Abstract
While factor analyses have characterized pace, rhythm and variability as factors that explain variance in gait performance in older adults, comprehensive analyses incorporating many gait parameters have not been undertaken and normative data for many of those parameters are lacking. The purposes of this study were to conduct a factor analysis on nearly two dozen spatiotemporal gait parameters and to contribute to the normative database of gait parameters from healthy, able-bodied men and women over the age of 70. Data were extracted from 294 participants enrolled in the Mayo Clinic Study of Aging. Spatiotemporal gait data were obtained as participants completed two walks across a 5.6-m electronic walkway (GAITRite®). Five primary domains of spatiotemporal gait performance were identified: a “rhythm” domain was characterized by cadence and temporal parameters such as stride time; a “phase” domain was characterized by temporophasic parameters that constitute distinct divisions of the gait cycle; a “variability” domain encompassed gait cycle and step variability parameters; a “pace” domain was characterized by parameters that included gait speed, step length and stride length; and a “base of support” domain was characterized by step width and step width variability. Several domains differed between men and women and differed across age groups. Reference values of 23 gait parameters are presented which researchers or clinicians can use for assessing and interpreting gait dysfunction in aging persons.
Keywords: Gait, Aging, Sex Characteristics, Reference Values
1. Introduction
Gait may be used to assess quality of life [1], health status [2], and physical function [3] in older adults. Specific parameters may be used to assess risk of dementia [4], risk of falling [5], and even risk of early mortality [6]. Understanding how gait is associated with these clinical phenomena is challenging, in part because dozens of gait parameters can be measured and consensus on which are most relevant is lacking. Moreover, normative data for many parameters are lacking and in studies that report reference values, there is a great deal of variability among the data reported [2,7–11].
Verghese et al, [4] while studying the relationship between gait and risk of dementia, identified three domains that characterize gait performance in older adults. Pace differences characterized by gait speed and stride length were associated with reduced executive function; rhythm differences characterized by cadence, swing time and stance time were associated with memory decline; and variability differences characterized by stride length variability distinguished subtypes of mild cognitive impairment. The variability domain may also best predict falls in older adults [5]. Those three domains of gait, however, constitute only a small proportion of gait parameters that can be quantified. Additional parameters may yield greater insight into how gait is associated with other clinical phenomena.
In addition to understanding which parameters characterize gait performance, classifying gait as being dysfunctional necessitates that a clinician understands what “normal” gait is. While normal gait is not readily defined, normative and population-based data provide insight about what one might expect the magnitude of certain gait parameters to be. Normative data represent descriptive or prescriptive measurements as they ought to be; hence normative studies examine parameters in healthy participants. In contrast, population-based data represent measures as they are in a population; hence population-based studies examine parameters in participants oftentimes regardless of health status. Gait speed is the most often reported reference value for gait performance. Reported values of mean gait speed in adults aged 70–79 range from approximately 90 to 130 cm/s [2,7–11]. Normative studies [2,9–11] typically report higher values than population-based studies [7,8], presumably because the normative studies describe gait in healthy individuals whereas population-based studies include participants who may have pathological conditions affecting their gait performance. While reference values for other spatiotemporal parameters have been reported, the magnitudes of those measurements, similar to gait speed, are quite variable. Normative data for many parameters—particularly those quantifying variability—are lacking.
The purpose of this study was twofold. First, we conducted a factor analysis on nearly two dozen gait parameters to examine the spatiotemporal domains of gait that researchers and clinicians may consider measuring to enhance their understanding of gait performance. Factor analysis organizes multiple observations into communalities that correlate with a lesser number of unobserved thematic constructs, thus allowing an investigator to partition a large number of parameters into a lesser number that characterize distinct domains of the parameters being measured. Second, we sought to contribute to the normative database of gait parameters in older, able-bodied adults. Establishing normative data may provide clinicians and researchers values against which measurements can be compared for assessing and interpreting gait dysfunction.
2. Methods
2.1 Participants
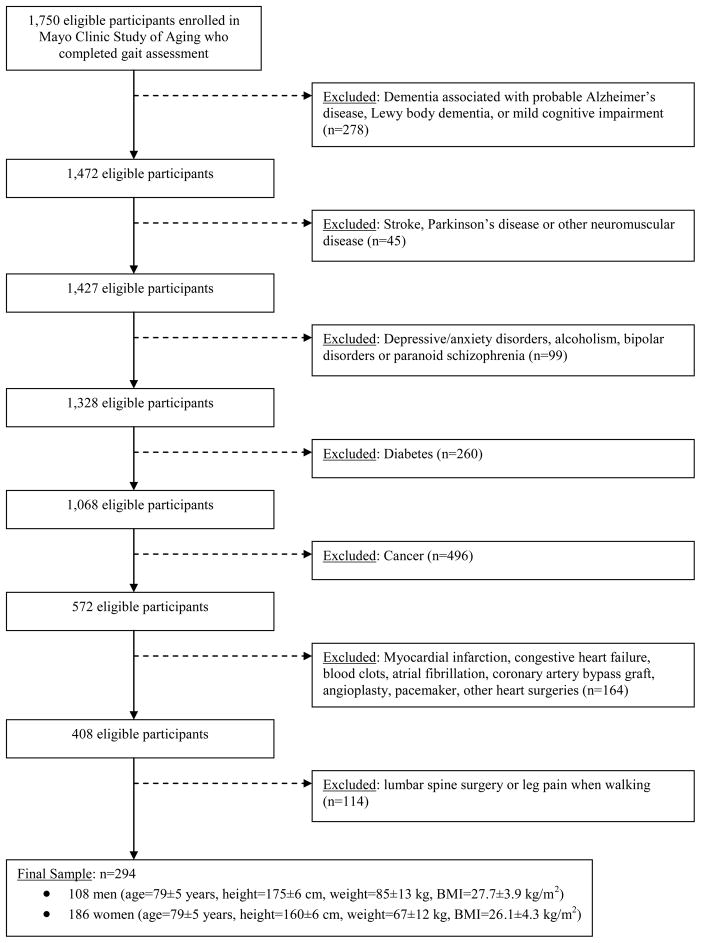
Data were extracted from 1,750 ambulatory participants aged 70+ who were enrolled in the Mayo Clinic Study of Aging, a population-based study of aging [12]. Participants were recruited via stratified sampling in which Olmsted County, Minnesota, residents from within four strata (men aged 70–79 and 80–89, and women aged 70–79 and 80–89) were randomly selected and invited to participate in the study. Most participants were Caucasian (93%), retired (94%), lived in their own dwelling (85%) and were married (59%). Data from participants who presented with morbidities that affect gait were excluded from the analysis (Figure 1). After exclusion, 108 male participants and 186 female participants remained, each of whom rated their health status as good to excellent on a 5-point ordinal scale. The study was approved by the Mayo Foundation Institutional Review Board and all subjects provided informed consent prior to participating in the study.
