Abstract
Subacromial impingement is a frequent and painful condition among athletes, particularly those involved in overhead sports such as baseball and swimming. There are generally two types of subacromial impingement: structural and functional. While structural impingement is caused by a physical loss of area in the subacromial space due to bony growth or inflammation, functional impingement is a relative loss of subacromial space secondary to altered scapulohumeral mechanics resulting from glenohumeral instability and muscle imbalance. The purpose of this review is to describe the role of muscle imbalance in subacromial impingement in order to guide sports physical therapy evaluation and interventions.
INTRODUCTION
According to the late neurologist Vladimir Janda MD, there are 2 approaches to classification of musculoskeletal pathologies: structural and functional.1 The structural approach focuses on actual damage to musculoskeletal structures such as rotator cuff tendonitis or a ligament injury. The functional approach examines factors that contribute to structural lesions. This approach is most useful for physical therapy management of chronic ‘dysfunctions’ such as persistent joint pain and tendonitis.
Shoulder impingement accounts for 44 to 65% of shoulder complaints during physician visits.2–3 First described by Neer,4 shoulder impingement has been classified into two main categories: structural and functional. Subacromial impingement can be caused by narrowing of the subacromial space (SAS) resulting from a reduction in the space due to bony growth or soft-tissue inflammation, (“structural”) or superior migration of the humeral head caused by weakness and/or muscle imbalance (“functional”).5–8 It is possible that some subacromial impingement results from a combination of both structural and functional factors.
Subacromial impingement occurs when the structures in the SAS (rotator cuff, biceps tendon long head, and subacromial bursa) become compressed and inflamed under the coracoacromial ligament.9 The suprasinatus tendon in particular is at highest risk for irritation and subsequent injury because it is the most likely to contact the acromion when the humerus is abducted to 90° and internally rotated 45°.10
Patients with impingement have significantly less (–68%, p < .05) SAS during shoulder elevation compared to the asymptomatic side when measured using MR imaging,11 even though their SAS is not significantly different from healthy shoulders in the resting anatomical position.12 When compared to normal subjects, patients with impingement demonstrate more proximal translation of the humeral head during abduction, thus reducing the SAS.6,13
Functional impingement is related to glenohumeral instability14 and is sometimes described as “functional instability,” occurring mostly in overhead athletes less than 35 years of age.15 The act of throwing may cause tissues below the coracoacromial arch to be subjected to subtle microtrauma, leading to inflammation and tendinitis.16–17
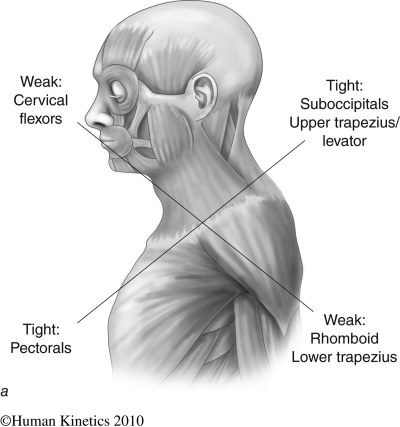
The shoulder complex relies on muscles to provide dynamic stability during its large range of mobility. Proper balance of the muscles surrounding the shoulder complex is also necessary for flexibility and strength; a deficit in flexibility or strength in an agonistic muscle must be compensated for by the antagonist muscle, leading to dysfunction. These muscular imbalances lead to changes in arthrokinematics and movement impairments, which may ultimately cause structural damage. Dr. Janda suggested that subacromial impingement results from a characteristic pattern of muscle imbalance including weakness of the lower and middle trapezius, serratus anterior, infraspinatus, and deltoid, coupled with tightness of the upper trapezius, pectorals and levator scapula.1 This pattern is often referred to as part of Janda's “Upper Crossed Syndrome.” (See Figure 1)
Figure 1.
Janda's Upper Crossed Syndrome. Reprinted, with permission, from Page et al, 2010, Assessment and Treatment of Muscle Imbalance: The Janda Approach (Champaign, IL: Human Kinetics).
While structural impingement sometimes requires surgery to alleviate pain, functional instability requires the implementation of precise therapeutic exercises with the goal of restoration of normal neuromuscular function. It is important for clinicians to understand the pathomechanics of functional impingement in order to guide appropriate examination, assessment, and intervention, as well as to consider prevention. The purpose of this clinical suggestion is to describe muscle imbalances associated with functional impingement in overhead athletes and to offer suggestions to guide intervention choices and prevention strategies.
