Abstract
Purpose
The purpose of this study was to objectively evaluate if the double bundle ACL reconstruction can better restore the normal translational and rotational laxities than the conventional single bundle ACL reconstruction among the reported biomechanical studies.
Methods
A systematic literature search was conducted to identify in vitro and in vivo (intra-operative) biomechanical studies that compared the laxities (anterior or anteroposterior or rotational) between single and double bundle ACL reconstructions. Due to a large variability among the loading conditions and testing methods used to determine the rotational laxities between the studies, a meta-analysis of rotational laxities was not feasible.
Results
Seven in vitro and three in vivo studies were included in this analysis based on the predefined inclusion criteria. The overall mean difference calculated by the random effects model in the anteroposterior laxity between the single bundle and double bundle ACL reconstruction techniques at 0°, 30°, 60° and 90° of flexion were 0.99 mm, 0.38 mm, 0.34 mm, and 0.07 mm respectively. No statistical significant difference was noted between the two treatments at all flexion angles. Among the nine studies that compared the rotational laxity of single bundle and double bundle ACL reconstructions, four studies reported that double bundle reconstruction can provide a better rotational control compared to the single bundle reconstruction. The other five studies could not identify any significant difference between the two reconstructions in terms of the rotational laxity.
Conclusions
Both single and double bundle treatment options for anterior cruciate ligament injury result in similar anteroposterior knee joint laxity at time-zero. No 1 conclusive evidence on the superiority of one reconstruction technique over the other in terms of rotation laxity can be obtained due to several variations in the experimental protocol and the parameters used to measure the rotational laxity among the studies.
Level of Evidence
Level III
INTRODUCTION
Due to a large number of anterior cruciate ligament (ACL) injuries not only among the high performance athletes but also among the general population, there have been numerous efforts aimed at effectively managing an ACL injury. Single bundle ACL reconstruction has been the most commonly employed operative treatment for an ACL injury where an autogenous or allogeneic graft is fixed in a single tibial and femoral tunnel.1 However, it is reported that only 67% to 76% of the ACL reconstructed patients with either hamstring tendon graft or bone-patellar tendon-bone graft could return to their preinjury level of activity.2 Further, development of degenerative changes in the knee joint remains a major concern after such surgical interventions.3,4 Some of these complications have been attributed to inefficient control of tibial rotation after single bundle ACL reconstruction.5–8
To further improve on the current single bundle ACL reconstruction techniques and with a greater understanding of the ACL anatomy, double bundle ACL reconstruction techniques are being advocated to reproduce the native anatomy of the ACL more closely and hence potentially provide a better stability to the knee joint.9–11 While there is an apparent theoretical advantage of reconstructing both bundles of the ACL, a consensus has yet to be established on the superiority of double bundle ACL reconstruction over the conventional single bundle ACL reconstruction.11–13
Recently, a meta-analysis of outcomes showed a significantly smaller side-to-side difference in KT-1000 arthrometer measurement after a double bundle ACL reconstruction compared to single bundle ACL reconstruction, but this difference was deemed to be clinically insignificant.13 Further, they found no significant difference between the two reconstructions in terms of the pivot shift testing when the results were dichotomized as normal/nearly normal versus abnormal/severely abnormal. However, “nearly normal” could be argued as not being good enough, especially in young and high performance ACL injured patients.14 Furthermore, current clinical outcome measurements have been criticized for the lack of accuracy, reliability and are known to be subjective.15–19 In order to accurately assess the superiority of a particular reconstruction technique for the treatment of ACL injury, such confounding factors need to be minimized. Various in vitro and in vivo biomechanical studies have used more objective, accurate and reliable testing tools such as the navigation system and robotic testing system to evaluate the efficacy of various reconstruction techniques.11,19–25 Therefore, the primary objective of this study was to systematically review the literature on the efficacy of double and single bundle ACL reconstruction techniques in restoring normal joint laxity among the in vitro and in vivo (intra-operative) biomechanical studies. We hypothesized that double bundle ACL reconstruction can better restore the translational and rotational knee joint laxities compared to single bundle ACL reconstruction at time-zero.
MATERIALS AND METHODS
DATA SOURCES
A systematic search of MEDLINE and EMBASE (January 1990 – March 2010) was conducted to identify in vitro and in vivo (intra-operative) biomechanical studies that compared the laxity (anterior or anteroposterior or rotational) between double bundle and single bundle ACL reconstructions. These databases were searched for the relevant articles by using the following key words: anterior cruciate ligament, single bundle anterior cruciate ligament, double bundle anterior cruciate ligament, anterior cruciate ligament reconstruction, and anterior cruciate ligament biomechanics. References of each selected article were manually searched for any articles that may have been missed during the database search. Two authors performed the search for the relevant articles and the identified articles were included in this study on consensus.
STUDY SELECTION
The selected articles were further screened to be included in this systematic review based on the following inclusion criteria. All studies included have reported at least one of the laxity (anterior or anteroposterior or rotational) measurement regardless of the language that they were published in. There were no restrictions applied to the source of grafts or fixation devices used in the reconstruction procedures. Studies which did not use human knees or that used synthetic graft materials were excluded from this analysis. Furthermore, included studies were analyzed to ensure that reported data were not duplicated in different reports of the same trial. Sensitivity analyses were performed to examine if there were any significant differences in the conclusion when the analysis was performed on studies grouped as 1) in vitro studies, 2) in vivo studies, 3) studies that used two tibial tunnels for double bundle reconstruction, and 4) studies that used one tibial tunnel for double bundle reconstruction.
DATA EXTRACTION
Data extraction from each included study was performed by 2 different authors independently and was recorded in a Microsoft Excel worksheet (Microsoft, CA). The following data was extracted from each included study: first author, year of publication, number of specimens/ subjects used in each treatment group, mean anterior/anteroposterior laxity measurements at 0°, 30°, 60° and 90° of flexion angles and their corresponding variance. All the outcomes were extracted as continuous variables from the included studies. The means and variances that were only reported in the form of a figure were extracted by open source digitizing software (Engauge Digitizer 4.1). Figure 4 from Yagi et al26 was digitized to obtain the mean and variance at full extension and 60° of flexion. Similarly, figure 4A from Mae et al24 was digitized for the mean and variance at 60° and 90° flexion. Additional data that were extracted included number of femoral and tibial tunnels, tunnel positions, graft material, graft fixation angle, initial graft tension and loading conditions.
