Abstract
Background:
Power lifting places the shoulder complex at risk for injury. Microfracture is a relatively new procedure for chondral defects of the glenohumeral joint and is not well described in the literature.
Objectives:
The purpose of this case report is to describe the post-operative rehabilitation used with a power lifter who underwent a microfracture procedure to address glenoid and humeral chondral defects, debridement of type I superior labral anterior-posterior lesion, and a subacromial decompression.
Case Description:
The patient was a 46 year-old male who was evaluated nine weeks status-post arthroscopic microfracture procedure for glenoid and humeral chondral defects, debridement of superior labral anterior-posterior (SLAP) lesion, and subacromial decompression. Rehabilitation consisted of postural education, manual therapy, rotator cuff and scapular strengthening, dynamic stabilization, weightbearing exercises, and weight training over nine weeks (24 sessions). Lifting modifications were addressed.
Outcomes:
Results of the QuickDASH indicate that activities of daily living (ADLs), work, and sports modules all improved significantly, and the patient was able to return to recreational power lifting with limited discomfort or restrictions.
Discussion:
A structured post-operative physical therapy treatment program allowed this patient to return to recreational power lifting while restoring independent function for work-related activities and ADLs.
Keywords: articular cartilage, microfracture, rehabilitation, shoulder
INTRODUCTION
Power lifting is recognized both nationally and internationally as a highly competitive sport where participants attempt to reach the highest one repetition maximum in a series of lifts including the deadlift, squat, and bench press. Athletes compete in classifications separated by age, weight, and gender.1,2 Current International Powerlifting Federation (IPF) men's records in the bench press, squat, and deadlifts surpass the lifter's body mass by three times, five times, and five times, respectively.1 These extremely high loads may place the lifter at risk for a host of injuries. Power lifting has been associated with more than 1 injury per year or 2.6-4 injuries per 1,000 hours of training.1,2 Not surprisingly, the most frequently injured body part in power lifters is the shoulder.1,2 Raske and Norlin2 found that 93% of shoulder injuries in power lifters lasted more then one month, suggesting these injuries commonly result in prolonged periods away from sport.
The term superior labral anterior-posterior (SLAP) lesion was coined in the early 1990s by Snyder.3 He categorized these lesions into four types based on involvement of the glenoid labrum and the tendon of the long head of the biceps. Type I lesions are classified as an intact labrum and biceps tendon with fraying of the superior labrum.3,4 This type of lesion is commonly degenerative, seen in patients that are middle-aged and elderly, and may or may not be symptomatic.4 Type I SLAP lesions may be treated with arthroscopic debridement, although this technique has not been shown to be effective in the long term.4
Arthroscopic subacromial decompression was first documented by Ellman.5 He stated that this procedure had the advantage over open decompression first described by Neer6 in that it spares the disruption and reattachment of the deltoid insertion. In the arthroscopic procedure, the coracoacromial ligament is released, the anterior acromion is resurfaced, osteophytic changes removed, and involved bursae are debrided.7 Arthroscopic procedures have primarily been used for subacromial impingement syndrome, partial tears of the supraspinatus tendon, and osteoarthritic changes seen in the acromioclavicular joint.8,9 Good to excellent results in function, return to work, pain, and ROM have been reported in 75-93% of subjects for those undergoing subacromial decompression for partial-thickness tears and impingement syndrome between the ages of 17 and the mid-60s.8,10,11
Articular cartilage defects can occur as a direct result from high impact loading, acute trauma, or repetitive compressive/torsional/shear loads placed on cartilaginous tissue,12,13 all of which place the athlete at risk for injury. Brittberg & Winalski14 have described the International Cartilage Repair Society's method of evaluating cartilage defects. These deficits are classified based on the depth and location of the area damaged, as shown in Table 1. This method has been most widely used in classifying chondral defects. Athletes at risk for glenohumeral cartilage damage are those involved with overhead activity, including weight lifters.15
Table 1.
Articular cartilage classification system.
| Grade I | Superficial lesions/cracks/indentations |
| Grade II | Lesions extending <50% in depth |
| Grade III | Lesions extending >50% in depth, not including subchondral bone |
| Grade IV | Extending into subchondral bone |
Higher grades indicate greater extent of depth in cartilage lesion.
Articular cartilage defects rarely heal spontaneously regardless of whether acute, chronic, or degenerative.12,13 The limited ability to heal is due to the avascular nature of cartilage16,17 and a lack of both chondrocyte division and migration to the injured site throughout the stages of healing.17 The articular cartilage lesion often leaves individuals with joint effusion, activity-related-pain, and reduced quality of life,16,17 and with regard to the athlete, decreased or inability to participate in sports. For the past 30 years, total shoulder arthroplasty and debridement techniques have been the treatment of choice for symptomatic articular deficits in the shoulder complex.15 Unfortunately, these techniques rarely result in the athlete returning to sport, even at a recreational level.
Cartilage restoration procedures that have emerged over the past two decades, along with an enhanced understanding of the structure and function of cartilage, has led to changes in surgical intervention for articular defects. These techniques attempt to retard the progression of the defect, relieve pain, maximize function, and return individuals to sport, in many cases at the professional level. One popular surgical technique that has recently been supported in the literature for the lower extremity, particularly in the tibiofemoral and patellofemoral joint, is the microfracture procedure. The goal of the microfracture procedure is the perforation of the subchondral bone in order to induce an associated bleeding response.12,13,16,17,19,20 This allows for the release of marrow elements including undifferentiated mesenchymal stem cells, fibroblasts, growth factors, and a host of inflammatory and chemotactic factors necessary for attempted repair and remodeling of the damaged area.12,13,15,16–18,20 A fibrin clot fills the breeched surface that provides an environment for differentiation into hyaline-like cells and stable tissue.12,13,15,16,18,20 This operative procedure has been performed in the hip,18 tibiofemoral and patellofemoral,16,19–22,23 and talocrural joints.24
The advantages of microfracture are that it is a relatively safe, straightforward procedure with low associated comorbidity, and should the procedure fail, other options can be implemented.16,22,23 The main disadvantage is that the resultant cartilage is hybrid of hyaline and fibrocartilage. Fibrocartilage has been shown to have inferior mechanical properties when compared to hyaline cartilage,20 in that it is less stiff12,13 and does not resist compression and shear loads as well.17 This may place the rejuvenated cartilage at risk for future breakdown. Various percentages of native hyaline and fibrocartilage have been found in both animal and human models at 12-72 months postoperatively in the tibiofemoral,21-2,26 glenohumeral,27 and carpal25–6 joint surfaces.
