Abstract
Background
To track mortality and rehospitalizations over 5 years post-stroke in a stroke cohort (SC) and compare long-term risks of complications to a matched non-stroke cohort (NSC).
Methods
A cohort design with a matched NSC comparison was used. The SC constituted a validated database of acute ischemic stroke patients, 65 years or older, hospitalized across 19 Minnesota hospitals in the year 2000. The NSC was constructed from the year 2000 General Medicare Population by matching SC members on age, race and sex. Both cohorts were tracked across 5 years of Medicare claims data to identify dates and causes of rehospitalization and death dates. Kaplan-Meier survival curves estimated cumulative incidence rates. Cox models calculated adjusted hazard ratios (HR).
Results
Event rates and adjusted HR were: Mortality: 1 year SC=24%, NSC=4%; 5 years SC=49%, NSC= 24%; HR: 4.4 (95% confidence intervals (CI) 3.6-5.5). Overall rehospitalization rates: 1 year SC=49%, NSC=20%; 5 years SC=83%; NSC=63%; HR: 2.6 (95% CI 2.2-3.0). Cause specific 5-year rehospitalization rates were significantly higher in SC versus NSC for recurrent ischemic stroke, heart failure, cardiac events, any vascular events, pneumonia, and hip fractures. The excess risk of mortality and rehospitalizations in the SC persisted beyond the initial aftermath of the acute stroke (i.e. beyond 30 days post-stroke) and persisted even after 1 year post-stroke. Average acute care Medicare charges in SC more than doubled those in NSC.
Conclusions
The high rates of acute care post-stroke readmissions indicate a need for trials to prevent long-term complications in stroke survivors.
Keywords: Stroke Outcomes, Rehospitalization after Stroke, Stroke Mortality
INTRODUCTION
The estimated 2010 direct and indirect cost of stroke in the United States is $73.7 billion. 1 The direct medical costs of stroke include acute hospitalization and rehabilitation costs of the index event and subsequent outpatient care and also the recurrent acute care costs due to rehospitalizations from stroke related complications. 1-4 While there are established and accruing data on the post-stroke survival and vascular events after stroke, 3-9 information on other post-stroke complications such as hip fractures, pulmonary embolism and gastrointestinal hemorrhages over the long-term are sparse. 10 The goals of the work described herein are to track events over a 5-year period in a cohort of patients hospitalized with acute ischemic stroke, ascertain short-term versus long-term risks of various complications leading to subsequent acute hospitalizations and compare event rates of the stroke cohort to a matched non-stroke cohort.
METHODS
Overall Study Design
A cohort study design with a stroke cohort and a matched non-stroke comparison cohort was used. Both cohorts were tracked for mortality and rehospitalization outcomes over a 5-year period by linkage with Medicare claims databases. Medicare is a health insurance system for people in the United States 65 years and older and also those with certain disabilities. Approximately 98% of Americans 65 years and older are Medicare beneficiaries. The Centers for Medicare and Medicaid Services compiles data on medical care received and billed for by healthcare providers. A description of Medicare datasets can be found at http://www.resdac.umn.edu/Medicare/Data_File_Descriptions_RIF.asp, accessed August 10, 2010.)
IRB approval
This study was approved as secondary data analysis by the institutional review boards (IRB) of the University of Minnesota. Individual patients were not contacted.
Study Patients
Stroke cohort
The Project for Improvement of Stroke Care Management in Minnesota (PRISMM) was a clinical trial to improve stroke care quality in 19 Minnesota hospitals. The PRISMM patient population is described in Lakshminarayan et al. 11 We used the baseline pre-intervention data compiled by PRISMM for the current Medicare Linkage Study. Subjects included in the PRISMM database were hospitalized patients aged 30-84 years, discharged with ICD-9 (International Classification of Diseases, 9th Revision) codes 434.x and 436.x and confirmed as having an acute ischemic stroke by physician review. PRISMM subjects included all ischemic stroke patients discharged during July-December 2000 from the 19 participating hospitals. For this Medicare Linkage Study we restricted PRISMM patients to those age 65 years or older and Minnesota residents at the time of the index stroke event (83% of all ischemic strokes entered into PRISMM). These Medicare eligible patients from the PRISMM database were identified in the Year 2000 Medicare Denominator file through their Medicare Beneficiary ID. The Medicare Denominator file contains demographic and enrollment information about each beneficiary enrolled in Medicare during a calendar year. Patients from the PRISMM database who were identified in the Medicare Denominator file formed the stroke cohort for the Medicare Linkage Study.
