Abstract
Regular participation in organized youth sports does not ensure adequate exposure to skill- and health-related fitness activities; and sport training without preparatory conditioning does not appear to reduce risk of injury in young athletes. Recent trends indicate that widespread participation in organized youth sports is occurring at a younger age, especially in girls. Current public health recommendations developed to promote muscle strengthening and bone building activities for youth aged 6 and older, along with increased involvement in competitive sport activities at younger ages, has increased interest and concern from parents, clinicians, coaches and teachers regarding the optimal age to encourage and integrate more specialized physical training into youth development programs. This review synthesizes the latest literature and expert opinion regarding when to initiate neuromuscular conditioning in youth and presents a how to integrative training conceptual model that could maximize the potential health-related benefits for children by reducing sports-related injury risk and encouraging lifelong regular physical activity.
INTRODUCTION
Over the past decade, the total number of participants in organized youth sports has increased; although the relative number of boys and girls involved in these programs has shown little change at 66% boys and 34% girls. (1) Compared to inactive youth, children and adolescents who regularly engage in physical activity have higher levels of musculoskeletal strength, enhanced cardiorespiratory function, and reduced risk of sports- and other physical activity-related injuries.(98, 104) Moreover, sustained enjoyment and participation in activities designed to improve physical fitness and health during childhood and adolescence may be effective in prompting regular physical activity as an ongoing lifestyle choice into adulthood (91, 93) In an effort to more comprehensively and effectively address health and fitness promotion for children and adolescents, current public health objectives now aim to increase the number of youth aged 6 and older who regularly participate in “muscle strengthening” and “bone strengthening” activities (104).
Recent trends indicate that widespread participation in organized youth sports is occurring at a younger age.(1) The combination of recent recommendations targeted to promote youth involvement in strength and conditioning activities along with earlier involvement in competitive sport activities has raised interest and concern from parents, clinicians, coaches and teachers regarding the optimal age to encourage and integrate more specialized physical training into youth development programs.(5, 27, 78, 79) Many parents ask if it is safe for their child to “lift weights” or want to know the “best age” for their child to start regular participation in structured conditioning activities. This underscores a long-standing concern regarding the appropriate starting age for specialized physical training (i.e., strength and conditioning, performance enhancement or injury prevention training).
This issue is particularly important for aspiring young athletes who may be ill-prepared for the physical demands of sports practice and competition. While many factors can contribute to sports-related injuries in youth (e.g., previous injury, muscle imbalances, nutritional deficiencies, improper footwear), poor conditioning seems to play a primary role. Insufficient readiness for sports practice and competition may be a consequence of the contemporary decline in unstructured physical activity among children and adolescents in the United States. (78, 79). Based on accelerometer-determined steps per day, almost 42% of US boys and 21% of US girls are sedentary; and the decline in physical activity appears to progress steadily after age 6 for both sexes.(103) Basterfield and colleagues reported low levels of habitual physical activity and high levels of sedentary behavior in an initial group of 405 seven-year-old boys and girls. At two years follow-up, the then 9-year-olds demonstrated even more relative sedentary time with measurably lower physical activity levels.(4) This troubling trend underscores the importance of initiating efforts to avert this decline during this developmental period and encourage regular participation in age-appropriate moderate-to-vigorous-physical activity beginning in childhood.(4)
Many experts agree that one's level of physical activity is influenced by extrinsic factors (e.g., environment, family, peers, socioeconomic status, culture, and self-efficacy) that can affect a child's desire and ability to be physically active. However, adequate development of fundamental motor skills and enhanced confidence and competence to perform these activities is cited as a primary underlying determinant for increased physical activity among youth.(97) Therefore, as more children and adolescents participate in sports and conditioning activities in schools, fitness centers and private clubs, it is important to establish age-appropriate guidelines for the initiation of integrative training activities that are purposely designed to enhance neuromuscular function, muscular strength and capacity specific to sport-like activities. This review synthesizes the latest literature and expert opinion regarding when to initiate neuromuscular conditioning in youth to maximize the health-related benefits through reduced sports-related injury risk and encouraging lifelong participation in a variety of physical activities.
OPERATIONAL DEFINITIONS
For simplicity, the term “youth” refers to children (Tanner stages 1 and 2 of sexual maturation; approximately up to age 11 years in girls and 13 years in boys) and adolescents (Tanner stages 3 and 4 of sexual maturation; approximately ages 12 to 18 years in girls and 14 to 18 years in boys). The term pre-adolescent refers to boys and girls who have not yet developed secondary sex characteristics. Although the terms “resistance training” and “weightlifting” are sometimes used synonymously, the term resistance training refers to a specialized type of conditioning that involves the progressive use of a wide range of resistive loads and a variety of training modalities; whereas the term weightlifting refers to a sport which involves lifting maximal amounts of weight in competition. Integrative neuromuscular training is a conceptual training model that is operationally defined herein as a supplemental training program that incorporates general (e.g., fundamental movements) and specific (e.g., exercises targeted to motor control deficits) strength and conditioning activities, such as resistance, dynamic stability, core focused strength, plyometric and agility, that are designed to enhance health and skill-related components of physical fitness. The cornerstone of integrative neuromuscular training is age-appropriate education and instruction by qualified professionals who understand the fundamental principles of pediatric exercise science and genuinely appreciate the physical and psychosocial uniqueness of children and adolescents. Integrative training is designed to help youth to master fundamentals, improve movement mechanics, and gain confidence in their physical abilities, while participating in a program that includes variety, progression and proper recovery intervals.(27, 69)
IS MOTOR COMPETENCE MODIFIABLE DURING YOUTH?
While there is no single gene that codes for motor performance in children, there are nervous system limits that differentiate between each child's opportunity to exploit critical maturational thresholds for the development of dynamic interceptive actions (i.e., physical acts for which the body or an implement must be moved into the right place at the right time in order to accomplish a task).(18, 90) Shenk articulately described the intricate interaction of genetics and environment in his commentary which states “Contrary to what we have been taught, genes do not determine physical and character traits on their own. Rather, they interact with the environment in a dynamic, ongoing process that continually refines an individual.”(96) Skill-related fitness may not be an innate functionality hardwired at conception or gestation. Rather it is more likely to be an accumulation of developed skills driven by the interaction between genes and the environment. Tryon's artificial selection experiment on maze-running ability in rats supports the theory that environment can indeed influence motor performance. After raising several generations by breeding the best and worst maze-running rats, generations of rats were produced that provided two distinct lines of maze-running ability.(101, 102) The offspring of each of these lines consistently performed as did their parents with good performance from the “bright” offspring and poor or reduced performance in the “dull” line of rats, even though the offspring were raised in identical environments. Notably, this distinct difference in performance ability between breeding lines, which was demonstrated for multiple generations, disappeared in one generation when the rats were raised in enriched (i.e., more activity-based and social interaction) environments.
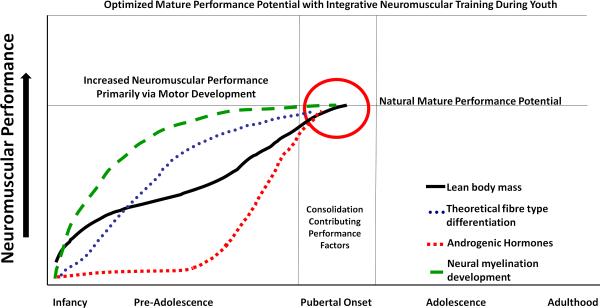
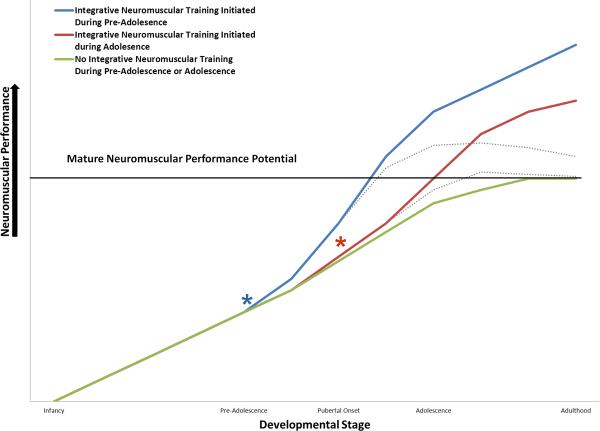
Genetic epidemiologists frequently observe that certain diseases such as obesity cluster in families; but individual family members sometimes do not demonstrate that common phenotypic expression.(87) Likewise, children may inherit sensitivity to the effects of limited physical activity (i.e., sedentary environments) that can trigger reduced motor development during youth.(35) In adolescent youth, multidisciplinary interventions that incorporated progressive and periodized resistance training were vital to improving health in previously sedentary adolescents.(35) Multidisciplinary integrative training models provided to pre-adolescent (both non-obese and obese) youth may also enrich their motor learning environment during this period of time (Figure 1). Environments enriched with integrative neuromuscular training may not only help youth overcome genetic limitations, (17) but may also help children achieve a level of motor competence that is beyond their expected adult potential without such training(Figure 2).
