Abstract
The benefits and proposed physiological mechanisms of eccentric exercise have previously been elucidated and eccentric exercise has been used for well over seventy years. Traditionally, eccentric exercise has been used as a regular component of strength training. However, in recent years, eccentric exercise has been used in rehabilitation to manage a host of conditions. Of note, there is evidence in the literature supporting eccentric exercise for the rehabilitation of tendinopathies, muscle strains, and in anterior cruciate ligament (ACL) rehabilitation. The purpose of this Clinical Commentary is to discuss the physiologic mechanism of eccentric exercise as well as to review the literature regarding the utilization of eccentric training during rehabilitation. A secondary purpose of this commentary is to provide the reader with a framework for the implementation of eccentric training during rehabilitation of tendinopathies, muscle strains, and after ACL reconstruction.
Keywords: eccentric exercise, rehabilitation, tendinopathy, muscle strain, negative work, anterior cruciate ligament
INTRODUCTION
Over approximately the last fifteen years, use of eccentric exercise in rehabilitation has increasingly gained attention in the literature as a specific training modality. That being said, the concept of eccentric exercise is not new. To the authors' knowledge, the earliest investigation of eccentric versus concentric exercise was published in 1938.1 Eccentric exercise has been primarily described in the rehabilitation literature describing the management of tendinopathies. However, evidence is mounting to support its use in the treatment of muscle strains, with most of the rehabilitation literature relating to the use of eccentric training in rehabilitation after hamstring injuries. Finally, eccentric training has been used in recent years as a part of rehabilitation following ACL reconstruction. The purpose of this clinical commentary is to present the physiologic basis for eccentric exercise and to discuss the evidence in support of eccentric exercise in the management of patients recovering from tendinopathies, muscle strains, and ACL reconstructions. Additionally, suggested implementation of eccentric exercise in the management of these conditions will be highlighted. Although important to the clinician, the causes of these injuries as well as the mechanisms and origins of pain associated with these injuries are beyond the scope of this commentary. Further, other interventions used typically with these conditions such as stretching and modalities will not be discussed. It is important to note that although the focus of this commentary details the benefits of eccentric training, it is the authors' suggestion that a comprehensive rehabilitation approach include both concentric and eccentric training. It is not the authors' intent to advocate exclusive use of eccentric training, but rather to point out the investigated benefits of and utilization of eccentric exercise as a part of a comprehensive rehabilitation program.
PHYSIOLOGY OF ECCENTRIC EXERCISE
During voluntary contraction of a muscle, speed of contraction and ability to exert tension are inversely related. The faster a muscle contracts concentrically, the lower the tension it is able to generate.1 Tension in muscle fibers when lengthening is considerably greater than when muscle fibers are shortening.2–4 During negative work (eccentric exercise), the oxygen consumption rarely rises to more than twice the resting value.5–9 Previous studies have shown that when a muscle is eccentrically lengthened, the energy requirement falls substantially in comparison to concentric contractions because ATP breakdown and heat production are both slowed.8–10 Bigland-Ritchie et al11 found: 1) less muscle activity was required to maintain the same force during negative work, 2) fewer muscle fibers were required to exert a given force, and 3) there was a substantial reduction in oxygen uptake when fibers were eccentrically lengthened. Furthermore, with increased heat generation during concentric/positive work, there is a concurrent increase in cellular metabolism. Thus, more waste products will be generated with concentric work, potentially leading to chemical irritation of nerves and eventually pain. Abbott et al5 measured oxygen uptake in subjects during bicycle ergometry. Positive work (concentric exercise) resulted in more oxygen consumption than negative work. Abbott and others6 then performed a follow up study examining the relationship between oxygen consumption and work. Oxygen consumption was nearly three times larger at great force and low speed than at small force and high speed. The above studies show that eccentric exercise results in less oxygen consumption, greater force production, and less energy expenditure than concentric exercise.
TENDINOPATHY
Tendon injuries account for 30-50% of injuries in sports.12 Specifically, chronic problems caused by overuse of tendons result in 30% of all running-related injuries, and elbow tendon injuries can be as high as 40% in tennis players.13 Incidence of patellar tendinopathy is reported to be as high as 32% and 45% in basketball and volleyball players, respectively.14 Tendon pathologies not only lead to lost time and performance declines in sports, but also can result in long term damage to tendons that can affect daily function.
REVIEW OF LITERATURE: ECCENTRIC TRAINING IN TENDINOPATHY
Many studies recently have substantiated eccentric exercise as an effective treatment for tendinopathies. Eccentric training may be effective for tendinopathies based on work by Williams15 who found that oxygen consumption is seven and a half times lower in tendons/ligaments than in skeletal muscle. A low metabolic rate and anaerobic energy generating capacity are needed to carry loads and maintain tension for long periods as is typical of tendons. However, the low metabolic rate results in slow healing after tendon injury. Based on data presented previously on the physiology of eccentric work requiring less oxygen consumption than concentric work, eccentric training may be ideally suited for the rehabilitation of tendinopathies.
In 1998, Alfredson16 performed, to the authors' knowledge, the first study investigating the effects of eccentric exercise on diseased tendons. The protocol utilized has since been used in most studies on eccentric training. In a prospective study of 15 athletes with chronic achilles tendinosis, three sets of 15 repetitions of bent knee and straight knee calf raises were performed, twice a day, seven days per week over 12 weeks. Athletes were told to work through pain, only ceasing exercise if pain became disabling. Training load was increased in 5 kg increments with use of a backpack that allowed for the addition of the weight once training with bodyweight was pain free. All fifteen athletes returned to pre-injury levels of activity. Additionally, they had a significant decrease in pain with a significant increase in strength.
Positive changes in tissue structure and mechanical properties as a result of eccentric training have been previously described. Shalabi et al17 evaluated 25 patients with chronic achilles tendinopathy before and after an eccentric program using the Alfredson et al16 protocol. Subjects' tendon volume and intratendinous signal were measured via magnetic resonance imaging (MRI). Eccentric training resulted in decreased tendon volume and decreased intratendinous signal, which correlated to improved pain and subjective performance.. Reduction in fluid content within the tendon may suggest increased healthy collagen deposition. Langberg et al18 found that Type I collagen synthesis increased after eccentric training in a group of twelve soccer players with unilateral achilles tendinosis, offering a possible explanation for the mechanism of tendon healing. Ohberg et al19 also found a decrease in tendon thickness and normalized tendon structure measured by ultrasound in most patients, both of which correlated with less pain, in a group of subjects with chronic Achilles tendinosis who were trained using the Alfredson et al16 eccentric calf protocol. Mahieu et al20 found that eccentric training of the plantar flexors resulted in positive changes to the mechanical properties of the plantar flexor muscle-tendon tissue including passive resistive torque, dorsiflexion range of motion, and stiffness.
Several authors have conducted studies that support the use of eccentric exercise in the treatment of a variety of tendinopathies. Jonsson and Alfredson21 studied athletes with jumpers knee (patellar tendinopathy) who were randomized into either an eccentric or concentric exercise group and treated for 12 weeks. At mean follow-up of 32 months, the eccentric exercise group was still satisfied subjectively and “sports active”, although it was not specifically stated whether they returned to sport or not. Subjects in the concentric exercise group had undergone surgery or sclerosing injections. In another study of elite volleyball players with patellar tendinopathy, Young et al22 found that subjects improved from baseline at 12 weeks and 12 months. In contrast, Visnes et al23 found no effect of eccentric training on jumper's knee in volleyball players during the competitive season. The lack of results from eccentric training in this study may be due to the fact that athletes continued to participate in volleyball during the competitive season. Because rest is often advocated as a component of rehabilitation, failing to cease the aggravating activity may have perpetuated their injury and contributed to the lack of results.
