Abstract
Background
This report describes the characteristics associated with successful enrollment of smokers in the social networks (i.e., family and close friends) of patients with lung cancer into a smoking cessation intervention.
Methods
Lung cancer patients from four clinical sites were asked to complete a survey enumerating their family members and close friends who smoke, and provide permission to contact these potential participants. Family members and close friends identified as smokers were interviewed and offered participation in a smoking cessation intervention. Repeated measures logistic regression model examined characteristics associated with enrollment.
Results
A total of 1,062 eligible lung cancer patients were identified and 516 patients consented and completed the survey. These patients identified 1,325 potentially eligible family and close friends. Of these, 496 consented and enrolled in the smoking cessation program. Network enrollment was highest among patients who were white and had late-stage disease. Social network members enrolled were most likely to be female, a birth family, immediate family, or close friend, and live in close geographic proximity to the patient.
Conclusions
Proactive recruitment of smokers in the social networks of lung cancer patients is challenging. In this study, the majority of family members and friends declined to participate. Enlisting immediate female family members and friends, who live close to the patient as agents to proactively recruit other network members into smoking cessation trials could be used to extend reach of cessation interventions to patients’ social networks. Moreover, further consideration should be given to the appropriate timing of approaching network smokers to consider cessation.
Keywords: recruitment, social network, smoking cessation, lung cancer
Introduction
Although cigarette smoking is the single largest preventable cause of death, approximately one-fifth of Americans continue to smoke [1]. About 80% of all primary lung cancers are attributable to smoking [2]. Smokers who successfully quit, however, reduce their risk of lung cancer significantly [3]. Families have similar smoking and smoking cessation patterns, suggesting both genetic susceptibility to nicotine withdrawal sensitivity and behavioral correlates [4,5]. Because the link between lung cancer and smoking is widely known, a lung cancer diagnosis of a loved one may motivate close friends and family members to quit smoking [6-8]. Family members of lung cancer patients who smoke report distress related to the patients’ lung cancer diagnoses, and 79% of family members stated that the diagnosis of lung cancer increased their desire to quit [9]. Despite their relatively strong desire to quit, 71% of family members continued to smoke after their loved ones’ diagnoses [9]. Therefore, family members of patients with smoking-related cancer potentially represent a motivated population in which to target smoking cessation programs.
Social network members, such as family and close friends of patients with cancer, are often overlooked for health promotion efforts. Members of social networks may share behavioral risk factors such as excessive sun exposure, poor diets, or physical inactivity [10,11]. Moreover, social networks exert influence on and share information with their members [12]. For example, when a smoker is successful in quitting smoking, his or her success can spread throughout the social network [13]. In a social network established as part of the Framingham Heart Study, smoking cessation by a spouse decreased a person's chances of smoking by 67% [13]. Thus, engaging patients’ social networks may be an effective method of recruiting smokers into a cessation intervention.
Most smoking cessation interventions employ a reactive approach to enrollment, in which smokers seek out services when they are ready to take action to quit smoking [14]. In that the majority of smokers report no plans to quit smoking in the next 12 months [15], proactive recruitment is needed to broaden the reach of smoking cessation interventions. Thus, it is imperative to develop effective methods of proactively recruiting smokers that are not planning to seek out smoking cessation services on their own to address the underutilization of effective smoking cessation interventions.
Effective strategies to proactively recruit participants into smoking cessation programs are those that appeal to smokers and are responsive to their concerns [16]. Knowledge about the characteristics of patients with lung cancer, and factors associated with members of their social networks’ participation in smoking cessation interventions may provide clinicians with information to engage lung cancer patient's social networks to take steps towards smoking cessation. To this end, Family Ties used a proactive method of recruiting patients’ social networks of smokers to consider participating in a smoking cessation trial.
