Abstract
Background
Surgical treatment of obesity is cost-effective and improves life expectancy. Roux-en-Y gastric bypass (RYGB) and adjustable gastric banding (AGB) are dominant surgical techniques, but RYGB is the only publicly insured procedure in all Canadian provinces. Private clinics currently offer AGB with minimal wait times. We sought to compare RYGB in public facilities with AGB in private clinics in terms of cost, wait times and certain aspects of patient care.
Methods
We conducted telephone interviews of all bariatric surgery providers across Canada (100% response rate). We asked about various aspects of care, such as wait time, cost, pre- and postoperative care and surgeon experience.
Results
The median out-of-pocket cost for AGB at private facilities is $16 000 (range $13 160–$18 375). Private clinics have much shorter wait times for AGB than public facilities do for RYGB (1 v. 21 mo, p < 0.001). Private clinics provide significantly fewer preoperative visits with multidisciplinary health professionals (2.7 v. 4.3, p = 0.045), and 5 of 12 (42%) private clinics conduct AGB surgeries without on-site critical care for high-risk (based on the respondents’ definitions) patients.
Conclusion
Private clinics performing AGB offer short wait times, but the cost is high. We found a great deal of variation between pre- and postoperative care among bariatric surgery facilities, and in some cases patient care appears to be less comprehensive. Our findings suggest that further research on obesity treatment is needed to inform policy so that all Canadians can have equitable and timely access to proven, evidence-based care.
Abstract
Contexte
Le coût du traitement chirurgical de l’obésité présente un bon rapport coût-efficacité et améliore l’espérance de vie. Le pontage gastrique Roux-en-Y (PGRY) et l’anneau gastrique ajustable (AGA) constituent les principales techniques chirurgicales, mais le PGRY est la seule intervention assurée par le secteur public dans toutes les provinces du Canada. Les cliniques privées offrent actuellement l’AGA après un temps d’attente minimal. Nous avons cherché à comparer la technique PGRY pratiquée dans des établissements publics à celle de l’AGA pratiquée dans des cliniques privées pour ce qui est des coûts, des temps d’attente et de certains aspects du soin des patients.
Méthodes
Nous avons réalisé des entrevues téléphoniques auprès de tous les four-nisseurs de services de chirurgie bariatrique au Canada (taux de réponse de 100 %). Nous avons posé des questions sur divers aspects des soins comme les temps d’attente, le coût, les soins préopératoires et postopératoires, et l’expérience du chirurgien.
Résultats
Le coût direct médian de l’AGA dans les établissements privés s’établit à 16 000 $ (intervalle de 13 160 $ à 18 375 $). Les cliniques privées affichent des temps d’attente beaucoup plus courts pour l’AGA que les établissements publics dans le cas du PGRY (1 c. 21 mois, p < 0,001). Les cliniques privées fournissent un nombre significativement moins élevé de consultations préopératoires avec des équipes multidisciplinaires de professionnels de la santé (2,7 c. 4,3, p = 0,045) et 5 cliniques privées sur 12 (42 %) pratiquent des interventions chirurgicales de mise en place d’un AGA sans offrir de soins intensifs sur place pour les patients à risque élevé (selon les définitions des répondants).
Conclusion
Les cliniques privées qui posent des AGA offrent des temps d’attente plus courts, mais le coût est élevé. Nous avons constaté une variation importante au niveau des soins préopératoires et postopératoires offerts par les établissements qui pratiquent la chirurgie bariatrique et dans certains cas, le soin des patients semble moins complet. Nos constatations indiquent qu’une recherche plus poussée sur le traitement de l’obésité s’impose pour éclairer les politiques afin que tous les Canadiens puissent avoir un accès équitable et opportun à des soins factuels et éprouvés.
