Abstract
Objective
Monocyte recruitment and interaction with the endothelium is imperative to vascular recovery. Tie2 plays a key role in endothelial health and vascular remodeling. We studied monocyte-mediated Tie2/Angiopoietin signaling following interaction of primary monocytes with endothelial cells and its role in endothelial cell survival.
Methods and results
The direct interaction of primary monocytes with subconfluent endothelial cells resulted in transient secretion of Angiopoietin-1 from monocytes and the activation of endothelial Tie2. This effect was abolished by preactivation of monocytes with TNFα. While primary monocytes contained high levels of both Angiopoietin 1 and 2, endothelial cells contained primarily Angiopoietin 2.
Seeding of monocytes on serum starved endothelial cells reduced caspase-3 activity by 46% ± 5.1%, and 52% ± 5.8% after TNFα treatment, and decreased detected single strand DNA levels by 41% ± 4.2% and 40± 3.5% respectively. This protective effect of monocytes on endothelial cells was reversed by Tie2 silencing with specific siRNA. The anti-apoptotic effect of monocytes was further supported by the activation of cell survival signaling pathways involving PI3K, STAT3 and AKT.
Conclusions
Monocytes and endothelial cells form a unique Tie2/Angiopoietin-1 signaling system which effects endothelial cell survival and may play critical a role in vascular remodeling and homeostasis.
Introduction
Tie2, an endothelial cell (EC)-specific transmembrane receptor tyrosine kinase, is essential for vascular health. Tie2 mediates vascular remodeling and the survival and apoptosis of EC from a wide range of vascular beds 1–6, and in the face of varying stimuli including exposure to TNFα, serum deprivation, oxidized low-density lipoproteins, hyperosmolarity and irradiation 2, 3, 5–9. The remodeling endothelium controls a diverse set of activities that includes control of hemostasis and thrombosis, leukocyte adhesion, transmigration and proliferation and vascular smooth muscle cell biology 10–18. Circulating monocytes are among the first to respond to endothelial activation - localizing, binding and passing through damaged endothelium. Recruited monocytes play a unique role in vascular remodeling and actively participate in the initiation and progression of angiogenesis 11, 13–17.
Previously we demonstrated that monocyte binding to injured or subconfluent EC can actively promote endothelial proliferation by activating endothelial Met through a contact-dependent mechanism 19. We now report on the importance of early monocyte-mediated secretion of Angiopoietin 1 (Ang-1) and endothelial Tie2 phosphorylation in promoting survival of subconfluent EC under low nutrient and cytokine stress conditions. These findings shed new light on the active role of monocytes in the regulation of endothelial function and may well enhance therapeutic modulation of vascular repair and angiogenesis in a range of critical diseases.
Methods
Cells
Primary human umbilical vein endothelial cells (HUVEC) were purchased from Cambrex (Walkersville, MD). Primary monocytes were separated prior to each assay from blood drawn from healthy male subjects under formal protocols sanctioned by the MIT Committee on Use of Humans in Experimental Sciences, and separated employing a negative isolation method (Miltenyi Biotec, Auburn, CA). Monocyte were unactivated following negative selection as was previously demonstrated by following mRNA levels of TNFα and IL1-β in freshly isolated monocytes.20 Monocyte separation yield was over 90% and validated employing FACS analysis with anti CD14-RPE antibodies (DakoCytomation, Carpinteria, CA). Monocyte viability following negative selection was over >98% as measured by trypan blue staining.
For starvation induced EC apoptosis, HUVEC were grown to subconfluence (5×104 cells/cm2) in 3.5 cm tissue culture plates, followed by serum starvation (DMEM, 2% heat inactivated FBS, 24 hr). Following the initial 24 hr starvation period, cultures were exposed to a second starvation period in DMEM, 0.5% heat inactivated FBS for 24 hr. When monocytes were seeded in transwell inserts residing above EC cultures the volume of medium was increased to allow full submerging of the monocytes. For analysis of monocytes and EC following coculture assays, monocytes were separated from EC by repeated washes (PBS, EDTA, 2min) as previously described 19, 21 and the purity of separated monocytes and EC was verified by FACS analysis as previously described 19. Measured Tie2 and other target molecules were designated as primarily of endothelial origin as only trace numbers of monocytes were observed by CD14 FACS analysis following the separation of monocytes from EC-monocyte cocultures.
Tie2 siRNA silencing and EC survival
The role of endothelial Tie2 in monocyte-induced EC survival was studied though down regulation of Tie2 expression by siRNA silencing. EC were seeded in 6 cm plates (2×105 cells/plate) in DMEM 10% inactivated FBS without antibiotics. Prior to transfection cells were washed with transfection medium (Santa Cruz Bio-. technology, Santa Cruz, CA) and transfected with 60 pmol Tie2 siRNA or control siRNA in transfection reagent (Santa Cruz Bio-. technology, Santa Cruz, CA) following the manufacturer protocol. Assays employing monocyte interaction were performed 48 hr following transfection. Cleaved Caspase-3 activity was measured in HUVEC using a Caspase-Glo assay kit (Promega, WI), and ssDNA with an apoptosis ELISA kit (Millipore, Bedford, MA).
Western blot and ELISA
10 min prior to cell harvesting cultures were treated with 0.5mM sodium orthovanadate to preserve phosphorylation. Whole cell extracts of EC and monocytes were separated on glycin-SDS gels, transferred to PVDF membranes and immunobloted with the indicated antibodies. Ang-1 and 2 were measured in conditioned medium and cell lysates from HUVEC and monocytes alone or from cocultures using specific ELISA assays (R&D Systems, Minneapolis, MN). p-Tie2,Tie2, p-AKT, p-ERK, p-PI3K, p-STAT3, β-actin antibodies were purchased from Cell Signaling Technology (Beverly, MA).
Data analysis
All assays were performed in minimum of duplicates and repeated at least three times (n = number of replicates). Data are presented as mean ± SD or ± 20% for log graphs. When applicable, values were compared by Student’s T-test or ANOVA. P<0.05 was considered to be statistically significant.
