Abstract
A 5-year-old girl presented with a 3-day history of pain and distension of abdomen, bilious vomiting, bleeding per rectum and a hard lump in the left iliac fossa. Intussusception was clinically diagnosed. On exploratory laparotomy, trichobezoar showing cast of the stomach, duodenal C-loop and tail were extracted. The stomach cast was impacted at the distal ileum, while its tail traversed the ileum, ileocecal valve and extended up to the hepatic flexor. At the site of impaction, a large ileal perforation, covered by bezoar was present. Hence, x-ray did not reveal pneumoperitoneum. There was no evidence of trichobezoar in the stomach. Perforation was exteriorised as loop ileostomy. She was of normal intelligence. Psychological evaluation of the child was performed and a behaviour therapy was advocated. Ileostomy closure was done after 2 months. At 6 months follow-up, no recurrence was found.
Background
Trichobezoar are usually found in the stomach presenting as epigastric discomfort, early satiety, anaemia and malnutrition with epigastric lump.1 2 Small bowel obstruction (SBO) rarely occurs because of primarily formed phytobezoar, as a result of stasis or in the diverticula, or daughter balls formed by endoscopic fragmentation of trichobezoar.2 We herein report a unique case, yet to be found in the literature, in which the entire trichobezoar migrated en bloc from the stomach to the terminal ileum. There was no residual bezoar in the stomach or proximal bowel. The child’s clinical presentation mimics intussusception because the classical triad of pain in abdomen, lump in abdomen and bleeding per rectum was present along with the features of SBO. It was only after exploratory laparotomy that we came with the diagnosis of a complicated Rapunzel syndrome. On extensive search of the literature, we found that the youngest child who presented with trichobezoar was a 5-year-old girl, the same age at that of our patient, but was mentally retarded.3
Case presentation
A 5-year-old girl was admitted to the Department of Pediatric Surgery, Chhatrapati Shahuji Maharaj Medical University, Lucknow, Uttar Pradesh, India, with complaints of bilious vomiting, abdominal pain and distension, absolute constipation and maroon bleeding per rectum for 3 days. Three months before she had suffered from non-bilious vomiting, epigastric pain and a swelling in the epigastrium, which were managed conservatively at a peripheral hospital. She was relieved of symptoms with a disappearance of the epigastric swelling, but no further investigations were done for the lump at that time. Since then, she had had episodes of mild abdominal pain but her parents did not consult a doctor for the condition.
On examination, the child had grade ΙΙ malnutrition (Indian Academy of Pediatrics),4 and was anaemic and dehydrated. Her respiratory rate was 30/min and pulse rate was 140 per minute. The abdomen was distended, and bowel sounds were absent. An intra-abdominal non-tender, smooth, rounded, hard lump of 15×6 cm size was present in the left iliac fossa. The lump was slightly mobile in both its axis. Its lower margin was reachable. Per rectal and bimanual examination done to rule out ovarian pathology or tumours of the sacrum, which can present with lower abdominal lump compressive symptoms on bowel and bowel infiltration as bleeding per rectum, it was revealed that the lump was separate from internal genitalia and sacrum. The examining finger on removal was tinged with blood.
Investigations
Blood investigations showed anaemia and electrolyte imbalance. Erect abdominal x-ray suggested SBO. Bed-side ultrasonography showed an intraluminal hyperechoic mass sized 20×8 cm with arch-like surface and marked posterior acoustic shadow present in the left iliac fossa. There were no pressure effects.
Differential diagnosis
-
▶
Intussusception.
Treatment
After adequate resuscitation and electrolyte correction, emergency laparotomy was undertaken under general anaesthesia. A 2×2 cm sized ileal perforation of unhealthy margins was present 2 feet proximal to ileocecal junction. Through the perforation, a slimy, glistening, putrid, black, hard mass was visible inside the lumen. The perforation was sealed by the impacted mass. Perforation was probably due to pressure necrosis by hard bezoar (figure 1). The proximal bowel was dilated. A 20×10×6 cm sized mass was impacted in the ileum 2.5 feet proximal to ileocecal junction, while its tail was extended through the ileocecal valve up to hepatic flexure. The mass was found to be trichobezoar. Whole trichobezoar with its tail was extracted en bloc through the perforation (figure 2). The stomach and rest of the small bowel were free from any associated trichobezoar. The extracted bezoar was composed of hair, threads and long strings. It had a cast of stomach-sized 20×10×6 cm, duodenal bulb, C-loop of duodenum and a long tail of 70 cm with a weight of 300 g (figure 3). Because of the poor general condition of the child, the perforation was exteriorised as loop ileostomy.
