Abstract
Clinical researchers have attempted many methods to translate scientific evidence into routine clinical practice, with varying success. Practice-based research networks (PBRNs) provide an important, practitioner-friendly venue to test these methods.
Dentist practitioner-investigators from “The Dental PBRN” (DPBRN) completed a detailed questionnaire about how they diagnose and treat dental caries. Next, they received a customized report that compared their answers to answers from all other practitioner-investigators. Then, 126 attended DPBRN's first network-wide meeting of practitioner-investigators from all five of its regions. Certain questions were repeated and new ones were asked about intention to change how they diagnose or treat dental caries.
Less than one-third of practitioner-investigators intended to change how they diagnose or treat caries as a result of receiving the customized report. However, as a result of the meeting, the majority of these same practitioner-investigators stated an intention to change toward a more-conservative, less surgically-invasive, approach.
These findings are consistent with the notion that the highly-interactive meeting with fellow practitioner-investigators may be an effective means to translate scientific findings into clinical practice. Practitioner-investigators are open to changing how they treat patients as a result of engaging fellow practitioner-investigators in the scientific process.
Keywords: Implementation research, practice-based research, dentistry, quality improvement, private practice
Introduction
It can take many years before clinically-important scientific evidence is incorporated into routine clinical practice, and as a result a substantial percentage of patients receives health care that is not consistent with current scientific evidence, is not needed, or is even potentially harmful.1-4 Therefore, determining how best to move recent evidence into regular practice is important, so as to ensure that it quickly reaches the patients for whom it is intended. Clinical researchers have tried many different methods to accomplish this. The most effective methods have been educational outreach done in the practice itself, reminder systems, financial incentives, and interactive educational meetings that encourage discussion and practice.5-9 Passive dissemination of materials, developing clinical guidelines, or simply attending didactic meetings generally have not been effective, and use of opinion leaders and audit and feedback approaches have had variable effectiveness.10, 11 In order for patients to receive high-quality care, the dental community should prioritize determining how best to move research results into widespread practice.
The practice-based research network (PBRN) is an important venue in which to test these methods.12 PBRNs have continued to grow in number. This is because of the unique advantages they offer both to research and quality improvement, as well as because of their ability to bring practice-relevant topics onto the research agenda and their potential to reduce the time that it takes for scientific advances to become part of daily practice.13-15 One such PBRN is “The Dental Practice-Based Research Network (DPBRN)”.16 Many details about DPBRN are publicly available at its web site,17 but briefly, it comprises practitioner-investigators and staff in outpatient dental practices from five regions: AL/MS: Alabama/Mississippi, FL/GA: Florida/Georgia, MN: dentists employed by HealthPartners Dental Group and private practitioners in Minnesota, PDA: Permanente Dental Associates, and SK: the Scandinavian countries of Denmark, Norway, and Sweden. DPBRN has a wide representation of practice types, treatment philosophies, and patient populations, including diversity with regard to the race, ethnicity, geography and rural/urban area of residence of both its practitioner-investigators and their patients. Analyses of these characteristics confirm that DPBRN dentists have much in common with dentists at large,18 while at the same time offering substantial diversity with regard to these characteristics.19 DPBRN emphasizes doing “practical science” about, in, and for the benefit of “real world” clinical practice. This means that the practitioner-investigators themselves actively participate in developing ideas for studies as well as in designing, conducting, and communicating this research - all with the intent of having a direct, practical impact on clinical practice in non-academic settings.
DPBRN holds annual regional meetings of its practitioner-investigators and has held one network-wide meeting. These meetings provide opportunities to learn about and discuss the latest results from DPBRN studies and how they might impact regular clinical practice. Additionally, practitioner-investigators design future studies, network with colleagues, and obtain continuing education credit. These meetings also provide a mechanism for practitioner-investigators to discuss the challenges of clinical practice, instilling a sense of belonging to a network that is something much larger than themselves. They also help create an acceptance of responsibility for improving one's own clinical practice, by understanding what is happening in one's own practice and in the practices of fellow DPBRN practitioner-investigators. Most presentations are done by the practitioner-investigators themselves - not academic faculty - and practitioner-investigators have reported that they are more influenced by the study results and the value of DPBRN participation when they hear presentations from practitioner-investigators themselves. This may be because academic faculty are typically held up as experts, and a tension might exist between wanting to learn from an expert but also not wanting to be told what to do, especially when there is concern that the expert does not understand “my patients” and/or “my practice”. Also, academic faculty may be seen as less credible than fellow practitioner-investigators when it comes to commenting on results from studies done in non-academic settings. When data from a large number of fellow practitioner-investigators, their practices, and their patients are collected in a scientific manner as is done in DPBRN studies, practitioner-investigators have reported informally that they are more likely to use this information and change their clinical practice.20
Instead of relying on informal and anecdotal reports, we sought to formally collect data on stated clinical practice and intention to change it. This was justified based on the role that intention has in improving clinical practice. For example, in a study of dental radiographs the authors concluded that intention may be a worthy proxy for actual clinical behavior, making it useful when evaluating an intervention before conducting a full-scale experimental trial of it.21 Therefore, the objective for this report is to test the hypothesis that participation in DPBRN activities is associated with significant changes in practitioner-investigators' stated clinical practice and intention to change it.
