Abstract
Purpose
Degenerative cervical spondylolisthesis has received insufficient attention, in contrast to degenerative lumbar spondylolisthesis. In fact, degenerative cervical spondylolisthesis may be more common than previously thought.
Methods
In order to provide appropriate guidelines for the treatment of degenerative cervical spondylolisthesis, a systematic review of degenerative cervical spondylolisthesis was performed. An English literature search from January 1947 to November 2010 was completed with reference to radiological examination and management of degenerative cervical spondylolisthesis.
Results
Of 102 patients with degenerative cervical spondylolisthesis, 52 patients (51%) had neck or occipital pain, 23 patients (22.5%) were referred with radiculopathy and 65 patients (63.7%) presented with myelopathy or myeloradiculopathy. Degenerative cervical spondylolisthesis was most common in C3/4 and C4/5, occurring in 81 patients at C3/4 (46%) and 87 at C4/5 (49.4%). Disc degeneration and facet hypertrophy were the main causes of this clinical entity. Of 123 patients, 57 (46.3%) were found to have segmental instability as shown by flexion-extension lateral radiographs. There are two classification systems for degenerative cervical spondylolisthesis. Surgery was indicated in patients who had radiologically proven cervical spondylolisthesis with instability and/or spinal cord compression.
Conclusion
Prospective studies should be designed in the future to draw a more reliable conclusion about the management of degenerative cervical spondylolisthesis.
Introduction
Degenerative lumbar spondylolisthesis is a common condition in the elderly. The main cause is disc degeneration and facet joint arthrosis. However, in the cervical spine, trauma may be the most common cause of anterior displacement of one vertebral body relative to the subjacent one. Injuries that lead to this deformity include traumatic spondylolisthesis of the axis (hangman fracture) [1], uni- or bilateral facet dislocation and facet fracture subluxation. In addition, Hardouin et al. reported 4 cases of cervical spondylolisthesis, which they attributed to renal osteodystrophy in 80 haemodialysis patients [2]. Perlman and Hawes [3] first reported a case of congenital absence and hypoplasia of the C6 pedicles with resultant C6–C7 spondylolisthesis. These cervical spondylolistheses appear to correspond to the traumatic, pathological and dysplastic types in the lumbar spine as characterised by Newman. Another well-described form of cervical spondylolisthesis can be classified as degenerative. In 1986, Lee et al. [4] studied the radiographic differences between degenerative and traumatic slippage of the cervical spine.
The current authors reviewed reports published on cervical spondylolisthesis from January 1947 to November 2010 and focused on the clinical data, classification and management of this disorder.
Materials and methods
Eligibility criteria
The following criteria were used in selecting articles: (1) target population, individuals with degenerative cervical spondylolisthesis; (2) radiographic examination or surgical intervention; and (3) article in English.
Identification of studies
We conducted a PubMed search of articles published from January 1947 to November 2010, identifying the population with degenerative cervical spondylolisthesis. Keywords of ‘cervical spondylolisthesis’ AND ‘degeneration’ were used.
The titles were reviewed and, if the title suggested any possibility that the article might meet the eligibility criteria, the abstracts were retrieved and reviewed. All abstracts were printed and close reading was performed by two surgeons with rich experience in spinal surgery. The different information extracted from the same article was compared and reread until the information could be agreed upon. If it was difficult for them to obtain a consensus, a third reviewer was consulted. Finally, a total of eight papers were selected to review. The full text of each paper was found, and then careful reading and data extraction were performed independently by the two surgeons mentioned above. Eventually, all the extracted information was imported into an electronic spreadsheet—Microsoft Excel.
Statistical analysis
The unpaired t test and Fisher’s exact test were used for statistical analysis. All P values <0.05 were considered statistically significant.
Results
After screening the abstracts, eight articles underwent further analysis [4–11]. The detailed data are listed in Table 1.
Table 1.