Figure 1.
In youth there are several factors which contribute to motor control and strength expression. In children, motor control and strength may be less related to hypertrophy and more likely associated with neural development. It is proposed that integrative neuromuscular training focused on skill-related fitness (e.g. Agility, reaction time, coordination, power, speed and balance) can maximize neural development during pre-adolescence and optimally prepare youth to capitalize on the consolidated factors which contribute to motor performance following the onset of puberty. Figure modified from Kraemer, W. J., A. C. Fry, P. N. Frykman, B. Conroy and J. Hoffman (1989). “Resistance Training and Youth.”Pediatric Exercise Science 1: 336–350.
Figure 2.
Conceptual model which compares the effects of integrative neuromuscular training initiated at different times in youth. “*” represent the initiation of these integrative training techniques during pre-adolescence (Blue) and adolescence (Red) which will likely improve motor capacity and performance beyond natural adult potential (without such training). It is suggested that integrative neuromuscular training initiated in pre-adolescence and maintained into adolescence will maximize the potential to achieve optimal adulthood motor capacity. Broken lines indicate potential detrimental effects of overtraining youth without structured recovery periods included as an integral component of the integrative training model.
Although speculative, a child in a non-enriched environment which is deficient in opportunities to regularly engage in activities that enhance fundamental motor skills may suffer long-lasting detrimental effects on health and disease risk later in life. This view is supported by the recent work of Lopes et al. (2010) who found that 6-year-old children with low and average levels of motor coordination had lower levels of physical activity 5 years later compared with children with high motor coordination.(58) Furthermore, in a 10-year longitudinal study of 630 adolescents, the participants first became involved in organized youth sports clubs between the ages 6–10 years. (52) Interestingly, those who reported becoming members of a sports team at an even earlier age were more physically active as adults than adolescents who initiated sports involvement at older ages.(52) It has been proposed that the high degree of plasticity in neuromuscular development during pre-adolescence combined with appropriately timed implementation and progression of integrative neuromuscular training may allow for strengthened physical, mental, and social development that contributes favorably to their athleticism during adolescence. It is also possible that the improved motor competence developed through adolescence facilitates the establishment of desired behaviors and habits that may carry over into adulthood (Figures 1 and 2).(52) On the basis of motor skill learning, pre-adolescence may provide an “optimal” window to train and develop long-lasting fundamental movement skills in boys and girls.(36, 59) Following maturation, young adult's cortico-motor plasticity and potential for learning dynamic interceptive actions may be strongly diminished.(38, 89, 90) Although speculative, children who do not regularly participate in this type of neuromuscular training in physical education classes, recreation programs, and youth sport centers may never reach their true genetic potential during adulthood.
WHEN IS MOTOR COMPETENCE AND SKILL-RELATED FITNESS MOST MODIFIABLE IN YOUTH?
Studies investigating the trainability of youth with resistance and integrative-type training protocols have demonstrated significant improvements in selected performance measures in children and adolescents following progressive training programs (19, 25, 29–31, 75, 81, 86, 94, 95, 105). The observable benefits of this type of training are greater than those attributable to normal growth and development alone. These gains stem largely from neuromuscular adaptations (i.e., more comprehensive and synchronous firing of muscle units) during pre-adolescence. In contrast, measurable training-induced gains prompted by increased fat-free mass are observable during adolescence, owing to testosterone and other hormonal influences on muscle hypertrophy that are operant during and after puberty (Figure 1) (53).
Pubertal female athletes (12 years old) who self-reported previous participation in resistance training demonstrated a 13.4% improved lower extremity control from the first to second year of testing, compared to an average decrease of 21.7% in the other groups of pubertal and post-pubertal (14 years) females who did not report participation in resistance training in the previous year. In addition, hamstring strength was significantly greater in both the pubertal and post-pubertal groups who participated in resistance training exercises. Ultimately, the athletes who participated in resistance training during earlier stages of development (early maturation, prior to 12 years old) demonstrated the greatest benefits from participation in resistance training as evidence by reduced lower extremity deficits. (32) Moreover, regular participation in a progressive integrative training program has been found to positively influence several other measurable indices of health and fitness.(5, 24, 72, 75) Regular participation in an integrative or multi-faceted resistance training program with qualified instruction can also provide an opportunity for children and adolescents to learn proper exercise technique, receive basic education on program design, learn about healthy lifestyle choices and gain confidence in their abilities to be physically active.
Children purportedly are born with a predetermined level of skill-related fitness capacity.(18) Without an environment enriched with opportunities and encouragement to participate in integrative training during this developmental period, children and adolescents will be less likely to reach their true skill-related fitness potential (Figure 2).(18) Kraemer and colleagues suggested that a consolidation of performance factors (e.g., increased neural myelination and androgenic hormonal influence) create an optimal opportunity to expose youth to an enriched environment of integrative training before the onset of pubertal maturation (Figure 1).(53) Integrative neuromuscular training is vitally important for youth whose cognitive and motor capabilities are highly “plastic” and amenable to age-appropriate interventions, and may be even more beneficial to youth with a decreased genetic potential for motor development and competence.(38, 83) Considering the potential for motor skill learning, along with the need to capitalize on the consolidation of factors which contribute to enhanced motor skill performance during preadolescence (Figure 1) (53), regular participation in integrative neuromuscular training as part of physical education, recreational fitness training, or preparatory sports conditioning should begin during middle childhood (about age 7–10 years depending on maturity) and continue through adolescence (Figure 2). On this basis, integrative neuromuscular training that is designed to enhance development of fundamental movement skills during this optimum period may provide the most lasting benefits during adolescence and possibly adulthood.(36, 59)
DOES MATURITY (SOMATIC OR PSYCHOSOCIAL) AFFECT WHEN TO INITIATE INTEGRATIVE NEUROMUSCULAR TRAINING?
While chronological age may historically be used for initial participation and grouping of sports teams, it is clear that maturity-related differences in body size exist around 6–7 years of age.(62) Somatic maturational assessments are traditionally the best way to identify rapid adolescent growth.(61) Individually determined percentage of adult height may also be used as a relatively quick and non-invasive indicator of maturity status.(62)The Khamis-Roche method of estimated adult stature was developed from the Fels Longitudinal Study (51) and uses individual stature, mass, age and mid-parental stature in a regression equation for boys and girls. Peak height velocity (PHV) is the maximum growth rate during the adolescent growth spurt and occurs at approximately age 12 in girls and age 14 in boys.(92, 99) A potential window of opportunity may exist for the optimal initiation of integrative neuromuscular training based on measures of somatic maturity. Specifically, it seems most beneficial and thus desirable to initiate integrative training programs during pre-adolescence prior to the period of PHV when youth are growing the fastest. Children with earlier somatic maturation (growth) may particularly benefit from earlier participation in integrative neuromuscular training.
