line by endosteal callus formation. When union appeared to be present (grade V regenerate in transported patients) the frame was dynamised for a three- to four-week period, followed by frame removal. In case of delayed callus formation (more than 16 weeks) a patellar tendon bearing cast was applied for three to four weeks with the patient bearing full weight. The final follow-up examination took place one year after the discontinuation of all immobilisation or support. Tucker's criterion was used to evaluate the final results [5]. An excellent result was defined as fracture union with full knee extension and more than 125° flexion, ankle range of motion >75% of normal, limb length discrepancy <1 cm, no angulation >7° in any plane, no rotation >7° and absence of infection. A good result indicated fracture union with one criterion missing, and a fair result was fracture union with two criteria missing. A poor result indicated fracture union with three missing criteria or non-union.
Results
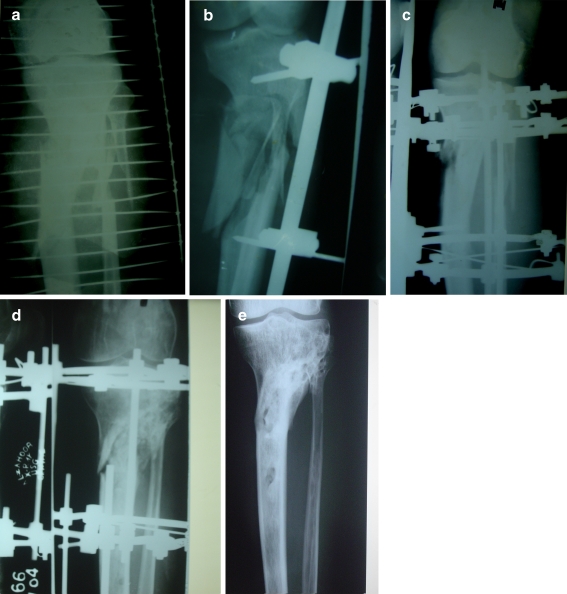
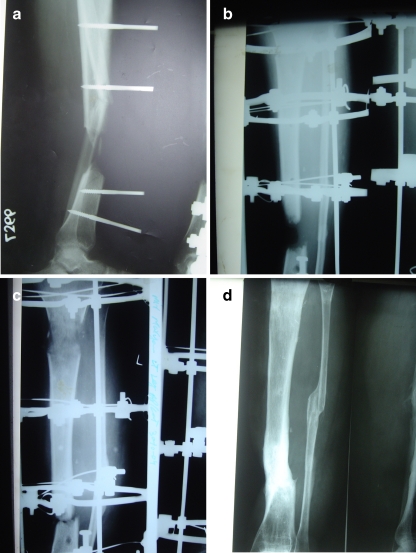
Union was achieved in all patients. The earliest evidence of radiological union at the fracture site was observed after two months of the procedure. Union time was defined as the time when both clinical (absence of pain or movement with the patient bearing full weight on the limb; the fixator attached but dynamised) and radiological union (presence of bridging callus in two planes) were complete and all types of support or immobilisation was removed. The time taken to achieve union in the patients who underwent monofocal osteosynthesis varied between 12 weeks and 33 weeks; the mean time to union was 22.24 weeks. The mean time to union in type IIIB fractures (without bone loss) was 23.04 weeks (standard deviation [SD] 4.36), 21.1 weeks (SD 3.18) in type II fractures and 21.7 weeks (SD 3.57) in type IIIA. The mean time to union in patients with type IIIB fractures (with or without bone loss) was 24.9 weeks (SD 5.14). There was no statistically significant difference in the union times of patients with type IIIB (without bone loss) and those with type II and IIIA fractures (p ≥ 0.05). Eleven patients with a bone defect between 3 cm and 7.2 cm (average defect 4.8 cm) underwent bone lengthening. The duration of fixator application in these patients was between 24 weeks and 45 weeks and the mean time to union was 29.1 weeks (SD 6.63). The healing index ranged from 1.3 to 2 months/cm (average 1.5). The difference between union times in type IIIB patients (with or without bone loss) and type II or IIIA was statistically significant (p < 0.05) (Figs. 1a–e and 2a–d).