Non-stroke cohort
A sampling frame was constructed using the Minnesota state segment of the Year 2000 Medicare Denominator file. A 5:1 sampling ratio was used with 5 non-stroke members for each member of the stroke cohort. Matching variables included age (within +/− 2 years), sex and race. Each sampled member of the non-stroke cohort had to be alive up until the index stroke hospitalization discharge date of their matched stroke cohort member.
We ensured the non-stroke status of non-stroke cohort members by checking each sampled non-stroke member against the Year 2000 Medicare Provider Analysis and Review (MedPAR) file to ensure that they did not have an acute stroke hospitalization (ICD-9 430-437) up until and including the discharge date of the index hospitalization of their matched stroke cohort member. The MedPAR file contains inpatient hospital “stay” records summarizing services rendered to a beneficiary during hospitalization. Each stay record has up to 10 diagnosis codes which are the ICD-9 codes identifying the primary disease condition or co-existing conditions present in the medical records.
Outcome Ascertainment
Death
The occurrence of death and the death date for both cohorts was identified from the Denominator file and confirmed in the MedPAR file. Death during the index hospitalization was also confirmed from the PRISMM database. The unique Medicare Beneficiary ID was used to track individual stroke and non-stroke cohort members across the years through Denominator and MedPAR files from 2000-2005 to obtain 5-year mortality.
Rehospitalization
Acute care rehospitalization events and their dates were identified from the years 2000-2005 MedPAR files. Cohort members who were part of a managed care organization (Medicare Advantage) in the year 2000 were not tracked for rehospitalizations events since their claims data would not be represented in MedPAR. (Unlike rehospitalizations claims, Medicare versus managed care enrollment did not affect mortality since death dates were recorded in the Denominator file regardless of entitlement status.) Rehospitalization events were ascertained using acute care hospitalizations. Rehabilitation and nursing home transfers were excluded. Outcome events were acute rehospitalizations for recurrent ischemic stroke, intracerebral hemorrhage, cardiac events including heart failure, myocardial infarction (MI) and arrhythmias, pneumonia, pulmonary embolism, gastrointestinal (GI) hemorrhages, urinary tract infections (UTI), and hip fractures. Events were identified using ICD-9 codes as listed in e-Table 1. Only the primary diagnosis code was used to enhance specificity.
Time to event and censoring
Time to event in person-years for mortality was calculated from discharge date of the index hospitalization (day 0) to event occurrence. The day 0 for a member of the stroke cohort was also assigned as day 0 of their matched non-stroke cohort members. Time to event for rehospitalization outcomes was calculated from day 1. Only the first event in each outcome category was counted for each person. Cohort members were censored when they died, went to managed care (Medicare Advantage), left Medicare enrollment, and when the event of interest occurred. Patients who died during the index stroke hospitalization and those who were in managed care at baseline did not contribute person-years to rehospitalization rates. There were no significant differences in the mortality outcomes of the baseline managed and non-managed care enrollees.
Comorbidity assessment
Pre-existing comorbidity conditions which could potentially influence outcomes were identified using one Part A institutional/inpatient claim or two outpatient/Part B physician/supplier claims from a 6 month period prior to the index hospitalization. The following ICD-9 codes were used: diabetes mellitus (250, 357.2, 362, 366.41; hypertension 404-405, 362.11, 437.2; myocardial infarction (MI) 410-411; COPD (chronic obstructive pulmonary disease) 490-496; dyslipidemia 272; heart failure 428; peptic ulcer disease 531-535.
Socioeconomic status
Socioeconomic status (SES) is a strong determinant of health outcomes. We used the median income of cohort members’ zip code (obtained from census record) as a surrogate variable indicating individual SES. 12-13
Charges to and payments by Medicare for hospital admissions
We calculated the average Medicare covered charges as well as the payments made by Medicare per person year of follow-up time using all acute care admissions (not just the first event) for each cohort. Member-time was censored on death, when members left Medicare enrollment and when they went to managed care.
Statistical Analysis
Baseline characteristics of stroke cohort and non-stroke cohorts when not part of the matching criteria were compared using the chi-square test for categorical variables and the t-test or Wilcoxon rank sum test for continuous variables.
Kaplan-Meier (KM) survival curves (PROC LIFETEST, SAS) were used to obtain cumulative incidence (%) with 95% confidence limits at 7 days, 30 days, 1-year and 5-years for the outcome events described earlier in the stroke and non-stroke cohorts. KM estimates for rehospitalization outcomes were compared to cumulative incidence estimates from survival models that accounted for the competing risk of mortality (PROC LIFETEST, Nelson Aalen estimates) to evaluate for possible bias.
