Abstract
Acetabular retroversion may contribute to femoroacetabular impingement and lead to osteoarthritis of the hip. Retroversion has been measured on computed tomography scans. In recent years, assessment of acetabular version on anteroposterior pelvic views has gained increasing attention. We therefore aimed to determine the reliability of radiographic signs of acetabular retroversion and its association with the rater’s experience. Five orthopedic surgeons (o1 to o5) rated the crossover sign, ischial spine sign and posterior wall sign on X-rays of 40 hip joints. Also, we determined the rater’s experience in recognizing acetabular retroversion with a questionnaire and correlated intraobserver reliability to the calculated experience score. The intraobserver results were 0.325 (o1), 0.848 (o2), 0.684 (o3), 0.701 (o4), and 1.000 (o5) for the crossover sign, 0.750 (o1), 0.890 (o2), 0.593 (o3), 0.483 (o4), and 0.946 (o5) for the posterior wall sign; and 0.578 (o1), 0.680 (o2), 0.595 (o3), 0.375 (o4), and 0.800 (o5) for the ischial spine sign. Interobserver reliability was 0.514 for the crossover, 0.633 for the posterior, and 0.543 for the ischial spine sign wall. The experience sum score correlated to the kappa results for the crossover (r=0.527), posterior wall (r=0.738), and ischial spine sign (r=0.949). Assessing acetabular version on plain radiographs is subject to intra- and interindividual error and related to the observer’s individual experience.
Introduction
Acetabular retroversion may lead to pincer type femoro-acetabular impingement [1] and osteoarthritis of the hip [2, 3]. Up to 48 percent of the overall population may be affected by posterior orientation of the acetabular aperture [4]. Radiographic signs of acetabular retroversion [5] and accompanying insufficient posterior femoral head coverage have been described [6, 7]. As plain radiographs increase in popularity they are beginning to supplant computed tomography scans for the determination of acetabular version [6, 7]. Recognising acetabular retroversion on X-rays is dependent on the extent of retroversion and correct radiographic technique [8, 9]. It was our intention to accurately define the reliability of the crossover, posterior wall [6] and ischial spine sign [5]. Also, we analysed the impact of personal experience on that reliability.
Materials and methods
Forty hip joints on 20 anteroposterior (AP) pelvic X-rays of patients treated for non-arthritic hip pain were randomly chosen by one orthopaedic surgeon experienced in judging acetabular version on radiographs. There were 15 female and five male patients with a mean age of 26.2 ± 8.7 years (range, 16.4–44.6 years).
At our institution, pelvic radiographs are obtained in the supine position with both hips fully extended and internally rotated 20 degrees. The film-focus-distance is 120 cm. The central beam is directed to the midpoint of a line connecting the symphysis to the midpoint of a line connecting both anterior superior iliac spines. Care was taken to choose physiologically inclined (distance between tip of coccyx and symphysis was 1–2 cm) [9] and non-malrotated radiographs (tip of coccyx pointing to symphysis) for this study. The 20 X-ray films were independently presented to five orthopaedic surgeons from a department for orthopaedic surgery that annually performs approximately 200 hip preserving operations. The observers rated three signs of acetabular retroversion on two occasions six weeks apart to be either present or not. Prior to first judgment, each observer filled out a questionnaire investigating his or her individual experience in the application of retroversion assessment (see Appendix).
The signs for acetabular retroversion were the crossover sign [6], the posterior wall sign [6] (which actually indicates insufficient posterior femoral head coverage accompanying acetabular retroversion), and the ischial spine sign [5]. The crossover sign was considered positive when the anterior and posterior acetabular borders crossed prior to meeting at the lateral border of the weight bearing zone [6] (Fig. 1). The posterior wall sign was considered positive when the centre of the femoral head lay lateral to the posterior acetabular border [6] (Fig. 2). The ischial spine sign was considered positive when the ischial spine projected inside the pelvic cavity [5] (Fig. 3).
