Abstract
Beginning in 2009, the Centers for Medicare & Medicaid Services started publicly reporting hospital readmission rates as part of the Hospital Compare website. Hospitals will begin having payments reduced if their readmission rates are higher than expected starting in fiscal year 2013. Value-based purchasing initiatives including public reporting and pay-for-performance incentives have the potential to increase quality of care. There is concern, however, that hospitals providing service to minority communities may be disproportionately penalized as a result of these policies due to higher rates of readmissions among racial and ethnic minority groups. Using 2008 Medicare data, we assess the risk for readmission for minorities and discuss implications for minority-serving institutions.
Keywords: readmissions, disparities, health policy, Medicare, Hospital Compare, nursing
The quality of health care in the United States is often variable, particularly for racial and ethnic minorities (Hasnain-Wynia et al., 2007). Efforts to reduce racial and ethnic health disparities include recent value-based purchasing initiatives through the Centers for Medicare and Medicaid Services (CMS), which aim to improve quality through various types of public reporting and payment incentives (U.S. Department of Health and Human Services, 2007). Public reporting relies on providing comparative information of hospitals and providers, to monitor health outcomes, assess quality, and facilitate consumer choice. Through increased transparency and accountability, public reporting gives providers incentive to improve their quality of care. A related policy initiative involves direct payment incentives for quality outcomes (Institute of Medicine, 2006). Pay-for-performance directly incentivizes quality by making a portion of payments to providers or hospitals dependent on quality-related outcomes.
Value-based purchasing initiatives, if properly designed, hold promise for enhancing the quality of care at institutions serving a disproportionate share of minority patients (Chien, Chin, Davis, & Casalino, 2007). One concern however, is that these policy efforts may induce unintended negative consequences including the paradoxical effect of increasing racial and ethnic health disparities (Casalino et al., 2007; Hasnain-Wynia & Jean-Jacques, 2009; Ho, Moy, & Clancy, 2010; Hood, 2007; Werner & Asch, 2005). Given the risks of unintended consequences, examining how these quality initiatives differentially affect hospitals caring primarily for minority patients should be thoroughly considered, particularly if minority patients are at higher risk for the outcomes of interest. In this article, we focus on a pair of related policies: a public reporting requirement and payment incentive reform aimed at reducing preventable readmissions among Medicare beneficiaries. We begin with an overview of Medicare’s readmission policies and what is known about disparities in readmissions. We follow with a discussion of the theoretical risks embedded within these policies and the threat of widened health disparities. Then, using the CMS Hospital Compare readmission indicators as a guide, we examined baseline racial and ethnic disparities in the odds of all-cause 30-day readmission among Medicare beneficiaries with the conditions that will be affected by the policies (acute myocardial infarction [AMI], heart failure, and pneumonia). We end with the results of our analysis and implications.
Overview of Medicare’s Readmissions Policies
The Medicare Payment Advisory Commission (2007) reported to Congress that 75% of Medicare readmissions were potentially preventable and cost Medicare an extra US$15 billion per year, prompting a recommendation that Medicare introduce policies aimed at reducing readmissions. As part of an overall value-based purchasing initiative, CMS implemented a series of reforms, including public reporting requirements and pay-for-performance measures aimed at reducing preventable readmissions.
The Reporting Hospital Quality Data for Annual Payment Update, initiated pursuant to the Medicare Prescription Drug, Improvement and Modernization Act of 2003 and extended by the Deficit Reduction Act of 2005, established public reporting requirements for hospitals participating in the CMS Inpatient Prospective Payment System. These data began being publicly reported by CMS in concert with the Hospital Quality Alliance in 2004 on the Hospital Compare web site as an external incentive to improve quality and determine reimbursement. Through Hospital Compare, acute care facilities are now required to publicly report a range of quality measures to receive their annual payment updates as part of CMS’s overall value-based purchasing effort (Centers for Medicare & Medicaid Services, 2008). The three publicly reported conditions—AMI, heart failure, and pneumonia—were selected for inclusion in the Hospital Compare readmission measures because they are particularly common, costly, and often preventable. Public reporting of readmission rates is intended to bring about quality improvements by either motivating providers to increase their quality of care or by increasing the likelihood that patients select high-quality providers (Werner et al., 2009).
Under the 2010 Patient Protection and Affordable Care Act (PPACA; P.L. 111-148), as amended by the Health Care and Education Reconciliation Act (HCERA; P.L. 111-152), beginning in fiscal year 2013, hospitals with higher than expected readmission rates for AMI, heart failure, and pneumonia will receive a lower payment through the Medicare Inpatient Prospective Payment System than they otherwise would have received (Averill et al., 2009). Beginning with fiscal year 2015, the Secretary of the Department of Health and Human Services is also required, to the extent practicable, to expand the applicable conditions beyond the three current conditions. Goals of this performance-based payment policy include reducing Medicare costs and improving quality of care for Medicare beneficiaries.