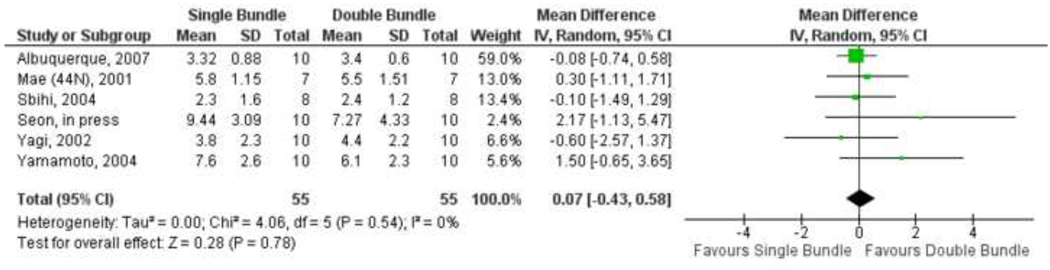
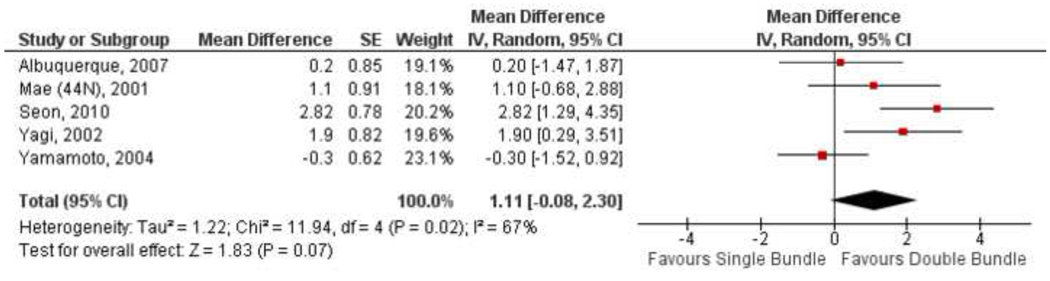
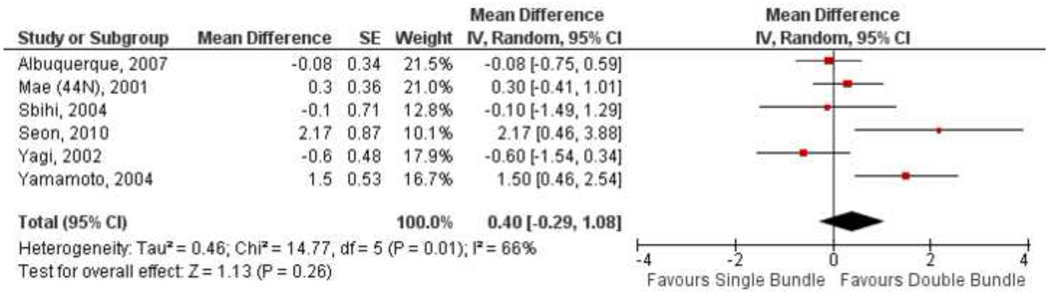
Figure 4.
Forest plot of anterior/ anteroposterior laxities of SB and DB ACL reconstructions at 90° of flexion. The mean difference in laxities for each study is represented by the square and its size represents the weight of the study; the horizontal line running through the square represents the 95% confidence interval; the overall estimate of the mean difference is represented as a diamond, with its horizontal tips representing the 95% confidence interval.
DATA ANALYSIS AND STATISTICAL METHODS
The absolute difference between means, variance and the 95% confidence interval for each individual trial were calculated. In order to account for both the between-study and within-study variances, a random effects model was used to calculate the overall mean difference between the two treatments and its corresponding 95% confidence interval. Four24,26–28 among the ten11,24–32 studies included in the meta-analysis had a paired study design where the efficacy of each treatment was investigated by use a robotic testing system in the same specimen. The other six10,11,25,29,31,32 studies used two independent groups of patients/ specimens for each treatment. Paired analyses results for three24,26,28 of the four studies that used a paired design were not available from the manuscript. These studies only reported the means and standard deviations for each treatment separately. Therefore, measurements reported for each treatment were included in the meta-analysis as if they were obtained from independent groups for each treatment. Another approach to include the studies with a paired design in the meta-analysis was explored by an attempt to approximate the paired analysis. Paired analysis results were estimated by imputing the correlation coefficient from Seon et al.27 for three studies.24,26,28 The results of this analysis is presented in detail in the appendix.
To assess the robustness of the meta-analysis results, the influence of variables (in vitro/ in vivo study design, number of tibial tunnels used in double bundle reconstruction and graft source) on the pooled estimate of the treatment difference was explored by performing a series of subgroup analyses. All statistical analysis was performed by using RevMan 5.0.18.33
Due to a large variability among the loading conditions and testing methods used to determine the rotational laxity between the studies, a meta-analysis of these studies was not feasible. Instead, the results from the original articles on the rotational laxities are presented as a systematic review.
RESULTS
Our literature search produced 21 biomechanical studies (in vitro and in vivo) that compared the laxities following single bundle and double bundle ACL reconstructions.9,11,22–32,34–41 Ten studies from these 21 studies were excluded, four22,23,39,41 because no variance and/or means were reported, one9 study that used prosthetic ligament for reconstruction, one37 study that used sheep knee specimens, one34 study that used a rectangular femoral tunnel for single bundle ACL reconstruction, two38,40 studies due to duplication of data and one35 review article. One of the included studies reported only rotational laxity.36 Seven in vitro24–29,32 and three in vivo11,30,31 studies were selected based on the predefined inclusion criteria for this analysis. Of the included studies, four of the seven in vitro studies24,26,28,29 used two femoral tunnels and one tibial tunnel for their double bundle ACL reconstructions and three studies25,27,32 reamed two separate tunnels for each of the bundles on the femur and tibia. All of the included in vivo studies used two separate tunnels for each of the bundles on the femur and tibia for the double bundle ACL reconstruction. A summary of the data extracted from these studies is presented in table 1 and table 2.
Table 1.
Summary of in vitro biomechanical studies
| Study | Femoral tunnel placement |
Tibial tunnel placement |
Graft material | Graft fixation angle/ Tension |
Testing equipment/ Loading conditions |
Graft fixation methods |
Conclusion |
|---|---|---|---|---|---|---|---|
| Albuquerque et al29 | SB: “30° from the central position” | SB: 5 mm anterior to the medial intercondylar tubercle | SB: QT | SB: 30°/ manual | Universal Kratos® Model k5002 testing machine/ 100 N anterior force | Tibia: Bicortical screw and washer | Both the ACL reconstruction techniques are not capable of restoring intact knee stability |
| DB: AMB: same as SB with a smaller diameter PLB: 2mm posterior-inferior from AMB | DB: same as SB | DB: AMB: Split QT PLB: Split QT | DB: AMB: 30°/ manual PLB: 30°/ manual | Femur: Suture and bicortical screw | |||