Although there is no minimum age for participation in integrative neuromuscular training programs, all participants must be able to follow coaching instructions and be able to handle the attention demands of a training program. In general, a child that is deemed ready for structured sports participation (about age 7 or 8 years) would typically be ready for some type of resistance and other integrative training.(5, 24) However, regardless of the starting age, all youth should receive instruction on safety concerns including sensible starting weights, repetitions, and jumping heights, for example. Proper handling of equipment and safe spotting procedures when appropriate are also important. This is particularly important in schools and recreation centers because untrained youth tend to overestimate their physical abilities and this may increase their risk of injury.(84) While somatic maturation helps define periods that are optimal to gain motor competence with integrative training, ultimately it is the child's psychosocial status (ability to follow coaching instructions, adhere to safety rules and handle the attention demands of a training program) is paramount in the decision process regarding his or her participation in a structured integrative neuromuscular training program.
DOES SEX AFFECT WHEN TO INITIATE INTEGRATIVE NEUROMUSCULAR TRAINING?
Children with low motor competence are less able and sometimes less willing to participate in many sports and recreational activities typically enjoyed by their more well-coordinated peers (add ref). For both males and females, motor competence is associated with improved fitness measures.(39) Adolescent males commonly outperform females in measures of physical performance, and these motor competence measures are related to better health outcomes in adults. Males demonstrate power, strength and coordination increases with increasing chronological age that correlate to maturational stage; while females show significantly smaller changes throughout puberty.(10, 61) For example, vertical jump height (a measure of whole-body power) increases steadily in males during puberty, but not in females.(50, 61, 85) Hewett and colleagues demonstrated that as males mature they employ a more efficient strategy for muscular dampening of forces.(45) The improved motor control likely reflects natural adaptive changes in contraction patterns of the adductors and abductors of both the hip and the knee.(57, 100) Brent and colleagues demonstrated that hip abduction strength relative to body mass in males improves with each subsequent age group (11 to 17 years). In contrast, hip abduction strength does not change in females across the same age range. These findings may indicate that integrative neuromuscular training protocols should include hip abduction strengthening exercises and should be implemented for young females prior to age 11 when the gender-specific reduction in relative hip strength diverges.(14)
Musculoskeletal growth during puberty, in the absence of sufficient corresponding neuromuscular adaptation, may facilitate the development of abnormal mechanics during certain activities.(33, 42) These intrinsic risk factors, if not addressed at the proper time, may continue through adolescence into maturity and predispose female athletes to increased risk of a variety of musculoskeletal injuries.(46, 70) In a recent longitudinal study, Ford and colleagues noted that pubertal females have an increased change in abnormal landing mechanics over time.(34) In addition, important contributing risk factors for knee injury were significantly greater across consecutive years in young post-pubertal female athletes compared to males. Integrative neuromuscular training programs have been successful at reducing these abnormal biomechanics(48, 73–75) and appear to decrease injury rates in female athletes. Integrative neuromuscular training utilized to enrich the motor learning environment in early youth may also initiate adaptation and help low motor competence children “catch-up” with their peers in these measures.(17, 38, 89, 90) Preliminary data indicate integrative neuromuscular training protocols implemented in pre-adolescent (Tanner 1) and early adolescent (Tanner 2) may artificially induce the “neuromuscular spurt” (defined as the natural adaptation of increased power, strength and coordination that occurs with increasing chronological age and maturational stage in adolescent boys), especially related to relative posterior chain strength postural control and neuromuscular power which is often reduced as young female athletes mature.(67) An induced neuromuscular spurt may decrease differences in neuromuscular control of the lower extremity between adolescent male and female athletes and has the potential to reduce the risk of sports-related injury in adolescent female athletes.(41, 43, 48, 71) These data provide further support that preadolescence may be an optimal time to institute programs aiming to reduce these deficits that accelerate during maturation and lead to increased musculoskeletal injury risk.
WHAT ARE THE RISKS ASSOCIATED WITH INTEGRATIVE NEUROMUSCULAR DURING PRE-ADOLESCENCE?
As with any exercise or sports-related activity, youth participation in integrative neuromuscular training activities involves some degree of inherent risk of musculoskeletal injury. However, when children and adolescents are appropriately supervised and the training program is consistent with individual needs and abilities, risk of injury can be much less than in other sports and recreational activities in which children and adolescents regularly participate. (28, 108) Zariczyj and colleagues evaluated the incidence of sports-related injuries (based on accident reports) in school-age youth over a one year period and found that resistance training resulted in 0.7% of 1576 injuries; whereas American football resulted in 19% of all injuries or a nearly 30 times greater relative incidence. (108) Many of the sustained forces and impulse loads that youth are exposed to in sports and recreational activities are greater in duration and magnitude than properly prescribed and performed resistance and plyometric exercises. For example, during certain dynamic sports activities characteristic of recreational or competitive play, athletes can expose their lower extremity to ground reaction forces reaching five to seven times their own body mass.(20, 47, 64) Impulse ground reaction loads can be tremendously magnified and compounded during running and other single-limb stance plyometric activities inherent in some sports. Thus, appropriate integrative neuromuscular training protocols pose less of a risk to children and adolescents than traditional recreational and competitive sport activities.(28, 69)
Integrative skill-related movements may be required to positively influence motor adaptations in youth that can prepare them to meet the demands of recreational and sport activities. Regular participation in integrative neuromuscular training programs that include weightlifting exercises (e.g., modified cleans, pulls and presses) and plyometric exercises (single and double-leg hops and jumps) with qualified instruction and sensible progression have been found to enhance functional biomechanics and abilities and reduce the number of sport-related injuries in young athletes.(43, 63, 75) Although some organizations and observers do not support participation in weightlifting or maximal load lifting until physical or skeletal maturity (2, 66, 107), others suggest that childhood may be the ideal time to develop the coordination and skill technique to perform these lifts correctly. (5, 23, 53, 82) However, unsupervised and poorly performed resistance and plyometric exercise should not be performed under any circumstances, because of the potential for accidental and musculoskeletal overload injury (11, 76, 88) In pre-adolescent populations (aged 8–13), two-thirds of all reported injuries during resistive and integrative training are to the hand and foot and are related to “dropping” and “pinching”.(77) The authors concluded that the majority of youth resistance training injuries are the result of accidents that are potentially preventable with increased supervision and stricter enforced safety guidelines.(77)
If appropriately supervised and sensibly progressed, integrative neuromuscular training programs can be safe, effective and enjoyable for children and adolescents.(5, 6, 19, 24, 60) However, because unsupervised and poorly designed training programs can be injurious, qualified professionals should design individualized exercise programs that are consistent with the needs, interests and abilities of each participant and closely supervise all training sessions For example, without quality supervision and instruction, youth are more likely to attempt to lift weights that exceed their capabilities or engage in other risky behavior in the training center.(28, 49, 77) Adults who teach and coach youth should have practical experience working with children and adolescents and a philosophy about training youth that is consistent with the needs, interests and goals of younger populations.
INTEGRATIVE NEUROMUSCULAR TRAINING DURING PRE-ADOLESENCE TO REDUCE RISK OF SPORTS-RELATED INJURIES IN YOUTH – IS IT EFFECTIVE?