Methods
This study engaged DPBRN dentist practitioner-investigators on five key occasions, each of which is described below in turn: (1) an enrollment questionnaire; (2) a baseline questionnaire entitled “Assessment of Caries Diagnosis and Treatment”; (3) a mailing before DPBRN's first network-wide meeting, in which results from the baseline questionnaire were reported; (4) a questionnaire completed at the meeting's registration desk; and (5) a questionnaire completed upon leaving the meeting.
DPBRN Enrollment Questionnaire
As part of enrollment in DPBRN, all practitioner-investigators complete a 101-item Enrollment Questionnaire about their practice characteristics and themselves. This questionnaire is at http://www.dopm.uab.edu/PBRN/welcome.aspx, and the distribution of these characteristics for DPBRN dentists has been reported previously.18, 19 As of December 2008, a total of 1,204 dentists had enrolled.
Baseline Questionnaire Entitled “Assessment of Caries Diagnosis and Treatment”
All DPBRN dentist practitioner-investigators who indicated on their Enrollment Questionnaire that they do at least some restorative dentistry (n = 998) were invited to participate in this baseline questionnaire, of whom 565 did so. Methodologic particulars, such as sample selection, the recruitment process, length of the field phase, the data collection process, and procedures used during a pilot study and pre-testing of the questionnaire, have been reported previously.22 The full questionnaire, which comprised DPBRN's first study to involve all five DPBRN regions, is publicly available.23 A subset of these questions was repeated at the network-wide meeting, the content of which is detailed below.
The Mailing Before DPBRN's First Network-Wide Meeting
Forty-five days before the network-wide meeting, each practitioner-investigator who had registered for the meeting (133 persons) was mailed a summary of the results of the baseline questionnaire. This summary included results from all five DPBRN regions as well as the responses that this particular practitioner-investigator had provided for each item, such that each summary was unique to that practitioner-investigator, thereby allowing each practitioner-investigator to compare his or her individual responses to others in his or her region and to all practitioner-investigators in the network. An accompanying letter reminded the recipient of the specific aims for the questionnaire, a request to bring the packet to the meeting, and an explanation about how these results would be discussed at the meeting during “breakout sessions” (groups of 8-10 attendees). The full report and its accompanying letter are publicly available.23
Invitations to the meeting were mailed in batches according to practitioner-investigators' level of engagement in DPBRN activities to date. This included participation in the baseline questionnaire, in the first network-wide clinical study entitled study “Reasons for placements of restorations on previously un-restored surfaces”, as well as other DPBRN activities to that date.
Meeting Context
The network-wide meeting was held in Atlanta, Georgia because of its relatively central location to DPBRN's five regions and its ease of airport access, and occurred from a Thursday evening to a Saturday afternoon. The full agenda is publicly available.23 Key objectives were to: (1) provide an organized venue for collegial interaction, including discussion with colleagues from all DPBRN regions about results from the baseline questionnaire, with the goal of improving clinical practice to more closely follow the latest scientific evidence; (2) present the latest results from two DPBRN studies, both of which had to do with caries diagnosis and treatment, and which were intentionally related to the questionnaires provided at the meeting's completion; (3) present the latest evidence from the literature about caries diagnosis (dental explorer usage, Diagnodent® laser fluorescence, air drying, and magnification), prevention (fluoride usage), and treatment (when to intervene surgically on caries lesions). Discussions with colleagues not only included panel discussions with question-and-answer sessions, but also informal gatherings and formal breakout sessions in which groups of eight to 10 practitioner-investigators discussed pre-assigned topics at assigned tables. Each table was assigned to ensure that each group would have at least one practitioner-investigator from each DPBRN region. These round table discussions lasted about two hours. Each group was responsible for formally presenting its findings and conclusions to all attendees during a plenary session.
Questionnaire Completed at the Meeting's Registration Desk
Attendees were asked to complete a five-item questionnaire when they first checked in at the registration desk at the meeting. The content is evident from the results in Table 1, although the full questionnaire is publicly available.23
Table 1. Summary of responses provided at the meeting registration desk, overall and by DPBRN region.
