Abstract
Objective
The primary aim of this study was to test a psychosocial model of medication adherence among people taking antiretroviral medications. This model was based primarily on social cognitive theory and included personal (self-efficacy, outcome expectancy, stigma, depression, and spirituality), social (social support, difficult life circumstances), and provider (patient satisfaction and decision-making) variables.
Design
The data for this analysis were obtained from the parent study, which was a randomized controlled trial (Get Busy Living) designed to evaluate an intervention to foster medication adherence. Factor analysis was used to develop the constructs for the model, and structural equation modeling was used to test the model. Only baseline data were used in this cross sectional analysis.
Methods
Participants were recruited from a HIV/AIDS clinic in Atlanta, GA. Prior to group assignment, participants were asked to complete a questionnaire that included assessment of the study variables.
Results
A total of 236 participants were included in the analysis. The mean age of the participants was 41 years; the majority were male, and most were African-American. In the final model, self-efficacy and depression demonstrated direct associations with adherence; whereas stigma, patient satisfaction, and social support were indirectly related to adherence through their association with either self-efficacy or depression.
Conclusion
These findings provide evidence to reinforce the belief that medication-taking behaviors are affected by a complex set of interactions among psychosocial variables and provide direction for adherence interventions.
Keywords: AIDS, Medication adherence, Antiretroviral medication
Introduction
The advent of combination antiretroviral therapy (ART) for treatment of human immunodeficiency virus (HIV) began a new era of HIV care. The ability to control HIV infection through the use of medications has reduced mortality and prolonged life expectancy (Machtinger and Bangsberg 2005). Studies show that individuals who take 95% or more of their prescribed ART medication benefit more from treatment than those who take less than 95% (Bangsberg et al. 2001; Paterson et al. 2000). The proportion of people taking 95% or more of their prescribed medications is relatively small. Paterson et al. (2000) found that approximately 30% of patients were able to achieve this level, and Golin and colleagues (2002) found that only 4% of patients took 95% or more of their medications consistently. In addition, adherence rates tend to decline over time (Howard et al. 2002; Ickovics et al. 2002).
Fluctuating or inadequate blood/serum levels of anti-retroviral medications interfere with full viral suppression, which minimizes the effect of antiretroviral therapy and increases the likelihood of drug resistance (Bangsberg et al. 2001). Inadequate or inconsistent medication intake is a concern for health care providers, who are aware of the side effects and lifestyle changes required for their patients to take these medications. Research shows that medication-taking difficulties can be due to medication-related factors such as pill burden, side effects, and complicated regimens (Bartlett et al. 2001; Fogarty et al. 2002; Ickovics et al. 2002). As new generations of drugs become available, pharmaceutical companies are addressing these concerns by developing pills that include more than one drug and regimen schedules that offer once or twice per day dosing with fewer and smaller pills.
Another area that has received attention with regard to ART adherence is the personal and social characteristics that might serve to foster or hinder adherence efforts. For example, researchers have found that depression (Ammassari et al. 2004; Kleeberger et al. 2004; Sledjeski et al. 2005) and low self-efficacy (Catz et al. 2000; Godin et al. 2005) contribute to low levels of reported adherence, and that having a good support system and positive attitudes (Catz et al. 2000; Godin et al. 2005) about medication taking foster adherence. While HIV adherence literature provides a good understanding of the personal and social variables that are most likely to play a role in ART adherence, the complexity of the interrelationships among these variables may be less well understood. From a practical standpoint, the complexity of these relationships may make it difficult to determine exactly which variables should be the focus of intervention programs.
A number of studies examining correlates of ART adherence have relied on an examination of bivariate relationships or have approached the analysis via multiple linear regression. (Ammassari et al. 2002; Ickovics et al. 2002). While providing useful information, these types of analyses fail to account for the complex relationships among variables that are likely to influence ART adherence. An investigation of factors influencing ART adherence may be better approached using structural equation modeling (SEM), a technique designed to explore both the direct and indirect effects of variables on an outcome of interest. In the analysis reported here, we developed and tested a model of ART adherence using personal and social variables identified in the ART adherence literature and elaborated within the framework of social cognitive theory.
Theoretical Perspective
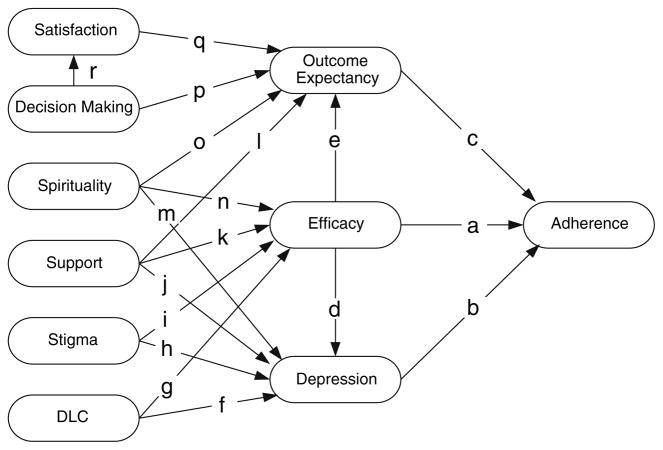
There are a number of personal and social factors that have been identified as possible factors in ART adherence (Ammassari et al. 2002; Fogarty et al. 2002; Ickovics et al. 2002). In order to create a realistic model for testing, we used a systematic method to select the most salient variables to include in the model using social cognitive theory (SCT) as the guiding framework. Thus, the first set of variables (self-efficacy, outcome expectancy, depression, and social support) was derived from SCT, and the second set was composed of variables (spirituality, stress, stigma, patient satisfaction, and patient participation in decision-making) with evidence of relationships to the core SCT variables. Evidence for relationships in the proposed model (Fig. 1) was obtained from both theoretical and empirical sources.
Fig. 1.
Full proposed model of adherence
SCT proposes that personal factors, environmental (social) factors, and behavioral factors all interact to determine behavior (Bandura 1997). The central construct of the SCT is perceived self-efficacy, defined by Bandura (p. 21) as “a judgment of one’s ability to organize and execute given types of performances.” Self-efficacious people are more successful in performing specific behaviors because they are more likely than others to persevere even under difficult situations until their goals are achieved. The results of several studies examining ART adherence support the relationship between self-efficacy and adherence in which higher levels of self-efficacy correspond to higher rates of ART adherence (Catz et al. 2000; Gifford et al. 2000; Tuldra et al. 1999).
A second core SCT variable is outcome expectancy, which is defined as “a judgment of the likely consequence [a] performance will produce” (Bandura p. 21). People who expect positive outcomes associated with behaviors are more likely to perform that behavior than people who expect negative or neutral outcomes. The relationship between outcome expectancy and ART adherence has received some support, particularly when outcome expectancy is conceived of as a person’s belief in medication efficacy or attitude towards adherence (Godin et al. 2005; Viswanathan et al. 2005).