Data of publications on degenerative cervical spondylolisthesis
| Authors | Year | Patients (n) | Male | Female | Age (years) | Level | Stability | Slippage | Symptoms and signs |
|---|---|---|---|---|---|---|---|---|---|
| Lee et al. [4] | 1986 | 42 | NA | NA | 73 (41–89) | NA | NA | 28 patients (anterior slippage): 5 mm(2–9 mm); 14 patients (posterior slippage): 2.5 mm (2–4 mm) | NA |
| Deburge et al. [5] | 1995 | 8 | 3 | 5 | 71 (65–82) | Total levels: 10; C3/4: 3; C4/5: 6; C7/T1: 1 | Unstable patients: 8 | NA | Neck pain: 8; brachialgia: 1; myelopathy: 2 |
| Boulos et al. [6] | 1996 | 5 | 4 | 1 | 66.8 (55–77) | Total levels: 5; C3/4: 4; C7/T1: 1 | Unstable patients: 2 | 3.8 ± 0.9 mm | Neck pain: 3; myelopathy: 4; upper weakness and numbness: 4 |
| Tani et al. [7] | 2003 | 47 | 18 | 29 | 76 (65–86) | Total levels: 68; C2/3: 5; C3/4: 29; C4/5: 26; C5/6: 8 | NA | 3.1 ± 0.9 mm (2–6 mm) | NA |
| Woiciechowsky et al. [8] | 2004 | 16 | 9 | 7 | 67.6 (50–75) | Total levels: 18; C3/4: 5; C4/5: 5; C5/6: 5; C7/T1:3 | Unstable patients: 5 | 2.9 ± 0.9 mm | Neck pain: 3; myelopathy: 8; myeloradiculopathy: 5 |
| Kawasaki et al. [9] | 2007 | 79 | 33 | 46 | 75 (65–88) | Severe spondylolisthesis: total levels: 27; C3/4: 15; C4/5: 10; C5/6: 1; C7/T1: 1 | Unstable patients: 27 | Severe spondylolisthesis: 4.2 ± 0.7 mm (3.5–6 mm); mild spondylolisthesis: 1.1 ± 0.8 mm (0–1.9 mm) | NA |
| Dean et al. [10] | 2009 | 58 | 27 | 31 | 63 (36–86) | Total levels: 72; C2/3: 4; C3/4: 16; C4/5: 31; C5/6: 10; C6/7: 4; C7/T1: 7 | Unstable levels: 17 | 4.02 ± 1.17 mm (3–7 mm) | Neck or occipital pain: 38; radiculopathy: 18; myelopathy: 28; myeloradiculopathy: 11 |
| Shigematsu et al. [11] | 2010 | 15 | 9 | 6 | 72.4 | Total levels: 22; C2/3: 3; C3/4: 9; C4/5: 9; C5/6: 1 | Unstable patients: 15 | 3.1 ± 0.6 mm | Myelopathy: 15 |
NA not available
There were a total of 228 patients with degenerative cervical spondylolisthesis, and 103 patients (45.2%) were male and 125 (54.8%) were female in 7 studies. The difference in the incidence between men and women is not statistically significant (P > 0.05, df = 6).
A total of 102 patients in four studies had detailed data about clinical presentation. Of these, 52 patients (51%) had neck or occipital pain [5, 6, 8, 10]. A total of 54 cases (52.9%) were referred with cord compression symptoms and signs, such as wide-based gait, hyperreflexia and Hoffmann sign [5, 6, 8, 10], and 11 patients (10.8%) complained of symptoms and signs of mixed myeloradiculopathy. Twenty-three patients (22.5%) presented with symptoms of radiculopathy, such as brachialgia, and upper weakness and numbness [5, 6, 10].
