Abstract
Background:
Tuberculosis is a communicable disease requiring prolonged treatment.The therapeutic regimens as recommended by WHO have been shown to be highly effective for both preventing and treating tuberculosis but poor adherence to medication is a major barrier to its global control.
Aim:
The aim was to elicit reasons of treatment default from a cohort of tuberculosis patients treated under Directly Observed Treatment Short course chemotherapy.
Settings and design:
Thiscross-sectional study was conducted in Agra city using the multistage simple random sampling.
Materials and Methods:
A total of 900 patients attending DOTS centres of the selected designated microscopy centers (DMCs) were included in the study from January 2007 onward. The information was obtained from treatment cards of patients and those who defaulted were further interviewed in community.
Statistical analysis:
Chi-square test was applied to observe the significance of association using the Epi Info software (version 6).
Results:
More default was observed among the age group of >45 years (22.8%), male (18.7%), business men (30.6%), and retired and unemployed patients. Other factors associated with higher default were pulmonary disease (18.2%), retreatment cases (30.6%) and category II patients (26.4%). Important reasons of default were side effects following medication (43.2%), improvement in symptoms (14.4%), and lack of time (13.5%). No relief in symptoms and lack of awareness were other important reasons.
Conclusions:
Noncompliance was found to be mainly due to side effects of medicines, lack of time, and unawareness. So educating the patient about various aspects of tuberculosis and some measures to decrease side effects are of utmost importance.
Keywords: DOTS, noncompliance, RNTCP, tuberculosis
Introduction
Tuberculosis (TB) is a communicable disease requiring prolonged treatment, and poor adherence to a prescribed treatment increases the risk of morbidity, mortality, and spread of disease in the community.(1) The World Health Organization (WHO) declared TB a global public health emergency in 1993 and since then intensified its efforts to control the disease worldwide.(2) Tuberculosis control has been accorded a high priority within the health sector as it is a major public health problem.(3)The therapeutic regimens given under direct observation as recommended by WHO have been shown to be highly effective for both preventing and treating TB but poor adherence to antituberculosis medication is a major barrier to its global control.(4)
Revised National Tuberculosis Control Program (RNTCP) with Directly Observed Treatment Short course (DOTS) is the internationally recommended strategy, to ensure cure of tuberculosis; it has become the standard for the diagnosis, treatment, and monitoring of tuberculosis worldwide and has been implemented in 187 out of 211 countries, covering more than 89% of world's population.(5)
At the national level, the program has nearly achieved its twin objectives of case detection and cure rates during the second quarter 2007,(6) and the program has continued to achieve it at the national level during the first quarter, 2009.(7)But it is to be realized that even after achieving 70% case detection and 85% cure rate, we are actually curing 59% patients. What about the remaining 41% of the cases in the community? By curing only 59% of patients, the goal of RNTCP cannot be achieved.
Further poor adherence to treatment leads to emergence of multi-drug-resistant bacilli, so ensuring compliance is of utmost importance to control TB and halt the MDR TB epidemic at its beginning. So there is continuing need to sustain and further intensify the actions being undertaken to reduce default. The focus must remain on dealing with important reasons of default and timely retrieval of patients who interrupt treatment. This paper identifies reasons for noncompliance to treatment among defaulters, elicited during home visits.
Materials and Methods
This cross-sectional type of study was conducted in Agra city using the multistage simple random sampling and a total of 900 patients attending DOTS centers of the selected designated microscopy centers (DMCs) were included in the study. By using overall prevalence (10.2%) of defaulters among patients put on DOTS,(8) the sample size came out to be 880; keeping the dropouts and nonrespondents in consideration, the sample size was increased and rounded off to 900.
Agra district is divided into eight tuberculosis units (TUs), with five TUs covering rural areas while three in urban Agra. All the three TUs of urban Agra were included in the study and two DMCs from each TU were selected randomly. All the patients registered in all the DOTS centers of the selected DMCs from January 2007 onward were included in the study until the desired sample size was complete. Treatment cards of these patients were obtained from their respective DMCs and all the required information was collected on predesigned pretested schedules. Patients who defaulted on treatment were further traced in community and interviewed thoroughly regarding reasons of default and other associated factors.