Figure 1.
The flow sheet describes participant selection, with exclusion criteria.
2.2 Instrumentation
Gait performance was measured with GAITRite® instrumentation (CIR Systems Inc., Havertown, PA) consisting of an electronic walkway 5.6 meters in length and 0.9 meters in width. The walkway encapsulated multiple sensor pads placed on 1.27 cm centers that were activated under pressure at footfall and deactivated at toe-off, enabling the system to capture the relative arrangement of footfalls as a function of time. Data were sampled at 80 Hz and processed using GAITRite® Platinum software.
2.3 Procedures
Subjects completed two walks across the walkway, initiating and terminating their walks one meter fore and aft of the walkway to minimize acceleration effects. Data from both walks were combined and considered as a single test. Subjects were instructed to walk at their normal pace and were not permitted to use gait aids during testing. Testing was conducted within a clinical research center.
We collected data from 16 spatiotemporal and temporophasic parameters that quantify mean values (Table 1). Additionally, we quantified variability in step length, stride length, step width, step time, stride time, stance time, swing time, stride speed and step width. We used the coefficient of variation (%CV) to reflect variability for each of the parameters with the exception of step width, for which we used the SD. Step width variability was expressed as the SD because the mean step width is relatively small in magnitude and therefore the %CV (the SD normalized to the magnitude of the mean) was excessively large in several cases and skewed the data, making parametric statistical analyses difficult to interpret.
Table 1.
Operational Definitions of Gait Parameters
| Gait Parameter | Operational Definition |
|---|---|
| Spatial Parameters | |
| Step Length (cm) | • Anterior-posterior distance from the heel of one footprint to the heel of the opposite footprint |
| Stride Length (cm) | • Anterior-posterior distance between heels of two consecutive footprints of the same foot (left to left, right to right); two steps (e.g., a right step followed by a left step) comprise one stride or one gait cycle |
| Step Width (cm) | • Lateral distance from heel center of one footprint to the line of progression formed by two consecutive footprints of the opposite foot |
| Temporal Parameters | |
| Cadence (steps/min) | • Number of steps per minute, sometimes referred to as step rate |
| Step Time (s) | • Time elapsed from initial contact of one foot to initial contact of the opposite foot |
| Stride Time (s) | • Time elapsed between the initial contacts of two consecutive footfalls of the same foot |
| Stance Time (s) | • The stance phase is the weight bearing portion of each gait cycle initiated at heel contact and ending at toe off of the same foot; stance time is the time elapsed between the initial contact and the last contact of a single footfall |
| Swing Time (s) | • The swing phase is initiated with toe off and ends with initial contact of the same foot; swing time is the time elapsed between the last contact of the current footfall to the initial contact of the next footfall of the same foot |
| Single Support Time (s) | • Single support occurs when only one foot is in contact with the ground; single support time is the time elapsed between the last contact of the opposite footfall to the initial contact of the next footfall of the same foot |
| Double Support Time (s) | • Double support occurs when both feet are in contact with the ground simultaneously; double support time is the sum of the time elapsed during two periods of double support in the gait cycle |
| Temporophasic Parameters | |
| Stance Time (%GC) | • Stance time normalized to stride time |
| Swing Time (%GC) | • Swing time normalized to stride time |
| Single Support Time (%GC) | • Single support time normalized to stride time |
| Double Support Time (%GC) | • Double support time normalized to stride time |
| Spatiotemporal Parameters | |
| Gait Speed (cm/s) | • Calculated by dividing the distance walked by the ambulation time |
| Stride Speed (cm/s) | • Calculated by dividing stride length by the stride time |
Note: cm = centimeters; s = seconds; %GC = % gait cycle
2.4 Data Analysis
Data were analyzed with SPSS 15.0 software (SPSS Inc., Chicago, IL). Principal components factor analysis with varimax rotation was used to examine factors with eigenvalues exceeding 1.0 that characterized gait performance. Parameters with correlation loadings of 0.5 or higher were interpreted as being significant contributors to the factor. Once the factor analysis was completed, then data under each domain were analyzed with two-way multivariate analysis of variance (MANOVA), comparing gender and age group (ages 70–74, 75–79, 80–84, and 85+) as independent variables (α = 0.05), and post-hoc Bonferroni corrections for multiple comparisons for significant MANOVAs.
3. Results
3.1 Factor Analysis
Five factors accounted for 83.3% of the variance in gait performance (Table 2). The first factor accounted for 25.8% of the variance in gait performance and loaded highly on temporal parameters quantifying cadence, step time, stride time, swing time, stance time and single limb support time. We labeled this factor a “rhythm” factor. The second factor accounted for 20.0% of the variance and loaded highly on temporophasic divisions of the gait cycle comprising swing, stance, single limb support, and double limb support as well as double limb support time. We labeled this factor a “phase” factor. The third factor accounted for 19.1% of the variance and loaded highly on the variability parameters, excluding step width variability. We labeled this factor a “variability” factor. The fourth factor accounted for 11.6% of the variance and loaded highly on gait speed, step length and stride length. We labeled this factor a “pace” factor. The last factor accounted for 6.9% of the variance in gait performance and loaded highly on step width and step width variability. We labeled this factor a “base of support” factor.