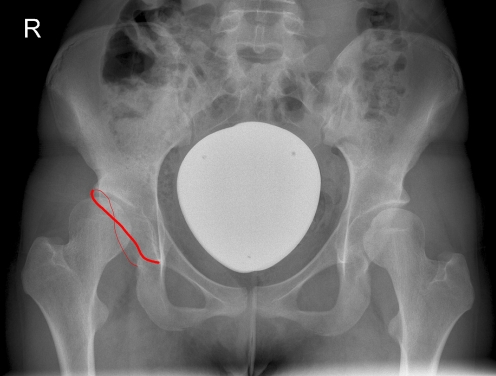
Fig. 1.
Anteroposterior radiograph of a 22-year-old female with hip dysplasia and a positive cross over sign at the right sided hip joint. The broad line marks the anterior, the slim line the posterior acetabular rim
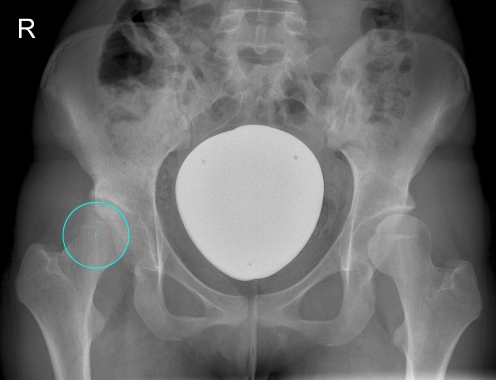
Fig. 2.
The same anteroposterior view as in Fig. 1 with the posterior wall sign; the centre of the femoral head is located lateral to the posterior acetabular rim
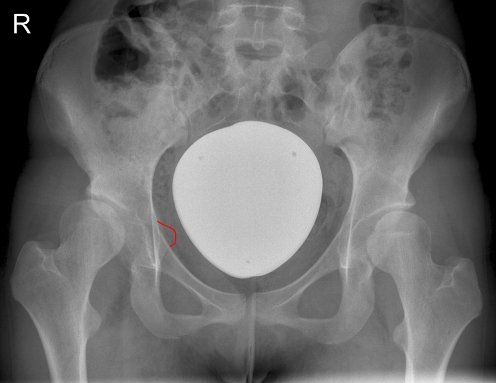
Fig. 3.
The same anteroposterior view as in Fig. 1 with the ischial spine projecting into the pelvis marked by the solid line indicating a positive ischial spine sign
To estimate intraobserver agreement, agreement in percentage terms, McNemar's test (to exclude a significant difference between repeated judgments), the phi-coefficient (analysing the strength of agreement between repeated measurements), and Cohen’s kappa (intraobserver reliability) were calculated. For interobserver reliability, agreement in percentage and Fleiss’ kappa were calculated.
We evaluated experience in judging acetabular retroversion by a 17-item questionnaire (see Appendix). Questions were formulated so that positive answers indicated experience. One point was assigned to each positive answer so that a high sum score indicated experience. Results of kappa intraobserver reliability were correlated to the sum scores by Kendall’s tau. Similarly, kappa intraobserver reliability results were correlated to years of clinical experience.
We used SPSS version 17 (SPSS, Chicago, Illinois) for statistical analysis. The results for Cohen’s kappa were ranked according to Landis and Koch [10]. Significance was assumed for p < 0.05. We obtained approval from our institutional review board (inquiry 300/09).
Results
Intraobserver reliability was fair to perfect with an average kappa value of 0.712 and a phi-coefficient of 0.727 for the crossover sign, 0.732 and 0.752 for the posterior wall sign, and 0.625 and 0.653 for the ischial spine sign. Between repeated measurements, no significant difference was detected with McNemar’s test except for one observer’s posterior wall sign judgement (Table 1). Interobserver reliability was moderate for the crossover and ischial spine sign and substantial for the posterior wall sign (Table 2).
Table 1.