Methods
Study Overview
These data were collected as part of Family Ties, a two-arm randomized controlled smoking cessation trial. The intervention condition consisted of six telephone-based smoking cessation counseling calls plus tailored self-directed materials. The active control condition consisted of tailored self-directed materials only. Participants in the counseling arm received up to six telephone calls from a trained counselor. The telephone counseling combined motivational interviewing techniques with training in adaptive coping skills and managing stress. All participants received self-directed materials including: a letter from an oncologist that encouraged the participant to quit smoking, self-directed quit kit (including a smoking cessation guide from the American Lung Association, straws, candy, cards, and a notepad), and a graphically rich individually tailored information booklet. The tailored booklet's objectives were to: 1) increase or reinforce the salience of the loved one's lung cancer diagnosis as an impetus for the social network to quit smoking; 2) provide stage-based information to encourage engagement with cessation kit materials; and 3) increase smokers’ confidence in their ability to take steps toward quitting. Participants were also offered nicotine patches. We chose nicotine patches for this study due to standardized usage guidelines and clear dosing recommendations as well as relatively limited side effect profile. Participants were mailed a two-week starter kit with 21mg nicotine patches, if contraindications were not reported. They could call and request a two-week supply of 14mg and 7mg patches, as needed. The goal of Family Ties was to increase the likelihood that patients’ close social network of smokers would quit smoking. We conducted two levels of study recruitment – patients and their social networks. We asked patients who had at least one family member or close friend who smoked to complete a patient survey to enumerate smokers in their social network (i.e., defined as relatives and close friends of the index patient).
Study Sites
We recruited patients with lung cancer from Duke University Medical Center's Thoracic Oncology Program (Duke), Durham Veteran's Administrative Medical Thoracic Oncology Clinic (Durham VA), University of North Carolina Medical Center's Multidisciplinary Thoracic Oncology Program (UNC), and Division and Program of Thoracic Oncology, H. Lee Moffitt Cancer Center and Research Institute (Moffitt) from September 2004 to July 2006. The institutional review boards of each participating site approved this study.
Patient recruitment
Eligible patients were aged 18 and over, diagnosed with lung cancer, intended to continue care at one of the study sites, and had at least one person in their social network who smoked. In both the introductory letter and the phone consent, it was explained that we were doing a survey with patients who were being treated for lung cancer to provide and evaluate services for their family members who currently smoke cigarettes and that the purpose of the study was to investigate new ways to help family members stop smoking. In describing patient participation, it was stated that in addition to answering questions about their own smoking history and receiving materials to assist in stopping smoking, patients would be asked to identify, provide contact information for, and provide consent for the study to contact any family members who smoke. We employed two methods of identifying eligible patients based on local IRB site requirements. At UNC and Moffitt we employed an active (in clinic) recruitment method. Patients at these two institutions were identified in the clinic by study clinicians and coordinators and provided written consent to be contacted by a trained interviewer to complete the baseline survey over the telephone. Study recruiters then provided patients with brochures about the study that patients could pass on to potential participants in their social network. At Duke and the Durham VA we were allowed to employ passive recruitment methods. Study clinicians provided a list of potentially eligible patients who were mailed an introductory letter and then contacted by a trained interviewer who assessed eligibility and obtained phone consent.
Patients who smoked were sent a self-help smoking cessation guide from the American Lung Association. Patients who reported that they were planning to quit in the next 30 days were also sent a 6-week supply of nicotine patches, if they did not report contraindications to nicotine replacement therapy.
Social network recruitment
Study recruiters asked patients’ permission to contact members of their social networks who smoke aged 18 and older. The social network included immediate, birth, and extended family, as well as anyone who the patient perceived as family, such as close friends. All social network members for whom the patient gave permission to contact and for whom the patient gave a valid address were sent an introductory letter describing the study. The letter provided social network members with a toll-free number to call to decline participation. After seven days, we called those who did not decline participation, obtained verbal consent, and administered a 30-minute baseline survey. Social network member eligibility criteria included cognitive ability to give consent to participate, access to a telephone, having smoked at least 100 cigarettes in his/her life, and having smoked at least seven cigarettes in the past seven days. All surveys were conducted using a computer-assisted telephone interviewing program (CATI) at the Durham, North Carolina, office of Battelle Centers for Public Health Research and Evaluation.
Measures
Patient variables
Patients from all four sites were contacted by a trained interviewer and asked to complete a brief telephone survey. Questions included smoking history and demographics (e.g., age, race, gender). Age was categorized at the median split (<65 vs. >65 years). Other patient variables included stage of lung cancer, time since diagnosis retrieved from medical records, and mode of recruitment (active (in clinic) vs. passive).