Table 2.
Factor Loadings of Gait Parameters on Five Factors Rotated and Extracted by Factor Analysis
| Gait Parameter | Rhythm | Phases | Variability | Pace | Base of Support |
|---|---|---|---|---|---|
| Gait Speed (cm/s) | −0.463 | 0.368 | −0.087 | 0.779 | 0.088 |
| Cadence (steps/min) | −0.940 | 0.021 | 0.228 | 0.016 | 0.009 |
| Mean Step Time (s) | 0.955 | −0.080 | −0.093 | −0.027 | −0.091 |
| Mean Step Length | 0.135 | 0.335 | −0.173 | 0.900 | 0.055 |
| Mean Stride Time (s) | 0.970 | −0.063 | −0.143 | −0.035 | −0.116 |
| Mean Stride Length (cm) | 0.123 | 0.380 | −0.211 | 0.874 | 0.022 |
| Mean Step Width (cm) | 0.202 | −0.012 | −0.080 | −0.123 | −0.841 |
| Mean Swing (%GC) | −0.015 | 0.910 | −0.007 | 0.245 | 0.043 |
| Mean Swing Time (s) | 0.838 | 0.447 | −0.120 | 0.123 | −0.067 |
| Mean Stance (%GC) | 0.028 | −0.894 | 0.010 | −0.199 | 0.032 |
| Mean Stance Time (s) | 0.898 | −0.356 | −0.135 | −0.109 | −0.100 |
| Single Support (%GC) | 0.159 | 0.759 | −0.339 | 0.145 | 0.101 |
| Single Support Time (s) | 0.826 | 0.397 | −0.263 | 0.094 | −0.018 |
| Double Support (%GC) | −0.088 | −0.921 | 0.217 | −0.233 | −0.068 |
| Double Support Time (s) | 0.541 | −0.756 | 0.037 | −0.243 | −0.140 |
| Step Length Variability (%CV) | −0.374 | −0.112 | 0.593 | −0.213 | −0.084 |
| Step Time Variability (%CV) | −0.322 | −0.024 | 0.695 | −0.108 | −0.055 |
| Stride Length Variability (%CV) | −0.100 | −0.036 | 0.883 | −0.093 | 0.041 |
| Stride Time Variability (%CV) | −0.130 | −0.117 | 0.921 | −0.018 | 0.136 |
| Swing Time Variability (%CV) | −0.273 | −0.167 | 0.832 | 0.009 | 0.079 |
| Stance Time Variability (%CV) | 0.008 | −0.059 | 0.702 | −0.042 | 0.379 |
| Stride Speed Variability (%CV) | 0.188 | −0.113 | 0.526 | −0.036 | 0.058 |
| Step Width Variability SD (cm) | −0.035 | 0.136 | 0.166 | −0.027 | 0.778 |
| % of Variance | 25.8 | 20.0 | 19.1 | 11.6 | 6.9 |
Note: Bolded correlation coefficients are interpreted as significant contributors to the identified factor.
3.2 Gender and Age Group Comparisons
Descriptive data for parameters constituting the five domains of gait performance, by gender and age, are presented in Table 3.
Table 3.
Normative Data (Mean±SD) for Parameters Constituting Rhythm, Phases, Variability, Pace and Base of Support Domains of Gait Performance by Gender and Age
| Parameter | Men (N=108) | Women (N=186) | ||||||
|---|---|---|---|---|---|---|---|---|
| 70–74 | 75–79 | 80–84 | 85+ | 70–74 | 75–79 | 80–84 | 85+ | |
| N=27 | N=30 | N=37 | N=14 | N=33 | N=77 | N=43 | N=33 | |
| Rhythm | ||||||||
| Cadence (steps/min)* | 102±8 | 106±10 | 103±8 | 102±11 | 113±20 | 114±13 | 110±9 | 108±10 |
| Step Time (s)† | 0.59±.05 | 0.56±.05 | 0.59±.04 | 0.59±.08 | 0.53±.06 | 0.53±.06 | 0.55±.05 | 0.56±.05 |
| Stride Time (s)‡ | 1.18±.08 | 1.13±.09 | 1.16±.08 | 1.19±.14 | 1.06±.13 | 1.06±.12 | 1.10±.09 | 1.12±.11 |
| Swing Time (s)§ | 0.43±.03 | 0.41±.03 | 0.42±.04 | 0.42±.05 | 0.39±.05 | 0.38±.05 | 0.39±.04 | 0.40±.04 |
| Stance Time (s)¶ | 0.75±.07 | 0.72±.06 | 0.74±.06 | 0.78±.11 | 0.68±.10 | 0.67±.08 | 0.71±.07 | 0.72±.09 |
| Single Support Time (s)# | 0.44±.03 | 0.42±.03 | 0.42±.04 | 0.42±.04 | 0.39±.06 | 0.38±.06 | 0.39±.04 | 0.40±.04 |
| Phases | ||||||||
| Swing (%GC) | 36.6± 1.5 | 36.7±1.5 | 36.6±2.8 | 35.1±2.69 | 36.6±2.6 | 36.1±3.0 | 35.5±2.5 | 35.7±2.6 |
| Stance (%GC) | 63.2±2.1 | 64.0±2.5 | 63.8±2.7 | 64.9±2.7 | 63.3±3.1 | 63.9±3.0 | 64.5±2.6 | 64.5±2.5 |
