Abstract
We now stand at a critical juncture for rheumatic fever (RF) and rheumatic heart disease (RHD) control. In recent years, we have seen a surge of interest in these diseases in regions of the world where RF/RHD mostly occur. This brings real opportunities to make dramatic progress in the next few years, but also real risks if we miss these opportunities. Most public health and clinical approaches in RF/RHD arose directly from programmes of research. Many unanswered questions remain, including those around how to implement what we know will work, so research will continue to be essential in our efforts to bring a global solution to this disease. Here we outline our proposed research priorities in RF/RHD for the coming decade, grouped under the following four challenges: Translating what we know already into practical RHD control; How to identify people with RHD earlier, so that preventive measures have a higher chance of success; Better understanding of disease pathogenesis, with a view to improved diagnosis and treatment of ARF and RHD; and Finding an effective approach to primary prevention. We propose a mixture of basic, applied, and implementation science. With concerted efforts, strong links to clinical and public health infrastructure, and advocacy and funding support from the international community, there are good prospects for controlling these RF and RHD over the next decade.
Keywords: Rheumatic fever, rheumatic heart disease, prevention
INTRODUCTION
We now stand at a critical juncture for rheumatic fever (RF) and rheumatic heart disease (RHD) control. There have been three surges of activity in RF/RHD research and control over the past half-century. The first began in North America and Europe in the mid-20th Century, during which we learned most of what we now know about primary and secondary prevention. This was followed by more global interest during the late 20th Century, when the World Health Organization (WHO) and the International Society and Federation of Cardiology (subsequently known as the World Heart Federation, WHF) established their Global Programme on Rheumatic Fever and Rheumatic Heart Disease (which was disbanded in 2001) and the WHO established their network of Streptococcal Collaborating Centres. The first decade of the 21st Century saw RF/RHD research and control steadily recede from the global public health agenda. During this time, support for the development of a group A streptococcal (GAS) vaccine was downgraded in priority by the WHO and the Bill and Melinda Gates Foundation, and the WHO, aside from producing an update of their excellent reference document about RF/RHD (Technical Resource Series document 923)[1] and supporting some research around treatment of streptococcal pharyngitis,[2] has been notably inactive in this field. A review of the WHO's activities in controlling GAS diseases (by one of us--Carapetis) in 2004[3–5] produced a number of recommendations for mobilizing the WHO in this field, but none of these were implemented.
Despite this, we are currently witnessing a new surge in activity, which differs from those in the 20th Century in that it is largely driven from parts of the world where RF/RHD mostly occur. Research, as well as public health programmes and political advocacy, are now centered in developing countries and those subpopulations within middle- and high-income countries where high burdens of disease still exist (in these latter categories, we give as examples the work happening in poorer regions of Brazil and South Africa and the indigenous populations of Australia and New Zealand). This has been a long time coming. The leading institution in global RF pathogenesis research is now in Brazil; a new African approach to RHD control (called ASAP--Advocacy, Surveillance, Awareness, and Prevention[6]) involves many countries and is led out of South Africa; programmes to promote surgery and screening for RHD are being established in Mozambique, Rwanda, and Ethiopia; there is a new RF/RHD partnership between India, South Africa, and Brazil; a world-leading programme of RHD control in Pacific Island nations has individuals from Tonga, Fiji, and Samoa at the helm; in India, numerous people are working to advance the field, and the list goes on.
This activity is also having an effect on global organizations. Since the early 2000s, the WHF has made a major commitment to leading the charge on RHD control, taking the mantle from the WHO, and supporting programmes in the Pacific, Africa, establishing an international web-based resource in RF/RHD (RHDnet – see (www.worldheart.org/rhd) and in their most recent strategic plan, committing to “Eliminating rheumatic fever and minimizing the burden of rheumatic heart disease.” But even the WHO appears to be listening; for example, the next step in progressing the global effort to produce a GAS vaccine will be a workshop hosted by WHO in June 2011.
So, it seems that are real opportunities to make dramatic progress in the next few years, but also real risks if we miss these opportunities. The challenge is to use this renewed attention to demonstrate what we have been saying all along--that RF/RHD can be controlled if only we can raise awareness, undertake advocacy, and mobilize political will. The funding required is relatively meager by international standards--most RHD control programmes can be run for only a fraction of the cost of performing heart valve surgery on severe RHD patients.[7]
It is also important that we do not claim to have all of the answers, and thus ignore the importance of research. Indeed, most public health and clinical approaches in RF/RHD arose directly from programmes of research. Many unanswered questions remain, including those around how to implement what we know will work, so research will continue to be essential in our efforts to bring a global solution to this disease.