Some authors have advocated for a period of post-operative non-weightbearing for lesions that have been treated within the tibiofemoral/patellofemoral21,28, and talocrural joints.24 Others suggest partial weightbearing for the hip18,29 and tibiofemoral/patellofemoral joints16,19,20,22,23,30 for the first four to eight weeks post-operatively. This period of protective weight bearing is prescribed in order to protect the differentiating cartilage tissue. During this period, continuous passive motion (CPM) is typically used in the tibiofemoral,19,20,22,23 hip,18,29 and glenohumeral joints27 in order to enhance nutrient and metabolic activity in the articular cartilage and hypothetically push undifferentiated cells to become hyaline-like in nature.16 However, no functional differences were found between subjects who did or did not use CPM in smaller lesions (less than 2 cm2) in the knee.30
For patients who undergo the microfracture procedure for lesions of the tibiofemoral/patellofemoral,16,19,20,22,24,28 hip,18 and talocrural joints most authors advocate for a course of intensive physical therapy with a subsequent return to sport after four to six months.24 Unfortunately, there is no guarantee of return to prior level of performance. Mithoefer et al found that only 44% of subjects with tibiofemoral chondral defects returned to high-impact, pivoting sports such as football, soccer, basketball, skiing, tennis, and squash.23 Perhaps return to sport was initiated too soon, as Steadman et al report that maximum function is often not demonstrated until two to three years post-operatively.19 Subjects have been shown to return to recreational activity, such as tennis or jogging five days per week, and have sustained that level of participation at 4.2 to 11.3 year average follow-up.19,22,30 Individuals older than age 4030 and 4519 and those with lesions in the lower extremity of greater size than 2 cm230 have demonstrated poor outcomes. Cartilage defects of greater than 12 months23 in duration have also been implicated as a contributor to poorer outcomes, although conflicting evidence exists.19
In the glenohumeral joint, there is a paucity of published literature with regards to the use of microfracture technique for treatment of chondral defects. Well-defined rehabilitative protocols following microfracture procedure of this joint are limited. In a case series of five subjects, Siebold et al27 reported that after three weeks usage of a CPM, subjects were progressed to passive and active ROM until full range was achieved, upon which a rotator cuff strengthening program was initiated. All subjects noted positive results in ADLs, range of motion (ROM), and pain improvement. One high level swimmer was able to return to recreational swimming. However, a periosteal flap was used in addition to the microfracture procedure for the treatment of that athlete. In those with microfracture and periosteal transplantation, McCarthy and Cole31 noted that after six weeks of 600 pendulum exercises performed daily, patients are allowed to progress to AROM and are cleared for unrestricted activity at six months post-operatively.
The purpose of this case report is to describe the post-operative rehabilitation program that was individually designed for a former power lifter who underwent arthroscopy for a microfracture procedure to address glenoid and humeral chondral defects, concurrent with debridement of a SLAP lesion, and a subacromial decompression. The University of Illinois at Chicago Institutional Review Board approved of this study, and informed consent was obtained from the patient.
CASE DESCRIPTION
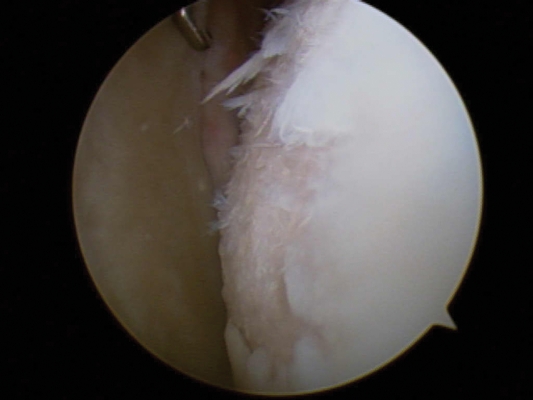
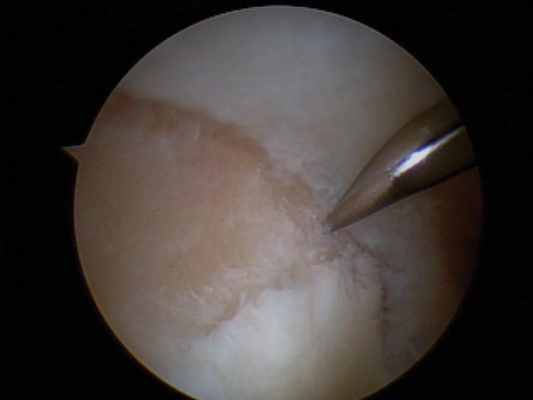
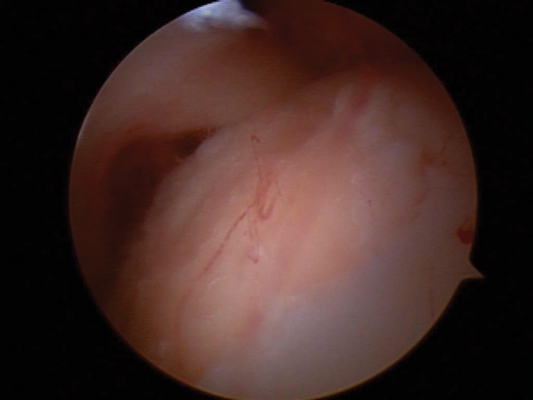
The patient was a 46-year-old, right hand dominant, Caucasian, mesomorphic male, 1.89 meters (74 inches) tall and weighing 151 kilograms (332 pounds). Approximately nine months prior to physical therapy initial evaluation, the patient was deadlifting 181.8 kilograms when he noted a diffuse yet intense pain in his right shoulder region. He continued to weight train for the next seven months, until the pain became unbearable. He decided to follow-up with his physician. Radiographs demonstrated a minimal degree of osetoarthritis in the glenohumeral joint and moderate degree of osteoarthritis in the acromioclavicular joint. Magnetic resonance imaging (MRI) revealed both a glenoid and a humeral cartilage lesion. His physician recommended arthroscopic evaluation and treatment. Arthroscopic surgery revealed a grade IV chondral lesions on the humeral head (Figure 1) and articulating surface of the superior glenoid rim (Figure 2), both of which were 2-3 cm in diameter, accompanied by a type I SLAP lesion. Microfracture procedure (Figure 3) was performed to both articulating surfaces of the glenohumeral joint, along with debridement of SLAP lesion and a subacromial decompression, the latter to ensure clearance of the subacromial space. His initial physical therapy visit occurred at the beginning of the ninth week post-arthroscopy.
Figure 1.
Humeral head cartilage lesion.
Figure 2.
Superior glenoid cartilage lesion.
Figure 3.
Status-post microfracture procedure to the humeral head. Note bleeding from subchondral bone.
At initial examination, the patient noted functional difficulty conducting his work-related activities as a gym owner, such as moving and cleaning weights. Because most of his destinations were within walking distance, he did not report driving as a limitation. Household activities, such as cleaning dishes, floors, and rugs were difficult to complete.
This patient's past medical history included right infraspinatus, supraspinatus, and pectoralis major partial-thickness muscle tears while conducting a bench press approximately six years prior. This injury was treated conservatively with a positive outcome, and the patient decided to discontinue competitive lifting, but continued to train recreationally. He noted that his ROM and strength were worse on the right side after this injury. Subjective reports of his maximum lifts prior to his present injury as well as those achieved post-operatively are described in Table 2. The patient stated that he no longer desired to reach his lifting maximums for fear of damage to his body. His goal was to continue lifting at least 50% of his previous maximum lifts.
Table 2.
Patient reported values for Lifts.
| Lifts Type | Max Prior to injury | Max Two years post-operatively |
|---|---|---|
| Squat | 530 lbs. ×10 | 400 lbs. 4×15 |
| Deadlift | 600 lbs. ×1 | 365 lbs. 4×15 |
| Bench Press | 240lbs. ×2 | 150 lbs. 4×15 |
INITIAL EXAMINATION
On initial physical therapy examination, the patient presented with forward shoulders bilaterally, downwardly rotated scapulae (right greater then left) and minimal levoscoliosis and kyphosis in the thoracic region. Atrophy was noted throughout the right shoulder musculature, including the trapezius, deltoid, supraspinatus, external rotators, latissimus dorsi, and pectoralis major, and the musculature of the upper brachium, including the biceps and triceps. The surgical sites were well healed without loss of sensation. Sensation to light touch was intact throughout the rest of the upper extremities.