Social network member variables
During baseline surveys, we assessed participants’ race and gender. We also assessed participants’ relationships with the patient. Patient relationship was categorized as follows: immediate family (spouse/partner, daughter and son); birth family (parent, sister, and brother), extended family (niece, nephew, cousin, grandchild, aunt, uncle or grandparent, in-laws (sister or brother, son or daughter), spouse of extended family and spouse's family); and close friend (reported to be “like family” by the patient). Geographic proximity was calculated using patients’ and participants’ home address zip codes.
Statistical Analysis
Chi-square and t-tests were used, as appropriate, to test for correlates of patient enrollment (yes/no). Repeated measures logistic regression was used to test for predictors of participant enrollment (yes/no). The repeated measures model was used, as it allowed for correlation among study participants identified by the same patient. We tested both univariate and covariate-adjusted correlates of participant enrollment. For the covariate-adjusted tests, all variables were included in the model, regardless of their p-value. A two-sided alpha of 0.05 was used for all tests. The repeated measures logistic regression model was fit using the GLIMMIX procedure of SAS 9.1.
Results
Recruitment
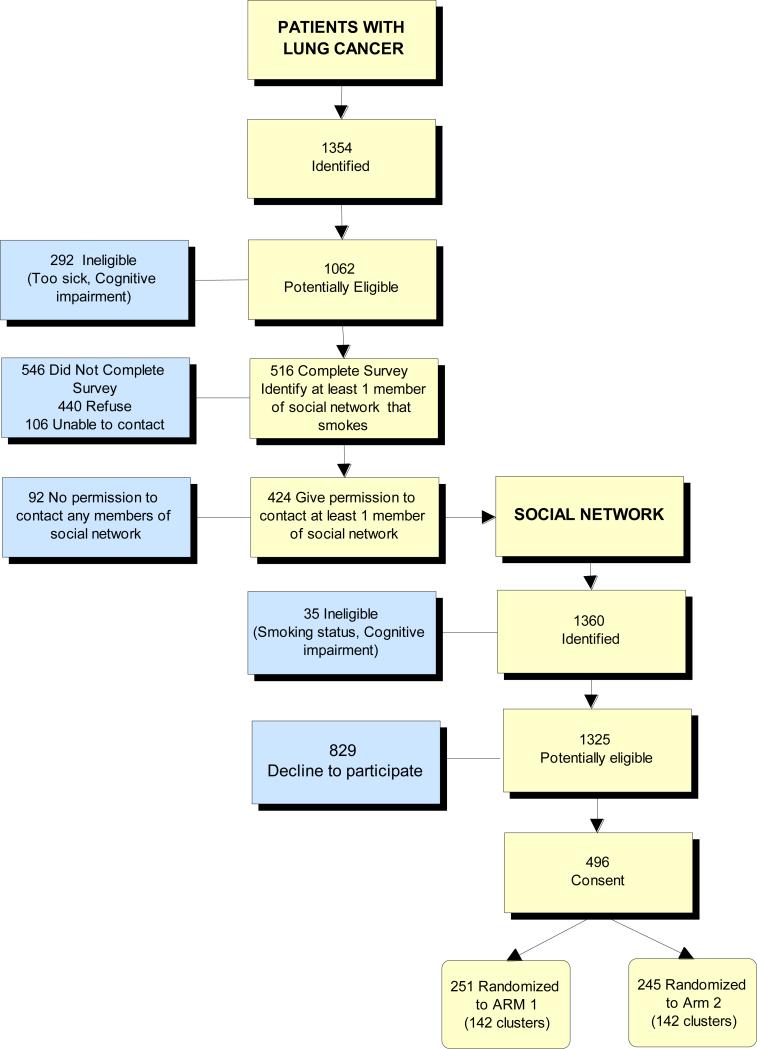
A total of 1,062 eligible patients with lung cancer were identified across the four sites. Among these patients, 516 (49%) completed baseline surveys and enumerated smokers in their social network. (Figure 1). Among the 516 patients who consented and completed the survey, 424 (82%) gave researchers permission to contact at least one member of their social network. The 424 patients listed 1,360 potential participants and 35 were excluded for the following reasons: 2 smoked less than 100 cigarettes in lifetime; 27 smoked less than 7 cigarettes in prior 7 days, and 6 were unable to complete survey because of cognitive impairments. Overall, 496 (37%) of the 1,325 potentially eligible members of the patient's social network agreed to participate in the smoking cessation program. These participants came from 284 patients; 161 of the patients had only 1 participant enroll; 70 had 2 participants enroll, and 53 had 3 or more participants enroll.