PATHOMECHANICS OF MUSCLE IMBALANCE IN SUBACROMIAL IMPINGEMENT
Muscle tightness has been implicated in subacromial impingement. In particular, during elevation, anterior shoulder girdle muscle tension may affect the tension on the leading edge of the coracoacromial ligament, predisposing it to tightness ultimately leading to structural impingement.16 Tightness of the pectoralis major creates an anterior force on the glenohumeral joint with a consequent decrease in stability.18 A tight pectoralis minor limits scapular upward rotation, external rotation, and posterior tilt, thereby reducing SAS.19 This alteration in scapular kinematics occurs in three separate planes of movement and differs from scapular kinematics of those with normal muscle length.20–21
Imbalances in glenohumeral rotation range of motion may also contribute to altered shoulder kinematics. Specifically, excessive external rotation leads to increased anterior and inferior translation of the humerus, leading to anterior instability.22 In contrast, a lack of external rotation due to anterior muscular tightness alters the scapulohumeral rhythm and decreases posterior scapular tilt.23 Posterior capsular tightness, often demonstrated by a loss of internal rotation, may lead to more superior and anterior translation of the humeral head.23–25 This loss of internal rotation is known as glenohumeral internal rotation deficit, or “GIRD,” and is defined as a loss of internal rotation greater than or equal to 20° compared to the contralateral side.26 GIRD is a relatively new concept in the literature that requires more research regarding its incidence and effects in normal, athletic, and injured populations. Recent evidence suggests that overhead athletes with impingement often display signs and symptoms of GIRD.27–29
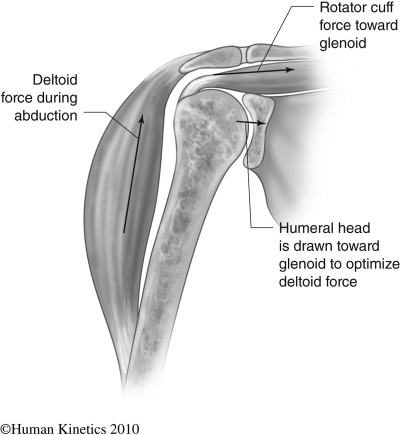
Imbalances or deficits in muscular strength and activation levels can lead to functional impingement. Both glenohumeral and scapulothoracic muscle imbalances can contribute to shoulder complex dysfunction. The pathomechanics of functional impingement may involve one or both of the shoulder force couples: deltoid/rotator cuff and scapular rotators. (Figures 2-3) Because of the lack of prospective studies, researchers have not determined whether muscle imbalance is a contributor to or result of impingement.
Figure 2.
Rotator Cuff / Deltoid Force Couple. Reprinted, with permission, from Page et al, 2010, Assessment and Treatment of Muscle Imbalance: The Janda Approach (Champaign, IL: Human Kinetics).
Figure 3.
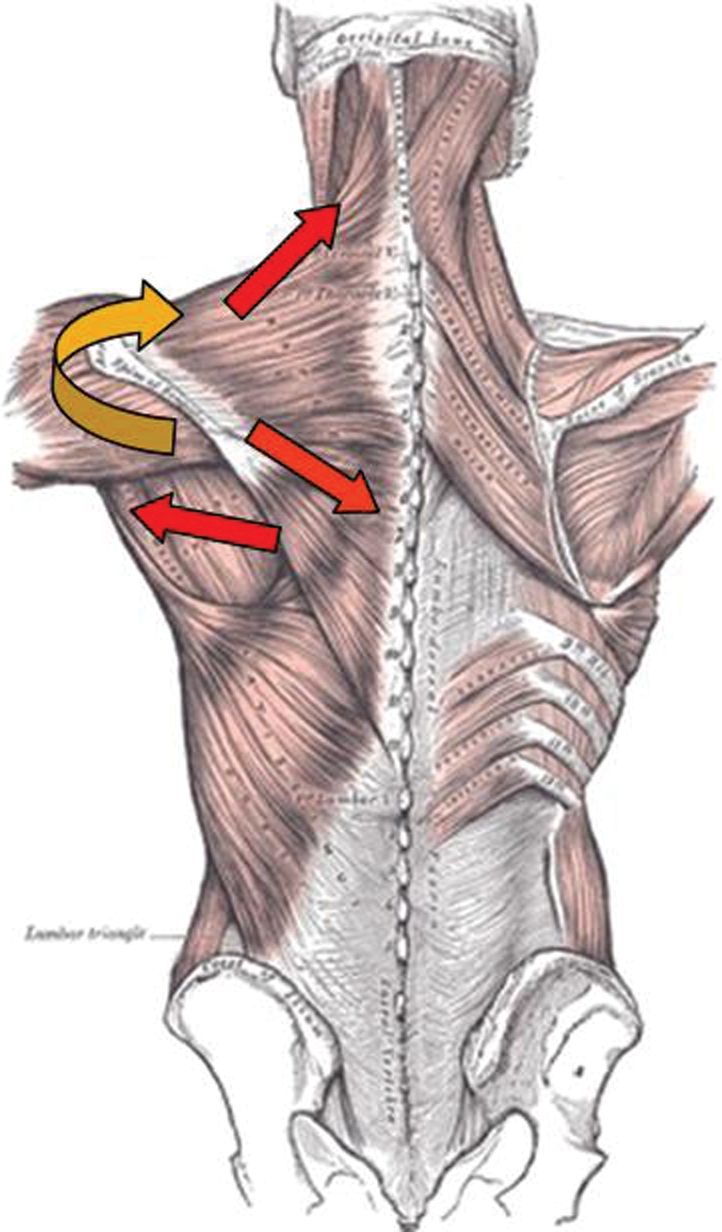
Trapezius / Serratus Force Couple.
GLENOHUMERAL IMBALANCES