| Single Support (%GC) | 37.1±1.8 | 37.0±1.7 | 36.5±2.2 | 35.2±2.1 | 37.0±3.20 | 35.8±4.8 | 35.6±2.4 | 35.7±2.8 |
| Double Support (%GC) | 26.3±3.0 | 26.5±2.3 | 27.4±4.7 | 30.3±3.5 | 27.14±4.0 | 28.4±6.4 | 29.0±4.6 | 28.7±4.8 |
| Double Support Time (s)** | 0.31±.05 | 0.30±.04 | 0.32±.06 | 0.36±.08 | 0.29±.06 | 0.30±.06 | 0.32±.06 | 0.32±.08 |
| Variability | ||||||||
| Step Length (%CV) | 4.6±6.7 | 5.4±2.7 | 5.1±2.8 | 5.8±3.4 | 7.7±11.6 | 5.7±7.2 | 5.9±2.7 | 6.2±2.4 |
| Step Time (%CV) | 5.2±6.9 | 4.1±2.9 | 4.7±2.0 | 5.0±1.7 | 7.1±8.6 | 5.9±6.4 | 5.5±2.6 | 5.5±2.6 |
| Stride Length (%CV) | 2.9±1.1 | 4.2±4.6 | 3.8±2.0 | 5.7±3.2 | 4.1±4.7 | 4.7±5.6 | 4.3±2.1 | 5.2±5.2 |
| Stride Time (%CV) | 3.5±2.2 | 3.8±4.4 | 3.3±1.9 | 5.3±3.7 | 3.9±3.9 | 5.2±6.9 | 4.4±1.9 | 4.9±5.3 |
| Swing Time (%CV) | 4.5±2.2 | 4.5±7.8 | 5.1±2.2 | 8.6±11.4 | 6.2±10.5 | 8.5±9.5 | 6.2±2.2 | 8.0±9.7 |
| Stance Time (%CV) | 4.9±4.6 | 5.9±7.0 | 4.7±3.0 | 5.3±2.9 | 5.7±4.4 | 5.3±5.1 | 5.3±2.9 | 5.6±4.1 |
| Stride Speed (%CV) | 5.0±2.9 | 5.5±4.4 | 5.5±3.2 | 7.3±3.8 | 5.6±3.4 | 5.5±2.7 | 6.8±3.2 | 6.9±3.3 |
| Pace | ||||||||
| Gait Speed (cm/s)†† | 117±16 | 122±15 | 112±17 | 101±22 | 116±20 | 112±17 | 101±15 | 98±20 |
| Step Length (cm)‡‡ | 69±8 | 68±7 | 65±8 | 59±10 | 61±9 | 59±7 | 55±7 | 54±9 |
| Stride Length (cm)§§ | 139±14 | 137±12 | 131±17 | 119±21 | 123±17 | 118±15 | 111±14 | 109±18 |
| Base of Support | ||||||||
| Step Width (cm)¶¶ | 9.7±3.0 | 8.9±5.2 | 11.2±4.0 | 9.9±4.8 | 7.0±3.5 | 7.7±4.0 | 7.9±4.1 | 9.1±2.6 |
| Step Width SD (cm) | 3.1±2.2 | 2.9±1.9 | 3.3±2.3 | 2.8±1.2 | 3.4±2.4 | 3.2±2.5 | 3.6±3.1 | 3.0±1.1 |
mean difference in cadence between genders is 8.3 steps/min (p<0.001, 95%CI=5.4–11.1 steps/min);
mean difference in step time between genders is 0.04 s (p<0.001, 95%CI=0.03–0.06 s);
mean difference in stride time between genders is 0.09 s (p<0.001, 95%CI=0.06–0.11 s);
mean difference in swing time between genders is 0.03 s (p<0.001, 95% CI=0.02–0.04 s);
mean difference in stance time between genders is 0.05 s (p=0.004, 95%CI=0.03–0.07 s);
mean difference in single limb support time between genders is 0.04 s (p<0.001, 95%CI=0.03–0.05 s);
mean difference in double support time between genders is 0.02 s (p=0.05, 95%CI=0.00–0.03 s);
mean difference in gait speed between genders is 7 cm/s (p=0.002, 95%CI=2.7–11.5 cm/s);
mean difference in step length between genders is 9.0 cm (p<0.001, 95%CI=7.0–11.0 cm); mean difference in stride length between genders is 17.5 cm (p<0.001, 95%CI=13.6–21.5 cm);
mean difference in step width between genders is 2.2 cm (p<0.001, 95%CI=1.2–3.1 cm).
3.2.1 Rhythm
The gender main effect was significant (F6,281=7.030, p<0.001), though neither the age group main effect (F18,849=1.612, p=0.051) nor gender × age group interaction (F18,849=0.749, p=0.783) were statistically significant. Men walked at a lower cadence and with greater step times, stride times, swing times, stance times, and single limb support times than did women. Men walked at approximately 103 steps/min and had mean step and stride times of 0.58 and 1.16 s, respectively; mean swing and stance times of 0.42 and 0.74 s, respectively; and mean single limb support times of 0.43 s. Women, in contrast, walked at approximately 112 steps/min and had shorter mean step and stride times of 0.54 s and 1.08 s, respectively; shorter mean swing and stance times of 0.39 s and 0.69 s, respectively; and shorter mean single limb support times of 0.39 s.
