Abstract
The aim of this study is to examine how physicians use clinical practice guidelines that call for routine HIV screening in a general adolescent medicine clinic and to determine how adolescent patients respond to routine screening. Physicians offered screening to 116 of 217 patients (53%) aged 13-21 who completed a survey. Physicians’ offers conformed to the latest Centers for Disease Control and Prevention (CDC) guidelines with 73% of patients because some patients not offered a test had been screened within the last year. Physicians were three times more likely (OR = 3.0; 95% CI = 1.3-6.8) to offer HIV screening to sexually active adolescents than to adolescents who reported no sexual history. Adolescent medicine physicians and their patients endorse the idea of routine screening as embodied in the latest CDC recommendations, but adolescents with no sexual history are less likely than other adolescents to accept screening when it is offered and to support a clinic policy of routine screening. Both physicians and their adolescent patients continue to test based on risk assessments.
In 2006 the U.S. Centers for Disease Control and Prevention (CDC) released revised recommendations for HIV testing in health care settings in the United States (Branson et al., 2006). The recommendations, which are also clinical practice guidelines, call for health care providers in public and private health care facilities to screen all patients between the ages of 13 and 64 for HIV without regard to risk unless the patient opts out of testing. Patients at “known risk” for HIV are to be screened at least annually. The recommendations also call for measures to streamline the screening process. The CDC suggests that separate, written consent for HIV testing and prevention counseling should no longer be mandated as part of the screening process.
Researchers and practitioners have argued that the roughly 250,000 Americans living with HIV without knowledge of their serostatus—an estimated 25% of all Americans with HIV—represent an obstacle to HIV prevention efforts (Duran, Beltrami, Stein, Voetsch, & Branson,2006). The proportion of people living with HIV who are unaware of their sero-status is higher among adolescents than in the total population (Rotheram-Borus & Futterman, 2000), making screening programs for adolescents critical to the overall effort to prevent the spread of HIV. Screening programs in which people learn their HIV status are expected to lead to behavior change among those who test positive and to reductions in the HIV transmission rate (Holtgrave & Anderson, 2004; Marks, Crepaz, Senterfitt, & Janssen, 2005). Getting people diagnosed with HIV on antiretroviral therapies is also expected to reduce the HIV transmission rate by reducing viral loads and infectivity (Fauci, 2007).
In this article we examine how physicians in a general adolescent medicine clinic screen patients for HIV and how adolescents respond to routine screening. We focus on physicians’ screening practices because previous studies suggest that not being offered a test for HIV is one of the major reasons adolescents cite for not having been tested (Goodman, Tipton, Hecht, & Chesney, 1994; Peralta, Deeds, Hipszer, & Ghalib, 2007; Samet, Winter, Grant, & Hingson, 1997). Not much is known about how physicians use clinical practice guidelines for routine HIV screening (Bernstein, Begier, Burke, Karpati, & Hogben, 2008). In many states the implementation of routine screening, following the CDC recommendations or some other set of guidelines, has lagged, as legislative changes and changes in organizational procedures required to implement routine screening are put in place. One study with adolescent patients in an urban, pediatric emergency department in Tennessee, where there were no legislative hurdles to the implementation of routine screening, showed that 78% of health care providers were unaware of the CDC's revised testing guidelines, 37% of patients were offered opt-out screening, and 13% of patients offered screening opted out (Minniear et al., 2009). Another recent study suggests that internal medicine physicians are mostly unaware of the guidelines and continue to screen patients based on an assessment of their risk (Jain, Wyatt, Burke, Sepkowitz, & Begier, 2009). In general, research on clinical practice guidelines suggests that guidelines have a limited effect on physician behavior (Baiardini, Bradio, Bonini, Compalati, & Canonica, 2009; Cabana et al., 1999; Francke, Smit, deVeer, & Mistiaen, 2008). The aim of this study is, then, to determine how physicians and their adolescent patients in a general adolescent medicine clinic respond to calls for routine screening and to consider the implications of their responses in light of the latest CDC recommendations and the movement to introduce routine screening protocols in health care settings around the country.
METHODS
This study was carried out in a general adolescent medicine clinic that is part of a major teaching hospital in Baltimore, Maryland. Baltimore is a city with one of the highest rates of AIDS in the country (CDC, 2009). The adolescent medicine clinic is located in an area of the city with high HIV prevalence.