| Ho et al25 | SB: 25% and 28.5% from posterior femoral cortex and Blumensaat line respectively | SB: 44% and 43% from medial tibial cortex and anterior tibial cortex | SB: ST/ GRA | SB: 30°/ 67 N | Navigation system/ 133 N anterior force | Tibia: BioRCI biointerference screw | Both reconstruction s can equally restore joint stability |
| DB: AMB: Center of AMB PLB: Center of PLB | DB: AMB: Center of AMB PLB: Center of PLB | DB: AMB: ST PLB: GRA | DB: AMB: 60°/ 67 N PLB: full extension/ 67 N | Femur: EndoButton CL | |||
| Mae et al24 | SB: 11:00/ 1:00 o’clock | SB: Center of ACL footprint | SB: ST/ GRA | SB: 20°/ 44N and 88N | Robotic simulator/ 100 N anterior & posterior force | Tibia: Custommade force gauges | Two femoral sockets ACL reconstruction provided better anteriorposterior stability compared to single femoral socket ACL reconstruction |
| DB: AMB: 11:00/ 1:00 o’clock PLB: 9:30/ 2:30 o’clock | DB: same as SB | DB: AMB: ST PLB: GRA | DB: AMB: 20°/ 22N and 44N PLB: 20°/ 22N and 44N | Femur: EndoButton | |||
| Sbihi et al32 | SB: 11:00/ 1:00 o’clock | SB: Posteromedial portion of the ACL footprint | SB: ST/ GRA | SB: NI/ 50N | Rolimeter™/ maximum manual force | Tibia: Interference screw with staples | DB ACL reconstruction only resulted in a small improvement in anterior laxity compared to SB ACL reconstruction |
| DB: AMB: 11:00/ 1:00 o’clock PLB: 9:30/ 2:30 o’clock | DB: AMB: 7–8 mm anterior to the PLB PLB: Anterior to anterolateral tibial spine, 7 mm anterior to PCL | DB: AMB: ST PLB: GRA | DB: AMB: 45° to 90°/ 50N PLB: 15°/ 50N | Femur: Suture and bicortical screw | |||
| Seon et al27 | SB: 10:30/ 1:30 o’clock | SB: Center of ACL footprint | SB: ST/ GRA | SB: Full extension/ 40N | Robotic testing system/ 134 N anterior load | Tibia: Tibial IntraFix | DB ACL reconstruction can better restore the AP laxity than SB ACL reconstruction |
| DB: AMB: Center of AMB PLB: Center of PLB | DB: AMB: Center of AMB PLB: Center of PLB | DB: AMB: ST PLB: GRA | DB: AMB: 60°/ 20N PLB: Full extension/ 20N | Femur: EndoButton CL | |||
| Yagi et al26 | SB: 11:00/ 1:00 o’clock | SB: 5–7 mm anterior to PCL | SB: ST/ GRA | SB: 30°/ 44N | Robotic testing system/ 134 N anterior load | Tibia: Bicortical screw and washer | DB ACL reconstruction provides better rotational stability than SB ACL |
| DB: AMB: Center of AMB PLB: Center of PLB | DB: same as SB | DB: AMB: ST PLB: GRA | DB: AMB: 60°/ 22N PLB: 15°/ 22N | Femur: EndoButton CL | |||
| Yamamoto et al28 | SB: “approximate the PL bundle of the ACL” | SB: 5–7 mm anterior to PCL | SB: ST/ GRA | SB: 30°/ 44N | Robotic testing system/ 134 N anterior load | Tibia: Spiked washer and screw | Lateralized SB ACL reconstruction is comparable to DB ACL reconstruction at low flexion angles |
| DB: AMB: Center of AMB PLB: Center of PLB | DB: same as SB | DB: AMB: ST PLB: GRA | DB: AMB: 60°/ 22N PLB: 15°/ 22N | Femur: EndoButton CL |
AMB, Antreomedial bundle; AP, Anterior-Posterior; BPTB, Bone-patellar tendon-Bone; DB, Double bundle ACL reconstruction; GRA, Gracilis tenson; NI, No information available; PCL, posterior cruciate ligament; PLB, Posterolateral bundle; QT, Quadriceps tendon; SB, Single bundle ACL reconstruction; ST, Semitendinosus tendon
Table 2.
Summary of in vivo biomechanical studies
| Study | Femoral tunnel placement |
Tibial tunnel placement |
Graft material | Graft fixation angle/ Tension |
Testing equipment/ Loading conditions |
Graft fixation methods |
Conclusion |
|---|---|---|---|---|---|---|---|
| Ferretti et al30 | SB: 11:00/ 1:00 o’clock | SB: 7 mm anterior to PCL | SB: ST/ GRA | SB: NI | Navigation system/maximum manual force | Tibia: SB: Evolgate DB: Interference screws | Both reconstruction s improved anteroposterior and rotational stability without any significant differences between them |
| DB: AMB: insertion site of AMB PLB: insertion site of PLB | DB: AMB: insertion site of AMB PLB: insertion site of PLB | DB:AMB: ST PLB: GRA | DB: AMB: 60°/ manual PLB: 15°/manual | Femur: SB: SwingBridgeDB: Mini- SwingBridge | |||
| Hofbauer et al31 | SB: 10:00/ 2:00 o’clock | SB: Center of AMB footprint | SB: ST (17 patients), ST/ GRA (10 patients) | SB: NI | Navigation system/ maximum manual force | Tibia: Suture disc | No significant difference between the two techniques was observed in terms of AP laxity |
| DB: AMB: 11:00/1:00 o’clock PLB: 9:30/ 2:30 o’clock | DB: NI | DB: ST (5 patients), ST/ GRA (23 patients). Thicker graft for AMB and thinner graft for PLB | DB: NI | Femur: EndoButton CL | |||
| Song et al11 | SB: 11:00/1:00 o’clock | SB: Center of ACL footprint | SB: tibialis anterior | SB: 10°–20°/ manual maximal tension | Navigation system/maximum manual force | Tibia: Bioabsorbable interference screws and staple | DB ACL reconstruction can provide better anteroposterio r and rotational stability than SB ACL reconstruction |