Results
Monocyte contact activates endothelial Tie2
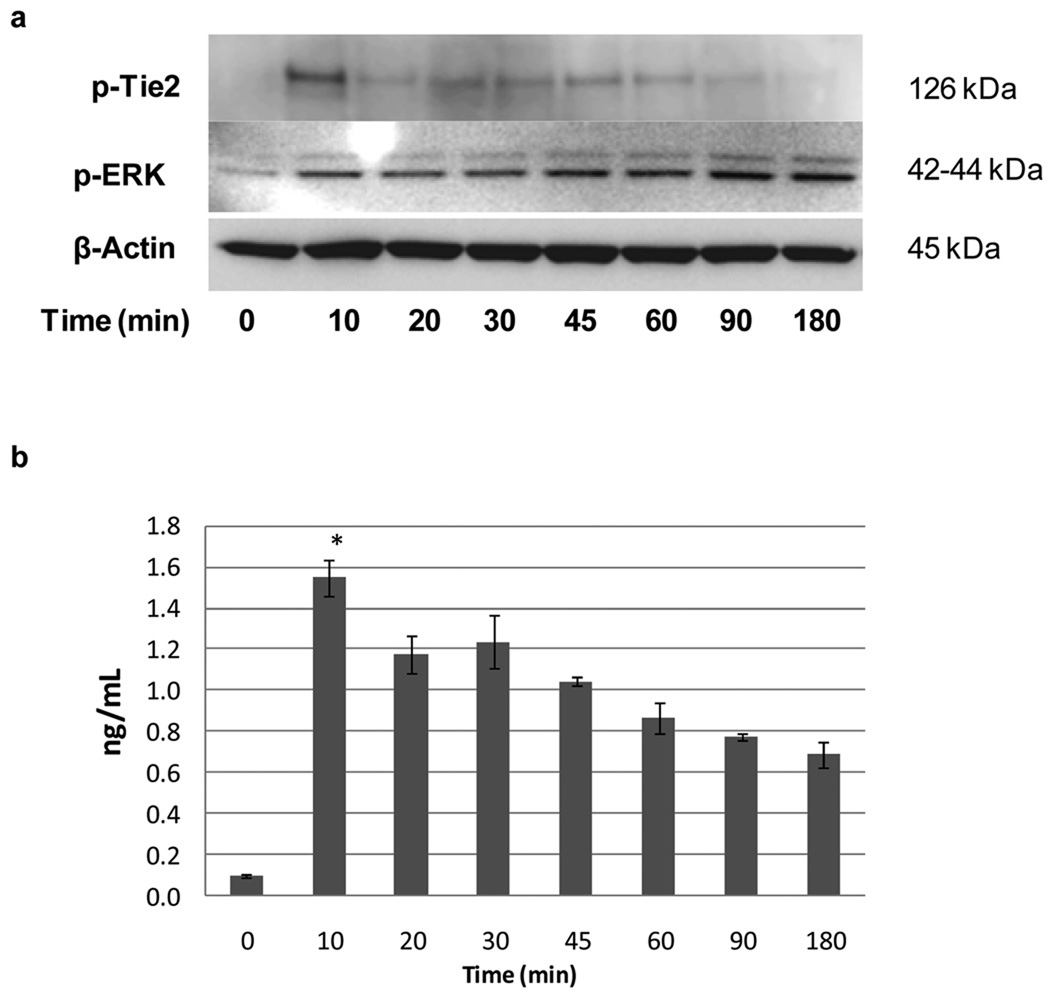
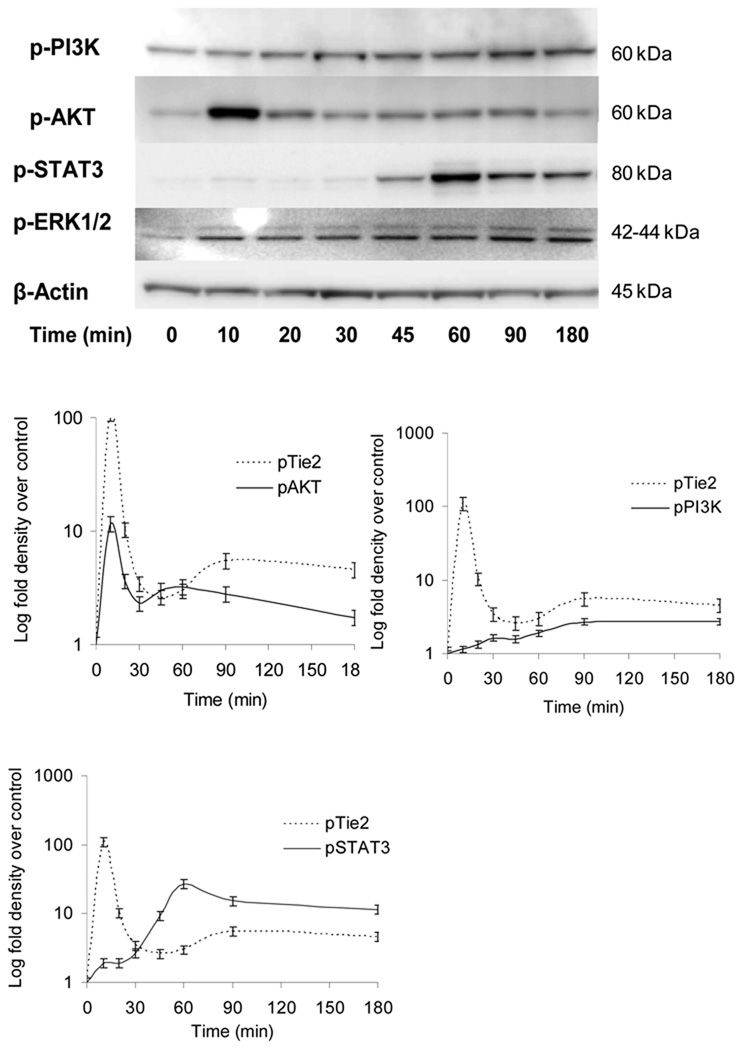
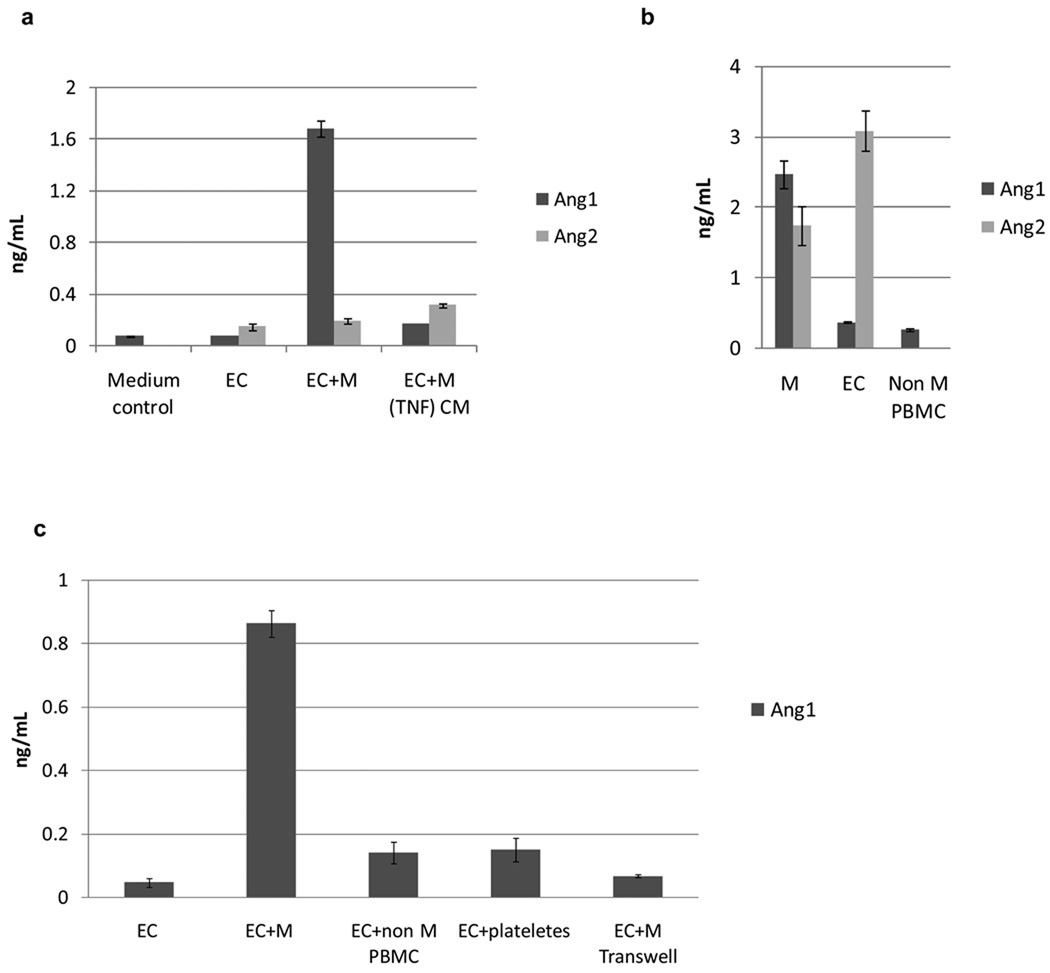
Direct contact of primary monocytes with HUVEC resulted in transient secretion of Ang-1 and activation of endothelial Tie2 as early as 10 min following monocyte addition (Fig 1 a,b). EC Tie2 phosphorylation and Ang-1 levels fell in the following 20 min and increased again between 45 and 180 min. Measurement of Ang-1 and Ang-2 in conditioned medium taken from subconfluent EC alone and 10 min following the addition of primary unactivated monocytes showed over 21 fold increase in Ang-1 in the later (Fig 2 a). Preactivation of monocytes with TNFα for 30 min prior to their addition to subconfluent EC abolished the secretion of Ang-1 and resulted in over 60% increase in the levels of Ang-2.
Figure 1. Monocytes secretion of Ang-1 and activation endothelial Tie2.
(a) Western blot of endothelial tie2 and ERK showing the kinetics of endothelial Tie2 and ERK phosphorylation following interaction with primary unactivated monocytes.
(b) Ang-1 levels measured in culture medium of EC-monocyte coculture over 180 min showing the kinetics of Ang-1 secretion. (n=3, *p<0.01).
Figure 2. Monocytes differentially secrete Ang-1 following interaction with EC.
