Introduction
Over population has always been the prime problem of developing countries like India forcing toward birth control. Industrial revolution improved quality of living and increased longevity. While developmental processes are in full swing at one angle, fertility is fast declining at the other angle due to the modern lifestyle and usage of chemicals which impair reproduction.(1)
World Health Organization explains primary infertility as inefficiency to conceive after 2 years of unprotected sex and secondary if not conceived following previous pregnancy. Biological and social factors including stress due to economic status, religious attitudes, age of marriage, urbanization leading to modernization, higher literacy, contraceptive usage and nuclear families play a significant role in lowering fertility.(2)
A survey was undertaken to study the occurrence of infertility cases and major factors influencing infertility in southern districts of India.
Materials and Methods
Enormous information generated through survey works in abroad as what lacks in India. Collection of data on infertility (sensitive issue) was very difficult in our conservative societies. Owing to high literacy in the selected study area, we expected some open communication.
About 150 married couples in Kanyakumari, 165 in Thirunelveli, and 204 in Thiruvananthapuram were randomly interviewed to ascertain the prevalence of infertility. Data were collected from the patients contacting the Department of Obstetrics and Gynecology in infertility clinics. Definitive protocols including their age, region, religion, education, occupation, lifestyle, type of infertility, family history of infertility, and menstrual history were followed to determine the etiology of infertility.
Statistical analysis
The data collected were subjected to mean, standard error, percentage and Pearson's correlation analysis.
Results
Occurrence of infertility
In Kanyakumari district, the incidence of female infertility was 45.67%, male infertility 54.33%, 82.48% were primarily and 17.52% secondarily infertile. Male infertility was higher in all the three study areas with Thiruvananthapuram displaying minimum female infertility [Table 1].
Table 1.
Occurrence of infertility in three different study areas
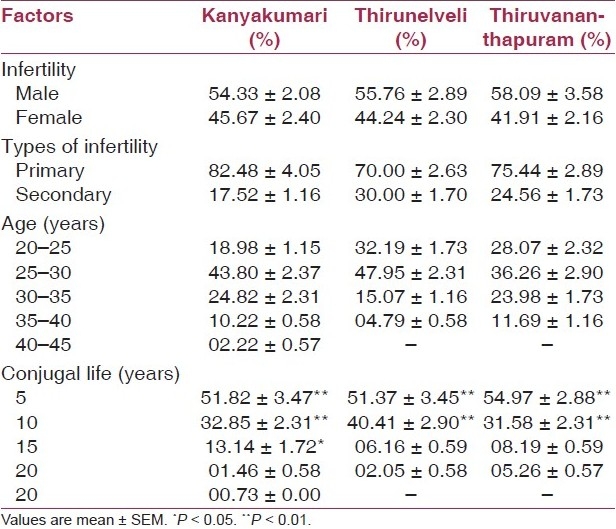
Age group
Maximum infertility of females visiting infertility clinics prevailed between 25 and 30 years of age, with 43.80%, 47.95% and 36.26% in Kanyakumari, Thirunelveli and Thiruvananthapuram, respectively [Table 1].
Infertility and conjugal life
Out of 137 infertile females interviewed in Kanyakumari, 51.82% were infertile for 5 years, 32.85% for 10 years, 13.14% for 15 years, 01.46% for 20 years and only 00.73% for 25 years after marriage [Table 1]. Almost the same trend (P < 0.01) prevailed in Thirunelveli and Thiruvananthapuram.
Region and religion
The percentage of infertile females was more in urban than rural in all the three study areas (P < 0.01). Infertile females were reported from all religions, Hindu, Christian and Muslim [Table 2].
Table 2.
Sociodemographic characteristics of infertile females in three different study areas
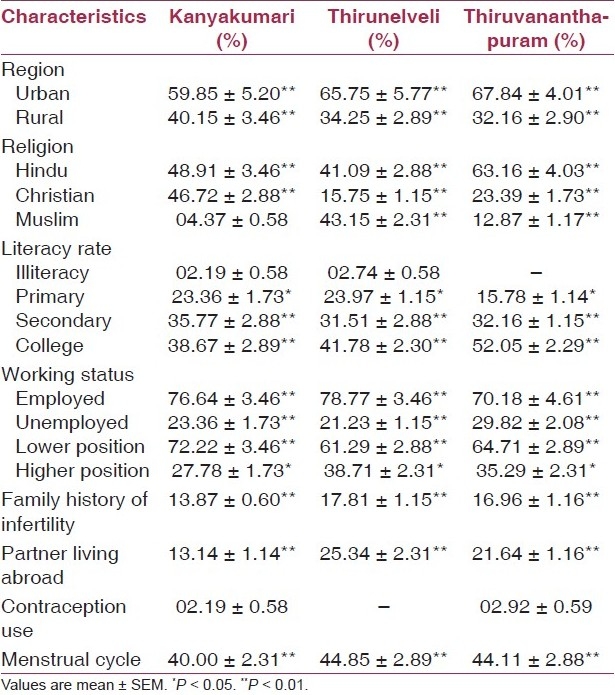
Education
Educational status being the most important variable, women with secondary school education and above had markedly lower average fertility (P < 0.01) than the less educated [Table 2].
