Abstract
Total hip replacement has shown good outcomes for patients with rheumatoid arthritis. Can hip resurfacing give similar results for patients with rheumatoid arthritis? Using an international hip resurfacing register, 47 patients with rheumatoid arthritis were identified and age and gender matched to a group of 131 randomly selected patients with osteoarthritis of the hip joint. Patients completed a questionnaire to record function and implant revision. Hierarchical regression, Cox regression and Kaplan-Meier method were used for analysis. There was a significant increase in post operative hip score in both groups (p < 0.001) with rheumatoid group scoring higher as compared to the osteoarthritis group (p = 0.23). The post operative score was not significantly influenced by pre-operative score and age (p = 0.15 and 0.84, respectively) but the pre-operative score was a predictor of implant failure (p = 0.02). Patient mobility was affected by age with younger patients scoring high on mobility as compared to older patients (p = 0.01). The Kaplan-Meier analysis showed a survival rate of 96.3% in the rheumatoid group and 97.8% in the osteoarthritis group. This difference was not significant (Log rank test, p = 0.45). Our results from an independent and international register show that hip resurfacing provides good post-operative hip function and excellent implant survival for patients with rheumatoid arthritis of the hip joint. This procedure can be considered as a viable option for management of rheumatoid arthritis of the hip joint.
Introduction
Rheumatoid arthritis is a complex condition with an overall incidence of 1% in the general population. It has a progressive course, leads to significant disability and predisposes to increased mortality. The protocols for management of this condition vary from anti-inflammatory medication to joint arthroplasty [25, 29, 30]. In spite of recent refinements in the medical management of this condition, its progressive nature leads to disability and loss of quality of life. When this medical therapy fails to control the disease process, these patients become candidates for surgical treatment. Although the incidence of rheumatoid hips undergoing surgery is gradually declining [28], some patients do end up with hip arthroplasty.
Total hip arthroplasty for rheumatoid arthritis provides a complete relief from pain and stiffness, reduces morbidity, gives good to excellent function and implant survival in mid- to long-term follow-up [4, 6, 23, 43, 48, 50, 53, 56]. These results are, however, beset by complications of total hip arthroplasty such as aseptic loosening, deep infections, dislocations and periprosthetic fractures. The incidence of these complications is above average in patients with rheumatoid arthritis of the hip joint and they are responsible for most of the revisions following total hip arthroplasty [5, 7, 26, 27, 42, 55].
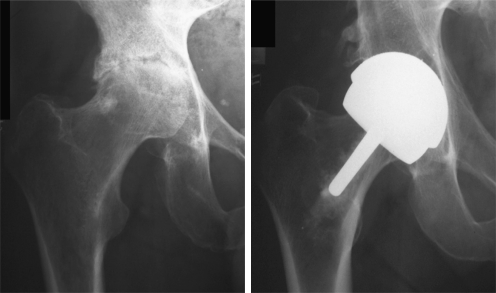
Metal-on-metal hip resurfacing is a new procedure for hip joint replacement which aims to preserve femoral bone stock and provides high levels of activity in young patients [33, 44] (Fig. 1). The short- to mid-term results of this procedure have been promising, especially in patients with osteoarthritis of the hip joint [1, 14, 15, 40, 52]. Favourable results have also been reported for management of osteonecrosis and dysplasia of the hip joint [2, 32, 36, 41]. Kim et al. [20] reported good results following THARIES resurfacing in rheumatoid patients but similar results have not been reported for the new generation metal-on-metal hip resurfacing. As recent as 2006, surgeons have been advised to be cautious in offering resurfacing arthroplasty to patients with rheumatoid arthritis [35]. However, the recommendations of the FDA [16] do include rheumatoid arthritis as an indication for resurfacing arthroplasty. It is unclear if metal-on-metal hip resurfacing should be considered as an option for the management of patients with rheumatoid arthritis.
Fig. 1.