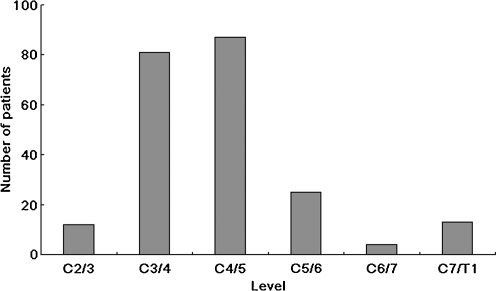
Of 176 patients in six studies, 222 levels with spondylolisthesis were involved (Fig. 1) [5–11]. Degenerative cervical spondylolisthesis was most common in C3/4 and C4/5, occurring in 81 patients at C3/4 (46%) and 87 at C4/5 (49.4%). Other levels were located at C2/3 in 12 cases (6.8%), another level C5/6 in 25 cases (14.2%), a further level C6/7 in four cases (2.3%) and the other level C7/T1 in 13 cases (7.4%).
Fig. 1.
Distribution of the involved levels in patients with degenerative cervical spondylolisthesis
Only one study described a history of cervical surgery in five patients with cervical degenerative spondylolisthesis. Boulos et al. [6] reported two patients with a history of cervical surgery in 5 patients. One had a prior cervical laminectomy of C3–C5, and the other had an anterior cervical fusion from C4 to C5.
Radiographic examinations of lateral views in flexion and extension were used to evaluate for evidence of an instability pattern at the involved levels of 181 patients in six studies. Of 123 patients, 57 patients (46.3%) were found to be unstable using flexion-extension views in five studies [5, 6, 8, 9, 11]. In the other study, Dean et al. [10] reported 17 unstable levels (23.6%) of the 72 levels in 58 patients with degenerative cervical spondylolisthesis. However, the criteria for the diagnosis of instability in these studies were not identical (Table 2). Magnetic resonance imaging (MRI) was used to determine the location and extent of neurological compression at the level of spondylolisthesis in seven studies [5–11].
Table 2.
Criteria for the diagnosis of instability
| Authors | Year | Criterion for the diagnosis of instability |
|---|---|---|
| Deburge et al. [5] | 1995 | NA |
| Boulos et al. [6] | 1996 | Movement with flexion-extension |
| Woiciechowsky et al. [8] | 2004 | Mobility on flexion-extension radiographs |
| Kawasaki et al. [9] | 2007 | Horizontal displacement of 3.5 mm or more |
| Dean et al. [10] | 2009 | At least 1 mm of motion on flexion-extension radiographs |
| Shigematsu et al. [11] | 2010 | More than 2.5 mm of slippage displacement was observed on flexion-extension views |
NA not available
There are two classification systems for degenerative cervical spondylolisthesis. Dean et al. [10] identified two types of cervical degenerative spondylolisthesis. The first and more common listhesis (type I or adjacent) occurred adjacent to relatively stiff, spondylotic cervical levels; and the second and less common type (type II or spondylotic) occurred within spondylotic cervical segments. The other classification system was proposed by Woiciechowsky et al. [8] based on the radiographic findings: spondylolisthesis with degeneration of the facet joints; spondylolisthesis with degeneration of the facet joints and vertebral bodies; and spondylolisthesis with severe cervical spine deformity.
Degenerative cervical spondylolisthesis can be described according to the degree of severity. Kawasaki et al. [9] categorised their patients with degenerative cervical spondylolisthesis into three grades according to the measured values of the maximum horizontal displacement on radiographs obtained in either flexion or extension: severe spondylolisthesis, moderate spondylolisthesis and mild spondylolisthesis. Patients with severe spondylolisthesis had unequivocal horizontal displacement of 3.5 mm or more, a criterion established by White et al. [12] as suggestive of instability in the cervical spine, whereas those with moderate spondylolisthesis had horizontal displacement of 2.0–3.4 mm, and those with mild spondylolisthesis had a horizontal displacement of less than 2.0 mm.
Of 212 patients, horizontal displacement of one vertebra in relation to that immediately below it was measured on lateral radiographs in seven studies [4, 6–11]; these patients had an average horizontal displacement of 3.9 mm.