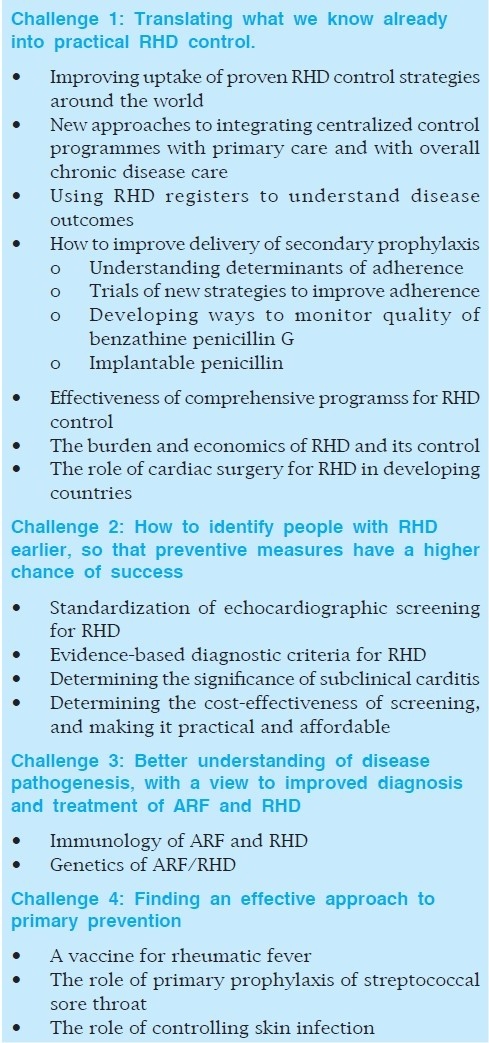
Here, we present a summary of the four major challenges that need to be addressed in the next decade (see Table 1). We note that little of this is new, and indeed many of these topics are already being tackled by individuals and consortia around the world. If we do all this, there is a good chance that we will dramatically reduce the burden of both ARF and RHD, foment a global approach that allows countries to learn from each others’ experiences, increasingly place RHD control on the international agenda, and progress GAS vaccine development to the point where we move to clinical trials of promising combination vaccines.
TABLE 1.
GLOBAL RESEARCH PRIORITIES IN RHEUMATIC FEVER AND RHEUMATIC HEART DISEASE
CHALLENGE 1: TRANSLATING WHAT WE KNOW ALREADY INTO PRACTICAL RHD CONTROL
Improving uptake of proven rheumatic heart disease control strategies around the world
It is universally accepted that the most cost-effective approach to RHD control is delivery of secondary prophylaxis and improved clinical care of ARF/RHD patients using register-based RHD control programs.[1,8] Yet, despite the WHO and the WHF recommending these strategies, there has yet to be established a sustained, national program in any developing country. There are examples of successful RHD control programs in some jurisdictions within countries (e.g., the Pinar del Rio region of Cuba,[1,8] and around Chandigarh in northern India[9]). There have also been excellent examples of implementation of register-based control programs as components of broader “comprehensive” strategies (e.g., the French Caribbean[10]).
Yet, currently, there are only two large countries that continue to implement register-based RHD control programs widely. New Zealand introduced RHD registers more than two decades ago, with considerable success, leading to dramatic reductions in the rate of acute rheumatic fever (ARF) recurrences.[11] Australia introduced a National RF Strategy in 2009, which includes core national funding for control programme staff in key jurisdictions and the unique approach of a national coordination unit.
The progress in Pacific countries shows promise. With the help of the WHF, Fiji and Tonga have established RHD control programmes that are now embedded as part of the health structure and have the right ingredients for long-term sustainability. The challenge is to understand better how to fast-track the uptake of RHD control programmes in other developing countries.
This is a form of implementation science, and explores the boundaries between research and advocacy. It could be seen as having two components: The creation of a global RHD agenda, and construction of a platform for information sharing between affected countries. The key elements will include establishing the need for a control strategy by demonstrating disease burden and the potential benefits of a preventive approach; communicating the evidence that proves the value of the control approach to key decision makers using appropriate and effective channels; and ensuring that there is adequate support (technical support, resources such as registers and educational materials, and reliable supplies of high quality penicillin) for countries that choose to implement control strategies.
New approaches to integrating centralized control programmes with primary care and with overall chronic disease care
RHD control programmes currently undertake little in the way of preplanned interactions with primary care staff. So far, nobody has outlined the most effective way that programme staff can provide support to primary care staff that improves service delivery. Moreover, in a world where the artificial dichotomy between vertical and horizontal programmes can be constraining, we need models of “diagonal” programming, whereby the essential centralized component that monitors and promotes RHD care can integrate with more horizontal chronic and noncommunicable disease care on the ground, particularly in health centers, and possibly including community-based care through the roles of community health workers and/or noncommunicable disease nurses.
Using rheumatic heart disease registers to understand disease outcomes
With a few exceptions, the paucity of population-based RF/RHD data found in the previous attempts at measuring the global disease burden persists today.[12,13] More widespread, and better used, RHD register data would allow us to construct sequential cohorts to track mortality, morbidity (including levels of heart failure, severity on echo, ARF recurrences), and outcomes of valve surgery, analyzed by age group, presence of carditis or chorea at presentation, level of RHD severity at presentation, and location and level of adherence to benzathine penicillin G (BPG).
