Introduction
Older Americans, the most rapidly growing age group, are the least physically active1 and generate the highest health care expenditures.2 For example, older persons who were functionally dependent accounted for 46% of the health care expenditures, but only made up 20% of the older adult population 3. Additionally, they spent $5,000 more per year than people who remain independent. Physical activity (PA) may play an important role in maintain the health and physical function while reducing the health care burden.4 Recommendations of PA began in 1975 with The American College of Sports Medicine’s (ACSM) guidelines for exercise testing and prescription. While little space was devoted to PA in older adults, likely due to the limited amount of research, today a wealth of literature is available touting its benefits. Throughout the past two decades many obstacles have been overcome with adopting PA a safe and effective modality for improving physical capacity in older adults. Many questions still remain, one in which we attempt to address in this brief review is whether PA can maintain physical function in older adults?
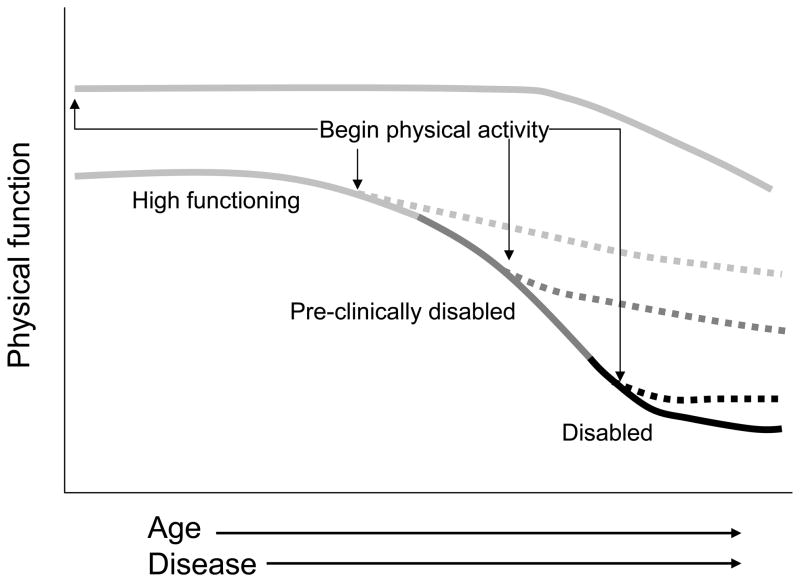
Physical activity has a myriad of effects that stem from physiological adaptations that may transfer to improvements in clinical outcomes such as reducing the risk of falls.5 The purpose of this article is to briefly review the current literature regarding whether PA can help maintain physical function in older adults and offer some suggestions for clinicians wanting to improve physical function with PA. As illustrated in Figure 1, individuals who begin a regular PA program early in life, and maintain this over the years will likely have high physical performance throughout the lifespan, although a decline in physical function is inevitable. Potentially more clinically relevant, is whether a PA program can set a person on a different trajectory over time (see curves in Figure 1). Although never formally tested in a clinical trial, scientists in the field anticipate that beginning a PA program can reset the normal trajectory of functional decline no matter what stage of disability. However, what will be gleaned from this review and others6, 7 is that while there is consistent support that various types of short-term PA programs improve physical capacity, very little is known whether PA can reduce the long-term incidence of physical disability.
Figure 1.
Physical function as viewed with increasing age and onset of disease. Physical activity (PA) is thought to impact physical function at many stages throughout life to change the trajectory of decline. Dotted lines represent new trajectory with beginning and maintaining a PA program Additionally, beginning a PA program at an early age may be associated with greater reserve capacity and a decline that occurs in later life.