The information thus collected was computerized in a specific program developed on Microsoft Office Excel 2007 software on a regular basis and the database so prepared was analyzed with the help of Epi Info software (version 6).
Results
The study was conducted among patients of Agra city who were treated for tuberculosis using the standard treatment regimen of DOTS. In the present study, 45.4% patients completed the treatment and 26.2% were declared cured. Among them, 15.1% defaulted, 5.9% died, 2.0% failed on treatment while 5.3% were transferred out to other centers. Biosocial characteristics of the patients were studied and the effect of various factors on patient's compliance to treatment was observed.
Table 1 shows that almost one-fourth (22.8%) patients of the >45-year age group defaulted, while only 3.5% patients defaulted in the <15-year age group. Male patients defaulted twice as common than females (18.7% of males and 9.5% of females). Almost one-third (30.6%) of businessmen and one-forth (25.0%) of retired and unemployed patients defaulted. Students and under-5 children were more compliant to treatment with 7.7% and 3.0% noncompliance, respectively, while 10.3% of housewives did not comply with the treatment.
Table 1.
Factors associated with noncompliance to treatment
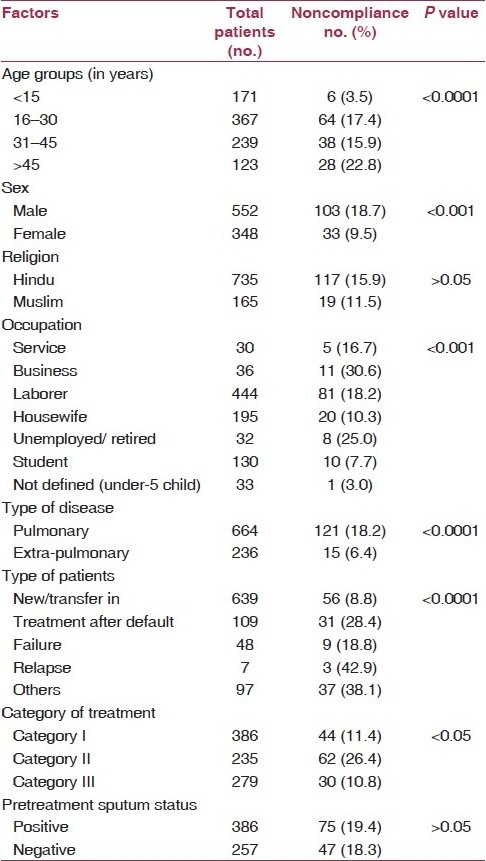
Patients with pulmonary disease defaulted three times as common as compare to those with extra-pulmonary disease (18.2% and 6.4%, respectively). On analyzing the effect of the type of patient, a very high rate of noncompliance was observed among retreatment cases (30.6%), while 8.8% of new patients defaulted. Among different treatment categories, almost one-forth patients (26.4%) of category II defaulted, while it was 11.4% among category I and 10.8% among category III patients. Religion and pretreatment sputum smear status were not found to have any significant association with patient's compliance.
Patients who defaulted were interviewed at their home. Overall noncompliance rate in our study was found to be 15.1% that is 136 patients. For purpose of exploring the reasons of default, these patients were followed in community and interviewed in detail for the reasons. A total of 111 defaulters could be located and interviewed. Rest of defaulters either changed their home, or refused to answer or died after treatment interruption.