Alterations in deltoid and rotator cuff co-activation and rotator cuff imbalances have been described in patients with impingement.30–34 The deltoid plays an important role in the pathomechanics of impingement due to its ability to offer upwardly directed force which must be balanced by the synchronous function of the rotator cuff musculature. Muscle imbalances in within the deltoid and rotator cuff force couple can cause compression within the SAS.7,35 The deltoid has been found to be atrophied and infiltrated with connective tissue in patients with shoulder impingement,36–37 and it exhibits lower levels of EMG activation in patients with impingement.33,38 While it is assumed that these effects on the deltoid are caused by impingement, it is unclear if the deltoid pathology precedes or is a result of impingement.
The rotator cuff is important in maintaining normal humeral head position in the glenoid during elevation (flexion and abduction) movements. The compressive forces of the rotator cuff stabilize the humerus against the glenoid, thereby providing dynamic stabilization of the glenohumeral joint.39–40 Weakness of the infraspinatus reduces this compressive force, promoting instability.18 This instability may lead to functional impingement.
When the dynamic stabilizing forces of the rotator cuff are removed from the glenohumeral joint in a cadaver model, there is a significant increase in superior and anterior migration of the humeral head during elevation, which would lead to impingement.35,41-42 Downward compressive forces of the inferior rotator cuff are necessary to neutralize the upwardly directed shear forces of the deltoid.35 Without rotator cuff stabilization in cadaveric models, the humeral head migrated 1.7 mm vs. 0.7 mm with rotator cuff stabilization at 60° of abduction, and 2.1 mm vs. 1.4 mm at 90° of abduction.42 Clearly, while cadaveric models do not accurately reflect the effect of dynamic neuromuscular activation (muscle activation and timing) of glenohumeral and scapulothoracic muscles during glenohumeral kinematics, they may offer some insight into the role of the rotator cuff.
Decreased rotator cuff EMG activity may also contribute to humeral head superior translation during early abduction, leading to impingement.33 Experimentally-induced fatigue of the rotator cuff leads to superior migration of the humeral head at the initiation of abduction,43–44 however, the effects of fatigue experienced after actually participating in an activity (such as repeated throwing) have not been investigated. Since these two studies only assessed scapular plane elevation, it is possible that other muscles may compensate for upward migration of the humeral head during functional activities that occur in planes other than the scapular plane. Few studies have assessed simultaneous rotator cuff EMG and glenohumeral kinematics in patients with impingement, leaving many questions unanswered regarding the exact pathomechanics of impingement.
