Abstract
Purpose
We used Organization Risk Analyzer (ORA), a dynamic network analysis tool, to identify patient care unit communication patterns associated with patient safety and quality outcomes. Although ORA had previously had limited use in healthcare, we felt it could effectively model communication on patient care units.
Methods
Using a survey methodology, we collected communication network data from nursing staff on seven patient care units on two different days. Patient outcome data were collected via a separate survey. Results of the staff survey were used to represent the communication networks for each unit in ORA. We then used ORA's analysis capability to generate communication metrics for each unit. ORA's visualization capability was used to better understand the metrics.
Results
We identified communication patterns that correlated with two safety (falls and medication errors) and five quality (e.g., symptom management, complex self care, and patient satisfaction) outcome measures. Communication patterns differed substantially by shift.
Conclusion
The results demonstrate the utility of ORA for healthcare research and the relationship of nursing unit communication patterns to patient safety and quality outcomes.
Keywords: communication networks, ORA, informatics, safety, quality, nursing
I. Introduction
In this paper, we describe our use of Organization Risk Analyzer (ORA), a dynamic network analysis tool, to identify nursing unit communication patterns associated with patient safety and quality outcomes. The specific research questions posed in the exploratory study were:
Can ORA's visualizations be used to identify nursing unit network communication patterns that affect patient safety and quality outcomes?
Do unit network characteristics differ by shift?
What network characteristics measured by ORA metrics are related to specific safety and quality measures?
Communication has been implicated in much of the literature on safety and quality outcomes. Indeed effective communication is critical to assuring quality care. [1] Problems with communication have been linked to missed patient care, [2] poor patient outcomes, increased length of stay, increased costs and resource utilization, and even caregiver dissatisfaction and turnover. [3] Researchers have demonstrated the importance of communication for effective handoffs; [1, 4] preventing falls; [5, 6] improving job satisfaction, [7] and reducing medication errors. [8]
Stahl and colleagues showed that information degraded in a trauma unit over a 24-hour period, in part due to the multiple teams of caregivers with different schedules and responsibilities. [9] Failure to communicate critical information may be occurring in as many as 30% of team exchanges. [10] In one study, communication issues were linked to missed care 30% of the time, with most due to breakdowns in nurse-physician communication. [2]
This is not surprising given the amount of communication that takes place in healthcare. In acute care hospitals, for example, communication occurs on admission, during the process of providing patient care, during handoffs, and at discharge. The communication may be verbal, written, or computer-based. Some, perhaps a great deal, of the communication is actually interruptive. Some communication, such as the SBAR (Situation, Background, Assessment, and Recommendation) format that has become popular for shift or transfer reporting and SOAP (Subjective data, Objective data, Assessment, Plan) notes in electronic or paper documentation systems, is structured. Other communication is free-form. Some communication may be hierarchical in nature (i.e., top-down and directive); other communication is more diffuse and multidirectional.
To date, most research on nursing communication has involved person-to-person (e.g., doctor-nurse; patient-nurse) or team to team communication (e.g., handoffs, shift report). We speculated that analysis of a larger network (e.g., a patient care unit) might provide further information. However, conducting large group-level communication network studies would require different tools and metrics. One possible tool is social network analysis.
Social Network Analysis (SNA) is becoming increasingly popular for studying communication. SNA typically probes the patterns in relationships among people or organizations. [11] SNA can help visualize the connections between and among individuals, groups, or organizations, as well as provide metrics to clarify the communication patterns and communication-related roles in groups. SNA has been used to study processes such as the effect of competition, [12] the effect of centrality on perceived power, [13] turnover, [14] and social interaction after technology change.[15] However, SNA is useful only for small, well-bounded networks and assumes a static, position-based view of individuals, making it inadequate for modeling communication on dynamic patient care units.
Carley and colleagues extended SNA using an approach derived from knowledge management, operations research and social networks techniques. [16, 17] The resulting “dynamic network analysis” (DNA) represents an organization as a set of relations connecting people, knowledge, resources and tasks and the changes in those relations over time. DNA measures allow researchers to assess the structure or health of the organization and analyze organizational performance. [18] DNA can simulate large dynamic organizational networks, assess the current state of the organization and predict the potential impact of changes in those networks on organizational performance. DNA treats individuals as actively involved in communication, storing information, and learning. Both networks and individuals (agents) change dynamically and can learn. One DNA tool, ORA, was designed to identify individuals or groups that are potential risks to the organization. Although ORA had previously had limited use in healthcare, it had the capacity to model communication on busy patient care units. The communication networks developed in ORA can be explored at the unit or shift levels, visualized for better understanding, and compared using up to 80 metrics. Here we report the results of a study using ORA to examine the links between network communication on patient care units and patient safety and quality outcomes. The study is part of a larger research project aimed at developing a dynamic network analysis decision support tool for nurse managers.