Aging and physical function
Aging is clearly associated with a decline in most physiological systems that culminate to limit physical capacity. The cardiovascular and musculoskeletal systems have received the most attention as they are involved with the most basic functions of everyday life. Regarding the cardiovascular system, aging is associated with a dramatic decline in maximal aerobic performance that is due to a decrease in cardiac output (i.e. the delivery of oxygenated blood to muscles) and oxygen uptake at the muscle.8 Maximal strength is also reduced with age, which results from a combination of loss in muscle mass (also termed sarcopenia) and neural control.9 While it is commonly thought that high levels of PA can thwart the aging process, age-related changes continue to be evident despite life-long high intensity PA. For example, masters marathon runners 10 and power lifters 11 who continue to train 2–4 hours per day remain susceptible to physiological declines seen with age. However, it is likely that an individual who begins and maintains a PA program throughout the lifespan will have a greater reserve capacity to maintain high function into late-life (Figure 1). The age-related decline in physiological systems becomes clinically and socially relevant when they impact societal roles and expectations that feed the pathway to disablement.12
Evidence for physical activity and improved physical function
Epidemiological studies have clearly demonstrated a dose-response pattern for PA that is associated with a lower risk of physical limitations.13–15 Additionally, many small studies have reported beneficial effects of PA on physical capacity and precursors of physical disability.16–19 For example, chronic resistance and aerobic exercise increase muscle strength, aerobic capacity and bone density.20–23 This effect even occurs in frail elderly24, 25 and in persons with specific diseases highly associated with disability (i.e. osteoarthritis and cardiovascular disease).26, 27 Specifically, resistance training has a moderate to large effect on muscle strength with similar findings on endurance due to aerobic exercise. These effects do seem to transfer to functional activities such as sit-to-stand, stair climbing and walking tasks.19, 21, 26, 28
It remains unclear whether improvements in physical function can lead to lower rates of disability.6 Older disabled older adults with osteoarthritis who were enrolled into The Fitness Arthritis and Seniors Trial (FAST) and underwent a 1.5 year PA program (aerobic or resistance training) showed modest improvements in disability, physical function and pain.29 Additional evidence suggests that PA may reduce the incidence of disability as Penninx and coworkers found that older adults free of limitations in the FAST study and who participated in the intervention program were approximately 40% less likely to develop incident disability than controls.30
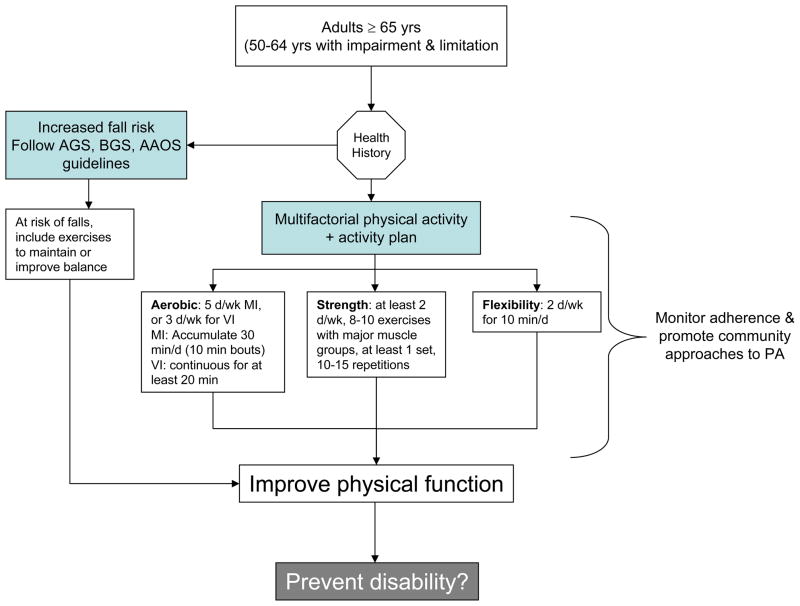
Emerging evidence for the effects of PA on markers of disability comes from the LIFE-P study where 424 sedentary persons at risk of disability were randomized to a 12 month PA program or health education control group. For example, scores on the short physical performance battery (SPPB) improved with PA while the successful aging education control group demonstrated no change. Considering that SPPB scores are consistently associated with incident disability in older adults, the improvement in SPPB scores >1 point suggests a meaningful change that may transition into reduced disability. Additionally, time until major mobility disability, defined as the incidence of not being able to complete the 400 meter walk, showed a strong trend toward reduction PA group (see hazard ratios in figure 2). Further research with a longer follow-up time is needed to definitely conclude on the effects of PA on the onset of disability.