Pre-op and five year post-op radiographs of a patient with rheumatoid arthritis managed with hip resurfacing
The aim of this study was to discover if metal-on-metal hip resurfacing can provide comparable results for patients with rheumatoid arthritis as it does for patients with osteoarthritis, osteonecrosis and hip dysplasia.
Patients and methods
Between 1997 and 2002, 4,536 patients were registered in a prospective multicentre registry by the outcome centre. We identified all 47 patients who had rheumatoid arthritis of the hip joint and constructed an age and gender matched cohort of another 131 patients who had osteoarthritis of the hip joint. These patients were enrolled in this study by 51 surgeons from 13 different countries. All patients were entered in this study after written informed consent. This study was approved by the institutional review board and also by the regional ethics committee.
Demographic and clinical details of each patient were provided by the respective operating surgeon. These details were stored on a secure electronic database in the Outcome Centre and patients were followed up annually to determine outcomes of function, complications, revision and death. This was done via a standard questionnaire which included a Harris hip score [13] modified for patient self assessment. The patient details were kept up to date by postal, telephonic and electronic channels. In case the patients did not mail a reply, they were contacted via email or telephone and any change in address was updated. In case this approach failed, the respective surgeons were contacted and they helped to restore communication. This ensured that no patients were lost to follow-up. All patients had uncemented acetabular and cemented femoral hip resurfacing with Birmingham Hip Resurfacing implant (Smith & Nephew, Warwick, UK) using the posterior approach.
The data was checked for errors and normality and the two groups of patients with OA and RA were compared with respect to demographics, function, complications and implant survival. The Kaplan-Meier method [17] was used to calculate implant survival in both groups and the Log rank test was used to compare the implant survival in both groups. The basis of the Kaplan-Meier method is estimation of survival probability of the remaining subjects in a study for a specified event. This method is commonly used in mortality studies but the event is not limited to that and can be used for estimation of time-specific probabilities for the failure of an instrument or device of a certain type. In this study each patient reported a functional score annually over a period of 11 years. This data therefore forms a nested repeated measure where a number of annual scores are nested within each patient. We used hierarchical regression or multilevel modelling to compare the scores between two groups of patients. An advantage of multilevel modelling over repeated measures ANOVA is that the latter is unable to handle missing values in data and thus deletes all observations related to patients with a missing score [11, 12, 24, 39]. Multilevel modelling is capable of handling this which helps to use all the available data for analysis. Annual post-operative scores were used as dependent variables and we used preoperative diagnosis, age at operation, preoperative score and gender as independent variables for this analysis. A Cox model was used to evaluate influence of pre-operative score, gender, pre-operative diagnosis and age on the risk of failure. All statistical analysis was done using STATA 9.0 software package (STATA Corp, Texas, US). A p value less than 0.05 was considered significant in all analyses.
Results
Demographics
The rheumatoid group consisted of 47 patients (54 hips) with 23 males and 24 females whereas the osteoarthritis group had 131 patients (138 hips) with 61 males and 70 females. There were seven bilateral procedures in each group with two males and five females in the rheumatoid group and one male and six females in the osteoarthritis group. The mean age of the rheumatoid group was 43.1 years (range 19.5–66.7) and that of the osteoarthritis group was 43 years (range 16.1–67). A comparison of age distribution in both groups using an independent t-test showed no significant difference (p = 0.97). The mean follow-up for the rheumatoid group was 8.1 years (range 6.5–11.1) and that for the osteoarthritis group was 8.4 years (range 6.5–11.1). No patients were lost to follow-up but there were four deaths during the follow-up period. Two patients from rheumatoid group died after five and 7.8 years following the operation. In the osteoarthritis group one patient died 6.7 years post-op and another one year postoperatively and this death was unrelated to the procedure.