2. Methodology
After obtaining approval from the University of Arizona Investigational Review Board and site approval from each hospital, we collected communication network data from individual nursing staff on seven patient care units in three Magnet hospitals in the Southwest. Data were collected on two different days. The specific days were pre-selected for each unit to have the least possible overlap of individual staff with the additional constraint that only week days were used. Our rationale for using only week days was that often weekends have fewer staff, which would have introduced another variable (weekend vs. week day) and also would have decreased the likelihood of an adequate response rate because of the increased workload.
The data were collected via an Organizational Network Analysis questionnaire adapted from [19]. The questionnaire listed all staff scheduled to work on that day (including the preceding and subsequent shifts) and asked staff to identify the individuals with whom they had interacted by placing a check mark beside their names. Staff were then asked to note how frequently they “got information from,” “gave information to,” or “discussed patient care with” those individuals with whom they had interacted using a 0–4 rating scale (0 = not at all; 1 = rarely, 2 = some, 3 = a lot, and 4 = constantly). To alleviate any privacy concerns, staff names were printed on a tear-off overlay that participants were instructed to remove before placing the questionnaire in a closed box on the patient care unit. This procedure ensured that the questionnaires the research team received listed only codes for each staff (e.g., RN 13). The questionnaire also allowed us to collect several demographic variables (Unit, Shift, Highest Level of Education, Length of Time Worked on the Unit, Length of Time Worked in the Hospital, Whether Certified in a Specialty, and Whether Full Time, Part Time, or Per Diem). As part of the larger study, we had previously collected a set of patient outcome data on the same units. The patient outcomes used in this study, together with their definitions and sources, are shown in Table I.
Table I.
Safety and Quality Outcome Variables, Definitions and Data Source
| Outcome | Definition | Data Source |
|---|---|---|
| Safety Outcomes | ||
| Total Falls | Falls (with and without injury) per 1000 patient days, averaged over the 3 months for which data were collected | Quality Improvement Survey |
| Total ADEs | Total adverse drug events (with and without injury) per 1000 patient days/averaged over 3 months | Quality Improvement Survey |
| Quality Outcomes | ||
| Symptom Management Difference | % of patients meeting a goal of a 1 point increase in their ability to manage their symptoms from admission to discharge | Patient Questionnaire scale [20] |
| Symptom Management Capacity | % of patients meeting a goal of a 1 point increase (from admission to discharge) in the ratio of symptom management to symptom distress. | Patient Questionnaire [20] |
| Simple Self Care Management | % of patients meeting a goal of 7.5 or higher on a Self Care scale (6 items related to simple self care) | Patient Questionnaire – Self Care Scale adapted from [21] |
| Complex Self Care Management | % of patients meeting a goal of 7.5 or higher on a Self Care scale (4 items related to complex self care) | Patient Questionnaire – Self Care Scale adapted from [21] |
| General Satisfaction with Nursing Care | % of patients meeting goal of score > 3 on Well Cared For Scale (6 items) | Well Cared For Patient Questionnaire [20] |
| Satisfaction with Caring | % of patients meeting goal of score > 3 on Well Cared For Scale (5 items) | Well Cared For Patient Questionnaire [20] |
| Satisfaction with Individual Needs being met | % of patients meeting goal of score > 3 on Well Cared For Scale (4 items) | Well Cared For Patient Questionnaire [20] |
Because network analyses are highly sensitive to response rates, for this study we used each unit's data from the day with the higher response rate. Data from the Organizational Network Analysis survey were used to create matrix structures called “metamatrices” in ORA by first creating Excel .csv files that listed, for each respondent, the individuals with whom they had discussed patient care with and the frequency of that discussion. These files were then entered into ORA, using a “Create metamatrix from table data” function. We used a similar procedure to link demographic characteristics (shift, age, education level, etc.) to the individuals (nodes) in the network.
Using ORA's visualization capability allowed us to check for data entry errors before analyzing the networks via ORA metrics. We found it useful to visualize the networks by shift (node color was used to differentiate the shifts) so that we could examine the links within and across shifts. Node size was used to visually display individual differences in specific ORA metrics. In this study, node size corresponds to Eigenvector Centrality values. Higher measures of Eigenvector Centrality indicate individuals who are connected to highly connected people (Table 2). Link color corresponds to communication frequency ratings. Thus, we were able to see, not only the connections among the staff by shift, but which staff were assigned to the day or night shift, how frequently they discussed patient care with each other, and which individuals were most frequently connected to other highly connected people.
Table II.