Readmissions and Disparities
Another objective of the readmissions policies is reducing racial and ethnic health disparities (The Hospital Quality Alliance, 2010). Research has suggested that racial and ethnic minorities are more apt to experience a preventable hospital readmission. For instance, Alexander, Grumbach, Remy, Rowell, and Massie (1999) found that African Americans were more likely than Whites to be rehospitalized for many diagnoses including heart failure. In addition, Rathore et al. (2003) found that Black Medicare patients had higher rates of readmission following heart failure treatment than White Medicare patients. Though diabetes is not currently one of the readmission conditions considered by CMS, Jiang, Andrews, Stryer, & Friedman (2005) found higher readmission rates related to diabetes for non-White Hispanics and Blacks than for Whites.
Risks and Unintended Consequences
It may prove useful to construct public reporting and payment arrangements that encourage quality competition where the market has failed to do so; however, there is reasonable concern that such interventions may negatively affect those institutions that are undercapitalized and most in need of increased resources to improve quality of care (Rosenthal, Fernandopulle, Song, & Landon, 2004). Several studies have revealed threats to revenue for practices servicing high concentrations of minority patients in ambulatory care settings (Friedberg, Safran, Coltin, Dresser, & Schneider, 2010). Studies of hospitals caring disproportionately for racial and ethnic minorities also suggest that these institutions may be less able to earn bonus payments in Medicare’s hospital pay-for-performance program than those who do not (Werner, Goldman, & Dudley, 2008).
Performance ratings have equally drawn criticism from physicians in community settings caring for large numbers of minorities. Physicians in California, for example, contested the receipt of unfavorable clinical quality and patient satisfaction scores because clinical process measures favored the majority population and, therefore, disadvantaged physicians who served populations that were disproportionately minority with high disease burden (Hood, 2007). In light of such responses, there is concern that institutions and providers that provide most of the care to minority patients with increased chronic illness may be further burdened by the CMS readmissions policies as resources are steered away from these institutions. This is particularly concerning given research showing that a very small percentage of U.S. hospitals care for the large majority of elderly Black and Hispanic patients in the United States. (Jha, Orav, & Epstein, 2008; Jha, Orav, Li, & Epstein, 2007).
Another concern is that although it is assumed that hospitals will improve their quality of care to maintain high publicly reported values and receive payment incentives, they may also engage in less positive responses in an effort to “game” the system. Various researchers (Balsa & McGuire, 2003; Schulman et al., 1999; van Ryn & Burke, 2000) have found that many providers believe that minority patients are more likely to have high-risk social characteristics including being less educated, more likely to refuse treatment, less likely to comply with treatment, and delay seeking care for their comorbid conditions. It is unclear what underlies these beliefs, although bias (prejudice), clinical uncertainty, and stereotyping are possible reasons. When faced with the incentives of public reporting and pay-for-performance, however, individual providers may avoid minority patients who they believe will reduce their publicly reported ratings or result in a financial loss (Ryan, 2009). To the extent that such avoidance behaviors could occur in the context of hospital-based care, such actions may exacerbate health care related disparities in access and outcomes (Bhalla & Kalkut, 2010). As these policies begin to be implemented, it will be important to monitor for disparities. Thus the goal of our study was to examine the baseline risk of readmission by race following a hospitalization for one of the three conditions (heart failure, AMI, pneumonia) covered by the CMS readmissions policies.
Method
Data and Sample
We used data from the Medicare Provider Analysis and Review (MEDPAR) file for the year 2008. The MEDPAR data contain billing data for Medicare beneficiaries (except those in managed-care plans) discharged from CMS Inpatient Prospective Payment System participating hospitals.
We identified the first admission in 2008 as the index admission to calculate 30-day all-cause readmissions for all Medicare fee-for-service patients discharged from a short-term acute care hospital in 2008 with a principal diagnosis of heart failure, AMI, or pneumonia respectively. The specific ICD-9 codes used for identifying each of the conditions can be found at the Quality Net (2010) web site outlining the methodology for generating the Hospital Compare data. Transfers to another acute care facility were considered part of the same admission. Admissions were linked with a Beneficiary Identification Code.
We identified race using indicator variables based on the categorical race variable in the MEDPAR file, which indicates race as White, Black, Hispanic, Asian, North American native, Other, or unknown. Although Hispanic is often classified as ethnicity, CMS classifies Hispanic as a distinct race category in the MEDPAR file.
We also linked data from the American Hospital Association’s Annual Survey of hospitals from 2008. These data were used to identify hospital characteristics including teaching status, bed size, and technological status. Hospital bed size was defined as the number of hospital unit beds set up and staffed. Hospitals were categorized as small (fewer than 100 beds), medium-sized (100–250 beds), and large (250 or more beds) hospitals. Teaching status was based on the postgraduate trainee-to-bed ratio. Hospitals were classified as nonteaching if they had no postgraduate trainees, minor-teaching if they had a trainee–bed ratio of 1:4 or smaller, or major teaching if the trainee–bed ratio was higher than 1:4. Hospitals were classified as having high technological status if they provided transplant or cardiac surgery services.
Analysis
We estimated generalized estimating equation models (Zeger, Liang, & Albert, 1988) to evaluate the effect of race on the odds of 30-day all-cause readmission. Robust variance estimate techniques were used to calculate standard errors and confidence intervals. We used the Elixhauser, Steiner, Harris, & Coffey (1998) comorbidity indicators as well as the CMS Chronic Condition Data Warehouse indicators of comorbidity to identify comorbid illness. Models were estimated using SAS version 9.2 (SAS Institute Inc., 2008).