Obesity, defined as a body mass index (BMI) of 30 or above, is a serious health concern. It is a clinically important risk factor for hypertension, type 2 diabetes, coronary artery disease and several forms of cancer.1,2 There is a growing obesity epidemic, with the rate of morbid obesity (BMI > 40) rapidly increasing.3 As a result of the numerous health complications in this group, average health costs exceed $10 000 per patient per year.4 There are several options for the medical management of weight loss, but most empiric studies have demonstrated limited sustained efficacy and cost-effectiveness.5 Current findings indicate that surgical treatment of morbid obesity is cost-effective and offers lower long-term mortality than medical management.6–14
Many types of bariatric surgery have been used to reconfigure a patient’s digestive system, resulting in weight loss.15,16 Two surgical procedures have become dominant: adjustable gastric banding (AGB) and Roux-en-Y gastric bypass (RYGB).17 Both procedures require a general anesthetic, which is associated with greater risk in morbidly obese individuals. Adjustable gastric banding is a relatively simple laparoscopic procedure in which a saline-filled band is placed around the upper stomach, resulting in early satiety when the upper pouch fills. In contrast, RYGB is a more complex surgical procedure involving reattachments of the gastrointestinal tract. It has become the most popular bariatric procedure worldwide and is considered by many bariatric surgeons to be the most effective technique.18–21 To our knowledge, the only randomized controlled trial (RCT) to compare these 2 procedures showed superior weight loss with RYGB,21 and a systematic review also found that RYGB had an improved resolution of comorbidities, lower reoperation rates and higher patient satisfaction.7 Conversely, AGB has faster recovery time and is sometimes preferred by patients because it has lower perioperative mortality and is completely reversible.22
Roux-en-Y gastric bypass is to varying extents an insured medical service in all Canadian provinces, although not in the territories.23 However, lengthy wait times have been reported, with some reports suggesting that waits are the longest for any surgically treated condition and average about 5 years.24–26 Reasons include limited availability of trained surgeons, operating room (OR) time, availability of postoperative beds and low prioritization owing to the chronic nature of obesity. In contrast, AGB is insured in 2 provinces: Alberta and New Brunswick. In some provinces where the government does not insure AGB, private facilities have opened and offer outpatient AGB at an out-of-pocket expense to patients, with some of these facilities advertising short wait times. We were interested in investigating whether these facilities offered comprehensive patient care with multidisciplinary treatment. We sought to identify all public and private bariatric surgery providers in Canada and compare publicly funded RYGB and AGB offered in private clinics based on cost, wait times and certain aspects of patient care.
Methods
We identified all bariatric surgery facilities in Canada for the purpose of conducting telephone interviews. We defined private facilities as those that were distinct from government- or other publicly insured bodies27,28 and required payment for services. We identified facilities through a series of standardized Internet searches that found news articles, private commercial websites (private clinics only), bariatric surgery associations, obesity support groups and government resources. From these resources, we developed a list of potential clinics and surgeons. We verified the registration status, demographic information and practice locations of these providers with the provincial medical regulatory authorities. Telephone conversations with the individual facilities included confirming the names of practising surgeons and inquiring about other clinics. The entire process was iterative and was continued until no new surgeons or clinics could be identified.
Structured telephone interviews were conducted with clinic staff at each public and private bariatric surgery facility between March and September 2009. During these conversations, the interviewer asked to speak with a clinic employee who could best answer administrative questions over the phone about the process involved in obtaining surgery (i.e., consultation, patient selection, surgery and follow-up). The interviewer identified himself as an interested party but did not disclose research intent. These interviews were based on a standardized script (Box 1), with small variations in phrasing used to keep the conversation flowing naturally; for example, the conversation sometimes prompted question 1 to be phrased as follows: “How soon could someone get surgery booked?” (Box 1). Data collected included wait time for surgery from the initial request or referral for a consultation, cost, surgeon experience, number and type of pre- and postoperative appointments, location of the surgery and availability of on-site critical care. Clinics that perform surgery outside of hospitals with critical care facilities were asked if they offer surgery in-hospital for high-risk patients; we left the definition of high risk up to the respondents. We also asked clinic staff about patient selection procedures to determine whether each clinic employed selection criteria that would help surgeons exclude certain patients and to elicit staff opinion on general trends of how often patients were offered surgery. Each facility was contacted by 2 different interviewers (A.M. and J.K.) 1–6 months apart. Discrepancies between the findings were resolved by subsequent phone calls (A.M.).
Box 1. Telephone interview scripts.
Script of questions for phone interview of private clinics
For personal reasons, I am interested in bariatric surgery. Is there someone who is available to answer my questions?
How soon is the earliest that surgery is available?
What types of surgery do you offer?
Where is the surgery performed? (In hospital or in separate clinic) Is there an ICU or critical care on-site? (If answer is no) Is that the same for high-risk patients?*
How much does it cost?
Is there any payment plan available? (If yes) What is the company?
I’d like to know more about your surgeons. What are the names of the surgeons in your clinic?
I’ve heard some surgeons complete a fellowship specifically in bariatric surgery or minimally invasive. Have these surgeons done so?