| DPBRN region | |||||||
|---|---|---|---|---|---|---|---|
| Overall | AL/MS | FL/GA | MN | PDA | SK | Statistical significance of the association between the response and region | |
|
| |||||||
| Number of attendees | 126 | 42 | 26 | 15 | 21 | 22 | -- |
|
| |||||||
| Before the meeting, did you receive a packet that contained your results? | |||||||
| - Yes | 97% | 95% | 96% | 100% | 95% | 100% | ns |
|
| |||||||
| About how much time did you spend reviewing this packet? | |||||||
| - less than 15 minutes | 10% | 11% | 13% | -- | 16% | 5% | ns |
| - 15-30 minutes 15-30 minutes | 44% | 51% | 50% | 57% | 47% | 11% | |
| - 30 minutes to one hour | 32% | 27% | 29% | 36% | 21% | 53% | |
| - more than one hour | 14% | 11% | 8% | 7% | 16% | 32% | |
|
| |||||||
| Did you discuss these results with any other practitioner-investigators? | |||||||
| - Yes | 35% | 11% | 20% | 36% | 50% | 89% | p < 0.001 |
|
| |||||||
| As a result of considering these results, how much did you change how you diagnose dental caries? | |||||||
| - a large amount | 2% | 0% | 4% | 7% | -- | -- | ns |
| - a small amount | 28% | 28% | 38% | 29% | 20% | 20% | |
| - none | 71% | 73% | 58% | 64% | 80% | 80% | |
|
| |||||||
| As a result of considering these results, how much did you change how you treat (prevention and restoration) dental caries? | |||||||
| - a large amount | -- | -- | -- | -- | -- | -- | p = 0.038 |
| - a small amount | 27% | 18% | 46% | 43% | 25% | 14% | |
| - none | 73% | 82% | 54% | 57% | 75% | 86% | |
Column values do not add to 100% in all instances due to rounding.
the association between responses and DPBRN region was not statistically significant (p > 0.05).
Questionnaire Completed Upon Leaving the Meeting
Attendees were also asked to complete a questionnaire after the meeting ended. The content of some questions is evident in Tables 2 and 3, but certain questions require more detail because they have to do with clinical situtations. These clinical questions were in two categories: (1) diagnostic methods used by that practitioner-investigator; and (2) treatment scenarios in which practitioner-investigators stated how they would treat these hypothetical patients if they appeared in their practices. All questions were excerpted from the baseline “Assessment of Caries Diagnosis and Treatment” questionnaire and are publicly available.23 Therefore, we could compare how these practitioner-investigators responded at baseline to how they responded after the meeting was completed. The mean (S.D.) number of months between baseline and the questionnaire completed after the meeting was 20.3 (4.4), with a range from 6.1 to 26.3 months. The wide range in the number of months was only because there was substantial variation in the date on which practitioner-investigators completed the baseline questionnaire. Some practitioner-investigators enrolled in DPBRN early and some enrolled in the network as late as six months before the Atlanta meeting.
Table 2. Summary of responses provided after the meeting ended, overall and by DPBRN region.
| DPBRN region | |||||||
|---|---|---|---|---|---|---|---|
| Overall | AL/MS | FL/GA | MN | PDA | SK | Statistical significance of the association between the response and region | |
|
| |||||||
| As a result of this meeting, how much do you think that you will change how you diagnose dental caries? | |||||||
| - a large amount | 10% | 8% | 13% | 7% | 17% | 4% | p = 0.016 |
| - a small amount | 49% | 61% | 46% | 57% | 61% | 17% | |
| - none | 42% | 31% | 42% | 36% | 22% | 78% | |
|
| |||||||
| As a result of this meeting, how much do you think that you will change how you treat (prevention and restoration) dental caries? | |||||||
| - a large amount | 14% | 12% | 26% | 14% | 11% | 5% | p = 0.022 |
| - a small amount | 68% | 74% | 70% | 71% | 74% | 48% | |
| - none | 19% | 15% | 4% | 14% | 16% | 48% | |
|
| |||||||
| I liked meeting with fellow DPBRN practitioner-investigators at this meeting. | |||||||
| - strongly agree | 94% | 97% | 83% | 93% | 100% | 96% | ns |
| - agree | 6% | 3% | 17% | 7% | -- | 4% | |
| - neither agree nor disagree | -- | -- | -- | -- | -- | -- | |
| - disagree | -- | -- | -- | -- | -- | -- | |
| - strongly disagree | -- | -- | -- | -- | -- | -- | |
|
| |||||||
| Overall, the meeting was useful to my clinical practice. | |||||||
| - strongly agree | 57% | 55% | 63% | 57% | 70% | 43% | ns |
| - agree | 40% | 45% | 33% | 43% | 30% | 48% | |
| - neither agree nor disagree | 3% | -- | 4% | -- | -- | 9% | |
| - disagree | -- | -- | -- | -- | -- | -- | |
| - strongly disagree | -- | -- | -- | -- | -- | -- | |
|
| |||||||
| Attending this meeting increased my interest in participating in future DPBRN studies. | |||||||
| - strongly agree | 82% | 84% | 83% | 64% | 90% | 83% | ns |
| - agree | 15% | 13% | 13% | 29% | 10% | 17% | |
| - neither agree nor disagree | 3% | 3% | 4% | 7% | -- | -- | |
| - disagree | -- | -- | -- | -- | -- | -- | |
| - strongly disagree | -- | -- | -- | -- | -- | -- | |
Column values do not add to 100% in all instances due to rounding.
the association between responses and DPBRN region was not statistically significant (p > 0.05).