Cox-proportional hazards regression models were used to compare adjusted event rates in the two cohorts and calculate hazard ratios (HR) with 95% confidence intervals (CI). The proportional-hazards assumption was tested for each outcome and if this assumption was violated we used the extended Cox regression modeling framework for that outcome.14 All Cox models were adjusted for relevant co-morbid conditions and SES. Cox models for mortality were also adjusted for MA status. Since age, sex and race were matching variables they were not used in further model adjustment.
We calculated the above described Cox model hazard ratios comparing the stroke and non-stroke cohorts with three starting points for event observation. The first compared 5-year event rates between the two cohorts starting on day 0 for mortality and day 1 for rehospitalization outcomes. In the second, events were ascertained starting on day 31. The risk set for this model was all members alive on day 31. Events between day 1 and day 30 were ignored. The outcome clock for everyone in the risk set was restarted and the first event in each outcome category (regardless of prior events) starting day 31 was counted. Early events up could presumably be due to the index hospitalization itself and could suggest opportunities to improve acute stroke care. In the third model, we started event observation at day 366 (1 year). Again, only the first event in each category starting day 366 was counted. We examined outcome ascertainment starting on day 366 to examine if the risk of various outcomes in the stroke cohort returned to non-stroke levels after 1 year.
RESULTS
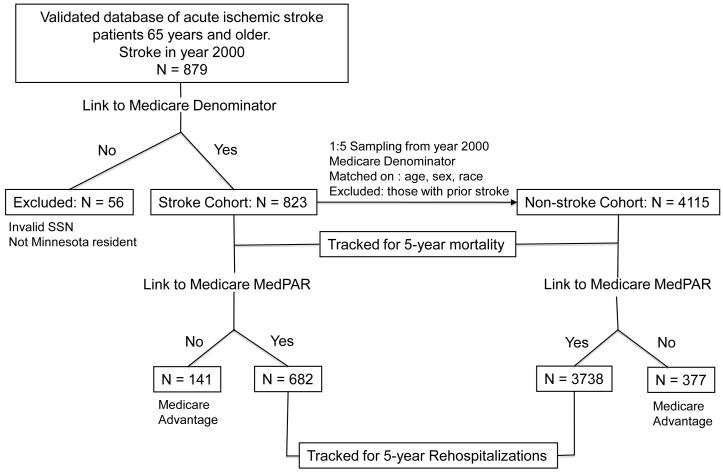
Figure 1 shows the study design.
Figure1.
Study Design and Formation of the Stroke and Non-stroke Cohorts. SSN = Social Security Number. MedPAR = Medicare Provider Analysis and Review file (claims data).
Linkage
Of 879 acute ischemic stroke patients 65 years and older in the baseline PRISMM database, a total of 823 patients were linked to the year 2000 Minnesota state segment of the Medicare Denominator file for a linkage rate of 94%. Non-linkage was commonly due to lack of a valid social security number (26 patients, 3%) or non-Minnesota residence (21 patients, 2.4%).
These 823 patients formed the stroke cohort. The non-stroke cohort, formed by the 5:1 sampling described above, had 4115 patients. These two cohorts formed the denominator for tracking 5-year mortality.
Of 823 patients in the stroke cohort, 141 (17%) had Medicare Advantage at baseline. The remaining 682 stroke cohort members were linked to MedPAR and tracked for 5-year rehospitalization events. Of the 4115 non-stroke cohort members, 377 (9%) had Medicare Advantage at baseline. The remaining 3738 non-stroke cohort members were linked to MedPAR and tracked for 5-year rehospitalization events.
Table 1 shows comparisons of baseline (pre-index date) co-morbid characteristics. These comparisons show significantly higher rates of vascular risk factors in stroke cohort members versus the non-stroke cohort members including hypertension 65% versus 19%; diabetes mellitus 26% versus 9%; dyslipidemia 24% versus 11%; MI 5% versus 1%; HF 9% versus 4%. COPD rates were also different: 14% in the stroke cohort versus 4% in the non-stroke cohort. Rates of GI ulcers were not significantly different. The stroke cohort lived in higher median income neighborhoods compared to the non-stroke cohort.
Table 1.