Fig. 1.
a Initial anteroposterior (AP) radiograph shows a comminuted fracture of the tibia and fibula. b Initial radiograph after temporary fixation with external fixator. c Immediate postoperative radiograph following Ilizarov external fixator (IEF) application. d Radiograph at eight weeks with union in progress. e Final radiograph after removal of the frame depicts sound bony union and good alignment
Fig. 2.
a Initial radiograph of patient with compound fracture with bone loss of 4 cm. b Radiograph after application of Ilizarov external fixator (IEF) showing gap at the fracture site. c At ten weeks the lengthening was almost complete and the regenerate at the corticotomy site was consolidating. d Final radiograph at 28 weeks shows union at both fracture and corticotomy sites and restored length
An advantage of this procedure was in the wound care and closure. We performed delayed primary wound closure (at the time of Ilizarov application) in 27 patients, split skin grafting in 11 and muscle and fasciocutaneous flaps in three, while the remaining 19 patients were managed by secondary intent healing (Table 2). All the type II and most of type IIIA wounds were closed by delayed primary closure. Four patients with type IIIB fractures required additional debridement under anaesthesia before undergoing a plastic surgery procedure (SSG in two and flap in two). After bone transport one patient required a “peg in hole” docking to achieve proper alignment. With the exception of two patients, all the patients had equal limb length (<1 cm difference between two limbs). The patients with limb length discrepancy were given the choice of limb lengthening which they refused. At the final follow-up, four patients had a residual angulation (>7° in any plane) and no patient had residual rotation (>15° in any plane).
Table 2.
Method of management of wound
| Management procedure | Type II | Type IIIA | Type IIIB | Total |
|---|---|---|---|---|
| Delayed primary closure | 11 | 12 | 4 | 27 |
| Healing by second intent | - | - | 19 | 19 |
| Skin grafting | - | 1 | 10 | 11 |
| Flaps | - | - | 3 | 3 |
| Total | 11 | 13 | 36 | 60 |
The procedure was associated with a number of complications (Table 3). However, most of these complications were mild. Pin tract infection was the most common complication associated with the procedure, observed in 32 patients (77 pin sites). Only three patients had grade IV infections (Moore & Dahl classification) and required systemic antibiotics, and pin removal was performed in one patient. The rest of the patients had mild infections (grade II in 22 and grade III in seven patients) which all healed satisfactorily after pin-site dressings and local antibiotics. Grade V (osteolysis) and VI (ring sequestrum) infections were not seen in any patient. Fifteen patients had mild pain at the fracture site which was managed by analgesics and subsided. Two patients had an eczematous reaction around the pin site which responded to medications. None of the patients had refracture, either in the frame or after removal of the frame.
Table 3.
Complications
| Complication | Type II | Type IIIA | Type IIIB | Total |
|---|---|---|---|---|
| Pin tract infections | ||||
| Grade 2 | 3 | 4 | 15 | 22 |
| Grade 3 | 2 | 2 | 3 | 7 |
| Grade 4 | - | 1 | 2 | 3 |
| Pain | 3 | 3 | 9 | 15 |
| Decreased knee flexion | - | - | 3 | 3 |
| Knee extensor lag | - | - | 1 | 1 |
| Restricted ankle ROM | - | 1 | 2 | 3 |
| Eczematous reaction | 1 | 1 | - | 2 |
| Retained IM rod | - | - | 1 | 1 |
| Limb length discrepancy (>1 cm) | - | - | 2 | 2 |
ROM range of motion, IM intramedullary
We started early knee and ankle physiotherapy and were thus able to achieve good knee and ankle range of motion (ROM). Three patients had restricted knee flexion (<125°), including one with flexion <110° and one patient had extensor lag. Three patients had ankle ROM <75% of the normal ankle. This included one patient with pre-operative foot drop which improved but the patient continued to have restricted movements of the ankle. A unique complication was the retention of an intramedullary rod used as transporting device. Radiographs showing examples of application of the IEF, various fracture types, union and complications can be seen in Figs. 1, 2 and 3.
Fig. 3.

Complication arising out of the procedure with retention of the intramedullary rod used as a transporting device
The final results were graded after a minimum of one year of discarding all form of support using Tucker criterion. Forty-eight patients (80%) had excellent results, ten had good (16.7%) and two patients (3.3%) had fair results. None of the patients had a poor result.