SCT proposes that beliefs about one’s abilities influence both thoughts and affective states. Highly efficacious people tend to think about positive outcomes associated with behaviors, thus the proposed link between self-efficacy and outcome expectancy (Fig. 1). In addition, low self-efficacious people are prone to self-disparaging thoughts and demoralization that in turn lead to depressive ideation. The latter proposition is supported by empirical evidence showing a relationship between self-efficacy and depression (Arnstein et al. 1999; DiIorio et al. 2004; Ong and Walsh 2001). Moreover, several investigators have found that higher levels of depression correspond to lower levels of ART adherence (Ammassari et al. 2004; Gonzalez et al. 2004; Kleeberger et al. 2004).
Another core SCT variable is social support which is important to the development of self-efficacy beliefs (Bandura 1997). Studies among people with HIV provide evidence for a positive relationship between support and self-efficacy (Godin et al. 2005) and a negative relation between being in a primary relationship and depression (Goldstein et al. 2005).
The second set of variables included in the model was composed of those identified in ART adherence literature and related to the above set of core SCT variables. These variables are spirituality, stigma, stress, patient satisfaction, and patient participation in decision-making. Studies show that people with HIV who are more spiritual report more positive health practices (Latkin et al. 2002), more hope and social support (Ironson et al. 2002), less affective or emotional distress (Ironson et al. 2002; Sowell et al. 2000), and fewer depressive symptoms (Coleman 2004; Sterk et al. 2003). In contrast both stigma and stress have been noted to have negative effects on well being. People who report higher levels of stigma or stress tend to be less efficacious (Airlie et al. 2001; Reynolds et al. 2004) and report more depressive symptoms (Lee et al. 2002; Mazure and Maciejewski 2003).
Finally, a patient’s relationship with their health care provider plays an important role in adherence (Altice et al. 2001; Heisler et al. 2002; Murphy et al. 2004; Schneider et al. 2004). In a longitudinal analysis of adherence to HIV medication, Godin et al. (2005) found patient-doctor satisfaction to be a significant predictor of attitude. In a study of antiretroviral adherence among incarcerated HIV-infected women, Mostashari et al. (1998) found that women expressing more positive relationships with the physicians also reported higher levels of ART adherence.
In summary, we hypothesized that the personal and social variables of self-efficacy, outcome expectancy, and depression mediate the relationships of the personal and socially related variables of social support, spirituality, stigma, stress, patient satisfaction, and patient participation in decision-making to ART adherence.
Methods
The data for this analysis came from the Get Busy Living study, a 5-year study funded by the National Institute of Nursing Research. The primary aim of the project was to evaluate an intervention based on Motivational Interviewing (MI) designed to promote adherence to ART. The study was conducted at a clinic that serves people with HIV located in a large southeastern metropolitan area.
Prior to the initiation of the study, the protocol was reviewed and approved by the Emory University Institutional Review Board and by the research boards serving the clinic. Clients were eligible if they were referred by a nurse educator at the clinic and met the following inclusion criteria: (1) infected with HIV; (2) prescribed a multi-drug regimen for the first time or made a change in one or more of their current drugs; (3) 18 years of age or older; (4) spoke English; (5) had a telephone and VCR or access to one; (6) mentally stable as determined by screening assessments; and (7) willing to participate.
Participants signed informed consent forms and then were screened for eligibility. Eligible participants returned within three weeks for a baseline assessment. Following the assessment, they were randomly assigned to the treatment and control groups. Data for this analysis were from the baseline assessment. (See DiIorio et al 2007 for a more detailed description of the study methods).
Measures
The analysis began with developing and testing measurement models for each latent variable. Each variable was measured using standard scales, which varied in length from 4–50 items. The goal of the initial analysis was to select the observed variables (items) that best represented the constructs included in the model. Four to six observed variables for each latent construct were selected from among the items appearing on the scales that had been selected as measures of the study variables. The results of item analysis and factor analysis were used to identify items for potential inclusion as observed measures of a construct. First, factor analysis was used to determine the underlying structure of each scale, and for scales in which factors were clearly identified, items were selected from one factor and the construct refined. For scales in which factors were not clearly identified, item analysis was used to select the items for use in the measurement model. Below each of the original study measures is described along with the process used to select the items and the list of items used to measure the construct.
Adherence was measured using 14 self report items from The UCSF Adherence Questionnaire (Chesney et al. 2000) that describe reasons for missing medication during the past 30 days. Higher scores indicate fewer reasons for missing medication and thus are associated with greater adherence. Five items that loaded together during factor analysis were selected for use in the measurement model. The construct consisted of questions that addressed logistical problems with remembering to take the medication as opposed to conscious decisions about the pills themselves. The five items composing the construct were: Were away from home; Were busy with other things; Simply forgot; Had a change in daily routine; and Fell asleep/slept through dose time. The internal consistency of the five items as measured by Cronbach’s alpha was .86.
Medication-taking self-efficacy was measured using four items from the Antiretroviral Self-Efficacy Scale. The 19-item scale was based on Bandura’s (1997) conceptualization of self-efficacy and on a similar scale used for people with epilepsy (DiIorio et al. 2004). The four items available at baseline were: I can always take my HIV medications when I am away from home; I can stay on my HIV medications most of the time; I can always take my HIV medications on holidays, birthdays, vacations, and other special occasions; I can always follow my HIV medication schedule. Higher ratings correspond to higher levels of perceived self-efficacy. The items reflected acceptable internal consistency with a Cronbach’s alpha of .83.
Expected outcomes or attitudes related to taking anti-retroviral medications as ordered were measured using a scale called the Antiretroviral Attitude Scale, adapted from a similar scale developed for people with epilepsy (DiIorio et al. 2004). The following four items were asked in the baseline assessment: If I take my HIV medications, my viral load will go down; If I take my HIV medications, my T cells or immune cells will go up; If I take my HIV medications, I will live longer; If I take my HIV medications, I will get back to my usual weight. Higher levels signify more positive outcome expectancies of adhering to medication. Cronbach’s alpha for these items was .79.
Depression was measured by the Center for Epidemiologic Studies Depression Scale (CES-D), developed for assessment of symptoms of depression in the general population (Radloff 1977). Higher scores indicate higher levels of depression. Thus, four items with the highest item to total correlations were selected to represent this construct in the measurement model. These items were: I felt depressed; I felt sad; I felt that I could not shake off the blues even with the help of my family and friends; I felt lonely. Cronbach’s alpha for the set of items was .84.
The Personal Resource Questionnaire85 Part 2 (PRQ85-2, (Brandt and Weinert 1981) was used to measure social support. Higher scores indicate greater levels of support. The four items with the highest item to total correlation were selected for use in the measurement model. All four were within the Intimacy subscale. The items were: I have people to share social events and fun activities with; If I need advice there is someone who would assist me to work out a plan for dealing with the situation; When I am upset there is someone I can be with who lets me be myself; There is someone who loves and cares about me. The Cronbach’s alpha was .83.