Baseline characteristics of the Medicare linked stroke cohort and the matching non-stroke cohort.
| Variable | Stroke Cohort N=823 |
Non-stroke Cohort N=4115 |
p-value |
|---|---|---|---|
| Mean age, years (SD) | 76 (5.5) | 76 (5.5) | Matching variable |
| Female sex, n (%) | 426 (51.8) | 2130 (51.8) | Matching variable |
| Race | Matching variable |
||
| White, n (%) | 786 (95.5) | 3930 (95.5) | |
| Black, n (%) | 21 (2.6) | 105 (2.6) | |
| Other, % | 16 (1.9) | 80 (1.9) | |
| Median Income in zip | $49,942 | $42,407 | <0.0001 |
| code of residence (range) | ($15575-$95372) | ($7188-$95372) | |
| Comorbidity, n (%) | |||
| Hypertension | 537 (65.3) | 768 (18.7) | <0.0001 |
| Diabetes Mellitus | 217 (26.4) | 356 (8.7) | <0.0001 |
| Dyslipidemia | 201 (24.4) | 444 (10.8) | <0.0001 |
| COPD | 114 (13.9) | 180 (4.4) | <0.0001 |
| Gastrointestinal Ulcer | 7 (0.9) | 15 (0.4) | 0.06 |
| Myocardial Infarction | 40 (4.9) | 58 (1.4) | <0.0001 |
| Heart Failure | 71 (8.6) | 164 (4.0) | <0.0001 |
COPD = Chronic Obstructive Pulmonary Disease.
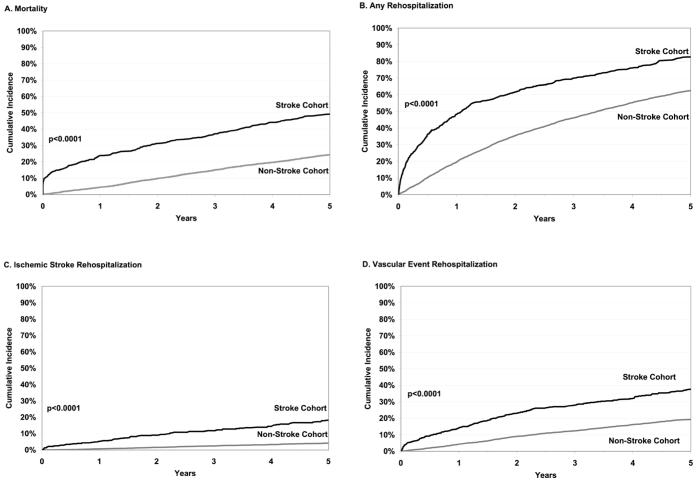
Figure 2 and Table 2 and e-Table 1 show comparative outcomes in the stroke and non-stroke cohorts. Table 3 shows hazard ratios and 95% confidence intervals from the Cox models comparing adjusted event rates in the 2 cohorts. These are discussed below.
Figure2.
Cumulative Incidence of Outcome Events in Stroke and Non-Stroke Cohorts. Panel A shows mortality, panel B shows any rehospitalization, panel C shows ischemic stroke rehospitalization and panel D shows rehospitalization for any vascular event.
Table 2.
Cumulative incidence estimates of outcome events at 30 days, 1 year and 5 years in stroke and non-stroke cohorts.
| Outcome (ICD-9) | Cumulative Incidence Rates (%) | P-value | |||
|---|---|---|---|---|---|
| 30 days | 1 year | 5 years | |||
| Death | Stroke | 11.1 | 23.7 | 49.1 | < 0.0001 |
| Non-stroke | 0.3 | 4.4 | 24.3 | ||
| Any rehospitalization | Stroke | 13.9 | 48.7 | 82.9 | < 0.0001 |
| Non-stroke | 1.5 | 20.0 | 62.6 | ||
| Specific rehospitalizations | |||||
| Recurrent ischemic | Stroke | 1.6 | 5.1 | 18.0 | < 0.0001 |
| stroke (434, 436) | Non-stroke | 0.03 | 0.7 | 4.1 | |
| ICH | Stroke | 0.2 | 0.7 | 2.7 | 0.0002 |
| (430, 431, 432) | Non-stroke | - | 0.1 | 1.0 | |
| Myocardial Infarction (MI) | Stroke | 0.6 | 2.1 | 5.7 | 0.78 |
| (410, 411) | Non-stroke | 0.05 | 1.2 | 6.1 | |
| Heart Failure (HF) | Stroke | 0.2 | 3.9 | 14.8 | < 0.0001 |
| (428) | Non-stroke | 0.03 | 1.3 | 6.5 | |
| Dysrhythmias | Stroke | 1.6 | 3.6 | 8.0 | 0.01 |
| (427) | Non-stroke | 0.2 | 1.4 | 6.0 | |
| Any cardiac | Stroke | 2.4 | 8.6 | 23.1 | < 0.0001 |
| (MI, HF, dysrhythmias) | Non-stroke | 0.2 | 3.5 | 15.7 | |
| Any vascular | Stroke | 4.2 | 13.8 | 37.8 | < 0.0001 |
| (cardiac or stroke) | Non-Stroke | 0.3 | 4.3 | 19.2 | |
| Aspiration pneumonia | Stroke | 0.3 | 1.2 | 5.0 | < 0.0001 |
| (507.00) | Non-stroke | 0.03 | 0.1 | 1.5 | |
| Any pneumonia | Stroke | 1.0 | 6.5 | 19.5 | < 0.0001 |
| (507.00,480-487) | Non-stroke | 0.2 | 1.6 | 9.6 | |
| GI hemorrhage | Stroke | 0.2 | 0.5 | 5.2 | < 0.0001 |
| (578) | Non-stroke | 0.05 | 0.3 | 1.4 | |
| Pulmonary embolism | Stroke | - | 0.5 | 1.0 | 0.94 |
| (415.1) | Non-stroke | 0.05 | 0.2 | 1.0 | |
| Hip fractures | Stroke | 0.5 | 3.3 | 9.5 | < 0.0001 |