Intraobserver measurements
| Intraobserver measurements | Agreement | McNemar’s test | Phi-coefficient | Cohen’s kappa | p |
|---|---|---|---|---|---|
| Observer 1 | |||||
| Crossover sign | 0.65 | 0.057 | 0.353 | 0.325 | 0.26 |
| Posterior wall sign | 0.86 | 0.375 | 0.759 | 0.750 | <0.0001 |
| Ischial spine sign | 0.80 | 0.289 | 0.591 | 0.578 | <0.0001 |
| Observer 2 | |||||
| Crossover sign | 0.93 | 0.250 | 0.858 | 0.848 | <0.0001 |
| Posterior wall sign | 0.95 | 0.500 | 0.896 | 0.890 | <0.0001 |
| Ischial spine sign | 0.85 | 1.000 | 0.680 | 0.680 | <0.0001 |
| Observer 3 | |||||
| Crossover sign | 0.88 | 0.063 | 0.721 | 0.684 | <0.0001 |
| Posterior wall sign | 0.83 | 1.000 | 0.594 | 0.593 | <0.0001 |
| Ischial spine sign | 0.80 | 0.289 | 0.608 | 0.595 | <0.0001 |
| Observer 4 | |||||
| Crossover sign | 0.85 | 0.687 | 0.704 | 0.701 | <0.0001 |
| Posterior wall sign | 0.80 | 0.040 | 0.564 | 0.483 | <0.0001 |
| Ischial spine sign | 0.90 | 0.250 | 0.480 | 0.375 | 0.002 |
| Observer 5 | |||||
| Crossover sign | 1.00 | 1.000 | 1.000 | 1.000 | <0.0001 |
| Posterior wall sign | 0.98 | 1.000 | 0.947 | 0.946 | <0.0001 |
| Ischial spine sign | 0.95 | 0.500 | 0.904 | 0.899 | <0.0001 |
Table 2.
Interobserver measurements
| Intraobserver measurements | Crossover sign | Posterior wall sign | Ischial spine sign |
|---|---|---|---|
| Agreement (%) | 77.1 | 82.9 | 77.5 |
| Fleiss’ kappa | 0.514 | 0.633 | 0.543 |
The sum score for observer’s experience ranged from 6 to 17. Kendal’s tau results for the correlation with years of clinical experience was −0.111, and for the correlation with kappa results were 0.527 (crossover sign), 0.738 (posterior wall sign), and 0.949 (ischial spine sign).
Discussion
The normal human acetabulum is anteverted in order to allow impingement free range of motion including flexion, adduction, and internal rotation. Acetabular retroversion may occur in hip dysplasia [11], Legg-Calvé-Perthes disease [12], bladder exstrophy complex [13], proximal femoral focal deficiency [14], or after pelvic osteotomy [15, 16] and may lead to labral tearing [17], pincer type femoro-acetabular impingement [1], possibly femoral neck stress fractures [18] and osteoarthritis [2, 3].
Acetabular version is conventionally evaluated on CT scans [6, 7]. After the concept of femoro-acetabular impingement was introduced, radiographic signs for acetabular retroversion started to be increasingly recognised. These signs are however only just beginning to be used in everyday clinical practice and are not yet part of the regular medical university curriculum. Therefore, learning to recognise acetabular retroversion starts with residency. Correct judgment of acetabular retroversion is dependent on pelvic rotation and inclination [9]. Signs of acetabular retroversion also vary with the extent of retroversion. Therefore, judging acetabular retroversion requires accurate teaching and involves a learning process.
In this study, we aimed to determine the intra- and interobserver reliability of three popular radiographic signs of acetabular retroversion: the crossover [6], posterior wall [6], and ischial spine sign [5]. We found that while all three signs displayed substantial intra-observer agreement, only the posterior wall sign had substantial interobserver agreement on average. We also demonstrated that reliability depends on experience with the identification of retroversion rather than years of clinical practice, even in a department specialised in hip preserving surgery.