SCAPULOTHORACIC IMBALANCES
Scapular rotation force couple imbalance leads to altered muscular activation patterns. When studying patients with impingement, most researchers describe an increase in upper trapezius EMG activation coupled with a decrease in activation of the middle trapezius, lower trapezius, and the serratus anterior.45–51 In contrast, other researchers have reported increased EMG activation in both the upper and lower trapezius in patients with impingement when compared to normal subjects.48 Ludewig and Cook hypothesized that the increased lower trapezius activation was an attempt to compensate for decreased serratus anterior activation. Interestingly, Lin et al studied subjects with various types of shoulder dysfunction and found decreased serratus anterior activity and increased upper trapezius activity without a change in lower trapezius activity when compared to normals.52
The lower trapezius may play the most important role in the scapular rotation force couple because it acts primarily as a scapular stabilizer.53–54 Decreased activation of the lower trapezius or increased activation of the upper trapezius may lead to an alteration of scapular rotation position which in turn leads to an upward migration of the axis of rotation of the glenohumeral joint, thus causing impingement. It is assumed that the lower trapezius demonstrates increased activity if the humeral head migrates upward during shoulder elevation,53 however, research has not verified this notion. Researchers have simultaneously measured trapezius EMG and 3-dimensional kinematics in patients with shoulder dysfunction.48,52 These studies found no significant change in humeral elevation, and either no change52 or an increase48 in lower trapezius activation. Ludewig and Cook48 reported small but significant increases in anterior-posterior translation of the humerus, possibly leading to decreased SAS.
Several authors have studied athletes with shoulder pain and have described altered EMG patterns and patterns of muscle imbalance.50,55–57 Overhead athletes with shoulder dysfunction typically have increased upper trapezius activation,51 as well as decreased activation levels of the serratus anterior,47 and lower trapezius,47,51 supporting Janda's belief that the lower trapezius and serratus are most prone to weakness.58 Researchers have compared the EMG activity of the trapezius in normal individuals, overhead athletes, and those with impingement.45-46,59 Cools et al51 reported that athletes with impingement have a significantly higher upper trapezius activation compared to normal subjects, a significant decrease in lower and middle trapezius activation, and altered trapezius muscle balance (See Table 1).
Table 1.
EMG activation of subjects with and without impingement during isokinetic abduction at 120°/s reproduced from cools et al, 2007.
| Patient Group | Upper Trap Activation | Lower Trap Activation | UT:LT ratio |
|---|---|---|---|
| Involved side (impingement) | 95%MVIC | 48%MVIC | 2.19 |
| Involved side (Control) | 73%MVIC | 62%MVIC | 1.23 |
| Uninvolved side (impingement) | 74%MVIC | 56%MVIC | 1.56 |
| Involved side (control) | 74%MVIC | 62%MVIC | 1.36 |
Overhead athletes with impingement have delayed onset of middle and lower trapezius fibers in response to a sudden downward movement.46 If the lower trapezius reacts too slowly when compared to the upper trapezius, the upper trapezius may become overactive, leading to scapular elevation rather than upward rotation.46 Freestyle swimmers with impingement are reported to have increased variability in timing of the onset of scapular rotators compared to healthy swimmers.50 These alterations in activation patterns are often seen bilaterally in patients with chronic tendinosis,31,46,50,59-60 supporting a neuromuscular mechanism. Since both painful and non-painful shoulders exhibit altered activation patterns, it is possible that the dysfunction is related to a faulty motor program within the central nervous system (CNS).
CONCLUSIONS
In summary, functional impingement may be associated with muscle imbalance; therefore, careful examination of flexibility and strength of important muscles about the shoulder complex is vital to understanding the root cause of impingement and prescribing effective treatment. Janda's approach to muscle imbalance suggests a possible neuromuscular component to functional impingement due to the predisposition of certain muscles to be tight or weak. The literature substantiates that imbalances in the glenohumeral and scapulothoracic musculature are present in patients with subacromial impingement.
Most believe that functional impingement is best managed with conservative treatment. While structural impingement sometimes requires surgical intervention, surgery for functional impingement may make patients worse. Successful treatment of functional impingement related to muscle imbalance is often accomplished by addressing the cause of the problem rather than symptomatic treatment of the pain. By understanding muscle imbalances associated with functional impingement, physical therapists can prescribe appropriate exercises for both treatment and prevention.