How to improve delivery of secondary prophylaxis
Although there is evidence that establishing register-based control programmes will, in itself, lead to improved adherence with secondary prophylaxis regiments, we are still largely ignorant of the specific ways to dramatically improve the proportion of scheduled benzathine penicillin G injections that are actually delivered. There are remarkably few studies of this. Some subthemes here are as follows:
Understanding determinants of adherence
We need qualitative and quantitative research to better understand perceptions and knowledge of patients, families, and health staff about ARF/RHD and secondary prophylaxis, and practices used by staff and local health systems to deliver care, beyond the small studies available to date.[14,15]
Trials of new strategies to improve adherence
Promising strategies from the above studies could then be trialled at the primary care level. There will likely be a range of designs, depending on the setting and level of health center. Where possible, we need controlled trials which could be in the form of staged rollouts (e.g., stepped-wedge designs) or randomized controlled trials. Some elements that, based on current knowledge, could be considered include (either stand-alone or in combination) implementation of continuous quality improvement approaches,[16] allocating responsibility for RHD care to particular primary health center staff, streamlining care in clinics so that people are not kept waiting for routine injections, implementing an active recall process (which might include mobile phones or text messages), using information technology to track patients from mobile populations in order to continue prophylaxis at other centers, delivering BPG injections in homes and schools, intensive training for health center staff on RHD management including pain-minimizing injection techniques, patient empowerment strategies such as hand-held records or prescriptions, and use of community mobilization (including community workers, patient support groups).
Developing ways to monitor quality of benzathine penicillin G. There are problems with both the consistency of supply and quality of benzathine penicillin G around the world. There are a number of studies documenting that different batches from suppliers may have variable pharmacokinetic properties, and the batches may vary physically (e.g., some are very difficult to draw up into a syringe and administer).[17–21] It is clear that many forms of benzathine penicillin G presently used around the world do not reliably lead to adequate serum penicillin levels after 28 days. The consequence of this problem is that people continue to have recurrences of ARF despite adhering to regular benzathine penicillin G injections. It is not clear that there are clear global guidelines or standards for the manufacture of this medication, or that there are mechanisms for assuring the quality of the product. Benzathine penicillin G is on the Core List of Essential Medicines for developing countries, so it is critical that we find a solution to this problem.
Implantable penicillin
An implantable form of penicillin could be a major advance. Naltrexone implants provide a promising model, given that the equivalent daily dose is similar to what would be required for penicillin.[22] There would be no problem recruiting participants in clinical trials of a penicillin implant, given the hundreds of thousands of patients around the world currently receiving 3- or 4-weekly benzathine penicillin G injections.
Effectiveness of comprehensive programmes for rheumatic heart disease control
Successful comprehensive strategies overseas have included registers, support to improve clinical care and delivery of secondary prophylaxis, emphasis on primary prevention (sore throat and skin sore treatment), raising awareness of the symptoms of ARF and the need to seek medical care, improving knowledge of ARF/RHD, their management, and control among health staff, and broad awareness campaigns in the general community.[10,23] This comprehensive approach has never been tried in most countries, and requires widespread implementation and evaluation, particularly to determine the cost, cost-effectiveness, practicality, and sustainability of scaling-up programmes beyond individual communities and small regions.
The burden and economics of RHD and its control
To date, there have been only two economic analyses of RHD control, both conducted by the same World Bank group, relying largely on data collected in the USA in the mid-20th century.[24,25] We need comprehensive disease burden estimates (using DALYs) and thorough analyses of the costs of ARF/RHD to model the cost-benefit and cost-effectiveness of different approaches to RF/RHD control. The results will not only be valuable for health policy making and service planning (including planning for GAS vaccines), but will also be adapted into a simple costing model for more widespread use in developing countries.
The role of cardiac surgery for RHD in developing countries
Middle-income countries such as South Africa, India, and Brazil have a growing capacity for cardiac surgery as well as capabilities to assist lower-income countries to operate on RHD patients. The availability of in-country cardiac surgery is increasing in some lower-income countries as well. In addition, prosthetic valve replacement potentially carries with it significant morbidity and mortality, with devastating complications occurring due to infection, and hemorrhage or thrombosis related to difficulties in managing anticoagulant therapy.[26–28] There are two categories of further work raised by these issues,:
How to improve the availability and long-term outcomes of life-saving cardiac surgery for RHD in resource-poor settings, including outlining the most effective forms of surgical (and nonsurgical) interventions, and improving ongoing management to reduce complication rates.
How to ensure that valuable resources are not devoted mainly to cardiac surgical treatments at the expense of public health-focused prevention and control programmes. There are many countries that devote substantial proportions of their health and aid budgets to surgical treatments for patients with severe RHD, yet do not have effectively functioning RHD prevention and control programmes in order to reduce the flow of new candidates for surgery.[7] We have heard some claim that an initial focus on cardiac surgery can be a mechanism for interesting policy makers and donors in the RF/RHD issue, with a view to subsequently leveraging further support for prevention programmes. Successes in this approach need to be documented, if it is to continue to be argued.