| (820, 821) | Non-stroke | 0.03 | 0.6 | 4.5 | |
| Urinary Tract Infection | Stroke | 0.3 | 1.0 | 4.3 | 0.01 |
| (599.0) | Non-stroke | 0.05 | 0.4 | 2.3 | |
Starting N for death: stroke cohort =823; non-stroke cohort =4115; Starting N for rehospitalization: stroke cohort = 682; non-stroke cohort = 3738. ICD-9 = International Classification of Diseases, 9th Revision. ICH = Intracerebral hemorrhage. GI = Gastrointestinal. P-values are from the unadjusted comparisons between stroke and non-stroke cohorts using Log-rank test. Confidence interval estimates for all event rates and 7-day outcomes are available in e-Table 1.
Table 3.
Hazard ratios (HR) and 95% confidence limits (CI) from adjusted Cox models comparing outcomes in the stroke versus non-stroke cohorts.
| Outcome | Outcomes from day 0 / day 1 |
Outcomes from day 31 |
Outcomes from day 366 |
|||
|---|---|---|---|---|---|---|
| HR (95% CI) |
p-value | HR (95% CI) |
p-value | HR (95% CI) |
p-value | |
| Death | 4.4 (3.6-5.5) |
<0.0001 | 2.5 (2.0-3.2) |
<0.0001 | 1.4 (1.2-1.7) |
<0.0001 |
| Any rehospitalization |
2.6 (2.2-3.1) |
<0.0001 | 2.0 (1.7-2.3) |
<0.0001 | 1.2 (1.1-1.4) |
0.0015 |
| Specific Rehospitalizations | ||||||
| Recurrent ischemic stroke |
5.8 (3.4-9.9) |
<0.0001 | 3.6 (2.5-5.1) |
<0.0001 | 3.3 (2.2-4.9) |
<0.0001 |
| Intracerebral hemorrhage |
2.3 (1.0-5.3) |
0.04 | 2.2 (0.9-5.1) |
0.07 | 2.2 (0.8-5.9) |
0.10 |
| Myocardial Infarction (MI) |
0.8 (0.5-1.2) |
0.25 | 0.7 (0.4-1.1) |
0.15 | 0.6 (0.3-1.0) |
0.05 |
| Heart Failure (HF) |
1.9 (1.4-2.6) |
0.0001 | 1.8 (1.3-2.5) |
0.0002 | 1.8 (1.3-2.7) |
0.001 |
| Dysrhythmias | 3.5 (2.0-6.3) |
<0.0001 | 2.3 (1.2-4.4) |
0.01 | 1.1 (0.7-1.7) |
0.79 |
| Any cardiac (MI, HF, Dysrhythmias) |
2.2 (1.5-3.1) |
<0.0001 | 1.6 (1.1-2.4) |
0.01 | 1.1 (0.8-1.5) |
0.52 |
| Any vascular (cardiac or stroke) |
2.8 (2.1-3.7) |
<0.0001 | 1.8 (1.4-2.1) |
<0.0001 | 1.5 (1.2-1.9) |
0.0002 |
| Aspiration pneumonia |
3.6 (2.1-6.2) |
<0.0001 | 3.5 (2.0-6.1) |
<0.0001 | 3.0 (1.6-5.7) |
0.0005 |
| Any pneumonia | 2.0 (1.5-2.5) |
<0.0001 | 1.9 (1.5-2.5) |
<0.0001 | 1.6 (1.2-2.2) |
0.0015 |
| Gastrointestinal hemorrhage |
3.7 (2.1-6.4) |
<0.0001 | 3.6 (2.1-6.4) |
<0.0001 | 4.3 (2.4-7.7) |
<0.0001 |
| Pulmonary embolism |
1.0 (0.4-3.0) |
0.95 | 1.1 (0.4-3.1) |
0.91 | 0.5 (0.1-2.3) |
0.36 |
| Hip fractures | 3.9 (2.1-7.3) |
<0.0001 | 2.1 (1.5-3.1) |
<0.0001 | 1.5 (0.9-2.3) |
0.09 |
| Urinary tract infections |
1.9 (1.1-3.2) |
0.02 | 1.7 (1.0-3.0) |
0.06 | 1.5 (0.8-2.9) |
0.20 |
Adjusted for comorbid conditions and SES. We present HR for events starting day 0/1 post-discharge for mortality/rehospitalization as well as HR for events starting from day 31 to eliminate the effects of the acute hospitalization in the stroke cohort and HR for events starting 1 year post-stroke to examine late effects of the disease. Those in or entering Medicare Advantage were censored in analyses of hospital readmissions (but not for mortality outcomes). Censored at baseline, 141 (of 823) of the stroke cohort and 377 (of 4115) non-stroke-cohort members were enrolled in Medicare Advantage. Subsequently, over 5 years, 38 additional stroke cohort members and 256 non-stroke cohort members entered Medicare Advantage and were censored at the date of entry into Medicare Advantage.