ROM examination of the cervical spine, elbow, forearm, wrist and hand revealed no significant deficits. Table 3 denotes ROM values for the shoulder complex at initial examination and discharge. This patient was limited primarily by pain with all active and passive right shoulder movements. He was unable to don/doff a shirt with his right arm, nor was he able to reach behind his head or back.
Table 3.
Range of motion, measured in degrees.
| Shoulder ROM | Left at Initial Examination(AROM/PROM) | Right at Initial Examination(Passive only) | Right at Discharge(AROM/PROM) |
|---|---|---|---|
| Flexion | 172/178 | N/t | 169/175 |
| Extension | 76/92 | 50& | 71/85 |
| Abduction | 143 | 73& | 143 |
| Scaption | 180 | 130& | 180 |
| Internal Rotation | 66* | 38&, @ | 57* |
| External Rotation | 90* | 32&, @ | 88* |
%measured supine,
&empty end-feel,
*measured at 90 degrees abduction,
@ measured at 0 degrees abduction
Joint mobility examination revealed hypomobility of the sternoclavicular, acromioclavicular, and scapulothoracic joints, thereby diminishing scapular upward rotation bilaterally, although greater on the surgical side. Glenohumeral joint examination exhibited deficits in inferior and posterior translation without pain.
Force generation capacity was severely limited, and therefore, manual muscle testing (MMT) for the shoulder complex was not assessed at initial examination. Grip strength testing revealed 139 pounds on the right, as compared to 159 pounds on the left, measured via hand-held dynamometer.
The QuickDASH was used as the primary self-reported functional outcome measure. The QuickDASH, developed from the original 30-item Disabilities of Arm, Shoulder, and Hand (DASH) questionnaire, is an 11-item, self-administered questionnaire for upper extremity function and disability.32 Scores for each individual item range from 1 to 5, 1 being no difficulty, 5 being unable. The QuickDASH also has an optional five question module for both work and sports that are scored separately. For scoring, a sum of the responses is divided by the number of responses, subtracting one, and multiplying by 25 for all three modules separately. Scores range from 0 to 100, 0 indicating no disability. When compared to the 30-item DASH, Beaton et al33 reported a Pearson's product-moment coefficient of correlation of .97 (Pearson's r), with test-retest reliability of .94, and similar construct validity to the DASH. The advantages of the QuickDASH are its simplicity and ease of use.
QuickDASH scores were assessed prior to surgery and post-operatively. Table 4 presents the patient's QuickDASH scores, with the 11-item ADL measure worsening post-operatively from 40.9 to 81.8. The work module also increased from 56.25 to 75, while the sports module remained unchanged at 100. Given that the intrarater reliability coefficient is .94 with standard deviation of 26.2 points,32 the calculated standard error of measurement (SEM) of 1 standard deviation is 12.8 at a 95% confidence interval (CI), indicating that he was significantly worse at this point after surgery compared to pre-operative function.
Table 4.
Quick DASH scores.
| Quick DASH Scores | Pre-Surgical | Initial Evaluation | Discharge | 2 year post operatively |
|---|---|---|---|---|
| 11-item ADL | 40.9 | 81.8 | 15.9 | 4.5 |
| Work Module | 56.25 | 75 | 25 | 6.25 |
| Sports Module | 100 | 100 | 75 | 25 |
*Note: Higher scores indicate greater disability.
Intervention
Note: Please refer to Appendix 1 for all details of the three phases of intervention.
Phase I-Protective PROM Phase- Weeks 0-8 Post-operatively
For the first six weeks post-operatively, prior to physical therapy consultation, the patient was issued a CPM machine set at 90 degrees of abduction in the scapular plane and 90 degrees of external rotation by his physician. He used this daily for six hours. For the following two weeks, the patient was allowed to conduct self-PROM into flexion and scapular plane abduction in the supine position as tolerated, per physician instruction. He was then referred to physical therapy for therapeutic management.
Phase II- AROM and Strengthening Phase- Weeks 9-14 Post-operatively
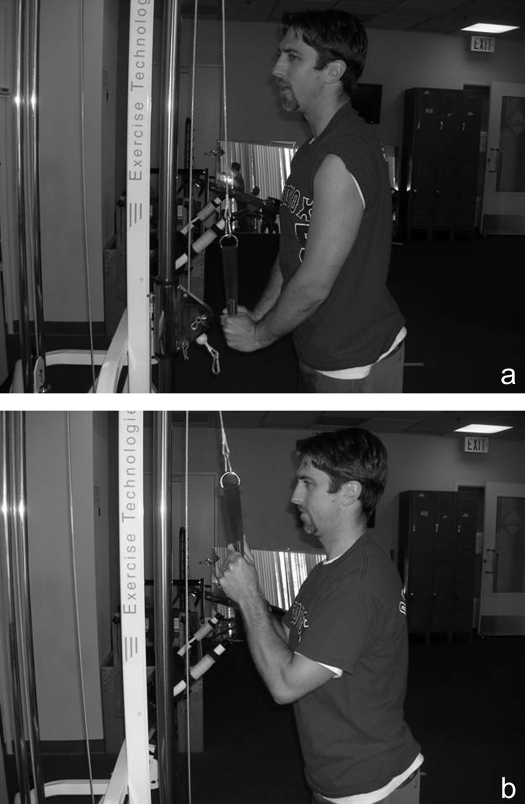
During the first six weeks of physical therapy (weeks 9-14 post-operatively), the treatment plan was designed to address postural dysfunction, normalize passive and active ROM on both sides, and strengthen the periscapular muscles, rotator cuff, and remaining limb musculature bilaterally. During week 9, the patient was educated regarding forward shoulder posture and how it has been linked to shoulder complex dysfunction and pain.33–5 Further, because thoracic position has been shown to have effects on shoulder ROM, kinematics, and strength,36 the patient was educated to avoid thoracic kyphosis or slumped posture. To address pain, grade I-II joint distraction was performed at the glenohumeral joint for pain modulation according to Kaltenborn.37 Pain-free right glenohumeral PROM was administered at every treatment session to enhance or maintain available ROM and nourish rejuvenating cartilaginous tissue. Supine AAROM and AROM exercises were added in multiple planes with a wand daily and were included in a home exercise routine. A rotator cuff strengthening program was conducted at home three days per week on non-consecutive days. Isometric exercise was issued for glenohumeral flexion, abduction, internal rotation (IR), external rotation (ER), and extension at varying angles within the patients available ROM. Each was conducted with 2 sets of 10 repetitions with 5-second holds and 5s rest breaks38 at maximal levels with 30 second rest breaks between sets. This was issued to prepare for a more complex exercise regime to come in later weeks. This time frame was promoted throughout all glenohumeral rotator cuff strengthening sessions to build muscular endurance, because muscle fatigue has been associated with faulty neuromuscular control.39–40 Standing bicep curls and tricep extensions (Figure 4) were progressed accordingly throughout physical therapy sessions. Forearm, wrist, and hand gripping exercises were also utilized throughout treatment sessions.