Figure 2.
Cumulative hazard of time until major mobility disability and until major mobility disability according to randomized groups [PA or a Successful Aging (SA) health education control group] in the LIFE-P study. (HR = hazard ratio; CI = confidence interval).
Consistent with the findings presented in the review noted above, The Surgeon General’s report on PA points to “promising evidence” that exercise in older adults may preserve the ability to maintain independent living. While this statement relies on clinical trial evidence regarding the effects of exercise on impairments such as decreased strength and balance, evidence supporting the beneficial effects of exercise on maintenance of physical function with PA is primarily based on observational studies.
Physical activity recommendations for older adults
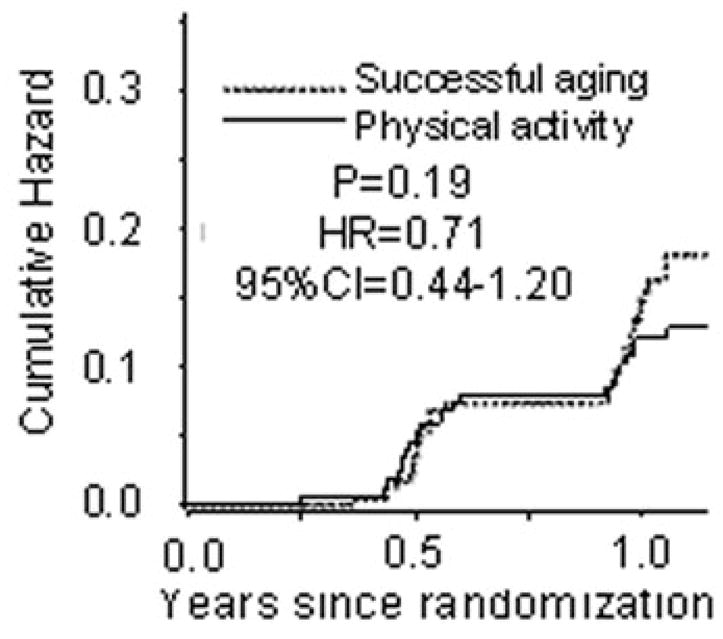
In 1995, The ACSM and Centers for Disease Control issued a preventative recommendation that “Every US adult should accumulate 30 minutes or more of moderate-intensity physical activity on most, preferably all, days of the week.”31 The recommendations are identical to those from the World Health Organization (WHO) Regional Office for Europe. ACSM and the American Heart Association (AHA) have recently amended these recommendations32 and made separate ones for all adults aged ≥65 yr and adults age 50–64 yr with clinically significant disease impairments and limitations.33 The WHO recommendations have remained the same.34 Because of the diverse disease etiology in older adults, a global recommendation is difficult to completely embrace. This difficulty is partly related to potential safety concerns in this diverse group, but it is becoming clear that the types and intensity of exercise being recommended are relatively safe in older adults and serious adverse events in clinical trials are rare.35, 36 The ACSM/AHA recommends that older adults take a multifactorial approach to PA by performing aerobic, strength, and flexibility exercise (An decision algorithm with an exercise prescription is outlined in Figure 2). Additionally, older adults should have an activity plan that incorporates each category of activity, but also they should consider how, when and where PA will be performed. For example, sedentary individuals should begin by performing shorter bouts of activity and gradually move toward performing more continuous bouts of activity.