| DB: AMB: 11:00/1:00 o’clock PLB: 5 to 8 mm anterior to LFC cartilage and 3 to 5 mm from the inferior LFC cartilage at 90° of flexion. | DB: AMB: 7 mm anterior and 5 mm medial to the PLB tunnel PLB: center of PLB footprint | DB: AMB: tibialis anterior PLB: tibialis anterior | DB: AMB: 60°–70°/manual maximal tension PLB: 10°–20°/ manual maximal tension | Femur: EndoButton |
AMB, Antreomedial bundle; AP, Anterior-Posterior; BPTB, Bone-patellar tendon-Bone; DB, Double bundle ACL reconstruction; GRA, Gracilis tenson; NI, No information available; PCL, posterior cruciate ligament; PLB, Posterolateral bundle; QT, Quadriceps tendon; SB, Single bundle ACL reconstruction; ST, Semitendinosus tendon
Anterior Laxity
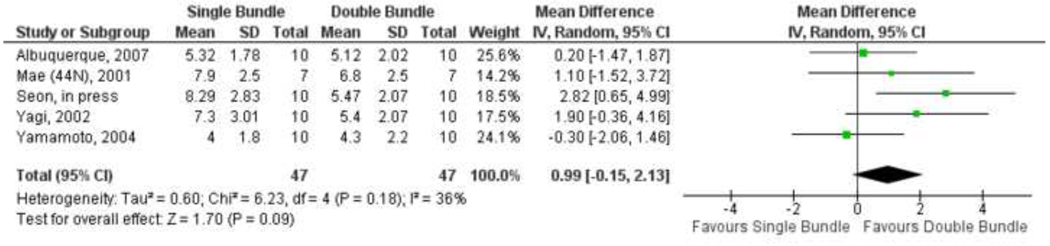
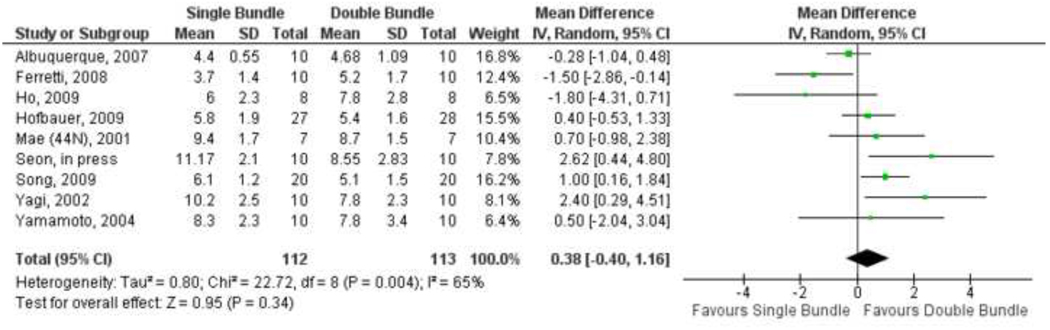
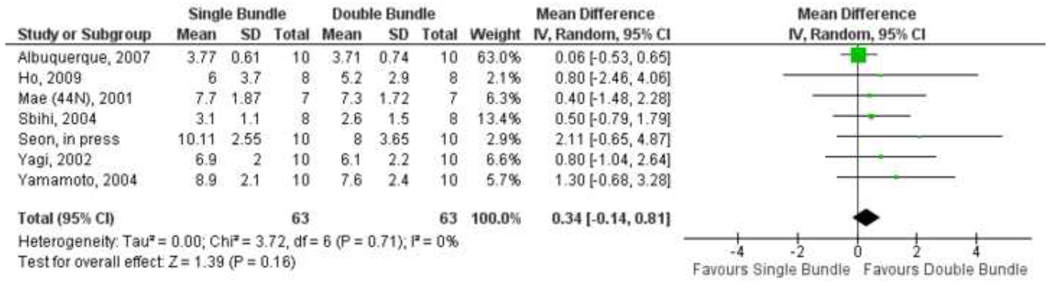
When all the included studies were analyzed together, the overall mean difference calculated by the random effects model in the anteroposterior laxity between the single bundle and double bundle ACL reconstruction techniques at 0° of flexion was 0.99 mm (95% CI: −0.15 to 2.13). This mean difference implies that on average a knee reconstructed by single bundle ACL reconstruction is 0.99 mm more lax in the anteroposterior direction at 0° than a knee reconstructed by double bundle ACL reconstruction. Similarly, the overall mean difference calculated by the random effects model in the anteroposterior laxity between the single bundle and double bundle ACL reconstruction techniques at 30°, 60° and 90° of flexion are 0.38 mm (95% CI: −0.40 to 1.16), 0.34 mm (95% CI: −0.14 to 0.81) and 0.07 mm (95% CI: −0.43 to 0.58) respectively. These results of the meta-analysis for 0°, 30°, 60° and 90° of flexion are presented in figures 1, 2, 3 and 4 respectively. No statistical significant difference was noted between the two treatments at all flexion angles. Similar overall mean differences between the two treatments were observed in the analysis where the correlation coefficient was imputed (appendix).
Figure 1.
Forest plot of anterior/ anteroposterior laxities of SB and DB ACL reconstructions at 0° of flexion. The mean difference in laxities for each study is represented by the square and its size represents the weight of the study; the horizontal line running through the square represents the 95% confidence interval; the overall estimate of the mean difference is represented as a diamond, with its horizontal tips representing the 95% confidence interval.
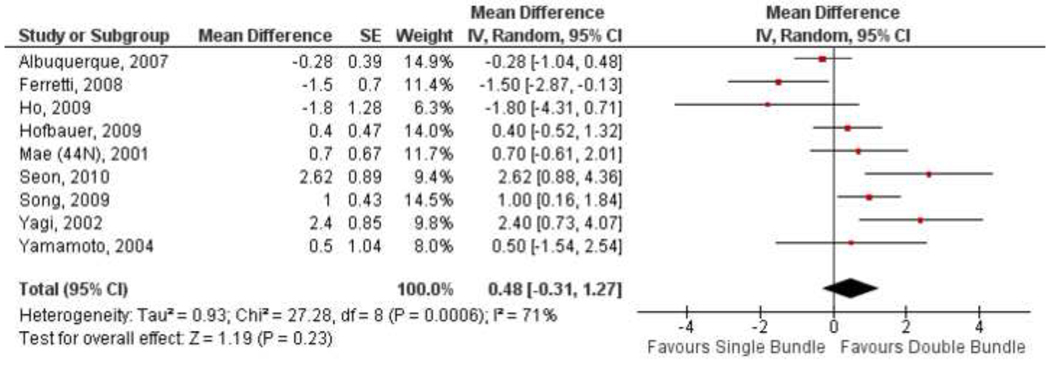
Figure 2.
Forest plot of anterior/ anteroposterior laxities of SB and DB ACL reconstructions at 30° of flexion. The mean difference in laxities for each study is represented by the square and its size represents the weight of the study; the horizontal line running through the square represents the 95% confidence interval; the overall estimate of the mean difference is represented as a diamond, with its horizontal tips representing the 95% confidence interval.
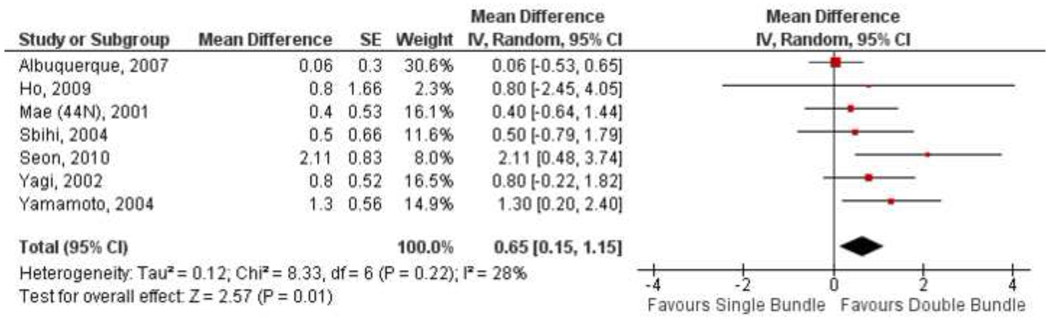
Figure 3.
Forest plot of anterior/ anteroposterior laxities of SB and DB ACL reconstructions at 60° of flexion. The mean difference in laxities for each study is represented by the square and its size represents the weight of the study; the horizontal line running through the square represents the 95% confidence interval; the overall estimate of the mean difference is represented as a diamond, with its horizontal tips representing the 95% confidence interval.
When in vitro and in vivo studies were analyzed separately, the overall mean difference between the single bundle and double bundle ACL reconstruction techniques at 30° of flexion was 0.64 mm (95% CI: −0.55 to 1.84) and 0.07 mm (95% CI: −1.21 to 1.35) respectively, with no statistical significant difference between the two treatments in either groups. Analysis of the in vitro studies as two separate groups (one tibial tunnel24,26,28,29 and two tibial tunnels25,27,32) revealed that the overall mean difference between the two treatments was < 1.0 mm which was not statistically significant. Finally, when in vitro25,27 and in vivo11,30,31 studies that used two tibial tunnels for their double bundle reconstructions were compared to the single bundle reconstructions, we found an overall mean difference of 0.38 mm (95% CI: −0.15 to 0.92) between the two techniques at 30° of flexion. Semitendinosus and gracilis tendons were used as graft material in eight of the ten included studies. Subgroup analyses of these studies resulted in an overall mean difference between the two treatments of 1.29 mm (95% CI: −0.16 to 2.73), 0.42 mm (95% CI: −0.71 to 1.56), 0.80 mm (95% CI: 0.03 to 1.58), and 0.29 mm (95% CI: − 0.50 to 1.09) at 0°, 30°, 60° and 90° of flexion respectively.