Mortality
In the stroke cohort, 24% of the patients were dead at 1 year and 49% were dead at 5 years. In the non-stroke cohort, 4% were dead at 1 year and 24% were dead at 5 years. These proportions were significantly different from each other. The adjusted HR for mortality from the Cox model when events were counted from day 0 was 4.4 (95% CI 3.6-5.5). When events were counted from day 31 the HR was still significant though lower at 2.5 (95% CI 2.0-3.2) and when events were counted from day 366, the HR was further attenuated but still significant at 1.4 (95% CI 1.2-1.7).
Overall Rehospitalization
In the stroke cohort, 14% were rehospitalized within 30 days, 49% were rehospitalized at least once at 1 year and 83% at 5 years. In the non-stroke cohort, 2% were hospitalized at 30 days, 20% at 1 year and 63% at 5 years. The adjusted HR was 2.6 (95% CI 2.2-3.0) when hospitalization events were counted from day 1, still significant at 2.0 (95% CI 1.7-2.3) when hospitalization events were counted starting at day 31 and attenuated but still significant at 1.2 (95% CI 1.1-1.4) when events were counted from day 366.
Hospitalization for Specific Conditions
Salient findings include significantly higher 5-year hospitalization rates in the stroke cohort compared to the non-stroke cohort for the following conditions: ischemic stroke (18% versus 4%), heart failure (15% versus 7%), cardiac events (23% versus 15%), any vascular event (38% versus 19%), pneumonia (20% versus 10%) and hip fractures (10% versus 5%), Table 2.
Setting aside composite vascular events, recurrent ischemic stroke (2%), dysrhythmias (2%) and pneumonia (1%) were the most common causes of hospital admission in the stroke cohort in the early, 30-day, post-discharge period. Notably, 70% of these early dysrhythmias hospitalizations in the stroke cohort were due to atrial fibrillation or flutter. Atrial arrhythmias were the most frequent cause of dysrhythmia admissions in the non-stroke cohort as well though overall event rates were much lower. Over 5 years, pneumonia (20%), recurrent ischemic stroke (18%), heart failure (15%) and hip fractures (10%) were the most frequent causes of hospitalization in the stroke cohort, Table 2. In the non-stroke cohort, pneumonia (10%) was the leading cause of hospitalization over the 5 year period though the rate was half that of the stroke cohort. KM estimates of cumulative incidence rates for rehospitalization outcomes, shown in Table 2 and e-Table 1, were almost identical to estimates obtained from survival models that adjusted for the competing risk of mortality.
Charges and Payments Made by Medicare
The average acute care hospital admission Medicare covered charges per person-year of follow-up time were $15,562 for the stroke cohort and $7,016 for the non-stroke cohort. The average acute-care related payment made by Medicare per person-year of follow-up time was $5,218 for the stroke cohort and $2,712 for the non-stroke cohort.
CONCLUSIONS
Many acute ischemic stroke patients who have survived their initial stroke hospitalization are rehospitalized over a 5-year period with recurrent ischemic stroke, pneumonia, cardiac events and hip fracture. Our results pertain to Minnesota residents but are consistent with those reported from other geographical areas.5, 6, 10, 15 For example, the strikingly high rehospitalization rates in our study are similar to those reported by Bravata et al. 10 who tracked stroke patients hospitalized in Connecticut from 1995 to 2000. Feng et al. reported on mortality and vascular events in South Carolina and those event rates are similar to those reported here. 6 The unique features of our study are the wide range of outcomes as well as the comparison to a matched non-stroke cohort illustrating the additional cost and morbidity entailed due by to stroke. The differential higher risks of mortality and hospitalization are seen in stroke patients even after the tumultuous early period after hospitalization (i.e. the first 30 days) and these risks persist long-term, as seen from the significant hazard ratios even when event observation is started 1 year post-stroke (Table 3).