A patient survey was conducted from January through May of 2008, in the months immediately preceding legislative changes that brought the state into close alignment with the CDC recommendations. The patient survey followed on the heels of a quality improvement program in the clinic that encouraged physicians to offer screening to all of their patients in anticipation of state-wide policy changes. As part of the quality improvement program, physicians were provided with copies of the CDC recommendations as well as skills training in HIV counseling, testing, and referral. At the time the patient survey was conducted, both written consent for HIV testing and pretest and posttest prevention counseling were still mandated. The surveys thus reflect physician testing practices prior to the implementation of streamlined screening protocols but during a period in which universal screening was nonetheless encouraged.
Adolescents 13 years of age and older who were HIV-negative and attending the clinic for nonacute care were eligible to participate in the patient survey. Research assistants screened patients for eligibility. They obtained informed consent from adolescents who agreed to complete the survey and from a parent or guardian when the adolescent was an accompanied minor. The study protocol and procedures were approved by the institutional review board (IRB) at the Johns Hopkins School of Public Health. Adolescents were provided with a $10 gift card for completing the survey.
The patient survey was self-administered and was completed in a private examination room without accompanying adults present. The survey included approximately 30 questions, regrouped under three broad topic areas: (a) standard risk assessment measures, including the patient's sexual history; (b) history of HIV testing; and (c) attitudes toward routine HIV testing. Risk assessment measures were modeled after the CDC's (2006) Comprehensive Risk and Counseling Services Guide, and included a question about whether the adolescent had ever had sex as well as questions about numbers of lifetime partners and partners in the last 3 months; frequency of condom use, history of pregnancy (for females), sexually transmitted infections (STIs), same-sex relationships, and sex with someone who had injected drugs. The survey included multiple questions related to patients’ history of HIV testing, including questions about whether the patient had ever been tested for HIV, time since the last HIV test for those who had previously been tested, the reason for the last HIV test; the total number of times tested, and the frequency of testing. Adolescents’ attitudes toward routine screening were assessed on the basis of three questions, including questions to know whether adolescents thought testing should be a “standard” part of care (“just like taking your blood pressure or checking your weight”), something that everyone who comes to the clinic does, and something for which patients should sign a consent form. Following the clinical care visit, adolescent patients were asked to record whether their physician offered them an HIV test during the visit. If applicable, they were also asked whether they agreed to be tested.
We examined how physicians screened their adolescent patients for HIV by comparing adolescents who were offered a test with those not offered a test on a range of demographic and behavioral measures. These included age, gender, type of services sought at the clinic, history of sexual activity, lifetime number of sexual partners, history of an STI, previous HIV test, and number of previous HIV tests. We also compared subgroups of adolescents—for example, those not offered screening for whom screening would be indicated under the CDC recommendations, or those offered screening who refused screening—and the general patient sample on these measures. Variables associated with being offered an HIV test at a level of statistical significance of P < .10 were entered into a multiple logistic regression model to identify factors independently associated with being offered a test.
We conducted interviews with physicians in 2008 and 2009, over the period when clinic procedures were changing in response to the CDC recommendations and legislative changes, to help interpret and explain the survey findings. Through letters and follow-up e-mails, we invited 51 clinicians who were authorized to order HIV tests in the adolescent medicine clinic to participate in an interview. All 20 of the residents and preceptors who responded to our invitation were interviewed in an office at the clinic or in another location on the hospital campus. Interviews lasted 45 minutes to 1 hour and were recorded and transcribed. The interview guide covered four broad topic areas: (a) how physicians approached adolescent patients about HIV testing; (b) the training, preparation, and support physicians received to implement routine testing; (c) how clinic policies, including auditing and oversight procedures, affected physicians’ decisions to order HIV tests; and (d) what public health outcomes physicians anticipated would follow from the move to routine testing. The emphasis on physician education and training in the clinic meant that residents, who made up the bulk of the physician sample, were able to report on clinical practice but also on the pedagogical moments in which they learned about HIV screening from their preceptors.
For the purposes of this article, analysis of the interview data consisted of reviewing the transcripts for text passages that help to interpret and explain the physician and patient testing patterns we found in the patient survey (Steckler, McLeroy, Goodman, Bird, & McCormick, 1992). We looked, for example, at text passages where physicians described the process of deciding whether to screen an adolescent patient and at the reasons physicians provided for not screening a particular patient. We produced analytic memos that were summaries of broad themes from the interviews—such as triggers for screening or how physicians manage uncertainty in the context of adolescents’ self-reports. Rather than presenting a comprehensive analysis of the interview data, in this article we focus on themes in the interviews that were directly related to the findings of the patient survey.
RESULTS
A total of 217 adolescents completed the patient survey. The sample was predominantly African American (91%) and female (72%). Patient ages ranged from 13 to 21 with a mean age of 16.