Systematic reviews of literature by Wasielewski & Kotsko24, as well as Kingma et al25 examined the effects of eccentrics in reducing pain and improving strength in subjects with lower extremity tendinosis and chronic achilles tendinopathy, respectively. These reviews revealed that eccentric exercise may reduce pain and improve strength in patients with lower extremity tendinopathies, but whether it is better than other forms of rehabilitation has yet to be determined. Therefore, no definitive conclusions can be made regarding whether or not the performance of eccentric exercise alone is superior to concentric-eccentric training or concentric-minimized training.
IMPLEMENTATION OF ECCENTRICS IN REHABILITATION OF TENDINOPATHIES
Regardless of the involved tendon, load and volume of exercise should be progressed gradually and should be dictated by the amount of pain experienced by the athlete. Because the athlete is recovering from injury, the authors of this commentary advise that training load not be determined by a one repetition maximum (1 RM). Further, some of the exercises are for targeted muscle groups (elbow extensors for elbow injury) and determining a 1 RM is not practical or advised. The Alfredson et al16 protocol has been used in previous studies and appears to be a safe, effective method of implementing the eccentric training program for tendinopathies. Unfortunately, the Alfredson protocol was described for and used in the treatment of achilles tendinopathies and their exact recommendations may not be appropriate for all tendons or regions. The clinician may use the protocol for an example of volume and frequency of training, but in lieu of added weights to a backpack, adding weights to a leg press or using various resistances of ankle weights and dumbbells would seem appropriate. For tendinopathies in the shoulder, elbow, or hand, increases by five-kilogram increments is likely inappropriate and resistances should be adjusted accordingly.
Curwin27 has previously proposed a method to determine training load in eccentric training for tendon injuries that is based on number of repetitions completed and the amount of pain experienced. One significant difference between Curwin's and Alfredson's programs is that the athlete performs both the concentric and eccentric portion of the exercise in Curwin's program, with the eccentric portion being performed faster. Alfredson encouraged a slow, 3-4 second eccentric contraction. In Curwin's protocol, they suggest that the athlete should experience pain and fatigue between 20 and 30 repetitions at a given load, when performing three sets of 10 repetitions. Their rationale for experiencing pain is based on the premise that exercise load should be determined by the tendon tolerance, which is indicated by pain experienced during the exercise. Curwin and Stanish determined empirically that pain felt before 20-30 repetitions would likely be accompanined by worsening of symptoms. Pain felt before that range is generally accompanied by worsening of symptoms and either load or speed is of contraction should be decreased. If there is no pain after 30 repetitions, the stimulus is inadequate. Either load or the speed of exercise performance should be increased, but not both simultaneously. Pain experienced during the exercise protocol should be similar to the pain experienced during the athlete's functional activity with an acceptable, moderate increase from that point on in the program. During the first session, load is increased until symptoms appear. After a general warm-up (bike, upper body ergometer), athletes perform two 30 second stretches of the involved muscle group.
Based on the clinical experience of the authors and Ratamess and others,28 it is recommended that 6-12 repetitions over four sets be completed to emphasize strength in the muscle-tendon complex. The athletes use the load from the six repetition resistance and build up to twelve repetitions prior to increasing load again. Anecdotally, the authors have found this method to be progressive, yet safe, with less overall volume to help enhance recovery. Additionally, the authors advocate three to four sessions per week instead of every day. The authors propose that “heavy load” is a misnomer in the Alfredson et al16 study because the volume of exercise is rather high and the load is low given the amount of exercise that is tolerated by the athletes. Ultimately however, dosing must be based on tendon reactivity and patient response.
The authors suggest having the clinician or athlete perform the concentric portion of the exercise passively or with the assistance of the uninvolved limb during closed chain exercises, followed by having the athlete perform the eccentric portion of the exercise independently. Based on clinical experience, the authors propose that the concentric portion of the exercise can be attempted without assistance once non-sport activities, like walking and stair climbing, are pain free. As with eccentric exercise, progression of the concentric portion of exercise should involve a gradual increase. Once the concentric portion of exercise is pain free, the authors suggest that athletes can begin jogging or more sport specific activities. A progression from individual drills to team activities is a disciplined way to reintroduce an athlete to their chosen sport. If they have pain, they should return to the previous regimen until they are pain free. A cool down activity (i.e recumbent bike) followed by stretching of involved muscles should follow the program. Although Thacker and others29 have found that there is insufficient evidence to support pre- or post-exercise stretching, lack of musculotendinous flexibility is a common finding in chronic tendinopathies27 and should be a part of the program if identified. Ice to the affected area is advised to limit post-exercise pain and potential inflammation. Athletes should be warned that eccentric exercise may make them sore initially, and that this is to be expected. Although the above recommendations are anecdotal in nature and reflect clinical experience, the authors of this review have had success with the combined stretching and icing approach.
HAMSTRING STRAIN
Most of the literature on muscle strains revolves around injuries to the hamstring muscle group, therefore, they will be the focus of this section. The reader is directed to the review by Hibbert et al30 on the effectiveness of eccentric strength training for the prevention of muscle strains.
Hamstring strains are among the most common injuries sustained by athletes.31–34 Hamstring muscle strains are currently the most common injury in professional soccer35 and they account for 29% of injuries in track and field sprinters.36 They are common in sports that require maximum sprinting, kicking, acceleration, and change of direction.36 The average amount of time lost from competition and training is 18 days,37 but has also been reported to vary between 8 and 25 days.38 Furthermore, athletes must deal with persistent symptoms and a likelihood of re-injury, found to be present in anywhere from 12-31% of those who sustain a hamstring strain.39,40 Highest risk of recurrence is within the first two weeks of returning to sport.41 Greig and Siegler42 performed an intermittent treadmill protocol to replicate soccer-specific fatigue. Peak isokinetic eccentric knee flexor strength was measured at three speeds at the end of a simulated (passive) halftime and at the end of the treadmill protocol. Eccentric hamstring strength decreased with increased work time and after the halftime interval. Athletes may therefore be at risk of injury with increased time in competition and shortly after halftime.
Muscle strain injuries are thought to occur when muscles are actively lengthened to greater than resting lengths.36 The combination of rapid eccentric contraction with active muscle contraction elsewhere in the musculotendinous unit can produce mechanical strain leading to muscle injury.43 In ball sports, hamstring injury tends to occur when turning sharply or cutting, whereas in sprinting the injury occurs while running at full speed without a change of direction.32,44,45 Because of the biarticular nature of the hamstrings, they can be vulnerable to injury during running, cutting, and sprinting; all of which involve a combination of hip flexion and knee extension, which maximally lengthens the hamstring group. Hamstrings have to contract rapidly to generate a large amount of power.44 Several authors have suggested that most hamstring injuries occur during the late swing and early contact phases of running.44–46 Because the biceps femoris has greater lengthening and electrical activity during the late swing phase of running,46 it may be more susceptible to injury than the medial hamstrings. Kouloris and Connell47 found that biceps femoris strains accounted for 80% of the 170 hamstring injuries that occurred in athletes. Small et al found that reductions in eccentric strength occur during later stages of simulated soccer match play.48 Consequently, greater muscle strength imbalance between eccentric hamstring and concentric quadriceps strength has also been observed in later stages of match play or with fatigue.48–50
Sugiura et al44 performed a prospective study of elite sprinters to determine a relationship between strength and hamstring injury within 12 months of testing. This was the first study to examine the concentric and eccentric isokinetic strength of the hip extensors, quadriceps, and hamstrings that reflects their actions in late swing or early contact. Testing was performed on 30 male elite sprinters. Injuries occurred in six subjects. Eccentric weakness of the hamstrings at 608 per second was found to be a common factor among those who sustained injuries. Side to side comparison revealed that the injury always occurred on the weaker side. Similar findings were elucidated by Orchard et al51 who found that hamstring muscle injury was associated with low hamstring-to-quadriceps ratio at 608 per second on the injured side and a low side-to-side peak torque at 608 per second in a group of Australian football players. Therefore, it may be advantageous to include eccentric training as part of either a training regimen or rehabilitation protocol to minimize asymmetries or to help maximize strength gains.