p < 0.05
Table 3. Comparison of individual baseline responses to the clinical questions to responses after the meeting to these same clinical questions.
| Response was more conservative after the meeting | Response was the same after the meeting | Response was less conservative after the meeting | Statistical significance (p value) | |
|---|---|---|---|---|
| Diagnostic methods a | ||||
| When you examine patients to determine if they have a primary occlusal caries lesion, on what percent of these patients do you use a dental explorer to help diagnose the lesion? b | 39% | 48% | 13% | p = 0.002 |
| Treatment scenarios | ||||
| Defective composite restoration with cementum-dentin margins c | 35% | 56% | 9% | p < 0.001 |
| Defective composite restoration with enamel margins c | 30% | 61% | 9% | p = 0.006 |
| Defective amalgam restoration c | 29% | 63% | 8% | p = 0.001 |
| Occlusal caries scenario 1 d | 11% | 88% | 1% | p = 0.002 |
| Occlusal caries scenario 2 d | 34% | 65% | 1% | p < 0.001 |
| Occlusal caries scenario 3 d | 38% | 51% | 11% | p = 0.001 |
| Proximal caries scenario e | 24% | 68% | 8% | p = 0.079 |
These diagnostic methods were also queried, but the differences in reported usage between baseline and after the meeting were not statistically significant (p > 0.05): (1) When you examine patients to determine if they have a primary caries lesion on the occlusal surface, on what percent of these patients do you use laser fluorescence (for example, Diagnodent®)?; (2) When you examine patients to determine if they have a primary caries lesion, on what percent of these patients do you use air-drying to help diagnose the lesion?; (3) When you examine patients to determine if they have a caries lesion on a proximal (mesial or distal) surface of an anterior tooth, on what percent of these patients do you use fiberoptic trans-illumination to help diagnose the lesion?; (4) When you examine patients to determine if they have a caries lesion, on what percent of these patients do you use some sort of magnification to help diagnose the lesion?; (5) Do you assess caries risk for individual patients in any way?
Response categories were: (1) never, or 0%; (2) 1% - 24%; (3) 25% - 49%; (4) 50% - 74%; (5) 75% - 99%; and (6) every time or 100%. A “more-conservative” response meant moving to a category with a lower number after having provided at baseline a response of a higher category. A “less-conservative” response meant moving to a category with a higher number after having provided at baseline a response of a lower category.
Response categories were: (1) no treatment or preventive treatment only; (2) polish, re-surface, or repair the restoration; and (3) replace the entire restoration. A “more-conservative” response meant moving to a category 1 response after having provided at baseline a response of category 2 or 3; or to a category 2 response after having provided at baseline a response of category 3. A “less-conservative” response meant moving to a category 3 response after having provided at baseline a response of category 1 or 2; or to a category 2 response after having provided at baseline a response of category 1.
Response categories were: (1) no treatment or preventive treatment only; (2) minimal intervention; and (3) complete restoration. A “more-conservative” response meant moving to a category 1 response after having provided at baseline a response of category 2 or 3; or to a category 2 response after having provided at baseline a response of category 3. A “less-conservative” response meant moving to a category 3 response after having provided at baseline a response of category 1 or 2; or to a category 2 response after having provided at baseline a response of category 1.
Response categories were to intervene surgically (i.e., restore the tooth) at this caries lesion depth: (1) outer half of enamel; (2) inner half of enamel; (3) outer one-third of dentin; (4) middle one-third of dentin; (5) inner one-third of dentin. A “more-conservative” response meant moving to a category with a lower number after having provided at baseline a category with a higher number. A “less-conservative” response meant moving to a category with a higher number after having provided at baseline a category with a lower number.
Questions about diagnostic methods
The first five of these questions asked about the frequency with which dentists reported using several diagnostic methods on the patients in their practices: (1) the dental explorer for primary occlusal caries; (2) laser fluorescence for primary occlusal caries; (3) air-drying for primary caries; (4) fiber-optic trans-illumination for proximal caries; and (5) magnification. The next question asked if the practitioner-investigator assessed caries risk for individual patients in any way, to which a ‘yes’ or ‘no’ response was provided, and if ‘yes’ was the response, whether or not a special form was used.
Questions about treatment scenarios
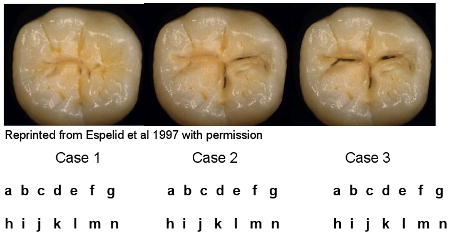
The next three questions were based on high-resolution photographs of various defective restorations accompanied by case descriptions. The first case had a defective composite restoration with cementum-dentin margins and a description of a patient who had been a regular dental patient and who had existing dental restorations. A second case had a defective composite restoration with enamel margins and a description of a patient at low caries risk. A third case had a defective amalgam restoration and a description of the same patient at low caries risk. Attendees were asked what type of treatment they would recommend to the patient if that patient appeared in their practices. The nine treatment options that were provided ranged from no treatment to replacement of the entire restoration. We categorized these nine treatment options into three categories: (1) no treatment or preventive treatment only; (2) polish, re-surface, or repair the restoration (as one provided choice); and (3) replace the entire restoration.