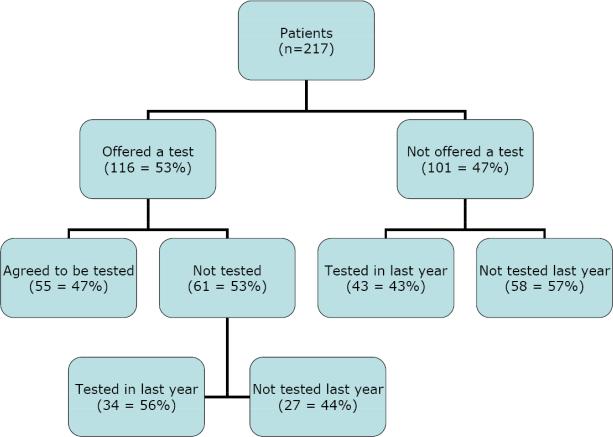
Based on patient reports, physicians offered HIV screening to 116 patients (53%) (Figure 1). An additional 43 patients not offered screening had been tested within the past year. Under the CDC guidelines, physicians might elect not to re-screen these patients, because the guidelines call for repeat screening of persons with known risk at least annually. Therefore, physicians’ actions could be said to be in line with the CDC guidelines with 159 of 217 patients, or with 73% of the patient sample.
FIGURE 1.
A schematic representation of physician screening practices
Whether an adolescent patient reported ever having sex was the only significant predictor of physician screening practices in a multiple variable regression model. Physicians were three times more likely to offer HIV screening to adolescents who reported some previous sexual activity than to adolescents who reported no sexual history (odds ratio [OR] = 3.0; 95% confidence interval [CI] = 1.3-6.8) after controlling for age, lifetime number of sexual partners, number of partners in the past 3 months, history of HIV testing, and history of an STI.
Physicians did not offer testing to 101 adolescents, including 58 adolescents (27% of the sample) who should have been offered screening under the CDC recommendations because they had never been screened or had not been screened within the last year. Bivariate analyses comparing this subsample of patients with the rest of the patient sample, whose screening was consistent with the CDC guidelines, show that in addition to being less likely to have a sexual history, these patients also tended to be younger than patients offered screening, male, without any history of HIV testing, and in the clinic for services other than reproductive health services (Table 1).
TABLE 1.
Patients Not Offered Screening and Not Screened in Last Year Compared with All Other Patients
| Variable | Not Offered Test and Not Tested in Last Year (n = 58) | All Other Patients (n = 159) | p Value |
|---|---|---|---|
| Ever had sex | 26% | 82% | <.001 |
| Mean age | 15.1 years | 16.8 years | <.001 |
| Male | 41% | 23% | .009 |
| Previously tested for HIV | 2% | 75% | <.001 |
| Seeking reproductive health services | 9% | 22% | <.001 |
Even as physicians offered HIV screening to slightly more than half of their adolescent patients (n = 116, 53%), most adolescents offered screening (n = 61; 53%) decided not to be screened as part of their clinic visit (see Figure 1). Adolescents who did not accept screening when it was offered and had not been tested in the past year (n = 27) tended to have no sexual history and to be younger than patients who were screened, without any history of HIV testing, and in the clinic for reasons other than reproductive health services (Table 2). This means that they were similar in profile to adolescents who were not offered screening.
TABLE 2.
Comparison of Patients Offered Test, Not Tested, and Not Tested in Last Year With Others in Compliance With CDC Recommendations
| Variable | Offered Test, Not Tested, and Not Tested in Last Year (n = 27) | All Other Patients Offered Testing or Tested Within Last Year (n = 132) | p Value |
|---|---|---|---|
| Ever had sex | 48% | 89% | <0.001 |
| Mean age | 16.1 years | 17.0 years | 0.03 |
| Previously tested for HIV | 22% | 86% | <0.001 |
| Seeking reproductive health services | 4% | 20% | 0.04 |
| Think routine screening should be adopted | 63% | 92% | 0.001 |
A strong majority of adolescents expressed a favorable view of routine screening. However, adolescents who had never had sex, who made up one third of the patient sample (n = 71; 32.7%), were less likely than other adolescents not only to be offered screening but to accept screening when it was offered (Table 3). Adolescents who had never had sex were also less likely than other adolescents to endorse the adoption of routine screening policies at the clinic as measured by affirmative responses to questions such as “Do you think everyone should be tested for HIV when they come to the clinic?” and “Do you think HIV testing should be a standard part of care, just like taking your blood pressure or checking your weight?”
TABLE 3.