Discussion
Open tibial fractures are the most common open fractures involving the long bones with an annual incidence of 5.6 per 100,000 persons in the United States [6]. These fractures continue to pose a challenge to orthopaedic surgeons worldwide. The precarious blood supply and lack of soft-tissue cover of the shaft of the tibia make these fractures vulnerable to non-union and infection [7]. The acceptable goals for open tibial diaphyseal fractures remain the prevention of infection; maintainance of normal length, alignment and rotation of the extremity; minimising additional damage to soft tissue and bone; preserving the remaining circulation and providing a mechanical environment which stimulates periosteal and endosteal responses which favour bone healing [5]. Plate fixation is associated with a number of complications, especially in communited fractures. A systemic review of 11 studies involving 492 open tibial fractures managed by plating revealed a revision rate ranging from 8–69% and a pooled estimate of deep infection rate of 11% [8]. Allan and Sigvard reported severe osteomyelitis in 19% of the open tibial fractures treated by plate fixation [9]. External fixation has been popular because of the relative ease of application and the limited effect on the blood supply of the tibia, but these advantages have been outweighed by the high incidence of non-union and pin-track infection, difficulties relating to soft-tissue management and the potential for malunion. Papaioannou et al. reported non-union in 20.3% of patients with open tibial fractures managed by external fixators, especially types II and III [10].
In recent years primary intramedullary nailing has gained wide acceptance in open tibial fractures in developed countries [11]. However, even in expert hands, IM nailing is associated with problems of infections (especially in type IIIB fractures) and delayed union [12]. Although some reports coming from the developed world have shown good results with IM nailing, extending these to developing countries, where patients report late and adequate facilities are not always available, is not an option [13]. In most centres in our region, these fractures are initially managed by external fixator due to unavailability of adequate instrumentation (image intensifier) and manpower in the emergency operation theatres. Intramedullary nailing in fractures initially treated by external fixation has been associated with a high rate of infection, especially when external fixation was associated with pin-track infection [14]. In the developing countries, external fixation remains the definitive treatment and a significant number of patients progress to non-union and malunion. Even in the centres with facilities for emergency IM nailing, the results have not been encouraging since most of the patients in our region report to hospital late. Joshi et al. had an infection rate of 10.7% in open tibial fractures managed by unreamed nailing, even after debridement and adequate soft tissue coverage [15]. They did not recommend nailing in type III fractures with delayed presentation to the hospitals.
Our region has witnessed a surge in open tibial fractures due to the ongoing conflict and the increase in the number of vehicles plying the roads. Our hospital, as the major orthopaedic centre, has been receiving the bulk of these patients. Our poor results with conventional external fixators and the unavailability of image intensifiers in the emergency operation theatre, coupled with the huge patient burden on the hospital, prompted us to use the Ilizarov external fixator (IEF) in these fractures. The Ilizarov device has been used in open tibial fractures mostly as a salvage procedure for the complications arising from other treatment methods [16]. Recently, it has been used as the primary management in open fractures in many centres throughout the world, especially Russia and Western Europe [17]. IEF combines the attributes of a solid fixation and early weight bearing with adequate management of the wounds while at the same time addressing the bone loss.
IEF provides a safe and effective treatment modality for open tibial fractures. The hallmark of the method is the high union rate. Hosny and Fadel achieved union in all 34 open tibial fractures managed by IEF [18]. Sidharthan et al. achieved union in all the 42 high energy tibial fractures managed with IEF and advocated the use of IEF in high energy tibial fractures since the device provides an early and definitive management of these fractures [19]. We also achieved union in all the 60 open tibial fractures managed by IEF. Our result is all the more gratifying since all our patients had either type II or III fractures, which have a poorer outcome with the traditional methods. Furthermore, we had a higher percentage of patients with type IIIB fractures (60%) and all fractures united without any case of post-traumatic osteomyelitis. The high rate of union with IEF can be attributed to the minimally invasive nature of the device which leads to minimal stripping of the soft tissues and the consequent interference with the vascularity of the bone and the fracture. This is in contrast to IM nailing which interferes with the intramedullary circulation. The interference with circulation is seen with both unreamed and reamed IM nailing, although the degree of compromise is a matter of controversy [20].