CHALLENGE 2: HOW TO IDENTIFY PEOPLE WITH RHD EARLIER, SO THAT PREVENTIVE MEASURES HAVE A HIGHER CHANCE OF SUCCESS
It is the unfortunate reality that most new patients entered onto ARF/RHD registers have already developed significant rheumatic valvular lesions. A major challenge, therefore, is to identify people with RHD early in the natural history of their illness, during a phase that often lasts many years when most cases are asymptomatic, so that preventive measures (secondary prophylaxis) can be instituted with the greatest effect. It is known that secondary prophylaxis delivered to people with mild RHD results in the vastmajority having no detectable disease 5 to 10 years later.[29,30] The only way to identify asymptomatic cases is to conduct screening. We and others are increasingly demonstrating that echocardiographic screening is preferable to auscultation,[31–33] but many unanswered questions remain before this can be routinely advocated.
Standardization of echocardiographic screening for rheumatic heart disease
There is currently an international collaboration founded on a process used by the WHO to standardize the reading of chest radiographs to diagnose pneumonia.[34] The aim is to share screening echocardiograms through a web-based interface, to compare interpretations by cardiologists and others around the world, with a view to making echo reading as objective as possible. The aim is for all echo readers to undergo training using a standard set of echocardiograms and agreed diagnostic criteria, with measurement of inter- and intraobserver variability before proceeding to read new screening echocardiograms.
Evidence-based diagnostic criteria for rheumatic heart disease
In 2005, a joint NIH-WHO working group developed standardized surveillance protocols for GAS diseases, which included a diagnostic definition of RHD on echocardiogram (see http://www3.niaid.nih.gov/topics/streptococcal/default.htm). This was a consensus definition based on opinion of an expert group, because of the absence of data. Since that time, however, there have been studies in which large numbers of children have undergone echocardiography in Australia, Fiji, New Zealand, South Africa, Mali, Nicaragua, Cambodia, and Mozambique.[31–33] The global collaboration needs to consolidate these data to develop evidence-based diagnostic criteria for RHD on echo.
Determining the significance of subclinical carditis
There is concern that the extremely high rates of subclinical RHD being found in some studies--often ten times more that found by relying on the presence of a significant cardiac murmur--has not been proven to represent true RHD, and that expansion of screening before this question is answered may lead to thousands of healthy children being offered long-term secondary prophylaxis. Conversely, this may indeed represent a massive undetected burden of RHD, but we have no confirmation that these cases are truly part of the spectrum of clinical RHD, that they may potentially progress to clinical disease, and that they would benefit from secondary prophylaxis. To provide this information, an international collaboration is needed to follow-up children with subclinical carditis detected in the current round of screening studies to determine progression of RHD and recurrence rates of ARF, stratifying results by level of adherence to secondary prophylaxis. Potentially, this could progress to a randomized controlled trial of secondary prophylaxis in children with subclinical carditis, although such a study would have substantial logistical and, potentially, ethical hurdles.
Determining the cost-effectiveness of screening, and making it practical and affordable
All of this information needs to be compiled in an objective case for screening, complete with economic analysis. If screening is warranted, the challenge then is to make it practical and scalable in developing countries. In all countries, routine screening of school-aged children is not feasible if it relies on highly trained echocardiography technicians using expensive portable machines. We need to explore the potential for nurses or even community health workers to be trained in this technique. These studies need to be expanded to determine to what level inexpert echocardiographers can be trained, what features of RHD on echocardiogram could be detected using this approach, and what technical specifications would be required of a screening machine. The aim would be to generate guidelines for screening accompanied by training curricula for inexpert screening echocardiographers, and an economic analysis to determine the cost per case detected in different settings. Finally, perhaps with the support of an international funding agency to obtain an advanced market commitment or negotiating reduced prices for developing countries, industry could be commissioned to produce an inexpensive portable echocardiogram and/or refine the newer hand-held machines for the purposes of mass screening.
CHALLENGE 3: BETTER UNDERSTANDING OF DISEASE PATHOGENESIS, WITH A VIEW TO IMPROVED DIAGNOSIS AND TREATMENT OF ARF AND RHEUMATIC HEART DISEASE
A better understanding of ARF/RHD pathogenesis is critical to developing preventive and therapeutic interventions. Current approaches to diagnosis and treatment of ARF have their foundations in the mid-20th Century.[35] The Jones Criteria have been revised and updated several times, and some countries have adapted them for their own circumstances,[8,36] but there continues to be cases of under- and overdiagnosis, often with tragic consequences.[37] Moreover, there is no intervention currently available that is known to alter the potential for RHD to develop following an episode of ARF.[8] Studies of immunomodulatory agents were largely undertaken several decades ago, or more recently have been relatively small and/or based on a crude understanding of ARF pathogenesis.[38] Similarly, attempts to develop a diagnostic test for ARF have been unsuccessful, and have largely relied on relatively crude tests of antibodies to a range of cardiac antigens that are potentially cross-reactive with GAS epitopes.[39]
Immunology of ARF and rheumatic heart disease
We need prospective, active recruitment of ARF cases with a view to using recent technologies to unravel the mysteries of the pathogenesis, particularly the immune response, of ARF. Using standardized data collection forms, each case would undergo thorough immunophenotypic profiling, drawing on the latest understanding of other autoimmune diseases as well as the latest technologies. A range of appropriate control patients would also need to be recruited, including healthy controls, patients with other GAS diseases, and patients with other inflammatory diseases. These studies could hopefully lead to subsequent multicenter clinical trials of promising therapeutic and diagnostic tests. We can also make more use of valve tissue from people with RHD undergoing surgery, particularly as younger patients are increasingly having valve repairs performed, which makes available more useful tissue for immunological studies.