(a) Levels of Ang-1 and 2 measured in conditioned medium (CM) from EC, EC-M coculture and EC cocultured with monocytes (M) preactivated with TNFα. (b) Levels of Ang-1 and 2 measured in cell lysate from EC, monocytes (M) and non monocytes PBMC. (c) Levels of Ang-1 measured in conditioned medium following 10 min of medium conditioning of subconfluent EC, EC+M, EC + non monocytes PBMC, EC + platelet enriched fraction and EC + monocytes in transwell. (n=3, *p<0.05).
Cell lysates taken from subconfluent HUVEC contained over 8-fold more Ang-2 than Ang-1. In contrast, primary unactivated monocytes contained Ang-1 and high levels of Ang-2 (Fig 2 b), suggesting that the early appearance of Ang-1, 10 min following the addition of primary unactivated monocytes to subconfluent EC, is primarily of monocyte origin. Analysis of Ang-1 content in non-monocyte peripheral blood mononuclear cells (PBMC) revealed that the high content of Ang-1 is unique to monocytes (Fig 2 b).
The specific effect of monocytes was further supported by comparing the levels of Ang-1 in the medium following the addition of primary monocytes to subconfluent EC to that obtained following the addition of platelet enriched fraction and similar numbers of PBMC (Fig 2 c). The role of contact in the release of Ang-1 from monocytes was confirmed when the monocytes added to subconfluent EC were separated by a transwell system. In this case detectable culture media Ang-1 levels dropped by more than 80% (Fig 2 c). The transwell system required use of higher volume of medium compared with those used in figure 2 a, resulting in higher medium/cell ratio and lower Ang-1 concentration (Fig 2c).