The next question involved clinical images of increasingly severe occlusal caries. Responses were again divided into three ordinal categories, by highest degree of clinical intervention recommended: (1) no treatment or preventive treatment only; (2) minimal intervention; and (3) complete restoration. The options for minimal intervention included: minimal drilling with sealant; minimal drilling with preventive resin restoration; air abrasion with a sealant; and air abrasion with preventive resin restoration. The options for complete restoration were amalgam restoration, composite restoration, and indirect restoration.
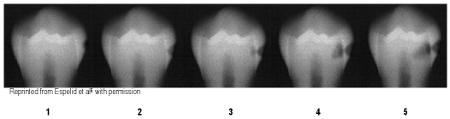
The next question involved five radiographic images of a caries lesion of increasing depth located in the interproximal surface of a mandibular premolar (outer half of enamel; inner half of enamel; outer one-third of dentin; middle one-third of dentin; inner one-third of dentin). Attendees were asked to indicate which image corresponded to the lesion depth at which they would recommend doing a permanent restoration rather than only preventive therapy.
Statistical Methods
All analyses were done using SAS.24 In addition to quantifying frequency distributions, we also cross-tabulated responses by DPBRN region to test for significant differences. When responses were on a binary scale, χ2 tests were used. When they were on an ordinal scale, Mantel-Haenszel χ2 trend tests were done. In Table 3, we cross-tabulated responses to the clinical questions from the baseline questionnaire with responses to the same questions repeated after the meeting had ended. McNemar's test and Bowker's test of symmetry25 were used to determine whether patterns of change in response were statistically significant for dichotomous and ordinal responses, respectively. Tests were done using the extended ordinal categories listed in the notes in Table 3, not using the more-conservative-to-less-conservative scale that summarizes the responses in Table 3. Statistical significance was assumed for a p-value less than 0.05. It is important to note that these statistics do not depend on the proportion of respondents whose answers change. Instead, they quantify whether they are more likely to change in one direction than another. Bowker's statistic generalizes McNemar's to cases where there are more than two response choices. It tests whether - among those whose answers changed - the direction of change was symmetrical. For example, did responses change from 2 to 3 as often as they changed from 3 to 2?
Results
Responses provided at the meeting registration desk
A total of 126 practitioner-investigators attended, all of whom completed this questionnaire (Table 1). At least 95% of the attendees from each region reported having received the report that compared their individual responses from the baseline questionnaire to other DPBRN dentists. The time spent reviewing the report varied widely. There was also considerable variability in the proportion who reported having discussed this individualized report before the meeting with their colleagues, and this varied significantly by DPBRN region.
A total of 30% said that as a result of considering these individualized results, that they have changed how they diagnose dental caries. This percentage did not significantly vary by DPBRN region. A similar percentage (27%) said that they would change how they treat dental caries, but this percentage did significantly vary by region, with practitioner-investigators from the FL/GA and MN regions reporting the highest percentages.
Post-meeting responses
Table 2 shows responses to the post-meeting questionnaire. Most (59%) practitioner-investigators said that as a result of the meeting, they will change how they diagnose dental caries. The percentage for change in treatment of caries was even higher (82%). The percentages for both diagnosis and treatment varied significantly by DPBRN region.
Table 2 also shows responses to three questions used to evaluate the effectiveness of the meeting. All practitioner-investigators liked meeting with fellow DPBRN practitioner-investigators. A total of 97% either agreed or strongly agreed with the statement that the meeting was useful to clinical practice, and 97% felt that the meeting increased their interest in participating in future DPBRN studies. None of the responses to these three questions varied significantly by DPBRN region.
Comparison of baseline and post-meeting responses to clinical questions
Diagnostic methods
Table 3 shows results of comparing responses to clinical questions at baseline with those reported after the meeting. Of the six questions about diagnostic methods, one significantly differed between these two time points: use of a dental explorer. The change was toward a more-conservative approach, meaning that the explorer would be used on a smaller percentage of patients.
Treatment scenarios
Table 3 also shows results of comparing responses to the seven treatment scenarios at baseline with those reported after the meeting. A statistically significant change toward a more-conservative approach was evident in six of the seven scenarios.