Spiritual well-being was assessed using the Religious Well Being (RWB) subscale of the Spiritual Well-Being Scale (SWBS) developed by Paloutzian and Ellison (1982). Higher scores correspond to increased levels of religious well being. The four items included in this analysis were selected based on factor loadings and reflect positive statements about a person’s relationship with God. The four items were: I believe that God is concerned about my problems; My relationship with God helps me not to feel lonely; I feel most fulfilled when I’m in close communion with God; My relation with God contributes to my sense of well-being. The internal consistency of these items was .89 as measured by Cronbach’s alpha.
Stigma was measured using the personal stigma items from the Perceived Stigma of HIV/AIDS Scale (Pequegnat et al. 2001). Higher scores signify higher levels of perceived stigma. Four items were selected from this scale using factor analysis. The resulting construct addressed the belief that others were justified in avoiding contact with someone with HIV and, conversely, the belief that their own illness was a matter of bad luck. The four items were: I understand why people would reject my friendship because I have HIV; I agree with mothers who do not want their children to play with my children because of my HIV; Because of my HIV, I should not hold a new infant; I think that my getting HIV was just a matter of bad luck. The Cronbach’s alpha for the items was .77.
The Difficult Life Circumstances Scale (Barnard 1994) was used to assess life-events of persons living in poverty or in ongoing stressful life circumstances. The scale provides an index of the number of stressful circumstances with which a person must contend. Four items were selected based on their item to total correlations: Do you feel that you do not have enough privacy? Does someone in your household other than you or your partner have problems with alcohol or drugs? Is someone other than your current partner presently abusing you sexually, physically, or emotionally? Are you having regular arguments or conflicts with any family members? The items reflected lack of privacy, arguments with family, and problems with drugs and abuse by someone other than the participant’s partner. The reliability coefficient, a Cronbach’s alpha of .51, was somewhat lower among these items as might be expected of an index.
The Patient Satisfaction Questionnaire-III from the Medical Outcomes Study (Marshall et al. 1993) was used to measure patient satisfaction. Higher scores translate to increased levels of satisfaction. The four items with the highest item to total correlation within the Communication Satisfaction subscale were used in the measurement model. These items were: Doctors are good about explaining the reasons for medical tests; During my medical visits, I am always allowed to say everything that I think is important; Doctors sometimes ignore what I tell them; Doctors listen carefully to what I have to say. The Cronbach’s alpha was .73.
The Multidimensional Desire for Control Scale (Anderson et al. 1989) was used to measure patient participation in decision-making (decision-making). The four items that correspond to shared decision making were selected for inclusion in the measurement model. Higher scores indicate more desire to share in decision making with one’s health care provider. The four items were: The doctor and I will be equal partners in establishing the treatment goals; The doctor and I will make decisions about my medical care together, on an equal basis; The doctor will give me a choice about what medication I should use at home; The doctor and I will supervise my treatment program together. The reliability coefficient for this subscale was .89 as measured by Cronbach’s alpha.
Data Analysis
Prior to testing the model, descriptive statistics for the observed variables, including skewness and kurtosis, were evaluated using SPSS Version 13.0. Variables within the Difficult Life Circumstances scale for which the participants selected not applicable were set to zero as the lack of applicability was assumed to mean that the participant was not experiencing the circumstance. Following this procedure, we replaced missing item responses within any scale with the participant’s mean score if the participant had completed 75% or more of the total scale.
Confirmatory factor analysis was performed using Lisrel 8.72 to test the measurement model for each latent construct. The fit of each measurement model was assessed using the Root Mean Square Error of Approximation (RMSEA) (Browne and Cudeck 1993) and the Goodness of Fit Index (GFI) (Jöreskog and Sorbom 1984). Model modification indices were consulted in cases where confirmatory factor analyses did not result in acceptable measures of fit (MacCallum 1986).
Structural equation modeling was then employed using Lisrel 8.72. Initially, the entire theoretically derived and literature based model was tested. We then proceeded to test five less complicated models by eliminating paths based on statistical (P > .10) and conceptual criteria. In order to identify the most salient constructs, we then included only the core variables of self-efficacy, outcome expectancy and depression with reasons for non-adherence as the dependent variable, and kept only those constructs that were significantly associated. Given the well-established theoretical framework from which we were working, we decided to retain the core variables of self-efficacy, outcome expectancy and depression with reasons for non-adherence as the dependent variable as long as empirically possible. Subsequently, we focused on the removal of more distal variables that were shown to be non-significant in the model. These resulting models were again evaluated using the RMSEA (Browne and Cudeck 1993) and the GFI (Jöreskog and Sorbom 1984) as the primary measures of fit along with χ2/df, AGFI, NFI, and NNFI.
Results
A total of 236 participants were included in the final model. Eleven participants were eliminated from the sample due to incomplete data for the selected variables. The age of those included in the analysis ranged from 22 to 61 years with a mean of 40.98 years (SD = 7.125). The majority of the sample was male (66.5%), and most participants were Black/African American (87.3%). A majority of the sample had completed high school (86.4%), and 30.5% had attended college or technical school, and an additional 6% had graduate or professional degrees. Slightly more than half of the sample had never been married (52.1%). Approximately 30% were separated, widowed or divorced, and the remaining 20% were married or in a committed relationship. For the most part, participants did not work for pay (80.8%) and a majority did not live alone (65.7%). Most participants (81.7%) reported an income of ≤$950 per month. The results of the analysis of demographic variables are displayed in Table 1.
Table 1.
Descriptive statistics for demographic variables
| Variable | Stratum | N | Col % | Adherence Score
|
|
|---|---|---|---|---|---|
| Mean | SD | ||||
| Age group | 20 | 10 | (4.2) | 37.50 | 4.33 |
| 30 | 85 | (36.0) | 35.52 | 7.07 | |
| 40 | 111 | (47.0) | 36.78 | 7.25 | |
| 50+ | 30 | (12.7) | 37.67 | 6.61 | |
| Gender | Female | 75 | (31.8) | 36.36 | 8.20 |
| Male | 157 | (66.5) | 36.50 | 6.48 | |
| Transgender | 4 | (1.7) | 37.25 | 3.59 | |
| Race | Black/African American | 206 | (87.3) | 36.10 | 7.28 |
| White | 18 | (7.6) | 38.94 | 3.56 | |
| Other | 12 | (5.1) | 39.08 | 4.94 | |
| Education | <High school | 32 | (13.5) | 34.59 | 9.22 |
| High school | 118 | (50.0) | 36.10 | 7.52 | |
| College/Technical school | 72 | (30.5) | 37.54 | 4.88 | |
| Graduate/Professional | 14 | (5.9) | 38.36 | 5.20 | |
| Monthly income | ≤$500 | 62 | (29.1) | 37.27 | 5.77 |
| $501–$750 | 88 | (41.3) | 35.51 | 8.21 | |
| $751–$950 | 24 | (11.3) | 36.13 | 6.06 | |
| $951–$1150 | 15 | (7.0) | 37.73 | 5.31 | |
| $1151–$6000 | 24 | (11.3) | 37.38 | 8.18 | |
| Marital status | Married/partner | 47 | (19.9) | 35.64 | 7.73 |
| Separate/widowed/divorced | 66 | (28.0) | 35.11 | 8.73 | |
| Never married | 123 | (52.1) | 37.52 | 5.41 | |
| Employment | Work for pay | 45 | (19.2) | 36.53 | 6.20 |
| Do not work for pay | 189 | (80.8) | 36.42 | 7.23 | |
| Living situation | Alone | 81 | (34.3) | 36.98 | 6.98 |
| Not alone | 155 | (65.7) | 36.21 | 7.04 | |
Analysis of internal consistency resulted in more than adequate reliability for all measures except difficult life circumstances, which fell below the cutoff of .70. Skewness was evident in all four of the self-efficacy variables, three of the four patient satisfaction variables, and two of the four social support items. The indicators for difficult life circumstances and decision-making also showed evidence of skew. These results are displayed in Table 2.