ORA Metrics Defined
| ORA Metric | Definition |
|---|---|
| Clustering Coefficient | Extent to which there are small clusters (cliques). The clustering coefficient gives a sense of the local characteristics of the network--how information spreads by means of employee groups. A higher clustering coefficient supports local information diffusion as well as a decentralized infrastructure because employees are likely to share information and know what is happening in their work group. |
| Component Count Strong | The number of strongly connected components in a network |
| Component Count Weak | The number of weakly connected components in a network |
| Density | Ratio of actual connections (technically “edges”) between individuals to possible connections for a network. It reflects the social level of organizational cohesion. |
| Diffusion | How fast information travels through the network. |
| Fragmentation | The proportion of entities (individuals) in a network that are disconnected. |
| Hierarchy | Degree to which the network has a purely hierarchical structure (i.e. unidirectional, usually top-down communication). |
| Isolates | Number of nodes (individuals) that have no connections or links. |
| Network Centralization In Degree | Number of connections coming into individual nodes (if higher, more individual connections) |
| Network Centralization Out Degree | Number of connections out of individual nodes (if higher, more individual connections) |
| Eigenvector Centrality | Measure of node connections to highly connected to highly connected people (node-level metric is averaged for network score). A person well-connected to well-connected people can spread information quickly and could be critical when rapid communication is needed. |
| Simmelian Ties | Number of strong ties embedded in cliques [22] |
| Betweenness Centrality | Measures the number of times that connections must pass through a single individual to be connected, (i.e., which person is the most central to the network as a whole and likely to be the most influential with the most group knowledge). Higher scores describe organizations in whom many people play this central role in multiple small groups. |
| Number of Triads | Connections among three nodes |
| Number of Cliques | The number of sub-groups where the members are completely connected to each other. |
We used ORA's analysis capability to generate overall network and individual node (staff) metrics for each unit. Prior to beginning the study, we had decided to utilize only 15 of ORA's over 80 metrics since many of the metrics are very similar and therefore provide largely redundant information. Table II displays the metrics discussed in this paper and their definitions.
3. Results
Results will be reported by research question.
3.1 Can ORA's visualizations be used to identify patient care unit network communication patterns that affect patient safety and quality outcomes?
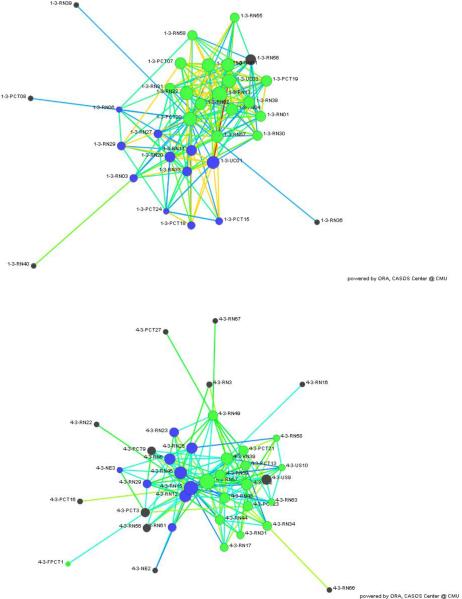
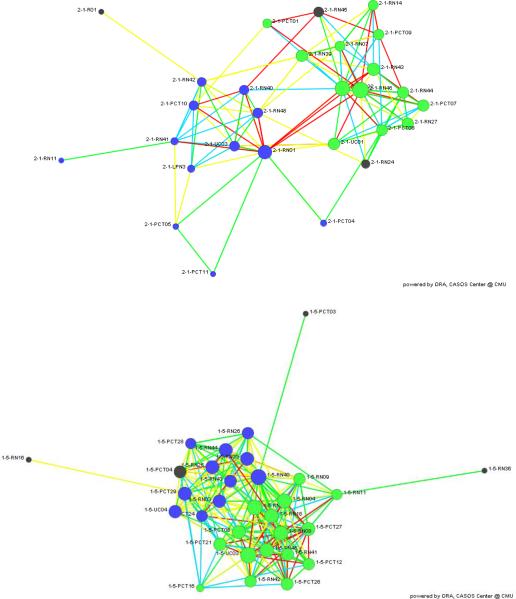
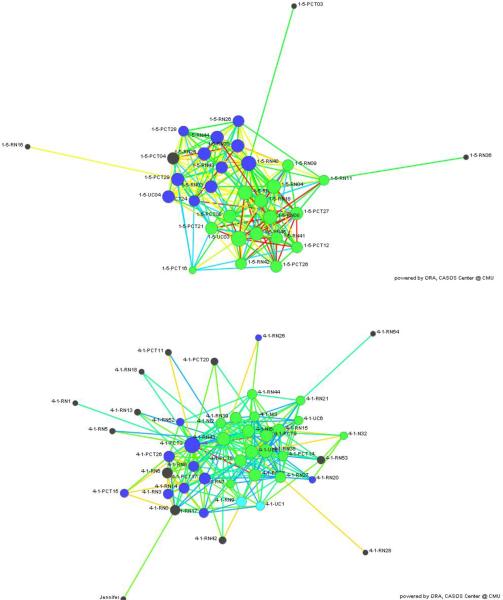
To answer this question, we compared the units with the highest and lowest: (a) Fall rates (7.52 and 1.66 falls per 1000 patient days, respectively); (b) ADE rates (13.5 and 1.7 ADEs per 1000 patient days, respectively; and (c) Patient Satisfaction with Caring scores (90% and 68%, respectively). The results are presented in Figures 1, 2, and 3. Node color indicates shift: green = day shift, blue = night shift, and black = unknown shift. Node size corresponds to Eigenvector Centrality. Link color corresponds to the frequency of communication: red = constantly, yellow = a lot, green = some; blue = rarely.