REVIEW OF LITERATURE: ECCENTRIC TRAINING IN PREVENTION OF HAMSTRING STRAINS
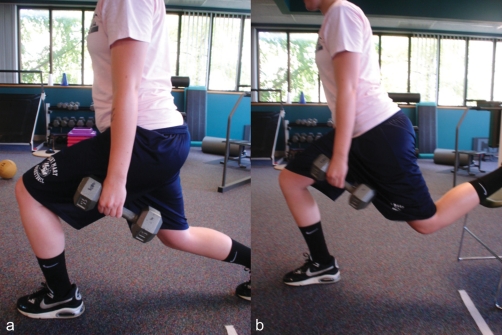
Small et al48 investigated the effect of eccentric hamstring strengthening during soccer training. The objective was to evaluate if there was a difference in eccentric strength with fatigability and to see if eccentric training would attenuate the effects of fatigue. Sixteen semiprofessional soccer players completed a 90-minute simulated soccer game. At half time and at the conclusion of the game, the athletes performed isokinetic testing at 1208 per second for the quadriceps and hamstrings. Two groups of subjects performed the “Nordic hamstring” eccentric exercise (Figure 1a, 1b) either during the cool-down or the warm-up period twice weekly during the 8-week intervention program. The group that performed the exercise in the cool down period showed significant increases in eccentric hamstring peak torque and the functional eccentric hamstring to concentric quadriceps ratio post-intervention compared to the warm-up group. Based on the results of this study, eccentric strength training conducted post-training significantly reduced the effects of fatigue. Therefore, performing eccentric training with fatigue may have a time-dependent beneficial effect.
Figure 1.
a, b. Nordic hamstring exercise.
Askling and others52 examined the relationship between eccentric training and subsequent injury in elite male soccer players. Thirty players were divided among two groups, one of which performed eccentric training in addition to the typical soccer team training 1-2x/week for 10 weeks, while the control group performed only the team training. Isokinetic hamstring strength and maximal running speed were measured in both groups before and after the training period. Injuries were monitored over 10 months. The eccentric training group had significantly fewer hamstring injuries (3/15) compared to the control group (10/15). In addition, the training group showed statistically significant improvements in strength and speed.
Arnason et al53 compared “eccentric hamstring lowers” (Nordic hamstring exercise) to contract-relax hamstring stretching with incidence and severity of hamstring strains in professional soccer players. Participants performed one of three interventions: warm up stretching performed independently with contract-relax stretching, partner-assisted contract-relax hamstring flexibility exercises, and eccentric hamstring exercises. The overall incidence of hamstring strains was 65% lower in the eccentric group. While incidence of hamstring injury was lower in the eccentric training group, injury severity and re-injury rates were not statistically significantly different.
Gabbe et al54 performed a randomized controlled trial that examined the relationship between eccentric strengthening and prevention of hamstring strains in 220 male football players in the Victorian Amateur Football Association. One group performed the “hamstring lowers” as previously described53 and the other performed stretching and range of motion exercises. Unfortunately, compliance was an issue in this study, but among players who completed at least two sessions, the incidence of hamstring strains in the eccentric group was 4% compared to 13% in the stretching and range of motion group. Brooks et al55 examined the effects of eccentric hamstring lowers and stretching on incidence and severity of hamstring strains in 546 professional rugby players. The intervention group was reported to display significantly lower incidence and severity of hamstring injury than the strengthening group and the conventional stretching/strengthening group.
Holcomb et al56 investigated whether a hamstring-emphasized resistance training program would improve isokinetic hamstring:quadriceps ratios in a group of 12 female NCAA soccer players. Subjects were tested before and after completing a six week training program with two randomly chosen specific exercises from a group of six exercises targeting the hamstrings. Subjects performed both the concentric and eccentric phases of the exercises. The hamstrings:quadriceps ratio was measured at 60, 180, and 2408 per second. Six weeks of strength training emphasizing the hamstrings significantly increased the eccentric hamstring:concentric quadriceps ratio from below 1.0 to over 1.0. Eccentric hamstring:concentric quadriceps ratio has been advocated to be at least 1.0.57,58
While the above studies used eccentric training in healthy subjects or in the context of prevention of future injury, the data is nonetheless promising about the positive effects of eccentric training on strength, altering hamstring to quadriceps ratios, and preventing injury. Because of that, the clinician can surmise that the use of eccentric training as a part of the recovery after hamstring strains may lead to improved outcomes and decreased risk of future injury. It should be noted that the authors are not advocating the elimination of the concentric portion of an isotonic exercise, but rather increasing eccentric emphasis by assisting during concentric exercise or concentrically-minimized exercises.
IMPLEMENTATION OF ECCENTRICS TRAINING IN HAMSTRING STRAINS
Based on the literature presented on the varied outcomes related to eccentric training, it is evident that there may be promise in making eccentric training an integral part of the rehabilitation program after a hamstring strain. The authors of this commentary wish to focus on exercise interventions in lieu of isokinetic exercise interventions because access to isokinetic devices for a majority of clinicians is limited. The exercises subsequently discussed undeniably have a concentric component. As stated previously, the authors are not advocating elimination of the concentric portion of any exercise. It is generally accepted that it is virtually impossible and undesireable to eliminate the concentric portion entirely. However, the authors suggest that clinicians should have an increased awareness regarding how to design exercises to have a greater eccentric emphasis and should also consider how eccentric exercise should be a part of a systematic and progressive approach to training after injury to the hamstrings.
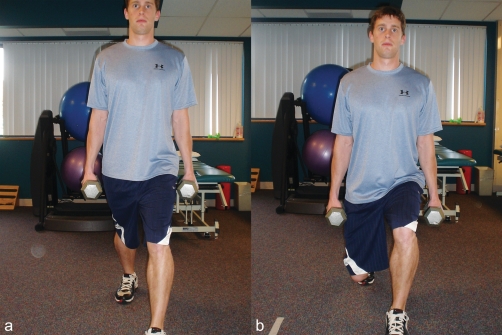
Comfort et al59 proposed a rehabilitation and conditioning continuum for hamstring rehabilitation. After the initial inflammatory phase resolves, initial goals are to restore range of motion and begin strengthening using hamstring-specific exercises that are primarily open kinetic chain and non-weight bearing. Once non-weight bearing exercises are tolerated, they suggest implementing low-velocity eccentric activities such as stiff leg dead lifts (Figure 2), eccentric hamstring lowers/Nordic hamstring exercise, and split squats (Figure 3a, 3b). The next phase involves higher velocity eccentric exercises that include plyometric and sport specific activities designed to increase hamstring torque and lower extremity power. Examples include squat jumps, split jumps, bounding, and depth jumps. Finally, sport specific progressions should complete the program. Comfort et al59 suggest progressing from unidirectional linear movements to bidirectional and then multidirectional movements. Some of these exercises may include single leg bounding, backward skips, lateral hops, lateral bounding, and zigzag hops and bounding.