Do your surgeons also work in a hospital? (If yes) Which one? Do they also perform weight-loss surgery there?
Before the surgery, can you tell me about all of the appointments? And are these with other health professionals?
How often are patients screened out? What are the criteria that have to be met?
After the surgery, does the patient stay overnight? What are all of the postoperative appointments?
Where do you accept patients from? Out of province?
Script of questions for phone interview of public clinics
For personal reasons, I am interested in bariatric surgery. Is there someone who is available to answer my questions?
How soon is the earliest that surgery is available?
What types of surgery do you offer?
Is there an ICU or critical care on-site where the surgery will be performed? (If no) Is that the same for high-risk patients?*
I’d like to know more about your surgeons. What are the names of the surgeons in your clinic?
I’ve heard some surgeons complete a fellowship specifically in bariatric surgery or minimally invasive. Have these surgeons done so?
Do your surgeons also work in a private clinic? (If yes) Which one? Do they also perform weight-loss surgery there?
Before the surgery, can you tell me about all of the appointments? And are these with other health professionals?
How often are patients screened out? What are the criteria that have to be met?
After the surgery, does the patient stay overnight? What are all of the postoperative appointments?
Where do you accept patients from? Out of province?
ICU = intensive care unit.
The definition of high-risk was left to the respondents’ discretion.
Although some public clinics offering RYGB also perform AGB or other types of surgery, including vertical sleeve gastrectomy and duodenal switch, we decided to focus our comparison on publicly funded RYGB providers and purely private AGB providers to simplify analysis. Clinics that were found to provide both publicly insured RYGB and AGB were only included in the public RYGB group. We felt this was a fair comparison because in Canada, these are the 2 types of surgery that most patients receive, and in most provinces (all except Alberta and New Brunswick in which AGB is also publicly funded) patients are faced with the decision to wait for RYGB in the public system or pay out of pocket for AGB. In addition, the surgeries are similar enough that much of the surrounding care (e.g., preoperative counselling, patient selection) can be compared directly. Our study protocol was approved by the St. Michael’s Hospital Research Ethics Board.
Statistical analysis
Data were tabulated, and we analyzed numeric data for significant differences between public and private facilities. We aggregated the number of appointments with various health professionals before and after surgery as a summary measure. Differences between the 2 groups were analyzed using a Student t test for normally distributed data or the Mann–Whitney U test for nonparametric data.
Results
We identified a total of 30 bariatric surgery clinics (18 public and 12 private) and 53 bariatric surgeons (29 in the public system, 18 in the private system and 6 operating in both systems) across Canada. Public facilities were found in Nova Scotia, New Brunswick, Quebec, Ontario, Saskatchewan, Alberta and British Columbia, and all of these offered RYGB. In provinces where RYGB facilities are not available despite the procedure being publicly funded, patients are referred out of province or out of country. Private clinics were identified in Quebec, Ontario, Manitoba and British Columbia, and all of these offered AGB. No facilities were found in Prince Edward Island, Newfoundland or the territories. We conducted telephone interviews with all clinics, achieving a 100% response rate. The respondents were clerical workers, registered nurses and managers. Findings from the telephone interviews are compared in Table 1.
Table 1.