Implant survival
There were two failures in the rheumatoid group and three in the osteoarthritis group. In the rheumatoid group there was one femoral neck fracture two months after surgery and one patient had an infection after 5.3 years. In the osteoarthritis group two patients were revised for aseptic loosening at two and 2.7 years postoperative. Another patient was revised after five years due to severe pain and intraoperative findings of metallosis were reported by the operating surgeon. All patients were revised to a cemented total hip replacement. The Kaplan-Meier analysis showed a survival rate of 96.3% in the rheumatoid group and 97.8% in the osteoarthritis group. This difference was not significant (log-rank test, p = 0.45).
Function
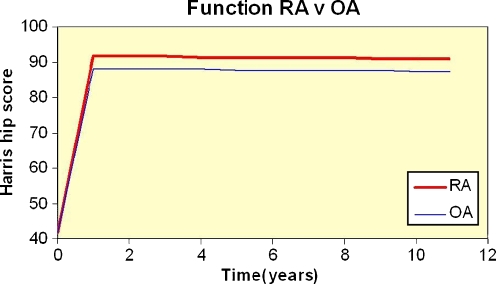
The mean preoperative score in both groups were similar. Independent t-test showed no difference in the preoperative scores (p = 0.99). The overall average score at one year post-op was 91.6 and this increase was highly significant (p < 0.001). The score at the latest follow-up was higher by 3.6 points in the rheumatoid group as compared to the osteoarthritis group, but this difference was not significant (p = 0.23). There was a difference of 2.8 points between males and females with the latter scoring low, but this difference was not significant (p = 0.40). The preoperative score and age at operation were not very significant predictors of functional outcome (p =0.15 and 0.84, respectively), but patients with a higher pre-operative score did have a higher post-operative score. There was an annual decline in function by a minimal 0.07 points but this was not significant (p = 0.76). The resultant score at 11 years was 90.9 in the RA group and 87.4 in the OA group (Fig. 2). Using Cox regression we found a significant effect of pre-operative functional score on implant failure (p = 0.02). The patients with higher pre-operative functional score had a slight but significantly lower risk of failure as compared to a lower pre-operative score (hazard ratio 0.93) (95% CI 0.87–0.99).
Fig. 2.
Comparative hip function following hip resurfacing for rheumatoid arthritis and osteoarthritis
Further analysis of individual domains of pain, mobility and range of motion showed a significant improvement in all three domains (p < 0.001) with maximum change in range of motion. A higher pre-operative score in these individual domains resulted in higher post-operative score, but this effect was not significant for range of motion (p = 0.40). These effects were highly significant for pain and mobility (p < 0.01). None of the other predictors significantly influenced post-operative pain, mobility and range of motion scores except age, which had a significant effect on post-operative mobility scores with increasing age resulting in lower post-op mobility scores (p = 0.01).
Discussion
Our study is an independent assessment of an international and multi-surgeon cohort. At a maximum follow-up of 11 years, the results from our centre show an excellent implant survival of 96.3% following hip resurfacing in patients with rheumatoid arthritis of the hip joint. The modified Harris hip score improved from an average of 42 to 91 after first year post-op.
Results from our independent and international hip resurfacing register contrast with results published from other total hip arthroplasty registers. Norwegian arthroplasty register reports a ten year implant survival of 79.4% for total hip arthroplasty in patients with rheumatoid arthritis of hip who were younger than 60 years of age [10]. Similarly, results from the Finnish arthroplasty register show an implant survival of 85–87% in patients aged 55 years and younger [9]. These comparative statistics show that implant survival was better in patients who had hip resurfacing than to those who had total hip replacement. To discover if this difference is really true and to account for other variables such as disease stage, activity level and surgical technique, there is a need for a prospective randomised trial.