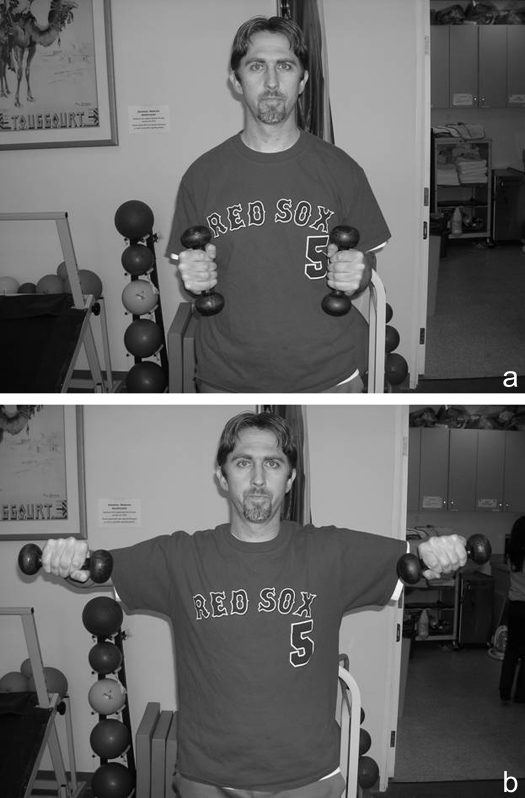
Figure 4.
Triceps extension.
4a. Initial and ending position. The patient stands with hands on handle bars, elbows in extension, shoulders neutral.
4b. Movement. The patient slowly allows the bar to be raised to 90 degrees of elbow flexion.
During this phase, the patient was allowed to begin squats and deadlifts with no external resistance in order to avoid significant atrophy of his lower extremities. Once the patient achieved supine glenohumeral AROM of flexion past 90 degrees, serratus anterior punches were added without external resistance. Resistance was progressed as the patient's strength increased.
During week 10, grade II-III mobilizations with both distraction and inferior/posterior glides were administered to address both pain and mobility,37sternoclavicular joint mobilizations, grade III-IV in a caudal direction, were conducted to improve scapular mobility.37 PROM into straight plane abduction and standing AAROM and AROM glenohumeral flexion and scapular plane abduction were added. Because the patient's girth did not allow for serratus anterior activity to be monitored with palpation while performing elevation, he was given verbal cues to utilize his serratus anterior while the primary author mobilized his scapula into upward rotation as needed throughout treatment, similar to the scapular assistance test described by Rabin et al.39 Inadequate scapulothoracic upward rotation has been linked to impingement.40 Standing rows with theraband were added to improve scapular strength.
At week 11, grade III-IV joint mobilizations of the glenohumeral joint were added to progress mobility.37 PROM into ER/IR at 90 degrees abduction was conducted. Isotonics began in the order of scaption, flexion, and abduction (Figure 5) to 90 degrees of elevation. Thirty second rest breaks between sets was issued in order to promote training of muscular endurance. The ultimate goal was to progress his scaption and flexion to three sets of 20 repetitions with five-pound dumbbells. The use of five pound weights with three sets of 20 repetitions in the shoulder has been used in the physical training of baseball positional players and pitchers.43 IR and ER at neutral abduction with 3 foot-long theraband was given. He was instructed to stand consistently 3 feet away from the door and place a towel roll between his humerus and body wall to avoid faulty compensations and optimize position of the rotator cuff.
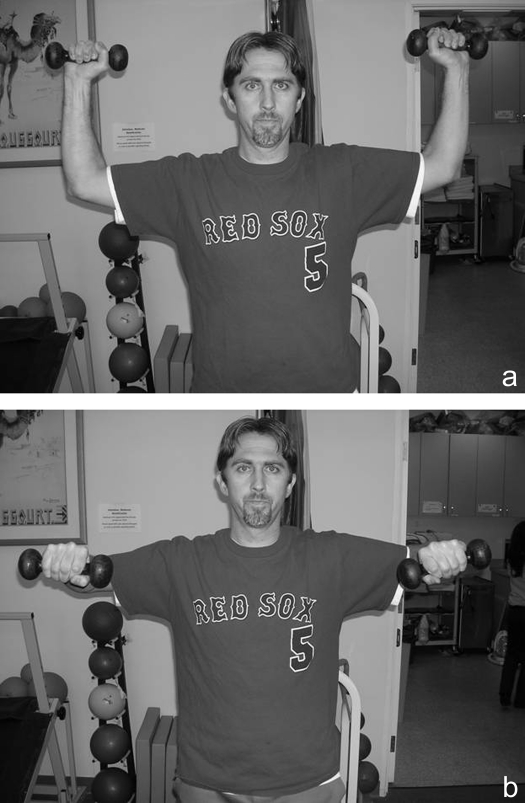
Figure 5.
Deltoid raises or “wings”.
5a. Initial and ending position. The patient stands with arms at side, elbows bent to 90 degrees of flexion.
5b. Movement. The patient raises shoulders to 90 degrees abduction.
During week 12, stretching with the hand behind head and back with a towel and pectoral stretches at 90 abduction and full available external rotation were added to address functional ROM. Grade III-IV postero-anterior joint mobilizations were performed later during rehabilitation as needed to the thoracic spine in accordance with Maitland's recommendations.44 Strength was progressed accordingly for all previously described exercises through week 14 with detail given in Appendix 1.
Phase III- Return to Sport Phase- Weeks 15-17 Post-operatively
At this point, the patient demonstrated a 4/5 on MMT into glenohumeral scaption, flexion, abduction, IR and ER (in neutral abduction), compared to the non-involved side. It was decided to use a 4/5 on MMT to all above stated shoulder actions, along with a six-week strengthening protocol, as markers to progress to this phase. 4/5 on MMT was chosen by the authors because it was deemed necessary to have at least moderate amounts of force generating capacity to maintain joint congruity at submaximal levels with higher level activity. Further, we elected to use six weeks, as this was thought to allow enough time to achieve hypertrophic strength gains and allowed for appropriate cartilage healing in the inherently unstable GH joint. During the return to sport phase, the main focus was to develop advanced strengthening, control, and introduce resistance to actions of the squat, deadlift, and bench press while continuing to maintain and improve available ROM through passive and active ROM and joint mobility as previously described. It was also critical that this patient be educated on proper weight lifting modifications. During week 15, isotonic exercise at or above 90 degrees of shoulder elevation such as ER at 90 degrees of glenohumeral abduction (scarecrows) were added to enhance rotator cuff strength and stability in an upper extremity position similar to squats (Figure 6). To address dynamic stability and improve joint position sense,45–47 Body Blade™ exercise drills were utilized in the clinic, with the patient standing and moving through multiple planes of ROM. This was continued until discharge. Pushups on the wall using various stable and unstable surfaces were incorporated to strengthen the rotator cuff and scapular stabilizers in a closed kinetic chain manner.48
Figure 6.
Standing External Rotation or “Scarecrows”
6a. Initial and ending position. The patient stands upright, with the glenohumeral joint placed in 90 degrees abduction and full external rotation, elbows in 90 degrees flexion, and forearms slightly pronated.
6b. Movement. The patient eccentrically lowers the forearms to neutral rotation with maintenance of all other joint angles.
At week 16, resistance was added to both the squat and deadlift. For the deadlift, the patient was instructed to concentrate on maximally contracting the lower extremities while using an underhand grip for the right hand during the deadlift (Figure 7) to avoid placing maximal stretch on the biceps muscle and tendon. Vertical pushups against the wall were progressed to an unstable surface for the upper extremities. The bench press was reintroduced at week 17. For the bench press, the patient was instructed to start with a ten-pound dumbbell in his involved arm with a spotter. He was allowed to progress by no more then five pounds per week. He also was educated to initiate barbell bench press when he was able to lift 50% of what he was lifting previously with dumbbells, in accordance with his goals. This was discussed to avoid compensating with his non-involved arm. Further, it was recommended to avoid excessive abduction and to maintain hand width no greater then 1.5x the biacromial width to avoid excessive strain on the rotator cuff.49 The patient was instructed to conduct lateral pull downs with his hands and elbows placed in front of his head. This avoids excessive shearing stress on the biceps long head tendon4 when the glenohumeral joint is at end-range external rotation at 90 degrees of abduction17 and also allows performance of the maneuver with the humerus in the scapular plane.