Previously we reported the unique kinetics of endothelial ERK1/2 activation following direct interaction with monocytes 19. The activation of endothelial Tie2 correlated closely with the activation of endothelial ERK1/2 demonstrating similar activation kinetics at the early (10 min) and late (45 min) interaction.
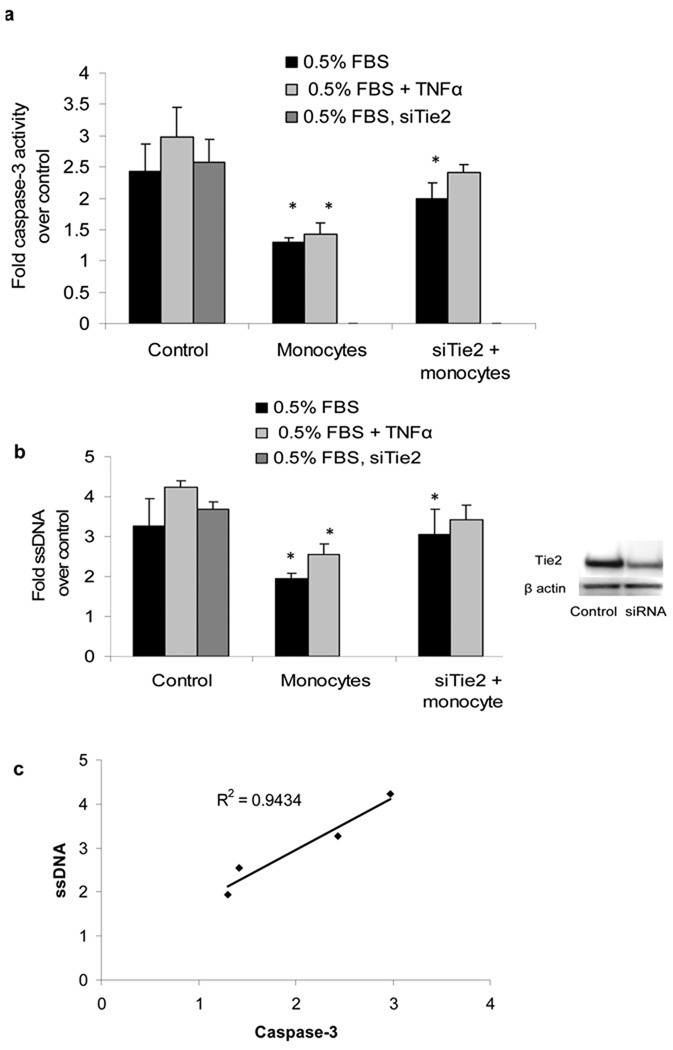
Silencing of EC Tie2 reverses monocyte-induced EC survival
Noble et al 15 reported that primary monocytes induce an anti-apoptotic effect in EC through a contact-dependent activation of EC bcl-2 homologue A1 expression. Tie2 is a well characterized mediator of EC cell survival 2, 3, 5. The transient activation of endothelial Tie2 by monocytes led us to investigate the effect of monocyte-mediated activation of EC Tie2 on EC survival. Untreated and siTie2 silenced HUVEC were starved (24 h, DMEM, 2% heat inactivated FBS) in a 96-well plate followed by a second starvation period in DMEM 0.5% FBS. Prior to the second starvation period, cultures were left untreated or treated with TNFα (2 ng/mL, 60 min) followed by 3 washes in starvation medium to remove remaining TNFα. Monocytes were added in proportional numbers and 23 hr later a luminescent substrate was applied to the cells (1 hr at 37°C), and the production of a luminescent signal was detected by a Fluoroskan. Prolonged starvation resulted in 2.4 fold increase in detected caspase-3 activity compared with unstarved cells. The addition of monocyte resulted in a reduction in apoptosis under starvation and TNFα exposure. Caspase-3 activity fell by 46%± 5.1% and identical 52%± 5.8% after TNFα exposure. Silencing of endothelial Tie2 reduced the protective effect of monocytes on apoptosis by 28% and 34% respectively (fig 3 a).
Figure 3. Monocytes reduce starvation and cytokine-induced caspase-3 activity and DNA degradation.
(a) Caspase-3 activity in untreated and siTie2 treated EC following starvation and TNFα treatment with and without monocytes. (b) Single stranded DNA measured in untreated and siTie2 treated ECs following TNFα treatment with and without monocytes. (c) Correlation graph of measured caspase-3 versus measured ssDNA. (n=3, R2=0.9434, *p<0.05)
The anti-apoptotic effect of monocytes was further confirmed by the detection of single stranded DNA (ssDNA) in starved EC using a formamide ssDNA ELISA assay 22. EC were seeded in 96 wells plate and grown to a density of 1×104 cells/well. Cultures were treated as described for the cleaved caspase-3 assay and apoptosis was analyzed employing ssDNA apoptosis ELISA kit (Millipore, Bedford, MA). Prolonged starvation alone, or in the presence of TNFα, resulted in 3.2± 0.7 and 4.2± 0.2 fold increase in detected ssDNA compared with unstarved cells. Treatment with monocytes reduced starvation and TNFα induced apoptosis identically by 41% ± 4.2% and 40± 3.5% respectively. Silencing endothelial Tie2 reversed the antiapoptotic effect of monocytes making it statistically insignificant in serum starved EC and 20% lower in TNFα treated EC (Fig 3 b).
Monocyte binding activates PI3k, AKT and STAT3 survival mediated signaling
To characterize further the effect of monocytes on EC survival we followed the changes in phosphorylation levels of other key cell survival mediators: PI3K, p-AKT and p-STAT3, following interaction with monocytes (Fig 4). PI3K and AKT are activated in EC downstream of Tie2 3, 4 and play a pivotal role in EC survival 23–26. STAT3 is activated downstream of ERK and was suggested to support cell survival in different cell types 27–29. HUVEC were exposed to starvation-induced apoptosis as described above. Following the second starvation period, unactivated primary monocytes were seeded over EC in proportional numbers and removed from cocultures in the indicated time points (Fig 4).