Due to the low standard deviation reported in Albuquerque et al.29 study at 60° and 90° of flexion, the weights assigned to this study were rather high 63% and 59% respectively. A sensitivity analysis was performed by excluding this study from the meta-analysis to explore its influence on the overall treatment difference. The overall mean differences between the single bundle and double bundle ACL reconstruction techniques with the exclusion of Albuquerque et al.29 at 60° and 90° of flexion were 0.80 mm (95% CI: 0.03 to 1.58) and 0.29 mm (95% CI: −0.50 to 1.09), respectively.
Rotational Laxity
Six in vitro22,25–28,36 and 3 in vivo11,30,31 biomechanical studies that compared the rotational laxities following single bundle and double bundle reconstruction techniques were identified. Various loading conditions have been used to evaluate the rotational laxity among these studies. The measurements reported following the application of these loads included anterior, anterior-posterior translations and internal, external, internalexternal rotations. The rotational laxities reported among the included studies are summarized in table 3. Among these 9 studies that compared the rotational laxities following single and double bundle ACL reconstructions, 2 in vitro26,27 studies and 2 in vivo11,31 studies found significant differences between the two techniques. The other five22,25,28,30,36 studies could not find any significant difference in the rotational laxities between single and double bundle reconstructed knees.
Table 3.
Rotational laxities of single bundle and double bundle ACL reconstructions
| Study | Loading condition | Flexion Angle (deg) |
Anterior/ Posterior Translation (Mean ± Standard Deviation [mm]) |
Internal/ External Rotation (Mean ± Standard Deviation [deg]) |
||
|---|---|---|---|---|---|---|
| SB | DB | SB | DB | |||
| Ferretti et al30 | Manual Internal/External load | 30° | × | × | 16.3 ± 5.4 (I) | 16.6 ± 3.8 (I) |
| 15.7 ± 4.3 (E) | 15.1 ± 2.4 (E) | |||||
| Ho et al25 | 10 N·m Internal torque | 30° | 6.9 ± 4.5 (A) | 8.8 ± 4.1 (A) | 24.1 ± 6.5 (I) | 24.8 ± 8.0 (I) |
| 60° | 4.7 ± 5.3 (A) | 4.5 ± 3.5 (A) | 18.6 ± 8.8 (I) | 18.5 ± 0.0 (I) | ||
| 10 N·m External torque | 30° | 0.1 ± 3.5 (P) | 0.9 ± 1.9 (P) | 17.5 ± 2.4 (E) | 16.3 ± 3.7 (E) | |
| 60° | 3.7 ± 2.8 (P) | 4.6 ± 2.9 (P) | 14.8 ± 2.3 (E) | 15.2 ± 5.7 (E) | ||
| Hofbauer et al31 | Manual Internal/External load | 30° | × | × | 20.3 ± 0.2 (I) | 12.3 ± 0.3a(I) |
| Markolf et al,36,‡ | Valgus moment (2.5 – 4.3 N·m)and Iliotibial band force (19.9 – 37.3 N) | 21° – 36° | 9.4 ± 6.3 (AP) | 6.8 ± 4.6a(AP) | 11.2 ± 5.2 (IE) | 11.1 ± 5.3 (IE) |
| Markolf et al22,‡ | 5 N·m Internal Torque | 0° | × | × | 11.5 ± NI (I) | 10.4 ± NI (I) |
| 15° | × | × | 20.4 ± NI (I) | 19.5 ± NI (I) | ||
| 30° | × | × | 25.1 ± NI (I) | 24.7 ± NI (I) | ||
| 60° | × | × | 30.1 ± NI (I) | 30.6 ± NI (I) | ||
| 90° | × | × | 33.2 ± NI (I) | 33.9 ± NI (I) | ||
| Seon et al27 | 5 N·m Internal and 10 N·m Valgus Tibial Torques | 0° | 2.0 ± 3.7 (A) | 0.6 ± 3.1a(A) | 12.7 ± 5.2 (I) | 9.9 ± 4.5a (I) |
| 30° | 3.1 ± 4.4 (A) | 1.4 ± 3.9a(A) | 19.1 ± 6.7 (I) | 18.2 ± 6.1 (I) | ||
| Song et al11 | Manual Internal/External load | 30° | × | × | 29.5 ± 3.8 (IE) | 23.3 ± 4.0a (IE) |
| Yagi et al26 | 5 N·m Internal and 10 N·m Valgus Tibial Torques | 15° | 8.5 ± 3.2 (A) | 6.1 ± 2.8a(A) | × | × |
| 30° | 9.5 ± 2.6 (A) | 7.5 ± 2.3 a(A) | × | × | ||
| Yamamoto et al28 | 5 N·m Internal and 10 N·m Valgus Tibial Torques | 15° | 4.8 ± 3.0 (A) | 4.8 ± 2.4 (A) | 15.6 ± 7.1 (I) | 16.0 ± 8.4 (I) |
| 30° | 6.5 ± 3.0 (A) | 6.7 ± 2.4 (A) | 19.1 ± 7.2 (I) | 19.4 ± 8.1 (I) | ||
A, Anterior translation; AP, Anterior-posterior translation; DB, Double bundle ACL reconstruction; E, External rotation; I, Internal rotation; IE, Internal-external rotation; NI, No information available; P, Posterior translation; SB, Single bundle ACL reconstruction;
P<0.05;significantly different from single bundle reconstruction.
Double bundle data is from protocol “DB1”
DISCUSSION
This study was undertaken to investigate if there is a consensus on the superiority of one reconstruction technique over the other among the biomechanical studies that compared the knee joint laxities following single bundle and double bundle ACL reconstructions. Meta-analysis of the ten included studies that reported anteroposterior laxity demonstrated no significant difference between the two treatment options for ACL injury at 0°, 30°, 60° and 90° of flexion. In regards to rotatory knee laxity, double bundle ACL reconstruction was reported to provide greater rotational stability than single bundle ACL reconstruction in four11,26,27,31 of the included studies and the remaining five22,25,28,30,36 studies could not find any significant advantage of one reconstruction technique over the other.
Our meta-analysis showed an overall mean difference between the two reconstructions ranging from 0.07 mm to 0.99 mm at 90° and 0° of flexion respectively with no statistical significant difference between the two treatments. Consistent with these findings, recently a meta-analysis of the clinical outcomes found that double bundle ACL reconstruction resulted in anterior stability closer to the intact knee by 0.52 mm compared to single bundle ACL reconstruction.13 While such differences in the biomechanical outcomes may have some clinical implications, currently the ability to detect these narrow differences accurately and reliably in the clinical setting is limited. There is a strong need for development of new tools that could accurately and reliably provide quantitative data in a clinical setting.
One of the main rationales for the introduction of double bundle ACL reconstruction was to address the persistent rotational instability of the knee after conventional surgical interventions.42 Currently the primary evaluation of rotational stability in clinical setting is performed by the pivot-shift examination. However, this physical examination has been criticized as being highly subjective in nature.17,43 Several confounding factors such as the concomitant soft tissue injuries, the amount of force used for the maneuver and patient guarding have been identified to hinder an accurate assessment of rotational stability using the pivot-shift examinations.43 Further, this examination is reported to have a high specificity (98%), but a low sensitivity (24%)1 and is prone to false positive result due to joint laxity in the absence of trauma.43 Even among the biomechanical studies that evaluated the rotational laxities, we noticed large variations in the experimental designs and the reported measurements. For example, various loading conditions such as manual internal/external torques, 10/5 N·m internal/external torques and combined valgus moment with iliotibiaFl band force have been used by different authors and they have reported the rotational laxity in terms of translations (anterior or anterior-posterior), rotations (Internal or external or internal-external) or both. Due to these variations we were unable to perform a meta-analysis on the rotational joint laxity.