Postoperative function is one of the most important outcomes for patients with rheumatoid arthritis. Our results echo the published reports of total hip arthroplasty for rheumatoid arthritis [6, 18, 19, 21, 22, 56]. In our study the patients with rheumatoid arthritis scored higher than patients with osteoarthritis, although this difference was not significant. This is in contrast to the results reported by other authors [21, 37, 56] where patients with OA have shown better results than RA. This may be due to the prosthesis itself, as hip resurfacing offers improved range of motion [35, 46] which can contribute to better function. Interestingly, age had an inverse effect on post-op mobility scores. Expectations from a total hip arthroplasty are higher in young patients as compared to old patients. This may be a contributing factor to the results seen above.
Total hip arthroplasty for rheumatoid arthritis provides pain relief and improves function, but it is associated with a relatively higher risk of complications as compared to osteoarthritis [3, 51]. The rate of dislocation following total hip arthroplasty for rheumatoid arthritis has been reported in different case series and arthroplasty registers varying from 2% to 10% [7, 11, 54, 55]. In our study there were no dislocations following hip resurfacing in rheumatoid patients. In a retrospective multivariate analysis of more than 6,000 total hip arthroplasties, Berry et al. reported a statistically significant relative risk of 1.5 in patients with inflammatory arthritis as compared to osteoarthritis [3]. It has been suggested that soft tissues are affected by the disease and this leads to inadequate soft tissue tension [55]. Another risk factor for dislocation following total hip arthroplasty is the size of femoral head; a large head (>32 mm) reduces the risk of dislocation following total hip replacement [5, 51]. It may suffice to say that hip resurfacing can help reduce the risk of dislocation in patients with rheumatoid arthritis of the hip joint.
Another complication which has a higher than normal incidence following hip arthroplasty in patients with rheumatoid arthritis is periprosthetic fractures of the femur. Results from the Finnish arthroplasty register show an incidence of 1.8% [9]; whereas in a report from Swedish registers, other case series report a hazard ratio of 1.56–2.1 [26, 27, 42] as compared to OA. It is well established that rheumatoid arthritis has a detrimental effect on bone growth and decreases the bone mineral density [34, 47, 49]. These effects tend to cause osteoporosis and weaken the femoral neck. There was only one neck of femur fracture in our study and it is possible that this complication was due to the procedure rather than underlying diagnosis. Indeed, fracture neck of femur is the most common complication in the first year following hip resurfacing arthroplasty [31, 45].
Limitations recognised in our study include lack of radiographic follow-up. This is because our database is comparable to a joint registry and radiographic information is not recorded. Our centre does however collect annual hip scores, and postoperative clinical scores have shown strong correlation with radiographic loosening following total hip replacement [8, 38]. We propose that future studies should try to include radiographic outcomes for follow-up of hip arthroplasty in patients with rheumatoid arthritis. Other limitations include the mid-term follow-up of this study and a relatively low number of patients, and thus a longer follow-up of a large cohort is necessary to establish the credibility of this procedure for management of rheumatoid arthritis.
Harris hip score is the only outcome measure used for assessing function in this study. Patients with rheumatoid arthritis generally have a polyarticular disease and Harris hip score is a specific outcome measure that reports hip joint function only. It does not necessarily relate to improvements in general function. We suggest that a generic outcome measure such as SF-36 or HAQ score be used in future studies to report outcomes of surgical procedures for rheumatoid arthritis patients.
The results of this study suggest that hip resurfacing provides good function and comparable implant survival in patients who have rheumatoid arthritis of the hip joint. With no dislocations following hip replacement, this procedure might help to reduce the incidence of this complication in patients with rheumatoid arthritis. In conclusion, hip resurfacing may be considered as a viable option for management of rheumatoid arthritis of the hip joint.
Acknowledgments
Conflict of interest No conflicts of interest are reported.
Footnotes
Research funding was received from Smith & Nephew, UK.
Institutional Review Board (IRB)/Ethics Committee approval was obtained.