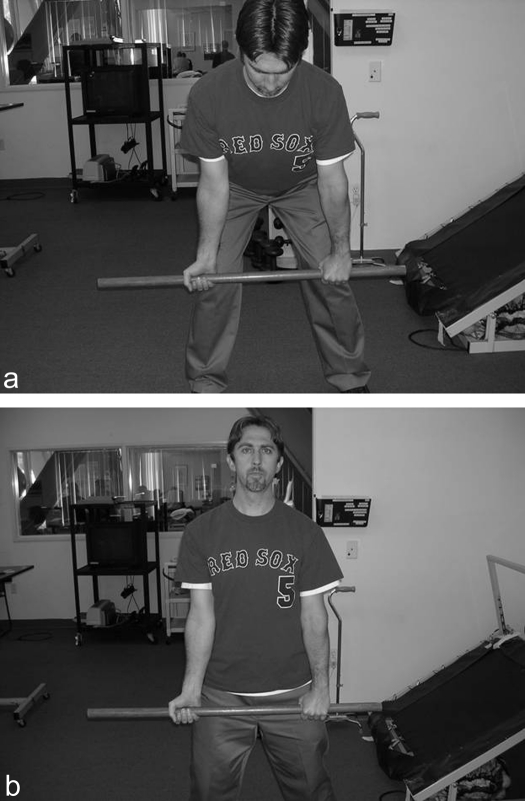
Figure 7.
Underhand deadlift.
7a. Initial and ending position. The patient stands with hips, knees, and ankles bent, involved wrist in supination to decrease maximal stretch on the biceps muscle and tendon.
7b. Movement. The patient raises the bar, extending with lower extremities and spine, to achieve upright posture.
OUTCOME
The patient was seen 24 times over a nine-week period. He was discharged from physical therapy services at week 17 post-operatively. Both the patient and the primary author were in agreement that he reached his goals, other than his lifting targets, which could be safely progressed by him while applying the technique modifications to which he had been educated. His ROM had plateaued, but was comparable to the non-involved side (Refer back to Table 3). He was independent with his HEP progression, was able to work and perform his ADLs independently, and understood how his posture could relate to shoulder dysfunction. Finally, QuickDASH scores showed improvements beyond the standard error of measurement. The patient made large gains in the ADL section, improving from 81.8 at initial evaluation to 15.9 at discharge. The work-related module changed from 75 to 31.25. Sports module improved only from 100 to 75. This section of the QuickDASH was unlikely to change remarkably at this point in time seeing that he had just begun his return to power lifting maneuvers with external resistance including squats, deadlifts, and bench press, and that he did not want to return to lifting at 100% of his previous maximum lifts. However, it was expected that because foundational strength was developed and proper education in progression in HEP was provided to the patient, it was likely that his scores in all modules would continue to improve over the next 12-18 months.
At a two year follow-up, QuickDASH scores continued to show improvement, mostly in the sport module from 75 to 25, followed by work module (31.25 to 6.25) and ADLs (15.9 to 4.5), as seen in Table 4. The patient reported that he was bench pressing 150 pounds, squatting over 400 pounds, and deadlifting 365 pounds at four sets of 15 repetitions each as noted in Table 2. He felt that although he could lift more, he was unwilling to attempt to do so for fear of reinjuring his right shoulder, or any part of his body. Although he did complain of minimal intermittent right shoulder stiffness deep in his glenohumeral joint the patient was very satisfied with overall results.
DISCUSSION
Chondral defects occur in response to macrotrauma or microtrauma inflicted upon articular cartilage and rarely heal on their own.12,13 While joint replacement has been the treatment of choice for articular cartilage deficits in the glenohumeral joint, it often leaves the patient unable to return to desired levels of function. In the case of athletes, return to recreational sports is difficult to accomplish after total joint arthroplasty of the glenohumeral joint. Articular cartilage techniques such as the microfracture procedure, which stimulates subchondral bone and may provide the potential for articular cartilage healing,13,16–20 offer the athlete a chance to return to sport at the recreational level and beyond.11,16,18–20,22–24,30
While post-operative rehabilitation following microfracture for the hip,18,29, tibiofemoral and patellofemoral,16,19–23,30 and talocrural joints24 have been defined, details regarding rehabilitation of the glenohumeral joint after microfracture procedures are lacking in the literature. The purpose of this case report was to describe the post-operative rehabilitation for a former power lifter who underwent an arthroscopic shoulder surgery for microfracture procedures of the glenohumeral joint, debridement of a type I SLAP lesion, and a subacromial decompression.
With regards to microfracture procedures performed in the tibiofemoral joint, patients older then 4030 and 4523 and those with lesion size greater then 2 cm223 have demonstrated poorer outcomes compared to those who are younger and have smaller lesions. Despite being older then 45 and having a lesion size greater then 2 cm2, this patient returned to recreational lifting, showed improvement on QuickDASH scores, and was satisfied with results at two-year follow up. Reinold et al reports a slower progression in patients with greater lesion sizes following microfracture procedure.50 It is possible that a rehabilitation program that advances slowly is more appropriate for those older then 40 years of age and/or with larger lesion sizes, and relate to why a successful outcome was achieved with this patient. Further, an accelerated progression was unnecessary as this patient was not interested in returning to a competitive sport that had a timeframe associated with return.
This patient was referred to physical therapy after eight weeks of CPM and self-induced PROM following arthroscopic microfracture procedures along with subacromial decompression and debridement of type I SLAP lesion. Placing initial AROM restrictions may have aided in avoiding movements that place the developing cartilage at risk. Frisbie et al26 states that hyaline-like cartilage was not found until eight weeks in the equine model. However, avoiding motion activates resorption of chondral surfaces51 and can likely weaken supporting joint musculature while causing joint restrictions and pain. The authors of this case report chose to err on the conservative side in order to ensure that abnormal forces were not placed across healing articular cartilage tissue. Future research should focus on whether early AROM places inappropriate torque or shear forces across the glenohumeral joint after chondral repair.
Some authors advocate for early post-operative weightbearing following microfracture procedure at the hip18,29 and tibiofemoral/patellofemoral16,19,20,22,23,30 joints. While it may be advantageous for early joint loading in to occur in the more stable hip and knee joints, compressive and shear forces placed on the less stable glenohumeral joint during UE CKC exercises may predispose it to injury. The authors chose to hold off on weight-bearing (CKC) activities in this patient until adequate strength (4/5 on MMT) was found on physical examination. It should be noted that the baseline strength in a power lifter is unlikely to be similar to the average person. A 4/5 on MMT, as used in this case report as a measure for progression to a more difficult regime, may not be applicable in other populations. In future research it may be interesting to study the effects of earlier compressive loading in the glenohumeral joint following cartilage repair procedures. As cartilage is designed to protect against compressive forces, loading mesenchymal cells into compression in the early stages may assist in differentiation into chondrocytes.