Our findings are in concordance with the results of Clohisy et al. who found kappa values for the assessment of acetabular version of 0.46 for intra-observer and 0.39 for intra-observer reliability [19]. Kalberer et al. found superior values for intraobserver and intra-observer reliability for both the crossover and ischial spine sign (intra-observer 0.83 and 0.92, intra-observer 0.92 and 0.91) [5]. Our results for the crossover sign reliability are comparable to the results of Jamali et al. [20] (intra-observer 0.647 and 0.698, intra-observer 0.628 and 0.698) or Tannast et al. [21] (interclass correlation coefficient 0.73–0.77 for intra-observer and 0.60 for the interobserver reliability). The latter also found comparable intra-observer (0.70 and 0.68) and interobserver reliability (0.62) for the posterior wall sign [21].
Radiographic signs of acetabular retroversion are susceptible to erroneous judgment. They tend to be false positive and increase in magnitude with increasing pelvic tilt and rotation to the affected side [9]. Also, usually only the superior part of the acetabulum is retroverted [6, 20]. This leads to the acetabular borders crossing over in the lateral part of the acetabulum and the impression of “a slight deformity” that may escape diagnosis. Furthermore, the posterior wall sign literally is a sign for insufficient posterior femoral head coverage and may also be positive in global insufficient coverage without acetabular retroversion, e.g. hip dysplasia. Furthermore, the ischial spine sign may be underestimated in pelves underexposed to radiation. Even though we paid close attention to excluding underexposed, malinclined and malrotated radiographs from our study, this is a potential source of misjudgment especially for the ischial spine and also for the crossover sign. The aforementioned are not a weakness inherent to our study but to signs of acetabular retroversion on plain radiographs in general. At least in cases of uncertainty, the gold standard of computed tomography still remains, even though determination of version is also dependent to pelvic inclination in computed tomography [22]. We did not use computed tomography data for this study since it was not our purpose to define the validity of radiographic retroversion signs, which has been done before [5, 20].
In summary, we conclude that the crossover, posterior wall, and ischial spine sign posses substantial intraobserver but only moderate to substantial interobserver reliability. Teaching how to recognise acetabular retroversion is the responsibility of orthopaedic surgeons performing hip preserving surgery in order to minimise false diagnoses in patients with hip disability. Prior to surgical treatment for isolated acetabular retroversion, we would recommend confirmation of the diagnosis by computed tomography.
Appendix
The 17-item questionnaire for determining experience with acetabular retroversion signs:
I am familiar with acetabular retroversion. yes/no
I am confident I can judge acetabular retroversion on a plain X-ray without additional imaging. yes/no
I am familiar with the crossover sign. yes/no
I am familiar with the posterior wall sign. yes/no
I am familiar with the ischial spine sign. yes/no
I use the crossover sign in my everyday practice. yes/no
I use the posterior wall sign in my everyday practice. yes/no
I use the ischial spine sign in my everyday practice. yes/no
I use the crossover sign to judge acetabular version in my everyday practice. yes/no
I use the posterior wall sign to judge acetabular version in my everyday practice. yes/no
I use the ischial spine sign to judge acetabular version in my everyday practice. yes/no
I know scientific publications describing or using the crossover sign. yes/no
I know scientific publications describing or using the posterior wall sign. yes/no
I know scientific publications describing or using the ischial spine sign. yes/no
Acetabular retroversion is associated with osteoarthritis of the hip. yes/no
Acetabular version can contribute to femoroacetabular impingement. yes/no
Acetabular version can lead to pincer type femoroacetabular impingement. yes/no
References