Figure 1.
ORA visualizations of the communication networks for the highest (top) and lowest (bottom) falls units).
Figure 2.
ORA visualizations of the communication networks for the highest (top) and lowest (bottom) ADE units).
Figure 3.
ORA visualizations of the communication networks for the highest (top) and lowest (bottom) Caring units. Note that the lowest ADE unit (Figure 2) was also the highest Caring Unit.
Inspection of Figure 1 shows substantial differences among the units. The high falls unit has more connections and more frequent communication among staff—especially on days (as indicated by the red and yellow links), but the shifts are quite well differentiated (more connections within a shift than across shifts). The high falls unit also has fewer pendants (single links that look like spikes coming out of the network). The low falls unit is less densely connected; and the frequency of communication among staff is lower (no yellow or red links indicating higher rates of communication).
Close inspection of Figure 2 (below) suggests that the high ADE unit (top) has several very influential staff members who are central to large portions of the network (that is, many communication paths run through these individuals). This observation is supported by the values of Network Centralization Betweeness (High ADE unit = .10; Low ADE unit = .04). These influential staff can facilitate quick communication in emergencies, but perhaps are not helpful for medication administration. In the low ADE unit, the communication network appears to be denser with more small groups; and ORA metrics confirm that observation (Density for the High ADE unit = .10 and for the Low ADE unit = .19; Clustering Coefficient for the High ADE unit = .51 and for the Low ADE Unit = .28).
Units with the highest and lowest Patients' Satisfaction with Caring are shown in Figure 3 (below). The unit with the fewest ADEs had the highest level of Satisfaction with Caring. Both networks appear quite dense, but the amount of communication among staff is less on the low Caring unit, as shown by link color (no red or yellow); and there are more triads and pendants in that network, also indicating fewer connections.
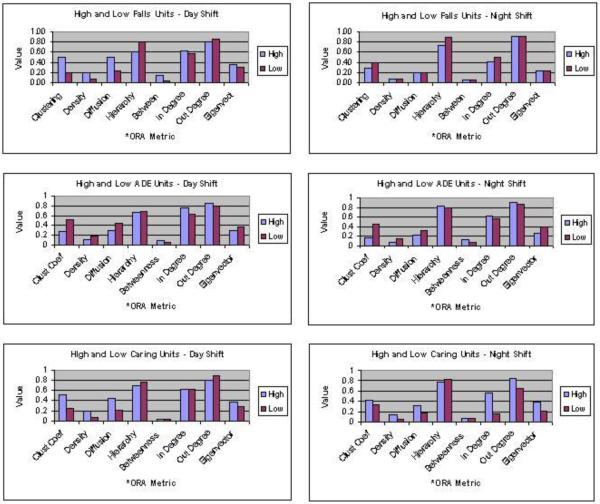
3. 2. Do unit network characteristics differ by shift?
Figure 4 depicts the differences between high and low Fall, ADE, and Caring units. The rank order of variables is very similar across shifts for ADEs, but less similar for Falls and Caring. Values for Clustering Coefficient, Density, and Diffusion are higher for the High Falls Unit on the Day Shift, but less than--or equal to--the Low Falls Unit on the Night Shift. For ADEs, values for Network Centralization In Degree (connections coming into individual staff nodes) are considerably lower on the Night Shift—especially for the High ADE unit. For Caring, there is a greater difference in Clustering Coefficient and Diffusion between High and Low Units on the Day Shift, but a greater difference in Eigenvector Centrality between High and Low Units on the Night Shift. More dramatic, perhaps, are the shift differences in Network Centralization In and Out Degree, which denotes much less communication to and from individuals on the Night Shift.
Figure 4.
ORA Metrics for High and Low Falls, ADEs, and Caring Units by Shift
3.3. What network characteristics measured by ORA metrics are related to specific safety and quality measures?
For this analysis, all seven units were used. Table III summarizes the statistically significant (p < .10) rank order (Spearman) correlations for the safety and quality outcomes. A significance level of .10 was adopted because of the low sample size.