A recent meta-analysis of clinical outcome studies could not find any statistically significant difference in the pivot-shift results between the two reconstruction techniques.13 Although, four of the nine biomechanical studies that reported rotational laxities found that a double bundle ACL reconstruction could resist rotational loads better than a single bundle ACL reconstruction, it is not feasible to draw any unbiased conclusions on the rotational stability provided by these two reconstruction techniques due to large variations that we observed between the studies. Kocher et al44 have found that the pivot-shift examination provides a better indication of the patients’ functional outcomes than the instrumented knee laxity or Lachman examination. Recently few authors have proposed innovative methods using open magnetic resonance imaging, computer navigation system and electromagnetic devices to quantitatively measure the rotational stability in a clinical setting.17,19,45 More emphasis needs to be placed on evaluating the applicability of such techniques as clinical tools to measure rotational stability quantitatively.
This study has certain limitations. We were unable to perform a quantitative meta-analysis of the rotational laxities among the biomechanical studies. While such an analysis could potentially answer an important question of whether a double bundle ACL reconstruction can restore the rotational stability better than a single bundle ACL reconstruction, there needs to be more investigations with a standardized measure to help better answer such a question. Since this is an analysis of only biomechanical studies which represent measurements at time-zero, we can not speculate on how the differences observed between the two techniques in this analysis may reflect in a clinical setting, nor hold up over time. Results of the meta-analysis are based on a relatively small sample size especially at 0° flexion. Most studies included in the analysis at this angle had a repeated measures design which have high precision even with a small sample size compared to independent group design. Finally, we did not take into account the various parameters of the reconstructions such as the graft fixation method, graft fixation angle and initial graft tensions as standard for these parameters is yet to be established.
More randomized controlled trials with accurate measurements of the outcomes need to be conducted which could play a significant role in confirming or refuting the superiority of a particular reconstruction over another. We hope that the readers of this article understand and appreciate the importance of the confounding factors and exercise greater caution while interpreting the published results of laboratory studies before they form the basis for any crucial clinical practice. Finally, it is imperative to emphasize the need for developing new tools that can accurately and reliably quantify clinical outcomes in conjunction with the current trend of proposing new and innovative surgical techniques.
CONCLUSION
Both single and double bundle treatment options for anterior cruciate ligament injury result in similar anteroposterior knee joint laxity at time-zero. No conclusive evidence on the superiority of one reconstruction technique over the other in terms of rotation laxity can be obtained due to several variations in the experimental protocol and the parameters used to measure the rotational laxity among the studies.
Acknowledgments
The authors gratefully acknowledge the support of the National Institutes of Health (R01AR055612). We thank Samuel K Van De Velde for his technical assistance.
Appendix
Four1–4 among the ten1–10 studies included in the meta-analysis had a paired study design where the efficacy of each treatment was investigated by use a robotic testing system in the same specimen. Paired analyses results for three of the four studies that used a paired design were not available. The standard deviation of the mean difference between the two treatments for these three studies was estimated by imputing the correlation coefficients (0.53, 0.38, 0.70, and 0.77 for 0°, 30°, 60° and 90° of flexion respectively) from Seon et al.2 study. A detailed description of the imputation procedure is given in Cochrane Handbook for Systematic Reviews of Interventions.11
When all the included studies were analyzed together, the overall mean differences calculated by the random effects model in the anteroposterior laxity between the single bundle and double bundle ACL reconstruction techniques were 1.11mm (95% CI: −0.08 to 2.30), 0.48mm (95% CI: −0.31 to 1.27), 0.65mm (95% CI: 0.15 to 1.15), 0.40mm (95% CI: −0.29 to 1.08), at 0°, 30°, 60° and 90° of flexion respectively. These differences were not statistically significant except at 60° of flexion. These results of the meta-analysis for 0°, 30°, 60° and 90° of flexion are presented in figures 1, 2, 3 and 4 respectively.
Figure 1.
Forest plot of anterior/ anteroposterior laxities of SB and DB ACL reconstructions at 0° of flexion. The mean difference in laxities for each study is represented by the square and its size represents the weight of the study; the horizontal line running through the square represents the 95% confidence interval; the overall estimate of the mean difference is represented as a diamond, with its horizontal tips representing the 95% confidence interval.
Figure 2.
Forest plot of anterior/ anteroposterior laxities of SB and DB ACL reconstructions at 30° of flexion. The mean difference in laxities for each study is represented by the square and its size represents the weight of the study; the horizontal line running through the square represents the 95% confidence interval; the overall estimate of the mean difference is represented as a diamond, with its horizontal tips representing the 95% confidence interval.
Figure 3.
Forest plot of anterior/ anteroposterior laxities of SB and DB ACL reconstructions at 60° of flexion. The mean difference in laxities for each study is represented by the square and its size represents the weight of the study; the horizontal line running through the square represents the 95% confidence interval; the overall estimate of the mean difference is represented as a diamond, with its horizontal tips representing the 95% confidence interval.
Figure 4.
Forest plot of anterior/ anteroposterior laxities of SB and DB ACL reconstructions at 90° of flexion. The mean difference in laxities for each study is represented by the square and its size represents the weight of the study; the horizontal line running through the square represents the 95% confidence interval; the overall estimate of the mean difference is represented as a diamond, with its horizontal tips representing the 95% confidence interval.