Genetics of ARF/rheumatic heart disease
There is an inherited susceptibility to ARF[40] , but the basis for this susceptibility has yet to be clarified.[41] We have never sought genetic markers for ARF/RHD using modern techniques. The aim should be to interrogate as many immunological loci across the genome as possible, in as fine detail as possible, for associations with RF/RHD. Over the last few years, accurate genetic assessment of large groups of individuals has been achieved through highly scalable microarray platforms that analyze thousands of samples at millions of genomic loci. We need to use these techniques to determine if there are areas of the human genome with polymorphisms highly associated with ARF/RHD, with a view to sequencing and further studying those areas of the genome to identify the nature of host susceptibility, and of course provide information about the features of the autoimmune response that is the basis of ARF. Ideally, this should be performed as part of an international consortium that can share protocols and compare data. Given the highly marginalized populations that suffer RF/RHD, a critical element of these studies must be extensive community consultation, developing and piloting of informed consent materials (including genetic literacy tools), and development of solid, long-term governance structures to ensure that genetic material and resulting data are not misused, and that the benefits of any such research, including commercialization, flow back to the populations in which the studies were conducted.
CHALLENGE 4: FINDING AN EFFECTIVE APPROACH TO PRIMARY PREVENTION
A vaccine for rheumatic fever
In March 2010, the new Hilleman Institute (a collaboration between the Wellcome Trust and Merck, having established an institute in India charged with developing vaccines for less-developed countries) convened a meeting to determine if their first priority vaccine would be for GAS. The meeting was a turning point for GAS disease control. It quickly became clear that GAS vaccines would not be chosen, for the following three reasons:
A vaccine was not sufficiently close to phase III trials;
The global GAS community has not worked sufficiently collaboratively; and
The current understanding of the immunopathogenesis of GAS diseases, particularly RF/RHD, is crude, and investigators have not taken advantage of the latest technologies.
Despite these sobering points, there were some positive outcomes of the meeting, :
It was widely agreed that a GAS vaccine is probably going to require a number of antigens, and there was willingness from those present to pool their expertise and intellectual property to identify the lead antigens to be incorporated into a combination vaccine.
The first steps were taken to form a global GAS vaccine consortium with a view to identifying the right vaccine composition and developing the immunological assays, as well as developing a better understanding of epidemiology, disease burden, and determinants of protection.
This work is critical, and requires international coordination as well as funding.
The role of primary prophylaxis of streptococcal sore throat
There is a disagreement internationally around the way in which primary prophylaxis should be incorporated into control strategies.[42–45] Everyone seems to be in agreement that promotion of sore throat diagnosis and treatment within existing primary healthcare systems is important, although it is not clear how this should be done. Increasingly, there are calls to accept that microbiological diagnosis of GAS pharyngitis is not likely to be practical or affordable in most developing countries for the foreseeable future, so the ongoing debate about the best clinical algorithms to use, and the relative roles of oral or intramuscular penicillin continues.
Another debate is around the role of systematic sore throat screening and treatment programmes in schools or communities, with one side claiming that there is sufficient evidence to promote this approach[46] and the other claiming that the evidence of efficacy, effectiveness, and cost-effectiveness is insufficient to recommend it.[43] We are of the belief that the existing evidence is insufficient, that a more definitive study would be logistically difficult and expensive, and further that, even if it were proven to be effective, such a strategy would be difficult to implement and most unlikely to be affordable in low-income countries. Therefore, we suggest that further research in this area is not perhaps as high a priority as other topics outlined here, and that research into primary prophylaxis should focus on ways of integration into existing primary care systems.
The role of controlling skin infection
There is circumstantial evidence from the Aboriginal population in Australia that skin infection may play a role in RF pathogenesis[47] which, in turn, raises the possibility that community-based programmes to reduce rates of impetigo and underlying scabies--increasingly being studied and demonstrated to be effective[48]--may provide an avenue to large-scale primary prevention of RF/RHD. However, for now, this remains only hypothetical. But this deserves further research, potentially by testing more intensively the hypothesis that streptococcal skin infection might, directly or indirectly, have a causative link with RF, or through intervention studies using either controlled trials or observational studies to map the rates of skin infections against rates of RF/RHD and monitoring changes over time.