Results
Table 1 shows patient characteristics by condition: heart failure, AMI, and pneumonia. Chronic disease comorbidities, including, for example, Alzheimer’s disease, diabetes, depression, heart disease, and hypertension, are particularly prevalent among each of the cohorts. Black beneficiaries are disproportionately represented in the heart failure cohort. Table 2 shows the distribution of patients by hospital type and demonstrates that patients were predominantly treated in large, nonteaching hospitals.
Table 1.
Descriptive Characteristics of Index Admissions
| Patient characteristics | Heart failure (n = 239,953) | Acute myocardial infarction (n = 193,421) | Pneumonia (n = 350,740) |
|---|---|---|---|
| Age | 80.32 (SD 8.75) | 78.55 (SD 8.55) | 80.01 (SD 8.60) |
| Male | 105,745 (44%) | 96,938 (50%) | 156,630 (45%) |
| Race | |||
| White | 197,809 (82%) | 169,799 (88%) | 306,939 (87%) |
| Black | 30,706 (13%) | 15,132 (8%) | 26,986 (8%) |
| Hispanic | 5,177 (2%) | 3,174 (2%) | 6,822 (2%) |
| Other | 6,261 (3%) | 5,316 (3%) | 9,993 (3%) |
| Comorbidities | |||
| AMI | 12,565 (5.24%) | 26,171 (13.53%) | 26,986 (1.69%) |
| Alzheimer dementia | 50,575 (21.08%) | 32,174 (16.63%) | 98,146 (27.98%) |
| Atrial fibrillation | 85,533 (35.65%) | 25,334 (13.10%) | 66,344 (18.92%) |
| Hip fracture | 3,198 (1.33%) | 1,804 (0.93%) | 5,373 (1.53%) |
| Ischemic heart | 192,079 (80.05%) | 178,276 (92.17%) | 200,389 (57.13%) |
| Osteoporosis | 27,788 (11.58%) | 20,361 (10.53%) | 57,649 (16.44%) |
| Stroke/TIA | 19,615 (8.17%) | 13,739 (7.10%) | 29,839 (8.51%) |
| Paralysis | 4,422 (1.84%) | 4,533 (2.34%) | 9,318 (2.66%) |
| Peripheral vascular disease | 18,785 (7.83%) | 17,088 (8.83%) | 17,941 (5.12%) |
| Chronic pulmonary disease | 104,176 (43.42%) | 53,929 (27.88%) | 188,887 (53.85%) |
| Diabetes w/o chronic complications | 118,658 (49.45%) | 79,680 (41.20%) | 131,583 (37.52%) |
| Diabetes w/chronic complications | 14,622 (6.09%) | 7,594 (3.93%) | 12,189 (3.48%) |
| Hypothyroidism | 28,824 (12.01%) | 17,667 (9.13%) | 43,480 (12.40%) |
| Renal failure | 118,202 (49.26%) | 58,120 (30.05%) | 105,053 (29.95%) |
| Liver disease | 2,254 (0.94%) | 887 (0.46%) | 2,857 (0.81%) |
| Metastatic cancer | 18,138 (7.56%) | 14,168 (7.32%) | 39,339 (11.22%) |
| Rheumatoid arthritis | 63,739 (26.56%) | 43,103 (22.28%) | 99,010 (28.23%) |
| Obesity | 12,512 (5.21%) | 8,495 (4.39%) | 10,039 (2.86%) |
| Weight loss | 6,217 (2.59%) | 4,631 (2.39%) | 19,941 (5.69%) |
| Fluid and electrolyte disorders | 47,410 (19.76%) | 33,231 (17.18%) | 111,565 (31.81%) |
| Deficiency anemias | 42,772 (17.83%) | 21,093 (10.91%) | 63,135 (18.00%) |
| Depression | 43,560 (18.15%) | 27,334 (14.13%) | 80,923 (23.07%) |
| Hypertension | 127,543 (53.15%) | 114,149 (59.02%) | 197,855 (56.41 %) |
Note: These are the characteristics of patients with index admissions. AMI = acute myocardial infarction; TIA = transient ischemic attack.
Table 2.
Distribution of Patients by Hospital Characteristics for Each Condition
| Hospital characteristics | Heart failure (n = 239,953) | Acute myocardial infarction (n = 193,421) | Pneumonia (n = 350,740) |
|---|---|---|---|
| Teaching status | |||
| Nonteaching | 140,096 (58%) | 106,221 (55%) | 218,237 (62%) |
| Minor teaching | 76,757 (32%) | 63,496 (33%) | 103,373 (29%) |
| Major teaching | 23,100 (10%) | 23,704 (12%) | 29,130 (8%) |
| Bed size | |||
| Small | 29,963 (12%) | 13,896 (7%) | 56,706 (16%) |
| Medium | 78,539 (33%) | 55,815 (29%) | 120,848 (34%) |
| Large | 131,451 (55%) | 123,710 (64%) | 173,186 (49%) |
| High technology hospitals | 128,448 (54%) | 127,502 (66%) | 177,657 (51%) |
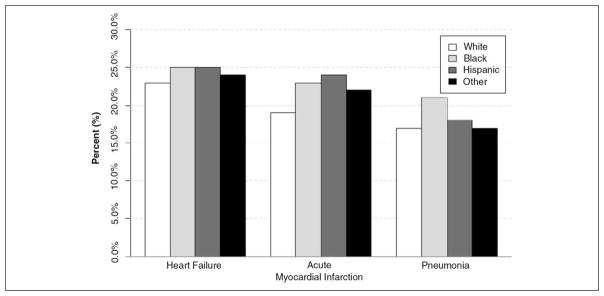
Figure 1 shows the percentage of readmissions by race. In all instances, Black and Hispanic Medicare beneficiaries were readmitted more frequently than White beneficiaries. Each of these differences between White and Black beneficiaries is significant (p < .01) and all differences between White and Hispanic beneficiaries are significant except for pneumonia (p < .01).