Table 2.
Descriptive statistics for dependent and psychosocial variables in the reduced models (N = 236)
| Variable | No. of items | Levels | α for selected items |
|---|---|---|---|
| Mean (SD) | Skewness | Kurtosis | |
| Adherence: reasons for missing | 14 (5 selected) | 0–3 | .863 |
| Away from home | 2.25 (.88) | −0.84 | −0.35 |
| Busy with other things | 2.44 (.80) | −1.27 | .70 |
| Simply forgot | 2.47 (.80) | −1.32 | 0.65 |
| Change in daily routine | 2.49 (.80) | −1.41 | 1.04 |
| Fell asleep/slept through dose time | 2.33 (.86) | −0.99 | −0.14 |
| Self-Efficacy | 4 (4 selected) | 1–10 | .827 |
| Take when away from home | 8.58 (2.16) | −1.65 | 2.28 |
| Can stay on most of the time | 9.13 (1.7) | −2.76 | 8.52 |
| Take on special occasions | 8.99 (2.07) | −2.51 | 5.83 |
| Can always follow schedule | 8.56 (1.91) | −1.54 | 2.22 |
| Depression | 20 (4 selected) | 0–3 | .844 |
| Felt depressed | 0.74 (.88) | 1.02 | 0.19 |
| Felt sad | 0.61 (.85) | 1.34 | 1.05 |
| Could not shake off blues | 0.61 (.86) | 1.24 | 0.62 |
| Felt lonely | 0.86 (1.0) | 0.96 | −0.21 |
| Stigma | 24 (4 selected) | 1–4 | .771 |
| Understand why people reject friendship | 2.18 (.99) | 0.50 | −0.74 |
| Other children should not play with my children | 2.03 (1.1) | 0.71 | −0.87 |
| I should not hold an infant | 2.06 (1.1) | 0.66 | −0.89 |
| Getting HIV was just bad luck | 2.31 (1.0) | 0.24 | −1.07 |
| Satisfaction | 50 (4 selected) | 1–5 | .733 |
| Doctors good about explaining reasons for tests | 4.30 (1.0) | −1.79 | 2.88 |
| Allowed to say what I think | 4.42 (1.0) | −2.05 | 3.52 |
| Doctors ignore me | 3.83 (1.3) | −0.78 | −0.62 |
| Doctors listen carefully | 4.28 (1.0) | −1.86 | 3.37 |
| Social support | 25 (4 selected) | 1–7 | .832 |
| People to share activities | 5.49 (1.6) | −1.32 | 0.86 |
| People to work out a plan | 5.69 (1.4) | −1.84 | 3.37 |
| Someone lets me be myself | 5.47 (1.7) | −1.41 | 1.10 |
| Someone loves and cares | 6.23 (1.2) | −2.41 | 6.84 |
| Difficult life | 33 (4 selected) | 0 or 1 | .509 |
| Not enough privacy | .43 (.50) | .29 | −1.93 |
| HH member with alcohol/drug problem | .16 (.37) | 1.86 | 1.46 |
| Non-partner abuse | .08 (.27) | 3.21 | 8.40 |
| Arguments/conflicts with family | .19 (.39) | 1.62 | .63 |
| Decision-making | 4 (4 selected) | 1–5 | .892 |
| Partners in est. treatment goals | 4.42 (1.2) | −2.11 | 3.24 |
| Make decisions about care together | 4.31 (1.2) | −1.81 | 2.18 |
| Doctor will give choice about meds | 4.28 (1.2) | −1.72 | 1.82 |
| Supervise my treatment together | 4.50 (1.1) | −2.34 | 4.52 |
In general, the pre-specified measurement model for each latent construct showed evidence of adequate fit and did not require additional modification. However, in the case of the latent construct for adherence, the modification indices indicated that the errors of the reasons “Simply forgot” and “Fell asleep/Slept through dose time” should be allowed to co-vary. This modification was implemented for all models tested.
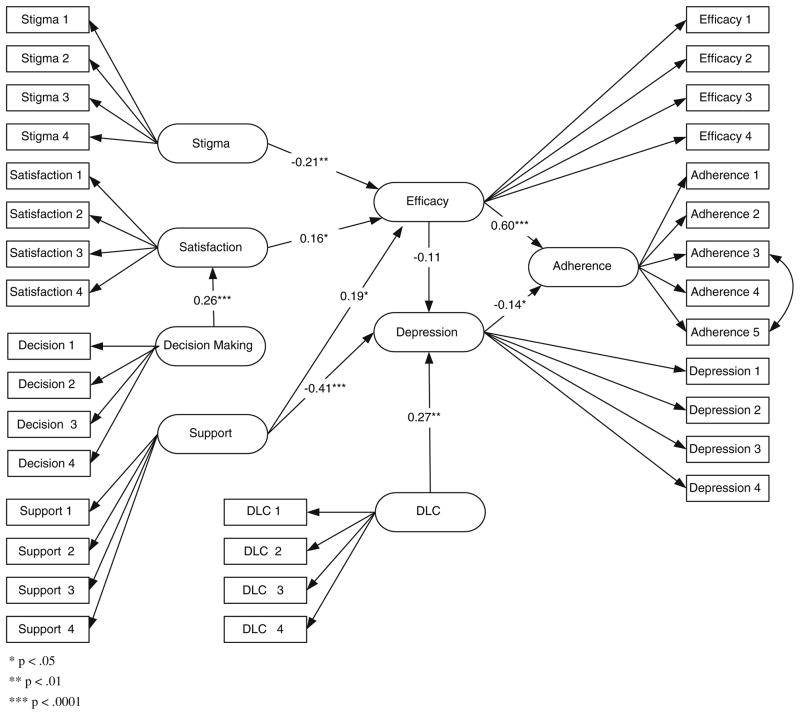
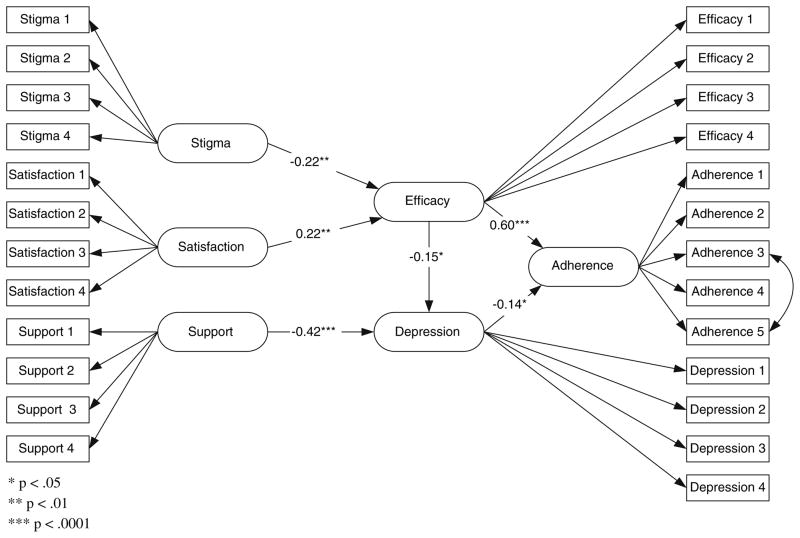
Although bivariate correlations among the latent variables indicated that some of the a priori specified paths would very likely be non-significant, we tested the full model as specified in Fig. 1. The fit statistics for this model are reported in Table 3. While these statistics could be considered adequate, there were nine non-significant paths with five of those having P-values far exceeding .10 (referring to the path letters in Fig. 1—c, h, l, m, n). The test statistics for paths e, d, g, and o suggested that they should initially remain in the model. In testing model A, we decided to retain outcome expectancy as this was a primary construct of the theoretical framework and to drop only paths h, l, m, and n. As might be expected, the fit statistics for this model were similar to those from the full model since the paths dropped were those contributing very little to the model. Given that outcome expectancy remained a non-significant predictor of adherence, we decided to remove this portion of the model and make one additional modification based on the observed bivariate relationships—a path from patient satisfaction to self-efficacy (s) was added maintaining path r (decision-making to satisfaction). As shown in Fig. 2, this model included the following paths: a, b, d, f, i, j, k, r, s. This model showed evidence of relatively good fit. The only non-significant path was that from self-efficacy to depression (t = −1.50). Two simpler models were also tested. The first, model C, was the same as model B with the path from decision-making to patient satisfaction eliminated. The final model tested was the model presented in Fig. 3 and in Table 3 as the reduced model. We made the decision to drop difficult life circumstances and decision-making because of previously identified distribution and measurement issues. Given the strength of the relationship between social support and depression and its relatively weaker relationship with self-efficacy, we decided to test a final reduced model with this path eliminated. These final model modifications were made, in part, to develop a model that would potentially have greater generalizability.