A total of 102 patients had surgical intervention. Of them, 77 underwent anterior surgery, including two anterior fusions, 72 anterior decompressions and fusions, and three combined anterior decompressions and fusions and augmented posterior facet fusions [5, 8, 10]. A total of 25 patients were treated with posterior surgery, including four posterior fusions, six posterior decompressions and fusions, and 15 double-door laminoplasties.
There were three complications (2.9%) related to surgical management in 102 patients which were operatively treated. Dean et al. [10] reported two complications in 58 patients. One was an avulsion fracture of the anterior superior iliac spine after bone graft harvest for strut grafting after vertebral corpectomy, and the other was a vertebral artery injury because of an anomalous artery. Screw pullout was found in one patient in the study of Boulos et al. [6], and halo vest fixation was required for four months. Nonfusion was found in three of 66 patients in two studies [5, 10].
The clinical outcomes of 102 patients operatively treated are listed in Table 3. However, there was no identical criterion for the outcome assessment in these studies. Deburge et al. [5] reported that satisfactory function was achieved in all eight patients. In another study of five patients, a striking improvement of walking ability was achieved in all patients. However, three patients with significant disability improved one Nurick grade, and the other two did not change their grade [6]. Of 16 patients treated with anterior decompression and fusion, neurological improvement was seen in 6 of 8 patients with myelopathy and four of five patients with myeloradiculopathy, and pain relief was noted in all patients who complained of pain preoperatively [8]. Dean et al. [10] also found that the average neurological improvement was 1.5 Nurick grades in 58 patients after anterior cervical decompression and fusion. Similarly, Shigematsu et al. [11] reported a 40% recovery rate of the Japanese Orthopaedic Association (JOA) score in 15 patients treated with laminoplasty.
Table 3.
Data on management of degenerative cervical spondylolisthesis
| Authors | Year | Patients (n) | Treatment | Complication | Follow-up | Outcome |
|---|---|---|---|---|---|---|
| Deburge et al. [5] | 1995 | 8 | Anterior fusion: 3; posterior fusion: 5; decompression: 2 | NA | 1–7 years | Bone fusion and satisfactory function in all patients |
| Boulos et al. [6] | 1996 | 5 | Posterior laminectomy with lateral mass plating: 2; posterior laminectomy with lateral mass plating and bone graft: 3 | Screw pullout: 1 | 2.5 years (1–3 years) | Striking improvement in all patients’ ability to walk; 3 patients with significant disability improved 1 Nurick grade, whereas the other 2 did not change grade |
| Woiciechowsky et al. [8] | 2004 | 16 | Anterior cervical decompression and fusion | NA | 6–52 months | According to Odom’s criteria, 4 patients had an excellent outcome, 6 patients had a good outcome, 3 patients had a satisfactory outcome and 3 patients had a poor outcome |
| Dean et al. [10] | 2009 | 58 | Anterior decompression and fusion | Avulsion fracture of the anterior superior iliac spine: 1; vertebral artery injury: 1 | 6.9 years (2–24 years) | Average neurological improvement: 1.5 Nurick grades; overall fusion rate: 92% |
| Shigematsu et al. [11] | 2010 | 15 | Double-door laminoplasty | NA | >3 years | JOA score at final follow-up: 10.9 ± 3.3; recovery rate: 40% |
NA not available
Discussion
Degenerative cervical spondylolisthesis is not a rare condition in the elderly, but has received insufficient attention, in contrast to degenerative lumbar spondylolisthesis. In fact, degenerative cervical spondylolisthesis may be more common than previously thought. However, up to now, degenerative cervical spondylolisthesis has not been extensively studied. It is characterised by hypertrophic facet arthropathy that results in joint erosions, marginal osteophytes and subluxation. The main cause is disc degeneration and hypertrophic spurring. If rigidity or ankylosis occurs, cervical spine mobility will diminish, thus increasing the stress on the adjacent discs and facets, especially during flexion and extension of the cervical spine. The increased stress may stretch the disc and ligaments, allowing slippage to occur [4]. With time, the repeated grinding action of flexion and extension causes facets to become ribbon-like [13, 14]. However, some [4] think that thinning of the facets and narrowing of the joint space may be the primary cause of degenerative cervical spondylolisthesis rather than the disc involvement. Regarding the mechanisms, the restabilisation of degenerative spine conditions may prevent progression of the disease and lead to various forms of the deformity.