Figure 1.
Thirty-day readmission (%) by race and condition
Note: Asian and Pacific Islander, North American Native, and unknown race groups were combined in Other for this table due to relatively small numbers. Chi-square and corresponding p value (χ2[p]) is calculated separately for each group in reference to the White group. For heart failure: Black 63.01 (p < .001); Hispanic 9.17 (p = .002); Other 7.29 (p = .007). For acute myocardial infarction: Black 131.84 (p = .001); Hispanic 34.06 (p = .001); Other 23.23 (p = .001). For pneumonia: Black 231.90 (p < .001); Hispanic 2.65 (p = .103); Other 0.13 (p = .717).
Table 3 shows the results of generalized estimating equation models that controlled for patient and hospital covariates. Black beneficiaries had a 9% (OR = 1.09, 95% CI = 1.12-1.05), 13% (OR = 1.13, 95% CI = 1.18-1.08), and 21% (OR = 1.21, 95% CI = 1.25-1.17) higher odds of 30-day readmission for heart failure, AMI, and pneumonia respectively relative to White beneficiaries. Hispanic beneficiaries had a 20% (OR = 1.20, 95% CI = 1.32-1.10) higher odds of 30-day readmission for AMI relative to White beneficiaries. The odds of readmission was not significantly higher for Hispanic beneficiaries with pneumonia or heart failure.
Table 3.
Odds Ratios for Readmission Based on Race, 2008
| Race by condition | Odds ratio | 95% Confidence interval |
|---|---|---|
| Heart failure | ||
| Black | 1.09 | [1.12, 1.05] |
| Hispanic | 1.04 | [0.96, 1.11] |
| Acute myocardial infarction | ||
| Black | 1.13 | [1.18, 1.08] |
| Hispanic | 1.20 | [1.32, 1.10] |
| Pneumonia | ||
| Black | 1.21 | [1.25, 1.17] |
| Hispanic | 1.01 | [0.94, 1.08] |
Note: Sample size for heart failure analysis (n = 239,953); sample size for acute myocardial infarction analysis (n = 193,421); sample size for pneumonia analysis (n = 350,740).
Discussion
Our study reveals that in 2008, Black Medicare beneficiaries with heart failure, AMI, and pneumonia were more likely than Whites to be readmitted following an initial hospitalization. Hispanic beneficiaries had significantly higher odds of readmission for AMI. These effects remained significant even after controlling for patient comorbidities and hospital characteristics such as teaching status, bed size, and technological status. Other studies have examined readmissions in minority patients and have noted no differences in readmission between Blacks, Hispanics and Whites (Deswal, Petersen, Souchek, Ashton, & Wray, 2004; Yancy et al., 2008). Our study, however, is consistent with previous research, which found that race was an important determinant of readmission in chronic conditions (Curtis et al., 2008; Friedman & Basu, 2004; Jiang et al., 2005; Philbin & DiSalvo, 1998; Rathore et al., 2003).
Readmissions are common, represent high costs (Friedman & Basu, 2004), and in some respects indicate clinical tasks and interventions left undone (Ashton, Del Junco, Souchek, Wray, & Mansyur, 1997). Early readmissions may (conversely) reflect complex underlying problems such as unobserved factors that are unrelated to care processes but equally influence admission rates. In the case of hospitals serving large communities of minority patients, the use of readmission rates as an outcome for value-based purchasing policies raises concerns because it may fail to account for several factors related to the specific health care practices and community attributes of minority patients. Though not entirely conclusive (Baker, Stevens, & Brook, 1994, 1996; Gaskin et al., 2007), studies have found that Black and Hispanic patients are more likely to rely on hospitals as the most convenient and reliable source of care (Baker et al., 1994; Fuda & Immekus, 2006; LaCalle & Rabin, 2010). This utilization pattern may arise due to a number of underlying structural, political, and economic factors that contribute to limited access to regular primary care providers in minority communities (Mayberry, Mili, & Ofili, 2000; Williams & Rucker, 2000). Continuity of care may be further fragmented if minorities are seen routinely by a range of different health care providers (Hargraves & Hadley, 2003). Physicians servicing large proportions of minority patients have reported that coordination of care, ability to spend adequate time with patients during office visits, and obtaining specialty care is more difficult in these practices (Reschovsky & O’Malley, 2008). The confluence of access issues and physician constraints threaten care continuity and may influence readmission rates in hospitals serving minority communities. Our findings suggest that further study and additional consideration should be given to whether including patient demographics, the clustering of hospitals in specific regions, differences in patient utilization patterns, access to providers, or other socioeconomic factors in risk-standardized statistical models of readmissions is appropriate (Bhalla & Kalkut, 2010).