Figure 4. Monocyte interaction with EC activates survival signaling mediated by PI3K, AKT and STAT3.
Unactivated monocytes introduced to subconfluent, serum-starved HUVEC in direct contact induce the activation of survival related signaling molecules PI3K, AKT and STAT3 measured by western blot analysis.
Monocytes induced a gradual increase in pI3K phosphorylation of up to 3 fold over untreated EC. AKT phosphorylation increased 12 fold, 10 min following direct contact with monocytes and gradually declined to 3 fold phosphorylation over control. STAT3 phosphorylation was apparent beginning with the second activation of ERK at 45min resulting in up to 27 fold increase in STAT3 phosphorylation 60 min following addition of monocytes.
Discussion
Julius Connheim identified the central role of monocytes in inflammation and vascular biology in the 1880s 30. Since then we have come to appreciate the complexity and sophistication of monocyte-EC biology in mediating vascular health 15, 31, 32. Activated monocytes induce a myriad of effects on vascular permeability, recruitment of leukocytes, elaboration of cytokines and other mediators, and progression to vascular inflammation, injury and hyperplasia 33. More recently we demonstrated a counter-balancing effect where unactivated monocytes restore endothelial health via a direct-contact mechanism, mediated in part by Met. We now report that upon direct physical interaction with EC primary unactivated monocytes secret high levels of Ang-1 leading to a transient activation of endothelial Tie2, and that this activation contributes to the regulation of EC survival.
Monocyte secreted Ang-1 activates EC Tie2
The presence of Ang-1 in the regulatory scheme of Tie-2 can help explain the dynamic regulation of monocyte-EC interactions. As an EC-specific transmembrane receptor tyrosine kinase Tie-2 is a prime factor for modulation of vascular biology. Indeed its effects are ubiquitous throughout the vascular system 1–6, and for a range of pathologic stresses 2, 3, 5–9. We now report that the kinetics of its regulation may make it even more potent a modulator of vascular events. Monocytes induce rapid activation of endothelial Tie2 followed by a secondary more sustained activation, and phosphorylation following a complex, rapidly responsive dynamic that is mediated by Ang-1.
Ang-1/2 together with Ang-3/4 belongs to a family of oligomeric-secreted glycoproteins which have been identified as a group of ligands of the tyrosine kinase Tie2 receptor. The angiopoietin and Tie families play a critical role in vascular remodeling and blood vessel stabilization. Ang-1 was previously shown to play a key role in organization and maturation of newly formed vessels 34, 35 and in the promotion of quiescence and survival in adult vasculature.3, 7, 36 Ang-2 acts as a competitive antagonist to Ang-1 effects with blockage of Tie2 phosphorylation and activation.37 The addition of primary monocytes to EC resulted in transient secretion of Ang-1 and activation of EC Tie2. The kinetics of Tie2 phosphorylation showed rapid decline in phosphrylated Tie2 which did not correlate with the moderate decline in Ang-1 levels.
Bogdanovic et al previously demonstrated that the addition of Ang-1 (800 ng/ml) induces 40% degradation of EC Tie2 in HUVEC culture after 15 min. 38 This regulation of Tie2 by Ang-1 may account for the reduction in measured pTie2 following the addition of monocytes and for the relatively low levels of pTie2 compared with soluble Ang-1 following the first 10 min of coculture.
Ang-1 and Ang-2 are differentially regulated during EC-monocyte interaction
Both Ang-1 and Ang-2 are found in high concentration in primary unactivated monocytes. Yet, Ang-1 is regulated differently by monocytes and EC, and differently than Ang-2 in monocytes. While Ang-1 was rapidly secreted into the medium, Ang-2, which could play an inhibiting role in Tie2 signaling during the interaction of the two cell types, remained in low concentrations. There is therefore differential regulation by monocytes of Ang-1 and Ang-2 as well as endothelial Ang-2 following direct interaction of the two cell types.
The selective secretion of Ang-1 and Ang-2 may be regulated by monocyte activation state as preactivation of monocytes with TNFα for 30 min prior to their addition to subconfluent EC abolished the secretion of Ang-1 and increased the secretion of Ang-2. The role of monocyte activation in the secretion of Ang-1 is supported further by the secretion of Ang-1 following the direct seeding of monocytes over tissue culture plates (data not shown).
Monocyte Ang-1 induces EC survival through EC Tie2
In the present work we used siRNA silencing of EC Tie2 to demonstrate the role of Ang-1/Tie2 signaling in monocyte-mediated EC survival. Monocyte contact with EC reduced cleaved caspase-3 levels as well as single stranded DNA following stress induced by serum starvation and exposure to TNFα. In a previous study in which soluble Tie2 receptor served as a neutralizing competitive antagonist 3 the protective effect of Ang-1 on EC was reversed, further supporting the role of monocytes/Ang-1 in the regulation of EC survival.