In conclusion, we have outlined four key challenges to guide current research priorities in RF/RHD. The major challenge, however, is not to miss the very real opportunity that now exists to translate current and future research into concrete action. It is clear that with concerted efforts, strong links to clinical and public health infrastructure and with strengthening advocacy and renewed international funding support, we have good prospects of controlling RF and minimizing the burden of RHD over the next decade.
Acknowledgments
LZ is supported by the National Institutes of Health Office of the Director, Fogarty International Center, Office of AIDS Research, National Cancer Center, National Eye Institute, National Heart, Blood, and Lung Institute, National Institute of Dental and Craniofacial Research, National Institute On Drug Abuse, National Institute of Mental Health, National Institute of Allergy and Infectious Diseases Health, and NIH Office of Women's Health and Research through the International Clinical Research Scholars and Fellows Program at Vanderbilt University (R24 TW007988), and the American Relief and Recovery Act.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.WHO Technical Report Series; 923. Geneva: World Health Organization; 2004. WHO Expert Consultation on Rheumatic Fever and Rheumatic Heart Disease (2001: Geneva Switzerland). Rheumatic fever and rheumatic heart disease: Report of a WHO Expert Consultation, Geneva, 29 October - 1 November 2001. [PubMed] [Google Scholar]
- 2.Rimoin AW, Hamza HS, Vince A, Kumar R, Walker CF, Chitale RA, et al. Evaluation of the WHO clinical decision rule for streptococcal pharyngitis. Arch Dis Child. 2005;90:1066–70. doi: 10.1136/adc.2004.069120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carapetis JR, Steer AC, Mulholland EK. The current evidence for the burden of group A streptococcal diseases (WHO/FCH/CAH/05.07) Geneva: World Health Organization; 2004. [Google Scholar]
- 4.Carapetis JR. Group A streptococcal vaccine development: Current status and issues of relevance to less developed countries (WHO/FCH/CAH/05.09 and WHO/IVB/05.14) Geneva: World Health Organization; 2004. [Google Scholar]
- 5.Carapetis JR. A review of the technical basis for the current WHO approach to the control of conditions associated with group A streptococcal infections (WHO/FCH/CAH/05.08) Geneva: World Health Organization; 2004. [Google Scholar]
- 6.Mayosi B, Robertson K, Volmink J, Adebo W, Akinyore K, Amoah A, et al. The Drakensberg declaration on the control of rheumatic fever and rheumatic heart disease in Africa. S Afr Med J. 2006;96:246. [PubMed] [Google Scholar]
- 7.Colquhoun SM, Carapetis JR, Kado JH, Steer AC. Rheumatic heart disease and its control in the Pacific. Expert Rev Cardiovasc Ther. 2009;7:1517–24. doi: 10.1586/erc.09.145. [DOI] [PubMed] [Google Scholar]
- 8.National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand. Diagnosis and management of acute rheumatic fever and rheumatic heart disease in Australia: An evidence-based review. Melbourne: National Heart Foundation of Australia; 2006. [Google Scholar]
- 9.Kumar R, Thakur JS, Aggarwal A, Ganguly NK. Compliance of secondary prophylaxis for controlling rheumatic fever and rheumatic heart disease in a rural area of northern India. Indian Heart J. 1997;49:282–8. [PubMed] [Google Scholar]
- 10.Bach JF, Chalons S, Forier E, Elana G, Jouanelle J, Kayemba S, et al. 10-year educational programme aimed at rheumatic fever in two French Caribbean islands. Lancet. 1996;347:644–8. doi: 10.1016/s0140-6736(96)91202-7. [DOI] [PubMed] [Google Scholar]
- 11.Wilson N. Rheumatic heart disease in indigenous populations--New Zealand experience. Heart Lung Circ. 2010;19:282–8. doi: 10.1016/j.hlc.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 12.Tibazarwa KB, Volmink JA, Mayosi BM. Incidence of acute rheumatic fever in the world: A systematic review of population-based studies. Heart. 2008;94:1534–40. doi: 10.1136/hrt.2007.141309. [DOI] [PubMed] [Google Scholar]
- 13.Carapetis JR, Steer AC, Mulholland EK, Weber M. The global burden of group A streptococcal diseases. Lancet Infect Dis. 2005;5:685–94. doi: 10.1016/S1473-3099(05)70267-X. [DOI] [PubMed] [Google Scholar]