The inclusion of race in risk adjustment models can be controversial and there are justifiable reasons for not including race as a factor in risk adjustment. One of the foremost reasons is that the adjustment may mask important racial disparities that would otherwise indicate biases in care and not patient differences. Another important issue is measurement. Although data quality has improved, race has been measured differently over time and the quality of data varies significantly by source (Arispe, Holmes, & Moy, 2005; Kaplan & Bennett, 2003; LaVeist, 1994). Continued evaluation of the most appropriate models for use in implementing the readmissions policies will be important for researchers going forward.
Despite the difficulties of implementation of the CMS policies, the focus on hospitals as a source of disparities in readmissions is justified. In its landmark report, the Institute of Medicine (2002) highlighted the presence of inequitable hospital care quality as a concerning source of racial and ethnic health disparities. A number of studies have found that differences between hospitals contribute significantly to disparities in a number of outcomes (Gaskin et al., 2008; Hasnain-Wynia et al., 2010). Nursing in particular has a prominent role to play in ensuring that quality initiatives are successful in improving care and reducing disparities. Regarding readmissions, nurses provide critical in-hospital care, deliver essential patient teaching and discharge instructions, and work with families and outside institutions to ensure smooth transitions and prevent readmissions. Nurses are also in key positions in postacute care settings where they can provide and manage transitional care to prevent readmission to the acute care hospital.
Many other value-based purchasing initiatives that will be implemented as part of health reform focus not only on readmissions but on patient safety and satisfaction; measures directly influenced by nursing care (Kutney-Lee et al., 2009). To the extent that the results of quality initiatives affect hospital ratings and revenue, the role of nurses and particularly those employed in hospitals serving minority communities will be critical to understand. Nurses must continue to make the business case that the bedside care, surveillance, discharge teaching, transitional care, and multidisciplinary team services they participate in are cost-effective in light of these new initiatives (Sochalski et al., 2009). Continuing to provide up-to-date evidence regarding cost-effective organizational interventions including appropriate nurse staffing levels and work environments supportive of professional nursing practice will be important as value-based purchasing initiatives are implemented more widely (Aiken, Clarke, Sloane, Lake, & Cheney, 2008; Dall, Chen, Seifert, Maddox, & Hogan, 2009; Mark, Lindley, & Jones, 2009; Rothberg, Abraham, Lindenauer, & Rose, 2005). This may be particularly important in underresourced institutions that could be caught in the spiral of poor outcomes and limited resources to improve performance, which may ultimately lead to lower reimbursement and continued poor outcomes.
Nurse-led coordinated care management models are currently in practice across the country and hold promise for cost effectively managing patients with chronic illness. The Transitional Care Model for instance emphasizes the role of advanced practice nurses in providing critical care to patients transitioning from the hospital to the home setting (Naylor et al., 1999, 2004). Similarly, the Care Transitions intervention for patients discharged from hospitals relies on nurses (called transition coaches) who provide necessary services for patients with chronic illness (Coleman, Parry, Chalmers, & Min, 2006). These models have been associated with significant reductions in emergency department visits, lower hospital costs, and decreased readmission days in clinical studies.
Addressing current trends in readmissions cannot rest solely on nurses. Management of complex disease processes such as heart failure and acute medical illness such as AMI requires the coordinated care services of a host of health care professionals and community resources. Comprehensive care management through nurse-led transitional care interventions, home health services and patient activation programs geared to engage patients in improved symptom management offers an important tool to avert early readmissions. These types of approaches are increasingly important as the health care system moves toward more multidisciplinary and integrated models of care such as the patient-centered medical home and accountable care organizations (Fisher & Shortell, 2010; Rittenhouse & Shortell, 2009). Further research should evaluate the effect of these integrated care approaches on reducing disparities. The attention to multidisciplinary care across settings also presents a window of opportunity for research examining the specific role of nurses in collaborative teams and the linkages between acute, ambulatory, and other community agencies (e.g., Public Health Departments, Community Health Centers, and Visiting Nursing Associations).
Conclusion
Policies aimed at reducing readmissions hold promise for promoting quality, cost-effectiveness, and may offer opportunities to focus on continuity of care: an area in which nurses act as key linchpins. They may also encourage hospital staff and providers outside of the hospital to work together to properly coordinate postdischarge care. To the extent that disparities in readmissions are due to underlying inequities in social institutions versus actual differences in quality of care during hospitalization—public reporting of readmissions and pay-for-performance initiatives may unfairly cast hospitals that care largely for minority communities as poor care providers without fully accounting for these mechanisms. Penalizing these hospitals may result in a disproportionate burden for the institutions that already provide health care to much of the nation’s most vulnerable populations. Continued vigilance following the implementation of value-based purchasing policies and their effects on disparities is important to ensure that policy interventions reduce disparities.
Acknowledgments
Funding
This research was supported by the Agency for Healthcare Research and Quality (K08-HS017551, McHugh, PI), the University of Pennsylvania University Research Foundation (McHugh, PI), and the National Institute of Nursing Research (K01-NR012006, Brooks Carthon, PI). The content is solely the responsibility of the authors’ and does not necessarily represent the official views of the Agency for Healthcare Research and Quality, the University of Pennsylvania, or the National Institute of Nursing Research. The funding sources had no role in the study design, data collection, analysis, or interpretation; or writing of the report.