The early post-discharge period is of special interest since it could be a marker for in-hospital care quality and the CMS has targeted 30-day readmissions for reporting in HF. The overall 30-day readmission rate for our stroke cohort, 14%, is lower than reported rates among Medicare beneficiaries for other conditions such as HF (27%), pneumonia (20%), and all cause hospitalizations (20%).16 The lower readmission rates for stroke could be due to stroke patients being discharged to inpatient rehabilitation or nursing homes rather than to a home situation. Regardless, the specific high frequency causes for 30-day post-stroke readmissions, dysrhythmias and recurrent ischemic stroke, present potential intervention targets. For instance, more aggressive Holter monitoring in the peri-stroke period may prevent admissions for dysrhythmias and post-discharge nurse follow-up may improve medication adherence and reduce recurrent strokes.
The greater burden of vascular risk factors in the stroke cohort including hypertension, diabetes mellitus and dyslipidemia (Table 1) explains the poor long-term vascular outcomes. While our data is not equipped to address the issue of long-term adherence to antithrombotic therapies or blood pressure management regimens in our cohorts, other studies have shown high rates of discontinuation and non-adherence to secondary prevention therapies in stroke patients and this may contribute to the continued high rates of vascular events after stroke. 17
We acknowledge the following weaknesses of our study. While the non-stroke cohort was constructed by matching to the stroke cohort and eliminating anyone with a prior stroke hospitalization, some of these non-stroke members could have had a prior stroke which was not represented in the Medicare data. Nevertheless, our results show a wide gap between the outcomes of stroke and non-stroke cohorts, suggesting that these two cohorts differ from each other substantially. Furthermore, stroke prevalence in the U.S. population is on the order of 2.9% in the general population. 1 Hence, any stroke contamination of the non-stroke cohort, if it exists, is likely small. A different drawback is that our outcomes were ascertained from Medicare administrative data and not from clinical records. We argue, however, that outcome tracking, such as that presented here, actually represents a good use of Medicare data due to their ready availability and the substantially lower costs of using administrative data rather than following the patients in the community for 5 years. The Medicare payments reported by us do not reflect the total expense of stroke since we do not have information on patient or private insurance payments. We have however, reported total Medicare covered charges as well the amounts paid out by Medicare per-person year to convey the implications of post-stroke readmissions. We also acknowledge that while our results pertain to the Medicare age population, a substantial fraction of ischemic strokes, (17% in our database), occur in those younger than 65 years. Uncommon causes of stroke (vasculitis, dissection) predominate in this younger population who may be sicker and the total cost of stroke may be higher in this group.
The results we have presented illustrate an important aspect of the public health burden of stroke, namely the continued economic costs due to recurrent acute care hospitalizations in stroke survivors. There are two take-home messages. First, while the differential rate of cause-specific hospitalizations in the stroke cohort is unsurprising and reflects the differential risk factor burden and consequences of stroke-related disability, it does suggest considerable room for improvement in tertiary prevention (i.e. prevention of complications) after stroke. Trials focusing on different models of healthcare delivery to stroke survivors in the community and interventions to improve the follow-up care to this population are needed. 18 Strategies to reduce morbidity, mortality and healthcare costs due to stroke have to continue over the long-term, beyond the first year after stroke. Second, current population based surveillance efforts primarily track stroke incidence and prevalence. 1, 8, 9 Based on our results, we argue that such surveillance should be expanded to include a more comprehensive tracking of stroke outcomes including post-stroke rehospitalizations.
Supplementary Material
Acknowledgments
FUNDING SOURCES This research was supported by K23NS051377 to Dr. Kamakshi Lakshminarayan.
Footnotes
DISCLOSURES Dr. Kamakshi Lakshminarayan receives significant salary and research support from the NIH (K23NS051377).