This power lifter, despite being trained in proper lifting modifications after injury, was not being seen by the physical therapist while he independently progressed his bench, squat, and deadlift. Once a baseline strength and stability was developed for the shoulder, and the patient was educated in proper technique with lifting maneuvers, it seemed feasible to allow for early discharge. Familiarity with lifting routine prior to injury allowed the patient to progress independently and appropriately. In this patient, the primary author felt it unlikely that this lifter would resume training too rapidly because the patient stated he was not interested in returning. However, early discharge may not necessarily be an optimal strategy for more competitive athletes who may rush or resume training too quickly or intensely.
CONCLUSION
In conclusion, this patient who underwent an arthroscopic glenohumeral microfracture procedures, subacromial decompression, and debridement of type I SLAP lesion effectively returned to a recreational weight lifting. He returned to this level of participation with the guidelines outlined in the protocol described in this case report. The protocol utilized with this patient and the outcomes achieved can not be generalized to other patients who undergo microfracture procedures about the glenohumeral joint and should only be used as a guideline. Controlled research using a larger sample size would help to determine if a protocol such as the one used in this case report would be successful with a larger group of athletes. Thus, additional research should focus on developing optimal post-operative rehabilitation for a quick and safe return to activities of daily living and sport after microfracture of chondral surfaces in the glenohumeral joint. Research should examine whether the microfracture technique for the glenohumeral joint is a viable surgical option for patients with articular cartilage injuries that wish to return to sport. Finally, studies that describe patient categorization, classification, and clinical prediction rules identifying those who would benefit from microfracture procedure in the glenohumeral joint would also be beneficial.
Appendix 1.
Post-operative rehabilitation following arthroscopic microfracture procedure with concominant debridement of SLAP type I lesion and subacromial decompression.
| I. Phase 1: protective PROM phase (day 1 post-arthroscopy-week 8) |
| Goals: |
| A. Protect surgical site from undue stress |
| B. Nourish articular cartilage to mold into appropriate tissue |
| C. Prevent negative effects of immobilization |
| D. Decrease pain and inflammation |
| Weeks 1-6 |
| 1. CPM at 90 degrees scaption, 90 degrees ER, 6H daily |
| 2. Cryotherapy as needed |
| Week 7-8 |
| 1. Self-PROM into flexion/scaption |
| 2. Cryotherapy as needed |
| II. Phase 2: AROM and strengthening phase (Week 9-14) |
| Goals: |
| A. Restore full ROM |
| B. Preserve integrity of tissue |
| C. Restore muscular strength and endurance |
| Week 9 |
| 1. Education regarding posture, cryotherapy |
| 2. PROM into glenohumeral flexion, scaption, extension, and external rotation (ER)/internal rotation (IR) in scapular plane |
| 3. Glenohumeral joint mobilizations, grade I-II for pain |
| 4. AAROM/AROM supine into glenohumeral flexion, scaption, ER/IR in scapular plane and neutral abduction |
| 5. Home exercise program (HEP) |
| a. Wand exercises in scaption, flexion, ER/IR in neutral abduction, lOxlOs holds, 5x/day |
| b. Squats, deadlifts with no external resistance |
| c. Isometrics in glenohumeral flexion, abduction, ER/IR in neutral abduction, 2x10 reps, 5s holds, lx/day, 5x/week |
| d. Forearm, wrist, hand-gripping exercises |
| e. Serratus anterior punches supine, 2x10-20 repetitions without external resistance, conducted lx/day, 5x/week |
| f. Tricep extensions/unilateral bicep curls standing, 2x20 repetitions, 5 pounds, 3x/week on non-consecutive days |
| Week 10 |
| 1. Progress PROM adding abduction |
| 2. Joint mobilizations |
| a. ternoclavicular joint, into both superior and inferior direction, grade 11I-1V |
| b. Scapulothoracic joint, into upward rotation, grade TII-IV |
| c. umeral joint, into posterior and inferior direction, grade 11-111 |
| 3. AAROM and AROM- glenohumeral flexion and scaption standing |
| 4. HEP |
| a. Wand exercises continued from week 9 |
| b. Squats, deadlifts with no external resistance continued from week 9 |
| c. Glenohumeral isometrics continued from week 9 |
| d. Forearm, wrist, hand-gripping exercises continued from week 9 |
| e. Increase serratus anterior punches to 1-2 pounds |
| f. Increase bicep/tricep exercises to 10 pounds |
| g. Standing rows with theraband, 2x20 repetitions, 3x/week on non-consecutive days |
| Week 11 |
| 1. Progress PROM adding ER/IR stretching at 90 degrees abduction |
| 2. Joint mobilizations- add grade III-IV to glenohumeral joint, same direction as week 10 |
| 3. AROM glenohumeral scaption and flexion continued from week 10 |
| 4. HEP |
| a. Wand exercises continued from week 9 |
| b. Squats, deadlifts with no external resistance continued from week 9 |
| c. Forearm, wrist, hand-gripping exercises continued from week 9 |
| d. Isotonic strengthening for glenohumeral joint, 2x20 repetitions, 3x/week, on non-consecutive days |
| i. Flexion and scaption standing with 1 pound |
| ii. Deltoid wings with 1 -2 pounds |
| iii IR/ER with theraband at neutral abduction |
| e. Increase serratus anterior punches to 3 pounds |
| f. Increase bicep/tricep exercises to 12 pounds |
| g. Standing rows with theraband continued from week 10 |
| Week 12 |
| 1. Progress PROM- add towel stretching behind head and back, wall pectoral stretch at 90 degrees abduction, 10x10 seconds 2-3x/day each, 5x/week |
| 2. Joint mobilizations- add thoracic spine mobilizations, into anterior direction, and continue with GH joint mobilizations from week 11 |
| 3. AROM glenohumeral scaption and flexion continued from week 10 |
| 4. HEP |
| a. Wand exercises continued from week 9 |
| b. Squats, deadlifts with no external resistance continued from week 9 |
| c. Forearm, wrist, hand-gripping exercises continued from week 9 |
| d. Isotonic strengthening- glenohumeral joint |
| i. Increase flexion and scaption to 2 pounds |
| ii. Increase deltoid wings to 3 pounds |
| iii. Increase IR/ER with theraband |
| e. Increase serratus anterior punches to 4 pounds |
| f. Increase biceps/triceps exercises to 15 pounds |
| g. Increase standing rows resistance with theraband |
| Week 13 |
| 1. Progress PROM |
| 2. Joint mobilizations- continue from week 12 |
| 3. AROM glenohumeral scaption and flexion continued from week 9 |
| 4. HEP |
| a. Wand exercises continued from week 9 |
| b. Squats, deadlifts with no external resistance continued from week 9 |