Figure 1.
Recruitment Flow Diagram for Patients and their Social Network
Patient characteristics associated with completing the patient survey
Younger patients were more likely to complete the patient survey than older patients (p<0.002) and current/former smokers were more likely to complete the survey than never smokers (p=0.02) (Table 1). Black or white patients were more likely to participate as compared to patients of other races (p= 0.05). Active recruitment at UNC and Moffitt yielded an 80% survey completion rate compared to 41% using passive recruitment at Duke and the Durham VA (p<0.001). Because more eligible patients were identified using the passive recruitment strategy (n=852), the majority of patients (70%) were recruited using this strategy.
Table 1.
Percent of eligible patients with lung cancer completing the baseline survey according to demographic and clinical characteristics (N=1,062)
| Patient characteristic |
Total eligible n =1062 |
% of patients who completed survey n =516 |
P-valuea |
|---|---|---|---|
| Age: | <0.002 | ||
| 64 or younger | 541 | 53 | |
| 65 or older |
521 |
44 |
|
| Race: | |||
| White | 842 | 49 | |
| Black | 179 | 51 | 0.05 |
| Other |
37 |
30 |
|
| Gender: | |||
| Male | 618 | 47 | |
| Female |
444 |
51 |
0.16 |
| Recruitment : | |||
| Passive | 852 | 41 | <0.001 |
| Active |
210 |
80 |
|
| Smoking status: | |||
| Never smoker | 102 | 37 | |
| Past Smoker | 689 | 51 | |
| Current |
239 |
54 |
0.02 |
| Disease stage: | |||
| Early (Ia-IIIa) | 418 | 51 | 0.17 |
| Late (IIIb – IV) |
644 |
47 |
|
| Time since diagnosis: | |||
| ≤90 days | 283 | 49 | |
| >90 days | 779 | 48 | 0.83 |
The p-value is a test of the association of the patient characteristic with whether or not the patient completed the survey.
Patient characteristics associated with social network member enrollment
Social network members of white (39%) or black (32%) patients were more likely to enroll, compared to compared to social network members of patients of other races (16%) (p=0.01) (Table 2). Social network members of late-stage cancer patients (41%) were more likely to enroll than members of early-stage patients (33%) (p=0.02).
Table 2.
Social network member enrollment in a proactive smoking cessation trial according to patient and participant characteristics (N=1,325)
| |
Total eligible Participants n=1,325 |
% of Participants enrolled n=496 |
P value (univariate; multivariate)a |
|---|---|---|---|
|
Patient characteristics
|
|
|
|
| Age (years) | 0.86 (0.95) | ||
| 64 or younger | 793 | 38 | |
| 65 or older |
532 |
37 |
|
| Race: | |||
| White | 1083 | 39 | 0.01 (0.01) |
| Black | 205 | 32 | |
| Other |
37 |
16 |
|
| Gender: | |||
| Male | 698 | 36 | 0.45 (0.39) |
| Female |
627 |
39 |
|
| Recruitment : | |||
| Passive | 461 | 36 | 0.37 (0.59) |
| Active |
864 |
38 |
|
| Smoking status: | |||
| Never smoker | 81 | 44 | 0.35 (0.25) |
| Past | 881 | 38 | |
| Current |
363 |
35 |
|
| Stage of disease: | |||
| Early (I-IIIa) | 584 | 33 | 0.02(0.01) |
| Late (IIIb-IV) |
741 |
41 |
|
| Time since diagnosis: | |||
| Less or equal to 90 days | 382 | 38 | 0.82 (0.53) |
| More than 90 days |
943 |
37 |
|
|
Family member and close friend characteristics
|
|
|
|
| Gender: | |||
| Male | 650 | 32 | <0.001 (<0.001) |
| Female |
675 |
43 |
|
| Relationship: | |||
| Immediate family | 403 | 47 | <0.001 (<0.001) |
| Birth family | 183 | 42 | |
| Close Friends | 161 | 45 | |
| Extended family |
578 |
27 |
|
| Distance to patient: | |||
| Same zip code | 480 | 43 | 0.003 (0.03) |
| Others | 845 | 34 |
The p-value is a test of the association of patient and social network characteristics with whether or not the participant enrolled in the smoking cessation trial.