Discussion
These findings are consistent with the informal reports that DPBRN practitioner-investigators had provided about the effectiveness of collegial interaction in changing clinical practice. The responses provided at the meeting registration desk suggest that only a minority (less than one-third) had any intention to change diagnosis or treatment based only on comparing how they diagnose and treat dental caries as an individual practitioner-investigator to how other practitioner-investigators do so. However, as a result of the meeting, the majority of these same practitioner-investigators stated an intention to change both diagnosis and treatment in some manner, and thereby had taken the next step toward implementing change and translating the latest scientific evidence into regular clinical practice. This movement from no stated intention to a stated intention is consistent with health change theory that suggests that movement to this “next step” is a prelude to the subsequent “next step” of actual implementation of change.26, 27
These findings are consistent with implementation theory and with literature about implementation methods used with other health care professionals. A change in knowledge about the latest evidence is necessary for change, but not sufficient.28 This is why passive dissemination of materials, developing clinical guidelines, or simply attending didactic meetings generally have not been effective.10 Interventions that target other barriers to change have a larger impact. These include interventions that take into account the context of the individual practice, such as that practice's patients and the constraints and incentives due to its particular financial and health care system circumstance.9, 29 This is why the PBRN research context might be especially useful – because practitioner-investigators are considering data from their own practices and are listening to views about these data from other practitioner-investigators who share many of the same constraints, incentives, and motivations. That is, participating in the PBRN activities may create an openness to change and fellow practitioner-investigators can themselves act as change agents. In the context of the DPBRN meeting, those who were most “eligible” to act as change agents were those who had already incorporated the more-conservative approaches to caries diagnosis and treatment, given that the more-conservative approach is the one supported by the scientific evidence. Additionally, these meetings encourage collegial interaction among peers and generation of ideas for new studies, activities which themselves may help speed translation of evidence into regular practice. Because this first investigation shows promise, further systematic investigations are warranted - investigations into which methods work best and in the most practical manner.
Study designs exist on a continuum of inferential power.30 At the highest end of the spectrum lies the one with the greatest rigor, the well-done double-masked randomized clinical trial. The design of the current study is toward the other end of that spectrum. This study did increase scientific inferential power by moving from informal anecdotal reports to collection of data from many practitioner-investigators, and by collecting these data in a standardized manner. Although we would like to include all DPBRN practitioner-investigators (not just the ones who attended the meeting) to answer the questionnaire about diagnostic and treatment scenarios, the study did benefit by having a “before/after” design in which responses from before the meeting were compared to those after the meeting - on the same individuals. Furthermore, the changes observed were in the expected direction: toward a more-conservative approach, the approach that is supported by the latest scientific evidence. “More-conservative” is defined in this context using the definitions stated in Table 3; namely, providing minimal, preventive, or no intervention, in contrast to doing a surgical/restorative intervention. Therefore, we can say that if the method of having a highly-interactive meeting that encourages frank discussion in a collegial setting - such as the one that we held - is effective in moving evidence into regular clinical practice, then the results we observed are consistent with that, although not conclusive of it. The fact that this change in intention was also associated with change in stated clinical practice (i.e., the questions about how you would diagnose and treat patients in your practice now) is also consistent with the conclusion that this method is effective. Appropriate next steps would be to query all DPBRN practitioner-investigators (not just the ones who attended the meeting), followed by a single-masked randomized trial to test the effectiveness of this translation-to-practice strategy.
Acknowledgments
This investigation was supported by NIH grants DE-16746 and DE-16747. We are grateful to James D. Bader, DDS, MPH of the University of North Carolina at Chapel Hill, DPBRN faculty investigator, for his comments on an earlier version of this manuscript. Persons who comprise the DPBRN Collaborative Group are listed at http://www.DPBRN.org/users/publications. Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health. The informed consent of all human subjects who participated in this investigation was obtained after the nature of the procedures had been explained fully.
Appendix 1: Treatment scenarios asked at baseline and after the meeting
[these are the first three treatment scenarios listed in Table 3 of the manuscript]
|
| ||||
| Please use the following guide for the treatment codes used in scenarios 1-3. For each question, circle the letters which correspond to the treatment codes you would choose for scenarios described. You may circle more than one treatment code per question. | ||||
|
| ||||
| Scenario 1 | Scenario 2 | Scenario 3 | ||
| a. | No treatment today, follow the patient regularly | a | a | a |
| b. | Instruct patient in plaque removal for the affected area | b | b | b |
| c. | In-office fluoride | c | c | c |
| d. | Prescription for fluoride | d | d | d |
| e. | Recommend non-prescription fluoride | e | e | e |
| f. | Use sealant or unfilled resin over tooth | f | f | f |
| g. | Chlorhexidine treatment | g | g | g |
| h. | Polish, re-surface, or repair restoration, but not replace | h | h | h |
| i. | Replace entire restoration | i | i | i |
|
| ||||
-
Imagine that the patient is a 30-year old female with no relevant medical history. She has no complaints and is in your office today for a routine visit. She has been attending your practice once every two years on a regular basis for the past 6 years. She has 5 existing restorations, and is not missing any teeth. Indicate what treatment you would provide to the restoration shown by the arrow in the first picture on the left. Please circle your answers above.
 Reprinted from Mjör, 2005,41 with permission
Reprinted from Mjör, 2005,41 with permission -
Now imagine the patient has no other dental restorations or dental caries and is not missing any teeth. Indicate what treatment you would provide to the restoration in the second picture on the left. Please circle your answers above.