3.2.2 Gait Cycle Phases
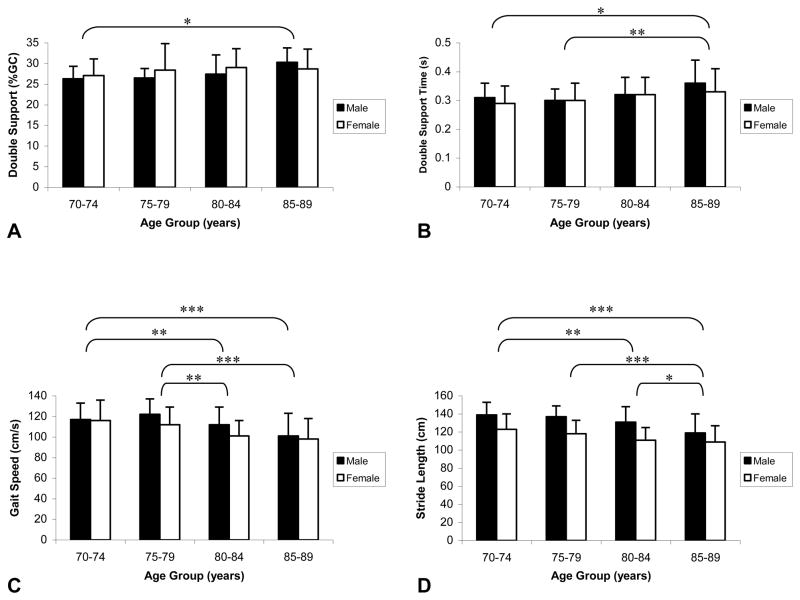
In contrast to the rhythm domain, for the phasic parameters both the gender (F5,282=4.981, p<0.001) and age group main effects (F15,852=1.750, p=0.037) were significant, though the gender × age group interaction was not (F15,852=0.956, p=0.500). On further analysis, only double limb support time differed between genders (F1,286=4.796, p=0.029). Double support time was approximately 0.32 s in men and 0.30 s in women. Age group effects (Figure 2) were only present in the double limb support phase (F3,286=3.199, p=0.024) and double limb support time parameters (F3,286=6.334, p<0.001). Participants in the 85+ age group spent longer periods in double limb support.
Figure 2.
The phase and pace domains of gait performance had significant age group effects. The proportion of the gait cycle spent in double limb support (A) was greater in the 85+ year age group than in the 70–74 year age group. Double limb support time (B) was greater in the 85+ year age group than in the 70–74 year age group and in the 75–79 year age group. Gait speed (C) in the 80–84 and 85+ year age groups was slower than in the 70–74 and 75–79 year age groups. Stride lengths (D) and step lengths (not illustrated because step length data are one-half the length of stride length data but show identical statistical comparisons) in the 85+ year age group were shorter than in the 70–74, 75–79 and 80–84 year age groups, and were shorter in the 80–84 year age group than in the 70–74 year age group. Note: * denotes Bonferroni-adjusted p<0.05, ** denotes Bonferroni-adjusted p<0.01, *** denotes Bonferroni-adjusted p<0.001.
3.2.3 Variability
Neither the gender (F7,278=0.651, p=0.713) nor age group main effects (F21,840=1.466, p=0.081) were statistically significant for the variability measurements, nor was the gender × age group interaction (F21,840=1.010, p=0.448).
3.2.4 Pace
For the pace domain of gait performance, the gender (F3,284=34.937, p<0.001) and age group main effects (F9,858=4.798, p<0.001) were statistically significant, though the gender × age group interaction was not (F9,858=1.076, p=0.378). Men walked faster and with longer step and stride lengths than did women. Men walked at approximately 115 cm/s and had mean step lengths of 66 cm and stride lengths of 133 cm. Women walked at approximately 108 cm/s and had mean step lengths of 57 cm and stride lengths of 115 cm. When normalized to height, however, the gender difference in gait speed was negated (F1,286=1.516, p=0.219). Gait speed, step lengths and stride lengths were greater in the 70–74 and 75–79 than in the 80–84 and 85+ age groups (Figure 2).
3.2.5 Base of Support
Similar to the rhythm domain analysis, the gender main effect was statistically significant in the base of support domain (F2,284=8.669, p<0.001), though neither the age group main effect (F6,570=1.897, p=0.079) nor gender × age group interaction (F6,570=0.940, p=0.466) were significant. Mean step width in men was approximately 10.0 cm whereas mean step width in women was approximately 7.9 cm. Step width variability did not differ between men and women.
4. Discussion
While several studies have provided reference values for gait [2,7–11], we believe the present study represents one of the most comprehensive analyses of normative spatiotemporal gait data in older adults. The breadth of gait parameters analyzed exceeds that of previous studies and, secondarily, the extent to which morbidities were controlled and participants excluded assured that data represent gait performance in able-bodied participants. Normative data for nearly two dozen spatiotemporal gait parameters comprising five domains of gait performance in older adults are provided from which results of other studies or clinical measures can be compared.
The findings expand on the factors that Verghese et al described [4]. First, while Verghese et al identified a rhythm factor characterized by cadence and swing time, our study suggests that several additional temporal parameters including step time, stride time, stance time and single limb support time also load highly on the factor. Second, while Verghese et al identified a variability factor that loaded highly on stride length variability, our study suggests several parameters contribute to a variability domain of gait performance. Gait cycle variability parameters including variability in stride length, stride time, stance time, swing time and stride speed all load highly on the factor, as do step variability parameters including step length and step time variability. Third, both studies identified a pace factor characterized by gait speed, step length and stride length. We believe two additional factors, however, also characterize gait performance: a phasic factor characterized by temporophasic proportions of the gait cycle spent in stance, swing and single and double limb support; and a base of support factor characterized by step width and step width variability.
Parameters in the pace domain have been studied most extensively among the domains identified in the present study and provide for readily available comparisons. Gait speed, for example, has been recommended as a “vital sign” for physical performance in older persons [1, 3] and 10 cm/s decreases in gait speed are associated with higher falls risk in older persons [13]. It is important that researchers and clinicians understand normative values for pace parameters in older adults. Mean gait speed (110±19 cm/s, 95%CI=107.8–112.2 cm/s) and stride length measurements (122±19 cm, 95%CI=119.8–124.2 cm) reported in our study are largely consistent with other studies reporting reference values for preferred gait speed in older adults. For example, Oh-Park et al [10], using similar methods and instrumentation to collect gait data and using similarly aged subjects, reported an overall mean gait speed of 106 cm/s and a mean stride length of 121 cm in 304 robust, healthy older individuals. Callisaya et al [8], also using similar methods and instrumentation, reported slightly greater mean gait speed (116 cm/s in men and 111 cm/s in women) and stride length measurements (approximately 130 cm in men and 115 cm in women) in a population-based sample of 411 older adults; those differences, however, may be accounted for because they included subjects aged 60–69 that were not included in our study or in the Oh-Park study. Given the relative similarities between studies, we believe our findings represent valid target values of pace parameters in persons over the age of 70 for assessing abnormal gait.