References
- 1.Amstutz HC, Beaule PE, Dorey FJ, Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six year follow-up study. J Bone Joint Surg Am. 2004;86:28. [PubMed] [Google Scholar]
- 2.Amstutz HC, Duff MJ, Harvey N, Hoberg M. Improved survivorship of hybrid metal-on-metal hip resurfacing with second-generation techniques for Crowe-I and II developmental dysplasia of the hip. J Bone Joint Surg Am. 2008;90(Suppl 3):12–20. doi: 10.2106/JBJS.H.00711. [DOI] [PubMed] [Google Scholar]
- 3.Berry DJ, Knoch M, Schleck CD, Harmsen WS. The cumulative long-term risk of dislocation after primary Charnley total hip arthroplasty. J Bone Joint Surg Am. 2004;86(1):9–14. doi: 10.2106/00004623-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Berry DJ, Scott Harmsen W, Cabanella ME, Morrey BF. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements. Factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am. 2002;84:171–177. doi: 10.2106/00004623-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Conroy JL, Whitehouse SL, Graves SE, Pratt NL, Ryan P, Crawford RW. Risk factors for revision for early dislocation in total hip arthroplasty. J Arthroplasty. 2008;23(6):867–872. doi: 10.1016/j.arth.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Cracchiolo A, Severt R, Moreland J. Uncemented total hip arthroplasty in rheumatoid arthritis diseases. A two- to six-year follow-up study. Clin Orthop Relat Res. 1992;277:166–174. [PubMed] [Google Scholar]
- 7.Creighton MG, Callaghan JJ, Olejniczak JP, Johnston RC. Total hip arthroplasty with cement in patients who have rheumatoid arthritis. A minimum ten-year follow-up study. J Bone Joint Surg Am. 1998;80(10):1439–1446. doi: 10.2106/00004623-199810000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Devitt A, O'Sullivan T, Quinlan W. 16- to 25-year follow-up study of cemented arthroplasty of the hip in patients aged 50 years or younger. J Arthroplasty. 1997;12(5):479–489. doi: 10.1016/S0883-5403(97)90169-8. [DOI] [PubMed] [Google Scholar]
- 9.Eskelinen A, Paavolainen P, Helenius L, Pulkkinen P, Remes V. Total hip arthroplasty for rheumatoid arthritis in younger patients: 2,557 replacements in the Finnish Arthroplasty Register followed for 0–24 years. Acta Orthop. 2006;77:853–865. doi: 10.1080/17453670610013132. [DOI] [PubMed] [Google Scholar]
- 10.Furnes O, Lie SA, Espehaug B, Vollset SE, Engesaeter LB, Havelin LI. Hip disease and the prognosis of total hip replacements. A review of 53,698 primary total hip replacements reported to the Norwegian Arthroplasty Register 1987–99. J Bone Joint Surg Br. 2001;83(4):579–586. doi: 10.1302/0301-620X.83B4.11223. [DOI] [PubMed] [Google Scholar]
- 11.Gilthorpe MS, Cunningham SJ. The application of multilevel, multivariate modeling to orthodontic research data. Community Dent Health. 2000;17(4):236–242. [PubMed] [Google Scholar]
- 12.Goldstein H, Browne W, Rasbash J. Multilevel modeling of medical data. Stat Med. 2002;21(21):3291–3315. doi: 10.1002/sim.1264. [DOI] [PubMed] [Google Scholar]
- 13.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty: an end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 14.Heilpern GN, Shah NN, Fordyce MJ. Birmingham hip resurfacing arthroplasty: a series of 110 consecutive hips with a minimum five-year clinical and radiological follow-up. J Bone Joint Surg Br. 2008;90(9):1137–1142. doi: 10.1302/0301-620X.90B9.20524. [DOI] [PubMed] [Google Scholar]