Social network member enrollment characteristics
Female social network members were more likely to enroll than males (43% versus 32%) (p<0.001) (Table 2). Immediate and birth family members and close friends of the patient were more likely to enroll than extended family members (47%, 42% and 45% versus 27% (p<0.001). Social network members living in the same zip code as the patient were more likely to enroll than those not in the same zip code (43% versus 34%) (p=0.03). Covariate-adjusted associations from the multivariate model were quite similar to the univariate associations (Table 2). The intraclass correlation of enrollment (yes/no) among study participants within the same social network was 0.13.
Discussion
The goal of this study was to promote smoking cessation in family members and close friends of patients with lung cancer. Although the majority of social network members identified as smokers declined to participate, our enrollment rates compare favorably with prior studies using a proactive approach (9-35% enrollment rates) [15,17,18]. However, other studies targeting parents of young children, report higher rates of participation in smoking cessation programs (56% to 67%) [19-21]. The main advantage of proactive recruitment is to broaden the reach of effective interventions, but the accrual rates are typically low because some smokers are not interested in quitting.
Lung cancer patients who were white, younger (less than 65 years old), and had a history of smoking were most likely to complete the patient survey and enumerate social network members who smoked. Patients selected by their clinicians and approached by research staff in the clinic setting were more likely to participate than patients who were mailed a letter. Direct interaction with patients in the oncology setting appears to be optimal for encouraging referral of network smokers. However, such recruitment methods are significantly more time consuming for both research and clinic staff.
We identified several characteristics associated with smoking cessation program participation among social networks of smokers identified by patients. In our study, female social network members were more likely to enroll than males. Others have suggested that women, particularly those in close relationships with the patient, may play key roles in social networks of families affected by cancer [22]. Moreover, women may be more involved in the care of an ill relative or friend with lung cancer [23] and, thus, may be more affected by their illness. It has been suggested that these women might be enlisted to engage other family members in behaviors such as uptake of cancer screening [22]. Future research should focus on enlisting women family members to encourage the more recalcitrant smokers in patients’ social networks to quit smoking.
We also found that social network members who live in the same zip code as patients were more likely to enroll in the smoking cessation program. Geographic proximity may enhance interactions and increase caregiver responsibilities. In turn, these increased interactions may serve to reinforce behavior change efforts. It is also possible that living near the patient with lung cancer gives the participant a better understanding of the patient's illness and personalizes the risks of smoking. Moreover, close proximity of the patient may increase psychological distress because it leads the participant to be more aware of and concerned about the negative health impacts of smoking around the patient. Mak et al (2006) found that smokers in the same home were more likely to participate in smoking cessation program targeting parents of young children, possibly due, in part, to concerns about the negative consequences of smoking on the family's health [19].
Social network members of late-stage lung cancer patients were more likely to enroll than members of early-stage patients. Family members and close friends may have been more distressed by a late-stage diagnosis and more motivated to quit smoking. Further research is needed to understand the optimal timing for behavior change among patients and their social network after a cancer diagnosis.
Extended family members (i.e., nieces and nephews) were less likely to enroll compared to birth family, immediate family, and close friends. This association remained significant even after adjusting for geographic proximity to the patient. Previous studies have found closeness of the relationship between the cancer patient and the family member can affect behavior change [24, 25]. Future studies targeting family members and close friends might consider asking the patient additional questions about his/her extended family to capture how close they are or how often they communicate.
Our study has some limitations. We only recruited patients with lung cancer and their family members and close friends. Lung cancer is a serious life-limiting illness with well-known links to smoking [26]. We did not have a comparison group (i.e., relatives of patients not diagnosed with cancer). In the absence of this, it is impossible to discern if the rate of referral and enrollment is dissimilar for cancer patients’ relatives. It is also unclear if we could replicate our efforts with other smoking-related illnesses such as cardiovascular disease or other smoking-related cancers such as esophageal cancer. Another potential limitation is our measure of geographic proximity based on zip code congruence. Street level data would improve our precision. However, our measure is a reasonable approximation of geographic proximity. We were unable to collect behavioral or smoking-related data on family members and close friends who did not participate in this study. If feasible, it would be useful to collect information from non-participants in future studies. Our study was also limited to adult family members and close friends (18 years and over). Future research should consider including adolescents; 90% of adult smokers report initiating smoking during childhood and adolescence [27].