Regarding gender differences in the pace domain, most studies indicate that gait speed and stride length in men exceeds that of women [8,10,11]. Our findings were similar. Gait speed in men exceeded that in women by approximately 7 cm/s (95%CI=2.7–11.5 cm/s) and stride length in men exceed that in women by approximately 18 cm (95%CI=13.6–21.5 cm). When gait speed was normalized to height, however, the difference between genders was no longer significant, indicating that gait speed is more a function of height than it is gender. Interestingly, when stride length and cadence were also normalized to height, the gender differences remained. Men tended to walk with longer strides but with lower cadences.
In cross-sectional comparisons, most studies indicate that gait speed and stride length decrease with age. Himann et al [14] reported that gait speed decreases 12% to 16% per decade after the age of 70. Oh-Park et al [10] reported similar reductions in gait speed and stride length in a population-based sample of people over the age of 70, although those reductions were minimized in a subsample characterized as robust, healthy individuals. Our cross-sectional findings suggest that parameters in the pace domain of gait are equivalent among persons in the 70–74 and 75–79 year age groups, but decrease significantly past the age of 80 (Figure 2). The functional impact becomes evident when one realizes that walking at 120 cm/s is necessary to navigate typical urban crosswalks [15]. Among participants aged 70–79 years, 42% walked at a speed that exceeded 120 cm/s. In the 80–84 and 85+ year age groups, however, those proportions dropped to 18% and 15%, respectively. These data suggest that, even in good health, some decline in gait performance is inevitable in older persons and that decline is likely to produce functional deficits.
A rhythm factor accounted for 25.8% of the variance in gait performance. It loaded highly on cadence and temporal parameters including step, stride, swing, stance and single limb support time. Rhythm measurements reported in the present study are largely consistent with other studies reporting reference values in older adults. The mean cadence (109±13 steps/min), for example, is slightly greater but similar to the cadence of 105.2 steps/min that Oh-Park et al reported [10]. Mean cadences for men (103 steps/min) and women (112 steps/min) are similar to values (107.2 and 114.6 steps/min, respectively) that Callisaya et al reported [8]. Likewise, the mean swing time (0.40±0.05 s) is similar to the 0.43-s swing time that Oh-Park et al reported [10]; and step times (0.58±0.05 s in men, 0.54±0.06 s in women) are similar to step times (0.56 and 0.53 s, respectively) that Callisaya et al reported [8]. Quantifying rhythm and understanding normative values for parameters representing the rhythm domain are important because changes in rhythm may be associated with increased risk of dementia and memory decline [4].
A variability factor accounted for 19.1% of the variance in gait performance in our study. Comparing variability values with other studies is hindered because of inconsistencies between studies that use the CV versus the SD to report variability. When our data are expressed as the SD, stride length variability (4.4±4.2 %CV, or 5.0±4.4-cm SD) and swing time variability data (6.6±9.3 %CV, or 0.03±0.03-cm SD) are very similar to the 4.6-cm and 0.03-cm variability values, respectively, that Verghese et al reported [4]. Likewise, stance time variability (5.3±4.5 %CV, or 0.037±0.030-s SD) is nearly identical to the 0.038-s stance time variability that Brach et al reported [16]. Our step variability data demonstrate similar consistencies with other studies. Step length variability (5.9±6.0 %CV, or 3.3±2.7-cm SD) is similar in magnitude to the 6.4 %CV step length variability that Brach et al reported [17] and to the 2.8-cm variability that Callisaya reported [8]. Step time variability (5.6±5.3 %CV, or 0.03±0.02-s SD) is similar in magnitude to the 0.02-s step time variability data that Callisaya reported. Given the relative similarities between studies, we believe our findings represent valid target variability parameters for assessing abnormal gait.
Increased variability reflects a loss of automaticity in walking that presumably makes persons more susceptible to falling. Variability parameters have been used to quantify falls risk, to assess risk of dementia and, under dual task conditions, to examine executive functioning in aging adults [4,5,18,19]. Variability parameters used to examine these capacities have included variability in stride speed [20,21], stride time [18], stride length [4], step time [22], step length [22], swing time [4,23] and step width [22,24]. Few studies have examined multiple modes of variability collectively, presumably because investigators assumed that each parameter, be it a marker of gait cycle variability, step variability or base of support variability, represents a similar construct. Some researchers have challenged that assumption, reporting that stride time variability and stride length variability, for example, respond differently to speed of walking and to dual task walking [25]. Findings from our study suggest that each of the gait cycle and step variability parameters, apart from stride width variability, represent one variability construct.
A phase factor representing temporophasic divisions of the gait cycle was a fourth factor identified in our study. While a phase factor was not previously identified in a factor analysis [4], considering gait phases is relevant. A 10% decrease in the swing phase proportion of the gait cycle, for example, may be associated with higher falls risk in older persons [13]. In our study, the stance phase represented 63.9% (95%CI=63.6–64.2 %GC) and the swing phase represented 36.1% of the gait cycle (95%CI=35.8–36.4 %GC), values that are consistent with the stance (63%) and swing (37%) phase proportions in healthy older men established by Murray et al [26]. Double limb support occupied 27.9% (95%CI=27.3–28.5 %GC) and single limb support occupied 36.2% of the gait cycle (95%CI=35.8–36.6 %GC). To our knowledge, normative values for all of these gait cycle phases have not been established for older adults. The values differ slightly from norms established by the Rancho Los Amigos (RLA) National Rehabilitation Center (stance phase 62%, swing phase 38%, double support 24% and single support 38% [27]), but that likely represents the fact that older participants in our study walked more slowly (110 cm/s) than presumably younger subjects represented in the RLA data, who walked at an average of 136 cm/s.