| c. Forearm, wrist, hand-gripping exercises continued from week 9 |
| d. Isotonic strengthening- glenohumeral joint |
| i. Increase flexion and scaption to 3-4 pounds |
| ii. Increase deltoid wings to 4 pounds |
| iii. Continue with therabands for IR/ER |
| e. Serratus anterior punches continued from week 12 |
| f. Increase biceps/triceps exercises to 20 pounds |
| g. Standing rows continue from week 12 |
| Week 14 |
| 1. Progress PROM |
| 2. Joint mobilizations continued from week 12 |
| 3. AROM glenohumeral scaption and flexion continued from week 10 |
| 4. HEP |
| a. Wand exercises continued from week 9 |
| b. Squats, deadlifts with no external resistance continued from week 9 |
| c. Forearm, wrist, hand-gripping exercises continued from week 9 |
| d. Isotonic strengthening- glenohumeral joint |
| i. Increase flexion and scaption to 5 pounds |
| ii. Increase deltoid wings to 5 pounds |
| iii. Increase IR/ER with theraband |
| e. Increase serratus anterior punches to 5 pounds |
| f. Biceps/triceps exercises continued from week 13 |
| g. Standing rows continued from week 13 |
| III. Phase 3: Return to recreational lifting/sport phase (Week 15-) |
| Goals: |
| A. Maintain full ROM |
| B. Improve muscular strength, endurance, and stability |
| C. Gradually return to power lifting tasks |
| Week 15 |
| 1. PROM |
| 2. joint mobilizations as needed, continued from week 12 |
| 3. AROM glenohumeral scaption and flexion continued from week 10 |
| 4. HEP |
| a. Wand exercises continued from week 9 |
| b. Squats, deadlifts with no external resistance continued from week 9 |
| c. Forearm, wrist, hand-gripping exercises continued from week 9 |
| d. Wall pushups, 2x20, on stable surface, 3x/week, on non-consecutive days |
| e. Body Blade exercise through full scaption ROM, 3x/week, on non-consecutive days 20x |
| f. Isotonic strengthening- glenohumeral joint |
| i. Flexion/scaption continued from week 14 |
| ii. Deltoid wings continued from week 14 |
| iii. IR/ER with theraband continued from week 14 |
| iv. Scarecrows, 1 -2 pounds, 2x20 |
| g. Serratus anterior punches continued from week 14 |
| h. Increase biceps/triceps exercises to 25 pounds |
| i. Add unilateral bent over rows, 20 pounds, 2x20 repetitions, 3x/week, on non-consecutive days |
| Week 16 |
| 1. PROM |
| 2. Joint mobilizations as needed, continued from week 12 |
| 3. AROM glenohumeral scaption and flexion continued from week 10 |
| 4. HEP |
| a. Wand exercises continued from week 9 |
| b. Forearm, wrist, hand-gripping exercises continued from week 9 |
| c. Wall pushups, 2x20, on unstable surface, 3x/week, on non-consecutive days |
| d. Body Blade exercises continued from week 15 |
| e. Dead lifts, 60 pounds, 2x20, 3x/week, on non-consecutive days |
| f. Squats, 95 pounds, 2x20, 3x/week, on non-consecutive days |
| g. Isotonic strengthening- glenohumeral joint |
| i. Flexion/scaption continued from week 14 |
| ii. Deltoid wings continued from week 14 |
| iii. IR/ER with theraband continued from week 14 |
| iv. Increase scarecrows to 3-4 pounds |
| h. Serratus anterior punches continued from week 14 |
| i. Increase biceps/triceps exercises to 30 pounds |
| j. Increase bent over rows to 25 pounds |
| Week 17 |
| 1. PROM |
| 2. Joint mobilizations as needed, continued from week 12 |
| 3. AROM glenohumeral scaption/flexion continued from week 10 |
| 4. HEP |
| a. Wand exercises continued from week 9 |
| b. Forearm, wrist, hand-gripping exercises continued from week 9 |
| c. Add dumbbell bench press, starting with 10 pounds unilaterally |
| d. Body Blade exercises continued from week 15 |
| e. Increase deadlifts to 70 pounds |
| f. Increase squats to 135 pounds |
| g. Isotonic strengthening- glenohumeral joint |
| i. Flexion/scaption continued from week 14 |
| ii. Deltoid wings continued from week 14 |
| iii. IR/ER with theraband continued from week 14 |
| iv. Increase scarecrows to 5 pounds |
| h. Serratus anterior punches continued from week 14 |
| i. Biceps/triceps exercises continued from week 16 |
| j. Increase bent over rows to 30 pounds |
REFERENCES
- 1. Keogh J, Hume PA, Pearson S. Retrospective injury epidemiology of one hundred one competitive Oceania power lifters: The effects of age, body mass, competitive standard, and gender. J Strength Cond Res. 2006;20:672–81 [DOI] [PubMed] [Google Scholar]
- 2. Raske A, Norlin R. Injury incidence and prevalence among elite weight and power lifters. Am J Sports Med. 2002;30:248–56 [DOI] [PubMed] [Google Scholar]
- 3. Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthroscopy. 1990;6:274–9 [DOI] [PubMed] [Google Scholar]
- 4. Wilk KE, Reinold MM, Dugas JR, et al. Current concepts in the recognition and treatment of superior labral (SLAP) lesions. J Orthop Sports Phys Ther. 2005;35:273–91 [DOI] [PubMed] [Google Scholar]
- 5. Ellman H. Arthroscopic subacromial decompression: Analysis of one- to three-year results. Arthroscopy. 1987;3:173–81 [DOI] [PubMed] [Google Scholar]
- 6. Neer CS., 2nd Anterior acromioplasty for the chronic impingement syndrome in the shoulder. 1972. J Bone Joint Surg Am. 2005;87:1399. [DOI] [PubMed] [Google Scholar]
- 7. Hawkins RJ, Plancher KD, Saddemi SR, et al. Arthroscopic subacromial decompression. J Shoulder Elbow Surg. 2001;10:225–30 [DOI] [PubMed] [Google Scholar]
- 8. Anderson NH, Sojbjerg JO, Johannsen HV, et al. Self-training versus physiotherapist-supervised rehabilitation of the shoulder in patients treated with arthroscopic subacromial decompression: a clinical randomized study. J Shoulder Elbow Surg. 1999;8:99–101 [DOI] [PubMed] [Google Scholar]
- 9. Prescher A. Anatomical basics, variations, and degenerative changes of the shoulder joint and shoulder girdle. Eur J Radiol. 2000;35:88–102 [DOI] [PubMed] [Google Scholar]
- 10. Ellman H, Kay SP. Arthroscopic subacromial decompression for chronic impingement. Two- to five-year results. J Bone Joint Surg Br. 1991;73:395–8 [DOI] [PubMed] [Google Scholar]
- 11. Roye RP, Grana WA, Yates CK. Arthroscopic subacromial decompression: two- to seven-year follow-up. Arthroscopy. 1995;11:301–6 [DOI] [PubMed] [Google Scholar]
- 12. Buckwalter JA. Articular cartilage injuries. Clin Orthop Relat Res. 2002;402:21–37 [DOI] [PubMed] [Google Scholar]
- 13. Buckwalter JA. Articular cartilage: Injuries and potential for healing. J Orthop Sports Phys Ther. 1998;28:192–202 [DOI] [PubMed] [Google Scholar]
- 14. Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85-A Suppl 2:58–69 [DOI] [PubMed] [Google Scholar]
- 15. Bishop JY, Flatow EL. Management of glenohumeral arthritis: A role for arthroscopy? Orthop Clin North Am. 2003;34:559–66 [DOI] [PubMed] [Google Scholar]
- 16. Gill TJ, Asnis PD, Berkson EM. The treatment of articular cartilage defects using the microfracture technique. J Orthop Sports Phys Ther. 2006;36:728–738 [DOI] [PubMed] [Google Scholar]