Working status
In Kanyakumari, 76.64% of infertile females were unemployed and 23.36% (P < 0.01) employed. Among employed, 72.22% (P < 0.01) were at lower positions and 27.78% (P < 0.05) were at high posts. In Thirunelveli and Thiruvananthapuram, infertility was more in unemployed women (78.77% and 70.18%, respectively). Similarly, females at lower positions were more infertile [Table 2].
Family history
Our results show that the family history of infertility is significantly correlated (P < 0.01) with infertility [Table 2] in the three study areas.
Partner living abroad
Positive correlation of infertility (P < 0.01) was recorded where the husband lived abroad due to occupation [Table 2].
Contraception
Infertile couples in all the three districts used minimum number of contraceptives showing negative correlation between infertility and usage of contraception [Table 2].
Menstrual irregularity
Menstrual irregularity was reported among infertile females in the three study areas (40%, 44.85%, 44.11% respectively) and was positively correlated with female infertility (P < 0.01).
Discussion
In the present study, an effort has been made to find out common factors responsible for female infertility in the three study areas. The prevalence of female infertility was 45.67% in Kanyakumari, 44.24% in Thirunelveli, and 41.91% in Thiruvananthapuram. Primary infertility is as common distressing problem in India as in other parts of the world. Zargar et al reported that the magnitude of primary infertility in India was 50%..(3) The present study clearly indicates that primary infertility was more dominating than secondary infertility in South India.
A woman reaches her maximum fertility potential at the age of 30.(4) We observed maximum number of infertile females in the age group of 25 - 30 years indicating a shift in the fertility potential age. Maximum women had 1- 5 years of infertility duration but Sumita and Ranjit reported that 57.5% were infertile for 2 - 5 years.(4)
We established more infertility in urban than rural areas while Mokhtar et al reported more infertility in rural areas.(5) In India, women with high school education and above have markedly higher infertility rate than the less educated.(6) Kerala had set an example by having high female literacy and lower infertility.
Interestingly, the infertility percentage of unemployed females was more in all three study areas than the employed suggesting lifestyle stress. The incidence of infertility among women with a positive infertility family history among mothers and sisters was 24% and 32%, respectively.(5) In Kanyakumari 13.14% couples, Thirunelveli 25.34% couples and Thiruvananthapuram 16.96% couples had a temporarily migrant male partner working abroad who failed to persist getting infertility treatment.
According to Dabral and Malik usage of family planning methods increases with education of women.(2) However, we observed very few educated couples using contraceptives. Frank found that women with PCOS were concomitant with increased risk of infertility.(7) Which is true in the present study where PCOS was the major cause for infertility.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Sharara FI, Seifer DB, Flaws JA. Environmental toxicants and female reproduction. Fertil Steril. 1998;70:613–22. doi: 10.1016/s0015-0282(98)00253-2. [DOI] [PubMed] [Google Scholar]
- 2.Dabral S, Malik SL. Demographic study of gujars of Delhi: VI. Factors affecting fertility, Infant mortality and use of BCM. J. of Hum. Ecol. 2005;17:85–92. [Google Scholar]
- 3.Zargar AH, Wani AI, Masoodi SR, Laway BA, Salahuddin M. Epidemologic and etiologic aspects of primary infertility in the Kashmir region of India. Fertil Steril. 1997;68:637–43. doi: 10.1016/s0015-0282(97)00269-0. [DOI] [PubMed] [Google Scholar]
- 4.Dutta S, Guha R. A clinico- anatomical study on the etiological factors pertaining to primary infertility in females using some common investigative procedures. J Anat Soc India. 2007;56:14–7. [Google Scholar]
- 5.Samiha Mokhtar, Hassan Ali Hassan, Nehad Mahdy, Fayek Elkhwsky, Gehan Shehata. Risk factors for primary and secondary female infertility in Alexandra: A hospital based care control study. J Med Res Inst. 2006;27:251–61. [Google Scholar]
- 6.Mandelbaum DG. Human fertility in India: Social components and policy perspectives. University of California Press: Berkeley; 1974. [Google Scholar]
- 7.Franks S. Polycystic Ovary Syndrome. N Engl J Med. 1995;333:853–61. doi: 10.1056/NEJM199509283331307. [DOI] [PubMed] [Google Scholar]