Table III.
Correlations (Spearman Rho) between ORA metrics and patient outcomes (n = 7)
| Falls | Adverse Drug Events | Symptom Management Capacity | Symptom Management Difference | Complex Self Care | Satisfaction with Caring | Satisfaction with Individual Needs Being Met | |
|---|---|---|---|---|---|---|---|
| Clustering Coeffficent | 0.70 | 0.70 | 0.72 | ||||
| Density | 0.75 | 0.70 | 0.93** | ||||
| Diffusion | 0.75 | 0.71 | |||||
| Hierarchy | −0.74 | −0.78* | −0.69 | ||||
| Betweeness Centrality | 0.73 | ||||||
| Centrality In Degree | −0.86* | −0.68 | |||||
| Centrality out Degree | −0.79* | −0.96** | |||||
| Eigenvector Centrality | 0.69 | 0.93** | |||||
| Simmelian Ties | 0.69 | 0.92** | |||||
| Triads | −0.75 | 0.82* | |||||
| Cliques | −0.82* |
p < .05;
p < .01;
all other correlations shown = p < .10
3.1 Correlations with safety outcomes
We examined two patient safety outcomes, Falls and Adverse Drug Events (ADEs). As network Diffusion of information increased, so did Patient Falls. This is consistent with what was observed in the visualizations. By contrast, as Hierarchy (the amount of unidirectional communication without feedback loops) increased, Falls decreased. It is possible that preventing falls involves more 1:1 communication rather than group discussion. ADEs presented a very different picture. Only higher Betweeness Centrality (more individuals in the shortest communication paths, hence likely to be gatekeepers) was associated with more ADEs.
3.3.2 Correlations with Quality Measures
We examined three types of quality measures: symptom management, self care, and patient satisfaction. Higher Clustering Coefficients and higher Density were associated with more patients' improving at least 1 point in Symptom Management Capacity and Symptom Management Difference (see Table 1 for definitions) during their hospitalization. The positive impact of small group communication is emphasized by the positive correlations of Symptom Management Capacity with Simmelian Ties (strong ties within cliques) and of Symptom Management Difference with Eigenvector Centrality (persons connected to highly connected people). By contrast, the number of connections from individuals (nodes) to others was negatively related to Symptom Management Difference.
None of the ORA metrics was associated with improvement in Simple Self Care activities. Only the number of Cliques was (negatively) related to Complex Self Care improvement. That is, more patients improved 1 point or more on the Complex Self Care scale during their hospitalizations when there was less small group communication.
Of the three satisfaction measures examined, only General Satisfaction was not correlated with any ORA metric. The survey questions measuring this outcome addressed patients' assessment of their caregivers' competence and knowledge, as well as the patients' opinions about the appropriateness and helpfulness of services they received. Given the focus of the scale, perhaps the lack of correlation with communication network metrics should not be surprising. Patients' satisfaction that their Individual Needs had been met was positively associated with more communication by small, 3-person triads, but negatively associated with more one-way communication without feedback loops (Hierarchy) and more links (connections) into individual staff nodes.
More ORA variables were correlated with Satisfaction with Caring than with any other outcome measure. The scale that measures this outcome includes items such as “When you talked to the person (or nurse) with whom you worked most closely, how closely did he or she listen to you?” and “How clearly did the person (or nurse) with whom you worked most closely understand your problem and how you felt about it?” These questions explicitly measure communication, which may be why so many of the metrics were related. ORA metrics that were positively associated with increased satisfaction with Caring included Density, Diffusion and the clustering-related metrics (Clustering Coefficient, Simmelian Ties, and Eigenvector Centrality). Hierarchy, Centrality In Degree and Centrality Out Degree were negatively associated, with the latter having a very high correlation (rho = −.96).
4. Discussion
These results show that ORA's visualizations indeed can identify different communication patterns in nursing units. Although not evident from the 2-D figures shown here, the visualizations can be manipulated to focus in on particular sections of the network—or even a single node. This is very helpful with larger networks. Rolling the cursor over that node allows the user to open a window that shows all demographic characteristics of the node, as well as all the connections and the absolute value of targeted metrics.
There were clear differences in networks for day and night shifts—and not simply in density. There were also differences (as seen in the visualizations) in the connectivity across shifts. These differences may reflect distinctions in change of shift reporting or handoffs.
We used two week days to collect data to avoid trying to collect data on the weekend when fewer staff are scheduled. In the future, we plan to include weekend days as well to ensure a more comprehensive view of nursing unit communication patterns.
Specific network metrics were correlated with the outcome variables in our study. There was consistency in the direction of the correlation across metrics. However, two variables (Falls and ADEs) differ from the rest. With these two safety outcomes, higher scores are not better. Given this, some of the network characteristics that improved quality outcomes also increased the number of falls or ADEs (that is, they worsened safety outcomes).