The time to achieve union with IEF varies in different studies, since different authors have used different criteria of union. Inan et al. reported bone union in 19 weeks in all type IIIA fractures and the time to union was significantly shorter than in the tibial nailing group [21]. The time to union in our patients undergoing monofocal osteosynthesis is comparable to that of Tucker who used the same criteria as we did for defining union. The union time in type IIIB patients without bone loss is not significantly different from that in type II or IIIA. However, when fractures with bone loss are also included the difference in union time when compared with type II or IIIA fractures becomes significant. This may be related to the severity of trauma in the former which leads to significant soft tissue damage and loss of blood supply to the bone. Inan et al. also found a significant difference between types IIIA and IIIB in terms of time to union [21]. The average union time in patients with bone loss in our series is directly related to the bone defect. Dagher and Roukoz did not find any correlation between defect length and union time [22]. However, most of their patients had already undergone other procedures before IEF, unlike our patients, in which all patients had Ilizarov as the primary procedure. The healing index of 1.52 months/cm seen in our patients is similar to that reported by Dendrios (1.78 months/cm) [23].
Soft tissue management holds the key to achieving a good functional result in open tibial fractures. The timing of soft tissue coverage is controversial, the standard teaching being repeated debridement of all necrotic tissue before wound closure [24]. This recommendation has been recently challenged, with authors advocating primary closure of open wounds in some cases. Shtarker et al. used primary suturing and Ilizarov fixation in the treatment of open tibial fractures with good results [25]. De Long et al. reported good results in type IIIB fractures with emergency fracture fixation and wound debridement and coverage (using pedicled or free muscle flap) [26]. A unique feature of our study is the high percentage of wounds in IIIB fractures which healed by second intent. This is due to the limited number of plastic surgeons available in our region who are not able to address all wounds early and most of these ultimately heal by second intention. Therefore, IEF is adequately suited to the less developed countries where plastic surgeons are not always available to assist the orthopaedic surgeons.
In healthy adults, wound healing proceeds for the first five days or so regardless of whether the wound is closed. Thus, delayed suture in wounds within five days is able to achieve wound strength equal to primary closure by the end of the second week [27]. Since we applied IEF after three to five days of the initial debridement, we were able to achieve wound closure in the majority of type II and IIIA fractures at the time of IEF application. The number of additional procedures required to achieve wound coverage (superficial skin graft or musculocutaneous flaps in type III fractures) is thus reduced by the use of IEF after three to five days of the injury. The additional anaesthesia required for IEF in our study can be justified since most of the open fractures also require debridement after three to five days in any event. This also significantly reduced the load on our emergency operation theatres while at the same time saving precious time in the routine theatres by using pre-assembled frames.
The overall number of secondary procedures required with IEF is less compared to other modalities. Wound coverage procedures constitute the bulk of secondary procedures with IEF. The bony procedures needed with IEF are usually related to pin replacement. In contrast, nailing is associated with a risk of non-union, infections and malunion, needing additional procedures. Tibial nailing is associated with a significant risk of infection by negatively influencing the intramedullary circulation, although the effect of reaming on infection is controversial. The Ilizarov device is minimally invasive with little interference to the biology of fracture. This leads to decreased incidence of infection and non-union. The decreased number of secondary procedures is an advantage as the additional admissions entail the occupancy of hospital beds and a financial burden to the patient.
IEF allows early mobilisation of the patient by allowing partial weight bearing within 48 hours progressing to full weight bearing within the limits of pain. This produces axial compressive forces at the fracture site which probably stimulate bone healing. Despite being less stiff in the axial compression, IEF is moderately to highly stiff in AP and lateral bending strains. Ilizarov wires provide multiple cortical interfaces and the multiplanar orientation of the wires virtually eliminates any late displacement of fragments leading to a low rate of malunion. An Ilizarov fixator also enables the surgeon to correct any malalignments arising during the course of treatment.
IEF is also associated with a number of complications, although most of these are minor. Pin tract infections form the bulk of complications associated with IEF [24]. Although the infection is superficial and mild in most of the cases, infection increases the risk of wire loosening and, due to the weight borne by the external fixator, causes frame instability. Good care of pin sites and aggressive management of superficial infections is essential to prevent deep infections and septic arthritis (associated with wires placed less than 1 cm from the subchondral bone). Insufficient pin care has been associated with higher incidence of pin tract complications [28]. Muscle contracture and joint stiffness are significant problems, especially seen in patients where fixator is applied for prolonged periods and in fractures near the joints [29]. Early and vigorous range of motion activities help in achieving a good functional outcome. Refracture in the consolidate is a troublesome complication, seen in up to 8% of cases [21]. These fractures usually arise due to early removal of the frame. Malunion, which is a frequent complication with nailing, is less common with IEF. IEF allows the surgeon to correct malalignments while the bone is undergoing union or lengthening.