Our study demonstrated that degenerative cervical spondylolisthesis was most common in C3/4 and C4/5, occurring in 81 of 176 patients at C3/4 (46%) and 87 at C4/5 (49.4%). The reasons why degenerative spondylolisthesis locates preferentially in the middle cervical spine can be explained by the relative hypermobility and the different pattern of movement in association with the relaxation of surrounding ligaments and degenerative articular changes. If the whole lower spine becomes rigid, spondylolisthesis may occur at the upper levels.
In patients with degenerative cervical spondylolisthesis, degeneration of the disc and the facet joints occurs firstly in association with neck pain. Neck pain is the initial symptom of degenerative cervical spondylolisthesis. Our study showed that 52 of 102 patients (51%) had neck or occipital pain. More patients were referred with myelopathy or myeloradiculopathy (63.7%) than with radiculopathy (22.5%). Intensive signals that indicate cord compression can be seen on MR images at the site of spondylolisthesis in patients with myelopathy. Degenerative cervical spondylolisthesis plays a pivotal role as the cause of myelopathy in the elderly [15–17]. However, it is difficult to correlate the symptoms to severity of spondylolisthesis. Clinical studies suggest the correlation of symptomatic progression of cervical spondylotic myelopathy and dynamic range of motion [18, 19]. In the study of Hayashi et al. [20], of 42 patients with cervical spondylotic myelopathy, 27 patients showed static canal stenosis, whereas 40 had dynamic canal stenosis, most commonly at C3/4 and C4/5. This suggests that dynamic canal measurements are most likely to correlate with progression of myelopathy than static ones, and older patients are particularly susceptible to dynamic canal stenosis from spondylolisthesis. The results of this study showed segmental instability as shown by flexion-extension lateral views of the cervical spine in 57 of 123 patients (46.3%) with degenerative cervical spondylolisthesis, suggesting that dynamic factors should be evaluated and addressed in patients with degenerative spondylolisthesis.
There are two classification systems of degenerative cervical spondylolisthesis. Dean et al. [10] presented two types of degenerative cervical spondylolisthesis. The first type, which is more common, occurs adjacent to a relatively stiffer spondylotic segment, the transition zone from stiff to more mobile segments. This type may in fact be accurately termed compensatory subluxation. Although, to some degree, disc degeneration is present in such a slip, it is radiographically and pathologically less in magnitude than in the adjacent levels with more advanced spondylosis. Osteoarthritic changes of the facet joints with erosions, joint remodelling and subluxation can be found in patients with this type of spondylolisthesis. In addition, the orientation of the facet joints is more horizontal, which would allow for more subluxation. This probably results, at least in part, from differential stiffness relative to other levels. The second type of spondylolisthesis occurs within spondylotic cervical segments and is associated with advanced disc degeneration.
Woiciechowsky et al. [8] categorised degenerative cervical spondylolisthesis into three types: spondylolisthesis with degeneration of the facet joints; spondylolisthesis with degeneration of the facet joints and vertebral bodies; and spondylolisthesis with severe cervical spine deformity. This classification is oriented towards clinical and morphological data, and it is based on the assumption that degeneration of the disc and the facet joints occurs firstly in association with instability and neck pain. At the early stage, degeneration of the vertebral bodies and discs may be mild. If instability proceeds faster than restoration, spondylolisthesis may become visible on radiographs at this early stage. However, this seems to be very rare in the cervical spine, in contrast to the lumbar spine. Facet joint degeneration is more frequently accompanied by spondylosis and discopathy, which leads to restabilisation and spinal canal stenosis. Therefore, a more reliable classification is necessary for degenerative cervical spondylolisthesis.