Figure 2.
Stiff leg deadlifts.
Figure 3.
a, b. Split squat and progression.
Brughelli and Cronin36 suggested a host of exercises in lieu of the “eccentric lowers/Nordic hamstring” exercise in the training of a non-injured athlete. They contend that while the “Nordic hamstring” may be a good exercise alternative, it is both bilateral and open chain. Because of this, one leg may be able to compensate for the involved limb. As stated previously, the hamstrings are a biarticular muscle and should be trained as such. Clark et al60 found that after four weeks of training with the Nordic hamstring exercise, vertical jump and peak torque of the hamstrings increased. Brughelli and Cronin36 propose that eccentric exercise interventions for reducing hamstring strains should include the following: high force, maximal muscle elongation, high velocity, multi-joint movements, closed-chain exercises, unilateral exercises, and easily implemented, cost-effective exercises. Isokinetic devices could be used for eccentric training, however are often cost-prohibitive, require proper patient training, and also require adequate space. Isokinetic exercise does not offer functional velocities for exercise training nor does it provide multi-joint, closed-chain options. In contrast, several exercises are advocated that require little equipment for effective implementation and fulfill the suggestions of Burghelli and Cronin.36 Some examples of these exercises include plyometric box jumps, eccentric backward steps (Figure 4), eccentric lunge drops (Figure 5a, 5b), eccentric forward pulls (Figure 6), single and double leg deadlifts, and in split stance deadlift (“good morning” exercise) with the load in front of the body, as opposed to a posterior load utilized during the traditional performance of this exercise (Figure 7a, 7b).
Figure 4.
Eccentric backward steps. The subject resists the clinician's attempt to push him/her backwards.
Figure 5.
a, b. Eccentric lunge drops. The subject begins in a split stance position and drops rapidly into a lunge position.
Figure 6.
Eccentric forward pulls. The subjects resists forward pull by the clinician.
Figure 7.
a, b. Split stance Zercher also called the “good morning” exercise. The subject is in a split stance position with the weight placed anteriorly to increase the lever arm on the hamstrings. The subject then leans forward through flexion at the hip..
Heiderscheit and others38 recently commented on hamstring injuries and provided a structural framework for rehabilitation. Once the initial inflammatory phase has resolved, low intensity, pain free exercises involving the entire lower extremity and trunk are implemented to minimize atrophy and develop neuromuscular control of the lower extremities and trunk. Phase two exercises involve progression of intensity and range of motion based on patient tolerance. In stage two, eccentric exercises are initiated. Exercises are submaximal at the mid-length of the muscle and also include trunk stabilization exercises and agility training in the frontal and transverse planes. Finally, stage three exercises involve sport-specific exercises that involve quick direction changes, functional movement patterns, and eccentric exercises progressing to include end-range movement.
The authors of this commentary agree with Heiderscheit et al38 that initial phases of rehabilitation should focus on controlling pain, edema, and inflammation as well as tolerance of pain-free concentric exercises prior to initiation of eccentrics. Intuitively, eccentric exercises should be initiated in low to middle ranges of motion in order to limit the risk of further injury. Walking lunges, multi-directional step ups, split squats, stiff leg dead lifts, and “modified good mornings” should be implemented within pain free range of motion. Additionally, the authors of this commentary recommend doing the Nordic hamstring/eccentric lowers with elastic band assistance (Figure 8) in rehabilitation, and the previously described technique (Figure 1a, 1b) would be a progression. By using a heavy-resistance band, the recovering athlete has the elasticity of the band to assist in both the concentric and eccentric portions of the exercise. As the athlete tolerates this exercise and completes it throughout the full range of motion, the band can be eliminated.
Figure 8.
Nordic hamstring exercise with elastic assistance.
The authors suggest agility ladder drills and shuffling can be used as either an “active recovery” or as an active warm-up. As the athlete continues to tolerate increased range of motion during exercises, load should be increased with a concomitant decrease in volume. For hamstring strengthening, the authors of this manuscript refer the reader to the American College of Sports Medicine's Position Statement by Ratamess and colleagues28 for progression of resistance exercise. The authors propose increasing speed of performance to more closely replicate sport demands. Athletes can perform exercises in a given time frame (i.e. continuous for 35-45 seconds for a hockey player) or with modifications in work: rest ratios (i.e. football player performing multiple 7-second exercise bouts with 25-35 second rest) to more closely mimic the metabolic demands of their sport. Once multi-directional closed and open chain exercises are tolerated, the athlete's program should be progressed to require the athlete to run up hill in order to improve stride length, and run downhill in order to improve stride frequency as well as to condition the athlete to tolerate frequent, rapid shifts between concentric and eccentric movements. Additionally, the authors propose performing eccentric hamstring exercises at the close of the training session when the athlete is fatigued. Previous researchers have found that strength production in the hamstrings declines with fatigue42, therefore training when fatigued may provide protection against injury.
ANTERIOR CRUCIATE LIGAMENT (ACL) RECONSTRUCTION
Injury to the ACL is a common and significant knee injury, potentially resulting in limitations in range-of-motion, degenerative changes of the knee joint and muscular atrophy.62 Muscular atrophy greater than 20% and strength loss exceeding 30% have been demonstrated strength persisting for several years after surgery.63,64,68–77 Hamstring and gracilis muscle volume deficits of 10% and 30% were found post ACL reconstruction with autologous semitendinosus-gracilis graft.77,78 Amelioration of these deficits continues to be a clinical challenge requiring systematically progressed strengthening protocols that encompass all components of lower extremity function.
High intensity and accelerated intervention programs have long been suggested as optimal and reported as safe following ACL reconstruction.71,79–83 LaStayo et al84 suggested that eccentric training for the quadriceps was more effective in recovery of strength deficits post ACL reconstruction due to this type of training promoting greater changes in neural activation and muscle hypertrophy. Investigation of higher intensity rehabilitation training (producing increasingly greater strain on the ACL graft) versus a program producing minimal strain on the graft found no differences in knee laxity, activity level, function, and patient satisfaction up to 2 years post-operatively.85
Although it was concluded that these higher intensity programs were safe, Beynnon et al85 emphasized use of caution with increasing the frequency and magnitude of quadriceps activity due to concern of increasing anterior knee laxity. Additionally, it has been demonstrated that when applied gradually and progressively, an eccentric (or negative-work) exercise training for the quadriceps is safe for these patients and can be tolerated without damage.84,86–89 Eccentric knee extensor training was purported to be essential for restoration of the functional capacity of the ACL reconstructed knee due to findings of significantly larger concentric and eccentric peak torque deficiencies in the knee extensors as compared to the knee flexors.90
Mikkelsen et al91 compared a closed kinetic chain (CKC) training program versus training with CKC and open kinetic chain (OKC) exercise starting at 6 weeks post ACL reconstruction. Anterior knee laxity (KT-1000 arthrometer), isokinetic concentric and eccentric quadriceps and hamstring muscle torque (isokinetic dynamometry before and six months after surgery), and return to preinjury sports level (questionnaire at an average of 31 months post surgery) were measured in 44 patients with unilateral ACL reconstruction. No significant differences in anterior knee laxity were noted between the groups at six months post surgery. Those performing OKC in addition to CKC increased their quadriceps torque to a significantly greater degree than those performing only CKC exercises. No significant differences were noted between groups for hamstring muscle torque. The number of patients returning to pre-injury sports level participation was greater in the OKC/CKC exercise group than the CKC exercise only group. Additionally, the OKC/CKC exercise group patients returned to this activity level two months earlier than the CKC exercise group. Mikkelsen et al91 concluded that the addition of OKC quadriceps strengthening (both concentric and eccentric) after ACL reconstruction leads not only to a significantly increased number of athletes returning to pre-injury sport level, but the speed at which they attained this level. The benefits of eccentric training is therefore demonstrated in both an OKC and CKC manner versus the traditional thought of OKC training being primarily concentric in nature. Controlled eccentric OKC training is safe and effective for the post ACL reconstruction patient.