While the total elimination of sports-related injuries in youth is an unrealistic goal, appropriately designed and sensibly progressed integrative neuromuscular training programs may help to reduce the likelihood of sports-related injuries in young athletes. (28, 40, 43) By addressing the risk factors associated with certain youth sport injuries (e.g., low fitness level, muscle imbalances and errors in training), acute and overuse injuries could be reduced by 15 to 50% (65). Lehnhard and colleagues significantly reduced injury rates with the addition of a strength training regimen in male soccer players. (56) Cahill and Griffith incorporated resistance training into preseason conditioning for adolescent football teams and, over four competitive seasons, reported a reduction in overall knee injuries including the incidence of knee injuries that required surgery. (16)Likewise, Emery and Meeuwisse found that integrated neuromuscular training was protective of all injuries including acute onset injury in young soccer players.(21) Notably, protocols that incorporate resistance training into pre-season and in-season conditioning programs reduce anterior cruciate ligament (ACL) injury risk factors and ACL injuries incidence in female athletes.(40, 43). Although only a small minority of young athletes participate in integrative neuromuscular conditioning programs prior to sports participation, (15) these data indicate that such multi-faceted conditioning programs may indeed reduce sports-related injuries in adolescents and that similar results would be observed in pre-adolescent populations if such programs were applied.(19, 37, 41)
HOW TO INITIATE INTEGRATIVE NEUROMUSCULAR TRAINING DURING PRE-ADOLESENCE
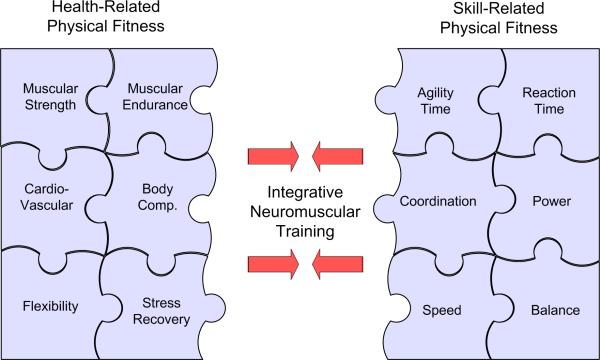
Rather than prolonged periods of aerobic exercise which may be less appealing for children, recent findings indicate that integrative neuromuscular training which incorporates intermittent-type activities into a well-designed plan may offer more effective health and fitness value to aspiring young athletes (Figure 3).(43, 44, 59, 68, 69, 72, 74, 75) Integrative neuromuscular training is characterized by short bursts of physical activity interspersed with periodic brief rest periods. The intermittent rather than continuous nature of integrative neuromuscular training is more consistent with how youth move and play.(3) It also includes a variety of training modalities which are sensibly prescribed and progressed over time.
Figure 3.
Integrative training model indicating a focus on the development of fundamental motor skills through activities which consolidate skill- and health-related fitness, may maximize efficacy of neuromuscular conditioning during pre-adolescence.
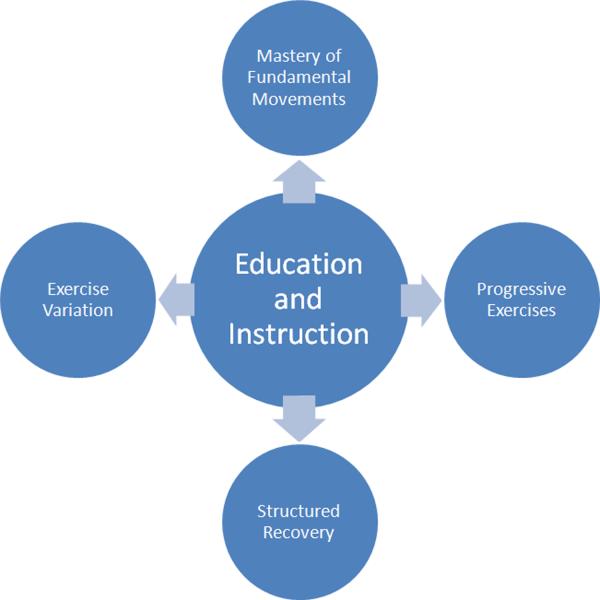
Adding integrative neuromuscular training to the total exercise dose of young athletes (i.e., sports practice, sports competition, and free play) should be carefully considered, as this could contribute to the chronic repetitive stress placed on developing musculoskeletal systems. The risk of overload or overuse injury unduly increases if the intensity, volume or frequency of training or competition greatly exceeds the ability of the participants to tolerate the load, perform technically sound movements, or to sufficiently recover from prior activity bouts.(8, 9, 12) An effective approach could be to integrate resistance, power and speed training into a progressive conditioning program in which the volume and intensity of training periodically change throughout the year (i.e., periodization). The systematic structuring of program variables, along with sufficient individual effort, qualified instruction and adequate recovery are key interrelated determinants of effective progressive integrative neuromuscular training (Figure 4). Adequate recovery between challenging training and competition sessions is often overlooked in youth conditioning programs that seem to be primarily focused on overload and progression. Safe and effective training of athletes at any age involves balancing the demands of training with the need for recovery to minimize injury risk and achieve training adaptation goals. This is particularly important for young athletes who represent different sports teams or participate in extracurricular sport activities at private training centers and in the community.
Figure 4.
Education and Instruction are the key components for effective implementation of integrative neuromuscular training. (Reprinted from Myer, GD, Faigenbaum AD, Chu DA, Falkel J, Ford KR, Best TM and Hewett TE (2011). Integrative Training for Children and Adolescents: Techniques and Practices for Reducing Sports-related Injuries and Enhancing Athletic Performance. Physician and Sports Medicine In Press. Copyright© 2011 JTE Multimedia. Used with permission.)
Children and adolescents should engage in 60 minutes or more of physical activity daily.(104). However, high-intensity training should only be performed two to three times per week on nonconsecutive days, to allow time for sufficient recovery between training sessions. (24) When young athletes participate in strength and conditioning activities more than three days per week, factors such as the overall training volume, training intensity, exercise selection, and nutritional intake should be carefully considered, as these factors directly influence the ability to recover from and appropriately adapt to the training program. As training programs and level of competition become more advanced and activity bouts are more frequent, proper exercise technique should be closely monitored by qualified professionals. Moreover, youth coaches should be cognizant of the signs and symptoms of overtraining (e.g., muscle soreness that lingers for several days, decrease in performance, increased perception of effort during exercise, frequent upper respiratory tract infections, sleep disturbances, loss of appetite, mood disturbances, shortness of temper, decreased interest in training and competition, decreased self-confidence, inability to concentrate) and should realize that some children with relatively immature musculoskeletal systems cannot safely tolerate the same amount of exercise that many of their teammates can endure.(12, 106)
The prescribed exercises, sets and repetitions for an effective integrative neuromuscular exercise program should be individualized and attainable for each athlete, and also modified as needed. Initial volume selection should be low to allow the athlete to learn how to perform each exercise with proper technique. Volume (or resistance, when applicable) should be increased after the athlete can properly perform the exercise at the prescribed volume and intensity. The professionals who supervise young athletes should be skilled in recognizing proper technique and should provide constructive feedback during the learning and development process, especially when improper technique increases injury risk. Once the young athlete becomes proficient with all exercises within a progression phase, s/he can advance to the next successive phase. Young athletes should participate periodically in less intense training (LIT) sessions to encourage and reinforce learning of specific movement patterns. (26) Accordingly, high intensity and/or high volume training sessions should be regularly balanced with LIT sessions, as well as other recovery strategies to maximize training adaptations while minimizing the risk of overtraining.(106)
While participation in organized school- and community-based youth sports programs provides an excellent medium to increase physical activity and improve health in youth, participation in organized sports activities does not ensure that youth meet the recommended requirement of at least 60 minutes of moderate to vigorous daily physical activity.(7, 55, 80) Moreover, a recent meta-analysis on youth resistance training indicates that improved muscular strength is dependent on adequate volume to provide sufficient adaptive stimulus.(6) Distefano and colleagues modified traditionally effective training programs previously used adolescents,(41, 63, 74) into a 9-week “integrated injury prevention program” for use as an additive training regimen during the warm-up period in young soccer player (10–12 years). The addition of integrative injury prevention training program into standard soccer training influenced improvements in balance ability and vertical jump height in the young soccer players.(19) Clearly, participation in physical activity should not begin with competitive sport but should evolve out of well-rounded preparatory fitness conditioning that is sensibly progressed over time. With addition of integrative neuromuscular training into existing practice activities, coaches can be better equipped to ensure that youth will see greater gains in skill-related fitness and health with likely reductions in risk of sports related injury.