There is no guideline for the treatment of degenerative cervical spondylolisthesis. A less severe spondylolisthesis (i.e. a 1- or 2-mm slip) may frequently cause few or no symptoms and may not represent a surgical problem in most patients. Surgical treatment is indicated in patients who have radiologically proven cervical spondylolisthesis with instability and/or spinal cord compression. The choice of surgical approach depends on the stage of spondylolisthesis, the side and degree of spinal cord compression, and the possibility of correction by extension and positioning in order to restore a balanced spine. However, this issue remains unsolved. Shigematsu et al. [11] reported a 40% recovery rate of the JOA score in 15 patients treated with double-door laminoplasty. Dean et al. [10] concluded that anterior cervical decompression and fusion yielded excellent union rates and neurological improvement in 72 patients having cervical degenerative spondylolisthesis and significant neurological sequelae who had failed nonoperative treatments. Of these patients, three patients were treated with anterior decompression and fusion augmented with posterior facet fusion. However, the necessity for combined anterior-posterior fusion for high-grade or unstable spondylolisthesis also remains questionable. Regarding decompression, most authors preferred decompression for patients with degenerative cervical spondylolisthesis, while Deburge et al. [5] performed decompression only in two of eight patients. We suggest that decompression may not be necessary in patients without radiculopathy or myelopathy.
A potential limitation might be due to an incomplete literature search. We think, however, that PubMed includes the most important articles of this field. We assessed articles in English. Articles written in other languages may have been missed. That the reviewed literature did not evaluate the stability using the same criteria was another limitation. Clinical outcomes were reported in the reviewed literature, but they did not compare clinical outcomes between anterior surgery and posterior surgery, and also did not extensively explain the factors that may have an influence on clinical outcomes.
In general, degenerative cervical spondylolisthesis is always referred with neck or occipital pain, radiculopathy, and myelopathy or myeloradiculopathy. Degenerative cervical spondylolisthesis is most common in C3/4 and C4/5. Many patients with degenerative cervical spondylolisthesis have segmental instability as shown by flexion-extension lateral radiographs. There are two classification systems for degenerative cervical spondylolisthesis. Surgery was indicated in patients who had radiologically proven cervical spondylolisthesis with instability and/or spinal cord compression.
Although this systematic review represented the clinical presentation, radiological examination and management of degenerative cervical spondylolisthesis, prospective studies should be designed in the future to draw a more reliable conclusion about the management of degenerative cervical spondylolisthesis.
References
- 1.Li XF, Dai LY, Lu H, Chen XD. A systematic review of the management of hangman’s fractures. Eur Spine J. 2006;15:257–269. doi: 10.1007/s00586-005-0918-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hardouin P, Flipo RM, Foissac-Gegoux P, Thevenon A, Pouyol F, Duquesnoy B, Delcambre B. Current aspects of osteoarticular pathology in patients undergoing hemodialysis: study of 80 patients. Part 1. Clinical and radiological analysis. J Rheumatol. 1987;14:780–783. [PubMed] [Google Scholar]
- 3.Perlman R, Hawes LE. Cervical spondylolisthesis. J Bone Joint Surg Am. 1951;33:1012–1013. [PubMed] [Google Scholar]