Progressive eccentric exercise implemented post ACL reconstruction has demonstrated benefit with respect to volume and cross-sectional area of the quadriceps and gluteus maximus,86,87,89 superior short-term improvement in quadriceps torque,86,87,92 hopping distance and activity level,86,87 and knee flexion/extension range of movement during gait92 compared to a traditional post ACL reconstruction program. Improvements in quadriceps muscle strength and hopping distance also were significantly greater in the eccentric exercise group, as compared to the traditional exercise group, one year post surgery.87
IMPLEMENTATION OF ECCENTRIC TRAINING AFTER ACL RECONSTRUCTION
The research regarding implementation of eccentric training during rehabilitation post ACL reconstruction is quite limited when compared to this type of training during rehabilitation of tendinopathy and muscle strains. As with any eccentric training program, systematic progression of training volume and intensity in the post ACL reconstruction patient is a necessity. Controlled eccentric training has been implemented safely as soon as three weeks post surgery in a modified CKC manner.88 This type of training was implemented on a mechanism similar to a modified ergometer.88 The authors of this review suggest the use of a total gym initially, with progression to a leg press machine, and eventually a squat rack. Both concentric and eccentric muscle training can be performed on each of these machines. Eccentric quadriceps contraction can be emphasized with training on these devices via increasing the knee flexion angle with the surgical lower extremity and straightening the leg (decreasing the knee flexion angle) with the non-surgical lower extremity. When implementing exercise using a squat rack in the later phases of rehabilitation, it is suggested to start with a Smith frame squat rack to limit potential transverse plane compensations on the part of the patient. The use of eccentric training on the non-involved lower extremity is also initially suggested since it has shown indication of being a useful mechanism in improving both the quadriceps muscle strength93 and the quadriceps accelerated reaction time in the surgical lower extremity.94 Table 2 details the specifics of the suggested implementation of a program as a guide to the eccentric component of a comprehensive strengthening program for the post ACL reconstruction patient. Ideally it is suggested that both OKC and CKC strengthening be employed in the rehabilitation program since OKC eccentric and concentric quadriceps strengthening has proven added benefit,91 yet sport related activities are primarily CKC. Although the focus of this commentary is detailing the benefits of eccentric training, it is the suggestion of the authors that this comprehensive approach, including both concentric and eccentric training be considered.
Table 2.
Proposed Eccentric Training Implementation during Post-operative Isolated Unilateral ACL Rehabilitation Program (based on syudies by gerber et al. 2006, 2007, 2009, and Mikkelsen et al. 2000)
| Phase | Description | Intensity (Rate of Perceived Exertion) |
|---|---|---|
| Phase I (Weeks 0-3) | Level I: CKC: Initiation of non-involved leg eccentric training for contralateral effect as early as day 2 post-operative unless restrictions or contraindicated. | Level I: Somewhat hard |
| Phase II (Weeks 3-12) | Level I: CKC: Initiation of eccentric training on total gym at lowest level. Subject lowers themselves down in limited ROM (initially 0-40°) with surgery leg and raises themselves back up to full knee extension with assistance from non-involved leg. ROM (to 90°) and resistance level is progressively increased dependent on patient tolerance and ability. | Level I: progressed from very light-fairly light-somewhat hard-hard |
| Level II: OKC: Approximately 6 weeks post-operatively strengthening initiated from 90° - 45° flexion either isokinetically with low resistance (30°- 90°/sec) or light weight (at mid shin) and repetitions in the range of 20-30. | Level II: progressed from very, very light-fairly light-somewhat hard-hard if tolerated | |
| Phase III (Weeks 12+) | CKC: leg press-resistance of moderate level (single leg): eccentric lowering with involved leg, followed by concentric knee straightening with non-involved leg. ROM should be in short range to start (0-30°) and systematically increased no greater than 90°. Smith frame squat rack-bilateral squats with eccentric emphasis on involved leg and concentric phase assistance by non-involved leg as with leg press. Smith frame-reverse lunges can be initiated here if patient tolerates. Eccentric phase with involved leg; patient then locks bar into frame, and bar is raised to starting position using both legs. Level I: CKC: leg press-moderate to heavy level resistance with technique as in phase II. ROM should be 0-90° unless otherwise contraindicated or not tolerated. Squat rack-bilateral squats as done in Smith frame in phase II. | Level I: progressed from somewhat hard to hard as tolerated. |
| OKC: Eccentric isokinetic training at speeds of 30°-240° or with weight (at mid shin) with high repetition range (30-60). | ||
| Level II: CKC: Squat rack-single leg lunges and reverse lunges progressed in intensity and ROM to 90° if not already achieved (Smith frame squat rack only if necessary)-eccentric emphasis only. | Level II: progressed from somewhat hard to hard as tolerated. | |
| Squat rack-single leg squats as done with bilateral squats in Level I. |
Table 1.
Nircahl's Stages of Tendinopathy16
| Stage | Diagnosis | Macroscopic Pathology | Histologic Findings | Clinical Signs |
|---|---|---|---|---|
| 0 | Healthy | No inflammation | Organized collagen, absent blood cells | Firm tendon, not painful, absent swelling, normal temperature |
| I | Acute tendinitis | Symptomatic tendon degeneration, Increased cellularity; vascular disruption; inflammation of paratenon | Degenerative changes w/ microtears, inflammatory cells in paratenon; focal collagen disorientation | Acute swelling, pain, local tenderness, warmth, dysfunction |
| II | Chronic tendinitis | Increased tendon degeneration and vascularity | Greater evidence of microtears, increased levels of collagen disorientation in tissue hypercellularity | Chronic pain w/ tenderness, increased dysfunction, person voluntarily unloads structure |
| III | Tendinosis | Intratendinous degeneration due to microtrauma, cellular/tissue aging; vascular compromise | Increased celluarity, neovascularization, focal necrosis, collagen disorganization and disorientation | Palpable tendon enlargement, swelling of tissues, increased dysfunction w/ or w/o pain, tendon sheath may be swollen |
| IV | Rupture | Tendon failure | Complete disruption of fibers | Weak and painful muscle testing, inability to move affected joint, + clinical tests for tendon disruption |
CONCLUSION
Eccentric exercise offers promise as an effective means to manage a host of common conditions encountered by the sports rehabilitation specialist. This promise is based upon both muscle and tendon physiology as they relate to performance. While evidence regarding the positive role of the varied uses of eccentrics in training, and prevention continues to emerge, it is but one component of a successful rehabilitation plan. Soft tissue mobilization, pain modulation, activity modification, patient education, biomechanical assessment, risk factor modification, and regional interdependence each play an integral role in the rehabilitation process. The challenge for the sports physical therapist is to clearly describe the ideal time to start eccentrics in the rehabilitation process, as well as how to manipulate training variables (load, volume, intensity, frequency) to provide a safe, yet progressive stimulus for eventual return to sport.