Biographies
Matthew D. McHugh, PhD, JD, MPH, RN, CRNP is an assistant Professor of Nursing at the University of Pennsylvania School of Nursing and faculty in the Center for Health Outcomes & Policy Research.
J. Margo Brooks Carthon, PhD, RN is an Assistant Professor at the University of Pennsylvania School of Nursing and is a faculty member in the Center for Health Outcomes and Policy Research.
Xiao L. Kang is a student researcher at the Center for Health Outcomes and Policy Research at the University of Pennsylvania School of Nursing.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T. Effects of hospital care environment on patient mortality and nurse outcomes. Journal of Nursing Administration. 2008;38:223–229. doi: 10.1097/01.NNA.0000312773.42352.d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander M, Grumbach K, Remy L, Rowell R, Massie BM. Congestive heart failure hospitalizations and survival in California: Patterns according to race/ethnicity. American Heart Journal. 1999;137:919–927. doi: 10.1016/s0002-8703(99)70417-5. [DOI] [PubMed] [Google Scholar]
- Arispe I, Holmes J, Moy E. Measurement challenges in developing the national healthcare quality report and the national healthcare disparities report. Medical Care. 2005;43(3) doi: 10.1097/00005650-200503001-00004. [DOI] [PubMed] [Google Scholar]
- Ashton CM, Del Junco DJ, Souchek J, Wray NP, Mansyur CL. The association between the quality of inpatient care and early readmission: A meta-analysis of the evidence. Medical Care. 1997;35:1044–1059. doi: 10.1097/00005650-199710000-00006. [DOI] [PubMed] [Google Scholar]
- Averill RF, McCullough EC, Hughes JS, Goldfield NI, Vertrees JC, Fuller RL. Redesigning the Medicare inpatient PPS to reduce payments to hospitals with high readmission rates. Health Care Financing Review. 2009;30(4):1–15. [PMC free article] [PubMed] [Google Scholar]
- Baker D, Stevens C, Brook R. Regular source of ambulatory care and medical care utilization by patients presenting to a public hospital emergency department. Journal of the American Medical Association. 1994;271:1909. [PubMed] [Google Scholar]
- Baker D, Stevens C, Brook R. Determinants of emergency department use: Are race and ethnicity important? Annals of Emergency Medicine. 1996;28:677–682. doi: 10.1016/s0196-0644(96)70093-8. [DOI] [PubMed] [Google Scholar]
- Balsa AI, McGuire TG. Prejudice, clinical uncertainty and stereotyping as sources of health disparities. Journal of Health Economics. 2003;22(1):89–116. doi: 10.1016/s0167-6296(02)00098-x. [DOI] [PubMed] [Google Scholar]
- Bhalla R, Kalkut G. Could Medicare readmission policy exacerbate health care system inequity? Annals of Internal Medicine. 2010;152(2):114–117. doi: 10.7326/0003-4819-152-2-201001190-00185. [DOI] [PubMed] [Google Scholar]
- Casalino LP, Elster A, Eisenberg A, Lewis E, Montgomery J, Ramos D. Will pay-for-performance and quality reporting affect health care disparities? Health Affairs. 2007;26:w405–w414. doi: 10.1377/hlthaff.26.3.w405. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. Roadmap for implementing value driven healthcare in the traditional medicare fee-for-service program. Washington, DC: Center for Medicare & Medicaid Services; 2008. [Google Scholar]
- Chien AT, Chin MH, Davis AM, Casalino LP. Pay for performance, public reporting, and racial disparities in health care: How are programs being designed? Medical Care Research and Review. 2007;64(Suppl 5):283S–304S. doi: 10.1177/1077558707305426. [DOI] [PubMed] [Google Scholar]
- Coleman EA, Parry C, Chalmers S, Min S. The care transitions intervention: Results of a randomized controlled trial. Archives of Internal Medicine. 2006;166:1822. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- Curtis LH, Greiner MA, Hammill BG, Kramer JM, Whellan DJ, Schulman KA, Hernandez AF. Early and long-term outcomes of heart failure in elderly persons, 2001–2005. Archives of Internal Medicine. 2008;168:2481–2488. doi: 10.1001/archinte.168.22.2481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dall TM, Chen YJ, Seifert RF, Maddox PJ, Hogan PF. The economic value of professional nursing. Medical Care. 2009;47(1):97–104. doi: 10.1097/MLR.0b013e3181844da8. [DOI] [PubMed] [Google Scholar]
- Deswal A, Petersen NJ, Souchek J, Ashton CM, Wray NP. Impact of race on health care utilization and outcomes in veterans with congestive heart failure. Journal of the American College of Cardiology. 2004;43:778–784. doi: 10.1016/j.jacc.2003.10.033. [DOI] [PubMed] [Google Scholar]
- Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- Fisher E, Shortell S. Accountable care organizations: Accountable for what, to whom, and how. Journal of the American Medical Association. 2010;304:1715. doi: 10.1001/jama.2010.1513. [DOI] [PubMed] [Google Scholar]
- Friedberg M, Safran D, Coltin K, Dresser M, Schneider E. Paying for performance in primary care: Potential impact on practices and disparities. Health Affairs. 2010;29:926. doi: 10.1377/hlthaff.2009.0985. [DOI] [PubMed] [Google Scholar]
- Friedman B, Basu J. The rate and cost of hospital readmissions for preventable conditions. Medical Care Research and Review. 2004;61:225–240. doi: 10.1177/1077558704263799. [DOI] [PubMed] [Google Scholar]
- Fuda K, Immekus R. Frequent users of Massachusetts emergency departments: A statewide analysis. Annals of Emergency Medicine. 2006;48(1):16. doi: 10.1016/j.annemergmed.2006.03.001. [DOI] [PubMed] [Google Scholar]
- Gaskin DJ, Arbelaez JJ, Brown JR, Petras H, Wagner FA, Cooper LA. Examining racial and ethnic disparities in site of usual source of care. Journal of the National Medical Association. 2007;99(1):22–30. [PMC free article] [PubMed] [Google Scholar]