While there is not one combination of exercises, sets and repetitions that has proven to optimize training adaptations, it appears that multi-faceted and integrative programs that increase muscle strength, enhance movement mechanics, and improve functional abilities appear to be the most effective strategy for reducing sports-related injuries in young athletes.(40) Integrative neuromuscular training that is initially focused on fundamental skill mastery in early childhood may improve the capacity to achieve sport-related and dynamic interceptive skills during adolescence. Likewise, fundamental movement skills competency in children and adolescents can increase physical activity, improve cardiorespiratory fitness and enhance body composition (BMI z-score).(59) Although there are many approaches to potentially reduce youth sports-related injuries (e.g., coaching education, safe equipment, proper nutrition), enhancing physical fitness as a preventative health measure is considered a cornerstone of multi-component programs for school-age youth. This is an important consideration for health care providers who often perform pre-participation physical examinations in order to assess a young athlete's readiness for sport (47). In addition to the medical examination (including a musculoskeletal assessment), health care providers should inquire about a patient's participation in physical activities over the past few months. Since training errors (e.g., “too much, too soon”) are a common theme in many sports-related injuries in youth (65), there is an on-going need to ensure that aspiring young athletes participate in integrative neuromuscular conditioning programs before the start of the sport season and continue training in a modified program throughout the competitive season. (13, 27, 28)
Proper education and instruction are paramount for safe, effective and enjoyable integrative neuromuscular training (Figure 4). However, initiation of integrative neuromuscular training in during pre-adolescence must also be challenging and enjoyable to keep the children interested and motivated in continuing participation. (22, 24) Age-appropriate education and qualified instruction are required to successfully integrate different components related to the mastery of fundamental movements, program variation, exercise progression and structured recovery. Because a growing number of school-age youth are exposed to strength and conditioning activities in physical education classes and community recreational and sports training programs,(24, 54) the importance of qualified and enthusiastic instruction that is consistent with individual needs, goals and abilities is critical. Children and adolescents who participate in integrative neuromuscular training programs should be knowledgeable of the potential risks and concerns associated with exercise equipment (e.g., treadmills, weight machines, barbells) and should be aware of the potential risk of injury if they do not follow established training guidelines and safety procedures. Ultimately, education and instruction will determine the levels of success that can be achieved within each component of an integrative neuromuscular training program (Figure 4).
SUMMARY AND CONCLUSIONS
Regular participation in organized youth sports does not ensure that youth are adequately exposed to fitness regimens and activities that sufficiently improve health and sports-specific fitness to minimize risk of injury and promote lifelong health and fitness. Accordingly, participation in physical activity should not begin with competitive sport, but should evolve out of regular participation in a well-rounded preparatory conditioning program. . Integrative neuromuscular training programs that integrate a variety of fundamental movements designed to enhance both health and skill-related fitness may be most beneficial if initiated during pre-adolescence. Moreover, integrative neuromuscular training is more likely to have long-lasting effects if qualified professionals focus on the process of developing fundamental motor skills rather than the product of enhanced sports performance. Integrative neuromuscular training maintained throughout childhood and adolescence will likely improve movement biomechanics, minimize the risk of sports-related injury, and promote positive health outcomes during adulthood. With a program based on the physical and psychosocial uniqueness of children, integrative neuromuscular training that is sensibly progressed over time and consistent with individual needs, goals and abilities can be integral to development and promotion of a health-oriented approach to lifelong physical activity.
ACKNOWLEDGEMENTS
The authors would like to acknowledge funding support from National Institutes of Health Grants R01-AR049735, R01-AR055563 and R01-AR056259.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.NCYS report on trends and participation in organized youth sports . Book NCYS report on trends and participation in organized youth sports. National Council on Youth Sports Web site; City: 2008. [Google Scholar]
- 2.American Academy of Pediatrics Strength training by children and adolescent. Pediatrics. 2008;121:835–840. doi: 10.1542/peds.2007-3790. [DOI] [PubMed] [Google Scholar]
- 3.Bailey RC, Olson J, Pepper SL, Porszasz J, Barstow TJ, Cooper DM. The level and tempo of children's physical activities: an observational study. Med. Sci. Sports Exerc. 1995;27:1033–1041. doi: 10.1249/00005768-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Basterfield L, Adamson AJ, Frary JK, Parkinson KN, Pearce MS, Reilly JJ. Longitudinal Study of Physical Activity and Sedentary Behavior in Children. Pediatrics. 2011;127:e24–e30. doi: 10.1542/peds.2010-1935. [DOI] [PubMed] [Google Scholar]
- 5.Behm DG, Faigenbaum AD, Falk B, Klentrou P. Canadian Society for Exercise Physiology position paper: resistance training in children and adolescents. Appl. Physiol. Nutr. Metab. 2008;33:547–561. doi: 10.1139/H08-020. [DOI] [PubMed] [Google Scholar]
- 6.Behringer M, Vom Heede A, Yue Z, Mester J. Effects of resistance training in children and adolescents: a meta-analysis. Pediatrics. 2010;126:e1199–1210. doi: 10.1542/peds.2010-0445. [DOI] [PubMed] [Google Scholar]
- 7.Bergeron MF. Improving health through youth sports: is participation enough? New Dir. Youth Dev. 2007;26:27–41. doi: 10.1002/yd.221. [DOI] [PubMed] [Google Scholar]
- 8.Bergeron MF. Youth sports in the heat: recovery and scheduling considerations for tournament play. Sports Med. 2009;39:513–522. doi: 10.2165/00007256-200939070-00001. [DOI] [PubMed] [Google Scholar]
- 9.Bergeron MF, Laird MD, Marinik EL, Brenner JS, Waller JL. Repeated-bout exercise in the heat in young athletes: physiological strain and perceptual responses. J. Appl. Physiol. 2009;106:476–485. doi: 10.1152/japplphysiol.00122.2008. [DOI] [PubMed] [Google Scholar]
- 10.Beunen G, Malina RM. Growth and physical performance relative to the timing of the adolescent spurt. Exerc. Sport Sci. Rev. 1988;16:503–540. [PubMed] [Google Scholar]
- 11.Brady T, Cahill B, Bodnar L. Weight training related injuries in the high school athlete. AmericanJournal of Sports Medicine. 1982;10:1–5. doi: 10.1177/036354658201000101. [DOI] [PubMed] [Google Scholar]