Monocyte interaction with the endothelium in areas of inflammation and ischemia indicate a putative role for EC-monocyte interaction in the regulation of EC survival.14 Direct interaction of monocytes with EC protects the latter from serum depravation-induced apoptosis by up regulation of bcl-2 homologue A1 in EC 15. Neutralization of TNFα and PECAM1 can reduce A1 expression in EC, but does not eliminate the protective effect of monocytes and cannot explain the contact dependency of this effect 15. A different mechanism for the protective effect of Ang-1 was proposed by Dallabrida et al suggesting that promotion of cardiac and skeletal myocyte survival by Ang-1 is mediated by integrins rather than Tie2 and results in activation of AKT and ERK42/44. 39 In our experiments inhibition of Tie2 by siRNA silencing only partially reversed the anti-apoptotic effect of monocytes indicating that other signaling cascades are acting to protect EC from apoptosis. Monocyte-derived VEGF promotes endothelial cell survival through the phosphatidylinositol 3'-kinase/Akt signal transduction pathway.25 Recently our group reported on the early secretion of hepatocyte growth factor by primary unactivated monocytes upon contact with EC which may also contribute to the protective effect of monocytes.19, 40
The In vivo effect of Ang-1 on EC survival was well demonstrated by Chung-Hyun Cho et al who used a stable Ang-1 variant to promote EC survival in irradiated mouse model.41 Little is known about the interaction of circulating monocytes with the endothelium prior to their binding and transmigration. The kinetics of Tie2 activation and its dependency on monocytes interaction should correlate with the time during which the two cell types come in contact in vivo. Although diapedesis takes place rapidly recent in vivo observations identified a new mode of monocyte interaction with the endothelium defined as “patrolling”. This interaction was demonstrated in mouse Ly6Clo monocytes (analogous to CD16+ human monocytes) and was much slower than cell motility observed during diapedesis.18 The specific role of human monocytes subsets in the regulation of EC Tie2 is the subject of future work that will require new negative separation tools to produce inactivated monocyte subset.
Monocyte interaction with EC differentially activates survival related signaling
There appears to be two phases of survival related signaling during monocytes/EC interaction - an early phase which correlates with strong Tie2 and AKT phosphorylation and a less intense late phase that corresponds to STAT3 and PI3K activation. The different activation kinetics of AKT and PI3K suggests that the initial activation of AKT may be independent of PI3K. STAT-3-ERK interactions depend upon a range of signals and can induce an anti-apoptotic effect by transcriptional regulation of Bcl-2, Mcl-1 and c-IAP2. 42, 43 The expression Bcl-2 by monocyte mediated STAT-3 activation may be part of the mechanism deriving monocyte-induced cell survival previously described by Noble et al.15
The present study offers new insight into the complex regulation of EC survival by monocytes. The secretion of Ang-1 by monocytes upon contact with EC followed by the activation of endothelial Tie2, and the role this cell-cell interaction plays in endothelial survival, sheds new light on the role of circulating monocytes in vascular homeostasis. The new form of monocyte-EC communication using Ang-1/Tie2 signaling may have additional significance in vascular remodeling and will be the subject of future studies.
Acknowledgments
This work was supported by grants from the National Institutes of Health to ERE (GM 49039, and HL67246), and the National Institute on Aging (T32-AG023480).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Jones N, Master Z, Jones J, Bouchard D, Gunji Y, Sasaki H, Daly R, Alitalo K, Dumont DJ. Identification of tek/tie2 binding partners. Binding to a multifunctional docking site mediates cell survival and migration. J Biol Chem. 1999;274:30896–30905. doi: 10.1074/jbc.274.43.30896. [DOI] [PubMed] [Google Scholar]
- 2.Papapetropoulos A, Garcia-Cardena G, Dengler TJ, Maisonpierre PC, Yancopoulos GD, Sessa WC. Direct actions of angiopoietin-1 on human endothelium: Evidence for network stabilization, cell survival, and interaction with other angiogenic growth factors. Lab Invest. 1999;79:213–223. [PubMed] [Google Scholar]
- 3.Kim I, Kim HG, So JN, Kim JH, Kwak HJ, Koh GY. Angiopoietin-1 regulates endothelial cell survival through the phosphatidylinositol 3'-kinase/akt signal transduction pathway. Circ Res. 2000;86:24–29. doi: 10.1161/01.res.86.1.24. [DOI] [PubMed] [Google Scholar]
- 4.Kim I, Kim JH, Moon SO, Kwak HJ, Kim NG, Koh GY. Angiopoietin-2 at high concentration can enhance endothelial cell survival through the phosphatidylinositol 3'-kinase/akt signal transduction pathway. Oncogene. 2000;19:4549–4552. doi: 10.1038/sj.onc.1203800. [DOI] [PubMed] [Google Scholar]
- 5.Kwak HJ, Lee SJ, Lee YH, Ryu CH, Koh KN, Choi HY, Koh GY. Angiopoietin-1 inhibits irradiation- and mannitol-induced apoptosis in endothelial cells. Circulation. 2000;101:2317–2324. doi: 10.1161/01.cir.101.19.2317. [DOI] [PubMed] [Google Scholar]