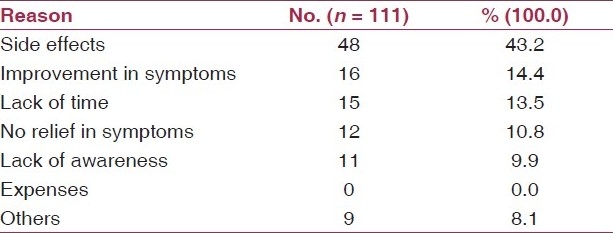
On analyzing the reasons of default among defaulters, side effects following medication were found to be the most common reason (43.2%). Next important reasons were improvement in symptoms and lack of time (14.4% and 13.5%, respectively). No relief in symptoms and lack of awareness about the duration of treatment and importance of full treatment were other important reasons behind default (10.8% and 9.9%, respectively). None of the patients stated financial problems as a reason of default. Some other reasons such as going out of station, alcoholism, and domestic problems were also found to have importance in 8.1% of patients [Table 2].
Table 2.
Most important reasons of non-compliance
Discussion
In the present study, 15.1% patients defaulted, which is much higher than what is expected under RNTCP, i.e., <5%.(9)
Default to treatment was found to be more among older patients (22.8%), while very good compliance to treatment was observed among pediatric patients (3.5% default), as also observed in other studies.(10,11) Kumar et al. observed maximum default in the 35-44-year age group (25.4%), followed by the patients aged above 45 years (18.1%).(12) The reason behind more default in older patients is mainly the self-neglect and neglect by family, while the development of more side effects was supposed to be another important reason. Further comparatively more default in the 16–30-year age group is mainly due to the subjects being economically productive members of the family, which led them to leave the treatment rather than to leave their earning of the day.
Another risk factor for default is male sex,(1,11) while no effect of sex on patient's compliance to treatment was observed by some researchers.(12) More default among males is supposed to be due to their being earning members of the family, and so they could not afford to get leave on job that frequently, while in contrast DOTS centers are present in most of the localities so females can visit the center regularly, and there is no need of someone to accompany.
Persons involved in various occupations, especially the businessmen, defaulted more as compared to housewives and students, but in contrast retired persons defaulted more inspite of having plenty of time. Jaggarajamma et al.(1)alsoobserved more default among employed patients, while few other did not find any association between patient's occupation and response to treatment.(11) The main reason behind the difference in compliance among persons with various occupations seems to be loss of wages and lack of time.
Other factors associated with default were observed to be pulmonary disease, category II of treatment and retreatment regimen, as also observed in other studies.(1,10) More default among these patients may be due to more concern of patients toward symptoms of extra-pulmonary disease, as well as less amount of medicines and shorter duration of treatment in most of extra-pulmonary cases, leading to lesser side effects and better compliance. Good response to treatment among new cases, whether they are of category I or category III, is mainly due to less severe disease initially, fewer side effects, shorter duration of treatment, and lesser patient fatigue. On the other hand, category II patients have to take more medicines and for longer duration. Additionally, medication in injectable form further increases the tendency to default. All these factors lead to patient fatigue, more side effects, and subsequently development of drug resistance.
The present study identifies side effects following medication as the most common reason of default. Other important reasons were improvement in symptoms (14.4%), lack of time (13.5%), no relief following medication (10.8%), and lack of awareness (9.9%). Almost similar reasons of default were observed in other studies.(1,13)
A study from Bihar and West Bengal reported that improvement in symptoms (40% and 56%), intolerance to drugs (20% and 9%), and other illnesses caused defaults in some patients.(14) A study from Malaysia also reported similar findings.(15) Some other important reasons were also observed, such as domestic problems,(16) migration,(17) taking treatment from other sources,(11,16) alcoholism, and going out of station.