REFERENCES
- 1. Hill AV. The heat or shortening and the dynamic constants of muscle. Proc Roy Soc B. 1938;126:136–195 [Google Scholar]
- 2. Leadbetter WB. Cell-matrix response in tendon injury. Clin Sports Med. 1992;11:533–578 [PubMed] [Google Scholar]
- 3. Mafulli N, Wong J, Almekinders LC. Types and epidemiology of tendinopathy. Clin Sports Med. 2003;22:675–692 [DOI] [PubMed] [Google Scholar]
- 4. Maganaris CN, MV Narici, LC Almekinders, Maffulli N. Biomechanics and Pathophysiology of overuse tendon injuries: ideas on insertional tendinopathy. Sports Med. 2004;34:1005–1017 [DOI] [PubMed] [Google Scholar]
- 5. Abbott BC, Bigland B, Ritchie JM. The physiological cost of negative work. J Physiol. 1952;117:380–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Abbott BC, B Bigland. The effects of force and speed changes on the rate of oxygen consumption during negative work. J Physiol. 1953;120:319–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Katz B. The relation between force and speed in muscular contraction. J Physiol. 1939;96:45–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wilkie DR. Heat, work, and phosphorylcreatine break-down in muscle. J Physiol. 1968;195:157–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wilkie DR. The relation between force and velocity in human muscles. J Physiol. 1949;110:249–280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Curtin NA, Davies RE. Chemical and mechanical changes during stretching of activated frog muscle. Cold Spring Harb Symp Quant Biol. 1970;37:619–626 [Google Scholar]
- 11. Bigland-Ritchie B, Woods JJ. Integrated electromyogram and oxygen uptake during positive and negative work. J Physiol. 1976;260:267–277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Khan KM, Scott A. Mechanotherapy: how physical therapists' prescription of exercise promotes tissue repair. Br J Sports Med. 2009;43:247–251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sharma P, Maffulli N. Biology of tendon injury: healing, modeling, and remodeling. J Musculoskelet Neuronal Interact. 2006;6:181–190 [PubMed] [Google Scholar]
- 14. Lian OB, Engebretsen L, Bahr R. Prevalence of jumper's knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med. 2005;33:561–567 [DOI] [PubMed] [Google Scholar]
- 15. Williams JG. Achilles tendon lesions in sport. Sports Med. 1986;3:114–135 [DOI] [PubMed] [Google Scholar]
- 16. Alfredson H, T Pietila, P Jonsson, Lorentzon R. Heavy-load eccentric calf muscle training for treatment of chronic Achilles tendinosis. Am J Sports Med. 1998;26:360–366 [DOI] [PubMed] [Google Scholar]
- 17. Shalabi A, M Kristoffersen-Wilberg, L Svensson, P Aspelin, Movin T. Eccentric training of the gastrocnemius-soleus complex in chronic Achilles tendinopathy results in decreased tendon volume and intratendinous signal as evaluated by magnetic resonance imaging. Am J Sports Med. 2004;32:1286–1296 [DOI] [PubMed] [Google Scholar]
- 18. Langberg H, H Ellingsgaard, T Madsen, J Jansson, SP Magnusson, P Aagaard, Kjaer M. Eccentric rehabilitation exercise increases peritendinous type I collagen synthesis in humans with Achilles tendinosis. Scand J Med Sci Sports. 2007;17:61–66 [DOI] [PubMed] [Google Scholar]
- 19. Ohberg L, R Lorentzon, Alfredson H. Eccentric training in patients with chronic Achilles tendinosis: normalized tendon structure and decreased thickness at follow-up. Br J Sports Med. 2004;38:8–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mahieu N, McNair P, Cools A, et al. Effect of eccentric training on the plantar flexor muscle-tendon tissue properties. Med Sci Sports Exerc. 2008;40:117–123 [DOI] [PubMed] [Google Scholar]
- 21. Jonsson P, Alfredson H. Superior results with eccentric compared to concentric quadriceps training in patients with jumper's knee: a prospective randomised study. Br J Sports Med. 2005;39:847–850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Young MA, JL Cook, CR Purdam, ZS Kiss, Alfredson H. Eccentric decline squat protocol offers superior results at 12 months compared with traditional eccentric protocol for patellar tendinopathy in volleyball players. Br J Sports Med. 2005;39:102–105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Visnes H, Hoksrud A, Cook J, et al. No effect of eccentric training on jumper's knee in volleyball players during the competitive season: a randomized controlled trial. Clin J Sport Med. 2005; 15(4):227–234 [DOI] [PubMed] [Google Scholar]
- 24. Wasielewski NJ, Kotsko DM. Does eccentric exercise reduce pain and improve strength in physically active adults with symptomatic lower extremity tendinosis? A systematic review. J Ath Train. 2007;42:409–421 [PMC free article] [PubMed] [Google Scholar]
- 25. Kingma JJ, de Knikker R, HM Wittink, Takken T. Eccentric overload training in patients with chronic Achilles tendinopathy: a systematic review. Br J Sports Med 2007; 41: e3 Epub 11 Oct 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kibler WB, TJ Chandler, Pace BK. Principles of rehabilitation after chronic tendon injuries. Clin Sports Med. 1992;11:661–671 [PubMed] [Google Scholar]
- 27. Curwin SL. Tendon injuries: Pathophysiology and treatment. In: Athletic Injuries and Rehabilitation. Zachazewski J, Magee DJ, Quillen WS, ed. Philadelphia, PA: WB Saunders Co. 27–54, 1996 [Google Scholar]
- 28. Ratamess NA, Alvar BA, Evetoch TK, et al. Progression models in resistance training for healthy adults: ACSM Position Stand. Med Sci Sports Exerc. 2009; 41(3):687–708 [DOI] [PubMed] [Google Scholar]
- 29. Thacker SB, J Gilchrist, D.F Stroup, Kinzey CD., Jr The impact of stretching on sports injury risk: a systematic review of literature. Med Sci Sports Exerc. 2004;36:371–378 [DOI] [PubMed] [Google Scholar]
- 30. Hibbert O, Cheong K, Grant A, et al. A systematic review of the effectiveness of eccentric hamstring strength training in the prevention of hamstring muscle strains in otherwise healthy individuals. North Am J Sports Phys Ther. 2008; 3(2):67–81 [PMC free article] [PubMed] [Google Scholar]
- 31. Croisier JL, Forthomme B, Namurois MH, et al. Hamstring muscle strain recurrence and strength performance disorders. Am J Sports Med. 2002;30:199–203 [DOI] [PubMed] [Google Scholar]
- 32. Agre JC. Hamstring injuries: proposed aetiological factors, prevention, and treatment. Sports Med. 1985;2:21–33 [DOI] [PubMed] [Google Scholar]
- 33. Clanton TO, Coupe KJ. Hamstring strain in athletes: diagnosis and treatment. J Am Acad Orthop Surg. 1998;6:237–248 [DOI] [PubMed] [Google Scholar]
- 34. Ekstrand J, Gillquist J. Soccer injuries and their mechanisms: a prospective study. Med Sci Sports Exerc. 1983;15:267–270 [DOI] [PubMed] [Google Scholar]