 Reprinted from Mjör and Toffenetii, 2000,43 with permission
Reprinted from Mjör and Toffenetii, 2000,43 with permission -
Continue to imagine the patient has no other dental restorations or dental caries and is not missing any teeth. Indicate what treatment you would provide to the restoration in the third picture on the left. Please circle your answers above.
 Courtesy of Dr. Ivar Mjör
Courtesy of Dr. Ivar Mjör
Appendix 2: Treatment scenarios asked at baseline and after the meeting
[these are the next three treatment scenarios listed in Table 3 of the manuscript – labeled as “Occlusal caries scenarios”]
|
| ||||
| SECTION 4: Please use the following guide for the treatment codes used in question 15. For each question, circle the letters which correspond to the treatment codes you would recommend for each of the five cases. If treatment code “n” (other) is used, please specify. You may circle more than one treatment code per case. | ||||
|
| ||||
| ||||
|
| ||||
The patient is a 30 year old female with no relevant medical history. She has no complaints and is in your office today for a routine visit. She has been attending your practice on a regular basis for the past 6 years.
15. Indicate how you would treat the tooth shown if the patient has no other teeth with dental restorations or dental caries and is not missing any teeth.
Appendix 3: Treatment scenarios asked at baseline and after the meeting
[this is the next treatment scenario listed in Table 3 of the manuscript – labeled as “Proximal caries scenario”]
Please circle the one number that corresponds to the lesion depth at which you think it is best to do a permanent restoration (composite, amalgam, etc.) instead of doing preventive therapy.
The patient is a 30-year old female with no relevant medical history. She has no complaints and is in your office today for a routine visit. She has been attending your practice on a regular basis for the past 6 years.
The patient has no dental restorations, no dental caries, and is not missing any teeth.
References
- 1.Agency for Healthcare Research and Quality. U.S. Department of Health and Human Services. National Healthcare Quality Report. [Accessed July 26, 2009];2007 AHRQ Publication No. 08-0040. Available at: “ www.ahrq.gov/qual/measurix.htm#quality”.
- 2.Asch SM, Kerr EA, Keesey J, Adams JL, Setodji CM, Malik S, McGlynn EA. Who is at greatest risk for receiving poor-quality health care? New Engl J Med. 2006;354(11):1147–1156. doi: 10.1056/NEJMsa044464. [DOI] [PubMed] [Google Scholar]
- 3.Schuster MA, McGlynn EA, Brook RH. How good is the quality of health care in the United States? Milbank Quart. 2005;83(4):843–895. doi: 10.1111/j.1468-0009.2005.00403.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hujoel P. Converting science into art: the challenge of the translationists. J Evid Based Dent Pract. 2008;(3):176–180. doi: 10.1016/j.jebdp.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 5.O'Brien MA, Rogers S, Jamtvedt G, Oxman AD, Odgaard-Jensen J, Kristoffersen DT, Forsetlund L, Bainbridge D, Freemantle N, Davis D, Haynes RB, Harvey E. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database Systematic Rev. 2007;(4) doi: 10.1002/14651858.CD000409.pub2. Art. No.: CD000409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O'Brien MA, Freemantle N, Oxman AD, Wolf F, Davis DA, Herrin J. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Systematic Rev. 2001;(1) doi: 10.1002/14651858.CD003030. Art. No.: CD003030. [DOI] [PubMed] [Google Scholar]
- 7.Chaix-Couturier C, Durand-Zaleksi I, Jolly D, Durieux P. Effects of financial incentives on medical practice: results from a systematic review of the literature and methodologic issues. Int J Qual Health Care. 2000;12(2):133–142. doi: 10.1093/intqhc/12.2.133. [DOI] [PubMed] [Google Scholar]
- 8.Clarkson JE, Turner S, Grimshaw JM, Ramsay CR, Johnston M, Scott A, Bonetti D, Tilley CJ, Maclennan G, Ibbetson R, MacPherson LMD, Pitts NB. Changing clinicians' behavior: a randomized controlled trial of fees and education. J Dent Res. 2008;87(7):640–644. doi: 10.1177/154405910808700701. [DOI] [PubMed] [Google Scholar]
- 9.McGlone P, Watt R, Sheiham A. Evidence-based dentistry: an overview of the challenges in changing clinical practice. Brit Den J. 2001;190(12):636–639. doi: 10.1038/sj.bdj.4801062. [DOI] [PubMed] [Google Scholar]
- 10.Farmer AP, Légaré F, Turcot L, Grimshaw J, Harvey E, McGowan JL, Wolf F. Printed educational materials: effects on professional practice and health care outcomes. Cochrane Database Systematic Rev. 2008;(3) doi: 10.1002/14651858.CD004398.pub2. Art. No.: CD004398. [DOI] [PubMed] [Google Scholar]
- 11.Jamtvedt G, Young JM, Kristoffersen DT, O'Brien MA, Oxman AD. Audit and feedback: effects on professional practice and health care outcomes. Cochrane Database Systematic Rev. 2006;(2) doi: 10.1002/14651858.CD000259.pub2. Art. No.: CD000259. [DOI] [PubMed] [Google Scholar]
- 12.Genel M, Dobs A. Translating clinical research into practice: practice-based research networks, a promising solution. J Invest Med. 2003;51(2):64–71. doi: 10.1136/jim-51-02-07. [DOI] [PubMed] [Google Scholar]
- 13.Westfall JM, Mold J, Fagnan L. Practice-based research: ‘blue highways’ on the NIH Roadmap. JAMA. 2007;297(4):403–406. doi: 10.1001/jama.297.4.403. [DOI] [PubMed] [Google Scholar]
- 14.Mold JW, Peterson KA. Primary care practice-based research networks: working at the interface between research and quality improvement. Ann Fam Med. 2005;3(supplement 1):S12–S20. doi: 10.1370/afm.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lindbloom EJ, Ewigman BG, Hickner JM. Practice-based research networks: the laboratories of primary care research. Med Care. 2004;42:III45–III49. [PubMed] [Google Scholar]
- 16.Gilbert GH, Williams OD, Rindal DB, Pihlstrom DJ, Benjamin PL, Wallace MA DPBRN Collaborative Group. The creation and development of The Dental Practice-Based Research Network. J Am Dent Assoc. 2008;139(1):74–81. doi: 10.14219/jada.archive.2008.0024. [DOI] [PubMed] [Google Scholar]
- 17.Dental Practice-Based Research Network. [July 26, 2009]; Available at: “ www.dentalpbrn.org”.