Emerging areas of research
Physical activity represents an extremely promising intervention; yet evidence for prevention of mobility and outright disability remains inconclusive,6 deriving only from secondary data analyses.37 Many cross-sectional and a few longitudinal studies have documented a clear association between PA and onset of disability. Additionally, dozens of studies demonstrate that older adults have a high propensity to improve upon physiological properties underlying disability (i.e. muscle strength and aerobic capacity) despite the occurrence of disease conditions.38, 39 These studies typically assess continuous measures of function that are sensitive indicators of the physiologic effects of interventions that have been useful for guiding the refinement of exercise interventions. However, it is imperative to adopt an objectively measured outcome that discriminates between being able or unable to perform a critical task of daily living. As an example, the findings from the Diabetes Prevention Program (DPP) offered definitive evidence that a lifestyle intervention could prevent the onset of diabetes, rather than just improving the continuous measure of blood sugar.141 One such outcome for disability has been proposed in the LIFE-P study. Major mobility disability, characterized as inability to walk 400 m, fits a description that encompasses important aspects of independent living and can be objectively measured. Additionally, unlike continuous measures of physical function that often improve with short duration of PA, a long follow-up time will be needed to assess when older individuals are unable to walk 400 m. Development of outcomes, such as major mobility disability, is an emerging area of research to move the field forward and create a clear message for public health and clinical practice.
In preparation for developing PA guidelines from the Department of Health Human Services, an advisory committee reported on the evidence on PA for improving health of Americans (Download report at http://www.health.gov/PAGuidelines/). The report includes a chapter dedicated to the functional health of older adults and reviews the literature related to PA for reducing the incidence of disability in older adults. The development of such guidelines is important step in recognizing the importance of PA in older adults and is thought to spearhead future investigations to identify ideal programs to maintain functional health in older adults.
An active research program aimed at discovering better PA methodologies to improve physical function remains ongoing. Leading the way are scientists interested in not only improving cardiovascular and musculoskeletal systems through traditional based exercise programs, but also incorporating task-specific exercise (TSE). TSE, which involves practicing tasks of everyday life in a progressively challenging manner has shown recent success at improving function as it incorporates task specificity and highlights the neural control of movement.40–44 As recently demonstrated in a clinical trial conducted by de Vreede and colleagues, a TSE program in healthy older adults resulted in enhanced physical function and muscle power without adaptation in maximal strength.43 This was contrary to results in the resistance training arm where individuals showed little change in physical function yet substantially increased their maximal force production. More importantly, a revaluation of participants 6 months after discontinuation of training showed that the TSE group maintained their physical function while the resistance trained group returned to baseline levels. Research into other modalities of exercise, such as TSE training, may lead to more effective interventions to maintain independence on tasks commonly encountered throughout the day.
Recommendation for the clinician
While there is no clear evidence that the current recommendations maintain physical function in older adults, many studies have demonstrated a robust effect of PA on acute improvements in physical function. It is thought that these acute improvements may alter the trajectory of decline in physical capacity in hopes of maintaining physical function into late-life. Using the current recommendations as a guideline, clinicians are encouraged to follow the algorithm illustrated in figure 3 as a guideline for maintain physical function. This algorithm highlights the ACSM/AHA current recommendations that older adults should be encouraged to perform moderate intensity aerobic PA for a minimum of 30 minutes on five days each week or vigorous intensity aerobic PA for a minimum of 20 minutes three days per week.33 This dose can be accumulated in sessions of 10 minutes or more. Additionally, older adults should perform at least two nonconsecutive days of moderate to high intensity resistance training each week. Additional pieces of figure 3 are to assess an individuals’ health history, monitor adherence and promote community approaches to PA. The assessment of health history can be performed using the Physical Activity Readiness Questionnaire (PAR-Q).45, but clinicians are encouraged to asses fall risk that leads to a separate exercise prescription as outlined by the guidelines to prevent falls in older adults.5 Future research will determine whether the current recommendations will maintain physical function that prevents physical disability in older adults.
Figure 3.
Algorithm summarizing the ACSM/AHA current recommendations for physical activity in older adults to improve physical function and potentially to prevent physical disability. Clinicians are encouraged to assess health history is guiding the exercise prescription for improving physical function. Moderate intensity (MI) exercise should be gauged as a 5–6 on a 10 point effort scale (0 = sitting & 10 = all-out effort). Vigorous intensity (VI) exercise should be a 7 or 8 on this same scale.