- 12.Brenner JS. Overuse injuries, overtraining, and burnout in child and adolescent athletes. Pediatrics. 2007;119:1242–1245. doi: 10.1542/peds.2007-0887. [DOI] [PubMed] [Google Scholar]
- 13.Brent JL, Klugman MA, Myer GD, Hewett TE. The Effects of Pre-Season and In-Season Neuromuscular Training on the Tuck Jump Assessment: a Test Used to Identify Risk of ACL Injury in Female Athletes. National Strength and Conditioning Association Annual Meeting.2010. [Google Scholar]
- 14.Brent JL, Myer GD, Ford KR, Hewett TE. A Longitudinal Examination of Hip Abduction Strength in Adolescent Males and Females. Am. J. Sports Med. 2011 Under Review. [Google Scholar]
- 15.Brooks MA, Schiff MA, Koepsell TD, Rivara FP. Prevalence of preseason conditioning among high school athletes in two spring sports. Med. Sci. Sports Exerc. 2007;39:241–247. doi: 10.1249/01.mss.0000246997.02095.5b. [DOI] [PubMed] [Google Scholar]
- 16.Cahill B, Griffith E. Effect of preseason conditioning on the incidence and severity of high school football knee injuries. American Journal of Sports Medicine. 1978;6:180–184. doi: 10.1177/036354657800600406. [DOI] [PubMed] [Google Scholar]
- 17.Cooper RM, Zubek JP. Effects of enriched and restricted early environments on the learning ability of bright and dull rats. Can J Psychol. 1958;12:159–164. doi: 10.1037/h0083747. [DOI] [PubMed] [Google Scholar]
- 18.Davids K, Baker J. Genes, environment and sport performance: why the nature-nurture dualism is no longer relevant. Sports Med. 2007;37:961–980. doi: 10.2165/00007256-200737110-00004. [DOI] [PubMed] [Google Scholar]
- 19.DiStefano LJ, Padua DA, Blackburn JT, Garrett WE, Guskiewicz KM, Marshall SW. Integrated injury prevention program improves balance and vertical jump height in children. J Strength Cond Res. 2010;24:332–342. doi: 10.1519/JSC.0b013e3181cc2225. [DOI] [PubMed] [Google Scholar]
- 20.Dufek JS, Bates BT. The evaluation and prediction of impact forces during landings. Med Sci Sports Exerc. 1990;22:370–377. [PubMed] [Google Scholar]
- 21.Emery CA, Meeuwisse WH. The effectiveness of a neuromuscular prevention strategy to reduce injuries in youth soccer: a cluster-randomised controlled trial. Br. J. Sports Med. 2010;44:555–562. doi: 10.1136/bjsm.2010.074377. [DOI] [PubMed] [Google Scholar]
- 22.Faigenbaum A, Farrell A, Radler T, Zbojovsky D, Chu D, Ratamess N, Kang J, Hoffman J. Plyo Play: A novel program of short bouts of moderate and high intensity exercise improves physical fitness in elementary school children. The Physical Educator. 2009;69:37–44. [Google Scholar]
- 23.Faigenbaum A, Kraemer W, Blimkie C, Jeffreys I, Micheli L, Nitka M, Rowland T. Youth resistance training: Updated position statement paper from the National Strength and Conditioning Association. Journal of Strength and Conditioning Research. 2009;23:S60–S79. doi: 10.1519/JSC.0b013e31819df407. [DOI] [PubMed] [Google Scholar]
- 24.Faigenbaum AD, Kraemer WJ, Blimkie CJ, Jeffreys I, Micheli LJ, Nitka M, Rowland TW. Youth resistance training: updated position statement paper from the national strength and conditioning association. J Strength Cond Res. 2009;23:S60–79. doi: 10.1519/JSC.0b013e31819df407. [DOI] [PubMed] [Google Scholar]
- 25.Faigenbaum AD, Loud RL, O'Connell J, Glover S, Westcott WL. Effects of different resistance training protocols on upper-body strength and endurance development in children. J Strength Cond Res. 2001;15:459–465. [PubMed] [Google Scholar]
- 26.Faigenbaum AD, Mcfarland J. Make Time for Less Intense Training. Strength and Conditioning Journal. 2006;28:77–79. [Google Scholar]
- 27.Faigenbaum AD, Myer GD. Pediatric resistance training: benefits, concerns, and program design considerations. Curr. Sports Med. Rep. 2010;9:161–168. doi: 10.1249/JSR.0b013e3181de1214. [DOI] [PubMed] [Google Scholar]
- 28.Faigenbaum AD, Myer GD. Resistance training among young athletes: safety, efficacy and injury prevention effects. Br. J. Sports Med. 2010;44:56–63. doi: 10.1136/bjsm.2009.068098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Faigenbaum AD, Westcott WL, Micheli LJ, Outerbridge AR, Long CJ, LaRosa-Loud R, Zaichkowsky LD. The Effects of Strength Training and Detraining on Children. J Strength Cond Res. 1996;10:109–114. [Google Scholar]
- 30.Faigenbaum AD, Zaichkowsky LD, Westcott WL, Micheli LJ, Fehlandt AF. The Effects of a Twice-a-Week Strength Training Program on Children. Pediatric Exercise Science. 1993;5:339–345. [Google Scholar]
- 31.Falk B, Mor G. The Effects of Resistance and Martial Arts Training in 6 to 8 Year Old Boys. Pediatric Exercise Science. 1996;8:48–56. [Google Scholar]
- 32.Ford KR, Myer GD, Hewett TE. Longitudinally decreased knee abduction and increased hamstrings strength in females withthat self-reported resistance training. Accepted to American College of Sports Medicine Annual Meeting; Denver, Colorado. 2011. [Google Scholar]
- 33.Ford KR, Shapiro R, Myer GD, VDB AJ, Hewett TE. Longitudinal Sex Differences during Landing in Knee Abduction in Young Athletes. Med Sci Sports Exerc. 2010;42:1923–1931. doi: 10.1249/MSS.0b013e3181dc99b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ford KR, Shapiro R, Myer GD, van den Bogert AJ, Hewett TE. Longitudinal Sex Differences during Landing in Knee Abduction in Young Athletes. Med. Sci. Sports Exerc. 2010 doi: 10.1249/MSS.0b013e3181dc99b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Foschini D, Araujo RC, Bacurau RF, De Piano A, De Almeida SS, Carnier J, Rosa TD, De Mello MT, Tufik S, Damaso AR. Treatment of obese adolescents: the influence of periodization models and ACE genotype. Obesity (Silver Spring) 2010;18:766–772. doi: 10.1038/oby.2009.247. [DOI] [PubMed] [Google Scholar]
- 36.Gallahue DL, Ozmun JC. Understanding motor development: infants, children, adolescents, adults. McGraw Hill; Boston: 2006. [Google Scholar]
- 37.Gilchrist J, Mandelbaum BR, Melancon H, Ryan GW, Silvers HJ, Griffin LY, Watanabe DS, Dick RW, Dvorak J. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am. J. Sports Med. 2008;36:1476–1483. doi: 10.1177/0363546508318188. [DOI] [PubMed] [Google Scholar]
- 38.Hands B. Changes in motor skill and fitness measures among children with high and low motor competence: a five-year longitudinal study. J Sci Med Sport. 2008;11:155–162. doi: 10.1016/j.jsams.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 39.Hands B, Larkin D, Parker H, Straker L, Perry M. The relationship among physical activity, motor competence and health-related fitness in 14-year-old adolescents. Scand J Med Sci Sports. 2009;19:655–663. doi: 10.1111/j.1600-0838.2008.00847.x. [DOI] [PubMed] [Google Scholar]
- 40.Hewett TE, Ford KR, Myer GD. Anterior Cruciate Ligament Injuries in Female Athletes: Part 2, A Meta-analysis of Neuromuscular Interventions Aimed at Injury Prevention. Am. J. Sports Med. 2006;34:490–498. doi: 10.1177/0363546505282619. [DOI] [PubMed] [Google Scholar]
- 41.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am. J. Sports Med. 1999;27:699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 42.Hewett TE, Myer GD, Ford KR. Decrease in neuromuscular control about the knee with maturation in female athletes. J. Bone Joint Surg. Am. 2004;86-A:1601–1608. doi: 10.2106/00004623-200408000-00001. [DOI] [PubMed] [Google Scholar]
- 43.Hewett TE, Myer GD, Ford KR. Reducing knee and anterior cruciate ligament injuries among female athletes: a systematic review of neuromuscular training interventions. J. Knee Surg. 2005;18:82–88. doi: 10.1055/s-0030-1248163. [DOI] [PubMed] [Google Scholar]