- 35. Small K, McNaughton L, Greig M, Lovell R. Effect of timing of eccentric hamstring strengthening exercises during soccer training: implications for muscle fatigability. J Strength Cond Res. 2009;23:1077–1083 [DOI] [PubMed] [Google Scholar]
- 36. Brughelli M, Cronin J. Preventing hamstring injuries in sport. Strength Cond J. 2008;30:55–64 [Google Scholar]
- 37. Woods C, Hawkins R, Maltby S. The Football Association Medical Research Programme: an audit of injuries in professional football – analysis of hamstring injuries. Br J Sports Med. 2004;38:36–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Heiderscheit BC, Sherry MA, Silder A, et al. Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. J Orthop Sports Phys Ther. 2010;40:67–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sherry MA, Best TM. A comparison of two rehabilitation programs in the treatment of acute hamstring strains. J Orthop Sports Phys Ther. 2004;34:116–125 [DOI] [PubMed] [Google Scholar]
- 40. Petersen J, Holmich P. Evidence based prevention of hamstring injuries in sport. Br J Sports Med. 2005;39:319–323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Orchard JW, Best TM. The management of muscle strain injuries: an early return versus the risk of recurrence. Clin J Sports Med. 2002;12:3–5 [DOI] [PubMed] [Google Scholar]
- 42. Greig M, Siegler JC. Soccer-specific fatigue and eccentric hamstrings muscle strength. J Ath Train. 2009;44:180–184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Friden J, Lieber R. Eccentric exercise-induced injuries to contractile and skeletal muscle fibre components. Acta Physiol Scand. 2001;171:321–326 [DOI] [PubMed] [Google Scholar]
- 44. Sugiura Y, Saito T, Sakuraba K, et al. Strength deficits identified with concentric action of the hip extensors and eccentric action of the hamstrings predispose to hamstring injury in elite sprinters. J Orthop Sports Phys Ther. 2008;38:457–464 [DOI] [PubMed] [Google Scholar]
- 45. Stanton P, Purdham C. Hamstring injuries in sprinting: the role of eccentric exercise. J Orthop Sports Phys Ther. 1989;10:343–349 [DOI] [PubMed] [Google Scholar]
- 46. Thelen D, Chumanov D, Hoerth M. Hamstring muscle kinematics during treadmill sprinting. Med Sci Sports Exerc. 2005;38:108–114 [DOI] [PubMed] [Google Scholar]
- 47. Kouloris G, Connell D. Evaluation of hamstring muscle complex following acute injury. Skeletal Radiol. 2003;32:582–589 [DOI] [PubMed] [Google Scholar]
- 48. Small K, McNaughton L, Greig M, et al. Effect of timing of eccentric hamstring strengthening exercises during soccer training: implications for muscle fatiguability. J Strength Cond Res. 2009; 23(4):1077–1083 [DOI] [PubMed] [Google Scholar]
- 49. Greig M. The influence of soccer-specific fatigue on peak isokinetic torque production of the knee flexors and extensors. Am J Sports Med. 2008;36:1403–1409 [DOI] [PubMed] [Google Scholar]
- 50. Rahnama N, Reilly T, Les A, Graham-Smith P. Muscle fatigue induced by exercise simulating the work rate of competitive soccer. J Sports Sci. 2003;21:933–942 [DOI] [PubMed] [Google Scholar]
- 51. Orchard J, Marsden J, Lord S, Garlick D. Preseason hamstring muscle weakness associated with hamstring muscle injury in Australian footballers. Am J Sports Med. 1997;25:81–85 [DOI] [PubMed] [Google Scholar]
- 52. Askling C, Karlsson J, Thorstensson A. Hamsring injury occurrence in elite soccer players after preseason strength training with eccentric overload. Scand J Med Sci Sports. 2003;13:244–250 [DOI] [PubMed] [Google Scholar]
- 53. Arnason A, Andersen TE, Holme I, et al. Prevention of hamstring strains in elite soccer: an intervention study. Scand J Med Sci Sport. 2008; 18(1): 40–48 [DOI] [PubMed] [Google Scholar]
- 54. Gabbe BL, Branson R, Bennell KL. A pilot randomized controlled trial of eccentric exercise to prevent hamstring injuries in community-level Australian football. J Sci Med Sport. 2006;9:103–109 [DOI] [PubMed] [Google Scholar]
- 55. Brooks J, Fuller C, Kemp S, Reddin D. Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. Am J Sports Med. 2006;34:1297–1306 [DOI] [PubMed] [Google Scholar]
- 56. Holcomb WR, Rubley MD, Lee HJ, Guadagnoli MA. Effect of hamstring-emphasized resistance training on hamstring:quadriceps strength ratios. J Strength Cond Res. 2007;21:41–47 [DOI] [PubMed] [Google Scholar]
- 57. Aagaard P, Simonsen SP, Magnusson B, et al. A new concept for isokinetic hamstring:quadriceps muscle strength ratio. Am J Sports Med. 1998;26:231–237 [DOI] [PubMed] [Google Scholar]
- 58. Aagaard P, Simonsen EB, Trolle M, et al. Isokinetic hamstring/quadriceps strength ratio: influence from joint angular velocity, gravity correction, and contraction mode. Acta Physiol Scand. 1995;154:421–427 [DOI] [PubMed] [Google Scholar]
- 59. Comfort P, Green CM, Matthews M. Training considerations after hamstring injury in athletes. Strength Cond J. 2009;31:68–74 [Google Scholar]
- 60. Clark R, Bryant A, Clugan J, Hartley B. The effects of hamstring strength training on dynamic jumping performance and isokinetic strength parameters. Phys Ther Sport. 2005;6:67–73 [Google Scholar]
- 61. Arnold JA, Coker TP, Heaton IM, Park JP, Harris WP. Natural history of anterior cruciate ligament tears. Am J Sports Med. 1979;7:305–313 [DOI] [PubMed] [Google Scholar]
- 62. Elmqvist LG, Lorentzon R, Johansson C, Langstrom M, Fagerlund M, Fugl-Meyer AR. Knee extensor muscle function before and after reconstruction of anterior cruciate ligament tear. Scand J Rehabil Med. 1989;21:131–139 [PubMed] [Google Scholar]
- 63. Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31:564–573 [DOI] [PubMed] [Google Scholar]
- 64. Meighan AA, Keating JF, Will E. Outcome after reconstruction of the anterior cruciate ligament in athletic patients. A comparison of early versus delayed surgery. J Bone Joint Surg Br. 2003;85:521–524 [DOI] [PubMed] [Google Scholar]
- 65. Grant JA, Mohtadi NG, Maitland ME, Zernicke RF. Comparison of home versus physical therapy-supervised rehabilitation programs after anterior cruciate ligament reconstruction: a randomized clinical trial. Am J Sports Med. 2005;33:1288–1297 [DOI] [PubMed] [Google Scholar]
- 66. Risberg MA, Holm I, Steen H, Eriksson J, Ekeland A. The effect of knee bracing after anterior cruciate ligament reconstruction. A prospective, randomized study with two years' follow-up. Am J Sports Med. 1999;27:76–83 [DOI] [PubMed] [Google Scholar]
- 67. Anderson JL, Lamb SE, Barker KL, Davies S, Dodd CA, Beard DJ. Changes in muscle torque following anterior cruciate ligament reconstruction: a comparison between hamstrings and patella tendon graft procedures on 45 patients. Acta Orthop Scand. 2002;73:546–552 [DOI] [PubMed] [Google Scholar]