Keeping in mind all the important reasons of default, initial counseling by the health personnel explaining the treatment plan before starting of the treatment, periodic motivation of patients, and prompt action to tackle any problem will enhance compliance. Adequate health education and information about tuberculosis has been demonstrated to be most effective when given as one-to-one counseling.(18) Providing DOTS as per patient's convenience through community DOTS providers with periodic monitoring may reduce the treatment default. Periodic monitoring of the community DOTS providers by the health staff is important to minimize default. Some work should also be done on anti-tuberculosis drugs to decrease the number of pills patient have to consume. Further availability of some medicines required for treating side effects can be ensured as side effects following treatment is a major problem among patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Jaggarajamma K, Sudha G, Chandrasekaran V, Nirupa C, Thomas A, Santha T, et al. Reasons for non compliance among patients treated under Revised National Tuberculosis Control Programme (RNTCP), Tiruvallur district, South India. Indian J Tuberc. 2007;54:130–5. [PubMed] [Google Scholar]
- 2.TB - A Global Emergence. Geneva: World Health Organization; 1994. World Health Organization. WHO/TB/94.177. [Google Scholar]
- 3.Dhuria M, Sharma N, Ingle GK. Impact of tuberculosis on the quality of life. Indian J Community Med. 2008;33:58–9. doi: 10.4103/0970-0218.39249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Addington WW. Patient compliance: The most serious remaining problem in the control of tuberculosis in the United States. Chest. 1979;76:741–3. doi: 10.1378/chest.76.6_supplement.741. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Geneva: Global Tuberculosis Control: Surveillance, Planning, Financing. WHO Report 2007. WHO/HTM/TB/2007.376. [Google Scholar]
- 6.New Delhi: Nirman Bhavan; 2007. RNTCP Performance Report, India, second quarter. Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare. [Google Scholar]
- 7.Chauhan LS. Status report on RNTCP. Indian J Tuberc. 2009;56:151–3. [PubMed] [Google Scholar]
- 8.New Delhi: Nirman Bhavan; 2005. RNTCP Performance Report, India, second quarter. Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare. [Google Scholar]
- 9.Vol. 25. New Delhi: Nirman Bhavan; 2005. RNTCP at a GLANCE. Central TB division, Directorate General of Health Services, Ministry of Health and Family Welfare. [Google Scholar]
- 10.Menzies D, Adhikari N, Tannenbaum T. Patient characteristics associated with failure of tuberculosis prevention. Tuberc Lung Dis. 1996;77:308–14. doi: 10.1016/s0962-8479(96)90094-5. [DOI] [PubMed] [Google Scholar]
- 11.Chandrasekaran V, Gopi PG, Subramani R, Thomas A, Jaggarajamma K, Narayanan PR. Default during the Intensive phase of treatment under DOTS programme. Indian J Tuberc. 2005;52:197–202. [Google Scholar]
- 12.Kumar M, Singh JV, Srivastava AK, Verma SK. Factors affecting the noncompliance in Directly Observed Short Course Chemotherapy in Lucknow District. Indian J Community Med. 2002;27:114–7. [Google Scholar]
- 13.Pandit N, Choudhary SK. A study of treatment compliance in Directly Observed Therapy for Tuberculosis. Indian J Community Med. 2006;3:241–3. [Google Scholar]
- 14.Chattergee P, Benerjee B, Dutt D, Pati RR, Mullick A. A Comparative Evaluation of Factors and Reasons for Defaulting in Tuberculosis Treatment in the States of West Bengal, Jharkhand and Arunachal Pradesh. Indian J Tuberc. 2003;50:17–21. [Google Scholar]
- 15.O’Boyle SJ, Power JJ, Imbrahim MY. Factors affecting patient compliance with anti-tuberculosis chemotherapy using the directly observed treatment, Short Course Strategy (DOTS) Int J Tuberc Lung Dis. 2000;6:307–12. [PubMed] [Google Scholar]
- 16.Masthi NR, Rajanna MS, Parasuramalu BG. A study on The Effectiveness of DOTS on tuberculosis patients treated under RNTCP. Indian J Public Health. 2006;50:55–7. [PubMed] [Google Scholar]
- 17.Katiyar SK, Bihari S, Arun S, Rawat T. An analysis of failure of category-II DOTS therapy. Indian J Community Med. 2008;33:129–30. doi: 10.4103/0970-0218.40886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cunio W, Snider DE. Enhancing Patient Compliance with tuberculosis therapy. Clin Chest Med. 1989;3:375–9. [PubMed] [Google Scholar]