- Gaskin DJ, Spencer CS, Richard P, Anderson GF, Powe NR, Laveist TA. Do hospitals provide lower-quality care to minorities than to whites? Health Affairs. 2008;27:518–527. doi: 10.1377/hlthaff.27.2.518. [DOI] [PubMed] [Google Scholar]
- Hargraves JL, Hadley J. The contribution of insurance coverage and community resources to reducing racial/ethnic disparities in access to care. Health Services Research. 2003;38:809–829. doi: 10.1111/1475-6773.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasnain-Wynia R, Baker DW, Nerenz D, Feinglass J, Beal AC, Landrum MB, Weissman JS. Disparities in health care are driven by where minority patients seek care: Examination of the hospital quality alliance measures. Archives of Internal Medicine. 2007;167:1233–1239. doi: 10.1001/archinte.167.12.1233. [DOI] [PubMed] [Google Scholar]
- Hasnain-Wynia R, Jean-Jacques M. Filling the gaps between performance incentive programs and health care quality improvement. Health Services Research. 2009;44:777–783. doi: 10.1111/j.1475-6773.2009.00972.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasnain-Wynia R, Kang R, Landrum MB, Vogeli C, Baker DW, Weissman JS. Racial and ethnic disparities within and between hospitals for inpatient quality of care: An examination of patient-level hospital quality alliance measures. Journal of Health Care for the Poor and Underserved. 2010;21:629–648. doi: 10.1353/hpu.0.0281. [DOI] [PubMed] [Google Scholar]
- Ho K, Moy E, Clancy C. Can incentives to improve quality reduce disparities? Health Services Research. 2010;45(1):1–5. doi: 10.1111/j.1475-6773.2009.01076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood RG. Pay-for-performance–financial health disparities and the impact on healthcare disparities. Journal of the National Medical Association. 2007;99:953–958. [PMC free article] [PubMed] [Google Scholar]
- The Hospital Quality Alliance. The hospital quality alliance: About us. 2010 Retrieved from http://www.hospitalqualityalliance.org/hospitalqualityalliance/aboutus/aboutus.html.
- Institute of Medicine. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2002. [PubMed] [Google Scholar]
- Institute of Medicine. Rewarding provider performance: Aligning incentives in Medicare. Washington, DC: National Academy Press; 2006. [Google Scholar]
- Jha AK, Orav EJ, Epstein AM. The characteristics and performance of hospitals that care for elderly Hispanic Americans. Health Affairs. 2008;27:528–537. doi: 10.1377/hlthaff.27.2.528. [DOI] [PubMed] [Google Scholar]
- Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Archives of Internal Medicine. 2007;167:1177–1182. doi: 10.1001/archinte.167.11.1177. [DOI] [PubMed] [Google Scholar]
- Jiang HJ, Andrews R, Stryer D, Friedman B. Racial/ethnic disparities in potentially preventable readmissions: The case of diabetes. American Journal of Public Health. 2005;95:1561–1567. doi: 10.2105/AJPH.2004.044222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan JB, Bennett T. Use of race and ethnicity in biomedical publication. Journal of the American Medical Association. 2003;289:2709–2716. doi: 10.1001/jama.289.20.2709. [DOI] [PubMed] [Google Scholar]
- Kutney-Lee A, McHugh MD, Sloane DM, Cimiotti JP, Flynn L, Neff DF, Aiken LH. Nursing: A key to patient satisfaction. Health Affairs. 2009;28:w669–w677. doi: 10.1377/hlthaff.28.4.w669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaCalle E, Rabin E. Frequent users of emergency departments: The myths, the data, and the policy implications. Annals of Emergency Medicine. 2010;56(1):42–48. doi: 10.1016/j.annemergmed.2010.01.032. [DOI] [PubMed] [Google Scholar]
- LaVeist TA. Beyond dummy variables and sample selection: What health services researchers ought to know about race as a variable. Health Services Research. 1994;29(1):1–16. [PMC free article] [PubMed] [Google Scholar]
- Mark BA, Lindley L, Jones CB. Nurse working conditions and nursing unit costs. Policy, Politics, and Nursing Practice. 2009;10(2):120–128. doi: 10.1177/1527154409336200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayberry R, Mili F, Ofili E. Racial and ethnic differences in access to medical care. Medical Care Research and Review. 2000;57(Suppl 4):108. doi: 10.1177/1077558700057001S06. [DOI] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission. Report to the Congress: Promoting greater efficiency in Medicare. Washington, DC: Author; 2007. Payment policy for inpatient readmissions; pp. 103–120. [Google Scholar]
- Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, Schwartz JS. Comprehensive discharge planning and home follow-up of hospitalized elders: A randomized clinical trial. Journal of the American Medical Association. 1999;281:613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- Naylor MD, Brooten DA, Campbell RA, Maislin G, McCauley KM, Schwartz JS. Transistional care of older adults hospitalized with heart failure: A randomized, controlled trial. Journal of American Geratrics Society. 2004;5:675–684. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- Philbin EF, DiSalvo TG. Influence of race and gender on care process, resource use, and hospital-based outcomes in congestive heart failure. American Journal of Cardiology. 1998;82(1):76–81. doi: 10.1016/s0002-9149(98)00233-1. [DOI] [PubMed] [Google Scholar]
- QualityNet. QualityNet—Readmission measures: Methodologies. 2010 Retrieved from http://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic/Page/QnetTier3&cid=1219069855841.