Comparison of publicly funded Roux-en-Y gastric bypass and private adjustable gastric banding providers
| Variable | AGB | RYGB | p value |
|---|---|---|---|
| No. clinics | 12 | 18 | |
| No. surgeons | 24 | 35 | |
| Out-of-pocket cost, median (range) Can$ | 16 000 (13 160–18 375) | 0§ | |
| Financing available, no. (%) of institutions | — | ||
| Direct | 2/12 (17) | ||
| Via third party | 6/12 (50) | ||
| Total | 8/12 (67) | ||
| Wait time, median (IQR) [range] mo | 1 (1.0–1.5) [0.5–2.5] | 18 (13–36) [9–60] | < 0.001 |
| Surgeries performed at location with critical care, no. (%) | |||
| All | 4/12 (33) | 18/18 (100) | |
| High-risk only | 3/12 (25) | ||
| None | 5/12 (42) | ||
| Surgeon experience, mean (SD) yr | |||
| Post-residency/certification | n = 18 14.6 | n = 11 14.0 | 0.85 |
| Post-MD | n = 20 22.7 (11.4) | n = 20 19.4 (9.2) | 0.32 |
| Multidisciplinary preoperative visits, mean (SD) no. | 0.045 | ||
| Total | 2.7 (1.6) | 4.3 (2.4) | |
| Surgeon | 1.0 (0.0) | 1.2 (0.4) | |
| Dietician | 0.4 (0.5) | 0.8 (0.4) | |
| Wellness coordinator* | 0.6 (0.5) | 0.6 (1.0) | |
| Psychologist | 0.3 (0.5) | 0.3 (0.5) | |
| Anesthesiologist | 0.1 (0.3) | 0.1 (0.3) | |
| Internist† | 0.1 (0.3) | 0.6 (0.6) | |
| Exercise physiotherapist | 0.0 (0.0) | 0.1 (0.3) | |
| Education class | 0.2 (0.4) | 0.7 (1.2) | |
| Multidisciplinary postoperative visits in first year, mean (SD) no.‡ | 0.28 | ||
| Total | 3.7 (1.6)¶ | 4.3 (1.6) | |
| Surgeon | 2.3 (0.7) | 2.1 (0.9) | |
| Dietician | 0.6 (0.8) | 1.1 (1.0) | |
| Wellness coordinator* | 0.8 (0.8) | 0.4 (0.6) | |
| Internist† | 0.0 (0.0) | 0.8 (0.9) | |
| Accept out of province, no. (%) | 11/12 (92) | 7/18 (39) |
AGB = adjustable gastric banding; IQR = interquartile range; RYGB = Roux-en-Y gastric bypass; SD = standard deviation.
Wellness coordinator also includes registered nurse or social worker.
Internist includes general internist or endocrinologist.
The duration of the postoperative visits was not determined.
The cost of RYGB to the public system was not estimated in this study.
Total includes planned band adjustments but not unplanned adjustments.
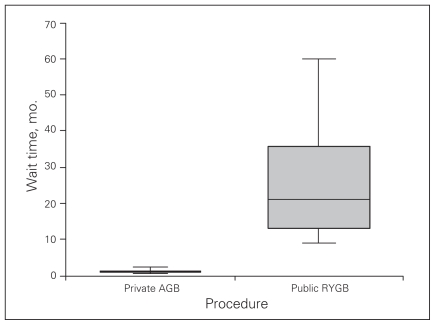
The median out-of-pocket cost for AGB surgery at private facilities in Canada was $16 000 (range $13 160–$18 375; Table 1). Among private facilities, 8 of 12 (67%) offered financing options to pay for the surgery, most often (6 of 8) through a third party. The median wait time for surgery in private facilities was significantly shorter than that in public facilities (1 [range 0.5–2.5] mo v. 21 [range 9–60] mo, p < 0.001; Fig. 1).
Fig. 1.
Comparison of wait times between private adjustable gastric banding (AGB) and publicly funded Roux-en-Y gastric bypass (RYGB).
Most clinics required consultations with a variety of health professionals (e.g., dietician, psychologist) in addition to the surgeon before and after surgery. The public clinics required significantly more preoperative multi-disciplinary visits than private clinics (mean 4.3 v. 2.7, p = 0.045). The most pronounced differences between the number of visits required by public and private clinics were the number of visits to internists/endocrinologists (0.6 v. 0.1) and the number of education classes (0.7 v. 0.2). The difference in the number of postoperative visits at the public and private clinics was not significant.
Among respondents at private facilities, 8 of 12 (67%) stated that surgery was performed without on-site critical care support. In the case of patients deemed high-risk based on the individual definitions of respondents, 5 of 12 (42%) operated without on-site critical care support. All 18 public facilities had on-site critical care support.
Detailed information on determination of patient eligibility was unavailable for most clinics. Respondents at 6 of 18 public clinics stated their eligibility process was still under development, but respondents at all 18 said they generally followed the current Canadian Clinical Practice Guidelines (CPGs).29 One respondent (5%) at a public clinic noted that up to 20% of potential patients are denied surgery. Respondents at most private clinics (75%) did not disclose information about their eligibility criteria or how many prospective patients are denied surgery. Respondents at 3 (25%) private clinics reported that they have little or no screening process. They also said that patients with a BMI less than 35 can have the surgery.