Comparison of Screening Attitudes and Practices Among Adolescents With And Without Any Sexual History
| Variable | Ever Had Sex (n = 146) | Never Had Sex (n = 71) | p Value |
|---|---|---|---|
| Offered HIV screening | 65.1% | 29.6% | <.001 |
| Screened at office visit (entire sample) | 38.4% | 5.6% | <.001 |
| Offered and accepted screening (n = 116) | 53.7% | 19.0% | .004 |
| Thinks everyone should be tested for HIV when they come to the clinic | 87.7% | 70.4% | 0.002 |
| Thinks HIV testing should be a standard part of care | 84.1% | 73.2% | .057 |
In interviews, physicians were unanimous in their endorsement of the CDC recommendations when those recommendations were considered in the abstract. However, when physicians spoke about adolescents who reported no sexual history, they diverged in their views of whether the recommendations should be applied. Some physicians worried that offering HIV screening suggested doubt or skepticism with regard to patients’ self-reports, and they were hesitant to offer screening if they felt it would breach the patient-provider relationship. Other physicians described drawing from multiple sources of data to make clinical decisions about HIV screening when patients reported no sexual or other risk behaviors. They considered information such as the quality of after-school supervision, the adolescent's developmental stage, and whether members of the adolescent's peer network were sexually active. Residents’ screening decisions were also influenced by the orientation of their preceptors toward routine screening with non-sexually active patients.
Time was not perceived to be a barrier to screening even with the mandate to obtain signed consent and provide prevention counseling that was still in effect at the clinic during the period of this study. Consent forms were available electronically and could be printed from the patient examination room, and other (non-physician) clinical staff were charged with drawing blood and conducting prevention counseling. However, physicians thought that patients declined their offers for screening owing to wait time.
DISCUSSION
The findings from this study suggest that adolescent risk for HIV, and specifically risk in the form of sexual activity, continues to be a critical determinant of physician screening practices. This stands counter to the stated objective of the CDC recommendations to remove considerations of risk from clinicians’ judgments about screening. In this regard, our findings echo those of two recent studies (Jain et al., 2009; Minniear et al., 2009) that showed that most physicians were offering tests based on assessments of risk for HIV.
Our findings diverge from the existing literature on routine screening in the explanation they suggest for the continuance of risk-based screening. Unlike previous studies, which point to physician time constraints and the need to streamline clinical practices, this study suggests that physicians, though expressing overwhelming support for the CDC recommendations, do not think of the guidelines as a prescriptive set of rules. In particular, physicians differ in their views of the appropriateness of the recommendations to adolescents who are not yet sexually active. The guidelines are one of many pieces of information they draw upon in deciding whether to offer HIV screening to this subset of the adolescent patient population.
Further, our study suggests that adolescents’ views about routine testing mirror those of their health care providers. Adolescents strongly endorse the CDC recommendations, including adolescents who have never been tested and who are not yet sexually active. Yet in the context of routine or nonemergency medical care, adolescents with no sexual history are significantly less likely than other adolescents to endorse routine screening and they are significantly less likely to accept screening when their health care providers offer it.
This study suggests that, with one important exception, routine screening is already practiced in an urban adolescent medicine clinic in a high HIV prevalence neighborhood of Baltimore. Once screening begins, the vast majority of adolescent patients are screened at least annually. However, a primary finding from this study is that a history of sexual activity is a critical trigger for initiating screening. Despite overwhelming enthusiasm for the CDC recommendations, adolescent medicine physicians diverge from them with patients with no sexual history. They do this not because they are unaware of guidelines or because of time constraints, but because they see the guidelines as inappropriate for some patients. The study findings suggest that we need more specificity in data collected on screening practices, since general endorsement of clinical practice guidelines like the CDC recommendations (attitudes) does not imply adherence to them on the part of physicians or their patients (practices). The findings also suggest that, as with other clinical practices guidelines, the CDC recommendations are likely to be used by physicians as a flexible guide to action but not as a rigid prescription.
Acknowledgments
This research was supported by the National Institute of Nursing Research Grant 1R21NR010442 and by grant 106874-42-RGAT from amfAR, the Foundation for AIDS Research. The authors thank Tia Alexander, Diane Coraggio, Darren Jackson, and Lisa Prokop for their assistance in recruiting patients and administering the patient survey. We would also like to thank the physicians and clinical staff who participated in interviews and facilitated this study.