References
- 1.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008 Jan;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 2.Rice DP, Fineman N. Economic implications of increased longevity in the United States. Annu Rev Public Health. 2004;25:457–473. doi: 10.1146/annurev.publhealth.25.101802.123054. [DOI] [PubMed] [Google Scholar]
- 3.Fried TR, Bradley EH, Williams CS, Tinetti ME. Functional disability and health care expenditures for older persons. Arch Intern Med. 2001;161(21):2602–2607. doi: 10.1001/archinte.161.21.2602. [DOI] [PubMed] [Google Scholar]
- 4.Wang G, Pratt M, Macera CA, Zheng ZJ, Heath G. Physical activity, cardiovascular disease, and medical expenditures in U.S. adults. Ann Behav Med. 2004 Oct;28(2):88–94. doi: 10.1207/s15324796abm2802_3. [DOI] [PubMed] [Google Scholar]
- 5.Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J Am Geriatr Soc. 2001 May;49(5):664–672. [PubMed] [Google Scholar]
- 6.Keysor JJ. Does late-life physical activity or exercise prevent or minimize disablement? A critical review of the scientific evidence. Am J Prev Med. 2003 Oct;25(3 Suppl 2):129–136. doi: 10.1016/s0749-3797(03)00176-4. [DOI] [PubMed] [Google Scholar]
- 7.Keysor JJ, Jette AM. Have we oversold the benefit of late-life exercise? J Gerontol A Biol Sci Med Sci. 2001 Jul;56(7):M412–423. doi: 10.1093/gerona/56.7.m412. [DOI] [PubMed] [Google Scholar]
- 8.Skinner J, Tipton C, Vailas A. Exercise, physical training and the aging process. In: Viidik A, editor. Lectures on Gerontology. 1B. London: Academic; 1982. pp. 407–439. [Google Scholar]
- 9.Clark BC, Manini TM. Sarcopenia != Dynapenia. J Gerontol A Biol Sci Med Sci. 2008 Aug;63(8):829–834. doi: 10.1093/gerona/63.8.829. [DOI] [PubMed] [Google Scholar]
- 10.Costill DL, Winrow E. Maximal oxygen intake among marathon runners. Arch Phys Med Rehabil. 1970 Jun;51(6):317–320. [PubMed] [Google Scholar]
- 11.The DJ, Ploutz-Snyder L. Age, body mass, and gender as predictors of masters olympic weightlifting performance. Med Sci Sports Exerc. 2003 Jul;35(7):1216–1224. doi: 10.1249/01.MSS.0000074582.55220.1C. [DOI] [PubMed] [Google Scholar]
- 12.Grembowski D, Patrick D, Diehr P, et al. Self-efficacy and health behavior among older adults. J Health Soc Behav. 1993 Jun;34(2):89–104. [PubMed] [Google Scholar]
- 13.He XZ, Baker DW. Body mass index, physical activity, and the risk of decline in overall health and physical functioning in late middle age. Am J Public Health. 2004 Sep;94(9):1567–1573. doi: 10.2105/ajph.94.9.1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hillsdon MM, Brunner EJ, Guralnik JM, Marmot MG. Prospective study of physical activity and physical function in early old age. Am J Prev Med. 2005 Apr;28(3):245–250. doi: 10.1016/j.amepre.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 15.Leveille SG, Guralnik JM, Ferrucci L, Langlois JA. Aging successfully until death in old age: opportunities for increasing active life expectancy. Am J Epidemiol. 1999 Apr 1;149(7):654–664. doi: 10.1093/oxfordjournals.aje.a009866. [DOI] [PubMed] [Google Scholar]
- 16.Brandon JL, Boyett LW, Gasch DA, Lloyd A. Effects of Lower Extermity Strength Training on Functional Mobility in Older Adults. J Aging Phys Activity. 2000;8:214–227. [Google Scholar]
- 17.Vincent KR, Braith RW, Feldman RA, Kallas HE, Lowenthal DT. Improved cardiorespiratory endurance following 6 months of resistance exercise in elderly men and women. Arch Intern Med. 2002 Mar 25;162(6):673–678. doi: 10.1001/archinte.162.6.673. [DOI] [PubMed] [Google Scholar]