- 4.Lee C, Woodring JH, Rogers LF, Kim KS. The radiographic distinction of degenerative slippage (spondylolisthesis and retrolisthesis) from traumatic slippage of the cervical spine. Skeletal Radiol. 1986;15:439–443. doi: 10.1007/BF00355101. [DOI] [PubMed] [Google Scholar]
- 5.Deburge A, Mazda K, Guigui P. Unstable degenerative spondylolisthesis of the cervical spine. J Bone Joint Surg Br. 1995;77:122–125. [PubMed] [Google Scholar]
- 6.Boulos AS, Lovely TJ. Degenerative cervical spondylolisthesis: diagnosis and management in five cases. J Spinal Disord. 1996;9:241–245. doi: 10.1097/00002517-199606000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Tani T, Kawasaki M, Taniguchi S, Ushida T. Functional importance of degenerative spondylolisthesis in cervical spondylotic myelopathy in the elderly. Spine. 2003;28:1128–1134. doi: 10.1097/01.BRS.0000067263.73474.97. [DOI] [PubMed] [Google Scholar]
- 8.Woiciechowsky C, Thomale UW, Kroppenstedt SN. Degenerative spondylolisthesis of the cervical spine–symptoms and surgical strategies depending on disease progress. Eur Spine J. 2004;13:680–684. doi: 10.1007/s00586-004-0673-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kawasaki M, Tani T, Ushida T, Ishida K. Anterolisthesis and retrolisthesis of the cervical spine in cervical spondylotic myelopathy in the elderly. J Orthop Sci. 2007;12:207–213. doi: 10.1007/s00776-007-1122-5. [DOI] [PubMed] [Google Scholar]
- 10.Dean CL, Gabriel JP, Cassinelli EH, Bolesta MJ, Bohlman HH. Degenerative spondylolisthesis of the cervical spine: analysis of 58 patients treated with anterior cervical decompression and fusion. Spine J. 2009;9:439–446. doi: 10.1016/j.spinee.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 11.Shigematsu H, Ueda Y, Takeshima T, et al. Degenerative spondylolisthesis does not influence surgical results of laminoplasty in elderly cervical spondylotic myelopathy patients. Eur Spine J. 2010;19:720–725. doi: 10.1007/s00586-010-1338-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.White AA, 3rd, Johnson RM, Panjabi MM, Southwick WO. Biomechanical analysis of clinical stability in the cervical spine. Clin Orthop Relat Res. 1975;109:85–96. doi: 10.1097/00003086-197506000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Epstein BS, Epstein JA, Jones MD. Degenerative spondylolisthesis with an intact neural arch. Radiol Clin North Am. 1977;15:275–287. [PubMed] [Google Scholar]
- 14.Fitzgerald JA, Newman PH. Degenerative spondylolisthesis. J Bone Joint Surg Br. 1976;58:184–192. doi: 10.1302/0301-620X.58B2.932080. [DOI] [PubMed] [Google Scholar]
- 15.Epstein JA, Carras R, Epstein BS, Levine LS. Myelopathy in cervical spondylosis with vertebral subluxation and hyperlordosis. J Neurosurg. 1970;32:421–426. doi: 10.3171/jns.1970.32.4.0421. [DOI] [PubMed] [Google Scholar]
- 16.Law MD, Jr, Bernhardt M, White AA., 3rd Evaluation and management of cervical spondylotic myelopathy. Instr Course Lect. 1995;44:99–110. [PubMed] [Google Scholar]
- 17.Penning L. Some aspects of plain radiography of the cervical spine in chronic myelopathy. Neurology. 1962;12:513–519. doi: 10.1212/wnl.12.8.518. [DOI] [PubMed] [Google Scholar]
- 18.Adams CB, Logue V. Studies in cervical spondylotic myelopathy. 3. Some functional effects of operations for cervical spondylotic myelopathy. Brain. 1971;94:587–594. doi: 10.1093/brain/94.3.587. [DOI] [PubMed] [Google Scholar]
- 19.Barnes MP, Saunders M. The effect of cervical mobility on the natural history of cervical spondylotic myelopathy. J Neurol Neurosurg Psychiatry. 1984;47:17–20. doi: 10.1136/jnnp.47.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hayashi H, Okada K, Hashimoto J, Tada K, Ueno R. Cervical spondylotic myelopathy in the aged patient. A radiographic evaluation of the aging changes in the cervical spine and etiologic factors of myelopathy. Spine. 1988;13:618–625. [PubMed] [Google Scholar]