REFERENCES
- 1. Page P., Frank C.C., Lardner R., Assessment and treatment of muscle imbalance: The Janda Approach 2010, Champaign, IL: Human Kinetics [Google Scholar]
- 2. van der Windt D.A., et al. , Shoulder disorders in general practice: prognostic indicators of outcome. Br J Gen Pract. 1996;46:519–523 [PMC free article] [PubMed] [Google Scholar]
- 3. Vecchio P., et al. , Shoulder pain in a community-based rheumatology clinic. Br J Rheumatol. 1995;34(5):440–442 [DOI] [PubMed] [Google Scholar]
- 4. Neer C.S., 2nd, Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am. 1972;54(1):41–50 [PubMed] [Google Scholar]
- 5. Brossmann J., et al. , Shoulder impingement syndrome: influence of shoulder position on rotator cuff impingement--an anatomic study. Am J Roentgenol. 1996;167(6):1511–1515 [DOI] [PubMed] [Google Scholar]
- 6. Hallstrom E., Karrholm J., Shoulder kinematics in 25 patients with impingement and 12 controls. Clin Orthop Relat Res. 2006;448:22–27 [DOI] [PubMed] [Google Scholar]
- 7. Jerosch J., et al. , [Etiology of sub-acromial impingement syndrome--a biomechanical study]. Beitr Orthop Traumatol. 1989;36(9):411–418 [PubMed] [Google Scholar]
- 8. Ludewig P.M., Cook T.M., Translations of the humerus in persons with shoulder impingement symptoms. J Orthop Sports Phys Ther. 2002;32(6):248–259 [DOI] [PubMed] [Google Scholar]
- 9. Bigliani L.U., Levine W.N., Subacromial impingement syndrome. J Bone Joint Surg Am. 1997;79(12):1854–1868 [PubMed] [Google Scholar]
- 10. Graichen H., et al. , Subacromial space width changes during abduction and rotation--a 3-D MR imaging study. Surg Radiol Anat. 1999;21(1):59–64 [DOI] [PubMed] [Google Scholar]
- 11. Graichen H., et al. , Three-dimensional analysis of the width of the subacromial space in healthy subjects and patients with impingement syndrome. Am J Roentgenol. 1999;172(4):1081–1086 [DOI] [PubMed] [Google Scholar]
- 12. Hebert L.J., et al. , Acromiohumeral distance in a seated position in persons with impingement syndrome. J Magn Reson Imaging. 2003;18(1):72–79 [DOI] [PubMed] [Google Scholar]
- 13. Deutsch A., et al. , Radiologic measurement of superior displacement of the humeral head in the impingement syndrome. J Shoulder Elbow Surg. 1996;5(3):186–193 [DOI] [PubMed] [Google Scholar]
- 14. Jobe F.W., Kvitne R.S., Giangarra C.E., Shoulder pain in the overhand or throwing athlete. The relationship of anterior instability and rotator cuff impingement. Orthop Rev. 1989;18(9):963–975 [PubMed] [Google Scholar]
- 15. Belling Sorensen A.K., Jorgensen U., Secondary impingement in the shoulder. An improved terminology in impingement. Scand J Med Sci Sports. 2000;10(5):266–278 [DOI] [PubMed] [Google Scholar]
- 16. Bigliani L.U., et al. , The relationship of acromial architecture to rotator cuff disease. Clin Sports Med. 1991;10(4):823–838 [PubMed] [Google Scholar]
- 17. Hawkins R.J., Kennedy J.C., Impingement syndrome in athletes. Am J Sports Med. 1980;8(3):151–158 [DOI] [PubMed] [Google Scholar]
- 18. Labriola J.E., et al. , Stability and instability of the glenohumeral joint: the role of shoulder muscles. J Shoulder Elbow Surg. 2005;14(1 Suppl S):32S–38S [DOI] [PubMed] [Google Scholar]
- 19. Borstad J.D., Ludewig P.M., The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. J Orthop Sports Phys Ther. 2005;35(4):227–238 [DOI] [PubMed] [Google Scholar]
- 20. Borstad J.D., Resting position variables at the shoulder: evidence to support a posture-impairment association. Phys Ther. 2006;86(4):549–557 [PubMed] [Google Scholar]
- 21. Mottram S.L., Dynamic stability of the scapula. Man Ther. 1997;2(3):123–131 [DOI] [PubMed] [Google Scholar]
- 22. Mihata T., et al. , Excessive humeral external rotation results in increased shoulder laxity. Am J Sports Med. 2004;32(5):1278–1285 [DOI] [PubMed] [Google Scholar]