Conclusion
The Ilizarov external fixator is a versatile instrument in the armentarium of an orthopaedic surgeon. It holds great promise in the management of open fractures of the tibia in the developing countries where facilities for IM nailing and plastic surgery are not always present, especially in the emergency operation theatres where most of these fractures are treated initially. Our protocol of debridement and initial temporary bony stabilisation with an external fixator, followed by IEF after three to five days, is an effective form of management associated with good bony and functional results, while at the same time reducing the load on the overburdened emergency facilities. IEF permits early weight bearing, good functional recovery, correction of deformities, attainment of adequate limb length and facilitates wound coverage. The complications associated with the procedure are minor and usually do not require surgical intervention. Despite technical difficulties and pin-tract related infections, we recommend IEF as the definitive primary fixation in type II, IIIA and IIIB fractures.
Acknowledgments
Conflict of interest No funds were received directly or indirectly by any of the authors in the funding of this study. No benefits in any form have been received or will be received by us from any commercial party directly or indirectly on the subject of the manuscript.
Footnotes
Authors’ contribution
ANB is the principal author of the manuscript and was involved in collection of literature and preparing the manuscript. NBW and KAK were responsible for organising the study, collection of data, overall patient care and decision-making. MRM was involved in arranging patient care and proof reading the manuscript.
References
- 1.Nicol SA. Closed and open management of tibial fractures. Clin Orthop Relat Res. 1974;105:144–153. doi: 10.1097/00003086-197411000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Gustilo RB, Markow RL, Templeman Current concept review: the management of open fractures. J Bone Joint Surg Am. 1990;72:299–303. [PubMed] [Google Scholar]
- 3.Bilat C, Leutenegger A, Ruedi T. Osteosynthesis of 245 tibial fractures, early and late complications. Injury. 1994;25:349–358. doi: 10.1016/0020-1383(94)90125-2. [DOI] [PubMed] [Google Scholar]
- 4.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24:742–746. doi: 10.1097/00005373-198408000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Tucker HL, Kendra JC, Kinnebrew TE. Management of unstable open and closed fractures using the Ilizarov method. Clin Orthop. 1992;280:125–135. [PubMed] [Google Scholar]
- 6.Court-Brown CM, Rimmer S, Prakash U, et al. The epidemiology of open long bone fractures. Injury. 1998;29:529–534. doi: 10.1016/S0020-1383(98)00125-9. [DOI] [PubMed] [Google Scholar]
- 7.Esterhai JL, Queenan J. Management of soft tissue wounds associated with type III open fractures. Orthop Clin North Am. 1991;22:427–432. [PubMed] [Google Scholar]
- 8.Giannoudis PV, Papakostidis C, Kouvidis G, Kanakaris NK. The role of plating in the operative treatment of severe open tibial fractures: a systematic review. Int Orthop. 2009;33(1):19–26. doi: 10.1007/s00264-007-0443-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bach AW, Hansen ST., Jr Plates versus external fixation in severe open tibial shaft fractures. A randomized trial. Clin Orthop Relat Res. 1989;241:89–94. [PubMed] [Google Scholar]
- 10.Papaioannou N, Mastrokalos D, Papagelopoulos PJ, et al. Non-union after primary treatment of tibia fractures with external fixation. Eur J Orthop Surg Trauma. 2001;11:231–235. doi: 10.1007/BF01686895. [DOI] [Google Scholar]