- 1.Mae T, Shino K, Miyama T, et al. Single-versus two-femoral socket anterior cruciate ligament reconstruction technique: Biomechanical analysis using a robotic simulator. Arthroscopy. 2001;17:708–716. doi: 10.1053/jars.2001.25250. [DOI] [PubMed] [Google Scholar]
- 2.Seon JK, Gadikota HR, Wu JL, Sutton KM, Gill TJ, Li G. Comparison of Single- and Double-Bundle Anterior Cruciate Ligament Reconstructions in Restoration of Knee Kinematics and Anterior Cruciate Ligament Forces. Am J Sports Med. 2010;38:1359–1367. doi: 10.1177/0363546510361494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:660–666. doi: 10.1177/03635465020300050501. [DOI] [PubMed] [Google Scholar]
- 4.Yamamoto Y, Hsu WH, Woo SL, Van Scyoc AH, Takakura Y, Debski RE. Knee stability and graft function after anterior cruciate ligament reconstruction: a comparison of a lateral and an anatomical femoral tunnel placement. Am J Sports Med. 2004;32:1825–1832. doi: 10.1177/0363546504263947. [DOI] [PubMed] [Google Scholar]
- 5.Albuquerque RF, Sasaki SU, Amatuzzi MM, Angelini FJ. Anterior cruciate ligament reconstruction with double bundle versus single bundle: experimental study. Clinics (Sao Paulo) 2007;62:335–344. doi: 10.1590/s1807-59322007000300020. [DOI] [PubMed] [Google Scholar]
- 6.Ferretti A, Monaco E, Labianca L, Conteduca F, De Carli A. Double-bundle anterior cruciate ligament reconstruction: a computer-assisted orthopaedic surgery study. Am J Sports Med. 2008;36:760–766. doi: 10.1177/0363546507305677. [DOI] [PubMed] [Google Scholar]
- 7.Ho JY, Gardiner A, Shah V, Steiner ME. Equal kinematics between central anatomic single-bundle and double-bundle anterior cruciate ligament reconstructions. Arthroscopy. 2009;25:464–472. doi: 10.1016/j.arthro.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 8.Hofbauer M, Valentin P, Kdolsky R, et al. Rotational and translational laxity after computer-navigated single- and double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18:1201–1207. doi: 10.1007/s00167-009-0992-9. [DOI] [PubMed] [Google Scholar]
- 9.Sbihi A, Franceschi JP, Christel P, Colombet P, Djian P, Bellier G. [Anterior cruciate ligament reconstruction: biomechanical comparison on cadaver specimens using a single or double hamstring technique] Rev Chir Orthop Reparatrice Appar Mot. 2004;90:643–650. doi: 10.1016/s0035-1040(04)70725-4. [DOI] [PubMed] [Google Scholar]
- 10.Song EK, Oh LS, Gill TJ, Li G, Gadikota HR, Seon JK. Prospective comparative study of anterior cruciate ligament reconstruction using the double-bundle and single-bundle techniques. Am J Sports Med. 2009;37:1705–1711. doi: 10.1177/0363546509333478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higgins JPT, Deeks JJ, Altman DG. Chapter 16: Special topics in statistics. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Chichester (UK): John Wiley & Sons; 2008. [Google Scholar]
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Spindler KP, Wright RW. Clinical practice. Anterior cruciate ligament tear. N Engl J Med. 2008;359:2135–2142. doi: 10.1056/NEJMcp0804745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Biau DJ, Tournoux C, Katsahian S, Schranz P, Nizard R. ACL reconstruction: a meta-analysis of functional scores. Clin Orthop Relat Res. 2007;458:180–187. doi: 10.1097/BLO.0b013e31803dcd6b. [DOI] [PubMed] [Google Scholar]
- 3.Liden M, Sernert N, Rostgard-Christensen L, Kartus C, Ejerhed L. Osteoarthritic changes after anterior cruciate ligament reconstruction using bone-patellar tendon-bone or hamstring tendon autografts: a retrospective, 7-year radiographic and clinical follow-up study. Arthroscopy. 2008;24:899–908. doi: 10.1016/j.arthro.2008.04.066. [DOI] [PubMed] [Google Scholar]
- 4.van der Hart CP, van den Bekerom MP, Patt TW. The occurrence of osteoarthritis at a minimum of ten years after reconstruction of the anterior cruciate ligament. J Orthop Surg. 2008;3:24. doi: 10.1186/1749-799X-3-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chouliaras V, Ristanis S, Moraiti C, Stergiou N, Georgoulis AD. Effectiveness of reconstruction of the anterior cruciate ligament with quadrupled hamstrings and bone-patellar tendon-bone autografts: an in vivo study comparing tibial internal-external rotation. Am J Sports Med. 2007;35:189–196. doi: 10.1177/0363546506296040. [DOI] [PubMed] [Google Scholar]
- 6.Ristanis S, Stergiou N, Patras K, Tsepis E, Moraiti C, Georgoulis AD. Follow-up evaluation 2 years after ACL reconstruction with bone-patellar tendon-bone graft shows that excessive tibial rotation persists. Clin J Sport Med. 2006;16:111–116. doi: 10.1097/00042752-200603000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Woo SL, Kanamori A, Zeminski J, Yagi M, Papageorgiou C, Fu FH. The effectiveness of reconstruction of the anterior cruciate ligament with hamstrings and patellar tendon. A cadaveric study comparing anterior tibial and rotational loads. J Bone Joint Surg Am. 2002;84-A:907–914. doi: 10.2106/00004623-200206000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Stergiou N, Ristanis S, Moraiti C, Georgoulis AD. Tibial rotation in anterior cruciate ligament (ACL)-deficient and ACL-reconstructed knees: a theoretical proposition for the development of osteoarthritis. Sports Med. 2007;37:601–613. doi: 10.2165/00007256-200737070-00004. [DOI] [PubMed] [Google Scholar]
- 9.Radford WJ, Amis AA. Biomechanics of a double prosthetic ligament in the anterior cruciate deficient knee. J Bone Joint Surg Br. 1990;72:1038–1043. doi: 10.1302/0301-620X.72B6.2147184. [DOI] [PubMed] [Google Scholar]
- 10.Crawford C, Nyland J, Landes S, et al. Anatomic double bundle ACL reconstruction: a literature review. Knee Surg Sports Traumatol Arthrosc. 2007;15:946–964. doi: 10.1007/s00167-007-0343-7. discussion 5. [DOI] [PubMed] [Google Scholar]
- 11.Song EK, Oh LS, Gill TJ, Li G, Gadikota HR, Seon JK. Prospective comparative study of anterior cruciate ligament reconstruction using the double-bundle and single-bundle techniques. Am J Sports Med. 2009;37:1705–1711. doi: 10.1177/0363546509333478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsuda E, Ishibashi Y, Fukuda A, Tsukada H, Toh S. Comparable results between lateralized single- and double-bundle ACL reconstructions. Clin Orthop Relat Res. 2009;467:1042–1055. doi: 10.1007/s11999-008-0604-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meredick RB, Vance KJ, Appleby D, Lubowitz JH. Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med. 2008;36:1414–1421. doi: 10.1177/0363546508317964. [DOI] [PubMed] [Google Scholar]
- 14.Irrgang JJ, Bost JE, Fu FH. Re: Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med. 2009;37:421–422. doi: 10.1177/0363546508327555. author reply 2. [DOI] [PubMed] [Google Scholar]
- 15.Pugh L, Mascarenhas R, Arneja S, Chin PY, Leith JM. Current concepts in instrumented knee-laxity testing. Am J Sports Med. 2009;37:199–210. doi: 10.1177/0363546508323746. [DOI] [PubMed] [Google Scholar]
- 16.Wiertsema SH, van Hooff HJ, Migchelsen LA, Steultjens MP. Reliability of the KT1000 arthrometer and the Lachman test in patients with an ACL rupture. Knee. 2008;15:107–110. doi: 10.1016/j.knee.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 17.Kubo S, Muratsu H, Yoshiya S, Mizuno K, Kurosaka M. Reliability and usefulness of a new in vivo measurement system of the pivot shift. Clin Orthop Relat Res. 2007;454:54–58. doi: 10.1097/BLO.0b013e31802b4a38. [DOI] [PubMed] [Google Scholar]