- 17. Lewis PB, McCarty LP, 3rd, Kang RW, et al. Basic science and treatment options for articular cartilage injuries. J Orthop Sports Phys Ther. 2006;36:717–27 [DOI] [PubMed] [Google Scholar]
- 18. Crawford K, Philippon MJ, Sekiya JK, et al. Microfracture of the hip in athletes. Clin Sports Med. 2006;25:327–35 [DOI] [PubMed] [Google Scholar]
- 19. Steadman JR, Briggs KK, Rodrigo JJ, et al. Outcomes of microfracture for traumatic chondral defects of the knee: Average 11-year follow-up. Arthroscopy. 2003;19:477–84 [DOI] [PubMed] [Google Scholar]
- 20. Steadman JR, Rodkey WG, Rodrigo JJ. Microfracture: Surgical technique and rehabilitation to treat chondral defects. Clin Orthop Relat Res. 2001;391:S362–9 [DOI] [PubMed] [Google Scholar]
- 21. Bae DK, Yoon KH, Song SJ. Cartilage healing after microfracture in osteoarthritic knees. Arthroscopy. 2006;22:367–74 [DOI] [PubMed] [Google Scholar]
- 22. Gobbi A, Nunag P, Malinowski K. Treatment of full thickness chondral lesions of the knee with microfracture in a group of athletes. Knee Surg Sports Traumatol Arthrosc. 2005;13:213–21 [DOI] [PubMed] [Google Scholar]
- 23. Mithoefer K, Williams RJ, 3rd, Warren RF, et al. High-impact athletics after knee articular cartilage repair: A prospective evaluation of the microfracture technique. Am J Sports Med. 2006:34:1413–8 [DOI] [PubMed] [Google Scholar]
- 24. Gobbi A, Francisco RA, Lubowitz JH, et al. Osteochondral lesions of the talus: Randomized controlled trial comparing chondroplasty, microfracture, and osteochondral autograft transplantation. Arthroscopy. 2006;22:1085–92 [DOI] [PubMed] [Google Scholar]
- 25. Frisbie DD, Oxford JT, Southwood L, et al. Early events in cartilage repair after subchondral bone microfracture. Clin Orthop Relat Res. 2003;407:215–27 [DOI] [PubMed] [Google Scholar]
- 26. Frisbie DD, Trotter GW, Powers BE, et al. Arthroscopic subchondral bone plate microfracture technique augments healing of large chondral defects in the radial carpal bone and medial femoral condyle of horses. Vet Surg. 1999;28:242–55 [DOI] [PubMed] [Google Scholar]
- 27. Siebold R, Lichtenberg S, Habermeyer P. Combination of microfracture and periostal-flap for the treatment of focal full thickness articular cartilage lesions of the shoulder: A prospective study. Knee Surg Sports Traumatol Arthrosc. 2003;11:183–9 [DOI] [PubMed] [Google Scholar]
- 28. Sledge SL. Microfracture techniques in the treatment of osteochondral injuries. Clin Sports Med. 2001;20:365–77 [DOI] [PubMed] [Google Scholar]
- 29. Enseki KR, Martin RL, Draovitch P, et al. The hip joint: Arthroscopic procedures and postoperative rehabilitation. J Orthop Sports Phys Ther. 2006;36:516–25 [DOI] [PubMed] [Google Scholar]
- 30. Marder RA, Hopkins G, Jr, Timmerman LA. Arthroscopic microfracture of chondral defects of the knee: A comparison of two postoperative treatments. Arthroscopy. 2005;21:152–8 [DOI] [PubMed] [Google Scholar]
- 31. McCarthy LP, 3rd, Cole BJ. Nonarthroplasty treatment of glenohumeral cartilage lesions. Arthroscopy. 2005;21:1131–42 [DOI] [PubMed] [Google Scholar]
- 32. Beaton DE, Wright JG, Katz JN. Development of the QuickDASH: Comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87:1038–46 [DOI] [PubMed] [Google Scholar]
- 33. Borstad JD. Resting position variables at the shoulder: Evidence to support a posture-impairment association. Phys Ther. 2006;86:549–57 [PubMed] [Google Scholar]
- 34. Finley MA, Lee RY. Effect of sitting posture on 3-dimensional scapular kinematics measured by skin-mounted electromagnetic tracking sensors. Arch Phys Med Rehabil. 2003;84:563–8 [DOI] [PubMed] [Google Scholar]
- 35. Greenfield B, Catlin PA, Coats PW, et al. Posture in patients with shoulder overuse injuries and healthy individuals. J Orthop Sports Phys Ther. 1995;21:287–95 [DOI] [PubMed] [Google Scholar]
- 36. Kebeatse M, McClure P, Pratt NA. Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinematics. Arch Phys Med Rehabil. 1999;80:945–50 [DOI] [PubMed] [Google Scholar]
- 37. Kaltenborn MF, Evjenth O, Kaltenborn JB, et al. Manual Mobilization of the Joints: Vol 1: The Extremities, 6th Ed. Oslo, Norway: Orthopedic Physical Therapy Products; 2002 [Google Scholar]
- 38. Hornby TG, Lewek MD, Thompson CK, Heitz R. Repeated maximal volitional effort contractions in human spinal cord injury: Initial torque increases. Neurorehabil and Neural Repair. 2009:23:928–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rabin A, Irrang JJ, Fitzgerald GK, Eubanks A. The intertester reliability of the scapular assistance test. J Orthop Sports Phys Ther. 2006;36:653–660 [DOI] [PubMed] [Google Scholar]
- 40. Kibler WB, McMullen J. Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg. 2003;11:142–151 [DOI] [PubMed] [Google Scholar]
- 41. Carpenter JE, Blasier RB, Pellizzon GG. The effects of muscle fatigue on shoulder joint position sense. Am J Sports Med. 1998;26:262–5 [DOI] [PubMed] [Google Scholar]
- 42. Ebaugh DD, McClure PW, Karduna AR. Scapulothoracic and glenohumeral kinematics following an external rotation fatigue protocol. J Orthop Sports Phys Ther. 2006;36:557–571 [DOI] [PubMed] [Google Scholar]
- 43. Coleman G. 52-week baseball training. 1st ed. Champaign, IL: Human Kinetics; 197–208, 2000 [Google Scholar]
- 44. Maitland GD. Maitland's Vertebral Manipulation 7th Ed. Philadelphia, PA: Elsevier; 2005 [Google Scholar]
- 45. Barden JM, Balyk R, Raso VJ, et al. Dynamic upper limb proprioception in multidirectional shoulder instability. Clin Orthop Relat Res. 2004;420:181–9 [DOI] [PubMed] [Google Scholar]
- 46. Myers JB, Wassinger CA, Lephart SM. Sensorimotor contribution to shoulder stability: effect of injury and rehabilitation. Man Ther. 2006;11:197–201 [DOI] [PubMed] [Google Scholar]
- 47. Rogol IM, Ernst G, Perrin DH. Open and closed kinetic chain exercises improve shoulder joint reposition sense equally in healthy subjects. J Athl Train. 1998;33:315–318 [PMC free article] [PubMed] [Google Scholar]
- 48. Giannakopoulos K, Beneka A, Malliou P, et al. Isolated vs. complex exercise in strengthening the rotator cuff muscle group. J Strength Cond Res. 2004;18:144–8 [DOI] [PubMed] [Google Scholar]
- 49. Fees M, Decker T, Snyder-Mackler L, et al. Upper extremity weight-training modifications for the injured athlete. A clinical perspective. Am J Sports Med. 1998;26:732–42 [DOI] [PubMed] [Google Scholar]
- 50. Reinold MM, Wilk KE, Macrina LC, et al. Current concepts in the rehabilitation following articular cartilage repair procedures in the knee. J Orthop Sports Phys Ther. 2006;36:774–94 [DOI] [PubMed] [Google Scholar]
- 51. Vanwanseele B, Lucchinetti E, Stussi E. The effects of immobilization on the characteristics of articular cartilage: Current concepts and future directions. Osteoarthritis Cartilage. 2002;10:408–19 [DOI] [PubMed] [Google Scholar]