- 18.Makhija SK, Gilbert GH, Rindal DB, Benjamin PL, Richman JS, Pihlstrom DJ, Qvist V DPBRN Collaborative Group. Dentists in practice-based research networks have much in common with dentists at large: evidence from The Dental PBRN. Gen Dent 2009. 2009;57(3):270–275. [PMC free article] [PubMed] [Google Scholar]
- 19.Makhija SK, Gilbert GH, Rindal DB, Benjamin PL, Richman JS, Pihlstrom DJ, Qvist V DPBRN Collaborative Group. Practices participating in a dental PBRN have substantial and advantageous diversity even though as a group they have much in common with dentists at large. doi: 10.1186/1472-6831-9-26. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dental Practice-Based Research Network. [Accessed July 26, 2009];Testimonials. Available at “ www.dpbrn.org/users/Testimonials/Default.asp”.
- 21.Bonetti D, Pitts NB, Eccles M, Grimshaw J, Johnston M, Steen N, Glidewell L, Thomas R, Maclennan G, Clarkson JE, Walker A. Applying psychological theory to evidence-based clinical practice: identifying factors predictive of taking intra-oral radiographs. Soc Sci Med. 2006;63(7):1889–1899. doi: 10.1016/j.socscimed.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 22.Riley JL, III, Qvist V, Fellows JL, Rindal DB, Richman JS, Gilbert GH, Gordan VV DPBRN Collaborative Group. Dentists' use of caries risk assessment in children: findings from The Dental PBRN. Gen Dent. 2009 accepted for publication. [PMC free article] [PubMed] [Google Scholar]
- 23.Dental Practice-Based Research Network. [Accessed July 26, 2009];Supplements to specific DPBRN publications. Available at: “ www.dentalpbrn.org/users/publications/Supplement.aspx”.
- 24.SAS Institute Inc. SAS Publishing; Cary, NC: 2006. [Accessed July 26, 2009]. SAS/STAT version 9.1. Available at: “ www.sas.com/apps/pubscat/complete.jsp”. [Google Scholar]
- 25.Bishop YMM, Fienberg SE, Holland PW. Discrete Multivariate Analysis. Cambridge: MIT Press; 1975. p. 283. [Google Scholar]
- 26.Painter JE, Borba CPC, Hynes M, Mays D, Glanz K. The use of theory in health behavior research from 2000 to 2005: a systematic review. Annals Behav Med. 2008;35(3):358–362. doi: 10.1007/s12160-008-9042-y. [DOI] [PubMed] [Google Scholar]
- 27.Prochaska JO. Decision making in the transtheoretical model of behavior change. Med Decis Making. 2008;28(6):845–849. doi: 10.1177/0272989X08327068. [DOI] [PubMed] [Google Scholar]
- 28.Rohrbach LA, Grana R, Sussman S, Valente TW. Type II translation: transporting prevention interventions from research to real-world settings. Eval Health Prof. 2006;29(3):302–333. doi: 10.1177/0163278706290408. [DOI] [PubMed] [Google Scholar]
- 29.Crabtree BF, Miller WL, Tallia AF, Cohen DJ, DiCicco-Bloom B, McIlvain HE, Aita VA, Scott JG, Gregory PB, Stange KC, McDaniel RR., Jr Delivery of clinical preventive services in family medicine offices. Ann Fam Med. 2005;3(5):430–435. doi: 10.1370/afm.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Editorial Board. Levels of evidence. J Evidence Based Dent Pract. 2007;7(4):4A–5A. [Google Scholar]