- 44.Hewett TE, Myer GD, Ford KR. Anterior Cruciate Ligament Injuries in Female Athletes: Part 1, Mechanisms and Risk Factors. Am. J. Sports Med. 2006;34:299–311. doi: 10.1177/0363546505284183. [DOI] [PubMed] [Google Scholar]
- 45.Hewett TE, Myer GD, Ford KR. Book Longitudinal increases in knee abduction moments during maturation. City: 2010. Longitudinal increases in knee abduction moments during maturation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hewett TE, Myer GD, Ford KR, Heidt RS, Jr., Colosimo AJ, McLean SG, van den Bogert AJ, Paterno MV, Succop P. Biomechanical Measures of Neuromuscular Control and Valgus Loading of the Knee Predict Anterior Cruciate Ligament Injury Risk in Female Athletes: A Prospective Study. Am. J. Sports Med. 2005;33:492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 47.Hewett TE, Myer GD, Ford KR, J.L. S. Preparticipation Physical Exam Using a Box Drop Vertical Jump Test in Young Athletes: The Effects of Puberty and Sex. Clin. J. Sport Med. 2006;16:298–304. doi: 10.1097/00042752-200607000-00003. [DOI] [PubMed] [Google Scholar]
- 48.Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes. Decreased impact forces and increased hamstring torques. Am. J. Sports Med. 1996;24:765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 49.Jones C, Christensen C, Young M. Weight training injury trends. Physician and Sports Medicine. 2000;28:61–72. doi: 10.3810/psm.2000.07.1086. [DOI] [PubMed] [Google Scholar]
- 50.Kellis E, Tsitskaris GK, Nikopoulou MD, Moiusikou KC. The evaluation of jumping ability of male and female basketball players according to their chronological age and major leagues. J Strength Cond Res. 1999;13:40–46. [Google Scholar]
- 51.Khamis HJ, Roche AF. Predicting adult stature without using skeletal age: the Khamis-Roche method. Pediatrics. 1994;94:504–507. [PubMed] [Google Scholar]
- 52.Kjonniksen L, Anderssen N, Wold B. Organized youth sport as a predictor of physical activity in adulthood. Scand. J. Med. Sci. Sports. 2009;19:646–654. doi: 10.1111/j.1600-0838.2008.00850.x. [DOI] [PubMed] [Google Scholar]
- 53.Kraemer WJ, Fleck SJ, Callister R, Shealy M, Dudley GA, Maresh CM, Marchitelli L, Cruthirds C, Murray T, Falkel JE. Training responses of plasma beta-endorphin, adrenocorticotropin, and cortisol. Med. Sci. Sports Exerc. 1989;21:146–153. [PubMed] [Google Scholar]
- 54.Lee S, Burgeson C, Fulton J, Spain C. Physical education and physical activity: Results from the school health policies and programs study 2006. J. Sch. Health. 2007;77:435–463. doi: 10.1111/j.1746-1561.2007.00229.x. [DOI] [PubMed] [Google Scholar]
- 55.Leek D, Carlson JA, Cain KL, Henrichon S, Rosenberg D, Patrick K, Sallis JF. Physical Activity During Youth Sports Practices. Arch. Pediatr. Adolesc. Med. 2010 doi: 10.1001/archpediatrics.2010.252. [DOI] [PubMed] [Google Scholar]
- 56.Lehnhard RA, Lehnhard HR, Young R, Butterfield SA. Monitoring injuries on a college soccer team: the effect of strength training. J Strength Cond Res. 1996;10:115–119. [Google Scholar]
- 57.Lloyd DG, Buchanan TS. Strategies of muscular support of varus and valgus isometric loads at the human knee. J. Biomech. 2001;34:1257–1267. doi: 10.1016/s0021-9290(01)00095-1. [DOI] [PubMed] [Google Scholar]
- 58.Lopes VP, Rodrigues LP, Maia JA, Malina RM. Motor coordination as predictor of physical activity in childhood. Scand. J. Med. Sci. Sports. 2010 doi: 10.1111/j.1600-0838.2009.01027.x. [DOI] [PubMed] [Google Scholar]
- 59.Lubans DR, Morgan PJ, Cliff DP, Barnett LM, Okely AD. Fundamental movement skills in children and adolescents: review of associated health benefits. Sports Med. 2010;40:1019–1035. doi: 10.2165/11536850-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 60.Malina RM. Weight training in youth-growth, maturation, and safety: an evidence-based review. Clin. J. Sport Med. 2006;16:478–487. doi: 10.1097/01.jsm.0000248843.31874.be. [DOI] [PubMed] [Google Scholar]
- 61.Malina RM, Bouchard C. Growth, maturation, and physical activity. Human Kinetics; Champaign, Il: 1991. Timing and sequence of changes in growth, maturation, and performance during adolescence; pp. 267–272. [Google Scholar]
- 62.Malina RM, Cumming SP, Morano PJ, Barron M, Miller SJ. Maturity status of youth football players: a noninvasive estimate. Med. Sci. Sports Exerc. 2005;37:1044–1052. [PubMed] [Google Scholar]
- 63.Mandelbaum BR, Silvers HJ, Watanabe DS, Knarr JF, Thomas SD, Griffin LY, Kirkendall DT, Garrett W., Jr. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am. J. Sports Med. 2005;33:1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 64.McNitt-Gray JL, Hester DME, Mathiyakom W, Munkasy BA. Mechanical demand on multijoint control during landing depend on orientation of the body segments relative to the reaction force. J of Biomech. 2001;34:1471–1482. doi: 10.1016/s0021-9290(01)00110-5. [DOI] [PubMed] [Google Scholar]
- 65.Micheli L. Preventing injuries in team sports: What the team physician needs to know. In: Chan K, Micheli L, Smith A, Rolf C, Bachl N, Frontera W, Alenabi T, editors. F.I.M.S. Team Physician Manual. CD Concepts; Hong Kong: 2006. pp. 555–572. [Google Scholar]
- 66.Miller MG, Cheatham CC, Patel ND. Resistance training for adolescents. Pediatr. Clin. North Am. 2010;57:671–682. doi: 10.1016/j.pcl.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 67.Myer GD, Brunner HI, Melson PG, Paterno MV, Ford KR, Hewett TE. Specialized neuromuscular training to improve neuromuscular function and biomechanics in a patient with quiescent juvenile rheumatoid arthritis. Phys. Ther. 2005;85:791–802. [PubMed] [Google Scholar]
- 68.Myer GD, Chu DA, Brent JL, Hewett TE. Trunk and hip control neuromuscular training for the prevention of knee joint injury. Clin. Sports Med. 2008;27:425–448. ix. doi: 10.1016/j.csm.2008.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Myer GD, Faigenbaum AD, Chu DA, Falkel J, Ford KR, Best TM, Hewett TE. Integrative Training for Children and Adolescents: Techniques and Practices for Reducing Sports-related Injuries and Enhancing Athletic Performance. Physician and Sports Medicine. 2011 doi: 10.3810/psm.2011.02.1854. In Press. [DOI] [PubMed] [Google Scholar]
- 70.Myer GD, Ford KR, Barber Foss KD, Goodman A, Ceasar A, Rauh MJ, Divine JG, Hewett TE. The incidence and potential pathomechanics of patellofemoral pain in female athletes. Clin Biomech. 2010;25:700–707. doi: 10.1016/j.clinbiomech.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Myer GD, Ford KR, Barber Foss KD, Liu C, Nick TG, Hewett TE. The relationship of hamstrings and quadriceps strength to anterior cruciate ligament injury in female athletes. Clin. J. Sport Med. 2009;19:3–8. doi: 10.1097/JSM.0b013e318190bddb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Myer GD, Ford KR, Brent JL, Hewett TE. The Effects of Plyometric versus Dynamic Balance Training on Power, Balance and Landing Force in Female Athletes. J Strength Cond Res. 2006;20:345–353. doi: 10.1519/R-17955.1. [DOI] [PubMed] [Google Scholar]
- 73.Myer GD, Ford KR, Brent JL, Hewett TE. Differential neuromuscular training effects on ACL injury risk factors in “high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007;8:1–7. doi: 10.1186/1471-2474-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Myer GD, Ford KR, McLean SG, Hewett TE. The Effects of Plyometric Versus Dynamic Stabilization and Balance Training on Lower Extremity Biomechanics. Am. J. Sports Med. 2006;34:490–498. doi: 10.1177/0363546505281241. [DOI] [PubMed] [Google Scholar]