Very few of the clinics were able to provide detailed information on the experience level of their surgeons specific to bariatric surgery. As a reasonable proxy, we tried to determine the number of years since completion of residency training and certification by the Royal College of Physicians and Surgeons of Canada and/or the number of years since completion of medical school (MD or equivalent degree). Both public and private clinics reported high experience levels for their surgeons. Most surgeons in both settings also had specialized fellowship training in bariatric or minimally invasive surgery (13 of 14 surgeons at public clinics where information was available and 9 of 11 surgeons at private clinics where information was available). We also noted that many surgeons in both groups held major administrative positions at their respective hospitals.
Discussion
We believe that we identified all providers in Canada that offer bariatric surgery as a treatment for obesity and found important differences between public and private facilities that affect patient care. Private clinics performing AGB offer extremely short wait times, but this type of surgery has been reported to be less effective than RYGB as a treatment for obesity.6,8,11,12,18,19 We also felt that several aspects of patient care in private clinics appeared to be less comprehensive than that in public clinics. Private clinics on average offer significantly fewer multidisciplinary pre-operative visits than public clinics, though it should be noted that we did not compare the duration of the visits between the private and public clinics, which would have been valuable information. In terms of postoperative care, we found no significant differences between private and public clinics. However, these results may have been confounded by differences in the type of postoperative care, which at AGB clinics often focused on regularly scheduled band adjustments and at public clinics often focused on recovery from surgery and nutrition. It should be noted that 4 of 12 (33%) private clinics offer comprehensive pre-and postoperative care plans that match or exceed the mean number of pre- and postoperative visits in public clinics, indicating a wide range of care among facilities. We also found differences in the availability of on-site critical care support between private and public facilities. Some private clinics (5 of 12, 42%) perform all procedures on site without critical care facilities and with no differentiation between high- and low-risk patients based on the respondents’ definition of risk, whereas the remaining 7 (58%) clinics opt to perform surgery in high-risk patients in hospital with on-site critical care rather than in the clinic setting. Surgeries performed without on-site critical care could encounter perioperative complications that may necessitate transfer by ambulance. This is a major concern with morbidly obese patients, who are at increased risk of complications during general anesthesia. This situation, where private facilities are allowed to perform AGB without on-site critical care, may be partially explained by a lack of regulation of private facilities.30 In addition, minimal patient eligibility criteria could allow inappropriate patients to receive surgery and put them at significant risk.
We found that the out-of-pocket cost to the patient for AGB is high. A portion of the fee presumably corresponds to surgeon remuneration, although we did not ask for this information as it was unlikely to be disclosed. An anecdotal estimate of remuneration for AGB is about $5000 per surgery, although that figure likely varies substantially. This figure is quite distinct from that in the public system, with Ontario surgeons earning just over $1300 per surgery. Some private clinics are able to schedule up to 4 AGB surgeries in a single day, whereas public clinics usually schedule 2 RYGB procedures, which are substantially longer and more complex, in 1 day.31 The high cost for private AGB constitutes a barrier for many patients, despite the availability of financing programs.
An incidental observation during our data collection was that several private clinics had information on their web-sites regarding the risks and benefits of AGB versus RYGB that was not consistent with the literature.
Our results demonstrate that the wait time for AGB in private clinics is significantly shorter than that for RYGB in public facilities. The difference, particularly in certain areas of Canada where the wait in the public system still approaches 5 years, could be enough of an incentive for patients to turn to AGB at private clinics, even if RYGB is their preferred procedure. This comparison suggests that further public funding for capacity increases and wait time improvements may be needed, particularly in provinces other than Ontario.32 However, it does not seem necessary that the wait time for publicly financed bariatric surgery needs to be reduced to that for AGB in private clinics. A period of weeks or even a few months between initial consultation and surgery may not be sufficient for appropriate psychological testing and lifestyle adjustment or to allow patients the chance to change their minds. In contrast, many public clinics and some private clinics have preoperative education and nutrition programs that require 6–12 months to complete, similar to presurgical behaviour modification recommendations in the literature.33,34 From this perspective, an appropriate wait time for surgery could be in this range, which may not be out of reach for the public system with modest improvements. However, it should be noted that our wait time findings (median 21 mo, range 9–60 mo) are significantly less than those reported in recent studies of bariatric surgery in Canada (range 48–60 mo).24–26 Some of this disparity may relate to the different methods of wait time calculation among studies. In addition, our work examines the current experience of a patient entering the queue for surgery, which may show shorter wait times owing to the recent influx in funding for bariatric surgery in many provinces.32
It is also clear that the field of bariatric surgery in Canada is in need of further standardization. Whereas the 2006 Canadian CPGs29 provide general criteria for surgery, there is still great variation among public and private clinics regarding what surgery types are offered and which patients are eligible to receive surgery. The guidelines also do not lay out a concise preoperative or postoperative standard of care, leaving each clinic to define its own program. This missing framework is essential to guide excellent care and protect those who should not receive surgery.