- 15.Hing CB, Back DL, Bailey M, Young DA, Dalziel RE, Shimmin AJ. The results of primary Birmingham hip resurfacings at a mean of five years. An independent prospective review of the first 230 hips. J Bone Joint Surg Br. 2007;89(11):1431–1438. doi: 10.1302/0301-620X.89B11.19336. [DOI] [PubMed] [Google Scholar]
- 16.US Food and Drug Association (2009) Birmingham hip resurfacing (BHR) system - P040033. http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/DeviceApprovalsandClearances/Recently-ApprovedDevices/ucm078189.htm. Accessed 18th September 2009
- 17.Kaplan E, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457. doi: 10.2307/2281868. [DOI] [Google Scholar]
- 18.Katsimihas M, Taylor AH, Lee MB, Sarangi PP, Learmonth ID. Cementless acetabular replacement in patients with rheumatoid arthritis: a 6- to 14-year prospective study. J Arthroplasty. 2003;18(1):16–22. doi: 10.1054/arth.2003.50012. [DOI] [PubMed] [Google Scholar]
- 19.Keisu KS, Orozco F, McCallum JD, Bissett G, Hozack WJ, Sharkey PF, et al. Cementless femoral fixation in the rheumatoid patient undergoing total hip arthroplasty: minimum 5-year results. J Arthroplasty. 2001;16(4):415–421. doi: 10.1054/arth.2001.23506. [DOI] [PubMed] [Google Scholar]
- 20.Kim WC, Grogan T, Amstutz HC, Dorey F. Survivorship comparison of THARIES and conventional hip arthroplasty in patients younger than 40 years old. Clin Orthop Relat Res. 1987;214:269–277. [PubMed] [Google Scholar]
- 21.Kirwan JR, Currey HL, Freeman MA, Snow S, Young PJ. Overall long-term impact of total hip and knee joint replacement surgery on patients with osteoarthritis and rheumatoid arthritis. Br J Rheumatol. 1994;33(4):357–360. doi: 10.1093/rheumatology/33.4.357. [DOI] [PubMed] [Google Scholar]
- 22.Lachiewicz PF. Porous-coated total hip arthroplasty in rheumatoid arthritis. J Arthroplasty. 1994;9(1):9–15. doi: 10.1016/0883-5403(94)90132-5. [DOI] [PubMed] [Google Scholar]
- 23.Lehtimäki MY, Kautiainen H, Lehto MUK, Hamalainen MMJ. Charnley low friction arthroplasty in rheumatoid arthritis. A survival study up to 20 years. J Arthroplasty. 1999;14(6):657–661. doi: 10.1016/S0883-5403(99)90218-8. [DOI] [PubMed] [Google Scholar]
- 24.Leyland AH, Groenewegen PP. Multilevel modeling and public health policy. Scand J Public Health. 2003;31(4):267–274. doi: 10.1080/14034940210165028. [DOI] [PubMed] [Google Scholar]
- 25.Li LC, Badley EM, MacKay C, Mosher D, Jamal SW, Jones A, et al. An evidence-informed, integrated framework for rheumatoid arthritis care. Arthritis Rheum. 2008;59(8):1171–1183. doi: 10.1002/art.23931. [DOI] [PubMed] [Google Scholar]
- 26.Lindahl H, Malchau H, Herberts P, Garellick G. Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty. 2005;20(7):857–865. doi: 10.1016/j.arth.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 27.Lindahl H, Malchau H, Odén A, Garellick G. Risk factors for failure after treatment of a periprosthetic fracture of the femur. J Bone Joint Surg Br. 2006;88(1):26–30. doi: 10.1302/0301-620X.88B1.17029. [DOI] [PubMed] [Google Scholar]
- 28.Louie GH, Ward MM. Changes in the rates of joint surgery among patients with rheumatoid arthritis in California, 1983-2007. Ann Rheum Dis. 2010;69(5):868–871. doi: 10.1136/ard.2009.112474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Luqmani R, Hennell S, Estrach C, Birrell F, Bosworth A, Davenport G, et al. British society for rheumatology and British health professionals in rheumatology guideline for the management of rheumatoid arthritis (the first two years) Rheumatology. 2006;45:1167–1169. doi: 10.1093/rheumatology/kel215a. [DOI] [PubMed] [Google Scholar]