Rush and colleagues found, through focus group discussions with nurses, that nurses used formal risk assessments on a regular (daily or per shift) basis.6 However the nurses in that study reported that the data collected via these tools was unreliable; i.e., falls occurred in patients that were deemed safe by the risk assessment tool. Nurses also used regular monitoring of patients at risk, as well as monitoring of the environment for potential safety threats. Nurses involved unlicensed assistive personnel in the monitoring activities (i.e., PCTs or patient sitters). The physical setting also played a role in nurses' ability to monitor patients effectively. Patients who were closer to the nursing station were easier to observe. Staffing issues also played a role; when staffing was less than optimal, monitoring was more difficult. Communication with both patients and families about fall risk—and activities that might precipitate falls was vital. However, when patients needed help quickly and nursing staff were not immediately available, the potential for falls increased.
Based on the results obtained by Rush and colleagues, [6] we might expect that falls would be fewer on units in which diffusion of information is higher and there is more non-hierarchical communication with feedback loops. However, our results did not support that conclusion. For the units in our study, more rapid diffusion of information across the network was associated with more patient falls; and a more hierarchical top-down communication structure was associated with fewer falls. Perhaps the difference in the two studies is related to the type of information that is being conveyed in each case; when staff are discussing information that improves the surveillance of patients at risk for falls, that kind of rapid diffusion could be extremely useful in preventing falls. On the other hand, if the information being discussed is related to other issues, it may not be helpful for preventing falls.
Still, the reason for more or less communication on the high and low falls unit cannot be fully determined. Given the small sample, other factors may have influenced the results. For example, falls and ADEs (particularly with injury) were not frequent occurrences and we measured the rate over a 3-month period, which may or may not have been typical for the unit. Certainly, units vary in the percentage of elderly patients. However, the differences in fall and ADE rates obtained across comparable types of units in the same hospital where the percentage of elderly was similar argues against that hypothesis. In future studies, a larger sample would allow us to explore more fully other explanations for the results.
ORA metric correlations with ADEs differed from those with falls. When more individuals were part of the shortest communication path, suggesting more well connected and highly influential staff members who function as information gatekeepers, ADEs increased. Medication administration differs from fall prevention in that it is a function of nurses, rather than of unlicensed assistive personnel. The communication process involved in medication administration involves several professions (medicine, pharmacy, and nursing), as well as direct communication with patients. Frequently the best connected individuals in our study were not nurses, but unlicensed assistive personnel (unit clerks or PCTs). It may be that these multiple gatekeepers are in some way disruptive--or even interruptive. Medication administration has been shown to be safer when interruptions and disruptions are minimized. [23, 24] Further research will be needed to test this hypothesis.
We measured two different aspects of symptom management. The first, Symptom Management Difference, measured the percentage of patients on each unit who met a goal of a 1-point improvement in their ability to manage their own symptoms from admission to discharge. The second, Symptom Management Capacity, measured the percentage of patients on each unit who met a goal of a 1-point improvement in a ratio of symptom management capacity to symptom distress during their hospitalization. Both variables were positively associated with network Density (more communication among staff) and with more small groups (Cliques), suggesting that more interaction—especially in the form of small group communication can facilitate this aspect of patient care. By contrast, the number of connections from individuals (network nodes) to others was negatively related to Symptom Management Difference. This may reflect the presence of more novices who need to ask someone else for advice.
Patients' Satisfaction that their Individual Needs had been met was positively associated with more communication by small, 3-person triads, but negatively associated with more oneway communication without feedback loops (Hierarchy) and more links (connections) into individual staff nodes. This may represent situations when there is a lot of top-down communication coming to staff. A preponderance of this type of directive communication appeared to interfere with care, perhaps due to its interruptive nature.
Increased Patient Satisfaction with Caring was associated with increased Density, Diffusion and the clustering metrics, but negatively with Hierarchy, Centrality In Degree and Centrality Out Degree. It appears to be important that people are talking in small groups; those small supportive groups then facilitate patients' perceptions of caring staff. However, one-way, top-down communication without feedback loops (Hierarchy and Centrality In Degree) may inhibit caring behaviors. Further, care may be impeded when there are many novice staff who must ask a lot of questions of more experienced staff as they provide care (Centrality Out Degree).