Last, a base of support factor characterized by step width and step width variability accounted for 6.9% of the variability in gait performance. Mean step width was 10.0 cm in men (95%CI=9.5–10.5 cm) and 7.9 cm in women (95%CI=7.5–8.3 cm), magnitudes similar to population-based step width data reported elsewhere [8]. Mean step width variability, which did not differ between genders, was 3.2 cm (95%CI=2.9–3.5 cm), approximately 1 cm greater than that reported elsewhere [8]. The influence of the base of support factor associated with aging is equivocal. Step width variability may distinguish older from younger adults [22] and may be associated with peripheral sensory impairments that contribute to gait dysfunction [28]. Others have characterized increased step width as an adaptation by aging persons who are fearful of falling, but reported that step width itself is not a predictor of falling [29]. In contrast, reduced and increased step width variability have been associated with falls histories [24]. While the association of step width and step width variability with aging and fall risk is not certain, findings of the present study indicate that examining a base of support factor is warranted.
Several limitations in the study should be considered. First, subjects walked at self-selected speeds, not at maximum speeds. Interpretations of the findings should not be generalized to one’s ability to walk faster than at self-selected speeds. Second, this study represents a secondary analysis of a population-based cohort study designed to investigate the prevalence, incidence and risk factors for dementia [12]. The primary study screened a variety of cardiovascular, neurological and other medical conditions like diabetes and cancer, but data on specific orthopedic or rheumatologic conditions that might influence gait were not collected. While the findings represent normative data for able-bodied older adults, the results may misrepresent gait parameters in older adults in whom specific orthopedic or rheumatologic conditions are definitively absent. Last, data for the study were collected from an average of 14±4 steps (7 strides) per participant. While there is evidence that measuring pace and rhythm parameters is highly reliable with even small numbers of strides, reliability for other gait domains, particularly variability, may be enhanced by collecting data from hundreds of strides [30]. Validity of that data may be questioned.
5. Conclusion
Data for 23 spatiotemporal gait parameters were collected from subjects aged 70+. Normative values are presented which researchers or clinicians can use for assessing and interpreting gait dysfunction. Based on factor analysis, five domains of gait performance were identified. A rhythm domain was characterized by cadence and temporal parameters (e.g., stride time). A phase domain was characterized by temporophasic divisions of the gait cycle. A variability domain encompassed gait cycle variability characterized by variability in stride measurements, and step variability characterized by variability in step measurements. A pace domain was characterized by gait speed, step length and stride length. A base of support domain was characterized by step width and step width variability. Several gender and age group differences were present among the domains. We recommend that data representing each of these domains be collected when gait analyses are conducted.
Acknowledgments
This work was supported by grants from the National Institute on Aging (P50 AG16574 and U01 AG06786), the National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01 AR30582), and by the Robert H. and Clarice Smith and Abigail Van Buren Alzheimer’s Disease Research Program. Study sponsors had no involvement in the study design; in the collection, analysis or interpretation of data; in the writing of the manuscript; nor in the decision to submit the manuscript for publication. The authors thank Matthew R. Miller for his assistance with data collection and organization.
Footnotes
Conflict of Interest Statement
None of the authors has a financial or personal relationship with people or organizations that could inappropriately influence this work.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ferrucci L, Baldasseroni S, Bandinelli S, de Alfieri W, Cartei A, Calvani D, Baldini A, Masotti G, Marchionni N. Disease severity and health-related quality of life across different chronic conditions. J Am Geriatr Soc. 2000;48:1490–1495. [PubMed] [Google Scholar]
- 2.Cesari M, Kritchevsky SB, Penninx BWHJ, Nicklas BJ, Simonsick EM, Newman AB, Tylavsky FA, Brach JS, Satterfield S, Bauer DC, Visser M, Rubin SM, Harris TB, Pahor M. Prognostic value of usual gait speed in well-functioning older people--results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53:1675–1680. doi: 10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- 3.Studenski S, Perera S, Wallace D, Chandler JM, Duncan PW, Rooney E, Fox M, Guralnik JM. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003;51:314–322. doi: 10.1046/j.1532-5415.2003.51104.x. [DOI] [PubMed] [Google Scholar]
- 4.Verghese J, Wang C, Lipton RB, Holtzer R, Xue X. Quantitative gait dysfunction and risk of cognitive decline and dementia. J Neurol Neurosurg Psychiatr. 2007;78:929–935. doi: 10.1136/jnnp.2006.106914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maki BE. Gait changes in older adults: predictors of falls or indicators of fear. J Am Geriatr Soc. 1997;45:313–320. doi: 10.1111/j.1532-5415.1997.tb00946.x. [DOI] [PubMed] [Google Scholar]
- 6.Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, Brach J, Chandler J, Cawthon P, Connor EB, Nevitt M, Visser M, Kritchevsky S, Badinelli S, Harris T, Newman AB, Cauley J, Ferrucci L, Guralnik J. Gait speed and survival in older adults. JAMA. 2011;305:50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bohannon RW. Population representative gait speed and its determinants. J Geriatr Phys Ther. 2008;31:49–52. doi: 10.1519/00139143-200831020-00002. [DOI] [PubMed] [Google Scholar]