- 18.Jakob RP, Staubli HU, Deland JT. Grading the pivot shift. Objective tests with implications for treatment. J Bone Joint Surg Br. 1987;69:294–299. doi: 10.1302/0301-620X.69B2.3818763. [DOI] [PubMed] [Google Scholar]
- 19.Lane CG, Warren RF, Stanford FC, Kendoff D, Pearle AD. In vivo analysis of the pivot shift phenomenon during computer navigated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;16:487–492. doi: 10.1007/s00167-008-0504-3. [DOI] [PubMed] [Google Scholar]
- 20.Fujie H, Mabuchi K, Woo SL, Livesay GA, Arai S, Tsukamoto Y. The use of robotics technology to study human joint kinematics: a new methodology. J Biomech Eng. 1993;115:211–217. doi: 10.1115/1.2895477. [DOI] [PubMed] [Google Scholar]
- 21.Yoo JD, Papannagari R, Park SE, DeFrate LE, Gill TJ, Li G. The effect of anterior cruciate ligament reconstruction on knee joint kinematics under simulated muscle loads. Am J Sports Med. 2005;33:240–246. doi: 10.1177/0363546504267806. [DOI] [PubMed] [Google Scholar]
- 22.Markolf KL, Park S, Jackson SR, McAllister DR. Anterior-posterior and rotatory stability of single and double-bundle anterior cruciate ligament reconstructions. J Bone Joint Surg Am. 2009;91:107–118. doi: 10.2106/JBJS.G.01215. [DOI] [PubMed] [Google Scholar]
- 23.Sasaki SU, Mota e Albuquerque RF, Pereira CA, Gouveia GS, Vilela JC, Alcaras Fde L. An in vitro biomechanical comparison of anterior cruciate ligament reconstruction: single bundle versus anatomical double bundle techniques. Clinics (Sao Paulo) 2008;63:71–76. doi: 10.1590/s1807-59322008000100013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mae T, Shino K, Miyama T, et al. Single- versus two-femoral socket anterior cruciate ligament reconstruction technique: Biomechanical analysis using a robotic simulator. Arthroscopy. 2001;17:708–716. doi: 10.1053/jars.2001.25250. [DOI] [PubMed] [Google Scholar]
- 25.Ho JY, Gardiner A, Shah V, Steiner ME. Equal kinematics between central anatomic single-bundle and double-bundle anterior cruciate ligament reconstructions. Arthroscopy. 2009;25:464–472. doi: 10.1016/j.arthro.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 26.Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:660–666. doi: 10.1177/03635465020300050501. [DOI] [PubMed] [Google Scholar]
- 27.Seon JK, Gadikota HR, Wu JL, Sutton KM, Gill TJ, Li G. Comparison of Single- and Double-Bundle Anterior Cruciate Ligament Reconstructions in Restoration of Knee Kinematics and Anterior Cruciate Ligament Forces. Am J Sports Med. 2010;38:1359–1367. doi: 10.1177/0363546510361494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yamamoto Y, Hsu WH, Woo SL, Van Scyoc AH, Takakura Y, Debski RE. Knee stability and graft function after anterior cruciate ligament reconstruction: a comparison of a lateral and an anatomical femoral tunnel placement. Am J Sports Med. 2004;32:1825–1832. doi: 10.1177/0363546504263947. [DOI] [PubMed] [Google Scholar]
- 29.Albuquerque RF, Sasaki SU, Amatuzzi MM, Angelini FJ. Anterior cruciate ligament reconstruction with double bundle versus single bundle: experimental study. Clinics (Sao Paulo) 2007;62:335–344. doi: 10.1590/s1807-59322007000300020. [DOI] [PubMed] [Google Scholar]
- 30.Ferretti A, Monaco E, Labianca L, Conteduca F, De Carli A. Double-bundle anterior cruciate ligament reconstruction: a computer-assisted orthopaedic surgery study. Am J Sports Med. 2008;36:760–766. doi: 10.1177/0363546507305677. [DOI] [PubMed] [Google Scholar]
- 31.Hofbauer M, Valentin P, Kdolsky R, et al. Rotational and translational laxity after computer-navigated single- and double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18:1201–1207. doi: 10.1007/s00167-009-0992-9. [DOI] [PubMed] [Google Scholar]
- 32.Sbihi A, Franceschi JP, Christel P, Colombet P, Djian P, Bellier G. [Anterior cruciate ligament reconstruction: biomechanical comparison on cadaver specimens using a single or double hamstring technique] Rev Chir Orthop Reparatrice Appar Mot. 2004;90:643–650. doi: 10.1016/s0035-1040(04)70725-4. [DOI] [PubMed] [Google Scholar]
- 33.Review Manager (RevMan) [Computer program]. Version 5.0. Copenhagen: The Nordic Cochrane Centre TCC; 2008. [Google Scholar]
- 34.Ishibashi Y, Tsuda E, Fukuda A, Tsukada H, Toh S. Intraoperative biomechanical evaluation of anatomic anterior cruciate ligament reconstruction using a navigation system: comparison of hamstring tendon and bone-patellar tendon-bone graft. Am J Sports Med. 2008;36:1903–1912. doi: 10.1177/0363546508323245. [DOI] [PubMed] [Google Scholar]
- 35.Ishibashi Y, Tsuda E, Fukuda A, Tsukada H, Toh S. Stability evaluation of single-bundle and double-bundle reconstruction during navigated ACL reconstruction. Sports Med Arthrosc. 2008;16:77–83. doi: 10.1097/JSA.0b013e318172b52c. [DOI] [PubMed] [Google Scholar]
- 36.Markolf KL, Park S, Jackson SR, McAllister DR. Simulated pivot-shift testing with single and double-bundle anterior cruciate ligament reconstructions. J Bone Joint Surg Am. 2008;90:1681–1689. doi: 10.2106/JBJS.G.01272. [DOI] [PubMed] [Google Scholar]
- 37.Radford WJ, Amis AA, Kempson SA, Stead AC, Camburn M. A comparative study of single- and double-bundle ACL reconstructions in sheep. Knee Surg Sports Traumatol Arthrosc. 1994;2:94–99. doi: 10.1007/BF01476480. [DOI] [PubMed] [Google Scholar]
- 38.Seon JK, Park SJ, Lee KB, Yoon TR, Seo HY, Song EK. Stability comparison of anterior cruciate ligament between double- and single-bundle reconstructions. Int Orthop. 2009;33:425–429. doi: 10.1007/s00264-008-0530-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kanaya A, Ochi M, Deie M, Adachi N, Nishimori M, Nakamae A. Intraoperative evaluation of anteroposterior and rotational stabilities in anterior cruciate ligament reconstruction: lower femoral tunnel placed single-bundle versus double-bundle reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17:907–913. doi: 10.1007/s00167-009-0757-5. [DOI] [PubMed] [Google Scholar]
- 40.Monaco E, Labianca L, Conteduca F, De Carli A, Ferretti A. Double bundle or single bundle plus extraarticular tenodesis in ACL reconstruction? A CAOS study. Knee Surg Sports Traumatol Arthrosc. 2007;15:1168–1174. doi: 10.1007/s00167-007-0368-y. [DOI] [PubMed] [Google Scholar]
- 41.Tsai AG, Wijdicks CA, Walsh MP, Laprade RF. Comparative Kinematic Evaluation of All-Inside Single-Bundle and Double-Bundle Anterior Cruciate Ligament Reconstruction: A Biomechanical Study. Am J Sports Med. 2010;38:263–272. doi: 10.1177/0363546509348053. [DOI] [PubMed] [Google Scholar]
- 42.Steckel H, Starman JS, Baums MH, Klinger HM, Schultz W, Fu FH. The double-bundle technique for anterior cruciate ligament reconstruction: a systematic overview. Scand J Med Sci Sports. 2007;17:99–108. doi: 10.1111/j.1600-0838.2006.00600.x. [DOI] [PubMed] [Google Scholar]
- 43.Lane CG, Warren R, Pearle AD. The pivot shift. J Am Acad Orthop Surg. 2008;16:679–688. doi: 10.5435/00124635-200812000-00001. [DOI] [PubMed] [Google Scholar]
- 44.Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:629–634. doi: 10.1177/0363546503261722. [DOI] [PubMed] [Google Scholar]
- 45.Tashiro Y, Okazaki K, Miura H, et al. Quantitative assessment of rotatory instability after anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37:909–916. doi: 10.1177/0363546508330134. [DOI] [PubMed] [Google Scholar]