More communication among unit staff was not always associated with better patient outcomes. Denser communication networks with more clustering were associated with better quality outcomes, but more rapid diffusion of information across the network was associated with more patient falls. Perhaps if there is too much small group interaction, the unit begins to focus more on maintaining the group process than on patient care
More Cliques (small group communication) led to greater improvement in patients' self-estimated abilities to carry out complex self care activities, such as deciding how to adapt their care regimen to changes in symptoms. However, more individual gatekeepers (higher Betweenness Centrality) were associated with more medication errors. Medication administration involves a different team (Physician, Pharmacist, Nurse, Patient) that is not well modeled in the small groups in this network consisting solely of nursing staff. However, small group communication among nursing staff maybe more interruptive than helpful for medication administration; and interruptions have been shown to be related to medication errors. [23, 24]
We limited our sample to nursing staff for several reasons. First, our interest lies in identifying factors that nurse managers have more control over, and therefore can potentially change. Therefore, our focus for this study was on the nursing unit staff. Second, in a previous study, we found that interprofessional teams are very difficult to identify on medical-surgical units. In that study, nurse managers were unable to identify who would constitute the pharmacy, physician, or dietary members of a team because they were not permanently assigned to the unit. There may be other units (for example, Emergency Departments or Rehabilitation units) where this situation differs, but including other professionals in this type of study must remain for future work. We did explore the contacts that nursing staff had with other professionals—but only from the nursing staff's perspective because of the difficulty in identifying the other players. Because the other professionals did not complete questionnaires, those data were not included in the analysis. To include physicians and other professionals is likely to require a more patient centric view of communication that focuses on the team involved in a particular patient's care, e.g. [4].
Generalization of the results of this exploratory study is limited by sample size and the homogeneity of the sample, which was comprised solely of medical/surgical units in Magnet hospitals in the Southwest. Therefore, this study should be replicated and extended to a larger, more diverse sample of patient care units. Within this sample, the study results provide a fairly clear picture of how unit staff communication interacts with patient outcomes. Beyond this sample, the results provide testable hypotheses for future research.
5. Conclusion
The results of the study clearly demonstrate the utility of ORA for healthcare research. Using ORA, we were able to examine the impact of unit level communication on patient safety and quality outcomes. The ORA visualizations were invaluable in helping us understand each network and clarify differences within and across networks. The metrics provided by ORA provided quantifiable measures that could be correlated with patient outcome data in ways that previously were not possible. We hope that these results will encourage other health system researchers to use dynamic network analysis tools for these kinds of complex systems analyses.
Summary Table.
What is known?
Communication issues contribute to errors in health care.
Doctor-nurse and person-to-person communication are known to contribute to errors.
Social network analysis can be used to study communication within small groups, but cannot be used for larger groups or organizations.
ORA is a tool that can accommodate the social network analysis large organizations, but has only begun to be used in healthcare.
What this manuscript contributes?
The utility of ORA for analyzing the communication patterns of nursing units is demonstrated.
Specific nursing unit communication patterns are identified using ORA's visualizer that correspond to high or low levels of patient safety and quality outcomes.
Specific ORA metrics for nursing networks are identified that were correlated with patient quality and safety outcomes.
Acknowledgements
This research was funded by the National Library of Medicine (NIH) 1R01LM009516-01A1. Portions of this manuscript were presented at the Western Institute of Nursing Research Conference in Phoenix, AZ, April 20, 2010, the ISSH Conference in New York City on July 14, 2010, the American Medical Informatics Association Fall Symposium in Washington DC on November 10, 2010, and the 44th Annual Meeting & Exposition of the American Organization of Nurse Executives in San Diego on April 15, 2011.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest Dr. Carley's company, Carley Technologies Inc. (CarleyTech) has been marketing a commercial version of ORA (ORATech) that is customizable to specific environments through its Netanomics Division since March 21, 2010, so we herein disclose a financial conflict of interest since Dr. Carley is the CEO of CarleyTech. A free version of ORA, which is what we use for our research, is still available for academic use at www.casos.cs.cmu.edu/projects/ORA.