- 75.Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19:51–60. doi: 10.1519/13643.1. [DOI] [PubMed] [Google Scholar]
- 76.Myer GD, Quatman CE, Khoury J, Wall EJ, Hewett TE. Youth vs. Adult “Weightlifting” Injuries Presenting to United States Emergency Rooms: Accidental vs. Non-accidental injury mechanisms. Journal ofStrength and Conditioning Research. 2008 doi: 10.1519/JSC.0b013e3181b86712. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Myer GD, Quatman CE, Khoury J, Wall EJ, Hewett TE. Youth versus adult “weightlifting“ injuries presenting to United States emergency rooms: accidental versus nonaccidental injury mechanisms. J StrengthCond Res. 2009;23:2054–2060. doi: 10.1519/JSC.0b013e3181b86712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nader P, Bradley R, Houts R, McRitchie S, O'Brien M. Moderate to vigorous physical activity from ages 9 to 15 years. Journal of the American Medical Association. 2008;300:295–305. doi: 10.1001/jama.300.3.295. [DOI] [PubMed] [Google Scholar]
- 79.Nyberg G, Nordenfelt A, Ekelund U, Marcus C. Physical activity patterns measured by accelerometry in 6- to 10-yr-old children. Medicine and Science in Sports and Exercise. 2009;41:1842–1848. doi: 10.1249/MSS.0b013e3181a48ee6. [DOI] [PubMed] [Google Scholar]
- 80.Pate RR, O'Neill JR. Youth Sports Programs: Contribution to Physical Activity. Arch. Pediatr. Adolesc. Med. 2010 doi: 10.1001/archpediatrics.2010.245. [DOI] [PubMed] [Google Scholar]
- 81.Pfeiffer R, Francis R. Effects of Strength training on Muscle development in prepubescent, pubescent, and postpubescent males. Phys Sportsmed. 1986;14:134–143. doi: 10.1080/00913847.1986.11709173. [DOI] [PubMed] [Google Scholar]
- 82.Pierce K, Brewer C, Ramsey M, Byrd R, Sands W, Stone M, Stone M. Youth resistance training. Professional Strength and Conditioning. 2008;10:9–23. [Google Scholar]
- 83.Ploughman M. Exercise is brain food: the effects of physical activity on cognitive function. DevNeurorehabil. 2008;11:236–240. doi: 10.1080/17518420801997007. [DOI] [PubMed] [Google Scholar]
- 84.Plumert J, Schwebel D. Social and temperamental influences on children's overestimation of their physical abilities: Links to accidental injuries. J Exp Child Psychol. 1997;67:317–337. doi: 10.1006/jecp.1997.2411. [DOI] [PubMed] [Google Scholar]
- 85.Quatman CE, Ford KR, Myer GD, Hewett TE. Maturation Leads to Gender Differences in Landing Force and Vertical Jump Performance: A Longitudinal Study. Am. J. Sports Med. 2006;34:806–813. doi: 10.1177/0363546505281916. [DOI] [PubMed] [Google Scholar]
- 86.Ramsay J, Blimkie C, Smith K, Garner S, MacDougall J, Sale D. Strength Training Effects in Prepubescent boys. Med Sci Sports Exerc. 1990;22:605–614. doi: 10.1249/00005768-199010000-00011. [DOI] [PubMed] [Google Scholar]
- 87.Razquin C, Marti A, Martinez JA. Evidences on three relevant obesogenes: MC4R, FTO and PPARgamma. Approaches for personalized nutrition. Mol. Nutr. Food Res. 2010 doi: 10.1002/mnfr.201000445. [DOI] [PubMed] [Google Scholar]
- 88.Risser WL. Weight-training injuries in children and adolescents. Am Fam Physician. 1991;44:2104–2108. [PubMed] [Google Scholar]
- 89.Rogasch NC, Dartnall TJ, Cirillo J, Nordstrom MA, Semmler JG. Corticomotor plasticity and learning of a ballistic thumb training task are diminished in older adults. J. Appl. Physiol. 2009;107:1874–1883. doi: 10.1152/japplphysiol.00443.2009. [DOI] [PubMed] [Google Scholar]
- 90.Rosengren KS, Geert JP, Savelsbergh JvdK. Development and learning: a TASC-based perspective of the acquisition of perceptual-motor behaviors. Infant Behavior and Development. 2003;26:473–494. [Google Scholar]
- 91.Rowland T. Promoting physical activity for children's health. Sports Medicine. 2007;37:929–936. doi: 10.2165/00007256-200737110-00001. [DOI] [PubMed] [Google Scholar]
- 92.Rowland TW. Exercise and children's health. Human Kinetics Books; Champaign, Ill.: 1990. [Google Scholar]
- 93.Ruiz J, Castro-Pinero J, Artero E, Ortega F, Sjostrom M, Suni J, Castillo M. Predictive validity of health related fitness in youth: a systematic review. British Journal of Sports Medicine. 2009;43:909–923. doi: 10.1136/bjsm.2008.056499. [DOI] [PubMed] [Google Scholar]
- 94.Sailors M, Berg K. Comparison of responses to weight training in pubescent boys and men. J Sports Med Phys Fitness. 1987;27:30–37. [PubMed] [Google Scholar]
- 95.Sewall L, Micheli L. Strength Training for Children. J Pediatr Orthop. 1986;6:143–146. doi: 10.1097/01241398-198603000-00004. [DOI] [PubMed] [Google Scholar]
- 96.Shenk D. The genius in all of us: why everything you've been told about genetics, talent, and IQ is wrong. Doubleday; New York: 2010. [Google Scholar]
- 97.Stodden DJ, Goodway S, Langendorfer S, Robertson M, Rudisill M, Garcia C. A developmental perspective on the role of motor skill competence in physical activity: An emergent relationship. Quest. 2008;60:290–306. [Google Scholar]
- 98.Strong WB, Malina RM, Blimkie CJ, Daniels SR, Dishman RK, Gutin B, Hergenroeder AC, Must A, Nixon PA, Pivarnik JM, Rowland T, Trost S, Trudeau F. Evidence based physical activity for school-age youth. J. Pediatr. 2005;146:732–737. doi: 10.1016/j.jpeds.2005.01.055. [DOI] [PubMed] [Google Scholar]
- 99.Tanner JM, Whitehouse RH, Marubini E, Resele LF. The adolescent growth spurt of boys and girls of the Harpenden growth study. Ann. Hum. Biol. 1976;3:109–126. doi: 10.1080/03014467600001231. [DOI] [PubMed] [Google Scholar]
- 100.Tibone JE, Antich TJ, Fanton GS, Moynes DR, Perry J. Functional analysis of anterior cruciate ligament instability. Am J Sport Med. 1986;14:276–284. doi: 10.1177/036354658601400406. [DOI] [PubMed] [Google Scholar]
- 101.Tryon RC. Genetic differences in maze-learning ability in rats. Yearbook of the National Society for the Study of Education. 1940;39:111–119. [Google Scholar]
- 102.Tryon RC. Comparative psychology. Prentice-Hall, Inc.; New York: 1942. [Google Scholar]
- 103.Tudor-Locke C, Johnson WD, Katzmarzyk PT. Accelerometer-determined steps per day in US children and youth. Med. Sci. Sports Exerc. 2010;42:2244–2250. doi: 10.1249/MSS.0b013e3181e32d7f. [DOI] [PubMed] [Google Scholar]
- 104.United States Department of Health and Human Services . Book Physical Activity Guidelines for Americans. City: 2008. Physical Activity Guidelines for Americans. www.health.gov/paguidelines. [Google Scholar]
- 105.Weltman A, Janney C, Rians CB, Strand K, Berg B, Tippitt S, Wise J, Cahill BR, Katch FI. The effects of hydraulic resistance strength training in pre-pubertal males. Med Sci Sports Exerc. 1986;18:629–638. [PubMed] [Google Scholar]
- 106.Winsley R, Matos N. Overtraining and elite young athletes. Med Sport Sci. 2011;56:97–105. doi: 10.1159/000320636. [DOI] [PubMed] [Google Scholar]
- 107.Young WK, Metzl JD. Strength training for the young athlete. Pediatric Annals. 2010;39:293–299. doi: 10.3928/00904481-20100422-10. [DOI] [PubMed] [Google Scholar]
- 108.Zaricznyj B, Shattuck L, Mast T, Robertson R, D”Elia G. Sports-related injuries in school-age children. American Journal of Sports Medicine. 1980;8:318–324. doi: 10.1177/036354658000800504. [DOI] [PubMed] [Google Scholar]