- 11.Finkemeier CG, Schmidt AH, Kyle RF, Templeman DC. A prospective, randomized study of intramedullary nails inserted with and without reaming for the treatment of open and closed fractures of the tibial shaft. J Orthop Trauma. 2000;14:187–193. doi: 10.1097/00005131-200003000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Hupel TM, Weinberg JA, Aksenov SA, Schemitsch EH. Effect of unreamed, limited reamed and standard reamed intramedullary nailing on cortical bone porosity and new bone formation. J Orthop Trauma. 2001;15:18–27. doi: 10.1097/00005131-200101000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Kuhn S, Hansen M, Rommens PM. Extending the indication of intramedullary nailing of tibial fractures. Eur J Trauma Emerg Surg. 2007;2:159–168. doi: 10.1007/s00068-007-7039-z. [DOI] [PubMed] [Google Scholar]
- 14.Maurer DJ, Merkow RL, Gustilo RB. Infection after intramedullary nailing of severe open tibial fractures initially treated with external fixation. J Bone Joint Surg Am. 1989;71(6):835–838. [PubMed] [Google Scholar]
- 15.Joshi D, Ahmed A, Krishna L, Lal Y. Unreamed interlocking nailing in open fractures of tibia. J Orthop Surg. 2004;12(2):216–221. doi: 10.1177/230949900401200215. [DOI] [PubMed] [Google Scholar]
- 16.Lalit M, Manish C, Jashan V, Kapoor S, Mehtani A, Dhaon BK. The Ilizarov method in infected non-union of fractures. Injury. 2000;31(7):509–517. doi: 10.1016/S0020-1383(00)00036-X. [DOI] [PubMed] [Google Scholar]
- 17.Ilizarov GA. Experimental studies of bone elongation. In: Coombs R, Green S, Sarmiento A, editors. External fixation and functional bracing. London: Orthotext; 1989. p. 375. [Google Scholar]
- 18.Hosny G, Fadel M. Ilizarov external fixator for open fractures of the tibial shaft. Int Orthop. 2003;27(5):303–306. doi: 10.1007/s00264-003-0476-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sidharthan S, Sujith A, Rathod AK, Pathak RH (2005) Management of high energy tibial fractures using the Ilizarov apparatus. Internet J Orthop Surg 2(2)
- 20.Ziran BH, Darowish M, Klatt BA, Agudelo JF, Smith WR. Intramedullary nailing in open tibia fractures: a comparison of two techniques. Int Orthop. 2004;28(4):235–238. doi: 10.1007/s00264-004-0567-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Inan M, Tuncel M, Karaoğlu S, Halici M. Treatment of type II and III open tibial fractures with Ilizarov external fixation. Acta Orthop Traumatol Turc. 2002;36(5):390–396. [PubMed] [Google Scholar]
- 22.Dagher F, Roukoz S. Compound tibial fractures with bone loss treated by Ilizarov technique. J Bone Joint Surg Br. 1991;73:316–321. doi: 10.1302/0301-620X.73B2.2005164. [DOI] [PubMed] [Google Scholar]
- 23.Dendrios GK, Kontos S, Cyritsis E. Use of Ilizarov technique for non-union of tibia associated with infection. J Bone Joint Surg Am. 1995;77(6):835–846. doi: 10.2106/00004623-199506000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Cierny G, Byrd HS, Jones RE. Primary versus delayed soft-tissue coverage for severe open tibial shaft fractures. Clin Orthop. 1983;178:54–63. [PubMed] [Google Scholar]
- 25.Shtarker H, David R, Stolero J, Grimberg B, Soundry M. Treatment of open tibial fractures with primary suture and Ilizarov fixation. Clin Orthop. 1997;335:268–274. [PubMed] [Google Scholar]
- 26.Delong WG, Jr, Born CT, Wei SY, Petrik ME, Ponzio R, Schwab CW. Aggressive treatment of 119 open fracture wounds. J Trauma. 1999;46:1049–1054. doi: 10.1097/00005373-199906000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Olson SA, Finkemeier CG, Moehring HD (2001) Open fractures. In: Bucholz RW, Heckman JD (eds). Rockwood and Green’s fractures in adults, 5th edn. Lippincott Williams & Wilkins, pp 285–318
- 28.Thayur RM, Balasundaram R, Manjunath KS, et al. Outcomes of Ilizarov ring fixation in recalcitrant infected tibial non-unions—a prospective study. J Trauma Manag Outcomes. 2008;2:6. doi: 10.1186/1752-2897-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Inan M, Halici M, Ayan I, Tuncel M, Karaoglu S. Treatment of type IIIA open fractures of tibial shaft with Ilizarov external fixator versus unreamed tibial nailing. Arch Orthop Trauma Surg. 2007;127(8):617–623. doi: 10.1007/s00402-007-0332-9. [DOI] [PubMed] [Google Scholar]