- 18.Morganti CM, Nelson ME, Fiatarone MA, et al. Strength improvements with 1 yr of progressive resistance training in older women. Med Sci Sports Exerc. 1995;27(6):906–912. [PubMed] [Google Scholar]
- 19.Manini T, Marko M, VanArnam T, et al. Efficacy of resistance and task-specific exercise in older adults who modify tasks of everyday life. J Gerontol A Biol Sci Med Sci. 2007 Jun;62(6):616–623. doi: 10.1093/gerona/62.6.616. [DOI] [PubMed] [Google Scholar]
- 20.Kelley GA, Kelley KS, Tran ZV. Resistance training and bone mineral density in women: a meta-analysis of controlled trials. Am J Phys Med Rehabil. 2001 Jan;80(1):65–77. doi: 10.1097/00002060-200101000-00017. [DOI] [PubMed] [Google Scholar]
- 21.Latham N, Anderson C, Bennett D, Stretton C. Progressive resistance strength training for physical disability in older people. Cochrane Database Syst Rev. 2003;(2):CD002759. doi: 10.1002/14651858.CD002759. [DOI] [PubMed] [Google Scholar]
- 22.Lemura LM, von Duvillard SP, Mookerjee S. The effects of physical training of functional capacity in adults. Ages 46 to 90: a meta-analysis. J Sports Med Phys Fitness. 2000 Mar;40(1):1–10. [PubMed] [Google Scholar]
- 23.Wolff I, van Croonenborg JJ, Kemper HC, Kostense PJ, Twisk JW. The effect of exercise training programs on bone mass: a meta-analysis of published controlled trials in pre- and postmenopausal women. Osteoporos Int. 1999;9(1):1–12. doi: 10.1007/s001980050109. [DOI] [PubMed] [Google Scholar]
- 24.Fiatarone MA, Marks EC, Ryan ND, Meredith CN, Lipsitz LA, Evans WJ. High-intensity strength training in nonagenarians. Effects on skeletal muscle. JAMA. 1990;263(22):3029–3034. [PubMed] [Google Scholar]
- 25.Fiatarone MA, O'Neill EF, Ryan ND, et al. Exercise training and nutritional supplementation for physical frailty in very elderly people. N Engl J Med. 1994;330(25):1769–1775. doi: 10.1056/NEJM199406233302501. [DOI] [PubMed] [Google Scholar]
- 26.Messier SP, Miller GD, Morgan TP, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the Arthritis, Diet and Activity Promotion Trial (ADAPT) Arthritis and Rheumatism. 2004;50:1501–1510. doi: 10.1002/art.20256. [DOI] [PubMed] [Google Scholar]
- 27.Messier SP, Royer TD, Craven TE, O'Toole ML, Burns R, Ettinger WH., Jr Long-term exercise and its effect on balance in older, osteoarthritic adults: results from the Fitness, Arthritis, and Seniors Trial (FAST) J Am Geriatr Soc. 2000;48(2):131–138. doi: 10.1111/j.1532-5415.2000.tb03903.x. [DOI] [PubMed] [Google Scholar]
- 28.Pahor M, Blair SN, Espeland M, et al. Effects of a physical activity intervention on measures of physical performance: Results of the lifestyle interventions and independence for Elders Pilot (LIFE-P) study. J Gerontol A Biol Sci Med Sci. 2006 Nov;61(11):1157–1165. doi: 10.1093/gerona/61.11.1157. [DOI] [PubMed] [Google Scholar]
- 29.Ettinger WH, Jr, Burns R, Messier SP, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST) JAMA. 1997;277(1):25–31. [PubMed] [Google Scholar]
- 30.Penninx BW, Messier SP, Rejeski WJ, et al. Physical exercise and the prevention of disability in activities of daily living in older persons with osteoarthritis. Arch Intern Med. 2001;161(19):2309–2316. doi: 10.1001/archinte.161.19.2309. [DOI] [PubMed] [Google Scholar]