- 6.Kim I, Moon SO, Han CY, Pak YK, Moon SK, Kim JJ, Koh GY. The angiopoietin-tie2 system in coronary artery endothelium prevents oxidized low-density lipoprotein-induced apoptosis. Cardiovasc Res. 2001;49:872–881. doi: 10.1016/s0008-6363(00)00295-9. [DOI] [PubMed] [Google Scholar]
- 7.Kwak HJ, So JN, Lee SJ, Kim I, Koh GY. Angiopoietin-1 is an apoptosis survival factor for endothelial cells. FEBS Lett. 1999;448:249–253. doi: 10.1016/s0014-5793(99)00378-6. [DOI] [PubMed] [Google Scholar]
- 8.Chen JX, Chen Y, DeBusk L, Lin W, Lin PC. Dual functional roles of tie-2/angiopoietin in tnf-alpha-mediated angiogenesis. Am J Physiol Heart Circ Physiol. 2004;287:H187–H195. doi: 10.1152/ajpheart.01058.2003. [DOI] [PubMed] [Google Scholar]
- 9.Papapetropoulos A, Fulton D, Mahboubi K, Kalb RG, O'Connor DS, Li F, Altieri DC, Sessa WC. Angiopoietin-1 inhibits endothelial cell apoptosis via the akt/survivin pathway. J Biol Chem. 2000;275:9102–9105. doi: 10.1074/jbc.275.13.9102. [DOI] [PubMed] [Google Scholar]
- 10.Niiyama H, Kai H, Yamamoto T, Shimada T, Sasaki K, Murohara T, Egashira K, Imaizumi T. Roles of endogenous monocyte chemoattractant protein-1 in ischemia-induced neovascularization. J Am Coll Cardiol. 2004;44:661–666. doi: 10.1016/j.jacc.2004.04.046. [DOI] [PubMed] [Google Scholar]
- 11.Kumar AG, Ballantyne CM, Michael LH, Kukielka GL, Youker KA, Lindsey ML, Hawkins HK, Birdsall HH, MacKay CR, LaRosa GJ, Rossen RD, Smith CW, Entman ML. Induction of monocyte chemoattractant protein-1 in the small veins of the ischemic and reperfused canine myocardium. Circulation. 1997;95:693–700. doi: 10.1161/01.cir.95.3.693. [DOI] [PubMed] [Google Scholar]
- 12.Kim JS, Gautam SC, Chopp M, Zaloga C, Jones ML, Ward PA, Welch KM. Expression of monocyte chemoattractant protein-1 and macrophage inflammatory protein-1 after focal cerebral ischemia in the rat. J Neuroimmunol. 1995;56:127–134. doi: 10.1016/0165-5728(94)00138-e. [DOI] [PubMed] [Google Scholar]
- 13.Moldovan NI, Goldschmidt-Clermont PJ, Parker-Thornburg J, Shapiro SD, Kolattukudy PE. Contribution of monocytes/macrophages to compensatory neovascularization: The drilling of metalloelastase-positive tunnels in ischemic myocardium. Circ Res. 2000;87:378–384. doi: 10.1161/01.res.87.5.378. [DOI] [PubMed] [Google Scholar]
- 14.Ren G, Dewald O, Frangogiannis NG. Inflammatory mechanisms in myocardial infarction. Curr Drug Targets Inflamm Allergy. 2003;2:242–256. doi: 10.2174/1568010033484098. [DOI] [PubMed] [Google Scholar]
- 15.Noble KE, Wickremasinghe RG, DeCornet C, Panayiotidis P, Yong KL. Monocytes stimulate expression of the bcl-2 family member, a1, in endothelial cells and confer protection against apoptosis. J Immunol. 1999;162:1376–1383. [PubMed] [Google Scholar]
- 16.Voskuil M, van Royen N, Hoefer IE, Seidler R, Guth BD, Bode C, Schaper W, Piek JJ, Buschmann IR. Modulation of collateral artery growth in a porcine hindlimb ligation model using mcp-1. Am J Physiol Heart Circ Physiol. 2003;284:H1422–H1428. doi: 10.1152/ajpheart.00506.2002. [DOI] [PubMed] [Google Scholar]
- 17.Ito WD, Arras M, Winkler B, Scholz D, Schaper J, Schaper W. Monocyte chemotactic protein-1 increases collateral and peripheral conductance after femoral artery occlusion. Circ Res. 1997;80:829–837. doi: 10.1161/01.res.80.6.829. [DOI] [PubMed] [Google Scholar]
- 18.Auffray C, Fogg D, Garfa M, Elain G, Join-Lambert O, Kayal S, Sarnacki S, Cumano A, Lauvau G, Geissmann F. Monitoring of blood vessels and tissues by a population of monocytes with patrolling behavior. Science. 2007;317:666–670. doi: 10.1126/science.1142883. [DOI] [PubMed] [Google Scholar]
- 19.Schubert SY, Benarroch A, Ostvang J, Edelman ER. Regulation of endothelial cell proliferation by primary monocytes. Arterioscler Thromb Vasc Biol. 2008;28:97–104. doi: 10.1161/ATVBAHA.107.157537. [DOI] [PubMed] [Google Scholar]
- 20.Schubert SY, Benarroch A, Monter-Solans J, Edelman ER. Monocyte activation state regulates monocyte-induced endothelial proliferation through met signaling. Blood. 2010;115:3407–3412. doi: 10.1182/blood-2009-02-207340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kataoka N, Iwaki K, Hashimoto K, Mochizuki S, Ogasawara Y, Sato M, Tsujioka K, Kajiya F. Measurements of endothelial cell-to-cell and cell-to-substrate gaps and micromechanical properties of endothelial cells during monocyte adhesion. Proc Natl Acad Sci U S A. 2002;99:15638–15643. doi: 10.1073/pnas.242590799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ito Y, Shibata MA, Kusakabe K, Otsuki Y. Method of specific detection of apoptosis using formamide-induced DNA denaturation assay. J Histochem Cytochem. 2006;54:683–692. doi: 10.1369/jhc.5A6799.2006. [DOI] [PubMed] [Google Scholar]
- 23.Nishimura K, Li W, Hoshino Y, Kadohama T, Asada H, Ohgi S, Sumpio BE. Role of akt in cyclic strain-induced endothelial cell proliferation and survival. Am J Physiol Cell Physiol. 2006;290:C812–C821. doi: 10.1152/ajpcell.00347.2005. [DOI] [PubMed] [Google Scholar]
- 24.Ahmad A, Ahmad S, Chang LY, Schaack J, White CW. Endothelial akt activation by hyperoxia: Role in cell survival. Free Radic Biol Med. 2006;40:1108–1118. doi: 10.1016/j.freeradbiomed.2005.10.045. [DOI] [PubMed] [Google Scholar]