- 1.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85-A(2):278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 2.Kim WY, Hutchinson CE, Andrew JG, Allen PD. The relationship between acetabular retroversion and osteoarthritis of the hip. J Bone Joint Surg Br. 2006;88(6):727–729. doi: 10.1302/0301-620X.88B6.17430. [DOI] [PubMed] [Google Scholar]
- 3.Giori NJ, Trousdale RT. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:263–269. doi: 10.1097/01.blo.0000093014.90435.64. [DOI] [PubMed] [Google Scholar]
- 4.Werner CM, Copeland CE, Ruckstuhl T, Stromberg J, Seifert B, Turen CH. Prevalence of acetabular dome retroversion in a mixed race adult trauma patient population. Acta Orthop Belg. 2008;74(6):766–772. [PubMed] [Google Scholar]
- 5.Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M. Ischial spine projection into the pelvis : a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466(3):677–683. doi: 10.1007/s11999-007-0058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81(2):281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 7.Dandachli W, Islam SU, Liu M, Richards R, Hall-Craggs M, Witt J. Three-dimensional CT analysis to determine acetabular retroversion and the implications for the management of femoro-acetabular impingement. J Bone Joint Surg Br. 2009;91(8):1031–1036. doi: 10.1302/0301-620X.91B8.22389. [DOI] [PubMed] [Google Scholar]
- 8.Kakaty DK, Fischer AF, Hosalkar HS, Siebenrock KA, Tannast M. The ischial spine sign: does pelvic tilt and rotation matter? Clin Orthop Relat Res. 2009;468(3):769–774. doi: 10.1007/s11999-009-1021-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 10.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 11.Li PL, Ganz R. Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop Relat Res. 2003;416:245–253. doi: 10.1097/01.blo.0000081934.75404.36. [DOI] [PubMed] [Google Scholar]
- 12.Ezoe M, Naito M, Inoue T. The prevalence of acetabular retroversion among various disorders of the hip. J Bone Joint Surg Am. 2006;88(2):372–379. doi: 10.2106/JBJS.D.02385. [DOI] [PubMed] [Google Scholar]
- 13.Nehme A, Oakes D, Perry MJ, Hawatmeh SI, Trousdale RT. Acetabular morphology in bladder exstrophy complex. Clin Orthop Relat Res. 2007;458:125–130. doi: 10.1097/BLO.0b013e3180380ed1. [DOI] [PubMed] [Google Scholar]
- 14.Dora C, Buhler M, Stover MD, Mahomed MN, Ganz R. Morphologic characteristics of acetabular dysplasia in proximal femoral focal deficiency. J Pediatr Orthop B. 2004;13(2):81–87. doi: 10.1097/00009957-200403000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Kiyama T, Naito M, Shiramizu K, Shinoda T. Postoperative acetabular retroversion causes posterior osteoarthritis of the hip. Int Orthop. 2009;33(3):625–631. doi: 10.1007/s00264-007-0507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dora C, Mascard E, Mladenov K, Seringe R. Retroversion of the acetabular dome after Salter and triple pelvic osteotomy for congenital dislocation of the hip. J Pediatr Orthop B. 2002;11(1):34–40. doi: 10.1097/00009957-200201000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Wenger DE, Kendell KR, Miner MR, Trousdale RT. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004;426:145–150. doi: 10.1097/01.blo.0000136903.01368.20. [DOI] [PubMed] [Google Scholar]
- 18.Kuhn KM, Riccio AI, Saldua NS, Cassidy J. Acetabular retroversion in military recruits with femoral neck stress fractures. Clin Orthop Relat Res. 2009;468(3):846–851. doi: 10.1007/s11999-009-0969-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clohisy JC, Carlisle JC, Trousdale R, Kim YJ, Beaule PE, Morgan P, et al. Radiographic evaluation of the hip has limited reliability. Clin Orthop Relat Res. 2009;467(3):666–675. doi: 10.1007/s11999-008-0626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, et al. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res. 2007;25(6):758–765. doi: 10.1002/jor.20380. [DOI] [PubMed] [Google Scholar]
- 21.Tannast M, Mistry S, Steppacher SD, Reichenbach S, Langlotz F, Siebenrock KA, et al. Radiographic analysis of femoroacetabular impingement with Hip2Norm-reliable and validated. J Orthop Res. 2008;26(9):1199–1205. doi: 10.1002/jor.20653. [DOI] [PubMed] [Google Scholar]
- 22.Kohnlein W, Ganz R, Impellizzeri FM, Leunig M. Acetabular morphology: implications for joint-preserving surgery. Clin Orthop Relat Res. 2009;467(3):682–691. doi: 10.1007/s11999-008-0682-9. [DOI] [PMC free article] [PubMed] [Google Scholar]