- 14.Mincham CM, Mak DB, Plant AJ. The quality of management of rheumatic fever/heart disease in the Kimberly. Aust N Z J Public Health. 2002;26:417–20. doi: 10.1111/j.1467-842x.2002.tb00340.x. [DOI] [PubMed] [Google Scholar]
- 15.Harrington Z, Thomas DP, Currie BJ, Bulkanhawuy J. Challenging perceptions of non-compliance with rheumatic fever prophylaxis in a remote Aboriginal community (mm ref 2769) Med J Aust. 2006;184:514–7. doi: 10.5694/j.1326-5377.2006.tb00347.x. [DOI] [PubMed] [Google Scholar]
- 16.Gardner KL, Dowden M, Togni S, Bailie R. Understanding uptake of continuous quality improvement in Indigenous primary health care: Lessons from a multi-site case study of the Audit and Best Practice for Chronic Disease project. Implement Sci. 2010;5:21. doi: 10.1186/1748-5908-5-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zaher S, Kassem A, Abou-Shleib H, El Khouly A, Madkour A, Kaplan E. Differences in serum penicillin concentrations following intramuscular injection of benzathine penicillin G (BPG) from different manufacturers. J Pharm Med. 1992;2:17–23. [Google Scholar]
- 18.Stollerman GH, Rusoff JH. Prophylaxis against group A streptococcal infections in rheumatic fever patients; Use of new repository penicillin preparation. J Am Med Assoc. 1952;150:1571–5. doi: 10.1001/jama.1952.03680160021005. [DOI] [PubMed] [Google Scholar]
- 19.Kassem AS, Zaher SR, Abou Shleib H, el-Kholy AG, Madkour AA, Kaplan EL. Rheumatic fever prophylaxis using benzathine penicillin G (BPG): Two- Week versus four-week regimens: Comparison of two brands of BPG. Pediatrics. 1996;97:992–5. [PubMed] [Google Scholar]
- 20.Kaplan EL, Berrios X, Speth J, Siefferman T, Guzman B, Quesny F. Pharmacokinetics of benzathine penicillin G: Serum levels during the 28 days after intramuscular injection of 1,200,000 units. J Pediatr. 1989;115:146–50. doi: 10.1016/s0022-3476(89)80352-x. [DOI] [PubMed] [Google Scholar]
- 21.Bass JW, Longfield JN, Jones RG, Hartmann RM. Serum levels of penicillin in basic trainees in the U.S. Army who received intramuscular penicillin G benzathine. Clin Infect Dis. 1996;22:727–8. doi: 10.1093/clinids/22.4.727. [DOI] [PubMed] [Google Scholar]
- 22.Ngo HT, Arnold-Reed DE, Hansson RC, Tait RJ, Hulse GK. Blood naltrexone levels over time following naltrexone implant. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32:23–8. doi: 10.1016/j.pnpbp.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 23.Nordet P, Lopez R, Duenas A, Sarmiento L. Prevention and control of rheumatic fever and rheumatic heart disease: The Cuban experience (1986-1996-2002) Cardiovasc J Afr. 2008;19:135–40. [PMC free article] [PubMed] [Google Scholar]
- 24.Michaud C, Rammohan R, Narula J. Cost-effectiveness analysis of intervention strategies for reduction of the burden of rheumatic heart disease. In: Narula J, Virmani R, Reddy KS, Tandon R, editors. Rheumatic fever. Washington DC: American Registry of Pathology; 1999. pp. 485–97. [Google Scholar]
- 25.Michaud C, Gutierrez J, Cruz C, Pearson T. The World Bank health sector priorities review: Rheumatic heart disease. Washington, D C: World Bank; 1991. pp. 1–31. [Google Scholar]
- 26.Carapetis JR, Powers JR, Currie BJ. Outcomes of cardiac valve replacement for rheumatic heart disease in Aboriginal Australians. Asia Pac Heart J. 2000;8:138–47. [Google Scholar]
- 27.Levine HJ, Pauker SG, Salzman EW. Antithrombotic therapy in valvular heart disease. Chest. 1986;89:36S–45. doi: 10.1378/chest.89.2_supplement.36s. [DOI] [PubMed] [Google Scholar]
- 28.Salem DN, Stein PD, Al-Ahmad A, Bussey HI, Horstkotte D, Miller N, et al. Antithrombotic therapy in valvular heart disease--native and prosthetic: The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:457S–82S. doi: 10.1378/chest.126.3_suppl.457S. [DOI] [PubMed] [Google Scholar]
- 29.Sanyal SK, Thapar MK, Ahmed SH, Hooja V, Tewari P. The initial attack of acute rheumatic fever during childhood in North India; A prospective study of the clinical profile. Circulation. 1974;49:7–12. doi: 10.1161/01.cir.49.1.7. [DOI] [PubMed] [Google Scholar]
- 30.Feinstein AR, Wood HF, Spagnuolo M, Taranta A, Jonas S, Kleinberg E, et al. Rheumatic Fever in Children and Adolescents.A Long-Term Epidemiologic Study of Subsequent Prophylaxis, Streptococcal Infections, and Clinical Sequelae. Vii. Cardiac Changes and Sequelae. Ann Intern Med. 1964;60:87–123. [PubMed] [Google Scholar]