- 68. Arangio GA, Chen C, Kalady M, Reed JF., 3rdThigh muscle size and strength after anterior cruciate ligament reconstruction and rehabilitation. J Orthop Sports Phys Ther. 1997;26:238–243 [DOI] [PubMed] [Google Scholar]
- 69. Bach BR, Jr, Jones GT, Sweet FA, Hager CA. Arthroscopy-assisted anterior cruciate ligament reconstruction using patellar tendon substitution. Two- to four-year follow-up results. Am J Sports Med. 1994;22:758–767 [DOI] [PubMed] [Google Scholar]
- 70. Ejerhed L, Kartus J, Sernert N, Kohler K, Karlsson J. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction? A prospective randomized study with a two-year follow-up. Am J Sports Med. 2003;31:19–25 [DOI] [PubMed] [Google Scholar]
- 71. Eriksson K, Hamberg P, Jansson E, Larsson H, Shalabi A, Wredmark T. Semitendinosus muscle in anterior cruciate ligament surgery: morphology and function. Arthroscopy. 2001;17:808–817 [DOI] [PubMed] [Google Scholar]
- 72. Hamada M, Shino K, Horibe S, Mitsuoka T, Miyama T, Shiozaki Y, Mae T. Single- versus bi-socket anterior cruciate ligament reconstruction using autogenous multiple-stranded hamstring tendons with EndoButton femoral fixation: a prospective study. Arthroscopy. 2001;17:801–807 [DOI] [PubMed] [Google Scholar]
- 73. Jansson KA, Linko E, Sandelin J, Harilainen A. A prospective randomized study of patellar versus hamstring tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31:12–18 [DOI] [PubMed] [Google Scholar]
- 74. Jarvela T, Kannus P, Latvala K, Jarvinen M. Simple measurements in assessing muscle performance after an ACL reconstruction. Int J Sports Med. 2002;23:196–201 [DOI] [PubMed] [Google Scholar]
- 75. Mattacola CG, Perrin DH, Gansneder BM, Gieck JH, Saliba EN, McCue FC., 3rdStrength, functional outcome, and postural stability after anterior cruciate ligament reconstruction. J Athl Train. 2002;37:262–268 [PMC free article] [PubMed] [Google Scholar]
- 76. Rosenberg TD, Franklin JL, Baldwin GN, Nelson KA. Extensor mechanism function after patellar tendon graft harvest for anterior cruciate ligament reconstruction. Am J Sports Med. 1992;20:519–526 [DOI] [PubMed] [Google Scholar]
- 77. Williams GN, Snyder-Mackler L, Barrance PJ, Axe MJ, Buchanan TS. Muscle and tendon morphology after reconstruction of the anterior cruciate ligament with autologous semitendinosus-gracilis graft. J Bone Joint Surg Am. 2004;86:1936–1946 [DOI] [PubMed] [Google Scholar]
- 78. Irie K, Tomatsu T. Atrophy of semitendinosus and gracilis and flexor mechanism function after hamstring tendon harvest for anterior cruciate ligament reconstruction. Orthopedics. 2002;25:491–495 [DOI] [PubMed] [Google Scholar]
- 79. Bynum EB, Barrack RL, Alexander AH. Open versus closed chain kinetic exercises after anterior cruciate ligament reconstruction. A prospective randomized study. Am J Sports Med. 1995;23:401–406 [DOI] [PubMed] [Google Scholar]
- 80. Haggmark T, Eriksson E. Cylinder or mobile cast brace after knee ligament surgery. A clinical analysis and morphologic and enzymatic studies of changes in the quadriceps muscle. Am J Sports Med. 1979;7:48–56 [DOI] [PubMed] [Google Scholar]
- 81. Noyes FR, Mangine RE, Barber S. Early knee motion after open and arthroscopic anterior cruciate ligament reconstruction. Am J Sports Med. 1987;15:149–160 [DOI] [PubMed] [Google Scholar]
- 82. Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. 1990;18:292–299 [DOI] [PubMed] [Google Scholar]
- 83. Shelbourne KD, Trumper RV. Preventing anterior knee pain after anterior cruciate ligament reconstruction. Am J Sports Med. 1997;25:41–47 [DOI] [PubMed] [Google Scholar]
- 84. LaStoya PC, Woolf JM, Lewek MD, Snyder-Mackler L, Reich T, Lindstedt SL. Eccentric muscle contractions: their contribution to injury, prevention, rehabilitation and sport. J Orthop Sports Phys Ther. 2003;33:557–571 [DOI] [PubMed] [Google Scholar]
- 85. Beynnon BD, Uh BS, Johnson RJ, et al. Rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind comparison of programs administered over 2 different time intervals. Am J Sports Med. 2005;33:347–359 [DOI] [PubMed] [Google Scholar]
- 86. Gerber JP, Marcus RL, Dibble LE, Greis PE, Burks RT, Lastoyo PC. Safety, feasibility, and efficacy of negative work exercise via eccentric muscle activity following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2007;37(1):10–18 [DOI] [PubMed] [Google Scholar]
- 87. Gerber JP, Marcus RL, Dibble LE, Greis PE, Burks RT, LaStoyo PC. Effects of early progressive eccentric exercise on muscle size and function after anterior cruciate ligament reconstruction: a 1-year follow-up study of a randomized controlled trial. Phys Ther. 2009;89:51–59 [DOI] [PubMed] [Google Scholar]
- 88. Gerber JP, Marcus RL, Dibble LE, Greis PE, Burks RT, LaStoyo PC. Effects of early progressive eccentric exercise on muscle structure after anterior cruciate ligament reconstruction. J Bone Joint Surg (Am). 2007; 89-A(3):559–570 [DOI] [PubMed] [Google Scholar]
- 89. Gerber JP, Marcus RL, Dibble LE, Greis PE, LaStoyo PC. Early application of negative work via eccentric ergometry following anterior cruciate ligament reconstruction: a case report. J Orthop Sports Phys Ther. 2006;36(5):298–307 [DOI] [PubMed] [Google Scholar]
- 90. Yoon T, Hwang J. Comparison of eccentric and concentric isokinetic exercise testing after anterior cruciate ligament reconstruction. Yonsei Med J. 2000;41:584–592 [DOI] [PubMed] [Google Scholar]
- 91. Mikkelsen C, Werner S, Eriksson E. Closed kinetic chain alone compared to combined open and closed kinetic chain exercises for quadriceps strengthening after anterior cruciate ligament reconstruction with respect to return to sports: a prospective matched follow-up study. Knee Surg Sports Traumatol Arthrosc. 2000;8:337–342 [DOI] [PubMed] [Google Scholar]
- 92. Coury HJCG, Brasileiro JS, Salvini TF, Poletto PR, Carnaz L, Hansson GA. Change in knee kinematics during gait after eccentric isokinetic training for quadriceps in subjects submitted to anterior cruciate ligament reconstruction. Gait Posture. 2006;24:370–374 [DOI] [PubMed] [Google Scholar]
- 93. Papandreou M, Paaioannou N, Antonogiannakis E, Zeeris H. The effect of cross exercise on quadriceps strength in different knee angles after the anterior cruciate ligament reconstruction. Br J Biometricity. 2007;1:123–137 [Google Scholar]
- 94. Papandreou M, Billis EV, Antonogiannakis EM, Papaioannou NA. Effect of cross exercise on quadriceps acceleration reaction time and subjective scores (Lysholm questionnaire) following anterior cruciate ligament reconstruction. J Orthop Surg Res. 2009;4:2–10 [DOI] [PMC free article] [PubMed] [Google Scholar]