Limitations
Our study was somewhat unique in that it looked at bariatric surgery in Canada from the patient’s perspective. The findings augment the body of research that examines the procedures themselves, and may be particularly useful to policymakers.6–8,11,12,18–20 However, there are several limitations to this research that should be recognized. The data collection method relied on the accuracy of the information provided by clinic employees, comprising nurses, managers and clerical staff. Responses were sometimes vague or uncertain, and certain questions were deferred by clinic staff to be answered by the surgeon during a consultation. We made an effort to mitigate these problems by having 2 investigators call independently multiple times, and repeatedly asking to speak with the clinic nurse for clarification. No attempt was made to speak directly with the surgeons for several reasons. This method was simple, and the data collected were mainly administrative and did not require medical expertise. However, we acknowledge that the ability of the clinic staff to answer questions about the patient selection process may be limited, and the surgeons would have been the best people to answer such questions. In addition, we felt that conversations with clinic staff could be conducted quickly with minimal disruption to their usual responsibilities and that the information might be given more freely by clinic staff than by surgeons. Our results could also be skewed by our decision to only include mixed RYGB/AGB facilities in the public RYGB group. However, we felt this approach was justified. The AGB surgeries in Alberta and New Brunswick are publicly financed and did not fit into either group in our comparison between RYGB in public facilities and AGB in private facilities. Also, the small number of these clinics (3) was not sufficient for comparison. The 3 public clinics in Ontario and British Columbia that also offer AGB for a private fee are unique in that they are all located within hospitals and primarily operate as public clinics with similar processes regardless of surgery type and with minimal or no advertising to our knowledge. Thus, we felt the most meaningful comparison was between public RYGB clinics and purely private AGB clinics. A further limitation is that our results are affected by rapidly changing policies, such as $75 million of funding reforms in Ontario that will increase the number of surgeries performed 5-fold.32 Furthermore, evidence regarding each type of surgery continues to emerge, and the procedures continue to evolve. Our approach was to capture a snapshot of the field at 1 point in time by minimizing our data collection period.
Future research is needed to quantify the differences in care and patient selection among public and private providers. This would require more detailed clinical information that might only be possible by interviewing surgeons or accessing patient records. However, this line of inquiry could supplement the patient registries and outcomes assessments that are currently ongoing.35 It would be interesting to obtain statistics on the type of surgery selected in provinces where both AGB and RYGB are insured, assuming the objectivity of the information provided to patients about the procedures.
Conclusion
Canadian regulatory and professional bodies need to focus on the current predicament involving bariatric surgery. The availability of private AGB clinics has contributed to unequal access to bariatric surgery services among those who can afford to pay out of pocket for the surgery and those who can not, and there appear to be important differences in the structures and processes of care among both private and public facilities providing bariatric surgery. At a minimum, private clinics should be monitored to ensure safe delivery of care, including providing patients with accurate, objective information about bariatric surgery options and having appropriate patient eligibility processes and sufficient critical care support. It also is imperative that a wait time target be set for insured RYGB surgery, similar to other procedures, so that patients in all jurisdictions have timely access to this service.36 Addressing the lengthy wait times that still exist in some provinces would also help close the gap between private and public facilities. An alternative solution could be for provinces in addition to Alberta and New Brunswick to insure AGB. In this scenario, the selection of surgery type would be in the hands of both the patient and surgeon and would eliminate financial barriers.
We hope that the present comparison between AGB in private clinics and RYGB in public facilities informs future research and obesity treatment policy so that all Canadians can have equitable and timely access to proven, evidence-based care. With appropriate policy changes and modest funding increases, we envision a situation whereby publicly insured bariatric surgery within 1 year is available across Canada and delivered with the highest quality by specialized centres of excellence.
Acknowledgements
Dr. Bell is supported by a Canadian Institutes of Health Research and Canadian Patient Safety Institute chair in Patient Safety and Continuity of Care. The funding agencies had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. The corresponding author had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Competing interests: None declared.
Contributors: All authors helped design the study, analyzed the data, reviewed the article and approved its publication. Dr. Martin and Mr. Klemensberg acquired the data. Drs. Martin and Bell wrote the article.