- 30.Majithia V, Geraci SA. Rheumatoid arthritis: diagnosis and management. Am J Med. 2007;120:936–939. doi: 10.1016/j.amjmed.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 31.Marker DR, Seyler TM, Jinnah RH, Delanois RE, Ulrich SD, Mont MA. Femoral neck fractures after metal-on-metal total hip resurfacing: a prospective cohort study. J Arthroplasty. 2007;22(7 Suppl 3):66–71. doi: 10.1016/j.arth.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 32.McBryde CW, Shears E, O'Hara JN, Pynsent PB. Metal-on-metal hip resurfacing in developmental dysplasia: a case-control study. J Bone Joint Surg Br. 2008;90(6):708–714. doi: 10.1302/0301-620X.90B6.20026. [DOI] [PubMed] [Google Scholar]
- 33.McMinn D, Daniel J. History and modern concepts in surface replacement. Proc Inst Mech Eng H. 2006;220(2):239–251. doi: 10.1243/095441105X68944. [DOI] [PubMed] [Google Scholar]
- 34.Mikuls TR. Co-morbidity in rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2003;17(5):729–752. doi: 10.1016/S1521-6942(03)00041-X. [DOI] [PubMed] [Google Scholar]
- 35.Mont MA, Ragland PS, Etienne G, Seyler TM, Schmalzried TP. Hip resurfacing arthroplasty. J Am Acad Orthop Surg. 2006;14:454–463. doi: 10.5435/00124635-200608000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Mont MA, Seyler TM, Marker DR, Marulanda GA, Delanois RE. Use of metal-on-metal total hip resurfacing for the treatment of osteonecrosis of the femoral head. J Bone Joint Surg Am. 2006;88(Suppl 3):90. doi: 10.2106/JBJS.F.00543. [DOI] [PubMed] [Google Scholar]
- 37.Nguyen-Oghalai TU, Ottenbacher KJ, Caban M, Granger CV, Grecula M, Goodwin JS. The impact of rheumatoid arthritis on rehabilitation outcomes after lower extremity arthroplasty. J Clin Rheumatol. 2007;13(5):247–250. doi: 10.1097/RHU.0b013e3181570ad4. [DOI] [PubMed] [Google Scholar]
- 38.Nilsson LT, Frazen H, Carlsson AS, Onnerfalt R. Early radiographic loosening impairs the function of a total hip replacement. The Nottingham health profile of 49 patients at five years. J Bone Joint Surg Br. 1994;76:235–239. [PubMed] [Google Scholar]
- 39.O'Connell AA, McCoach DB. Applications of hierarchical linear models for evaluations of health interventions: demystifying the methods and interpretations of multilevel models. Eval Health Prof. 2004;27(2):119–151. doi: 10.1177/0163278704264049. [DOI] [PubMed] [Google Scholar]
- 40.Ollivere B, Duckett S, August A, Porteous M (2009) The Birmingham hip resurfacing: 5-year clinical and radiographic results from a District General Hospital. Int Orthop Jun 9. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 41.Revell MP, McBryde CW, Bhatnagar S, Pynsent PB, Treacy RB. Metal-on-metal hip resurfacing in osteonecrosis of the femoral head. J Bone Joint Surg Am. 2006;88(Suppl 3):98–103. doi: 10.2106/JBJS.F.01070. [DOI] [PubMed] [Google Scholar]
- 42.Sarvilinna R, Huhtala HS, Sovelius RT, Halonen PJ, Nevalainen JK, Pajamäki KJ. Factors predisposing to periprosthetic fracture after hip arthroplasty: a case-control study. Acta Orthop Scand. 2004;75:16–20. doi: 10.1080/00016470410001708030. [DOI] [PubMed] [Google Scholar]