Table 3.
Bivariate correlations among latent variables and fit statistics for tested models
| ADH | SE | OE | DEP | SOC | SPR | STG | DFL | COM | |
|---|---|---|---|---|---|---|---|---|---|
| SE | .632*** | ||||||||
| OE | .077 | .202* | |||||||
| DEP | −.283*** | −.244** | −.128 | ||||||
| SOC | .156* | .266*** | .136 | −.456*** | |||||
| SPR | .001 | .093 | .234** | −.215** | .412*** | ||||
| STG | −.220** | −.233** | −.003 | .084 | −.134 | −.082 | |||
| DFL | −.224* | −.195 | −.145 | .321** | −.079 | .040 | .118 | ||
| COM | .140 | .229** | .380*** | −.165* | .338*** | .314*** | −.091 | −.031 | |
| DM | −.034 | .148* | .295*** | .012 | .052 | .206** | −.150* | .108 | .254*** |
| Model & fit statistics | |||||||||
| Model | Pathsa Included | χ2 (df) P-value | χ2/df | GFI | AGFI | NFI | NNFI | RMSEA | |
| Full | a–r | 921.87 (750) .00002 | 1.229 | .839 | .816 | .876 | .964 | .031 | |
| A | a–g, i–k, o–r | 923.09 (754) .00002 | 1.224 | .839 | .816 | .876 | .965 | .030 | |
| B | a, b, d, f, i–k, r, sb | 573.59 (479) .0019 | 1.197 | .871 | .849 | .894 | .973 | .029 | |
| C | a, b, d, f, i, j, s | 423.03 (363) .0161 | 1.165 | .890 | .868 | .911 | .983 | .027 | |
| Reduced | a, b, d, i, j, s | 322.95 (265) .0085 | 1.219 | .901 | .879 | .928 | .984 | .031 | |
See Fig. 1 for path
Model modified by adding a path from Communication Satisfaction to SE (noted as path s)
Note: ADH = Adherence, SE = Self Efficacy, OE = Outcome Expectancy, DEP = Depression, SOC = Social Support, SPR = Spirituality, STG = Stigma, DFL = Difficult Life Circumstances, COM = Communication Satisfaction, DM = Decision-making
P < .05,
P < .01,
P < .001
Fig. 2.
Model of adherence (model B)
Fig. 3.
Reduced model of adherence
Final Model
After testing multiple models, a final model was decided upon based on theoretical soundness, literature support and empirical tests. The final model is displayed in Fig. 3. In this model, self efficacy and depression were found to have direct associations with the measure of adherence; and stigma, patient satisfaction, and social support had indirect associations with adherence through either associations with self-efficacy or depression. The model revealed a positive and statistically significant association between self efficacy and fewer reasons for non-adherence (higher scores indicates better adherence) and a statistically significant, negative association between depression and fewer reasons for non-adherence. There was also a negative association between self efficacy and depression. This association was significant and equivalent to that between depression and reasons for non-adherence. Stigma and patient satisfaction were both significantly correlated with self efficacy, with the former relationship being negative and the latter being positive. Social support was significant in a negative association with depression.
The GFI for the final model was .90 and the RMSEA was 0.031 A GFI is considered acceptable if it is .90 or above (Jöreskog and Sorbom 1984) and the RMSEA should be less than or equal to 0.10 (Browne and Cudeck 1993). The chi-square was significant at 0.0085, but the chi-square value itself was only 1.2 times its degrees of freedom, which is considered within the acceptable threshold of twice the degrees of freedom for models with a large number of observed variables (Marsh and Hocevar 1985).
Discussion
The purpose of this study was to test a model of medication adherence among individuals taking antiretroviral medications. Structural equation modeling was used to test the proposed model examining the effects of several psychosocial variables on medication adherence. The core aspect of the model, derived from social cognitive theory, was partially supported. Self efficacy and depression were directly related to adherence, and self-efficacy was found to have a weak indirect relationship to adherence through its association with depression. These relationships lend further support to previous studies that have investigated both the role of self-efficacy and depression on medication adherence (Catz et al. 2000; Gonzalez et al. 2004; Kleeberger et al. 2004). Moreover, the results provide support for self-efficacy theory. Bandura (1997) reminds us that the relationships among behavior, efficacy beliefs and depression are quite complex. Under demanding conditions such as taking antiretroviral medications, highly self-efficacious people tend to confront challenges and persevere to overcome barriers to adherence. On the other hand low self-efficacious people are often quick to blame themselves for their inability to take their medications as ordered. Such negative self-evaluations can lead to despondency and depression, which in turn can exacerbate one’s inability to take medications.