Figure 1.
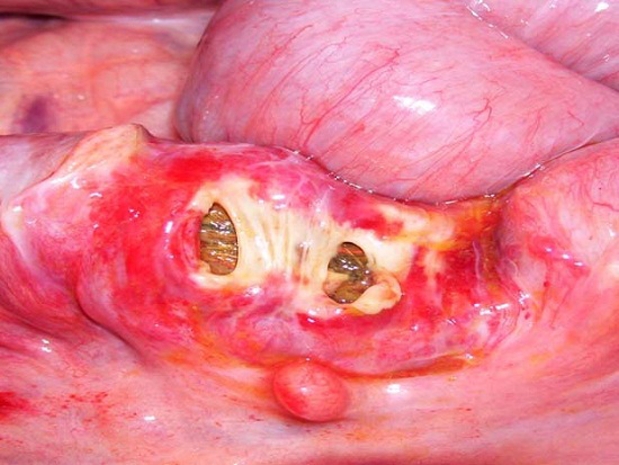
Covered perforation showing trichobezoar through perforation.
Figure 2.

En bloc extraction of trichobezoar with its tail.
Figure 3.

Whole tricobezoar showing stomach cast, duodenal cap, C-loop of duodenum and long tail.
Outcome and follow-up
Postoperative period was normal. To find out the cause, retrograde questionnaires from parents and child regarding history of poor school performance, emotional deprivation, trichotillomania or trichophagia were analysed. The child was assessed for IQ, which was 62. The child was discharged on the sixth postoperative day with proper advice for behaviour therapy and to overcome malnutrition. Parents were counselled for child care. During follow-up, there were no new complaints and the child gained weight as well. Ileostomy closure was done after 2 months. After a 6-month follow-up, the child was healthy with no recurrence.
Discussion
The word bezoar means ‘antidote’ and is derived from the Arabic word ‘bedzehr’ or the Persian word ‘pedzhar’, which means ‘protecting against poison’.5 Eighty per cent of trichobezoar occurs in females younger than 30 years of age.1 Only 10% of cases are seen in mentally retarded patients or in those with a psychiatric disorder (trichotillomania, trichophagia, child abuse, pica, obsessive compulsive disorder, depression and anorexia nervosa).1 6 Conversely, only 1% of patients with trichotillomania and trichophagia will develop trichobezoar.5
Trichobezoar are putrefied (sometimes causing halitosis), slimy and shiny black coloured (due to oxidative effect of gastric acid).3 Most common presentations are dull epigastric pain, anorexia, anaemia and vomiting, with a firm mobile epigastric lump.1 2 The primary site of trichobezoar formation is the stomach, where it usually forms a perfect cast of the stomach.1 2 5 6 Trichobezoar found in the small bowel are either extensions of gastric bezoar (known as Rapunzel syndrome) or due to daughter balls formed spontaneously. They may also be due to endoscopic/extracorporeal shock wave/enzymatic treatment of gastric trichobezoar.2 7–10
Complications arising due to trichobezoar are gastrointestinal bleeding and obstruction. Other rare complications reported are intussusceptions, obstructive jaundice and protein-losing enteropathy or even death.1 5 6 Rarely concealed intestinal perforation occurs due to pressure necrosis by impacted bezoar (the same as our patient), in which case, an x-ray will not show pneumoperitoneum.11
Our patient had a history of epigastric pain, vomiting and epigastric lump 4 months ago as the bezoar was present in the stomach at that time. Because the treating physician was unaware of this possibility, the child was not investigated further for the epigastric lump. The unusual picture when the child presented to us were the clinical features suggestive of intussusception with acute onset SBO, haematochazia and an intra-abdominal left iliac fossa lump. Erect abdominal x-ray did not reveal any pneumoperitoneum despite the presence of a large ileal perforation because the perforation site was covered by bezoar. This feature was supported by the fact that pneumoperitoneum is usually present in only 75% of perforation.11 12 Contrast-enhanced CT of the abdomen was not done because of poor general condition of the patient; instead, bed-side abdominal ultrasound was carried out.7 8
On extensive literature search, the youngest child reported with a bezoar was of the same age as our patient (5 years), but she was mentally retarded. In addition, our case is also unusual as distal SBO occurred due to dislodgement of entire gastric trichobezoar with its tail and not due to daughter balls. Few similar cases of SBO or perforation were reported in the literature but in none of these cases had migration of entire trichobezoar occurred.3 12
Learning points.