- Rathore SS, Foody JAM, Wang Y, Smith GL, Herrin J, Masoudi FA, Krumholz HM. Race, quality of care, and outcomes of elderly patients hospitalized with heart failure. Journal of the American Medical Association. 2003;289:2517. doi: 10.1001/jama.289.19.2517. [DOI] [PubMed] [Google Scholar]
- Reschovsky J, O’Malley A. Do primary care physicians treating minority patients report problems delivering high-quality care? Health Affairs. 2008;27:w222–w231. doi: 10.1377/hlthaff.27.3.w222. [DOI] [PubMed] [Google Scholar]
- Rittenhouse D, Shortell S. The patient-centered medical home: Will it stand the test of health reform? Journal of the American Medical Association. 2009;301:2038. doi: 10.1001/jama.2009.691. [DOI] [PubMed] [Google Scholar]
- Rosenthal MB, Fernandopulle R, Song HR, Landon B. Paying for quality: Providers’ incentives for quality improvement. Health Affairs. 2004;23(2):127–141. doi: 10.1377/hlthaff.23.2.127. [DOI] [PubMed] [Google Scholar]
- Rothberg MB, Abraham I, Lindenauer PK, Rose DN. Improving nurse-to-patient staffing ratios as a cost-effective safety intervention. Medical Care. 2005;43:785. doi: 10.1097/01.mlr.0000170408.35854.fa. [DOI] [PubMed] [Google Scholar]
- Ryan A. Has pay-for-performance decreased access for minority patients? Health Services Research. 2009;45(1):6–23. doi: 10.1111/j.1475-6773.2009.01050.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS (Version 9.2) SAS Institute Inc; 2008. [Google Scholar]
- Schulman KA, Berlin JA, Harless W, Kerner JF, Sistrunk S, Gersh BJ, Ayers W. The effect of race and sex on physicians’ recommendations for cardiac catheterization. New England Journal of Medicine. 1999;340:618. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- Sochalski J, Jaarsma T, Krumholz HM, Laramee A, McMurray JJ, Naylor MD, Stewart S. What works in chronic care management: The case of heart failure. Health Affairs. 2009;28:179–189. doi: 10.1377/hlthaff.28.1.179. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Report to Congress: Plan to Implement a Medicare Hospital Value-Based Purchasing Program. Washington, DC: U.S. Department of Health and Human Services; 2007. [Google Scholar]
- van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Social Science & Medicine. 2000;50:813–828. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- Werner RM, Asch DA. The unintended consequences of publicly reporting quality information. Journal of the American Medical Association. 2005;293:1239–1244. doi: 10.1001/jama.293.10.1239. [DOI] [PubMed] [Google Scholar]
- Werner RM, Goldman LE, Dudley RA. Comparison of change in quality of care between safety-net and non-safety-net hospitals. Journal of the American Medical Association. 2008;299:2180. doi: 10.1001/jama.299.18.2180. [DOI] [PubMed] [Google Scholar]
- Werner RM, Konetzka R, Stuart E, Norton E, Polsky D, Park J. Impact of public reporting on quality of postacute care. Health Services Research. 2009;44:1169–1187. doi: 10.1111/j.1475-6773.2009.00967.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D, Rucker T. Understanding and addressing racial disparities in health care. Health Care Financing Review. 2000;21(4):75–90. [PMC free article] [PubMed] [Google Scholar]
- Yancy CW, Abraham WT, Albert NM, Clare R, Stough WG, Gheorghiade M, Fonarow GC. Quality of care of and outcomes for African Americans hospitalized with heart failure: Findings from the OPTIMIZE-HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure) registry. Journal of the American College of Cardiology. 2008;51:1675–1684. doi: 10.1016/j.jacc.2008.01.028. [DOI] [PubMed] [Google Scholar]
- Zeger SL, Liang KY, Albert PS. Models for longitudinal data: A generalized estimating equation approach. Biometrics. 1988;44:1049–1060. [PubMed] [Google Scholar]