Based on theory and empirical data, we proposed a link between social support and two constructs—self-efficacy and depression. Model testing revealed a strong relationship between social support and depression. Thus, participants in this study reporting high levels of social support tended to have fewer depressive symptoms, which in turn supported greater adherence. In the full model and in models A and B, self-efficacy, was found to mediate the relationship between social support and adherence as proposed. In an exploratory model, in which we only included social support, self-efficacy, depression, and adherence, both self-efficacy and depression mediated the relationship between social support and adherence. This set of relationships was comparable to that of Simoni (2002) who found that both depression and self-efficacy served as mediators of social support among African American and Puerto Rican men and women. In our analysis, the path between social support and self-efficacy was diminished when the construct of patient satisfaction was included in the model. This latter finding suggests that the provider played a more important role in enhancing medication-taking efficacy than did general support from family and friends among our sample. DiMatteo (2003) has studied patient-provider communication extensively and has shown that patients do listen to their providers. Moreover, their perceptions of providers, including how well they communicate, can have long term consequences in how people manage their disease regimens. Much like our findings, Godin et al. (2005) found the patient’s relationship with their physicians predicted their level of efficacy, which in turn supported ART adherence. The current study adds to these studies by proving additional support for the role of providers in enhancing efficacy beliefs.
Outcome expectancy, a core social cognitive construct, failed to mediate the relationship between self-efficacy and adherence as expected based on theory. Preliminary analysis indicated that the relationship between outcome expectancy and adherence was relatively small. Moreover, the measurement model for outcome expectancy showed poor fit relative to the other latent constructs included in the model. The small bivariate relationship and the poor fit of the measurement model could, in part, be due to the limited variability and a ceiling effect noted in the responses to the individual outcome expectancy items. Our results are not unlike those of other investigators who have found that outcome expectancy may not be as strong a variable when other relationships are considered within adherence models. In a path analysis of epilepsy medication management, DiIorio et al. (2004) also reported a lack of association between outcome expectancy and self-management. In the full model, it was interesting to note that the paths o (spirituality), p (decision-making), and q (patient satisfaction) leading to outcome expectancy were statistically significant. This provides some support for the notion that the patient-provider relationship is an important determinant of a patient’s understanding of and outcome expectancy regarding engagement in a particular treatment regimen. These results point to a need to further explore the construct of outcome expectancy and its measurement.
As expected, self-efficacy mediated the relationship between stigma and adherence. The relationships were moderate and showed that high levels of perceived stigma tended to deflate one’s sense of confidence in taking medications, which in turn negatively affected adherence. The association between stigma and self-efficacy was alluded to by Goffman (1963) who noted that “the standards he [person with stigma] has incorporated from the wider society equip him to be intimately alive to what others see as his failing, inevitably causing him, if only for moments, to agree that he does indeed fall short of what he ought to be.”(p. 7). These results extend our understanding of how stigma can play a role in adherence behaviors by influencing perception of how well one can deal with the complexity of medication management.
Several variables that were tested but not retained in our final reduced model were spirituality, difficult life circumstances, and decision-making. We expected that spirituality might be an important variable because of the mention by the participants of the role of spirituality in dealing with the disease. While it may play an important role in how patients deal with the disease, it may not be associated with engaging in the specific behavior of taking one’s medication. The difficult life circumstances variable and the decision-making variable were not included in the final model because of concerns regarding measurement and specificity of the constructs, limiting generalizability and stability of the coefficients.
Implications for Practice
Overall the relationships within the model have implications for practice including the development of adherence interventions. Our results suggest that adherence interventions that support self-efficacy and address depressive symptoms may function to improve or maintain desirable levels of medication taking. Attempts to disrupt the vicious cycle of low self-efficacy, depression, and non adherence can begin with interventions directed at modifying depression or alternatively by enhancing self-efficacy and developing strategies to address real barriers to medication taking. While our results and those of others suggest that social support may play more of an indirect rather than direct role in promoting adherence, social support along with patient satisfaction and stigma play key roles in adherence behavior and should be considered in intervention approaches. Interventions that attempt to improve social support, improve patient satisfaction, and reduce stigma can serve to improve the core factors that are associated with medication adherence. A secondary contribution of this paper is the development of smaller scales with fewer items to measure complex adherence-related constructs. These scales demonstrated adequate reliability during testing with the present sample. The use of smaller scales as opposed to longer measures in adherence research reduces respondent burden. Future research should explore the reliability and validity of these scales and the feasibility for use in research studies.
Limitations
The model we tested was limited to psychosocial variables. As such, the model did not include other factors that might also influence medication adherence. These factors include medication related variables such as number of medications and number of doses. Access to care and financial concerns may also serve to interfere with adherence and were not considered in the present study. A second limitation was the presentation of a modified model as the final model. We urge caution in the interpretation of this model because we deleted several of the initial variables that were included based on theoretical or empirical evidence. Additional research is necessary to determine whether or not this exploratory model is supported. It is important to consider that replication of this model does not mean that other models do not exist. Once the model is validated, we suggest adding additional regimen specific and structural variables to develop a more comprehensive medication adherence model.
Acknowledgments
This study was funded by a grant from the National Institute of Nursing Research R01 NR04857. We wish to acknowledge the assistance of the Infectious Disease Program in the conduction of this study. We appreciate the assistance of the staff and the contributions of the participants who enrolled in the study.
Contributor Information
Colleen DiIorio, Email: cdiiori@sph.emory.edu, Department of Behavioral Sciences and Health Education, Rollins School of Public Health, Emory University, 1518 Clifton Rd., Room: 560, Atlanta, GA 30322, USA.
Frances McCarty, Email: fmccart@sph.emory.edu, Department of Behavioral Sciences and Health Education, Rollins School of Public Health, Emory University, 1520 Clifton Rd., Room: 224, Atlanta, GA 30322, USA.
Lara DePadilla, Email: ldepadi@sph.emory.edu, Department of Behavioral Sciences and Health Education, Rollins School of Public Health, Emory University, 1518 Clifton Rd., Room: 560, Atlanta, GA 30322, USA.
Ken Resnicow, Email: kresnic@umich.edu, Health Behavior & Health Education School of Public Health, University of Michigan, 1420 Washington Heights (SPH II) Room 5009, Ann Arbor, MI 48109-2029, USA.
Marcia McDonnell Holstad, Email: nurmmcd@emory.edu, Nell Hodgson Woodruff School of Nursing, Emory University, 1520 Clifton Rd., Room 310, Atlanta, GA 30322, USA.
Katherine Yeager, Email: kyeager@sph.emory.edu, Department of Behavioral Sciences and Health Education, Rollins School of Public Health, Emory University, 1520 Clifton Rd., Room: 224, Atlanta, GA 30322, USA.