- 31.Paar JA, Berrios NM, Rose JD, Cáceres M, Peña R, Pérez W, et al. Prevalence of rheumatic heart disease in children and young adults in Nicaragua. Am J Cardiol. 2010;105:1809–14. doi: 10.1016/j.amjcard.2010.01.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marijon E, Ou P, Celermajer DS, Ferreira B, Mocumbi AO, Jani D, et al. Prevalence of rheumatic heart disease detected by echocardiographic screening. N Engl J Med. 2007;357:470–6. doi: 10.1056/NEJMoa065085. [DOI] [PubMed] [Google Scholar]
- 33.Carapetis JR, Hardy M, Fakakovikaetau T, Taib R, Wilkinson L, Penny DJ, et al. Evaluation of a screening protocol using auscultation and portable echocardiography to detect asymptomatic rheumatic heart disease in Tongan schoolchildren. Nat Clin Pract Cardiovasc Med. 2008;5:411–7. doi: 10.1038/ncpcardio1185. [DOI] [PubMed] [Google Scholar]
- 34.Cherian T, Mulholland EK, Carlin JB, Ostensen H, Amin R, de Campo M, et al. Standardized interpretation of paediatric chest radiographs for the diagnosis of pneumonia in epidemiological studies. Bull World Health Organ. 2005;83:353–9. [PMC free article] [PubMed] [Google Scholar]
- 35.Jones TD. Diagnosis of rheumatic fever. JAMA. 1944;126:481–4. [Google Scholar]
- 36.Diagnosis, management and secondary prevention. Auckland: Heart Foundation of New Zealand; 2006. Heart Foundation of New Zealand and Cardiac Society of Australia and New Zealand. New Zealand Guidelines for Rheumatic Fever. 1. [Google Scholar]
- 37.Mataika R, Carapetis JR, Kado J, Steer AC. Acute rheumatic fever: An important differential diagnosis of septic arthritis. J Trop Pediatr. 2008;54:205–7. doi: 10.1093/tropej/fmm116. [DOI] [PubMed] [Google Scholar]
- 38.Cilliers AM, Manyemba J, Saloojee H. Anti-inflammatory treatment for carditis in acute rheumatic fever. Cochrane Database Syst Rev. 2003:CD003176. doi: 10.1002/14651858.CD003176. [DOI] [PubMed] [Google Scholar]
- 39.Towers RJ, Bolm M, Currie BJ, Chhatwal GS, Fagan PK. Autoantigens identified by screening a human heart cDNA library with acute rheumatic fever sera. Ann N Y Acad Sci. 2009;1173:83–91. doi: 10.1111/j.1749-6632.2009.04653.x. [DOI] [PubMed] [Google Scholar]
- 40.Engel ME, Sr, Vogel J Adeyemo AA, Mayosi BM. Genetic contribution to rheumatic fever: A systematic review and meta-analysis of twin studies.[Presented at the 8th National Congress of the South African Heart Association, Sun City, 22-25 November 2007] S Afr Med J. 2007;97:1094. [Google Scholar]
- 41.Bryant PA, Robins-Browne R, Carapetis JR, Curtis N. Some of the people, some of the time: Susceptibility to acute rheumatic fever. Circulation. 2009;119:742–53. doi: 10.1161/CIRCULATIONAHA.108.792135. [DOI] [PubMed] [Google Scholar]
- 42.Karthikeyan G, Mayosi BM. Is primary prevention of rheumatic fever the missing link in the control of rheumatic heart disease in Africa? Circulation. 2009;120:709–13. doi: 10.1161/CIRCULATIONAHA.108.836510. [DOI] [PubMed] [Google Scholar]
- 43.Carapetis J, Steer A. Prevention of rheumatic fever. Pediatr Infect Dis J. 2010;29:91–2. doi: 10.1097/INF.0b013e3181bf53f3. author reply 2. [DOI] [PubMed] [Google Scholar]
- 44.Carapetis JR. Letter by Carapetis regarding article, “Is primary prevention of rheumatic fever the missing link in the control of rheumatic heart disease in Africa?” Circulation. 2010;121:e384. doi: 10.1161/CIR.0b013e3181dbdde0. author reply e5. [DOI] [PubMed] [Google Scholar]
- 45.Lennon D, Stewart J, Farrell E, Palmer A, Mason H. School-based prevention of acute rheumatic fever: A group randomized trial in New Zealand. Pediatr Infect Dis J. 2009;28:787–94. doi: 10.1097/INF.0b013e3181a282be. [DOI] [PubMed] [Google Scholar]
- 46.Lennon D, Kerdemelidis M, Arroll B. Meta-analysis of trials of streptococcal throat treatment programs to prevent rheumatic fever. Pediatr Infect Dis J. 2009;28:e259–64. doi: 10.1097/INF.0b013e3181a8e12a. [DOI] [PubMed] [Google Scholar]
- 47.McDonald M, Currie BJ, Carapetis JR. Acute rheumatic fever: A chink in the chain that links the heart to the throat? Lancet Infect Dis. 2004;4:240–5. doi: 10.1016/S1473-3099(04)00975-2. [DOI] [PubMed] [Google Scholar]
- 48.Lawrence G, Leafasia J, Sheridan J, Hills S, Wate J, Wate C, et al. Control of scabies, skin sores and haematuria in children in the Solomon Islands: Another role for ivermectin. Bull World Health Organ. 2005;83:34–42. [PMC free article] [PubMed] [Google Scholar]