REFERENCES
- Baiardini I, Bradio F, Bonini M, Compalati E, Canonica GW. Why do doctors and patients not follow guidelines? Current Opinion in Allergy and Clinical Immunology. 2009;9:228–233. doi: 10.1097/ACI.0b013e32832b4651. [DOI] [PubMed] [Google Scholar]
- Bernstein K, Begier E, Burke R, Karpati A, Hogben M. HIV screening among US physicians, 1999-2000. AIDS Patient Care and STDs. 2008;22(8):649–656. doi: 10.1089/apc.2007.0261. [DOI] [PubMed] [Google Scholar]
- Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, et al. Revised recommendations for HIV testing of adults, adolescents and pregnant women in health-care settings. Morbidity and Mortality Weekly Report. 2006;55:1–17. [PubMed] [Google Scholar]
- Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, Rubin HR. Why don't physicians follow clinical practice guidelines?: A framework for improvement. Journal of the American Medical Association. 1999;282(15):1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [Septemer 27, 2010];Comprehensive risk counseling and services. 2006 from http://www.cdc.gov/hiv/topics/prev_prog/CRCS/resources/CRCS_Manual/introduction.htm.
- Centers for Disease Control and Prevention . HIV/AIDS Surveillance Report, 2007. Vol. 19. U.S. Department of Health and Human Services, CDC; Atlanta, GA: 2009. [Septemer 27, 2010]. from http://www.cdc.gov/hiv/topics/surveillance/resources/reports. [Google Scholar]
- Duran D, Beltrami J, Stein R, Voetsch A, Branson B. Persons tested for HIV : United States, 2006. Morbidity and Mortality Weekly Report. 2008;57(31):845–849. [PubMed] [Google Scholar]
- Fauci A. Pathogenesis of HIV disease: Opportunities for new prevention interventions. Clinical Infectious Diseases. 2007;45:S-06–S212. doi: 10.1086/522540. [DOI] [PubMed] [Google Scholar]
- Francke AL, Smit MC, deVeer AJE, Mistiaen P. Factors influencing the implementation of clinical guidelines for health care professionals: A systematic meta-review. BMC Medical Informatics and Decision Making. 2008;8(30) doi: 10.1186/1472-6947-8-38. doi:10.1186/1472-6947-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman E, Tipton AC, Hecht L, Chesney MA. Perseverance pays off: Health care providers’ impact on HIV testing decisions by adolescent females. Pediatrics. 1994;94:878–882. [PubMed] [Google Scholar]
- Holtgrave DR, Anderson T. Utilizing HIV transmission rates to assist in prioritizing HIV prevention services. International Journal of STD and AIDS. 2004;15:789–792. doi: 10.1258/0956462042563639. [DOI] [PubMed] [Google Scholar]
- Jain C, Wyatt C, Burke R, Sepkowitz K, Begier E. Knowledge of the Centers for Disease Control and Prevention's 2006 routine HIV testing recommendations among New York City internal medicine residents. AIDS Patient Care and STDs. 2009;23(3):167–176. doi: 10.1089/apc.2008.0130. [DOI] [PubMed] [Google Scholar]
- Marks G, Crepaz N, Senterfitt W, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the Unites States: Implications for HIV prevention programs. Journal of Acquired Immune Deficiency Syndromes. 2005;39:446–453. doi: 10.1097/01.qai.0000151079.33935.79. [DOI] [PubMed] [Google Scholar]
- Minniear TD, Gilmore B, Arnold SR, Flynn PM, Knapp KM, Gaur AH. Implementation of and barriers to routine HIV screening for adolescents. Pediatrics. 2009;124:1076–1084. doi: 10.1542/peds.2009-0237. [DOI] [PubMed] [Google Scholar]
- Peralta L, Deeds B, Hipszer S, Ghalib K. Barriers and facilitators to adolescent HIV testing. AIDS Patient Care and STDs. 2007;21(6):400–408. doi: 10.1089/apc.2006.0112. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Futterman D. Promoting early detection of human immunodeficiency virus infection among adolescents. Archives of Pediatrics and Adolescent Medicine. 2000;154:435–439. doi: 10.1001/archpedi.154.5.435. [DOI] [PubMed] [Google Scholar]
- Samet J, Winter RM, Grant L, Hingson R. Factors associated with HIV testing among sexually active adolescents: A Massachusetts survey. Pediatrics. 1997;100(3):371–37. doi: 10.1542/peds.100.3.371. [DOI] [PubMed] [Google Scholar]
- Steckler A, McLeroy KR, Goodman RM, Bird ST, McCormick L. Toward integrating qualitative and quantitative methods: An introduction. Health Education Quarterly. 1992;19:1–8. doi: 10.1177/109019819201900101. [DOI] [PubMed] [Google Scholar]