Conclusion
Our multi-site study used a proactive approach to recruit participants into a smoking cessation trial. By asking patients with lung cancer to enumerate family members and close friends who smoke, we may have been able to intervene with people ready to re-evaluate their smoking behavior. While the period following a cancer diagnosis has been widely suggested to be an opportune time to educate the patient's social network about behavior change, enlisting these individuals to consider interventions may not be straightforward. Results of this study provide important insights for oncologists interested in encouraging family members and close friends of their patients to quit smoking. More research is needed to make optimal use of social networks to influence friends and family of lung cancer patients to quit smoking.
Acknowledgments
This work was supported by National Cancer Institute grant 5U01-CA-92622.
This research was also supported [in part] by the Intramural Program of the National Human Genome Research Institute, National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NCI, NHGRI, NIH or the Department of Veterans Affairs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Clinical trials # NCT00345891
References
- 1.Centers for Disease Control and Prevention (CDC) Vital signs: current cigarette smoking among adults aged >or=18 years --- United States, 2009. MMWR Morb Mortal Wkly Rep. 2010 Sep 10;59(35):1135–40. [PubMed] [Google Scholar]
- 2.Ezzati M, Lopez AD. Estimates of global mortality attributable to smoking in 2000. Lancet. 2003;362:847–852. doi: 10.1016/S0140-6736(03)14338-3. [DOI] [PubMed] [Google Scholar]
- 3.Peto R, Darby S, Deo H, Silcocks P, Whitley E, Doll R. Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies. BMJ. 2000;321:323–329. doi: 10.1136/bmj.321.7257.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uhl GR, Liu QR, Drgon T, Johnson C, Walther D, Rose JE, David SP, Niaura R, Lerman C. Molecular genetics of successful smoking cessation: convergent genome-wide association study results. Arch Gen Psychiatry. 2008;65(6):683–93. doi: 10.1001/archpsyc.65.6.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hardin J, He Y, Javitz HS, Wessel J, Krasnow RE, Tildesley E, Hops H, Swan GE, Bergen AW. Nicotine withdrawal sensitivity, linkage to chr6q26 and association of OPRMI SNPs in the smoking in families (SMOFAM) sample. Cancer Epidemiol Biomarkers Prev. 2009;188:3399–406. doi: 10.1158/1055-9965.EPI-09-0960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gritz ER, Fingeret MC, Vidrine DJ, Lazev AB, Mehta NV, Reece GP. Successes and failures of the teachable moment: smoking cessation in cancer patients. Cancer. 2006;106(1):17–27. doi: 10.1002/cncr.21598. [DOI] [PubMed] [Google Scholar]
- 7.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18(2):156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- 8.McBride CM, Ostroff JS. Teachable moments for promoting smoking cessation: the context of cancer care and survivorship. Cancer Control. 2003;10(4):325–33. doi: 10.1177/107327480301000407. [DOI] [PubMed] [Google Scholar]
- 9.McBride CM, Pollak KI, Garst J, et al. Distress and motivation for smoking cessation among lung cancer patients’ relatives who smoke. J Cancer Educ. 2003;18(3):150–156. doi: 10.1207/S15430154JCE1803_08. [DOI] [PubMed] [Google Scholar]
- 10.Manne S, Fasanella N, Connors J, Floyd B, Wang H, Lessin S. Sun protection and skin surveillance practices among relatives of patients with malignant melanoma: prevalence and predictors. Prev Med. 2004 Jul;39(1):36–47. doi: 10.1016/j.ypmed.2004.02.028. [DOI] [PubMed] [Google Scholar]
- 11.Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult and Clin Psych. 1999;67:132–138. doi: 10.1037//0022-006x.67.1.132. [DOI] [PubMed] [Google Scholar]