- 31.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273(5):402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 32.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007 Aug;39(8):1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 33.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007 Aug 28;116(9):1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- 34.Organization TROfEotWH. Steps to health: A European framework to promote physical activity for health. Copenhagen: Scherfigsvej; 2007. [Google Scholar]
- 35.Gordon NF, Kohl HW, 3rd, Pollock ML, Vaandrager H, Gibbons LW, Blair SN. Cardiovascular safety of maximal strength testing in healthy adults. Am J Cardiol. 1995 Oct 15;76(11):851–853. doi: 10.1016/s0002-9149(99)80245-8. [DOI] [PubMed] [Google Scholar]
- 36.Pollock ML, Franklin BA, Balady GJ, et al. AHA Science Advisory. Resistance exercise in individuals with and without cardiovascular disease: benefits, rationale, safety, and prescription: An advisory from the Committee on Exercise, Rehabilitation, and Prevention, Council on Clinical Cardiology, American Heart Association; Position paper endorsed by the American College of Sports Medicine. Circulation. 2000 Feb 22;101(7):828–833. doi: 10.1161/01.cir.101.7.828. [DOI] [PubMed] [Google Scholar]
- 37.Penninx BW, Messier SP, Rejeski WJ, et al. Physical exercise and prevention of ADL disability in older persons with osteoarthritis. Arch Intern Med. 2001;161:2309–2316. doi: 10.1001/archinte.161.19.2309. [DOI] [PubMed] [Google Scholar]
- 38.Binder EF, Brown M, Sinacore DR, Steger-May K, Yarasheski KE, Schechtman KB. Effects of extended outpatient rehabilitation after hip fracture: a randomized controlled trial. Jama. 2004 Aug 18;292(7):837–846. doi: 10.1001/jama.292.7.837. [DOI] [PubMed] [Google Scholar]
- 39.Binder EF, Schechtman KB, Ehsani AA, et al. Effects of exercise training on frailty in community-dwelling older adults: results of a randomized, controlled trial. J Am Geriatr Soc. 2002 Dec;50(12):1921–1928. doi: 10.1046/j.1532-5415.2002.50601.x. [DOI] [PubMed] [Google Scholar]
- 40.Alexander NB, Galecki AT, Grenier ML, et al. Task-specific resistance training to improve the ability of activities of daily living-imparied older adults to rise from a bed and from a chair. Journal of the American Geriatric Society. 2001;49:1418–2001. doi: 10.1046/j.1532-5415.2001.4911232.x. [DOI] [PubMed] [Google Scholar]
- 41.Bean J, Herman S, Kiely DK, et al. Weighted stair climbing in mobility-limited older people: a pilot study. J Am Geriatr Soc. 2002;50(4):663–670. doi: 10.1046/j.1532-5415.2002.50160.x. [DOI] [PubMed] [Google Scholar]
- 42.Bean JF, Herman S, Kiely DK, et al. Increased Velocity Exercise Specific to Task (InVEST) training: a pilot study exploring effects on leg power, balance, and mobility in community-dwelling older women. J Am Geriatr Soc. 2004 May;52(5):799–804. doi: 10.1111/j.1532-5415.2004.52222.x. [DOI] [PubMed] [Google Scholar]
- 43.de Vreede PL, Samson MM, van Meeteren NL, Duursma SA, Verhaar HJ. Functional-task exercise versus resistance strength exercise to improve daily function in older women: a randomized, controlled trial. J Am Geriatr Soc. 2005 Jan;53(1):2–10. doi: 10.1111/j.1532-5415.2005.53003.x. [DOI] [PubMed] [Google Scholar]
- 44.Manini TM, Marko M, Van Arnam T, et al. Efficacy of resistance and task-specific exercise in older adults who modify tasks of everyday life. Journals of Gerontology: Medical Sciences. 2007;62:616–623. doi: 10.1093/gerona/62.6.616. [DOI] [PubMed] [Google Scholar]
- 45.Thomas S, Reading J, Shephard RJ. Revision of the Physical Activity Readiness Questionnaire (PAR-Q) Can J Sport Sci. 1992 Dec;17(4):338–345. [PubMed] [Google Scholar]