- 23. Lin J.J., Lim H.K., Yang J.L., Effect of shoulder tightness on glenohumeral translation, scapular kinematics, and scapulohumeral rhythm in subjects with stiff shoulders. J Orthop Res. 2006;24(5):1044–1051 [DOI] [PubMed] [Google Scholar]
- 24. Tyler T.F., et al. , Reliability and validity of a new method of measuring posterior shoulder tightness. J Orthop Sports Phys Ther. 1999;29(5):262–269 [DOI] [PubMed] [Google Scholar]
- 25. Harryman D.T., 2nd, et al. , Translation of the humeral head on the glenoid with passive glenohumeral motion. J Bone Joint Surg Am. 1990;72(9):1334–1343 [PubMed] [Google Scholar]
- 26. Burkhart S.S., Morgan C.D., Kibler W.B., The disabled throwing shoulder: spectrum of pathology Part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19(6):641–661 [DOI] [PubMed] [Google Scholar]
- 27. Kugler A., et al. , Muscular imbalance and shoulder pain in volleyball attackers. Br J Sports Med. 1996;30(3):256–259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Myers J.B., et al. , Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med. 2006;34(3):385–391 [DOI] [PubMed] [Google Scholar]
- 29. Tyler T.F., et al. , Quantification of posterior capsule tightness and motion loss in patients with shoulder impingement. Am J Sports Med. 2000;28(5):668–673 [DOI] [PubMed] [Google Scholar]
- 30. Burnham R.S., et al. , Shoulder pain in wheelchair athletes. The role of muscle imbalance. Am J Sports Med. 1993;21(2):238–242 [DOI] [PubMed] [Google Scholar]
- 31. Leroux J.L., et al. , Isokinetic evaluation of rotational strength in normal shoulders and shoulders with impingement syndrome. Clin Orthop Relat Res. 1994;30(4):108–115 [PubMed] [Google Scholar]
- 32. Myers J.B., et al. , Shoulder muscle coactivation alterations in patients with Subacromial impingement (Abstract). Med Sci Sports Exerc. 2003;35(5):S346 [Google Scholar]
- 33. Reddy A.S., et al. , Electromyographic analysis of the deltoid and rotator cuff muscles in persons with subacromial impingement. J Shoulder Elbow Surg. 2000;9(6):519–523 [DOI] [PubMed] [Google Scholar]
- 34. Warner J.J., et al. , Patterns of flexibility, laxity, and strength in normal shoulders and shoulders with instability and impingement. Am J Sports Med. 1990;18(4):366–375 [DOI] [PubMed] [Google Scholar]
- 35. Payne L.Z., et al. , The combined dynamic and static contributions to subacromial impingement. A biomechanical analysis. Am J Sports Med. 1997;25(6):801–808 [DOI] [PubMed] [Google Scholar]
- 36. Kronberg M., Larsson P., Brostrom L.A., Characterisation of human deltoid muscle in patients with impingement syndrome. J Orthop Res. 1997;15(5):727–733 [DOI] [PubMed] [Google Scholar]
- 37. Leivseth G., Reikeras O., Changes in muscle fiber cross-sectional area and concentrations of Na,K-ATPase in deltoid muscle in patients with impingement syndrome of the shoulder. J Orthop Sports Phys Ther. 1994;19(3):146–149 [DOI] [PubMed] [Google Scholar]
- 38. Michaud M., et al. , Muscular compensatory mechanism in the presence of a tendinitis of the supraspinatus. Am J Phys Med. 1987;66(3):109–120 [PubMed] [Google Scholar]
- 39. Inman V.T., Saunders J.B., Abbott L.C., Observations on the function of the shoulder joint. J Bone Joint Surg Am. 1944;26(1):1–30 [Google Scholar]
- 40. Poppen N.K., Walker P.S., Forces at the glenohumeral joint in abduction. Clin Orthop Relat Res. 1978;13(5):165–170 [PubMed] [Google Scholar]
- 41. Wuelker N., Korell M., Thren K., Dynamic glenohumeral joint stability. J Shoulder Elbow Surg. 1998;7(1):43–52 [DOI] [PubMed] [Google Scholar]
- 42. Sharkey N.A., Marder R.A., Hanson P.B., The entire rotator cuff contributes to elevation of the arm. J Orthop Res. 1994;12(5):699–708 [DOI] [PubMed] [Google Scholar]