- 12.Heaney CA, Israel BA. Social networks and social support. In: Glanz K, Lewis FM, Rimer B, editors. Health behavior and health education: Theory, research, and practice. 3rd ed. Jossey-Bass Publishers; San Francisco: 2002. pp. 185–209. [Google Scholar]
- 13.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358:2249–58. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lichtenstein E, Glasgow RE, Lando HA, Ossip-Klein DJ, Boles SM. Telephone counseling for smoking cessation: rationales and meta-analytic review of evidence. Health Educ Res. 1996 Jun;11(2):243–57. doi: 10.1093/her/11.2.243. [DOI] [PubMed] [Google Scholar]
- 15.Gilbert H, Nazareth I, Sutton S. Assessing the feasibility of proactive recruitment of smokers to an intervention in general practice for smoking cessation using computer-tailored feedback reports. Family Practice. 2007;24:395–400. doi: 10.1093/fampra/cmm028. [DOI] [PubMed] [Google Scholar]
- 16.Dahm JL, Cook E, Baugh K, Wileyto EP, Pinto A, Leone F, Halbert CH, Schnoll RA. Predictors of enrollment in a smoking cessation clinical trial after eligibility screening. J Natl Med Assoc. 2009;101:450–455. doi: 10.1016/s0027-9684(15)30931-7. [DOI] [PubMed] [Google Scholar]
- 17.Etter J, Perneger TV. Effectiveness of a computer-tailored smoking cessation program. Arch Intern Med. 2001;161:2596–2601. doi: 10.1001/archinte.161.21.2596. [DOI] [PubMed] [Google Scholar]
- 18.Lennox AS, Osman LM, Reiter E, Robertson R, Friend J, McCann I, Skatun D, Donnan PT. Cost effectiveness of computer tailored and non-tailored smoking cessation letters in general proactive: randomized controlled trial. BMJ. 2001;322:1–7. doi: 10.1136/bmj.322.7299.1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mak YW, Loke AY, Lam TH, Abdullah AS. Predictors of the participation of smoking parents in a proactive telephone-based smoking cessation program. Addict Behav. 2006 Oct;31(10):1731–43. doi: 10.1016/j.addbeh.2005.12.018. [DOI] [PubMed] [Google Scholar]
- 20.Abdullah AS, Mak YW, Loke AY, Lam TH. Smoking Cessation intervention in parents of young children: a randomised controlled trial. Addiction. 2005;100:1731–1740. doi: 10.1111/j.1360-0443.2005.01231.x. [DOI] [PubMed] [Google Scholar]
- 21.Winickoff JP, Hibberd PL, Case B, Sinha P, Rigotti NA. Child hospitalization: an opportunity for parental smoking intervention. Am J Prev Med. 2001 Oct;21(3):218–20. doi: 10.1016/s0749-3797(01)00355-5. [DOI] [PubMed] [Google Scholar]
- 22.Koehly LM, Peters JA, Kenen R, Hoskins LM, Ersig AL, Kuhn NR, Loud JT, Greene MH. Characteristics of health information gatherers, disseminators, and blockers within families at risk for hereditary cancer: implications for family health communication interventions. Am J Public Health. 2009;99:2203–9. doi: 10.2105/AJPH.2008.154096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Family Caregiver Alliance Selected caregiver statistics. http://www.caregiver.org.
- 24.Humpel N, Magee C, Jones SC. The impact of a cancer diagnosis on the health behaviors of cancer survivors and their family and friends. Support Care Cancer. 2007;15(6):621–30. doi: 10.1007/s00520-006-0207-6. [DOI] [PubMed] [Google Scholar]
- 25.Lemon SC, Zapka JG, Clemow L. Health behavior change among women with recent familial diagnosis of breast cancer. Prev Med. 2004;39(2):253–62. doi: 10.1016/j.ypmed.2004.03.039. [DOI] [PubMed] [Google Scholar]
- 26.Alberg AJ, Ford JG, Samet JM. Epidemiology of Lung cancer: ACCP Evidence-based clinical practice guidelines (2nd edition). Chest. 2007;132:29S–55S. doi: 10.1378/chest.07-1347. [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control Cigarette smoking among adults—United States, 2003. MMWR. 2005;54:509–13. [PubMed] [Google Scholar]