Sanjay M. Sharma, Email: sshar02@emory.edu, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, 341 Ponce de Leon Avenue, Room 402, Atlanta, GA, USA
Donald E. Morisky, Email: dmorisky@ucla.edu, Department of Community Health Sciences, UCLA School of Public Health, 650 Charles E. Young Drive South, Los Angeles, CA 90095-1772, USA
Brita Lundberg, Email: brita.lundberg@medscape.com, 5 Oakwood Terrace, Newton Centre, MA 02459, USA.
References
- Airlie J, Baker GA, Smith SJ, Young CA. Measuring the impact of multiple sclerosis on psychosocial functioning: The development of a new self-efficacy scale. Clinical Rehabilitation. 2001;15:259–265. doi: 10.1191/026921501668362643. [DOI] [PubMed] [Google Scholar]
- Altice FL, Mostashari F, Friedland GH. Trust and the acceptance of and adherence to antiretroviral therapy. Journal of Acquired Immune Deficiency Syndromes. 2001;28:47–58. doi: 10.1097/00042560-200109010-00008. [DOI] [PubMed] [Google Scholar]
- Ammassari A, Trotta MP, Murri R, Castelli F, Narciso P, Noto P, Vecchiet J, D’Arminio Monforte A, Wu AW, Antinori A AdICoNA Study Group. Correlates and predictors of adherence to highly active antiretroviral therapy: Overview of published literature. Journal of Acquired Immune Deficiency Syndromes. 2002;31(S3):s123–s127. doi: 10.1097/00126334-200212153-00007. [DOI] [PubMed] [Google Scholar]
- Ammassari A, Antinori A, Aloisi M, Trotta M, Murri R, Bartoli L, D’Arminio Monforte A, Wu AW, Starace F. Depressive symptoms, neurocognitive impairment, and adherence to highly active antiretroviral therapy among HIV-infected persons. Psychosomatics. 2004;45:394–402. doi: 10.1176/appi.psy.45.5.394. [DOI] [PubMed] [Google Scholar]
- Anderson LA, DeVellis RF, Boyles B, Feussner JR. Patients’ perceptions of their clinical interactions: Development of the multidimensional desire for control scales. Health Education Research. 1989;4:383–397. [Google Scholar]
- Arnstein P, Caudill M, Mandle CL, Norris A, Beasley R. Self efficacy as a mediator of the relationship between pain intensity, disability and depression in chronic pain patients. Pain. 1999;80:483–491. doi: 10.1016/S0304-3959(98)00220-6. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: W. H. Freeman and Company; 1997. [Google Scholar]
- Bangsberg DR, Perry S, Charlebois ED, Clark RA, Roberston M, Zolopa AR, Moss A. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15:1181–1183. doi: 10.1097/00002030-200106150-00015. [DOI] [PubMed] [Google Scholar]
- Barnard KE. Difficult life circumstances scale. Seattle: NCAST Publications; 1994. [Google Scholar]
- Bartlett JA, DeMasi R, Quinn J, Moxham C, Rousseau F. Overview of the effectiveness of triple combination therapy in antiretroviral-naive HIV-1 infected adults. AIDS. 2001;15:1369–1377. doi: 10.1097/00002030-200107270-00006. [DOI] [PubMed] [Google Scholar]
- Brandt PA, Weinert C. The PRQ-A social support measure. Nursing Research. 1981;30:227–230. [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park: Sage; 1993. pp. 136–162. [Google Scholar]
- Catz SL, Kelly JA, Bogart LM, Benotsch EG, McAuliffe TL. Patterns, correlates, and barriers to medication adherence among persons prescribed new treatments for HIV disease. Health Psychology. 2000;19:124–133. [PubMed] [Google Scholar]
- Chesney MA, Chambers DB, Ickovics JR, Gifford AL, Neidig J, Zwickl B, Wu AW. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: The AACTG adherence instruments. AIDS CARE. 2000;12:255–267. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- Coleman C. The contribution of religious and existential well-being to depression among African American heterosexuals with HIV infection. Issues in Mental Health Nursing. 2004;25:103–110. doi: 10.1080/01612840490249028-26. [DOI] [PubMed] [Google Scholar]
- DiIorio C, Shafer PO, Letz R, Henry TR, Schomer DL, Yeager KA. Project EASE: A study to test a psychosocial model of epilepsy medication management. Epilepsy and Behavior. 2004;5:926–936. doi: 10.1016/j.yebeh.2004.08.011. [DOI] [PubMed] [Google Scholar]
- DiIorio C, McCarty F, Resnicow K, Holstad MM, Soet J, Yeager K, Sharma SM, Morisky DE, Lundberg B. Using motivational interviewing to promote adherence to antiretroviral medications: A randomized controlled study. AIDS Cure. 2007 doi: 10.1080/09540120701593489. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMatteo MR. Future directions in research on consumer-provider communication and adherence to cancer prevention and treatment. Patient Education and Counseling. 2003;50:23–26. doi: 10.1016/s0738-3991(03)00075-2. [DOI] [PubMed] [Google Scholar]
- Fogarty L, Roter D, Larson S, Burke J, Gillespie J, Levy R. Patient adherence to HIV medication regimens: A review of published and abstract reports. Patient Education and Counseling. 2002;46:93–108. doi: 10.1016/s0738-3991(01)00219-1. [DOI] [PubMed] [Google Scholar]
- Gifford AL, Bormann JE, Shively MJ, Wright BC, Richman DD, Bozzette SA. Predictors of self-reported adherence and plasma HIV concentrations in patients in multidrug antiretroviral regimens. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2000;23:386–395. doi: 10.1097/00126334-200004150-00005. [DOI] [PubMed] [Google Scholar]
- Godin G, Cote J, Naccache H, Lambert LD, Trottier S. Prediction of adherence to antiretroviral therapy: A one-year longitudinal study. AIDS CARE. 2005;17:493–504. doi: 10.1080/09540120412331291715. [DOI] [PubMed] [Google Scholar]
- Goffman E. Stigma: Notes on the management of spoiled identity. Englewood Cliffs: Prentice-Hall, Inc; 1963. [Google Scholar]
- Goldstein RB, Johnson MO, Rotheram-Borus MJ, Kirshenbaum SB, Pinto RM, Kittel L, Pequegnat W, Mickalian MA, Weinhardt LS, Kelly JA, Lightfoot M NIMH Healthy Living Project Team. Psychological distress, substance use, and adjustment among parents living with HIV. Journal of the American Board of Family Practice. 2005;18:362–373. doi: 10.3122/jabfm.18.5.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golin CE, Liu H, Hays RD, Miller LG, Beck CK, Ickovics J, Kaplan AH, Wenger NS. A prospective study of predictors of adherence to combination antiretroviral medication. Journal of General Internal Medicine. 2002;17:756–765. doi: 10.1046/j.1525-1497.2002.11214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez JS, Penedo FJ, Antoni MH, Duran RE, Fernandez MI, McPherson-Baker S, Ironson G, Klimas NG, Fletcher MA, Schneiderman N. Social support, positive states of mind, and HIV treatment adherence in men and women living with HIV/AIDS. Health Psychology. 2004;23:413–418. doi: 10.1037/0278-6133.23.4.413. [DOI] [PubMed] [Google Scholar]