- 8.Callisaya ML, Blizzard L, Schmidt MD, McGinley JL, Srikanth VK. Ageing and gait variability--a population-based study of older people. Age Ageing. 2010;39:191–197. doi: 10.1093/ageing/afp250. [DOI] [PubMed] [Google Scholar]
- 9.Oberg T, Karsznia A, Oberg K. Basic gait parameters: reference data for normal subjects, 10–79 years of age. J Rehabil Res Dev. 1993;30:210–223. [PubMed] [Google Scholar]
- 10.Oh-Park M, Holtzer R, Xue X, Verghese J. Conventional and robust quantitative gait norms in community-dwelling older adults. J Am Geriatr Soc. 2010;58:1512–1518. doi: 10.1111/j.1532-5415.2010.02962.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Samson MM, Crowe A, de Vreede PL, Dessens JA, Duursma SA, Verhaar HJ. Differences in gait parameters at a preferred walking speed in healthy subjects due to age, height and body weight. Aging Clin Exp Res. 2001;13:16–21. doi: 10.1007/BF03351489. [DOI] [PubMed] [Google Scholar]
- 12.Roberts RO, Geda YE, Knopman DS, Cha RH, Pankratz VS, Boeve BF, Ivnik RJ, Tangalos EG, Petersen RC, Rocca WA. The Mayo Clinic Study of Aging: design and sampling, participation, baseline measures and sample characteristics. Neuroepidemiology. 2008;30:58–69. doi: 10.1159/000115751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Verghese J, Holtzer R, Lipton RB, Wang C. Quantitative gait markers and incident fall risk in older adults. J Gerontol A Biol Sci Med Sci. 2009;64:896–901. doi: 10.1093/gerona/glp033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Himann JE, Cunningham DA, Rechnitzer PA, Paterson DH. Age-related changes in speed of walking. Med Sci Sports Exerc. 1988;20:161–166. doi: 10.1249/00005768-198820020-00010. [DOI] [PubMed] [Google Scholar]
- 15.Langlois JA, Keyl PM, Guralnik JM, Foley DJ, Marottoli RA, Wallace RB. Characteristics of older pedestrians who have difficulty crossing the street. Am J Public Health. 1997;87:393–397. doi: 10.2105/ajph.87.3.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brach JS, Perera S, Studenski S, Katz M, Hall C, Verghese J. Meaningful change in measures of gait variability in older adults. Gait Posture. 2010;31:175–179. doi: 10.1016/j.gaitpost.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brach JS, Berthold R, Craik R, VanSwearingen JM, Newman AB. Gait variability in community-dwelling older adults. J Am Geriatr Soc. 2001;49:1646–1650. doi: 10.1046/j.1532-5415.2001.t01-1-49274.x. [DOI] [PubMed] [Google Scholar]
- 18.Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82:1050–1056. doi: 10.1053/apmr.2001.24893. [DOI] [PubMed] [Google Scholar]
- 19.Sheridan PL, Solomont J, Kowall N, Hausdorff JM. Influence of executive function on locomotor function: divided attention increases gait variability in Alzheimer’s disease. J Am Geriatr Soc. 2003;51:1633–1637. doi: 10.1046/j.1532-5415.2003.51516.x. [DOI] [PubMed] [Google Scholar]
- 20.Beauchet O, Kressig RW, Najafi B, Aminian K, Dubost V, Mourey F. Age-related decline of gait control under a dual-task condition. J Am Geriatr Soc. 2003;51:1187–1188. doi: 10.1046/j.1532-5415.2003.51385.x. [DOI] [PubMed] [Google Scholar]
- 21.Hollman JH, Kovash FM, Kubik JJ, Linbo RA. Age-related differences in spatiotemporal markers of gait stability during dual task walking. Gait Posture. 2007;26:113–119. doi: 10.1016/j.gaitpost.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 22.Owings TM, Grabiner MD. Step width variability, but not step length variability or step time variability, discriminates gait of healthy young and older adults during treadmill locomotion. J Biomech. 2004;37:935–938. doi: 10.1016/j.jbiomech.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 23.Hausdorff JM, Schweiger A, Herman T, Yogev-Seligmann G, Giladi N. Dual-task decrements in gait: contributing factors among healthy older adults. J Gerontol A Biol Sci Med Sci. 2008;63:1335–1343. doi: 10.1093/gerona/63.12.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brach JS, Berlin JE, VanSwearingen JM, Newman AB, Studenski SA. Too much or too little step width variability is associated with a fall history in older persons who walk at or near normal gait speed. J Neuroeng Rehabil. 2005;2:21. doi: 10.1186/1743-0003-2-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beauchet O, Dubost V, Gonthier R, Kressig RW. Dual-task-related gait changes in transitionally frail older adults: the type of the walking-associated cognitive task matters. Gerontology. 2005;51:48–52. doi: 10.1159/000081435. [DOI] [PubMed] [Google Scholar]
- 26.Murray MP, Kory RC, Clarkson BH. Walking patterns in healthy old men. J Gerontol. 1969;24:169–178. doi: 10.1093/geronj/24.2.169. [DOI] [PubMed] [Google Scholar]
- 27.Department of Pathokinesiology and Physical Therapy. Observational Gait Analysis Handbook. Downey, CA: Los Amigos Research and Education Institute, Inc., Rancho Los Amigos National Rehabilitation Center; 2001. [Google Scholar]
- 28.Brach JS, Studenski S, Perera S, VanSwearingen JM, Newman AB. Stance time and step width variability have unique contributing impairments in older persons. Gait Posture. 2008;27:431–439. doi: 10.1016/j.gaitpost.2007.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chamberlin ME, Fulwider BD, Sanders SL, Medeiros JM. Does fear of falling influence spatial and temporal gait parameters in elderly persons beyond changes associated with normal aging? J Gerontol A Biol Sci Med Sci. 2005;60:1163–1167. doi: 10.1093/gerona/60.9.1163. [DOI] [PubMed] [Google Scholar]
- 30.Hollman JH, Childs KB, McNeil ML, Mueller AC, Quilter CM, Youdas JW. Number of strides required for reliable measurements of pace, rhythm and variability parameters of gait during normal and dual task walking in older individuals. Gait Posture. 2010;32:23–28. doi: 10.1016/j.gaitpost.2010.02.017. [DOI] [PubMed] [Google Scholar]