- 43. Chen S.K., et al. , Radiographic evaluation of glenohumeral kinematics: a muscle fatigue model. J Shoulder Elbow Surg. 1999;8(1):49–52 [DOI] [PubMed] [Google Scholar]
- 44. Teyhen D.S., et al. , Rotator cuff fatigue and glenohumeral kinematics in participants without shoulder dysfunction. J Athl Train. 2008;43(4):352–358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cools A.M., et al. , Scapular muscle recruitment pattern: electromyographic response of the trapezius muscle to sudden shoulder movement before and after a fatiguing exercise. J Orthop Sports Phys Ther. 2002;32(5):221–229 [DOI] [PubMed] [Google Scholar]
- 46. Cools A.M., et al. , Scapular muscle recruitment patterns: trapezius muscle latency with and without impingement symptoms. Am J Sports Med. 2003;31(4):542–549 [DOI] [PubMed] [Google Scholar]
- 47. Cools A.M., et al. , Evaluation of isokinetic force production and associated muscle activity in the scapular rotators during a protraction-retraction movement in overhead athletes with impingement symptoms. Br J Sports Med. 2004;38(1):64–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ludewig P.M., Cook T.M., Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80(3):276–291 [PubMed] [Google Scholar]
- 49. Moraes G.F., Faria C.D., Teixeira-Salmela L.F., Scapular muscle recruitment patterns and isokinetic strength ratios of the shoulder rotator muscles in individuals with and without impingement syndrome. J Shoulder Elbow Surg. 2008;17(1 Suppl):48S–53S [DOI] [PubMed] [Google Scholar]
- 50. Wadsworth D.J., Bullock-Saxton J.E., Recruitment patterns of the scapular rotator muscles in freestyle swimmers with subacromial impingement. Int J Sports Med. 1997;18(8):618–624 [DOI] [PubMed] [Google Scholar]
- 51. Cools A.M., et al. , Trapezius activity and intramuscular balance during isokinetic exercise in overhead athletes with impingement symptoms. Scand J Med Sci Sports. 2007;17(1):25–33 [DOI] [PubMed] [Google Scholar]
- 52. Lin J.J., et al. , Functional activity characteristics of individuals with shoulder dysfunctions. J Electromyogr Kinesiol. 2005;15(6):576–586 [DOI] [PubMed] [Google Scholar]
- 53. Bagg S.D., Forrest W.J., Electromyographic study of the scapular rotators during arm abduction in the scapular plane. Am J Phys Med. 1986;65(3):111–124 [PubMed] [Google Scholar]
- 54. Johnson G., et al. , Anatomy and actions of the trapezius muscle. Clin Biomech (Bristol, Avon). 1994;9:44–50 [DOI] [PubMed] [Google Scholar]
- 55. Pink M., et al. , The painful shoulder during the butterfly stroke. An electromyographic and cinematographic analysis of twelve muscles. Clin Orthop Relat Res. 1993;288: p. 60–72 [PubMed] [Google Scholar]
- 56. Ruwe P.A., et al. , The normal and the painful shoulders during the breaststroke. Electromyographic and cinematographic analysis of twelve muscles. Am J Sports Med. 1994;22(6):789–796 [DOI] [PubMed] [Google Scholar]
- 57. Scovazzo M.L., et al. , The painful shoulder during freestyle swimming. An electromyographic cinematographic analysis of twelve muscles. Am J Sports Med. 1991;19(6):577–582 [DOI] [PubMed] [Google Scholar]
- 58. Janda V., Muscle strength in relation to muscle length, pain, and muscle imbalance, in Muscle Strength (International Perspectives in Physical Therapy) Harms-Ringdahl, Editor 1993, Churchill Livingstone: Edinburgh: p. 83–91 [Google Scholar]
- 59. Cools A.M., et al. , Rehabilitation of scapular muscle balance: which exercises to prescribe? Am J Sports Med. 2007;35(10):1744–1751 [DOI] [PubMed] [Google Scholar]
- 60. Roe C., et al. , Muscle activation in the contralateral passive shoulder during isometric shoulder abduction in patients with unilateral shoulder pain. J Electromyogr Kinesiol. 2000;10(2):69–77 [DOI] [PubMed] [Google Scholar]