References
- [1].Chaboyer W, McMurray A, Wallis M. Bedside nursing handover: A case study. Internat. J. Nurs. Pract. 2010;16:27–34. doi: 10.1111/j.1440-172X.2009.01809.x. [DOI] [PubMed] [Google Scholar]
- [2].Kalisch BJ, Landstrom G, illiams RA. Missed nursing care: Errors of omission. Nurs. Outlook. 2009;57:3–9. doi: 10.1016/j.outlook.2008.05.007. [DOI] [PubMed] [Google Scholar]
- [3].Pronovost P, Berenholtz S, Dorman T, Lipsett PA, Simmonds T, Haraden C. Improving communication in the ICU using daily goals. J. Crit. Care. 2003;18:71–76. doi: 10.1053/jcrc.2003.50008. [DOI] [PubMed] [Google Scholar]
- [4].Benham-Hutchins MM, Effken JA. Multi-professional patterns and methods of communication during patient handoffs. Internat. J. Med Informat. 2010;79:252–267. doi: 10.1016/j.ijmedinf.2009.12.005. [DOI] [PubMed] [Google Scholar]
- [5].Dykes PD, Carroll DL, urley AC. Why do patients in acute care hospitals fall? Can falls be prevented? J. Nurs Admin. 2009;39:299–304. doi: 10.1097/NNA.0b013e3181a7788a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Rush KI, Robey-Williams C, Patton LM, Chamberlain D, Bendyk H, Sparks T. Patient falls: Acute care nurses' experiences. J. Clin. Nurs. 2008;18:357–365. doi: 10.1111/j.1365-2702.2007.02260.x. [DOI] [PubMed] [Google Scholar]
- [7].McGilton K, Irwin-Robinson H, Boscart V, Spanjevic L. Communication enhancement: Nurse and patient satisfaction outcomes in a complex continuing care facility. J. Adv. Nurs. 2005;54:35–44. doi: 10.1111/j.1365-2648.2006.03787.x. [DOI] [PubMed] [Google Scholar]
- [8].Manojlovich M, DeCicco B. Healthy work environments, nurse-physician communication, and patients' outcomes. Am. J. Crit. Care. 2007;16:536–543. [PubMed] [Google Scholar]
- [9].Stahl K, Palileo BA, Schulman CI, Wilson K, Augenstein J, Kiffin C, McKenney M. Enhancing patient safety in the trauma/surgical intensive care unit. J. Trauma Inj. Infect. and Crit. Care. 2009;67:430–435. doi: 10.1097/TA.0b013e3181acbe75. [DOI] [PubMed] [Google Scholar]
- [10].Awad SS, Fagan SP, Bellows C, Albo D, Green-Rashad B, De la Garza M, Berger DH. Bridging the communication gap in the operating room with medical team raining. Am. J. Surg. 2005;190:770–774. doi: 10.1016/j.amjsurg.2005.07.018. [DOI] [PubMed] [Google Scholar]
- [11].Anderson JG. Evaluation in health informatics: Social Network Analysis. In: Anderson JG, Aydin CE, editors. Evaluating the Organizational Impact of Healthcare Information Systems. 2nd ed. Springer; New York, NY: 2005. pp. 189–220. [Google Scholar]
- [12].Burt RS. Structural holes: The Social Structure of Competition. Harvard University Press; Cambridge, MA: 1992. [Google Scholar]
- [13].Ibarra H, H., Andrews SB. Power, social influence, and sense making: Effects of network centrality and proximity on employee perceptions. Admin. Sci. Quart. 1993;38:277–303. [Google Scholar]
- [14].Feeley TH, Barnett GA. Predicting employee turnover from communication networks. Hum. Commun. Res. 1996;23:370–387. [Google Scholar]
- [15].Burkhardt ME. Social interaction effects following a technological change: a longitudinal investigation. Acad. Manage. J. 1994;37:869–898. [Google Scholar]
- [16].Carley KM, Kamneva NY. A Network Optimization Approach for Improving Organizational Design. Carnegie Mellon University, Center for Computational Analysis of Social and Organizational Systems; Pittsburgh, PA: 2004. [Google Scholar]
- [17].Krackhardt D, Carley KM. A PCANS model of structure in organizations. International Symposium on Command and Control Research and Technology; Monterey, CA. 1998. [Google Scholar]
- [18].Carley KM. Dynamic network analysis. Dynamic Social Network Modeling and Analysis: Workshop Summary and Papers; Washington, DC. 2002. [Google Scholar]
- [19].Merrill-Matzner JC. A Network Analysis of Information Use in a Public Health Organization, Unpublished dissertation. Columbia University; New York, NY: 2006. [Google Scholar]
- [20].Meek P, Verran JA, Badger T, Effken J. Emmons Award. College of Nursing, The University of Arizona; 2001. Initial Testing of Generic Nurse Sensitive Outcomes. [Google Scholar]
- [21].Lorig K, Stewart A, Ritter P, Gonzalez V, Laurent D, Lynch J. Outcome Measures for Health Education and other Health Care Interventions. Sage Publishing; Thousand Oaks, CA: 1996. [Google Scholar]
- [22].Krackhardt D. Simmelian tie: Super strong and sticky. In: Kramer RM, Neale M, editors. Power and Influence in Organizations. Sage; Thousand Oaks, CA: 1998. pp. 21–38. [Google Scholar]
- [23].Trbovich P, Prakash V, Stewart J, Trip K, Savage P. Interruptions during the delivery of high-risk medications. J. Nurs. Admin. 2010;40:211–218. doi: 10.1097/NNA.0b013e3181da4047. [DOI] [PubMed] [Google Scholar]
- [24].Westbrook JI, Woods A, Rob MI, Dunsmuir WT, Day RO. Association of interruptions with an increased risk and severity of medication administration errors. Arch. Int. Med. 2010;170:683–690. doi: 10.1001/archinternmed.2010.65. [DOI] [PubMed] [Google Scholar]