REFERENCES
- 1.American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics – 2010 update. Circulation. 2010;121:e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 2.Cadilhac DA, Carter R, Thrift AG, Dewey HM. Estimating the long-term costs of ischemic and hemorrhagic stroke for Australia: New evidence derived from the north east Melbourne stroke incidence study (NEMESIS) Stroke. 2009;40:915–921. doi: 10.1161/STROKEAHA.108.526905. [DOI] [PubMed] [Google Scholar]
- 3.Luengo-Fernandez R, Gray AM, Rothwell PM. Costs of stroke using patient-level data: A critical review of the literature. Stroke. 2009;40:e18–23. doi: 10.1161/STROKEAHA.108.529776. [DOI] [PubMed] [Google Scholar]
- 4.Taylor TN, Davis PH, Torner JC, Holmes J, Meyer JW, Jacobson MF. Lifetime cost of stroke in the United States. Stroke. 1996;27:1459–1466. doi: 10.1161/01.str.27.9.1459. [DOI] [PubMed] [Google Scholar]
- 5.Dhamoon MS, Tai W, Boden-Albala B, Rundek T, Paik MC, Sacco RL, Elkind MS. Risk of myocardial infarction or vascular death after first ischemic stroke: The Northern Manhattan Study. Stroke. 2007;38:1752–1758. doi: 10.1161/STROKEAHA.106.480988. [DOI] [PubMed] [Google Scholar]
- 6.Feng W, Hendry RM, Adams RJ. Risk of recurrent stroke, myocardial infarction, or death in hospitalized stroke patients. Neurology. 2010;74:588–593. doi: 10.1212/WNL.0b013e3181cff776. [DOI] [PubMed] [Google Scholar]
- 7.Hardie K, Jamrozik K, Hankey GJ, Broadhurst RJ, Anderson C. Trends in five-year survival and risk of recurrent stroke after first-ever stroke in the Perth community stroke study. Cerebrovasc Dis. 2005;19:179–185. doi: 10.1159/000083253. [DOI] [PubMed] [Google Scholar]
- 8.Lakshminarayan K, Anderson DC, Jacobs DR, Jr, Barber CA, Luepker RV. Stroke rates: 1980-2000: The Minnesota Stroke Survey. Am J Epidemiol. 2009;169:1070–1078. doi: 10.1093/aje/kwp029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shahar E, McGovern PG, Pankow JS, Doliszny KM, Smith MA, Blackburn H, Luepker RV. Stroke rates during the 1980s. The Minnesota Stroke Survey. Stroke. 1997;28:275–279. doi: 10.1161/01.str.28.2.275. [DOI] [PubMed] [Google Scholar]
- 10.Bravata DM, Ho SY, Meehan TP, Brass LM, Concato J. Readmission and death after hospitalization for acute ischemic stroke: 5-year follow-up in the Medicare population. Stroke. 2007;38:1899–1904. doi: 10.1161/STROKEAHA.106.481465. [DOI] [PubMed] [Google Scholar]
- 11.Lakshminarayan K, Borbas C, McLaughlin B, Morris NE, Vazquez G, Luepker RV, Anderson DC. A cluster-randomized trial to improve stroke care in hospitals. Neurology. 2010;74:1634–1642. doi: 10.1212/WNL.0b013e3181df096b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thomas AJ, Eberly LE, Smith G Davey, Neaton JD. Multiple Risk Factor Intervention Trial (MRFIT) Research Group. ZIP-code-based versus tract-based income measures as long-term risk-adjusted mortality predictors. Am J Epidemiol. 2006;164:586–590. doi: 10.1093/aje/kwj234. [DOI] [PubMed] [Google Scholar]
- 13.Vila PM, Swain GR, Baumgardner DJ, Halsmer SE, Remington PL, Cisler RA. Health disparities in Milwaukee by socioeconomic status. WMJ. 2007;106:366–372. [PubMed] [Google Scholar]
- 14.Fox J. An R and S-PLUS Companion to Applied Regression. 1 edition Sage Publications, Inc; 2002. Cox proportional-hazards regression for survival data; pp. 1-1–18. [Google Scholar]
- 15.Bravata DM, Ho SY, Brass LM, Concato J, Scinto J, Meehan TP. Long-term mortality in cerebrovascular disease. Stroke. 2003;34:699–704. doi: 10.1161/01.STR.0000057578.26828.78. [DOI] [PubMed] [Google Scholar]
- 16.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among Patients in the Medicare Fee-for-Service Program. The New England Journal of Medicine. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 17.Bushnell CD, Zimmer LO, Pan W, Olson DM, Zhao X, Meteleva T, Schwamm L, Ovbiagele B, Williams L, Labresh KA, Peterson ED, for the Adherence Evaluation After Ischemic Stroke-Longitudinal Investigators Persistence with stroke prevention medications 3 months after hospitalization. Arch Neurol. 2010;67:1456–63. doi: 10.1001/archneurol.2010.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saposnik G, Kapral MK. Poststroke Care: Chronicles of a Neglected Battle. Stroke. 2007;38:1727–1729. doi: 10.1161/STROKEAHA.107.487249. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.