See related commentary by Cobourn.
References
- 1.Abelson P, Kennedy D. The obesity epidemic. Science. 2004;304:1413. doi: 10.1126/science.304.5676.1413. [DOI] [PubMed] [Google Scholar]
- 2.Basrur S. 2004 Chief Medical Officer of Health Report. Healthy weights, healthy lives. Toronto (ON): Ministry of Health and Long-term Care; 2004. [Google Scholar]
- 3.Tjepkema M. Nutrition: findings from the Canadian Community Health Survey Adult obesity in Canada: measured height and weight. Ottawa (ON): Statistics Canada; 2004. [accessed 2008 Nov. 15]. Available: www.statcan.ca/english/research/82-620-MIE/2005001/articles/adults/aobesity.htm. [Google Scholar]
- 4.Ontario Medical Advisory Secretariat. Bariatric surgery. Health technology literature review. Toronto (ON): Ontario Ministry of Health and Long-term Care; 2005. [Google Scholar]
- 5.Snow V, Barry P, Fitterman N, et al. Pharmacologic and surgical management of obesity in primary care: a clinical practice guideline from the american college of physicians. Ann Intern Med. 2005;142:525–31. doi: 10.7326/0003-4819-142-7-200504050-00011. [DOI] [PubMed] [Google Scholar]
- 6.Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357:753–61. doi: 10.1056/NEJMoa066603. [DOI] [PubMed] [Google Scholar]
- 7.Tice JA, Karliner L, Walsh J, et al. Gastric banding or bypass? A systematic review comparing the two most popular bariatric procedures. Am J Med. 2008;121:885–93. doi: 10.1016/j.amjmed.2008.05.036. [DOI] [PubMed] [Google Scholar]
- 8.Ontario Health Technology Advisory Committee. OHTAC recommendation. Bariatric surgery. Toronto (ON): The Committee; January 21. 2005. 2005. [Google Scholar]
- 9.Clegg AJ, Colquitt J, Sidhu MK, et al. The clinical effectiveness and cost-effectiveness of surgery for people with morbid obesity: a systematic review and economic evaluation. Health Technol Assess. 2002;6:1–153. doi: 10.3310/hta6120. [DOI] [PubMed] [Google Scholar]
- 10.Clegg A, Colquitt J, Sidhu M, et al. Clinical and cost effectiveness of surgery for morbid obesity: a systematic review and economic evaluation [review] Int J Obes Relat Metab Disord. 2003;27:1167–77. doi: 10.1038/sj.ijo.0802394. [DOI] [PubMed] [Google Scholar]
- 11.Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 2004;240:416–23. doi: 10.1097/01.sla.0000137343.63376.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gallagher SF, Banasiak M, Gonzalvo JP, et al. The impact of bariatric surgery on the Veterans Administration healthcare system: a cost analysis. Obes Surg. 2003;13:245–8. doi: 10.1381/096089203764467144. [DOI] [PubMed] [Google Scholar]
- 13.Craig BM, Tseng DS. Cost-effectiveness of gastric bypass for severe obesity. Am J Med. 2002;113:491–8. doi: 10.1016/s0002-9343(02)01266-4. [DOI] [PubMed] [Google Scholar]
- 14.Sampalis JS, Liberman M, Auger S, et al. The impact of weight reduction surgery on health-care costs in morbidly obese patients. Obes Surg. 2004;14:939–47. doi: 10.1381/0960892041719662. [DOI] [PubMed] [Google Scholar]
- 15.Ontario Ministry of Health and Long-term Care. Backgrounder. Bariatric services in Ontario. Toronto (ON): The Ministry; August 16. 2007. 2007. [Google Scholar]
- 16.Robinson MK. Surgical treatment of obesity — weighing the facts. N Engl J Med. 2009;361:520–1. doi: 10.1056/NEJMe0904837. [DOI] [PubMed] [Google Scholar]
- 17.Maggard MA, Shugarman LR, Suttorp M, et al. Meta-analysis. Surgical treatment of obesity. Ann Intern Med. 2005;142:547–59. doi: 10.7326/0003-4819-142-7-200504050-00013. [DOI] [PubMed] [Google Scholar]
- 18.Smith SC, Edwards CB, Goodman GN, et al. Open vs laparoscopic Roux-en-Y gastric bypass: comparison of operative morbidity and mortality. Obes Surg. 2004;14:73–6. doi: 10.1381/096089204772787329. [DOI] [PubMed] [Google Scholar]