- Heisler M, Bouknight R, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. Journal of General Internal Medicine. 2002;17:243–251. doi: 10.1046/j.1525-1497.2002.10905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard AA, Arnsten JH, Lo Y, Vlahov D, Rich JD, Schuman P, Stone VE, Smith DK, Schoenbaum EE HER Study Group. A prospective study of adherence and viral load in a large multi-center cohort of HIV-infected women. AIDS. 2002;16:2175–2182. doi: 10.1097/00002030-200211080-00010. [DOI] [PubMed] [Google Scholar]
- Ickovics JR, Cameron A, Zackin R, Bassett R, Chesney M, Johnson VA, Kuritzkes DR Adult AIDS Clinical Trials Group 370 Protocol Team. Consequences and determinants of adherence to antiretroviral medication: Results from Adult AIDS Clinical Trials Group Protocol 370. Antiviral Therapy. 2002;7:185–193. doi: 10.1177/135965350200700308. [DOI] [PubMed] [Google Scholar]
- Ironson G, Solomon GF, Balbin EG, O’Cleirigh C, George A, Kumar M, Larson D, Woods TE. The Ironson–Woods Spirituality/Religiousness Index is associated with long survival, health behaviors, less distress, and low cortisol in people with HIV/AIDS. Annals of Behavioral Medicine. 2002;24:34–48. doi: 10.1207/S15324796ABM2401_05. [DOI] [PubMed] [Google Scholar]
- Jöreskog K, Sorbom D. LISREL-VI user’s guide. 3. Mooresville: Scientific Software; 1984. [Google Scholar]
- Kleeberger CA, Buechner J, Palella F, Detels R, Riddler S, Godfrey R, Jaconson LP. Changes in adherence to highly active antiretroviral therapy medications in the multicenter AIDS cohort study. AIDS. 2004;18:683–688. doi: 10.1097/00002030-200403050-00013. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Tobin KE, Gilbert SH. Shun or support: The role of religious behaviors and HIV-related health care among drug users in Baltimore, Maryland. AIDS and Behavior. 2002;6:321–329. [Google Scholar]
- Lee RS, Kochman A, Sikkema K. Internalized stigma among people living with HIV-AIDS. AIDS and Behavior. 2002;6:309–319. [Google Scholar]
- MacCallum RC. Specification searches in covariance structure modeling. Psychological Bulletin. 1986;100:107–120. [Google Scholar]
- Machtinger E, Bangsberg DR. Peiperl L, Volberding PA, editors. Adherence to HIV antiretroviral therapy. HIV insite knowledge base [textbook on-line] 2005 Available at http://hivinsite.ucsf.edu/InSite?page=kb-03-02-09.
- Marsh H, Hocevar D. Application of confirmatory factor analysis to the study of self-concept: First and higher order factor models and their invariance across groups. Psychological Bulletin. 1985;97:562–582. [Google Scholar]
- Marshall G, Hays R, Sherbourne C, Wells K. The structure of patient satisfaction with outpatient medical care. Psychological Assessment. 1993;5:477–483. [Google Scholar]
- Mazure CM, Maciejewski PK. A model of risk for major depression: Effects of life stress and cognitive style vary by age. Depression and Anxiety. 2003;17:26–33. doi: 10.1002/da.10081. [DOI] [PubMed] [Google Scholar]
- Mostashari F, Riley E, Selwyn PA, Altice FL. Acceptance and adherence with antiretroviral therapy among HIV-infected women in a correctional facility. Journal of Acquired Immune Deficiency Syndromes & Human Retrovirology. 1998;18:341–348. doi: 10.1097/00042560-199808010-00005. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD, Hoffman D, Steers WN. Predictors of antiretroviral adherence. AIDS CARE. 2004;16:471–484. doi: 10.1080/09540120410001683402. [DOI] [PubMed] [Google Scholar]
- Ong AD, Walsh DA. Nicotine dependence, depression, and the moderating role of goal cognitions. Psychology of Addictive Behaviors. 2001;15:252–254. [PubMed] [Google Scholar]
- Paloutzian RF, Ellison CW. Loneliness, spiritual well-being and quality of life. In: Peplau LA, Perlman D, editors. Loneliness: A sourcebook of current theory, research and therapy. New York: Wiley Interscience; 1982. pp. 224–237. [Google Scholar]
- Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, Wagener MM, Singh N. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Annals of Internal Medicine. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- Pequegnat W, Bauman LJ, Bray JH, DiClemente R, DiIorio C, Hoppe SK, Jemmott LS, Krauss B, Miles M, Paikoff R, Rapkin B, Rotheram-Borus MJ, Szapocznik J. Measurement of the role of families in prevention and adaptation to HIV/AIDS. AIDS and Behavior. 2001;5:1–19. [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Schneider J, Kaplan SH, Greenfield S, Wenjun L, Wilson IB. Better physician-patient relationships are associated with higher reported adherence to antiretroviral therapy in patients with HIV infection. Journal of General Internal Medicine. 2004;19:1096–1103. doi: 10.1111/j.1525-1497.2004.30418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Frick PA, Lockhart D, Liebovitz D. Mediators of social support and antiretroviral adherence among an indigent population in New York City. AIDS Patient Care and STDS. 2002;16:431–439. doi: 10.1089/108729102760330272. [DOI] [PubMed] [Google Scholar]
- Sledjeski EM, Delahanty DL, Bogart LM. Incidence and impact of posttraumatic stress disorder and comorbid depression on adherence to HAART and CD4+ counts in people living with HIV. AIDS Patient Care and STDs. 2005;19:728–736. doi: 10.1089/apc.2005.19.728. [DOI] [PubMed] [Google Scholar]
- Sowell R, Moneyham L, Hennessy M, Guillory J, Demi A, Seals B. Spiritual activities as a resistance resource for women with human immunodeficiency virus. Nursing Research. 2000;49:73–82. doi: 10.1097/00006199-200003000-00003. [DOI] [PubMed] [Google Scholar]
- Sterk C, Klein H, Elifson KW. Perceived condom use self-efficacy among at-risk women. AIDS and Behavior. 2003;7:175–182. doi: 10.1023/a:1023950425731. [DOI] [PubMed] [Google Scholar]
- Tuldra A, Ferrer MJ, Fumaz CR, Bayes R, Paredes R, Burger DM, Clotet B. Monitoring adherence to HIV Therapy. Archives of Internal Medicine. 1999;159:1376–1377. doi: 10.1001/archinte.159.12.1376. [DOI] [PubMed] [Google Scholar]
- Viswanathan H, Anderson R, Thomas J., 3rd Evaluation of an antiretroviral medication attitude scale and relationships between medication attitudes and medication nonadherence. AIDS Patient Care and STDs. 2005;19:306–316. doi: 10.1089/apc.2005.19.306. [DOI] [PubMed] [Google Scholar]