- 43.Severt R, Wood R, Cracchiolo A, Amstutz HC. Long-term follow-up of cemented total hip arthroplasty in rheumatoid arthritis. Clin Orthop Relat Res. 1991;265:137–145. [PubMed] [Google Scholar]
- 44.Shetty VD, Villar RN. Development and problems of metal-on-metal hip arthroplasty. Proc Inst Mech Eng H. 2006;220(2):371–377. doi: 10.1243/095441105X63264. [DOI] [PubMed] [Google Scholar]
- 45.Shimmin A, Back D. Femoral neck fractures following Birmingham hip resurfacing: a national review of 50 cases. J Bone Joint Surg Br. 2005;87:463–464. doi: 10.1302/0301-620X.87B4.15498. [DOI] [PubMed] [Google Scholar]
- 46.Shimmin A, Beaulé PE, Campbell P. Metal-on-metal hip resurfacing arthroplasty. J Bone Joint Surg Am. 2008;90(3):637–654. doi: 10.2106/JBJS.G.01012. [DOI] [PubMed] [Google Scholar]
- 47.Sinigaglia L, Varenna M, Girasole G, Bianchi G. Epidemiology of osteoporosis in rheumatic diseases. Rheum Dis Clin North Am. 2006;32(4):631–658. doi: 10.1016/j.rdc.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 48.Sochart DH, Porter ML. The long-term results of Charnley low-friction arthroplasty in young patients who have congenital dislocation, degenerative osteoarthrosis, or rheumatoid arthritis. J Bone Joint Surg Am. 1997;79(11):1599–1617. doi: 10.2106/00004623-199711000-00001. [DOI] [PubMed] [Google Scholar]
- 49.Star VL, Hochberg MC. Osteoporosis in patients with rheumatic diseases. Rheum Dis Clin North Am. 1994;20(3):561–576. [PubMed] [Google Scholar]
- 50.Tang WM, Chiu KY. Primary total hip arthroplasty in patients with rheumatoid arthritis. Int Orthop. 2001;25(1):13–16. doi: 10.1007/s002640000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tarasevicius S, Kesteris U, Robertsson O, Wingstrand H. Femoral head diameter affects the revision rate in total hip arthroplasty: an analysis of 1,720 hip replacements with 9–21 years of follow-up. Acta Orthop. 2006;77(5):706–709. doi: 10.1080/17453670610012872. [DOI] [PubMed] [Google Scholar]
- 52.Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty. A minimum follow-up of five years. J Bone Joint Surg Br. 2005;87(2):167–170. doi: 10.1302/0301-620X.87B2.15030. [DOI] [PubMed] [Google Scholar]
- 53.Wolfe F, Zwillich SH. The long-term outcomes of rheumatoid arthritis. A 23-year prospective, longitudinal study of total joint replacement and its predictors in 1,600 patients with rheumatoid arthritis. Arthritis Rheum. 1998;41(6):1072–1082. doi: 10.1002/1529-0131(199806)41:6<1072::AID-ART14>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 54.Woolson ST, Rahimtoola ZO. Risk factors for dislocation during the first three months after primary total hip replacement. J Arthroplasty. 1999;14:662–668. doi: 10.1016/S0883-5403(99)90219-X. [DOI] [PubMed] [Google Scholar]
- 55.Zwartelé RE, Brand R, Doets HC. Increased risk of dislocation after primary total hip arthroplasty in inflammatory arthritis: a prospective observational study of 410 hips. Acta Orthop Scand. 2004;75(6):684–690. doi: 10.1080/00016470410004049. [DOI] [PubMed] [Google Scholar]
- 56.Zwartele R, Peters A, Brouwers J, Olsthoorn P, Brand R, Doets C. Long-term results of cementless primary total hip arthroplasty with a threaded cup and a tapered, rectangular titanium stem in rheumatoid arthritis and osteoarthritis. Int Orthop. 2008;32(5):581–587. doi: 10.1007/s00264-007-0383-0. [DOI] [PMC free article] [PubMed] [Google Scholar]