- 19.Garcia JA, Martinez M, Elia M, et al. Obesity surgery results depending on technique performed: long-term outcome. Obes Surg. 2009;19:432–8. doi: 10.1007/s11695-008-9762-x. [DOI] [PubMed] [Google Scholar]
- 20.Guller U, Klein LV, Hagen JA. Safety and effectiveness of bariatric surgery: Roux-en-Y gastric bypass is superior to gastric banding in the management of morbidly obese patients. Patient Saf Surg. 2009;3:10. doi: 10.1186/1754-9493-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Angrisani L, Lorenzo M, Borrelli V. Laparoscopic adjustable gastric banding versus Roux-en-Y gastric bypass: 5-year results of a prospective randomized trial. Surg Obes Relat Dis. 2007;3:127–32. doi: 10.1016/j.soard.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 22.Longitudinal Assessment of Bariatric Surgery (LABS) Consortium. Flum DR, Belle SH, King WC, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009;361:445–54. doi: 10.1056/NEJMoa0901836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.CBC News. Obesity surgery. Availability across the country [interactive map] [accessed 2010 May 4]. Available: www.cbc.ca/news/interactives/map-obesitysurgery/
- 24.Christou NV, Efthimiou E. Bariatric surgery waiting times in Canada. Can J Surg. 2009;52:229–34. [PMC free article] [PubMed] [Google Scholar]
- 25.Christou N, Efthimiou E. Bariatric surgery: waiting times too long in Canada. Medical News Today. 2009. June 5. [accessed 2009 July 21]. Available: www.medical-newstoday.com/articles/152612.php.
- 26.Padwal RS, Sharma AM. Treating severe obesity: morbid weights and morbid waits. CMAJ. 2009;181:777–8. doi: 10.1503/cmaj.081508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Health Canada. Canada Health Act Annual Report 2003–2004. Ottawa (ON): Canada Health Act Division, Health Canada; 2004. [accessed 2008 Sept. 28]. Available: http://www.hc-sc.gc.ca/hcs-sss/alt_formats/hpb-dgps/pdf/pubs/cha-lcs-ar-ra/2003-04-eng.pdf. [Google Scholar]
- 28.Madore O. Private diagnostic imaging clinics and the Canada Health Act. PRB 05-02E. Ottawa (ON): Parliamentary Information and Research Service, Library of Parliament; 2005. [accessed 2008 Sept. 28]. Available: http://dsp-psd.pwgsc.gc.ca/Collection-R/LoPBdP/PRB-e/PRB0502-e.pdf. [Google Scholar]
- 29.Birch DW, Biron S, Grace DM. 15. Surgical treatment of obesity. In: 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children. CMAJ. 2007;176(8 Suppl):Online-72–5. [Google Scholar]
- 30.Lett D. Private health clinics remain unregulated in most of Canada. CMAJ. 2008;178:986–7. doi: 10.1503/cmaj.080412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ontario Medical Association. Schedule of fees. Surgical procedures: operations on the digestive system. Toronto (ON): The Association; 2008. [Google Scholar]
- 32.CBC News. Ontario expands access to weight-loss surgery. February 23. 2009. [accessed 2009 Mar. 10]. Available: www.cbc.ca/health/story/2009/02/23/bariatric-ont.html.
- 33.Elkins G, Whitfield P, Marcus J, et al. Noncompliance with behavioural recommendations following bariatric surgery. Obes Surg. 2005;15:546–51. doi: 10.1381/0960892053723385. [DOI] [PubMed] [Google Scholar]
- 34.Toussi R, Fujioka K, Coleman KJ. Pre- and postsurgery behavioural compliance, patient health, and postbariatric surgical weight loss. Obesity (Silver Spring) 2009;17:996–1002. doi: 10.1038/oby.2008.628. [DOI] [PubMed] [Google Scholar]
- 35.Ontario Ministry of Health and Long-term Care. Ontario bariatric surgery study: request for proposals bariatric surgery study. [accessed 2009 Oct. 14]. Available: www.health.gov.on.ca/english/providers/ministry/research/docs/bariatricregistry_call_proposals_20090715.pdf.
- 36.Esmail N. Hold the applause, please: wait times for health care in Canada still too long. Fraser Forum. 2008. Dec, [accessed 2011 Jan. 10]. pp. 22–9. Available: www.fraserinstitute.org/WorkArea/DownloadAsset.aspx?id=2950.