-
▶
Females, irrespective of being adults or children, presenting with intestinal obstruction should be suspected of having trichobezoar in the differential diagnosis.
-
▶
It is not necessary to find out the history of trichotillomania and trichophagia in all cases of trichobezoar.
-
▶
Trichobezoar can also present as distal SBO instead of gastric outlet obstruction.
-
▶
Rare complication of the Rapunzel syndrome can be its distal migration.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Cheshire NJ, Glazer G. Diverticula’s, volvulous, superior mesenteric artery syndrome and foreign bodies. In: Zinner MJ, Schwartz SI, Ashley SW, Ellis H, Mc Fadden DW, eds. Maingot’s Abdominal Operations. 10th edition. New York: Appleton and Lange Publication; 1994:913–37 [Google Scholar]
- 2.Chojnacki KA. Foreign body and bezoar of stomach and small intestine. In: Yeo CJ, Dempsy DT, Klein AS, Pemberton JH, Peter JH, eds. Shackelford’s Surgery of Alimentary Track. Philadelphia, PA: Elsevier Saunders; 2007:940–6 [Google Scholar]
- 3.Quintana JF, Walker RN, McGeehan A. Child with small bowel obstruction and perforation secondary to ileal bezoar. Pediatr Emerg Care 2008;24:99–101 [DOI] [PubMed] [Google Scholar]
- 4.Bhan MK, Bhandari N, Bahl R. Management of the severely malnourished child: perspective from developing countries. BMJ 2003;326:146–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gonuguntla V, Joshi DD. Rapunzel syndrome: a comprehensive review of an unusual case of trichobezoar. Clin Med Res 2009;7:99–102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gorter RR, Kneepkens CM, Mattens EC, et al. Management of trichobezoar: case report and literature review. Pediatr Surg Int 2010;26:457–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ho TW, Koh DC. Small-bowel obstruction secondary to bezoar impaction: a diagnostic dilemma. World J Surg 2007;31:1072–80 [DOI] [PubMed] [Google Scholar]
- 8.Salim AS. Small bowel obstruction with multiple perforations due to enterolith (bezoar) formed without gastrointestinal pathology. Postgrad Med J 1990;66:872–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benes J, Chmel J, Jodl J, et al. Treatment of a gastric bezoar by extracorporeal shock wave lithotripsy. Endoscopy 1991;23:346–8 [DOI] [PubMed] [Google Scholar]
- 10.Nomura H, Kitamura T, Takahashi Y, et al. Small-bowel obstruction during enzymatic treatment of gastric bezoar. Endoscopy 1997;29:424–6 [DOI] [PubMed] [Google Scholar]
- 11.Hiyama DT, Bennion R. Peritonitis and intraperitoneal abscess. In: Zinner MJ, Schwartz SI, Ashley SW, Ellis H, Mc Fadden DW, eds. Maingot’s Abdominal Operations. 10th edition New York: Appleton and Lange Publication; 1994:633–54 [Google Scholar]
- 12.Sharma V, Sharma ID. Intestinal trichobezoar with perforation in a child. J Pediatr Surg 1992;27:518–19 [DOI] [PubMed] [Google Scholar]