- 25.Gerber HP, McMurtrey A, Kowalski J, Yan M, Keyt BA, Dixit V, Ferrara N. Vascular endothelial growth factor regulates endothelial cell survival through the phosphatidylinositol 3'-kinase/akt signal transduction pathway. Requirement for flk-1/kdr activation. J Biol Chem. 1998;273:30336–30343. doi: 10.1074/jbc.273.46.30336. [DOI] [PubMed] [Google Scholar]
- 26.Garcia-Cardena G, Anderson KR, Mauri L, Gimbrone MA., Jr Distinct mechanical stimuli differentially regulate the pi3k/akt survival pathway in endothelial cells. Ann N Y Acad Sci. 2000;902:294–297. doi: 10.1111/j.1749-6632.2000.tb06325.x. [DOI] [PubMed] [Google Scholar]
- 27.Kanda N, Seno H, Konda Y, Marusawa H, Kanai M, Nakajima T, Kawashima T, Nanakin A, Sawabu T, Uenoyama Y, Sekikawa A, Kawada M, Suzuki K, Kayahara T, Fukui H, Sawada M, Chiba T. Stat3 is constitutively activated and supports cell survival in association with survivin expression in gastric cancer cells. Oncogene. 2004;23:4921–4929. doi: 10.1038/sj.onc.1207606. [DOI] [PubMed] [Google Scholar]
- 28.Song L, Turkson J, Karras JG, Jove R, Haura EB. Activation of stat3 by receptor tyrosine kinases and cytokines regulates survival in human non-small cell carcinoma cells. Oncogene. 2003;22:4150–4165. doi: 10.1038/sj.onc.1206479. [DOI] [PubMed] [Google Scholar]
- 29.Alonzi T, Middleton G, Wyatt S, Buchman V, Betz UA, Muller W, Musiani P, Poli V, Davies AM. Role of stat3 and pi 3-kinase/akt in mediating the survival actions of cytokines on sensory neurons. Mol Cell Neurosci. 2001;18:270–282. doi: 10.1006/mcne.2001.1018. [DOI] [PubMed] [Google Scholar]
- 30.Cohnheim JF. Lectures on general pathology: A handbook for practitioners and students. London: The New Sydenham Society; 1889. p. 1. [Google Scholar]
- 31.Eubank TD, Galloway M, Montague CM, Waldman WJ, Marsh CB. M-csf induces vascular endothelial growth factor production and angiogenic activity from human monocytes. J Immunol. 2003;171:2637–2643. doi: 10.4049/jimmunol.171.5.2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fan W, Zheng JJ, McLaughlin BJ. An in vitro model of the back of the eye for studying retinal pigment epithelial-choroidal endothelial interactions. In Vitro Cell Dev Biol Anim. 2002;38:228–234. doi: 10.1290/1071-2690(2002)038<0228:AIVMOT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 33.Rogers C, Welt FG, Karnovsky MJ, Edelman ER. Monocyte recruitment and neointimal hyperplasia in rabbits. Coupled inhibitory effects of heparin. Arterioscler Thromb Vasc Biol. 1996;16:1312–1318. doi: 10.1161/01.atv.16.10.1312. [DOI] [PubMed] [Google Scholar]
- 34.Suri C, Jones PF, Patan S, Bartunkova S, Maisonpierre PC, Davis S, Sato TN, Yancopoulos GD. Requisite role of angiopoietin-1, a ligand for the tie2 receptor, during embryonic angiogenesis. Cell. 1996;87:1171–1180. doi: 10.1016/s0092-8674(00)81813-9. [DOI] [PubMed] [Google Scholar]
- 35.Suri C, McClain J, Thurston G, McDonald DM, Zhou H, Oldmixon EH, Sato TN, Yancopoulos GD. Increased vascularization in mice overexpressing angiopoietin-1. Science. 1998;282:468–471. doi: 10.1126/science.282.5388.468. [DOI] [PubMed] [Google Scholar]
- 36.Huang J, Bae JO, Tsai JP, Kadenhe-Chiweshe A, Papa J, Lee A, Zeng S, Kornfeld ZN, Ullner P, Zaghloul N, Ioffe E, Nandor S, Burova E, Holash J, Thurston G, Rudge J, Yancopoulos GD, Yamashiro DJ, Kandel JJ. Angiopoietin-1/tie-2 activation contributes to vascular survival and tumor growth during vegf blockade. Int J Oncol. 2009;34:79–87. [PMC free article] [PubMed] [Google Scholar]
- 37.Maisonpierre PC, Suri C, Jones PF, Bartunkova S, Wiegand SJ, Radziejewski C, Compton D, McClain J, Aldrich TH, Papadopoulos N, Daly TJ, Davis S, Sato TN, Yancopoulos GD. Angiopoietin-2, a natural antagonist for tie2 that disrupts in vivo angiogenesis. Science. 1997;277:55–60. doi: 10.1126/science.277.5322.55. [DOI] [PubMed] [Google Scholar]
- 38.Bogdanovic E, Nguyen VP, Dumont DJ. Activation of tie2 by angiopoietin-1 and angiopoietin-2 results in their release and receptor internalization. J Cell Sci. 2006;119:3551–3560. doi: 10.1242/jcs.03077. [DOI] [PubMed] [Google Scholar]
- 39.Dallabrida SM, Ismail N, Oberle JR, Himes BE, Rupnick MA. Angiopoietin-1 promotes cardiac and skeletal myocyte survival through integrins. Circ Res. 2005;96:e8–e24. doi: 10.1161/01.RES.0000158285.57191.60. [DOI] [PubMed] [Google Scholar]
- 40.Ma H, Calderon TM, Fallon JT, Berman JW. Hepatocyte growth factor is a survival factor for endothelial cells and is expressed in human atherosclerotic plaques. Atherosclerosis. 2002;164:79–87. doi: 10.1016/s0021-9150(02)00062-x. [DOI] [PubMed] [Google Scholar]
- 41.Cho CH, Kammerer RA, Lee HJ, Yasunaga K, Kim KT, Choi HH, Kim W, Kim SH, Park SK, Lee GM, Koh GY. Designed angiopoietin-1 variant, comp-ang1, protects against radiation-induced endothelial cell apoptosis. Proc Natl Acad Sci U S A. 2004;101:5553–5558. doi: 10.1073/pnas.0307575101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bhattacharya S, Ray RM, Johnson LR. Stat3-mediated transcription of bcl-2, mcl-1 and c-iap2 prevents apoptosis in polyamine-depleted cells. Biochem J. 2005;392:335–344. doi: 10.1042/BJ20050465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hirano T, Ishihara K, Hibi M. Roles of stat3 in mediating the cell growth, differentiation and survival signals relayed through the il-6 family of cytokine receptors. Oncogene. 2000;19:2548–2556. doi: 10.1038/sj.onc.1203551. [DOI] [PubMed] [Google Scholar]